Abstract
Rationale
Binge drinking during adolescence is common and adolescents and young adults with alcohol problems may also have sleep difficulties. However, few studies have documented the effects of a history of adolescent binge drinking on sleep in young adulthood in high-risk minority populations.
Objectives
To quantify sleep disturbance, as indexed by the Pittsburgh Sleep Quality Index (PSQI), in a sample of young adult Mexican American and American Indian men and women (18–30yrs, n=800) with and without a history of alcohol binge drinking during adolescence, controlling for age, gender and race.
Results
Gender was found to affect PSQI responses with females reporting waking up at night, having more bad dreams, and later habitual bedtimes than males, and males reporting more problems with breathing and snoring. Increasing age was associated with: snoring or coughing, less hours spent in bed, and later evening bedtimes. Race also influenced the PSQI with American Indians reporting: longer sleep latencies and sleep durations, more hours spent in bed, and more trouble with coughing and snoring than Mexican Americans, and Mexican Americans reporting later bedtimes. A history of adolescent regular binge drinking was associated with: longer sleep latencies, more problems with breathing, bad dreams and an overall higher PSQI total score, when controlling for age, race and gender.
Conclusions
This report suggests, like what has been found in young adults in general population samples, that binge drinking during adolescence is associated with deleterious consequences on sleep quality in young adulthood in these high-risk and understudied ethnic groups.
Keywords: adolescence, alcohol, binge drinking, sleep, PSQI
INTRODUCTION
Several studies indicate that as many as 72% of high school seniors have tried alcohol and almost 30% have been drunk in the past 30 days (Johnston 2009). There is also data to suggest that when adolescents and young adults drink, they often report “binge drinking” (5 or more drinks for boys, 4 or more for girls per drinking occasion) (CDC 2012). Frequent binge drinking has been associated with health risk behaviors in teens (Miller et al. 2007) as well as risk for alcohol use disorders in adolescents and adults (Ehlers et al. 2006; Hasin and Grant 2015). There are also racial differences in the rates of binge drinking with American Indian adolescents having the highest rate of past-month binge drinking as compared to a nationally representative sample of White and Mixed-Race adolescents (Chen et al. 2012).
One health risk associated with adolescent alcohol can be problems in sleep regulation. Adolescents may be particularly sensitive to the ability of substances of abuse to impair sleep (Bartel et al. 2015; Hasler and Clark 2013; Hasler et al. 2014a, 2013a, 2014b, 2015). This is particularly important since adolescence is a time when both sleep problems and drug seeking behaviors begin to increase (Johnston 2009). The prevailing consensus of most studies is that there is a bidirectional relationship between sleep disturbances and substance dependence; with disturbed sleep being both a risk factor for substance use and also a result of its use (see Conroy and Arnedt 2014; Pasch et al. 2012; Pieters et al. 2015; Warren et al. 2017). Although longitudinal studies of childhood and early adolescence substance use and sleep are limited, one study found that chronic insomnia predicted alcohol use in adolescents 12 months after an initial assessment (Roberts et al. 2008) and another found that mother’s rating of early childhood sleep disturbances was associated with an early onset of the use of substances in adolescence (Wong et al. 2004, 2010, 2015). Recently, several longitudinal studies have linked sleep disturbance during adolescence with tobacco use (Bellatorre et al. 2017; Warren et al. 2017) and alcohol use (Miller et al. 2017; Nguyen-Louie et al. 2017; Sivertsen et al. 2015). Additionally, eveningness (a preference for later sleep-wake timing) (Hasler et al. 2017, 2015), and short sleep times (Terry-McElrath et al. 2016) have also been identified as risk factors for alcohol and/or marijuana use in adolescents.
Substance use itself has also been consistently demonstrated to be associated with changes in sleep hygiene in both adults (Chakravorty et al. 2016) and adolescents (see Colrain et al. 2014; Marmorstein 2017; Zhabenko et al. 2016). In one large scale study of adolescents in Japan, the prevalence of sleep disturbance symptoms was found to increase with the amount of alcohol consumed per drinking day as well as the number of days that alcohol was consumed in the previous month (Morioka et al. 2013). These data suggest that the quantity of alcohol use may be particularly important in determining the severity of the sleep disturbance. This study, and others (Bellatorre et al. 2017; Troxel et al. 2015) highlight the importance of considering ethnic groups and gender when evaluating the relationship between substance use and sleep disturbance. For instance, sleep duration in Korea and Japan is particularly short and sleep disturbance is a fairly common health issue in teens (see Morioka et al. 2013), yet alcohol use disorders are typically much lower in Asians. Additionally, women in the U.S. have a later age of onset of alcohol use and lower rates of alcohol use disorders than men (Hasin and Grant 2015), but typically have higher rates of sleep disorders. Thus, the relationship between disturbed sleep and substance use may have both gender and ethnic group risk factors that need to be taken into consideration.
Two ethnic groups where there is a paucity of studies evaluating sleep and substance use are American Indians and Hispanics. Although use of alcohol varies among tribes, as a whole, Native Americans suffer high rates of alcohol and drug dependence, and higher alcohol-related death rates than any other US ethnic group (Beals et al. 2005a, 2005b, Ehlers et al. 2004b; Grant et al. 2015; May 1982; Robin et al. 1998; Shalala et al. 1999). Among drinkers, adult male Hispanics, particularly those born in the U.S., are more likely to drink frequently and consume larger quantities of alcohol than Whites (Caetano et al. 2009, 2012). However, there is considerable heterogeneity across national Hispanic groups with Cubans and Mexican Americans generally being shown to be at higher risk for alcohol use disorders (AUD) and their associated consequences (Caetano et al. 2014; Vega et al. 1998). Drinking by some Hispanics and Native Americans has also been reported to result in higher cirrhosis mortality rates than other ethnic populations (Heron 2013; Stinson et al. 2001). Therefore, studying the effect of binge drinking on sleep in Mexican Americans and American Indians is important in order to address health disparities.
The present set of studies addressed gender and ethnic differences in the effects of adolescent binge drinking on sleep quality by investigating sleep disturbance, as indexed by the Pittsburgh Sleep Quality Index (PSQI), in a large sample of young adult Mexican Americans and American Indians (18–30yrs, n=800) with and without a history of binge drinking during adolescence.
MATERIALS AND METHODS
Human studies
Participants
The participants were individuals of American Indian and Mexican American descent that were recruited from the local community for larger studies investigating risk factors for substance dependence in these two ethnic groups. The American Indians were recruited from eight geographically contiguous reservations with a total population of about 3,000 individuals. They were recruited using a combination of a venue-based method (Kalton 1986; Muhib et al. 2001), and a respondent-driven procedure (Heckathorn 1997), as described previously (see Ehlers et al. 2004a, 2004b). American Indian participants were recruited in a wide age range (18–85 yrs), however, the present set of analyses focused on only those individuals who were between 18 and 30 years of age at the time of interview. Mexican American participants were recruited using a commercial mailing list that provided the addresses of individuals with Hispanic surnames in 11 zip codes in San Diego County, all of which had a population that was over 20% Hispanic and were within 25 miles of the research site. The mailed invitation stated that potential participants must be of Mexican American heritage, be between the ages of 18 and 30 years, be residing in the United States legally, and be able to read and write in English (see Ehlers et al. 2009, 2010, 2017). Based on the aims of the larger studies, for both ethnic groups, participants were excluded if they were pregnant, nursing, or currently had a major medical disorder that precluded them traveling to the research site. Participants were asked to refrain from alcohol or any other substance use for 24 hours prior to testing, and their breathalyzer blood alcohol levels had to be 0.00 g/dl to be included in the study.
Potential participants gave written informed consent, and responded to a screening questionnaire that was used to gather information on demographics, personal medical history, ethnicity and detailed measures of current and past substance abuse history, including adolescent binge drinking, using a time line follow back format (Schuckit 1985). Each participant also completed an interview with the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) (Bucholz et al. 1994) which was used to make DSM diagnoses (Association and DSM-IV 1994). Sleep quality was indexed by the Pittsburgh Sleep Quality Index (PSQI). The PSQI produces a global sleep quality score as well as scores for individual items such as: usual bedtime, actual hours slept, number of minutes to fall asleep, and nighttime awakenings. Global PSQI score was estimated for each participant as described previously (Buysse et al. 1989). The psychometric properties of the PSQI have also been described previously (Carpenter and Andrykowski 1998).
Data Analyses
The data analyses were based on the study aim which was to determine if any associations existed between a history of binge drinking during adolescence and the PSQI items, taking into consideration age, race, and gender. An adolescent history of regular binge drinking was defined as drinking 5 or more drinks for boys and 4 or more drinks for girls per drinking occasion at least once a month during their highest drinking period prior to the age of 19 years. To determine the relationships between binge drinking and the PSQI variables, the total score on the PSQI, and 7 individual items (sleep latency, sleep duration, wake up at night, cannot breathe, cough or snoring, bad dreams, hours in bed) and whether they habitually went to bed after 11:00 PM, were entered as individual predictor variables into a linear regression for continuous outcome variables or a logistic regression for dichotomous outcomes with predictor variables being: history of adolescent binge drinking, age, gender and ethnicity (all entered together). Significance was set at p<0.05.
RESULTS
The sample consisted of American Indian (n=218) and Mexican American (n=582) young adult (18–30 yrs old) participants. As seen in table 1, Fifty-six percent of the sample was female, half the sample was not currently employed, 24% of the sample had an annual income below 20K. The mean age was 23 ± 0.1 yrs, and the mean level of education was 12.93 ± 0.07. Forty six percent (n=369) of the sample reported adolescent binge drinking (5 drinks for men 4 drinks for women per drinking occasion at least once a month during their highest drinking period prior to the age of 19 years). Binge drinkers did not differ on gender or age but were more likely to be American Indian (Chi Square= 41.5, df=1, p<0.001). Adolescent Binge drinkers mean quantity per drinking occasion was 9.84 whereas non-binge drinkers reported drinking 2.15 drinks per drinking occasion. Figure 1 presents the range of the quantity of alcohol drank per occasion in the two ethnic groups.
Table 1.
Demographic characteristics of Mexican American (n=582) and Native American (n=218) participants according to adolescent binge drinking category
| Demographic Characteristic | Adolescent Binge Drinkers | Adolescent Non-Binge Drinkers | ||||||
|---|---|---|---|---|---|---|---|---|
| Mexican American (n=228) | Native American (n=141) | Overall (n=369) | Mexican American (n=354) | Native American (n=77) | Overall (n=431) | |||
|
| ||||||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Gender | ||||||||
| Male | 104 (45.6) | 69 (48.9) | 173 (46.9) | 139 (39.3) | 40 (51.9) | 179 (41.5) | ||
| Female | 124 (54.4) | 72 (51.1) | 196 (53.1) | 215 (60.7) | 37 (48.1) | 252 (58.5) | ||
| Married | ||||||||
| Yes | 35 (15.4) | 5 (3.5) | 40 (10.8) | 55 (15.5) | 2 (2.6) | 57 (13.2) | ||
| No | 193 (84.6) | 136 (96.5) | 329 (89.2) | 299 (84.5) | 75 (97.4) | 374 (86.8) | ||
| Employed | ||||||||
| Yes | 139 (61.0) | 28 (20.3) | 167 (45.6) | 201 (57.1) | 25 (32.9) | 226 (52.8) | ||
| No | 89 (39.0) | 110 (79.7) | 199 (54.4) | 151 (42.9) | 51 (67.1) | 202 (47.2) | ||
| Income ≥ $20,000/yr | ||||||||
| Yes | 174 (81.7) | 75 (62.5) | 249 (74.8) | 257 (76.9) | 47 (72.3) | 304 (76.2) | ||
| No | 39 (18.3) | 45 (37.5) | 84 (25.2) | 77 (23.1) | 18 (27.7) | 95 (23.8) | ||
| Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | Mean (SE) | |||
| Age (yrs) | 23.7 (0.2) | 21.5 (0.3) | 22.9 (0.2) | 23.7 (0.2) | 20.7 (0.4) | 23.2 (0.2) | ||
| Education (yrs) | 13.2 (0.1) | 11.6 (0.1) | 12.6 (0.1) | 13.5 (0.1) | 11.8 (0.2) | 13.2 (0.1) | ||
| Adolescent Binge Drinking Quantity (drinks/occasion) | 7.96 (0.4) | 12.86 (0.8) | 9.84 (0.4) | 2.19 (0.1) | 1.99 (0.2) | 2.15 (0.1) | ||
Figure 1.
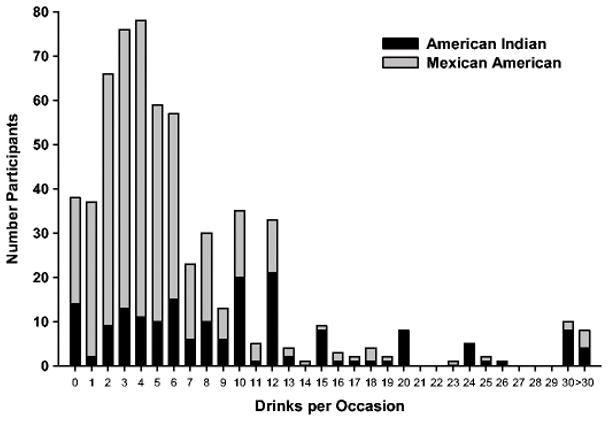
Quantity of drinking per occasion during the participants’ heaviest drinking period during adolescence (<age 19). Number of drinks per drinking occasion is shown for American Indians (black, N=188) and Mexican Americans (grey, N=442).
As seen in Table 2, gender was significantly associated with several items on the PSQI. Females were significantly more likely to wake up at night, report more bad dreams, and were more likely to have a later habitual bedtime. Whereas males were significantly more likely to report problems with breathing and snoring (all p’s <0.05). Increasing age was also associated with: a greater likelihood to snore or cough (t=1.93, p<0.05), a decrease in the number of hours spent in bed (t=−2.32, p<0.02), and later evening bedtimes (t=5.26, p>0.02) (data not shown). Race was also found to influence the PSQI with American Indians reporting: significantly longer sleep latencies and sleep durations, more hours spent in bed, and more trouble with coughing and snoring and Mexican Americans reporting later bedtimes, as also seen in table 2 (all p’s<0.05). As seen in table 3, a history of adolescent regular binge drinking was also found to be significantly associated with current responses on the PSQI using regression analyses that included age, race, and gender. Binge drinkers had: significantly longer sleep latencies, reported more problems with breathing and bad dreams and had an overall higher PSQI total score (all p’s<0.05).
Table 2.
Age and Gender effects on PSQI responses
| Gender | Regression | Race | Regression | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Male | Female | t stat | Pvalue | Δ | AI | MA | t stat | Pvalue | Δ | |
| Sleep latency | 28.4 ±1.8 | 27.9 ±1.1 | −0.007 | NS | 34.3 ±2.4 | 25.9 ±1.0 | −2.687 | 0.007 | AI>MA | |
|
| ||||||||||
| Sleep duration | 7.3 ±0.09 | 7.5 ±0.08 | 1.709 | NS | 7.8 ±0.14 | 7.3 ±0.06 | −3.001 | 0.003 | AI>MA | |
|
| ||||||||||
| Wake up at night | 1.2 ±0.06 | 1.3 ±0.05 | 2.006 | 0.05 | F>M | 1.3 ±0.07 | 1.3 ±0.05 | −0.19 | NS | |
|
| ||||||||||
| Cannot breathe comfortably | 0.3 ±0.03 | 0.2 ±0.03 | −2.36 | 0.02 | M>F | 0.2 ±0.04 | 0.2 ±0.02 | 0.304 | NS | |
|
| ||||||||||
| Cough or snore loudly | 0.5 ±0.05 | 0.3 ±0.03 | −3.974 | 0.0001 | M>F | 0.4 ±0.06 | 0.3 ±0.03 | −2.073 | 0.04 | AI>MA |
|
| ||||||||||
| Bad dreams | 0.5 ±0.05 | 0.7 ±0.04 | 2.053 | 0.04 | F>M | 0.6 ±0.06 | 0.6 ±0.03 | 0.048 | NS | |
|
| ||||||||||
| PSQI total score | 4.7 ±0.17 | 4.9 ±0.15 | 0.905 | NS | 4.9 ±0.24 | 4.7 ±0.13 | −0.2 | NS | ||
|
| ||||||||||
| Hours in bed | 8.3 ±0.09 | 8.4 ±0.07 | 1.778 | NS | 8.7 ±0.13 | 8.2 ±0.06 | −2.815 | 0.005 | AI>MA | |
|
| ||||||||||
| Bedtime >11pm | 73% ±2.4 | 61% ±2.2 | 12.36 a | 0.0001 | F>M | 62% ±3.3 | 68% ±1.9 | 7.96 a | 0.005 | MA>AI |
Means ± standard error and regression statistics shown for PSQI items for gender (M=male, F=female) and race (AI= American Indian, MA= Mexican American) as predictor variables. Δ indicates statistically significant items on the PSQI, > indicates direction of difference.
Value is a Wald stat.
Table 3.
History of Adolescent Binge drinking and current PSQI responses
| Adolescent Binge | Regression | ||||
|---|---|---|---|---|---|
|
|
|||||
| No | Yes | t stat | Pvalue | Δ | |
| Sleep latency | 25.3 ±1.2 | 32.0 ±1.8 | 2.513 | 0.012 | B>NB |
|
| |||||
| Sleep duration | 7.4 ±0.07 | 7.5 ±0.1 | 0.403 | NS | |
|
| |||||
| Wake up at night | 1.2 ±0.05 | 1.3 ±0.06 | 1.405 | NS | |
|
| |||||
| Cannot breathe comfortably | 0.1 ±0.02 | 0.3 ±0.04 | 3.583 | 0.0001 | B>NB |
|
| |||||
| Cough or snore loudly | 0.3 ±0.04 | 0.4 ±0.04 | 0.605 | NS | |
|
| |||||
| Bad dreams | 0.5 ±0.04 | 0.7 ±0.05 | 2.808 | 0.005 | B>NB |
|
| |||||
| PSQI total score | 4.6 ±0.15 | 5.1 ±0.18 | 1.969 | 0.049 | B>NB |
|
| |||||
| Hours in bed | 8.3 ±0.07 | 8.5 ±0.09 | 0.735 | NS | |
|
| |||||
| Bedtime >11pm | 65% ±2.3 | 67% ±2.5 | 0.81a | NS | |
Means ± standard error and regression statistics shown for PSQI items for adolescent bingeing (B) or not (NB) as the predictor variables. Δ indicates statistically significant items on the PSQI, > indicates direction of difference.
Value is a Wald stat.
DISCUSSION
Alcohol and other substance use, especially during early adolescence, has been linked to a number of long-terms health risks that include elevated risk for dependence later in life in a number of populations (Dawson et al. 2008; Ehlers et al. 2006). Adolescent substance use is also frequently associated with problems in sleep. Adolescents may be particularly sensitive to the ability of substances of abuse to impair sleep (Bartel et al. 2015; Hasler and Clark 2013; Hasler et al. 2014a, 2013a, 2014b, 2015), and the prevailing consensus of most studies is that there is a bidirectional relationship between substance use and sleep disturbances with disturbed sleep being both a risk factor for and a consequence of substance use (see Conroy and Arnedt 2014; Pasch et al. 2012; Pieters et al. 2015; Warren et al. 2017). This complex relationship between substance use and sleep may have a more substantial impact among vulnerable groups that have a disproportionate burden of substance use disorders (Grant et al. 2015). For instance, American Indian (AI) teens have the highest rates of alcohol and other drug use disorders of all ethnic groups, (Kim et al. 2012; Miller et al. 2012; Stanley et al. 2014; Wu et al. 2011). Yet there have been few studies evaluating the relationship between sleep and substance use in ethnic minority teens. We have found, in one group of American Indian young adults, that high rates of adolescent binge drinking are reported (Ehlers et al. 2014). In our present study, we found that this group of AI also had a longer sleep latency and sleep duration, as well as more complaints of breathing difficulties and coughing and snoring, and spent a longer number of hours in bed as compared to Mexican American (MA) young adults living in the same county. Interestingly, in the MA young adult population more participants reported later habitual bedtimes than the AI participants. The AI in the present study live in rural areas of the county as compared to the Mexican American young adults who are from urban and suburban areas. Thus, differences in eveningness could potentially differ based on rurality or cultural/family differences between the groups. Ethnic differences in eveningness have been reported in studies in Asia where short sleep and other sleep disturbance in adolescents is not rare and thus represents a common health issue (see Morioka et al. 2013).
We also found some differences in sleep in our present population of AI and MA young adults based on age and gender. Only 3 PSQI variables were found to differ based on age, with older participants reporting less time in bed, and increased tendency to have a later habitual bedtime, and they were more likely to report coughing or snoring. Gender differences were also observed in our study with women reporting waking up at night more often, having bad dreams and having a later habitual bedtime whereas men were more likely to report breathing, coughing or snoring problems. These data are consistent with the findings that risk for developing insomnia is 1.41 times greater in women (Manber et al. 2006). However, several studies have shown that the frequency of insomnia in patients receiving treatment for alcohol dependence did not differ between men and women (Brower 2001, 2001). Additionally, in another study, of recovering alcoholics, men appeared to have poorer sleep efficiency and more deficits in SWS than women, however, since no sex by diagnosis interactions were found the authors suggested that alcoholism does not differentially influence the sleep of men and women (Colrain et al. 2009). No sex differences in the acute effects of alcohol on the sleep in older adolescents were seen in another study (Chan et al. 2013). It has been suggested that larger groups of men and women are needed in order to fully study sex effects of alcohol on sleep (Colrain et al. 2014).
An adolescent history of binge drinking was found to be associated with a higher total score on the PSQI, in the present study, even taking into account: gender, age, and race. Decreases in sleep quality have been reported previously associated with alcohol use and alcohol use disorders in a number of populations, although studies are sparse in minorities (see Ehlers et al. 2010, 2017). An adolescent history of binge drinking was also associated with a longer sleep latency, trouble breathing, and having bad dreams. Dreams play an important cultural role in American Indians, and in AI veterans, trauma-related nightmares appear to be more common than what has been reported for other veteran populations (Shore et al. 2009). These data suggest that assessing young adults for bad dreams, difficulty falling asleep, and overall poorer sleep quality may be important in screening for substance associated sleep disturbances in these minority populations. These studies also suggest that the circadian contributions to sleep disturbances and substance use disorders seen in adolescents (Hasler et al. 2017, 2015) may be influenced by environmental and cultural factors in minority populations, such as what has been reported in Asians (Morioka et al. 2013) and what we found in the current study.
In conclusion, these data represent the first association analysis of sleep quality with a history of regular binge drinking during adolescence in American Indian and Mexican American populations. The results of this study should, however, be interpreted in the context of several limitations. First, the findings may not generalize to other American Indians or Mexican American young adults. Second, comparisons of association findings to non-American Indian or non-Mexican populations may be limited by differences in a host of potential demographic, genetic and environmental variables. Some of the data collected were retrospective and thus may suffer from problems of inaccurate recall. A longitudinal study of the relationship between adolescent binge drinking and the PSQI would represent a more powerful study design. Despite these limitations, this report represents an important step in an ongoing investigation to understand the developmental determinants associated with substance use disorders in high-risk and understudied ethnic groups.
Acknowledgments
FUNDING SOURCES
National Institutes of Health (NIH) funding for this study was provided by the National Institute on Alcoholism and Alcohol Abuse (NIAAA) AA006420, 5R37 AA010201, to CLE.
The authors wish to acknowledge the technical support of: Corrine Kim, Evie Phillips, Jessica Benedict, Mellany Santos and Philip Lau.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interests. The experiments comply with the current laws of the country in which they were performed.
References
- (CDC) CfDCaP. Vital signs: Binge drinking prevalence, frequency, and intensity among adults - United States 2010. MMWR Morb Mortal Wkly Rep. 2012;61:14–19. [PubMed] [Google Scholar]
- Association AP, DSM-IV TFo. Diagnostic and statistical manual of mental disorders (DSM-IV) American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Arch Gen Psychiatry. 2005a;62:99–108. doi: 10.1001/archpsyc.62.1.99. [DOI] [PubMed] [Google Scholar]
- Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Manson SM. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. Am J Psychiatry. 2005b;162:1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- Bellatorre A, Choi K, Lewin D, Haynie D, Simons-Morton B. Relationships Between Smoking and Sleep Problems in Black and White Adolescents. Sleep. 2017:40. doi: 10.1093/sleep/zsw031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brower KJ. Alcohol’s effects on sleep in alcoholics. Alcohol Res Health. 2001;25:110–125. [PMC free article] [PubMed] [Google Scholar]
- Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF. Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry. 2001;158:399–404. doi: 10.1176/appi.ajp.158.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, et al. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Caetano R, Mills BA, Vaeth PAC, Reingle J. Age at First Drink, Drinking, Binge Drinking, and DSM-5 Alcohol Use Disorder Among Hispanic National Groups in the United States. Alcoholism-Clinical and Experimental Research. 2014;38:1381–1389. doi: 10.1111/acer.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): The association between birthplace, acculturation and alcohol abuse and dependence across Hispanic national groups. Drug and Alcohol Dependence. 2009;99:215–221. doi: 10.1016/j.drugalcdep.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caetano R, Vaeth PA, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): Acculturation, Birthplace and Alcohol-Related Social Problems Across Hispanic National Groups. Hisp J Behav Sci. 2012;31:95–117. doi: 10.1177/0739986311424040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- Chakravorty S, Chaudhary NS, Brower KJ. Alcohol Dependence and Its Relationship With Insomnia and Other Sleep Disorders. Alcohol Clin Exp Res. 2016;40:2271–2282. doi: 10.1111/acer.13217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan JK, Trinder J, Andrewes HE, Colrain IM, Nicholas CL. The acute effects of alcohol on sleep architecture in late adolescence. Alcohol Clin Exp Res. 2013;37:1720–1728. doi: 10.1111/acer.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HJ, Balan S, Price RK. Association of contextual factors with drug use and binge drinking among White, Native American, and Mixed-Race adolescents in the general population. J Youth Adolesc. 2012;41:1426–1441. doi: 10.1007/s10964-012-9789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colrain IM, Nicholas CL, Baker FC. Alcohol and the sleeping brain. Handb Clin Neurol. 2014;125:415–431. doi: 10.1016/B978-0-444-62619-6.00024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colrain IM, Turlington S, Baker FC. Impact of alcoholism on sleep architecture and EEG power spectra in men and women. Sleep. 2009;32:1341–1352. doi: 10.1093/sleep/32.10.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy DA, Arnedt JT. Sleep and substance use disorders: an update. Curr Psychiatry Rep. 2014;16:487. doi: 10.1007/s11920-014-0487-3. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Chou SP, Ruan WJ, Grant BF. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res. 2008;32:2149–2160. doi: 10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Gilder DA, Criado JR, Caetano R. Acculturation stress, anxiety disorders, and alcohol dependence in a select population of young adult Mexican Americans. J Addict Med. 2009;3:227–233. doi: 10.1097/ADM.0b013e3181ab6db7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Gilder DA, Criado JR, Caetano R. Sleep quality and alcohol-use disorders in a select population of young-adult Mexican Americans. J Stud Alcohol Drugs. 2010;71:879–884. doi: 10.15288/jsad.2010.71.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Gilder DA, Wall TL, Phillips E, Feiler H, Wilhelmsen KC. Genomic screen for loci associated with alcohol dependence in Mission Indians. Am J Med Genet B Neuropsychiatr Genet. 2004a;129B:110–115. doi: 10.1002/ajmg.b.30057. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Slutske WS, Gilder DA, Lau P, Wilhelmsen KC. Age at first intoxication and alcohol use disorders in Southwest California Indians. Alcohol Clin Exp Res. 2006;30:1856–1865. doi: 10.1111/j.1530-0277.2006.00222.x. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Stouffer GM, Gilder DA. Associations between a history of binge drinking during adolescence and self-reported responses to alcohol in young adult Native and Mexican Americans. Alcohol Clin Exp Res. 2014;38:2039–2047. doi: 10.1111/acer.12466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Wall TL, Betancourt M, Gilder DA. The clinical course of alcoholism in 243 Mission Indians. Am J Psychiatry. 2004b;161:1204–1210. doi: 10.1176/appi.ajp.161.7.1204. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Wills DN, Lau P, Gilder DA. Sleep Quality in an Adult American Indian Community Sample. J Clin Sleep Med. 2017;13:385–391. doi: 10.5664/jcsm.6486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, et al. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1609–1640. doi: 10.1007/s00127-015-1088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Clark DB. Circadian misalignment, reward-related brain function, and adolescent alcohol involvement. Alcohol Clin Exp Res. 2013;37:558–565. doi: 10.1111/acer.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, et al. Eveningness and Later Sleep Timing Are Associated with Greater Risk for Alcohol and Marijuana Use in Adolescence: Initial Findings from the National Consortium on Alcohol and Neurodevelopment in Adolescence Study. Alcohol Clin Exp Res. 2017;41:1154–1165. doi: 10.1111/acer.13401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Martin CS, Wood DS, Rosario B, Clark DB. A longitudinal study of insomnia and other sleep complaints in adolescents with and without alcohol use disorders. Alcohol Clin Exp Res. 2014a;38:2225–2233. doi: 10.1111/acer.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Sitnick SL, Shaw DS, Forbes EE. An altered neural response to reward may contribute to alcohol problems among late adolescents with an evening chronotype. Psychiatry Res. 2013;214:357–364. doi: 10.1016/j.pscychresns.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Soehner AM, Clark DB. Circadian rhythms and risk for substance use disorders in adolescence. Curr Opin Psychiatry. 2014b;27:460–466. doi: 10.1097/YCO.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Soehner AM, Clark DB. Sleep and circadian contributions to adolescent alcohol use disorder. Alcohol. 2015;49:377–387. doi: 10.1016/j.alcohol.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44:174–199. [Google Scholar]
- Heron M. National vital statistics report. Vol. 62. National Center for Health Statistics; Hyattsville, MD: 2013. Deaths: Leading causes for 2010. [Google Scholar]
- Johnston LDOMPM, Bachman JG, Schulenberg JE. Monitoring the future national results on adolescent drug use: Overview of key findings 2008. 2009. (NIH Publication No. 09-7401) [Google Scholar]
- Kalton GA, DW Sampling Rare Populations. J Roy Stat Soc. 1986;149:65–82. [Google Scholar]
- Kim AK, Brown RM, Lawrence AJ. The role of orexins/hypocretins in alcohol use and abuse: an appetitive-reward relationship. Front Behav Neurosci. 2012;6:78. doi: 10.3389/fnbeh.2012.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manber R, Baker FC, Gress JL. Sex differences in sleep and sleep disorders: a focus on women’s sleep. Int J Sleep Disorders. 2006;1:7–15. [Google Scholar]
- Marmorstein NR. Sleep patterns and problems among early adolescents: Associations with alcohol use. Addict Behav. 2017;66:13–16. doi: 10.1016/j.addbeh.2016.11.002. [DOI] [PubMed] [Google Scholar]
- May PA. Substance abuse and American Indians: prevalence and susceptibility. Int J Addict. 1982;17:1185–1209. doi: 10.3109/10826088209056349. [DOI] [PubMed] [Google Scholar]
- Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among high school students. Pediatrics. 2007;119:76–85. doi: 10.1542/peds.2006-1517. [DOI] [PubMed] [Google Scholar]
- Miller KA, Stanley LR, Beauvais F. Regional differences in drug use rates among American Indian youth. Drug Alcohol Depend. 2012;126:35–41. doi: 10.1016/j.drugalcdep.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Janssen T, Jackson KM. The Prospective Association Between Sleep and Initiation of Substance Use in Young Adolescents. J Adolesc Health. 2017;60:154–160. doi: 10.1016/j.jadohealth.2016.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morioka H, et al. Associations between sleep disturbance and alcohol drinking: A large-scale epidemiological study of adolescents in Japan. Alcohol. 2013;47:619–628. doi: 10.1016/j.alcohol.2013.09.041. [DOI] [PubMed] [Google Scholar]
- Muhib FB, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl 1):216–222. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Louie TT, Brumback T, Worley MJ, Colrain IM, Matt GE, Squeglia LM, Tapert SF. Effects of sleep on substance use in adolescents: a longitudinal perspective. Addict Biol. 2017 doi: 10.1111/adb.12519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. J Youth Adolesc. 2012;41:1184–1196. doi: 10.1007/s10964-012-9784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieters S, Burk WJ, Van der Vorst H, Dahl RE, Wiers RW, Engels RC. Prospective relationships between sleep problems and substance use, internalizing and externalizing problems. J Youth Adolesc. 2015;44:379–388. doi: 10.1007/s10964-014-0213-9. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Duong HT. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42:294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin RW, Long JC, Rasmussen JK, Albaugh B, Goldman D. Relationship of binge drinking to alcohol dependence, other psychiatric disorders, and behavioral problems in an American Indian tribe. Alcohol Clin Exp Res. 1998;22:518–523. [PubMed] [Google Scholar]
- Schuckit MA. Genetics and the risk for alcoholism. JAMA. 1985;254:2614–2617. [PubMed] [Google Scholar]
- Shalala DE, Trujillo MH, Hartz PE, Paisano EL. Trends in Indian health 1998–99. v. United States Department Health and Human Services; Indian Health Service; Division of Program Statistics; Washington, D.C: 1999. [Google Scholar]
- Shore JH, Orton H, Manson SM. Trauma-related nightmares among American Indian veterans: views from the dream catcher. Am Indian Alsk Native Ment Health Res. 2009;16:25–38. doi: 10.5820/aian.1601.2009.25. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Skogen JC, Jakobsen R, Hysing M. Sleep and use of alcohol and drug in adolescence. A large population-based study of Norwegian adolescents aged 16 to 19 years. Drug Alcohol Depend. 2015;149:180–186. doi: 10.1016/j.drugalcdep.2015.01.045. [DOI] [PubMed] [Google Scholar]
- Stanley LR, Harness SD, Swaim RC, Beauvais F. Rates of substance use of American Indian students in 8th, 10th, and 12th grades living on or near reservations: update, 2009–2012. Public Health Rep. 2014;129:156–163. doi: 10.1177/003335491412900209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res. 2001;25:1181–1187. [PubMed] [Google Scholar]
- Terry-McElrath YM, Maslowsky J, O’Malley PM, Schulenberg JE, Johnston LD. Sleep and Substance Use among US Adolescents, 1991–2014. Am J Health Behav. 2016;40:77–91. doi: 10.5993/AJHB.40.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Ewing B, D’Amico EJ. Examining Racial/Ethnic Disparities in the Association between Adolescent Sleep and Alcohol or Marijuana. Use Sleep Health. 2015;1:104–108. doi: 10.1016/j.sleh.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Alderete E, Kolody B, Aguilar-Gaxiola S. Illicit drug use among Mexicans and Mexican Americans in California: the effects of gender and acculturation. Addiction. 1998;93:1839–1850. doi: 10.1046/j.1360-0443.1998.931218399.x. [DOI] [PubMed] [Google Scholar]
- Warren CM, Riggs NR, Pentz MA. Longitudinal relationships of sleep and inhibitory control deficits to early adolescent cigarette and alcohol use. J Adolesc. 2017;57:31–41. doi: 10.1016/j.adolescence.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcohol Clin Exp Res. 2004;28:578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Nigg JT, Zucker RA. Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcohol Clin Exp Res. 2010;34:1033–1044. doi: 10.1111/j.1530-0277.2010.01178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcohol Clin Exp Res. 2015;39:355–362. doi: 10.1111/acer.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhabenko O, et al. Substance Use as a Risk Factor for Sleep Problems Among Adolescents Presenting to the Emergency Department. J Addict Med. 2016;10:331–338. doi: 10.1097/ADM.0000000000000243. [DOI] [PMC free article] [PubMed] [Google Scholar]


