Abstract
Ayahuasca is a traditional psychoactive sacrament that's been used in Amazonian shamanic rituals for hundreds of years. Ayahuasca is notorious for its psychedelic properties produced from the combination of monoamine oxidase inhibitors (MAOIs) found in the Banisteriopsis caapi vine and N-N-dimethyltryptamine from Psychotria viridis or Diplopterys cabrerana. Recently, ritual use of ayahuasca has increased and garnered attention for its potential in treating mental illnesses, such as substance use and depressive disorders. Due to its MAOI properties, there are serious drug interactions that may be of concern among patients who participate in ayahuasca use. The objectives of this paper are to describe ayahuasca's pharmacology, potential drug interactions, and clinical data for its treatment potential in psychiatric illness.
Keywords: ayahuasca, monoamine oxidase, dimethyltryptamine, sacrament, harmine
Background
Psychedelic plant medicines, such as psilocybin-containing mushrooms, mescaline-containing San Pedro and Peyote cacti, and N-N-dimethyltryptamine (DMT) decoctions collectively termed ayahuasca, have been used for thousands of years as ritual sacraments. Recently, there's been renewed interest in psychedelics as a treatment for psychiatric illnesses, including depression and substance use disorders.1
Ayahuasca is used in shamanic ceremonies by indigenous peoples of the Amazon.2 Ceremonies are conducted at night and outlast the psychedelic effects of ayahuasca by a few hours. They are led by a shaman who provides the brew for each participant to drink and spiritual support. One to 2 drinks are typically offered per evening, and rituals may be conducted a few evenings in a row. A person's baseline mindset a priori to drug ingestion as well as the physical surroundings to the drug experience are thought to be crucial to minimizing harm and maximizing potential for benefit. These parameters are described in psychedelic literature as “set and setting.”3 In ritual context, the user prepares and approaches the experience with intention along with ingesting in a supportive, supervised, and spiritual setting, which is hypothesized to augment any potential benefits. Ayahuasca drinkers are primarily seeking a vehicle of self-development or healing, including treatment of psychiatric illness.4,5 Although the psychedelic effects of the ayahuasca attract the most attention in the literature and media, both preparation and integration phases pre- and postceremony are integral components to ritual ayahuasca use.
The Santo Daime and União do Vegetal (UDV) are two of the largest modern-day ayahuasca churches. Church membership has expanded to every inhabited continent.2,6 N-N-dimethyltryptamine is currently a schedule I controlled substance in the United States although the right to ritual drinking of ayahuasca for members of the UDV has been upheld by the Supreme Court under the Religious Freedom Restoration Act. Consumption in native areas of the Amazon as well as nonsanctioned ritual use in the West is also growing.7 The legal status of DMT poses a considerable barrier to adequate research of ayahuasca in the treatment of psychiatric illness.8
Pharmacology of Ayahuasca
Ayahuasca's psychedelic activity is attributed to DMT-containing plants Psychotria viridis or Diplopterys cabrerana. N-N-dimethyltryptamine, a tryptamine psychedelic, is a nonselective serotonin agonist although psychedelic effects have been primarily attributed to 5-hydroxytryptamine (5-HT)2A receptors.9 N-N-dimethyltryptamine is endogenously produced, structurally similar to serotonin, and is also a ligand for trace amine associated receptor and σ-1 receptors.10-12 Subjective effects of ayahuasca correlate closely with DMT blood concentrations; onset occurs around 20 minutes, peaks between 60 and 120 minutes, and resolution around 240 to 300 minutes. The half-life is approximately 1 hour.13,14
N-N-dimethyltryptamine lacks oral bioavailability under normal circumstances due to degradation by gastrointestinal and hepatic monoamine oxidase (MAO).15 Banisteriopsis caapi is a vine that contains a group of harmala alkaloids (also known as β-carbolines) that inhibit MAO-A and promotes oral bioavailability of DMT, eliciting a 4- to 6-hour psychedelic experience when brewed together with the aforementioned plants.16 Harmaline, harmine, and tetrahydroharmine are the primary harmala alkaloids responsible for bioactivation of DMT.17 Harmala alkaloids have psychoactive properties of their own and bind at dual specificity tyrosine phosphorylated and regulated kinase 1A, 5HT2A/C, dopamine transporters, and imidazoline I2 receptors.11 Harmala alkaloids exhibit reversible and selective inhibition of MAO-A, which differentiates them from irreversible pharmaceutical MAOIs.18-20 Reversible MAOIs, such as moclobemide, have a reduced propensity to lead to serotonin syndrome and hypertensive crises.21-23 Harmine has been shown to produce serotonin syndrome and myoclonic syndrome in rodents injected with tryptophan.24 Oral doses associated with ritual consumption in humans are at least an order of magnitude lower.11,25
Randomized, placebo-controlled trials of acute administration of ayahuasca in humans have demonstrated an acceptable safety profile using freeze-dried ayahuasca extracts.25-34 Doses of DMT administered ranged from 0.5 to 1 mg/kg.26 Concentrations of harmala alkaloids may display more variability than concentrations of DMT although they were reported as 1.4 mg/kg harmine, 1.15 mg/kg tetrahydroharmine, and 0.9 mg/kg harmaline in 1 study.27,30 Doses of up to 3.4 mg/kg harmine have been tolerated.11,25 The estimated lethal dose of ayahuasca determined in a pharmacologic safety review article27 was about 20 times the average amount consumed in ritual contexts. This may suggest a low therapeutic index with concentrated brews or repeat dosing of ayahuasca although propensity to induce vomiting may limit consumption.
Drug and Dietary Interactions
Due to MAO inhibition by harmala alkaloids, ayahuasca carries a higher risk of drug interactions than other psychedelics. Ayahuasca has previously been recognized to have interaction potential with selective serotonin reuptake inhibitors.35 Ayahuasca should also be avoided with other serotonergic agents, including tricyclic antidepressants, serotonin norepinephrine reuptake inhibitors, trazodone, and St John's wort. Non-antidepressants, such as lithium, triptans, metoclopramide, levodopa, phentermine, pseudoephedrine, linezolid, methadone, and dextromethorphan, may also have serotonergic effects.36 Psychoactive drugs, such as phenylethylamines (MDMA, mescaline, 2C compounds), methcathinones or “bath salts” (mephedrone, methylone), and tryptamines (LSD, 5-MeO-DMT, psilocybin) are high-risk combinations as fatalities have been reported when combined with harmala alkaloids in a recreational setting.37-40 Alternative combinations of extracted harmala alkaloids with DMT as well as other tryptamines was described by Ott as “Pharmauasca” and likely pose similar or greater drug-interaction risks than ayahuasca.39 Harmine is also a substrate and inhibitor of CYP2D6.11,41 Pharmacokinetic data of ayahausca users suggested genetic polymorphisms of CYP2D6 to play a significant role in harmine metabolism. However, similar DMT concentrations remained despite higher concentrations of harmala alkaloids, which indicates alternative metabolic routes for DMT apart from MAO.41
Effects of tyramine intake in subjects taking ayahuasca have not been described although extrapolation from pharmaceutical MAOIs suggest an increased risk of hypertensive crisis. Although not necessarily designed to minimize tyramine content, Amazonian dietas used in preparation of ritual ayahuasca involve bland foods that do not involve alcohol, cheese, or other fermented food items.
Neuroscience
In neuroimaging studies, ayahuasca has been found to increase blood flow to frontal cortical structures, including the medial temporal lobe, amygdala, hippocampus, and parahippocampal gyrus, that are involved in regulation of emotion and memory.30,31 The temporo-parieto-occipital junction is also activated and involved in association of sensory processes, resulting in synesthesia and other psychedelic phenomena.30,31 Visual effects of ayahuasca have been associated with decreased α-oscillations produced on electroencephalography, which is likely mediated by 5HT2A agonism.42 Long-term cross-sectional imaging studies in subjects that used ayahuasca at least 50 times in the past 2 years have shown increased cortical thickness in the anterior cingulate cortex (ACC) and thinning of the posterior cingulate cortex (PCC).43 Midline cortical structures, including the ACC and PCC, are involved with the default mode network (DMN), which helps to integrate environmental stimuli with cognitive and emotional processes.44 Default mode network hyperactivity has been suggested to play a role in depression, attention deficit-hyperactivity disorder, schizophrenia, and anxiety.45-48 Changes in DMN activity are thought to be beneficial in treating psychiatric illnesses and to be part of ayahuasca's mechanism of action.15 Changes in DMN activity may underlie the benefits of mindfulness, and ayahuasca has been demonstrated to increase mindfulness capacities.49,50
Tolerability
Ayahuasca, similar to other tryptamine psychedelics, is not considered to be an addictive substance although formal abuse liability studies are lacking.51 The drug has not been observed to produce withdrawal in studies to date. Ayahuasca is not well tolerated physically and frequently results in nausea, vomiting, and diarrhea as well as other somatic disturbances collectively known as purging or la purga. From the perspective of indigenous cultures, these adverse effects are considered to be cleansing and normal. Although a specific mechanism has not been established, these effects are consistent with mild serotonin toxicity. The frequency of vomiting reported with ayahuasca as well as being in an acutely altered state may increase risk of aspiration events. Mild and transient increases in cardiovascular parameters, such as increases in diastolic blood pressure of approximately 10 mmHg, as well as the somatic disturbances outlined above were common.25 Neuroendocrine activity, including transient increases in cortisol (12 μg/dL) and prolactin (14 ng/mL) that persist for approximately 6 hours with consequent immunomodulatory changes, has been identified and deserves further study.33 Many studies have been limited to healthy people with ayahuasca experience at baseline, which may skew reports on tolerability or objective or subjective effects. Few studies52-54 have included ayahuasca-naïve patients or patients diagnosed with a psychiatric illness.
There have been several reports of death, including an alleged homicide during an ayahuasca ceremony.40,55 Circumstances around deaths are generally unclear and may be related to shamans adding additional plants with increased toxicity to brews or inappropriately screening patients for drug interactions. There has never been a death observed during a clinical study.40 There was a single case report56 of a switch to mania in a patient with bipolar disorder who consumed ritual ayahuasca during a depressive episode. Ayahuasca does not appear to increase the risk of precipitating psychosis or schizophrenia among young adults with reported rates in the UDV being equal or less than that of the general population.27 One case report57 suggested that repeated use of smoked DMT may precipitate psychosis. Other persistent psychotic-like reactions have been described.40 One study58 reported reduced P50 sensory gating suppression with ayahuasca use and decreased P50 sensory gating is associated with schizophrenia. Given the paucity of data, ayahuasca may best be avoided in patients with a history of mania or psychosis.
Subjective Effects
Psychological effects have been assessed in short- and longer-term studies of psychiatrically stable church members. One study59 showed a decrease in working memory with acute administration although stimulus-response interference was decreased. Another showed increases in creative divergent thinking, which may be beneficial to mediating therapeutic interventions.60 Short-term effects were investigated prospectively in ayahuasca-naïve participants (n = 28) at 1 to 4 days and 7 to 14 days postritual.61 The Clinical Interview Schedule–Revised Edition, designed for measurement of minor psychiatric symptoms in community members, showed reduction in psychiatric symptoms.62 Altered states of consciousness most commonly experienced included visual phenomena, peace, numinous feelings, personal insight, and alterations in body image. However, 1 subject had a distressing reaction that resulted in worry and preoccupation persisting beyond the acute effects of ayahuasca. Within 7 to 14 days of use, feelings of serenity, assertiveness, joy, and satisfaction were reported. Other acute dysphoric reactions of approximately 20 minutes in duration have been reported.40 Longitudinal studies53,63-65 have demonstrated lower psychopathology scores; reduction in psychiatric symptom rating scales; and spiritual experiences leading to reduced alcohol intake, healthier diet, improved mood, and greater self-acceptance, which may be preventative of future morbidity if sustained. Although these studies do not show that ayahuasca is helpful for improving psychiatric illness, as included patients did not carry psychiatric diagnoses, it does suggest that ayahuasca does not induce symptoms of psychiatric illness in healthy subjects.
Clinical Studies of Ayahuasca
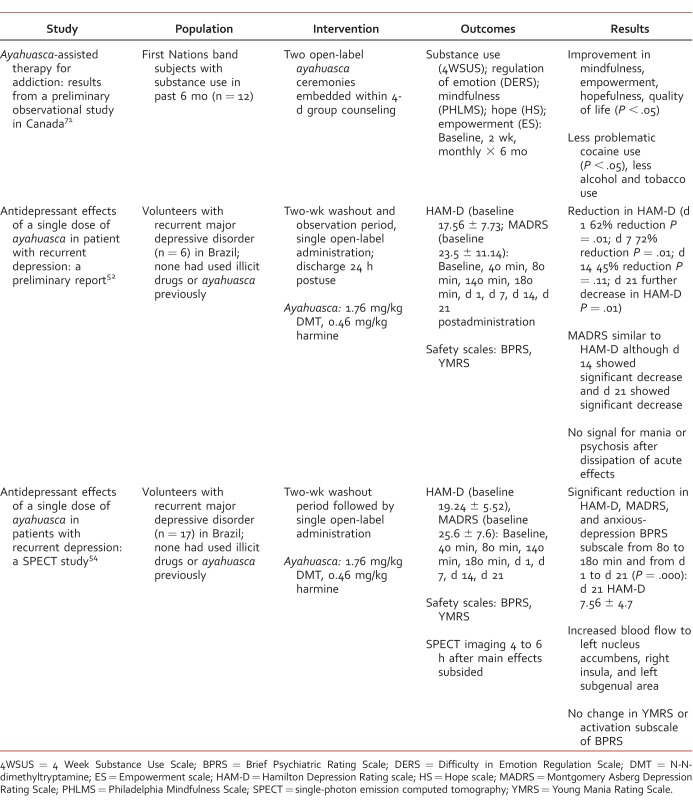
A PubMed search using the term “ayahuasca” from the time of database inception until September 6, 2016, was conducted for studies investigating the use of ayahuasca's effects for treatment of psychiatric illness. No randomized trials were identified, and studies were mostly retrospective in design or longitudinal cohort studies. A few open-label prospective experimental studies were found and are summarized in the Table.
TABLE:
Preliminary studies of ayahuasca in substance use and depression
Anecdotal clinician reports as well as naturalistic studies suggest ayahuasca may have positive effects on substance use disorders.51,63,66-68 Potential mechanisms in substance use disorders include modulation of serotonergic and dopamine neurotransmission that may help limbic processing of prior trauma and facilitate transcendent experiences.11,66,69,70 A preliminary observational study71 (n = 12) in Canada reported some benefits in reducing stimulant, alcohol, and tobacco use, including statistically significant reductions in cocaine use (Table).
Two open-label studies52,54 have investigated the antidepressant effects of ayahausca in patients with recurrent moderate major depressive disorder (Table). One study conducted in 6 patients in an inpatient setting showed rapid and sustained reductions in the Hamilton Depression Rating (HAM-D) scale and Montgomery Asberg Depression Rating Scale (MADRS). The second study assessed the impact of ayahuasca consumption on depression with concurrent neuroimaging in 17 patients. Rapid and sustained reductions in HAM-D and MADRS scores were replicated with single administrations without problematic increases in mania or psychosis rating scales.52,54
Conclusions
Ayahuasca has a complex pharmacologic mechanism that is not yet fully elucidated although it relies on inhibition of MAO by banisteriopsis caapi for bioactivation of DMT. Medication interactions are poorly understood, and ayahuasca should be avoided with medications possessing serotonergic potential. Current ayahuasca literature is limited by small sample sizes and convenience sampling of practicing church members. Control groups, blinding, or randomization are lacking in many circumstances. A publication bias toward favorable results may be present in the current literature. Various ayahuasca brews may vary in contents of active ingredients; however, standardization using freeze-dried extracts may create a different experience in the user than drinking the brew. Therapeutic effects observed may in part be attributable to ritual context opposed to purely a drug effect. Research with ayahuasca is difficult to conduct due to legality issues. Ritual use of ayahuasca has been touted for its benefit for centuries. There is limited evidence supporting clinical benefit in depression and substance use disorders, which makes the sacrament a promising area for future research. Approaches to minimize harm, maximize benefit, and reduce barriers to legitimate medical research are needed to protect patients who may be desperate and looking for alternatives for treatment of psychiatric illness.
References
- 1. Tupper KW, Wood E, Yensen R, Johnson MW. . Psychedelic medicine: a re-emerging therapeutic paradigm. CMAJ. 2015; 187 14: 1054- 9. DOI: 10.1503/cmaj.141124. PubMed PMID: 26350908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Blainey MG. . Forbidden therapies: Santo Daime, ayahuasca, and the prohibition of entheogens in Western society. J Relig Health. 2015; 54 1: 287- 302. DOI: 10.1007/s10943-014-9826-2. PubMed PMID: 24477460. [DOI] [PubMed] [Google Scholar]
- 3. Eisner B. . Set, setting, and matrix. J Psychoactive Drugs. 1997; 29 2: 213- 6. DOI: 10.1080/02791072.1997.10400190. PubMed PMID: 9250949. [DOI] [PubMed] [Google Scholar]
- 4. Winkelman M. . Drug tourism or spiritual healing? Ayahuasca seekers in Amazonia. J Psychoactive Drugs. 2005; 37 2: 209- 18. DOI: 10.1080/02791072.2005.10399803. PubMed PMID: 16149335. [DOI] [PubMed] [Google Scholar]
- 5. Kavenská V, Simonová H. . Ayahuasca tourism: participants in shamanic rituals and their personality styles, motivation, benefits and risks. J Psychoactive Drugs. 2015; 47 5: 351- 9. DOI: 10.1080/02791072.2015.1094590. PubMed PMID: 26514589. [DOI] [PubMed] [Google Scholar]
- 6. Anderson BT, Labate BC, Meyer M, Tupper KW, Barbosa PCR, Grob CS, et al. Statement on ayahuasca. Int J Drug Policy. 2012; 23 3: 173- 5. DOI: 10.1016/j.drugpo.2012.02.007. PubMed PMID: 22459485. [DOI] [PubMed] [Google Scholar]
- 7. Tupper KW. . The globalization of ayahuasca: harm reduction or benefit maximization? Int J Drug Policy. 2008; 19 4: 297- 303. DOI: 10.1016/j.drugpo.2006.11.001. PubMed PMID: 18638702. [DOI] [PubMed] [Google Scholar]
- 8. Riba J, Barbanoj MJ. . Bringing ayahuasca to the clinical research laboratory. J Psychoactive Drugs. 2005; 37 2: 219- 30. DOI: 10.1080/02791072.2005.10399804. PubMed PMID: 16149336. [DOI] [PubMed] [Google Scholar]
- 9. Halberstadt AL. . Recent advances in the neuropsychopharmacology of serotonergic hallucinogens. Behav Brain Res. 2015; 277: 99- 120. DOI: 10.1016/j.bbr.2014.07.016. PubMed PMID: 25036425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guchhait RB. . Biogenesis of 5-methoxy-N,N-dimethyltryptamine in human pineal gland. J Neurochem. 1976; 26 1: 187- 90. PubMed PMID: 1255170. [PubMed] [Google Scholar]
- 11. Brierley DI, Davidson C. . Developments in harmine pharmacology—implications for ayahuasca use and drug-dependence treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2012; 39 2: 263- 72. DOI: 10.1016/j.pnpbp.2012.06.001. PubMed PMID: 22691716. [DOI] [PubMed] [Google Scholar]
- 12. Bunzow JR, Sonders MS, Arttamangkul S, Harrison LM, Zhang G, Quigley DI, et al. Amphetamine, 3,4-methylenedioxymethamphetamine, lysergic acid diethylamide, and metabolites of the catecholamine neurotransmitters are agonists of a rat trace amine receptor. Mol Pharmacol. 2001; 60 6: 1181- 8. PubMed PMID: 11723224. [DOI] [PubMed] [Google Scholar]
- 13. Callaway JC, McKenna DJ, Grob CS, Brito GS, Raymon LP, . Poland RE, et al. Pharmacokinetics of Hoasca alkaloids in healthy humans. J Ethnopharmacol. 1999; 65 3: 243- 56. DOI: 10.1016/S0378-8741(98)00168-8. PubMed PMID: 10404423. [DOI] [PubMed] [Google Scholar]
- 14. Callaway JC, Raymon LP, Hearn WL, McKenna DJ, Grob CS, Brito GS, et al. Quantitation of N,N-dimethyltryptamine and harmala alkaloids in human plasma after oral dosing with ayahuasca. J Anal Toxicol. 1996; 20 6: 492- 7. DOI: 10.1093/jat/20.6.492. PubMed PMID: 8889686. [DOI] [PubMed] [Google Scholar]
- 15. McKenna D, Riba J. . New World tryptamine hallucinogens and the neuroscience of Ayahuasca. Curr Top Behav Neurosci. Epub 2015. February 6 DOI: 10.1007/7854_2015_368. PubMed PMID: 25655746. [DOI] [PubMed]
- 16. McKenna DJ. . Clinical investigations of the therapeutic potential of ayahuasca: rationale and regulatory challenges. Pharmacol Ther. 2004; 102 2: 111- 29. DOI: 10.1016/j.pharmthera.2004.03.002. PubMed PMID: 15163593. [DOI] [PubMed] [Google Scholar]
- 17. McKenna DJ, Towers GH, Abbott F. . Monoamine oxidase inhibitors in South American hallucinogenic plants: tryptamine and beta-carboline constituents of ayahuasca. J Ethnopharmacol. 1984; 10 2: 195- 223. PubMed PMID: 6587171. [DOI] [PubMed] [Google Scholar]
- 18. Abdel-Fattah AF, Matsumoto K, Murakami Y, El-Hady KA, Mohamed MF, Watanabe H. . Facilitatory and inhibitory effects of harmaline on the tryptophan-induced 5-hydroxytryptamine syndrome and body temperature changes in pargyline-pretreated rats. Jpn J Pharmacol. 1996; 72 1: 39- 47. PubMed PMID: 8902598. [DOI] [PubMed] [Google Scholar]
- 19. Samoylenko V, Rahman MM, Tekwani BL, Tripathi LM, Wang Y-H, Khan SI, et al. Banisteriopsis caapi, a unique combination of MAO inhibitory and antioxidative constituents for the activities relevant to neurodegenerative disorders and Parkinson's disease. J Ethnopharmacol. 2010; 127 2: 357- 67. DOI: 10.1016/j.jep.2009.10.030. PubMed PMID: 19879939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kim H, Sablin SO, Ramsay RR. . Inhibition of monoamine oxidase A by beta-carboline derivatives. Arch Biochem Biophys. 1997; 337 1: 137- 42. DOI: 10.1006/abbi.1996.9771. PubMed PMID: 8990278. [DOI] [PubMed] [Google Scholar]
- 21. Burkard WP, Bonetti EP, Da Prada M, Martin JR, Polc P, Schaffner R, et al. Pharmacological profile of moclobemide, a short-acting and reversible inhibitor of monoamine oxidase type A. J Pharmacol Exp Ther. 1989; 248 1: 391- 9. PubMed PMID: 2913284. [PubMed] [Google Scholar]
- 22. Rapaport MH. . Translating the evidence on atypical depression into clinical practice. J Clin Psychiatry. 2007; 68 Suppl 3: 31- 6. PubMed PMID: 17348765. [PubMed] [Google Scholar]
- 23. Bonnet U. . Moclobemide: therapeutic use and clinical studies. CNS Drug Rev. 2006; 9 1: 97- 140. DOI: 10.1111/j.1527-3458.2003.tb00245.x. PubMed PMID: 12595913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pranzatelli MR, Snodgrass SR. . Harmala alkaloids and related beta-carbolines: a myoclonic model and antimyoclonic drugs. Exp Neurol. 1987; 96 3: 703- 19. PubMed PMID: 3495451. [DOI] [PubMed] [Google Scholar]
- 25. Riba J, Valle M, Urbano G, Yritia M, Morte A, Barbanoj MJ. . Human pharmacology of ayahuasca: subjective and cardiovascular effects, monoamine metabolite excretion, and pharmacokinetics. J Pharmacol Exp Ther. 2003; 306 1: 73- 83. DOI: 10.1124/jpet.103.049882. PubMed PMID: 12660312. [DOI] [PubMed] [Google Scholar]
- 26. dos Santos RG. . Safety and side effects of ayahuasca in humans—an overview focusing on developmental toxicology. J Psychoactive Drugs. 2013; 45 1: 68- 78. DOI: 10.1080/02791072.2013.763564. PubMed PMID: 23662333. [DOI] [PubMed] [Google Scholar]
- 27. Gable RS. . Risk assessment of ritual use of oral dimethyltryptamine (DMT) and harmala alkaloids. Addiction. 2007; 102 1: 24- 34. DOI: 10.1111/j.1360-0443.2006.01652.x. PubMed PMID: 17207120. [DOI] [PubMed] [Google Scholar]
- 28. Riba J, Rodríguez-Fornells A, Urbano G, Morte A, Antonijoan R, Montero M, et al. Subjective effects and tolerability of the South American psychoactive beverage Ayahuasca in healthy volunteers. Psychopharmacology (Berl). 2001; 154 1: 85- 95. PubMed PMID: 11292011. [DOI] [PubMed] [Google Scholar]
- 29. Riba J, Anderer P, Morte A, Urbano G, Jané F, Saletu B, et al. Topographic pharmaco-EEG mapping of the effects of the South American psychoactive beverage ayahuasca in healthy volunteers. Br J Clin Pharmacol. 2002; 53 6: 613- 28. PubMed PMID: 12047486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Riba J, Anderer P, Jané F, Saletu B, Barbanoj MJ. . Effects of the South American psychoactive beverage ayahuasca on regional brain electrical activity in humans: a functional neuroimaging study using low-resolution electromagnetic tomography. Neuropsychobiology. 2004; 50 1: 89- 101. DOI: 10.1159/000077946. PubMed PMID: 15179026. [DOI] [PubMed] [Google Scholar]
- 31. Riba J, Romero S, Grasa E, Mena E, Carrió I, Barbanoj MJ. . Increased frontal and paralimbic activation following ayahuasca, the pan-Amazonian inebriant. Psychopharmacology (Berl). 2006; 186 1: 93- 8. DOI: 10.1007/s00213-006-0358-7. PubMed PMID: 16575552. [DOI] [PubMed] [Google Scholar]
- 32. Barbanoj MJ, Riba J, Clos S, Giménez S, Grasa E, Romero S. . Daytime Ayahuasca administration modulates REM and slow-wave sleep in healthy volunteers. Psychopharmacology (Berl). 2008; 196 2: 315- 26. DOI: 10.1007/s00213-007-0963-0. PubMed PMID: 18030450. [DOI] [PubMed] [Google Scholar]
- 33. Dos Santos RG, Valle M, Bouso JC, Nomdedéu JF, Rodríguez-Espinosa J, McIlhenny EH, et al. Autonomic, neuroendocrine, and immunological effects of ayahuasca: a comparative study with d-amphetamine. J Clin Psychopharmacol. 2011; 31 6: 717- 26. DOI: 10.1097/JCP.0b013e31823607f6. PubMed PMID: 22005052. [DOI] [PubMed] [Google Scholar]
- 34. Dos Santos RG, Grasa E, Valle M, Ballester MR, Bouso JC, Nomdedéu JF, et al. Pharmacology of ayahuasca administered in two repeated doses. Psychopharmacology (Berl). 2012; 219 4: 1039- 53. DOI: 10.1007/s00213-011-2434-x. PubMed PMID: 21842159. [DOI] [PubMed] [Google Scholar]
- 35. Callaway JC, Grob CS. . Ayahuasca preparations and serotonin reuptake inhibitors: a potential combination for severe adverse interactions. J Psychoactive Drugs. 1998; 30 4: 367- 9. DOI: 10.1080/02791072.1998.10399712. PubMed PMID: 9924842. [DOI] [PubMed] [Google Scholar]
- 36. Volpi-Abadie J, Kaye AM, Kaye AD. . Serotonin syndrome. Ochsner J. 2013; 13 4: 533- 40. PubMed PMID: 24358002. [PMC free article] [PubMed] [Google Scholar]
- 37. Lanaro R, Calemi DB, Togni LR, Costa JL, Yonamine M, . CazenaveSde O, et al. Ritualistic use of Ayahuasca versus street use of similar substances seized by the police: a key factor involved in the potential for intoxications and overdose? J Psychoactive Drugs. 2015; 47 2: 132- 9. DOI: 10.1080/02791072.2015.1013202. PubMed PMID: 25950593. [DOI] [PubMed] [Google Scholar]
- 38. Wiltshire PE, Hawksworth DL, Edwards KJ. . Light microscopy can reveal the consumption of a mixture of psychotropic plant and fungal material in suspicious death. J Forensic Leg Med. 2015; 34: 73- 80. DOI: 10.1016/j.jflm.2015.05.010. PubMed PMID: 26165663. [DOI] [PubMed] [Google Scholar]
- 39. Ott J. . Pharmahuasca: human pharmacology of oral DMT plus harmine. J Psychoactive Drugs. 1999; 31 2: 171- 7. DOI: 10.1080/02791072.1999.10471741. PubMed PMID: 10438001. [DOI] [PubMed] [Google Scholar]
- 40. dos Santos RG. . A critical evaluation of reports associating ayahuasca with life-threatening adverse reactions. J Psychoactive Drugs. 2013; 45 2: 179- 88. DOI: 10.1080/02791072.2013.785846. PubMed PMID: 23909005. [DOI] [PubMed] [Google Scholar]
- 41. Callaway JC. . Fast and slow metabolizers of Hoasca. J Psychoactive Drugs. 2005; 37 2: 157- 61. DOI: 10.1080/02791072.2005.10399797. PubMed PMID: 16149329. [DOI] [PubMed] [Google Scholar]
- 42. Valle M, Maqueda AE, Rabella M, Rodríguez-Pujadas A, Antonijoan RM, Romero S, et al. Inhibition of alpha oscillations through serotonin-2A receptor activation underlies the visual effects of ayahuasca in humans. Eur Neuropsychopharmacol. 2016; 26 7: 1161- 75. DOI: 10.1016/j.euroneuro.2016.03.012. PubMed PMID: 27039035. [DOI] [PubMed] [Google Scholar]
- 43. Bouso JC, Palhano-Fontes F, Rodríguez-Fornells A, Ribeiro S, Sanches R, Crippa JA, et al. Long-term use of psychedelic drugs is associated with differences in brain structure and personality in humans. Eur Neuropsychopharmacol. 2015; 25 4: 483- 92. DOI: 10.1016/j.euroneuro.2015.01.008. PubMed PMID: 25637267. [DOI] [PubMed] [Google Scholar]
- 44. Muthukumaraswamy SD, Carhart-Harris RL, Moran RJ, Brookes MJ, Williams TM, Errtizoe D, et al. Broadband cortical desynchronization underlies the human psychedelic state. J Neurosci. 2013; 33 38: 15171- 83. DOI: 10.1523/JNEUROSCI.2063-13.2013. PubMed PMID: 24048847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Whitfield-Gabrieli S, Ford JM. . Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012; 8: 49- 76. DOI: 10.1146/annurev-clinpsy-032511-143049. PubMed PMID: 22224834. [DOI] [PubMed] [Google Scholar]
- 46. Gudayol-Ferré E, Peró-Cebollero M, González-Garrido AA, Guàrdia-Olmos J. . Changes in brain connectivity related to the treatment of depression measured through fMRI: a systematic review. Front Hum Neurosci. 2015; 9: 582 DOI: 10.3389/fnhum.2015.00582. PubMed PMID: 26578927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hamilton JP, Farmer M, Fogelman P, Gotlib IH. . Depressive rumination, the default-mode network, and the dark matter of clinical neuroscience. Biol Psychiatry. 2015; 78 4: 224- 30. DOI: 10.1016/j.biopsych.2015.02.020. PubMed PMID: 25861700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sonuga-Barke EJ, Cortese S, Fairchild G, Stringaris A. . Annual research review: transdiagnostic neuroscience of child and adolescent mental disorders—differentiating decision making in attention-deficit/hyperactivity disorder, conduct disorder, depression, and anxiety. J Child Psychol Psychiatry. 2016; 57 3: 321- 49. DOI: 10.1111/jcpp.12496. PubMed PMID: 26705858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Marchand WR. . Neural mechanisms of mindfulness and meditation: evidence from neuroimaging studies. World J Radiol. 2014; 6 7: 471- 9. DOI: 10.4329/wjr.v6.i7.471. PubMed PMID: 25071887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Soler J, Elices M, Franquesa A, Barker S, Friedlander P, Feilding A, et al. Exploring the therapeutic potential of ayahuasca: acute intake increases mindfulness-related capacities. Psychopharmacology (Berl). 2016; 233 5: 823- 9. DOI: 10.1007/s00213-015-4162-0. PubMed PMID: 26612618. [DOI] [PubMed] [Google Scholar]
- 51. Fábregas JM, González D, Fondevila S, Cutchet M, Fernández X, Barbosa PCR, et al. Assessment of addiction severity among ritual users of ayahuasca. Drug Alcohol Depend. 2010; 111 3: 257- 61. DOI: 10.1016/j.drugalcdep.2010.03.024. PubMed PMID: 20554400. [DOI] [PubMed] [Google Scholar]
- 52. Osório Fde L, Sanches RF, Macedo LR, Santos RG, Maia-de-Oliveira JP, Wichert-Ana L, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a preliminary report. Rev Bras Psiquiatr. 2015; 37 1: 13- 20. DOI: 10.1590/1516-4446-2014-1496. PubMed PMID: 25806551. [DOI] [PubMed] [Google Scholar]
- 53. Barbosa PC, Cazorla IM, Giglio JS, Strassman R. . A six-month prospective evaluation of personality traits, psychiatric symptoms and quality of life in ayahuasca-naïve subjects. J Psychoactive Drugs. 2009; 41 3: 205- 12. DOI: 10.1080/02791072.2009.10400530. PMID: 19999673. [DOI] [PubMed] [Google Scholar]
- 54. Sanches RF, . de LimaOsório F, Dos Santos RG, Macedo LR, Maia-de-Oliveira JP, Wichert-Ana L, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a SPECT study. J Clin Psychopharmacol. 2016; 36 1: 77- 81. DOI: 10.1097/JCP.0000000000000436. PubMed PMID: 26650973. [DOI] [PubMed] [Google Scholar]
- 55. Plucinska J. . A British tourist has been killed at a Peruvian ayahuasca ceremony. Time [Internet]. 2015. December [cited 2016 May 3]. Available from: http://time.com/4154455/peru-ayahuasca-murder-amazon-hallucinogen
- 56. Szmulewicz AG, Valerio MP, Smith JM. . Switch to mania after ayahuasca consumption in a man with bipolar disorder: a case report. Int J Bipolar Disord. 2015; 3: 4 DOI: 10.1186/s40345-014-0020-y. PubMed PMID: 25713771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Paterson NE, Darby WC, Sandhu PS. . N,N-Dimethyltryptamine-induced psychosis. Clin Neuropharmacol. 2015; 38 4: 141- 3. DOI: 10.1097/WNF.0000000000000078. PubMed PMID: 26166234. [DOI] [PubMed] [Google Scholar]
- 58. Riba J, Rodríguez-Fornells A, Barbanoj MJ. . Effects of ayahuasca on sensory and sensorimotor gating in humans as measured by P50 suppression and prepulse inhibition of the startle reflex, respectively. Psychopharmacology (Berl). 2002; 165 1: 18- 28. DOI: 10.1007/s00213-002-1237-5. PubMed PMID: 12474114. [DOI] [PubMed] [Google Scholar]
- 59. Bouso JC, Fábregas JM, Antonijoan RM, Rodríguez-Fornells A, Riba J. . Acute effects of ayahuasca on neuropsychological performance: differences in executive function between experienced and occasional users. Psychopharmacology (Berl). 2013; 230 3: 415- 24. DOI: 10.1007/s00213-013-3167-9. PubMed PMID: 23793226. [DOI] [PubMed] [Google Scholar]
- 60. Kuypers KPC, Riba J, . de la Fuente Revenga M, Barker S, Theunissen EL, Ramaekers JG. Ayahuasca enhances creative divergent thinking while decreasing conventional convergent thinking. Psychopharmacology (Berl). 2016; 233 18: 3395- 403. DOI: 10.1007/s00213-016-4377-8. PubMed PMID: 27435062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Barbosa PC, Giglio JS, Dalgalarrondo P. . Altered states of consciousness and short-term psychological after-effects induced by the first time ritual use of ayahuasca in an urban context in Brazil. J Psychoactive Drugs. 2005; 37 2: 193- 201. DOI: 10.1080/02791072.2005.10399801. PubMed PMID: 16149333. [DOI] [PubMed] [Google Scholar]
- 62. Subramaniam K, Krishnaswamy S, Jemain AA, Hamid A, Patel V. . The Clinical Interview Schedule-Revised (CIS-R)–Malay Version, Clinical Validation. Malays J Med Sci. 2006; 13 1: 58- 62. PubMed PMID: 22589592. [PMC free article] [PubMed] [Google Scholar]
- 63. Halpern JH, Sherwood AR, Passie T, Blackwell KC, Ruttenber AJ. . Evidence of health and safety in American members of a religion who use a hallucinogenic sacrament. Med Sci Monit. 2008; 14(8):SR15-22. PubMed PMID: 18668010. [PubMed]
- 64. Bouso JC, González D, Fondevila S, Cutchet M, Fernández X, . RibeiroBarbosa PC, et al. Personality, psychopathology, life attitudes and neuropsychological performance among ritual users of Ayahuasca: a longitudinal study. PLoS One. 2012; 7 8: e42421 DOI: 10.1371/journal.pone.0042421. PubMed PMID: 22905130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Harris R, Gurel L. . A study of ayahuasca use in North America. J Psychoactive Drugs. 2012; 44 3: 209- 15. DOI: 10.1080/02791072.2012.703100. PubMed PMID: 23061320. [DOI] [PubMed] [Google Scholar]
- 66. Loizaga-Velder A, Verres R. . Therapeutic effects of ritual ayahuasca use in the treatment of substance dependence—qualitative results. J Psychoactive Drugs. 2014; 46 1: 63- 72. DOI: 10.1080/02791072.2013.873157. PubMed PMID: 24830187. [DOI] [PubMed] [Google Scholar]
- 67. Doering-Silveira E, Grob CS, de Rios MD, Lopez E, Alonso LK, Tacla C, et al. Report on psychoactive drug use among adolescents using ayahuasca within a religious context. J Psychoactive Drugs. 2005; 37 2: 141- 4. DOI: 10.1080/02791072.2005.10399794. PubMed PMID: 16149326. [DOI] [PubMed] [Google Scholar]
- 68. Da Silveira DX, Grob CS, de Rios MD, Lopez E, Alonso LK, Tacla C, et al. Ayahuasca in adolescence: a preliminary psychiatric assessment. J Psychoactive Drugs. 2005; 37 2: 129- 33. DOI: 10.1080/02791072.2005.10399792. PubMed PMID: 16149324. [DOI] [PubMed] [Google Scholar]
- 69. Liester MB, Prickett JI. . Hypotheses regarding the mechanisms of ayahuasca in the treatment of addictions. J Psychoactive Drugs. 2012; 44 3: 200- 8. DOI: 10.1080/02791072.2012.704590. PubMed PMID: 23061319. [DOI] [PubMed] [Google Scholar]
- 70. Winkelman M. . Psychedelics as medicines for substance abuse rehabilitation: evaluating treatments with LSD, peyote, ibogaine and ayahuasca. Curr Drug Abuse Rev. 2014; 7 2: 101- 16. DOI: 10.2174/1874473708666150107120011. PubMed PMID: 25563446. [DOI] [PubMed] [Google Scholar]
- 71. Thomas G, Lucas P, Capler NR, Tupper KW, Martin G. . Ayahuasca-assisted therapy for addiction: results from a preliminary observational study in Canada. Curr Drug Abuse Rev. 2013; 6 1: 30- 42. DOI: 10.2174/15733998113099990003. PubMed PMID: 23627784. [DOI] [PubMed] [Google Scholar]