Abstract
STUDY QUESTION
Does the provision of fertility (compared to control) information affect fertility-related knowledge, perceived threat of infertility, anxiety, physical stress and fertility plans in adolescents and emerging adults?
SUMMARY ANSWER
The provision of fertility information was associated with increased fertility knowledge (emerging adults) and greater infertility threat (adolescents and emerging adults).
WHAT IS KNOWN ALREADY
According to fertility education research, adolescents and emerging adults know less than they should know about fertility topics. Fertility knowledge can be improved through the provision of information in older adults.
STUDY DESIGN, SIZE, DURATION
Experimental design. Secondary and university students completed pre-information questionnaires, were randomly assigned via computer to an experimental group, read either fertility (FertiEduc group) or healthy pregnancy information (Control group), and completed post-information questionnaires. Data were collected in group sessions via an online portal.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Eligible participants were aged 16–18 (adolescents) or 21–24 years (emerging adults), childless, not currently pregnant (for men, partner not pregnant) or trying to conceive, presumed fertile and intending to have a child in the future. Of the 255 invited, 208 (n = 93 adolescents, n = 115 emerging adults) participated. The FertiEduc group received ‘A Guide to Fertility’, four online pages of information about fertility topics (e.g. ‘When are men and women most fertile?’) and the Control group received four online pages from the National Health Service (NHS) pregnancy booklet ‘Baby Bump and Beyond’. Participants completed a questionnaire (fertility knowledge, perceived threat of infertility, anxiety, physical stress and fertility plans, moderators) prior to and after the provision of information. Mixed factorial analysis of variance was used to examine the effects of information provision and hierarchical multiple regression to assess potential moderators of knowledge.
MAIN RESULTS AND THE ROLE OF CHANCE
The FertiEduc and Control groups were equivalent on age, gender, disability, relationship status and orientation at baseline. Results showed that fertility information significantly increased fertility knowledge for emerging adults only (P < 0.001) and threat of infertility for emerging adults and adolescents (P = 0.05). The moderators were not significant. Participation in the study was associated with an increase in feelings of anxiety but a decrease in physical stress reactions. Adolescents had more optimal fertility plans compared to emerging adults due to being younger.
LIMITATIONS, REASONS FOR CAUTION
This was an experimental study on a self-selected sample of men and women from selected educational institutions and only short term effects of information were studied.
WIDER IMPLICATIONS OF THE FINDINGS
Provision of fertility information can have benefits (increased fertility knowledge) but also costs (increase potential threat of infertility). Adolescents find fertility information positive but do not learn from it. Fertility education should be tailored according to age groups and created to minimise negative effects. Longitudinal examination of the effects of fertility information in multi-centre studies is warranted and should include measures of perceived threat of infertility.
STUDY FUNDING/COMPETING INTEREST(S)
Cardiff University funded this research. All authors have no conflicts of interest to declare.
Keywords: fertility awareness, education, knowledge, benefits and costs, adolescents, emerging adults
Introduction
There is voluminous research concerned with what young people know about fertility. Fertility awareness refers to knowledge about reproduction, fecundity, fecundability, risk factors for reduced fertility and societal and cultural factors affecting options to meet parenthood goals (Zegers-Hochschild et al., 2017). Applying academic standards to their knowledge levels would suggest that adolescents (16–18 years) and emerging adults (21–24 years) know less than they should about important fertility these topics (e.g. Byamugisha et al., 2006; Lampic et al., 2006; Tydén et al., 2006; Quach and Librach, 2008; Bretherick et al., 2010; Rovei et al., 2010; Virtala et al., 2011; Sabarre et al., 2013; Chan et al., 2014; Rouchou and Forde, 2015; Meissner et al., 2016; Mogilevkina et al., 2016). These findings have been used to support health education initiatives to help young people maintain fertility health (Hammarberg et al., 2017b; Harper et al., 2017).
A few studies have evaluated the effectiveness of fertility education in young people (18–25 years of age). These experimental pre and post studies have shown that the provision of fertility information (e.g. infertility, ART age-related fertility decline) can improve fertility knowledge (Williamson et al., 2014) and lower desired age for a first child (Wojcieszek and Thompson, 2013). One study using nurse led discussions also showed that improved fertility knowledge was maintained at two months (Stern et al., 2013). Despite benefits, a broader understanding is warranted. According to intervention development frameworks, the feasibility and acceptability of interventions should be examined before setting up definitive randomised trials (Bowen et al., 2009). This is especially true for provision of fertility information because there has not yet been an evaluation of benefits or costs in adolescents despite adolescents being current targets for fertility education initiatives (Harper et al., 2017). Information could be harmful if it encourages people unnecessarily to perceive themselves to be at risk for fertility problems. Maeda et al. (2016) showed that provision of fertility information was associated with an increase in knowledge but also in subjective anxiety in 20–24 year olds but data on adolescent groups were not available. The moderators of knowledge gain are also not known which could be important considerations in full RCTs. A recent systematic review suggests gender may be relevant because men and women benefit differently (Hammarberg et al., 2017a). Other moderators such as health literacy (i.e. the capacity to process and understand health information; Suka et al., 2013), optimism (i.e. the extent people hold favourable expectancies for their future; Carver et al., 2010) and topic relevance (Huang and Shen, 2016) are important in other health contexts but have not been studied in fertility.
Present study
Adolescents and emerging adults were randomly assigned to one of two informational groups receiving fertility (FertiEduc) information or control (Control) information about healthy pregnancy. It was hypothesised that fertility information would increase fertility knowledge and optimality of fertility plans (i.e. intended age at first and last child) for adolescents and emerging adults but that emerging adults would report more anxiety, physical stress and perceived threat of infertility than adolescents due to being closer to median age at first birth. We expected being male, having lower literacy, or fertility topic relevance, and higher optimism would moderate and reduce the effect of fertility information.
Method
Participants
Inclusion criteria were: aged between 16 and 18 (adolescents) or 21 and 24 years (emerging adults), childless, not currently pregnant (or for men, partner not pregnant) nor trying to conceive, presumed fertile and intending to have a child in the future. School of Psychology, Cardiff University Ethics committee provided ethical review and approval.
Measures
Questionnaires were completed prior to (Time 1 (T1)) and immediately after the provision of the information (Time 2 (T2)).
Data collected at T1 only
Age, gender, nationality, disability (yes, no), relationship status (single, in a relationship, same sex relationship).
Moderators: Health literacy was measured using the 12-item health literacy scale (range 0–60; Suka et al., 2013) and optimism the 10-item Revised Life Orientation test (range 0–30; Carver et al., 2010). Higher composite scores indicated greater health literacy and optimism (Cronbach alpha was 0.77 and 0.82, respectively). Fertility relevance was measured using summed score of personal relevance of fertility to person (1 = not at all to 5 = an extreme amount) and frequency of thinking about fertility (1 = never to 5 = always) with higher scores indicating greater fertility topic relevance.
Data collected at T1 and T2
Fertility knowledge about fertility facts, risks, and myths was measured using the 13-item Cardiff Fertility Knowledge Scale (CFKS, Bunting et al., 2013, see CFKS in their Appendix) and an additional two items on male fertility. The response scale was ‘true’, ‘false’ or ‘do not know’. Answers were scored one point (correct) or zero points (incorrect/do not know) and summed to create a total CFKS score (range 0–100% correct).
Perceived threat of infertility (hereafter infertility threat) was defined as perceived susceptibility to infertility multiplied by perceived severity of infertility (rated 1 = not at all, 5 = extremely) as per Rosenstock (1990) and Witte and Allen (2000) with higher scores indicating greater perceived infertility threat (range 0–25).
Anxiety was measured using the six-item State-Trait Anxiety Inventory (STAI, Marteau and Bekker, 1992) with higher scores indicating more anxiety (Cronbach alpha 0.83 and 0.82 for T1 and T2, respectively, range 20–80). Physical stress reactions were measured using the sum of the nine-item physical stress subscale of the Stress Profile questionnaire (Setterlind and Larsson, 1995). Higher scores (0–36) indicated more severe stress reactions (Cronbach alpha was 0.66 at T1 and T2).
Optimality of fertility plans was measured using the Habbema et al. (2015) matrix predicting the optimal age to start trying to have children based on desired number of children (1, 2 or 3), willingness to use ART (yes, no) and certainty of wanting children (50%, 75%, 90%). This matrix and participant replies to these questions was used to derive an optimal age to start trying to conceive for each participant. The difference in years between the derived optimal age and self-reported intended age was computed to gauge optimality of fertility plans (first and last birth). Higher positive scores indicated more optimal fertility plans (self-reported age lower than the predicted optimal age).
Data collected at only T2
Information Evaluation Scale (IES) (Lancastle and Boivin, 2008) was adapted and used to rate the information received on six cognitive and affective items on a seven-point scale. The mean of items was calculated with higher scores indicating more positive evaluations of information (Cronbach alpha 0.90). An open-ended question was used to elicit thoughts and feelings about the information provided.
Informational groups
The FertiEduc group read the ‘A Guide to Fertility’. The research team created the Guide from fertility information tested in past research, defining components of fertility awareness (Zegers-Hochschild et al. 2017) and relevance according to fertility experts consulted. The four pages of information were divided into eight questions (e.g. fecundity, infertility, risk factors, signs and symptoms, reproductive options), with seven graphics and a glossary of terms to aid learning (see Guide on: http://psych.cf.ac.uk/contactsandpeople/boivin.php#two).
To control for relevant health information participants might have acquired outside the experiment, the control group read four pages (pages 42–45) from the NHS (2014) booklet ‘Baby Bump and Beyond’. These pages focused on the effects of smoking and drinking alcohol in pregnancy.
Procedure
The materials were updated from pilot testing with parents, adolescents, emerging adults and fertility experts. Secondary and university students from two institutions in the same geographic region were invited to the study. Data were collected in groups (23 & 27 January 2017 for adolescents and 25 January & 2 March 2017 for emerging adults), in quiet rooms on computers. Participants completed the T1 questionnaire, were then randomly assigned to experimental condition via the online allocation system (i.e. Qualtrics) and then completed the T2 questionnaire. Researchers were blind to allocation. The study took 20–30 min to complete. Participants were debriefed and provided with a link to the NHS Choices (2014) website ‘Fertility Facts’. The procedure was the same for the two groups except that secondary students were invited to the study at their morning assembly, before the start of classes whereas emerging adults were recruited from the entry hall of the student union, during lunchtime with the added incentive of free pizza.
Statistical analysis
Isolated missing data were handled using prorated scores but were not substituted for person characteristics (e.g. nationality, relationship status) or when >50% missing items on a summed score. Descriptive statistics, chi-square, t-tests and multivariate analysis of variance (MANOVA) were used to examine differences at baseline. Analysis of variance (ANOVA) was used to examine the effects of information using a 2 (age group: adolescent, emerging adult) × 2 (informational group: FertiEduc, control) × 2 (time: T1, T2) design. Simple effects were used as follow-up tests. Hierarchical multiple regression analyses were used to test moderators, in this order: knowledge at T1 (Step 1), age-group, information group (Step 2), moderator (Step 3), two-way interaction with moderator (Step 4) and three-way interaction with moderator (Step 5). The regression table was deleted during the revision process, so this sentence is no longer relevant. Significant interaction blocks were followed up using simple slope analysis (Aiken and West, 1991). ANOVA was used to examine quantitative information evaluation responses whereas qualitative responses were coded as positive, negative, neutral or mixed according to content.
Results
Recruitment and participant profile at T1
In total 255 people were invited, 219 were randomised, and 208 completed the study (95.0%, n = 98 adolescents, n = 115 emerging adults).
Table I shows demographic characteristics of the groups. The experimental groups (FertiEduc versus Control) were equivalent on all demographic variables at T1 except that within emerging adults, the FertiEduc group comprised significantly more British participants than the Control group (χ2(1) = 4.97, P < 0.05).
Table I.
Descriptive statistics for the total sample according to age and experimental group.
| Adolescents (n = 93) | Emerging adult (n = 115) | ||||
|---|---|---|---|---|---|
| Total | FertiEduc | Control | FertiEduc | Control | |
| N = 208 | n = 46 | n = 47 | n = 60 | n = 55 | |
| Age Mean (SD) | 19.6 (2.31) | 17.2 (0.52) | 17.1 (0.55) | 21.6 (0.65) | 21.6 (0.74) |
| Gender n (% female) | 122 (58.7) | 23 (50) | 26 (55) | 39 (65) | 34 (62) |
| British Nationality n (% yes) | 180 (86.5) | 39 (85) | 39 (83) | 57 (95) | 45 (82) |
| Has disability n (% yes) | 1 (0.5) | 0 (0) | 1 (2) | 0 (0) | 0 (0) |
| Relationship status n (% yes) | |||||
| Single | 127 (61.1) | 36 (78) | 36 (77) | 25 (42) | 30 (55) |
| In a relationship | 81 (38.9) | 10 (22) | 11 (23) | 35 (58) | 25 (45) |
| Same sex relationship n (% yes) | 8 (10.0) | 2 (20) | 2 (18) | 2 (6) | 2 (8) |
Note: FertiEduc = fertility education group.
At baseline the multivariate test showed that the experimental groups were equivalent on psychological (Pillai = 0.015, multi F(4, 201) = 0.78, P = 0.54) and fertility variables (Pillai = 0.032, multi F(5, 184) = 1.21, P = 0.31) at T1 (see Supplementary Table SI).
Effect of provision of fertility information
Supplementary Table SII shows F-ratios for mixed design ANOVAs evaluating the effect of provision of fertility information.
Fertility knowledge
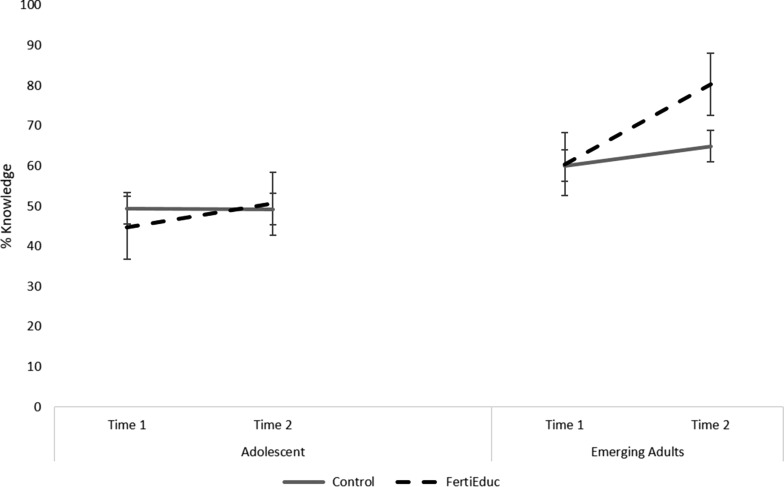
There was a main effect of time on knowledge, but the higher order three-way interaction (age group × information group × time) (F(1, 195) = 4.85, P = 0.03) showed that a fertility knowledge gain was only observed for the fertility education group in emerging adults (F(1111) = 31.74, P < 0.001, 32.9% gain) and not for adolescents (F(1,84) = 1.75, P = 0.19, 13.4% gain). Simple time comparisons showed the improvement in knowledge scores was larger for the FertiEduc group (change M = 2.91, SE = 0.33; F(1,57) = 78.76, P < 0.001) than the control group (M = 0.72, SE = 0.20; F(1,54) = 13.47, P = 0.001) (see Fig. 1). Finally, overall adolescents had poorer fertility knowledge than did emerging adults (main effect of age group).
Figure 1.
Cardiff Fertility Knowledge Scale (0–100% correct) according to age group (Adolescent, Emerging Adult) and information group (Control, FertiEduc). Dashed line refers to group receiving fertility education (FertiEduc). Bold line refers to group receiving control information (Control).
Infertility threat
There was a significant two-way interaction for information group × time (F(1, 194) = 4.65, P = 0.03). Simple main effects test for time showed infertility threat increased in the FertiEduc groups (both adolescent and emerging adults) from T1 to T2 (F(1, 100) = 3.81, P = 0.05) but not in the control groups (F(1, 96) = 0.38, P = 0.541). Overall adolescents reported less infertility threat than did emerging adults (significant main effect of age group).
Anxiety and physical stress
None of the interactions were significant. However, the main effect of time for anxiety (F(1, 202) = 4.57, P = 0.03) and physical stress (F(1, 203) = 26.76, P < 0.001) were significant. Overall anxiety increased from T1 to T2 (change M = 1.25, SE = 0.58) while physical stress decreased (change M = 0.65, SE = 0.13).
Optimality of fertility plan
None of the interactions were significant. However, the main effect of age group for first (F(1185) = 42.87, P < 0.001) and last birth (F(1185) = 30.76, P < 0.001) were significant, showing overall more optimal plans in adolescents. Adolescents planned to have a child 4–6 years before the predicted optimal time versus 1–2 years’ prior for emerging adults (see Supplementary Table SIII).
Moderators of fertility knowledge
We examined whether gender, optimism, health literacy and fertility relevance moderated the effect of provision of fertility information on fertility knowledge. None of the moderators were significant in affecting learning of fertility information.
Information evaluation
A 2 (information group) × 2 (age group) factorial ANOVA on IES ratings showed a significant main effect of intervention group (F(1199) = 5.57, P = 0.027). The FertiEduc groups rated their information as more favourable (M = 5.48, SE = 0.13) than the control groups (M = 5.06, SD = .12). The main effect of age group (P = 0.137) and interaction (P = 0.061) were not significant.
A total of 170 (81.7%) participants left a textual reply about the information they received. Of these, 88 (36 adolescents and 52 emerging adults) were in the control group and 82 (30 adolescents and 52 emerging adults) were in the FertiEduc group. Of the textual replies, 117 (68.8%) were positive, 24 (14.1%) were mixed, 20 (11.8%) were neutral and nine (4.3%) were negative. The ratings of textual replies were similar in FertiEduc and Control groups for percentage of positive (n = 57, 69.5% versus n = 60, 68.2%, respectively), mixed (n = 16, 18.2% n = 8, 9.8%), neutral (n = 9, 10.2% versus n = 11 14.3%) and negative (n = 6, 7.3% versus n = 3, 3.4%). The ratings were also similar for adolescents and emerging adults for percentage of mixed (n = 7, 10.6% versus n = 17, 16.3%), neutral (n = 7, 10.6% versus n = 13, 12.5%) and negative (n = 3, 4.5% versus n = 6, 5.8%, respectively). A higher percentage of adolescents left positive textual replies than did emerging adults (n = 49, 74.2% versus n = 68, 65.4%) (see Supplementary Table SIV for illustrative quotes).
Discussion
Findings show that it was possible to increase fertility knowledge in emerging adults with provision of specific fertility information but adolescents did not benefit more from it than what could be gained with standard health pre pregnancy advice. Importantly, the provision of fertility information could be accompanied by an increase in infertility threat in both adolescent and emerging adults. To achieve the goal of improved fertility awareness educational messages will need to be tailored to target audiences to minimise inadvertent worry. More research is required to understand variability in reactions to fertility information.
Emerging adults that read ‘A Guide to Fertility’ showed a 33% increase in fertility knowledge compared to about 8% in controls. Closer inspection of items of the CFKS showed that emerging adults in fertility education groups gained more on fertility specific items (e.g. age decline in fertility, reproductive technologies, prevalence of fertility problems) whereas the smaller gains for other groups was mainly related to global risks (e.g. effect of smoking or obesity). Male and female adolescents did not show a knowledge gain from provision of specific fertility information. One explanation could be that adolescents were more likely to ignore experimental instructions. However, about 80% of adolescents provided textual replies suggestive of them having read the information, time recording showed an expected time difference between age groups (adolescents slower to read) and adolescents had emotional reactions to the information, as has been shown previously (Maeda et al., 2016). Level of knowledge gain was not due to the moderators of personal relevance of the fertility topic, health literacy, or optimism. The latter is not in line with evidence of their moderations in other health contexts (Carver et al., 2010; Huang and Shen, 2016; Suka et al., 2013).
It could be that to improve knowledge among adolescents information needs to be tailored specifically for them (García et al., 2016). Adolescents have less interest in fertility than emerging adults (significantly lower fertility knowledge, infertility threat, fertility topic relevance, data not shown) but this difference did not moderate knowledge gain. Other issues to consider is what information should be imparted to different groups and what should be the benchmark for satisfactory knowledge gain. The eight key topics for young people in the ‘A Guide to Fertility’ were assessed via the CFKS and derived from past research and content considered relevant for them from past studies, defining components of fertility awareness and fertility experts. As such we assume the content is appropriate but the presentation of this content suboptimal for young people. Meta-analyses have shown that animations are associated with improved learning (i.e. remembering, understanding, applying, or analysing), especially of natural sciences such as biology (Berney and Bétrancourt, 2016) and may prove to be more useful with adolescents, especially as textual replies suggested they considered the Guide text-heavy.
The cost of providing fertility information was an increase in infertility threat. Recall that infertility threat comprised perceived susceptibility to infertility and perceived severity of this health condition. Most of the negative textual replies young people provided were about how threatening the information was (‘uncomfortable’, ‘quite daunting’, ‘worrying’) despite information being what past studies have recommended be provided and what fertility awareness comprises (e.g. fecundability, age-related fertility trajectory). Infertility threat might have attenuated benefits. However, adolescents provided overall more positive feedback about information. In other health contexts where fear is elicited, an increase is strongly related to motivation to improve health (i.e. seen as a benefit) but only if also accompanied by strong efficacy messages reinforcing ability to make positive health changes (Witte and Allen, 2000). In the present study information was provided but did not address what young people could do if, for example, they were exposed to risks (smoked cigarettes) other than the advice provided in links to trusted sources (e.g. national health service). Future research will need to identify how best to craft messages to guide adolescents and emerging adults to manage the worry fertility health information could elicit as has been done in fertility awareness tools (e.g. FertiSTAT, Bunting and Boivin, 2010) and fertility websites (e.g. yourfertilityorg, Hammarberg et al., 2017b). Initiatives to encourage inclusion of fertility in school curriculum are essential (e.g. Fertility Education Initiative, British Fertility Society, Harper et al. 2017).
The experimental setting for the provision of information may have contributed to the way in which the information was processed. The results showed that feelings of anxiety were elicited (feeling tense, nervous) as a result of participation itself. In the present study all participants read and processed information in groups via computer. One way to mitigate the anxiety of receiving fertility information might therefore be about managing the context of delivery. Previous studies have used clinical settings (Stern et al., 2013), or have instructed participants to complete the study in their own time on any computer with access to the internet (Wojcieszek and Thompson, 2013) but have not checked whether the setting produced anxiety.
We feel confident that better tailoring could help eventual integration of fertility health information in schools. Information evaluation ratings were significantly more positive for fertility education than the control information, and two-thirds of participants provided positive evaluations of the value, benefits and advantages of fertility-related information, whether from a dedicated fertility brochure, or gleaned through healthy pre-pregnancy information (i.e. control). As such the problem of fertility education seems more about tailoring then about the value of including it or not as part of the information young people currently receive or would like to have about fertility health. The World Health Organisation recently presented its approach to sexual and reproductive health (including fertility care), and promoted that both were of ‘equal weight’ to improve sexual health in young people (WHO, 2017). More detailed qualitative research is needed into perceptions of provision of specific fertility information to ascertain how best to make fertility education information beneficial to younger populations.
Limitations
We recognise several limitations to the present study. There was a violation of randomisation (i.e. FertiEduc group among emerging adults more likely to be British). Recruitment was convenience sampling (though with randomisation to groups) from only two education institutions. The two institutions comprised primarily middle class students. Results need to be replicated among young people from a broader socioeconomic background. We did not assess longer-term knowledge gain. Retention over the longer term should be a goal for future studies. Research in older women using online methods shows knowledge was not retained over six months (Daniluk and Koert, 2015). We did not assess what young people do with the information to influence their future fertility. The ‘A Guide to Fertility’ is aimed at improving informed decision-making about risk factors, fertility plans and help-seeking (if required) and these outcomes should be examined in longitudinal studies. According to the results, emerging adults only had one or two years remaining before the optimal time for them to start trying to have children (according to their expressed childbearing preferences) but the information provided did not have an effect on optimality of fertility plans. Factors apart from knowledge influence timing of parenthood (e.g. social structures, normative pressure) and these may emerge as more important in influencing timing than knowledge. Altogether, there is a need for replication but consistency with past research on some findings (e.g. knowledge gain, anxiety) increases confidence that results are valid beyond the specific young people sampled.
Conclusion
The study demonstrated the benefits and costs of the provision of specific fertility information. The mainly positive evaluations of the information suggest that fertility information is welcomed and could be integrated in the wider sexual and reproductive health education curriculum. However, tailoring to specific age groups is required to ensure young people know how to optimally use the information.
Authors’ roles
JB and CH contributed to study planning, development of design and materials, implementation, data collection and analysis, and prepared the first draft of the manuscript. TH, LO, KP and AP contributed to study design, questionnaire development, data collection, editing of the manuscript. EK contributed to study design, questionnaire development and editing of the manuscript.
Funding
The School of Psychology, Cardiff University funded this research.
Conflict of interest
All authors have none to declare.
Supplementary Material
Acknowledgements
Thanks to Amea Sandhu for helpful input in preparation of the study.
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. New York: Sage, 1991. [Google Scholar]
- Berney S, Bétrancourt M. Does animation enhance learning? A meta-analysis. Comput. Educ 2016;101:150–167. [Google Scholar]
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, Bakken S, Patrick Kaplan C, Squiers L, Fabrizio C et al. . How we design feasibility studies. Am J Prev Med 2009;36:452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bretherick KL, Fairbrother N, Avila L, Harbord SH, Robinson WP. Fertility and aging: do reproductive-aged Canadian women know what they need to know? Fertil Steril 2010;93:2162–2168. [DOI] [PubMed] [Google Scholar]
- Bunting L, Boivin J. Development and preliminary validation of the fertility status awareness tool: FertiSTAT. Human Reprod 2010;25:1722–1733. [DOI] [PubMed] [Google Scholar]
- Bunting L, Tsibulsky I, Boivin J. Fertility knowledge and beliefs about fertility treatment: findings from the International Fertility Decision-making Study. Hum Reprod 2013;28:385–397. [DOI] [PubMed] [Google Scholar]
- Byamugisha JK, Mirembe FM, Faxelid E, Gemzell-Danielsson K. Emergency contraception and fertility awareness among university students in Kampala, Uganda. Afr Health Sci 2006;6:194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev 2010;30:879–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan CHY, Chan THY, Peterson BD, Lampic C, Tam MYJ. Intentions and attitudes towards parenthood and fertility awareness among Chinese university students in Hong Kong: a comparison with Western samples. Hum Reprod 2014;30:364–372. [DOI] [PubMed] [Google Scholar]
- Daniluk J, Koert E. Fertility awareness online: the efficacy of a fertility education website in increasing knowledge and changing fertility beliefs. Hum Reprod 2015;30:353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García D, Vassena R, Prat A, Vernaeve V. Increasing fertility knowledge and awareness by tailored education: a randomized controlled trial. Reprod Biomed Online 2016;32:113–120. [DOI] [PubMed] [Google Scholar]
- Habbema JDF, Eijkemans MJ, Leridon H, te Velde ER. Realizing a desired family size: when should couples start? Hum Reprod 2015;30:2215–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammarberg K, Collins V, Holden C, Young K, McLachlan R. Men’s knowledge, attitudes and behaviours relating to fertility. Hum Reprod Update 2017. a;23:458–480. [DOI] [PubMed] [Google Scholar]
- Hammarberg K, Norman RJ, Robertson S, McLachlan R, Michelmore J, Johnson L. Development of a health promotion programme to improve awareness of factors that affect fertility, and evaluation of its reach in the first 5 years. Reprod BioMed Society Online 2017. b;4:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper J, Boivin J, O’Neill HC, Brian K, Dhingra J, Dugdale G, Edwards G, Emmerson L, Grace B, Hadley A et al. . The need to improve fertility awareness. Reprod BioMed 2017;4:18–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Shen F. Effects of cultural tailoring on persuasion in cancer communication: a meta‐analysis. J Commun 2016;66:694–715. [Google Scholar]
- Lampic C, Svanberg AS, Karlström P, Tydén T. Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum Reprod 2006;21:558–564. [DOI] [PubMed] [Google Scholar]
- Lancastle D, Boivin J. A feasibility study of a brief coping intervention (PRCI) for the waiting period before a pregnancy test during fertility treatment. Hum Reprod 2008;23:2299. [DOI] [PubMed] [Google Scholar]
- Maeda E, Nakamura F, Kobayashi Y, Boivin J, Sugimori H, Murata K, Saito H. Effects of fertility education on knowledge, desires and anxiety among the reproductive-aged population: findings from a randomized controlled trial. Hum Reprod 2016;31:2051–2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Bekker H. The development of a six‐item short‐form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br J Clin Psychol 1992;31:301–306. [DOI] [PubMed] [Google Scholar]
- Meissner C, Schippert C, von Versen-Höynck F. Awareness, knowledge, and perceptions of infertility, fertility assessment, and assisted reproductive technologies in the era of oocyte freezing among female and male university students. J Assist Reprod Genet 2016;33:719–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogilevkina I, Stern J, Melnik D, Getsko E, Tydén T. Ukrainian medical students’ attitudes to parenthood and knowledge of fertility. Eur J Contracept Reprod Health Care 2016;21:189–194. [DOI] [PubMed] [Google Scholar]
- Quach S, Librach C. Infertility knowledge and attitudes in urban high school students. Fertil Steril 2008;90:2099–2106. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. The health belief model: explaining health behavior through expectancies In: Glanz K, Lewis FM, Rimers BK (eds). Health Behavior and Health Education. San Francisco, CA: Jossey-Bass, 1990, 39–62. [Google Scholar]
- Rouchou B, Forde MS. Infertility knowledge, attitudes, and beliefs of college students in Grenada. Sci J Public Health 2015;3:353. [Google Scholar]
- Rovei V, Gennarelli G, Lantieri T, Casano S, Revelli A, Massobrio M. Family planning, fertility awareness and knowledge about Italian legislation on assisted reproduction among Italian academic students. Reprod Biomed Online 2010;20:873–879. [DOI] [PubMed] [Google Scholar]
- Sabarre KA, Khan Z, Whitten AN, Remes O, Phillips KP. A qualitative study of Ottawa university students’ awareness, knowledge and perceptions of infertility, infertility risk factors and assisted reproductive technologies (ART). Reprod Health 2013;10:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setterlind S, Larsson G. The stress profile: a psychosocial approach to measuring stress. Stress Health 1995;11:85–92. [Google Scholar]
- Stern J, Larsson M, Kristiansson P, Tydén T. Introducing reproductive life plan-based information in contraceptive counselling: an RCT. Hum Reprod 2013;28:2450–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suka M, Odajima T, Kasai M, Igarashi A, Ishikawa H, Kusama M, Nakayama T, Sumitani M, Sugimori H. The 14-item Health Literacy Scale for Japanese adults (HLS-14). Environ Health Prev Med 2013;18:407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tydén T, Svanberg AS, Karlström PO, Lihoff L, Lampic C. Female university students’ attitudes to future motherhood and their understanding about fertility. Eur J Contracept Reprod Health Care 2006;11:181–189. [DOI] [PubMed] [Google Scholar]
- Virtala A, Vilska S, Huttunen T. Kunttu K. Childbearing, the desire to have children, and awareness about the impact of age on female fertility among Finnish university students. Eur J Contracept Reprod Health Care 2011;16:108–115. [DOI] [PubMed] [Google Scholar]
- Williamson LE, Lawson KL, Downe PJ, Pierson RA. Informed reproductive decision-making: the impact of providing fertility information on fertility knowledge and intentions to delay childbearing. Int J Gynecol Obstet Canada 2014;36:400–405. [DOI] [PubMed] [Google Scholar]
- Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav 2000;27:591–615. [DOI] [PubMed] [Google Scholar]
- Wojcieszek AM, Thompson R. Conceiving of change: a brief intervention increases young adults’ knowledge of fertility and the effectiveness of in vitro fertilization. Fertil Steril 2013;100:523–529. [DOI] [PubMed] [Google Scholar]
- World Health Organization Sexual health and its linkages to reproductive health: an operational approach In Sexual health and its linkages to reproductive health: an operational approach. 2017.
- Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, Rienzi L, Sunde A, Schmidt L, Cooke ID et al. . The international glossary on infertility and fertility care. Fertil Steril 2017;32:1786–1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.