Abstract
Fibromyalgia (FM) is characterized by chronic widespread pain, unrefreshing sleep, physical exhaustion, and cognitive difficulties. It occurs in all populations throughout the world, with prevalence between 2% and 4% in general populations. Definition, pathogenesis, diagnosis, and treatment of FM remain points of contention, with some even contesting its existence. The various classification systems according to pain medicine, psychiatry, and neurology (pain disease; persistent somatoform pain disorder; masked depression; somatic symptom disorder; small fiber neuropathy; brain disease) mostly capture only some components of this complex and heterogeneous disorder. The diagnosis can be established in most cases by a general practitioner when the symptoms meet recognized criteria and a somatic disease sufficiently explaining the symptoms is excluded. Evidence-based interdisciplinary guidelines give a strong recommendation for aerobic exercise and cognitive behavioral therapies. Drug therapy is not mandatory. Only a minority of patients experience substantial symptom relief with duloxetine, milnacipran, and pregabalin.
Keywords: depression, fibromyalgia, small fiber neuropathy, somatic symptom disorder, somatoform disorder
Abstract
La fibromialgia (FM) se caracteriza por dolor crónico generalizado, sueño no reparador, agotamiento físico y dificultades cognitivas. Ella se presenta en todas las poblaciones a través del mundo, con una prevalencia entre el 2% y el 4% en la población general. La definición, la patogénesis, el diagnóstico y el tratamiento de la FM constituyen puntos de discusión, con algunos autores que incluso dudan de su existencia. Los diversos sistemas de clasificación de acuerdo con la medicina, la psiquiatría y la neurología del dolor (patología dolorosa, trastorno de dolor somatomorfo persistente, depresión enmascarada, trastorno de síntoma somático, neuropatía de fibra pequeña, enfermedad cerebral) en su mayoría incorporan sólo algunos componentes de este complejo y heterogéneo trastorno. En la mayoría de los casos un médico general puede establecer el diagnóstico, cuando los síntomas reúnen criterios reconocidos y se excluye una enfermedad somática que pueda explicar suficientemente dichos síntomas. Las guías interdisciplinarias basadas en la evidencia entregan una sólida recomendación respecto al ejercicio aeróbico y las terapias cognitivo conductuales. La terapia farmacológica no es obligatoria. Sólo una minoría de los pacientes presenta un alivio sintomático significativo con duloxetina, milnacipran y pregabalina.
Abstract
La fibromyalgie (FM) se caractérise par des douleurs chroniques généralisées, un sommeil non réparateur, un épuisement physique et des difficultés cognitives. Elle survient dans toutes les populations du monde, avec une prévalence entre 2 % et 4 % de la population générale. La définition, la pathogenèse, le diagnostic et le traitement de la FM restent un point de discorde, quelques-uns contestant même son existence. Les systèmes de classification variés selon la médecine, la psychiatrie et la neurologie de la douleur, (pathologie douloureuse ; trouble douloureux somatoforme persistant ; dépression masquée ; trouble à symptomatologie somatique ; neuropathie des petites fibres ; maladie cérébrale) n'appréhendent principalement que quelques composantes de ce trouble complexe et hétérogène. Le diagnostic peut être établi dans la plupart des cas par un généraliste quand les symptômes rencontrés remplissent les critères et quand une maladie somatique capable d'expliquer les symptômes est exclue. Des recommandations interdisciplinaires fondées sur des éléments probants recommandent fortement les exercices aérobiques et les thérapies cognitivo-comportementales. Le traitement médicamenteux n'est pas obligatoire. Seule une minorité de patients sont soulagés par la duloxétine, le milnacipran et la prégabaline.
Introduction
Many physicians—particularly rheumatologists, pain specialists, and general practitioners, but also mental health care specialists—have experience of patients who describe chronic widespread pain (pain all over the body), which is associated with a range of other symptoms including poor sleep, fatigue, and depression. This complex set of symptoms is now recognized as fibromyalgia (FM), but remains a challenging concept for numerous reasons.1
FM is “a bitterly controversial condition.”2 FM “wars” are fought on the legitimacy and clinical usefulness of the diagnostic label “FM,” the nosological classification, suggested etiology and pathophysiology, “ownership,” and the preferred treatment options.2,3
In the past 30 years, the scientific publications on FM have increased considerably. This surge might be explained by an increased awareness and shared interest of a number of stakeholders, including the patients who are suffering, patient self-help organizations, clinicians, researchers, and the pharmaceutical industry. This recognition of FM will serve to promote research to understand the underlying pathophysiology and thereby improve therapy. Beyond the altruistic goals of understanding and treating an illness, other factors may play a role in the attention given to FM, including the legitimization of symptoms and sickness for patients, influence for academics, economic gain for pharmaceutical companies, and legal interests.3,4
It is our opinion that some FM “wars” are fought because of the belief systems of medical and psychological specialties, the interests of patient self-help organizations, financial advantages for the pharmaceutical industry, and personal academic advancement, rather than the objective of valid scientific and clinical progress.2 Within these disputes, we may observe strong opinions about the nature of FM and treatment recommendations that are contrary to mainstream medicine and the current scientific knowledge. These we identify as the myths of FM.
In this paper, we discuss some of the myths concerning FM, with a special focus on those extolled bymental health specialists (psychiatry, psychosomatic medicine, and clinical psychology) and neurologists. We have based our facts on the interdisciplinary evidencebased clinical guidelines on FM of Canada,5 Germany,6 and the European League Against Rheumatism (EULAR).7 High-quality guidelines, based upon the best available scientific evidence and the clinical experience and consensus of patients with all specialties involved in the management of a disease, are designed to overcome dogmatic belief systems and to give patients, their families, and clinicians a guide to navigate the diagnostic and therapeutic challenges of FM, while respecting the societal context of fiscal responsibility within health care systems.8
Myths and facts
Legitimacy of symptoms
Fibromyalgia does not exist
Many patients diagnosed with FM by a rheumatologist or a pain medicine specialist report having another health care professional state that: “FM does not exist.”6,9 The discussion as to whether FM exists or not raises the question as to what defines the existence of a disease.10 A satisfactory definition of a disease is surprisingly difficult. What can be identified as a disease also changes over time, partly due to changes in diagnostic ability, but often on account of social and economic factors. One example is osteoporosis. Originally recognized as an unavoidable part of normal aging, it became a defined pathology when officially recognized as a disease by the World Health Organization (WHO) in 1994. Once a condition is recognized, numerous advantages accrue, including the validation of the illness and suffering, as well as fiscal advantages, which include treatment reimbursements.11 If official recognition by the WHO is a requirement for designation as a disease, then FM fulfills this condition. In 1994, the 10th revision of the International Classification of Diseases (ICD-10) listed FM under “diseases of the musculoskeletal system and connective tissue.”12 In contrast, if a defined etiology and pathophysiology are required for the definition of a disease, then FM is not a disease.13 The WHO uses the term ”disorder“ throughout the classification of mental disorders, thereby avoiding problems inherent in the use of terms such as “disease” and “illness.” However, “disorder” is not an exact term, but is used to imply the existence of a clinically recognizable set of symptoms or behaviors associated in most cases with distress and interference with personal functions.12 In this context, FM meets the criteria of a disorder.
In addition, the reluctance of some physicians to use the diagnostic label of FM can be explained by the preponderance of the biomedical model in medical practice. The model attributes a key role to biological determinants and explains a disease as a condition caused by external pathogens or disorder in the functions of organs and body systems. A disease is diagnosed by objective findings such as laboratory tests, imaging, or pathology findings.14 At this time, the diagnosis of FM cannot be based on objective findings.8 As for most mental disorders, the diagnosis of FM requires a history of a cluster of symptoms that define the disorder according to expert consensus and clinical studies. The diagnosis of FM is made if the symptoms reported by the patient meet predefined criteria and if a somatic disease sufficiently explaining the symptoms is excluded.8
FM can be seen as a continuum disorder similar to other diseases/disorders, such as diabetes, hypertension, and depression, rather than a discrete disorder that could be present or absent at a particular time point. The prevalence of the syndrome depends on the cutoffs used for the definition of the disease/disorder, but may wax and wane over time.8 Persons diagnosed with FM do not represent a discrete group; FM constitutes the end of a continuous spectrum of polysymptomatic distress (somatic and psychological symptom burden) within the population.15
Classification
Fibromyalgia is a pain disease
The International Association for the Study of Pain (IASP) established a task force for the classification of chronic pain for the upcoming 11th revision of the ICD. The goal is to create a classification system that is applicable in primary care and in clinical settings for specialized pain management. One such category is chronic primary pain, which is defined as pain in one or more anatomic regions that persists or recurs for longer than 3 months and is associated with significant emotional distress or significant functional disability (interference with activities of daily life and participation in social roles) and that cannot be better explained by another chronic pain condition. This new phenomenological definition was created because the etiology for many forms of chronic pain is unknown. The term “primary pain” was chosen in close liaison with the ICD -11 revision committee, who felt this was the most widely acceptable term, in particular, from a nonspecialist perspective.16 Dysfunction in pain modulation, demonstrated by allodynia and spontaneous pain, suggests that FM could be a pain disease owing to an increase in pain sensitivity and decrease in pain inhibitory controls.17
Whether FM is indeed only a pain disorder remains contested. As early as 1989, Turk and Flor stated that FM is more than chronic widespread pain and tender points.18 Tender points can be regarded as the “sedimentation rate” of somatic and psychological distress.19,20 The new diagnostic criteria for FM give unrefreshed sleep and fatigue a nearly equal weight for diagnosis and even include depression as a minor symptom.21- 23 The composite of symptoms that occur in patients with FM raises the question of whether these various other symptoms are merely the consequence of chronic pain or whether they occur uniquely as a critical component of this disorder. Individual patients may also attribute variable weight to the comorbid symptoms of FM, although chronic widespread pain remains the defining feature of FM.
Fibromyalgia is a masked depression
Another myth is that FM is a masked depression or an affective spectrum disorder.24 The lifetime prevalence of depressive disorders in FM patients ranges between 40% and 80%, depending on the instruments and diagnostic criteria used.25 However, not every patient with FM is depressed and not every patient with depressive disorder reports chronic widespread pain.13,26 The association of FM and depressive disorders can be explained by symptom overlap (eg, sleep problems, fatigue) and shared biological (eg, genes) and psychological (eg, childhood adversities) mechanisms.26 The German guidelines state that FM and (masked) depression are not interchangeable.13
Fibromyalgia is a persistent somatoform pain disorder
The absence of a defined pathology and the association of FM symptoms with psychosocial stress prompted some specialists in psychosomatic medicine to use the diagnostic label “persistent somatoform pain disorder” (ICD-10 F45.4). Indeed, 60% to 80% of FM patients meet the diagnostic criterion of either the onset or aggravation of FM symptoms by psychosocial stress and emotional conflicts.27 The German guideline states that FM and persistent somatoform pain disorder are not interchangeable.13
Fibromyalgia is a somatic symptom disorder
There has been a move to classify FM as a somatic symptom disorder (SSD). Recently, the American Psychiatric Association substituted the category “pain disorder” with SSD in the fifth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The diagnosis of SSD may be made when there are persistent (ie, typically longer than 6 months) somatic symptoms that are distressing and/or significantly disruptive of daily life (criteria A and C) and are accompanied by excessive and disproportionate symptomrelated thoughts, feelings, and behaviors (criteria B).28
There have been recent publications that classify FM as an SSD.29,30 However, in one study, only 26% of FM patients met the criteria for an SSD. The construct validity and the clinical utility of the diagnostic label SSD were limited in this study.31
Fibromyalgia is a brain disease
The best-established pathophysiological features of FM are those of central sensitization (ie, augmented pain and sensory processing in the brain), with increased functional connectivity to pronociceptive brain regions and decreased connectivity to antinociceptive regions, and accompanying changes in central nervous system (CNS) neurotransmitters, as well as in the size and shape of brain regions. When these CNS changes were targeted with pharmacologic or nonpharmacologic therapies known to influence CNS function, a subset of individuals reported improvement in the cardinal symptoms of FM. An association of these effects with corresponding improvement in functional, chemical, and structural neuroimaging findings, promoted the concept that FM is a brain disease.17
However, these changes are not unique or distinct to FM. Findings of CNS alterations that are used to support the idea of pain centralization also support other CNS-based hypotheses, including the consequences of personality traits (such as pain catastrophizing), sympathetic nervous system dysfunction, the evolutionary stress response, and the activation of homeostatic neural programs.4,32
Fibromyalgia is a small fiber neuropathy
After identification of small-nerve-fiber pathology in some FM patients, a claim was made that FM is a neurological disease (small fiber neuropathy).33 However, small fiber pathology findings cannot be detected in all patients meeting established FM criteria.34 In addition, some small-pathology findings, such as decreased intraepidermal nerve fiber density (IENFD) have been noted in most chronic pain conditions where this has been examined and in other conditions not normally associated with pain, such as postural tachycardia syndrome and amyotrophic lateral sclerosis.34,35 Finally, the typical clinical picture of patients with small fiber neuropathy differs considerably from that seen in most FM patients.34
Diagnosis
Fibromyalgia is a diagnosis of exclusion and requires tender point examination by a rheumatologist
The clinical diagnosis of FM should be made by the primary care physician at the point of care after a clinical encounter that comprises a complete history and physical examination. Although the tender point examination has been embedded in the culture of FM diagnosis over the past three decades, it is no longer accepted as a reliable clinical finding and is not included in current diagnostic criteria. It was previously used in clinical practice to confirm or refute a diagnosis of FM and was initially believed to be a semiobjective confirmatory test. The diagnosis of FM remains a challenge for physicians, especially for general practitioners and psychiatrists, as noted in a survey conducted in six European countries, Mexico, and South Korea.36 Lack of training about FM is often cited as the reason for uncertainty. Currently, there is no specific diagnostic laboratory test or biomarker available for the diagnosis of FM. Recent guidelines are in agreement that the diagnosis remains clinical, and the purpose of the physical examination and limited laboratory investigations is to rule out some other somatic disease that can sufficiently explain the symptoms.8 Although there are numerous medical conditions that may mimic FM, such as neurological and internal diseases (eg, multiple myeloma), these can be excluded by careful clinical evaluation.37 The diagnosis can and should be established in most cases by a primary care physician. A referral to a specialist (eg, rheumatologist, neurologist, or endocrinologist) should be limited to situations where there is a reasonable clinical suspicion of some other condition that is presenting similarly to FM.8
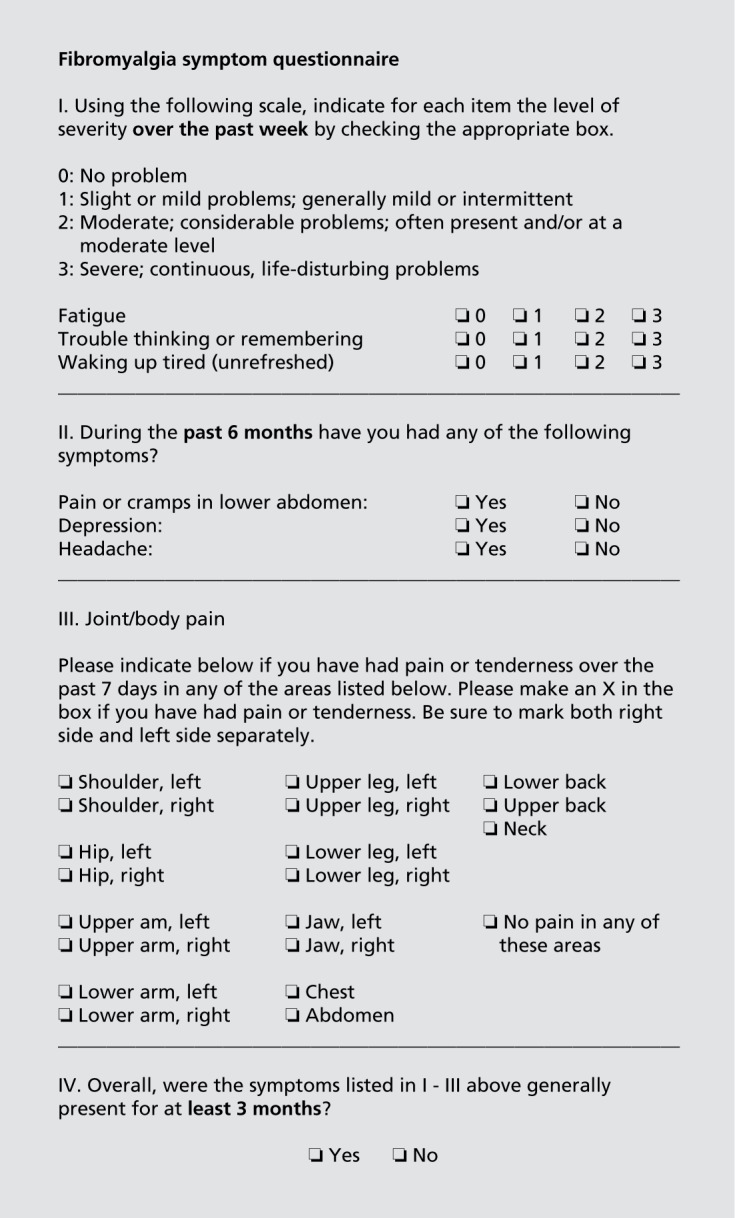
The preliminary American College of Rheumatology (ACR) 201 0 diagnostic criteria21 and the modified 201122 and 2016 criteria23 may be used to validate a clinical diagnosis of FM. These criteria do not require palpation of tender points. Instead, patients are assessed by the widespread pain index—which divides the body into 19 regions and scores the number of regions reported as painful—and a symptom severity score that assesses severity of fatigue, unrefreshing sleep, and cognitive symptoms. The widespread pain index and symptom severity scores have been combined into a single questionnaire with a maximum score of 31 and can be completed by self-report (Figure 1).22 A cutoff questionnaire score of 12 to 13 was statistically best at distinguishing those who fulfilled the ACR 2010 criteria from those who did not.38
Figure 1. Fibromyalgia symptom questionnaire. Adapted from reference 22: Wolfe F, Clauw DJ, Fitzcharles MA, et al. Fibromyalgia cri-teria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38(6):1113-1122. Copyright © 2011, The Journal of Rheumatology Publishing Company Limited.
Fibromyalgia is a diagnosis for middle-aged women
It is a myth that FM occurs only in middle-aged women. FM occurs in all populations across the world and can affect all ages. Symptom prevalence ranges between 2% and 4% in the general population. In clinical populations, women between 40 and 60 years of age are the majority with a female to male ratio of 8-10:l.4 However, in epidemiology studies that use the 2011 criteria, without tender point examination, the female-to-male ratio is 1 -2:1. 38,39
The differences in gender ratios between clinical and epidemiological studies can be explained by several hypotheses:
If the ACR 1990 classification criteria40 are used for diagnosis, a bias toward women is inherent by the tender point examination because positive tender points are more frequently reported by women than by men in the general population.41 The higher rate of positive tender points can be explained by a lower pain threshold in women than in men.42
In Western countries, women consult the health care system more frequently than men in cases of somatic and psychological symptoms.43
As FM is regarded to be a “disease of women,” physicians may neglect to consider this diagnosis when a man presents with chronic widespread pain, and/or a man may wish to avoid the stigma of a diagnosis of a predominantly female condition.44
Children and adolescents can meet the criteria of juvenile FM45 or the preliminary ACR 2010 diagnostic criteria. The data on the epidemiology of juvenile FM are conflicting.46
Management
Fibromyalgia is an unhelpful diagnosis for both patients and doctors
It is a myth that the diagnostic label of FM has negative implications. Concerns have been raised by representatives of psychiatry47 and pediatrics46 that the diagnostic label “FM” neglects psychosocial determinants of the symptoms of patients, has a disempowering effect on patients, and promotes medicalization and potential for iatrogenic harm.
In fact, some protagonists of the concept of “central sensitization” of FM claim that FM can be medically explained (as a neurologic disease) and that psychological processes such as somatization or catastrophizing are not relevant.48 Pregabalin, which was the first drug approved by the US Food and Drug Administration (FDA) to treat FM, is manufactured by the pharmaceutical company Pfizer, which supports FM self-help organizations in political campaigns emphasizing that “FM is a real disease.” For patient advocacy groups and doctors who have focused their medical practice on FM, the pregabalin approval was a milestone for the legitimization of FM, just as fluoxetine brought depression into the mainstream.49
Whether FM is a helpful or unhelpful diagnosis both for patients and doctors depends on the information given to the patient regarding the nature of the disorder, planned treatment strategy, and expected outcome after the initial diagnosis. All recent guidelines recommend that the diagnostic label FM (or FMS for FM syndrome) should be communicated to patients after the initial diagnosis. This approach is intended to reduce anxiety, which inherently accompanies chronic pain, and to reduce repeated unnecessary diagnostic procedures and inappropriate drug treatments. There is also consensus that patients should be informed of the concept of a biopsychosocial model for FM whereby biological factors (eg, genetic predisposition) and psychosocial factors (eg, stress) contribute to the predisposition, triggering, and perpetuating of FM symptoms.8 The German guidelines suggest that the following information could be useful in the education of patients:6
The symptoms are not caused by an organic disease (such as abnormality of muscles or joints) but are instead based on a functional disorder.
The legitimacy of the ailment should be acknowledged.
The symptoms are persistent in nearly all patients.
Total relief of symptoms is seldom achieved.
The symptoms do not lead to disability and do not shorten life expectancy.
Most patients learn to adapt to the symptoms over time.
The goals of treatment are improvement in quality of life, maintenance of function (functional ability in everyday situations), and reduction in symptoms.
The ability of the patient to modulate symptoms via self-management strategies should be emphasized.
The German guidelines group developed a patient version of the guidelines and handouts for patients and their significant others, which should be distributed to the patient after establishing the diagnosis.
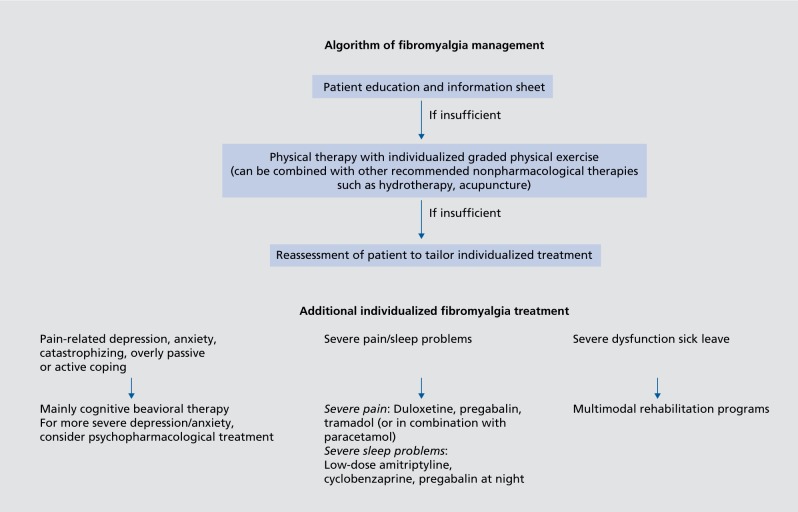
In addition, all recent guidelines stress the importance of nonpharmacological therapies in the management of FM. Aerobic exercise was the only treatment that received a strong recommendation by EULAR.7 In the updated German guidelines, aerobic exercise49 and cognitive behavioral therapies50 received strong recommendation. All guidelines stress that drug therapy is not obligatory, but optional. The German guidelines defined rules for discontinuation of drug therapies and recommended the discussion of drug holidays with responded to drug therapy after 6 months.6 In addition, screening for psychological distress51 and referral to a mental health care specialist in case of comorbid mental disorder are recommended (Figure 2). ,7,51
Figure 1. Algorithm of fibromyalgia management. Adapted from reference 7: Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318-328. Copyright © 2017, BMJ Publishing Group Limited.
In sum, guidelines recommend the use of the diagnostic label FM. It is also important to acknowledge the role of psychological factors in the etiology and management of FM and to promote the self-efficacy of patients through the medium of self -management strategies.
Class effect of antidepressants, anticonvulsants, and antipsychotics on fibromyalgia symptoms
The assumption that all psychopharmaclogical agents that have an effect on mental disorders are also effective for main FM symptoms (pain, sleep problems, fatigue) is not supported by evidence. Of all the tricyclic antidepressants, there is sufficient evidence only for amitriptyline.52 Effectiveness of monoamine oxidase inhibitors for the treatment of FM symptoms is limited; however, there have only been two studies, which included a small number of patients and a high risk of bias, on which to base this finding.53 The evidence for the efficacy of the serotonin reuptake inhibitors citalopram, fluoxetine, and paroxetine is limited due to small sample sizes and other risks of bias.54 The serotonin noradrenaline reuptake inhibitors (SNRIs) duloxetine and milnacipran have been approved by the FDA, but not by the European Medical Agency (EMA), for treatment of FM. One study each with duloxetine and milnacipran conducted in Europe failed to reach the primary end point, namely the superiority over placebo in mean pain intensity reduction. One large study with different dosages of desvenlafaxine did not demonstrate superiority over placebo for multiple end points.55 The anticonvulsant pregabalin has been approved by the FDA, but not by the EMA for FM. One study conducted in Europe failed to reach the primary end point, namely the superiority over placebo in mean pain intensity reduction. One medium size study with gabapentin in FM was compromised by high risks of bias.56 One study each with eslicarbazepine, lacosamide, and levetiracetam failed to demonstrate superiority over placebo in multiple outcomes. Some antipsychotics are licensed as add-on therapy for major depression refractory to antidepressants. Evidence of efficacy by randomized controlled trials (RCTs) on pain and sleep problems is only available for quetiapine.57 Therefore, evidence for a class effect of many agents, especially those used in the management of mental health disorders, is lacking for the treatment of FM.
FDA-approved drags (duloxetine, milnacipran, pregabalin) are effective and well tolerated
Cochrane reviews of the RCTs on which the decisions to approve medications for the treatment of FM by the FDA and EMA have demonstrated that only a minority of study participants (10% more than with placebo) reported a clinically relevant reduction in pain. The majority of study participants did not experience relevant pain relief and/or terminated the therapy because of side effects.58,59 Pregabalin, but not duloxetine and milnacipran, had a clinically relevant effect on sleep problems. The superiority of all three drugs over placebo on fatigue was not clinically relevant.55,56
The results of observational studies in natural settings confirm the limited efficacy and low tolerability of centrally acting drugs in FM. A longitudinal study of FM patients of the National Data Bank of Rheumatic Diseases found that pain scores were reduced minimally by 0.17 units (95% CI: 0.03-0.30) on an 11-point scale after initiation of a therapy with duloxetine, milnacipran, or pregabalin. Fatigue or functional status was not significantly improved by these drugs.60 In a retrospective analysis using the MarketScan claims database to identify adults with a first diagnosis of FM between 2009 and 2011, the discontinuation rates after 12 months were 51% for duloxetine, 62% for milnacipran, and 65% for pregabalin.61
Therefore, contrary to common belief, the effect of these FDA-approved drugs is less than satisfactory.
Psychodynamic therapy cures fibromyalgia
Cognitive behavioral therapies are intended to help patients better cope with their symptoms and improve health-related quality of life.62 In contrast, some protagonists of psychodynamic therapy claim that they can effect a cure of FM in some patients.63 To date, this argument has been tested by a single RCT in FM patients with major depression. Brief psychodynamic therapy (25 sessions, 1 session/week) was not superior to supportive therapy including antidepressant and analgesic medication (4 sessions within 6 months) with regard to somatic and psychological symptoms and health-related quality of life.64
Therefore, the evidence for curative psychodynamic therapy in FM is lacking.
Conclusion
Despite the participation of neurologists and mental health care specialists and their scientific societies in recent interdisciplinary evidence-based guidelines on FM, the diagnostic label FM remains contested by some mental health care specialists who hold to an obsolete psychiatric or psychosomatic concept of “medically unexplained somatic syndromes” such as masked depression and somatoform pain disorder. These myths are perpetuated even with the impressive progress in the field of FM in the past few decades. The advancement in the field of FM includes:
A biopsychosocial model of FM that highlights the neurological underpinnings of this condition and attributes importance to psychosocial factors in the predisposition, triggering, and chronification of FM symptoms.65
Interdisciplinary evidence-based guidelines that recommend screening for psychological distress and referral to a mental health care specialist in case of comorbid mental disorder.7,51
Interdisciplinary evidence-based guidelines that promote nonpharmacological therapies (aerobic exercise, cognitive behavioral therapies)6-8 and emphasize the need to reduce the “[overjmedicalization of misery.”66
Acknowledgments
WH received one honorarium by Grunenthal for an educational lecture in the last 3 years. JA has performed professional consulting on behalf of BrainSet Ltd. SP received honoraria from Pfizer, Lilly, and Gruüenthal in the last 3 years. MAF received consulting fees, speaking fees and/or honoraria (<$10,000) from ABBVIE, Abbott, Amgen, Bristol-Myers Squibb Canada, Janssen, Johnson & Johnson, Lilly, and Pfizer in the last 3 years.
Contributor Information
Winfried Häuser, Department Internal Medicine 1, Klinikum Saarbrücken, Saarbrücken, Germany. Department Psychosomatic Medicine and Psychotherapy, Technische Universität München, München, Germany.
Mary-Ann Fitzcharles, Division of Rheumatology, McGill University Health Centre, Quebec, Canada, Alan Edwards Pain Management Unit, McGill University Health Centre, Quebec, Canada.
REFERENCES
- 1.Rahman A., Underwood M., Carnes D. Fibromyalgia. BMJ. 2014;348:g1224. doi: 10.1136/bmj.g1224. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe F. Fibromyalgia wars. J Rheumatol. 2009;36(4):671–678. doi: 10.3899/jrheum.081180. [DOI] [PubMed] [Google Scholar]
- 3.Shir Y., Fitzcharles MA. Should rheumatologists retain ownership of fibromyalgia? J Rheumatol. 2009;36(4):667–670. doi: 10.3899/jrheum.081073. [DOI] [PubMed] [Google Scholar]
- 4.Hâuser W., Ablin J., Fitzcharles MA., et al. Fibromyalgia. Nat Rev Dis Primers. 2015;1:15022. doi: 10.1038/nrdp.2015.22. [DOI] [PubMed] [Google Scholar]
- 5.Fitzcharles MA., Ste-Marie PA., Goldenberg DL., et al. 2012 Canadian Guidelines for the diagnosis and management of fibromyalgia syndrome: executive summary. Pain Res Manag. 2013;18(3):119–126. doi: 10.1155/2013/918216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petzke F., Brückle W., Eidmann U., et al. General treatment principles, coordination of care and patient education in fibromyalgia syndrome: updated guidelines 2017 and overview of systematic review articles. Schmerz. 2017;31(3):246–254. doi: 10.1007/s00482-017-0201-6. [DOI] [PubMed] [Google Scholar]
- 7.Macfarlane GJ., Kronisch C., Dean LE., et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318–328. doi: 10.1136/annrheumdis-2016-209724. [DOI] [PubMed] [Google Scholar]
- 8.Fitzcharles MA., Shir Y., Ablin JN., et al. Classification and clinical diagnosis of fibromyalgia syndrome: recommendations of recent evidence-based interdisciplinary guidelines. Evid Based Complement Alternat Med. 2013;2013:528952. doi: 10.1155/2013/528952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choy E., Perrot S., Leon T., et al. A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Serv Res. 2010;10:102. doi: 10.1186/1472-6963-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emson HE. Health, disease and illness: matters for definition. CMAJ. 1987;136(8):811–814. [PMC free article] [PubMed] [Google Scholar]
- 11.Scully JL. What is a disease? EMBO Rep. 2004;5(7):650–653. doi: 10.1038/sj.embor.7400195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. International Classification of Diseases and Related Health Problems, 10th revision (ICD-10). 2015 version. World Health Organization. Available at: http://www.who.int/classifications/icd/en. [Google Scholar]
- 13.Eich W., Bar KJ., Bernateck M., et al. Definition, classification, clinical diagnosis and prognosis of fibromyalgia syndrome: updated guidelines 2017 and overview of systematic review articles. Schmerz. 2017;31(3):231–238. doi: 10.1007/s00482-017-0200-7. [DOI] [PubMed] [Google Scholar]
- 14.Havelka M., Lucanin JD., Lucanin D. Biopsychosocial model - the integrated approach to health and disease. Coll Antropol. 2009;33(1):303–310. [PubMed] [Google Scholar]
- 15.Häuser W., Schmutzer G., Brahler E., Glaesmer H. A cluster within the continuum of biopsychosocial distress can be labeled “fibromyalgia syndrome”—evidence from a representative German population survey. J Rheumatol. 2009;36(12):2806–2812. doi: 10.3899/jrheum.090579. [DOI] [PubMed] [Google Scholar]
- 16.Treede RD., Rief W., Barke A., et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–1007. doi: 10.1097/j.pain.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311(15):1547–1555. doi: 10.1001/jama.2014.3266. [DOI] [PubMed] [Google Scholar]
- 18.Turk DC., Flor H. Primary fibromyalgia is greater than tender points: toward a multiaxial taxonomy. J Rheumatol Suppl. 1989;19:80–86. [PubMed] [Google Scholar]
- 19.Wolfe F. The relation between tender points and fibromyalgia symptom variables: evidence that fibromyalgia is not a discrete disorder in the clinic. Ann Rheum Dis. 1997;56(4):268–271. doi: 10.1136/ard.56.4.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McBeth J., Macfarlane GJ., Benjamin S., Morris S., Silman AJ. The association between tender points, psychological distress, and adverse childhood experiences: a community-based study. Arthritis Rheum. 1999;42(7):1397–1404. doi: 10.1002/1529-0131(199907)42:7<1397::AID-ANR13>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 21.Wolfe F., Clauw DJ., Fitzcharles MA., et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Rheum. 2010;62(5):600–610. doi: 10.1002/acr.20140. [DOI] [PubMed] [Google Scholar]
- 22.Wolfe F., Clauw DJ., Fitzcharles MA., et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38(6):1113–1122. doi: 10.3899/jrheum.100594. [DOI] [PubMed] [Google Scholar]
- 23.Wolfe F., Clauw DJ., Fitzcharles MA., et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthr Rheum. 2016;46(3):319–329. doi: 10.1016/j.semarthrit.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Hudson JI., Pope HG. The concept of affective spectrum disorder: relationship to fibromyalgia and other syndromes of chronic fatigue and chronic muscle pain. Baillieres Clin Rheumatol. 1994;8(4):839–856. doi: 10.1016/s0950-3579(05)80051-2. [DOI] [PubMed] [Google Scholar]
- 25.Alciati A., Sgiarovello P., Atzeni F., Sarzi-Puttini P. Psychiatric problems in fibromyalgia: clinical and neurobiological links between mood disorders and fibromyalgia. Reumatismo. 2012;64(4):268–274. doi: 10.4081/reumatismo.2012.268. [DOI] [PubMed] [Google Scholar]
- 26.Gracely RH., Ceko M., Bushnell MC. Fibromyalgia and depression. Pain Res Treat. 2012;2012:486590. doi: 10.1155/2012/486590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Häuser W., Henningsen P. Fibromyalgia syndrome: a somatoform disorder? Eur J Pain. 2014;18(8):1052–1059. doi: 10.1002/j.1532-2149.2014.00453.x. [DOI] [PubMed] [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing; . 2013 [Google Scholar]
- 29.Tavel ME. Somatic symptom disorders without known physical causes: one disease with many names? Am J Med. 2015;128(10):1054–1058. doi: 10.1016/j.amjmed.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 30.Klaus K., Fischer S., Doerr JM., Nater UM., Mewes R. Classifying fibromyalgia syndrome as a mental disorder? An ambulatory assessment study. Int J Behav Med. 2017;24(2):230–238. doi: 10.1007/s12529-016-9603-6. [DOI] [PubMed] [Google Scholar]
- 31.Hauser W., Bialas P., Welsch K., Wolfe F. Construct validity and clinical utility of current research criteria of DSM-5 somatic symptom disorder diagnosis in patients with fibromyalgia syndrome. J Psychosom Res. 2015;78(6):546–552. doi: 10.1016/j.jpsychores.2015.03.151. [DOI] [PubMed] [Google Scholar]
- 32.Walitt B., Ceko M., Gracely JL., Gracely RH. Neuroimaging of central sensitivity syndromes: key insights from the scientific literature. Curr Rheumatol Rev. 2016;12(1):55–87. doi: 10.2174/1573397112666151231111104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oaklander AL., Herzog ZD., Downs HM., Klein MM. Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Pain. 2013;154(11):2310–236. doi: 10.1016/j.pain.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Üçeyler N., Burgmer M., Friedel E., et al. Etiology and pathophysiology of fibromyalgia syndrome: updated guidelines 2017, overview of systematic review articles and overview of studies on small fiber neuropathy in FMS subgroups. Schmerz. 2017;31(3):239–245. doi: 10.1007/s00482-017-0202-5. [DOI] [PubMed] [Google Scholar]
- 35.Clauw DJ. What is the meaning of “small fiber neuropathy” in fibromyalgia? Pain. 2015;156(11):2115–2116. doi: 10.1097/j.pain.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 36.Perrot S., Choy E., Petersel D., Ginovker A., Kramer E. Survey of physician experiences and perceptions about the diagnosis and treatment of fibromyalgia. BMC Health Serv Res. 2012;12:356. doi: 10.1186/1472-6963-12-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hâuser W., Sommer C., Perrot S., Shir Y., Fitzcharles MA. Diagnostic confounders of chronic widespread pain: not always fibromyalgia. Pain Rep. 2017;2(3):e598. doi: 10.1097/PR9.0000000000000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolfe F., Brahler E., Hinz A., Hauser W. Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care Res. (Hoboken). 2013;65(5):777–785. doi: 10.1002/acr.21931. [DOI] [PubMed] [Google Scholar]
- 39.Branco JC., Bannwarth B., Failde I., et al. Prevalence of fibromyalgia: a survey in five European countries. Semin Arthritis Rheum. 2010;39(6):448–453. doi: 10.1016/j.semarthrit.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 40.Wolfe F., Smythe HA., Yunus MB., et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 41.Wolfe F., Ross K., Anderson J., Russell IJ. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol. 1995;22(1):151–156. [PubMed] [Google Scholar]
- 42.Schiltenwolf M., Pogatzki-Zahn EM. Pain medicine from intercultural and gender-related perspectives. Schmerz. 2015;29(5):569–575. doi: 10.1007/s00482-015-0038-9. [DOI] [PubMed] [Google Scholar]
- 43.Aggarwal VR., McBeth J., Zakrzewska JM., Lunt M., Macfarlane GJ. The epidemiology of chronic syndromes that are frequently unexplained: do they have common associated factors? Int J Epidemiol. 2006;35(2):468–476. doi: 10.1093/ije/dyi265. [DOI] [PubMed] [Google Scholar]
- 44.Hâuser W., Kûhn-Becker H., von Wilmoswky H., Settan M., Brâhler E., Petzke F. Demographic and clinical features of patients with fibromyalgia syndrome of different settings: a gender comparison. Gend Med. 2011;8(2):116–125. doi: 10.1016/j.genm.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 45.Yunus MB., Masi AT. Juvenile primary fibromyalgia syndrome. A clinical study of thirty-three patients and matched normal controls. Arthritis Rheum. 1985;28(2):138–145. doi: 10.1002/art.1780280205. [DOI] [PubMed] [Google Scholar]
- 46.Draheim N., Ebinger F., Schnôbel-Muller E., Wolf B., Hâuser W. Definition, diagnostics and therapy of chronic widespread pain and the (so-called) fibromyalgia syndrome in children and adolescents: updated guidelines 2017. Schmerz. 2017;31(3):296–307. doi: 10.1007/s00482-017-0208-z. [DOI] [PubMed] [Google Scholar]
- 47.Bass C., Henderson M. Fibromyalgia: an unhelpful diagnosis for patients and doctors. BMJ. 2014;348:g2168. doi: 10.1136/bmj.g2168. [DOI] [PubMed] [Google Scholar]
- 48.Yunus MB. Fibromyalgia and overlapping disorders: the unifying concept of central sensitivity syndromes. Semin Arthritis Rheum. 2007;36(6):335–356. doi: 10.1016/j.semarthrit.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 49.Berenson A. Drug approved. Is disease real? New York Times. January 14, 2008. Available at: http://www.nytimes.com/2008/01/14/health/14pain. html. Accessed October 1, 2017 [Google Scholar]
- 50.Winkelmann A., Bork H., Brûckle W., et al. Physiotherapy, occupational therapy and physical therapy in fibromyalgia syndrome: updated guidelines 2017 and overview of systematic review articles. Schmerz. 2017;31(3):255–265. doi: 10.1007/s00482-017-0203-4. [DOI] [PubMed] [Google Scholar]
- 51.Kollner V., Bernardy K., Greiner W., et al. Psychotherapy and psychological procedures for fibromyalgia syndrome: updated guidelines 2017 and overview of systematic review articles. Schmerz. 2017;31(3):266–273. doi: 10.1007/s00482-017-0204-3. [DOI] [PubMed] [Google Scholar]
- 52.Moore RA., Derry S., Aldington D., Cole P., Wiffen PJ. Amitriptyline for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. CD008242.doi:10. 1002/1 4651858.CD008242.pub2. 2012;12 doi: 10.1002/14651858.CD008242.pub2. [DOI] [PubMed] [Google Scholar]
- 53.Tort S., Urrùtia G., Nishishinya MB., Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev. CD009807. 2012;(4) doi: 10.1002/14651858.CD009807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Walitt B., Urrutia G., Nishishinya MB., Cantrell SE., Hauser W. Selective serotonin reuptake inhibitors for fibromyalgia syndrome. Cochrane Database Syst Rev. CD01 1735. 2015;(6) doi: 10.1002/14651858.CD011735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Häuser W., Urrùtia G., Tort S., Üçeyler N., Walitt B. Serotonin and noradrenaline reuptake inhibitors (SNRIs) for fibromyalgia syndrome. Cochrane Database Syst Rev. CD010292. doi:10. 1002/14651858. CD010292. 2013;(1) doi: 10.1002/14651858.CD010292. [DOI] [PubMed] [Google Scholar]
- 56.Üçeyler N., Sommer C., Walitt B., Häuser W. Anticonvulsants for fibromyalgia. Cochrane Database Syst Rev. CD010782. doi:10.1002/14651858.CD010782. 2013;(10) doi: 10.1002/14651858.CD010782. [DOI] [PubMed] [Google Scholar]
- 57.Walitt B., Klose P., Uceyler N., Phillips T., Hauser W. Antipsychotics for fibromyalgia in adults. Cochrane Database Syst Rev. CD011804. 2016;(6) doi: 10.1002/14651858.CD011804.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Derry S., Cording M., Wiffen PJ., Law S., Phillips T., Moore RA. Pregabalin for pain in fibromyalgia in adults. Cochrane Database Syst Rev. CD011790. 2016;9 doi: 10.1002/14651858.CD011790.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cording M., Derry S., Phillips T., Moore RA., Wiffen PJ. Milnacipran for pain in fibromyalgia in adults. Cochrane Database Syst Rev. CD008244. doi:10.1002/14651858.CD008244.pub3. 2015;(10) doi: 10.1002/14651858.CD008244.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wolfe F., Walitt BT., Katz RS., Lee YC., Michaud KD., Hauser W. Longitudinal patterns of analgesic and central acting drug use and associated effectiveness in fibromyalgia. Eur J Pain. 2013;17(4):581–586. doi: 10.1002/j.1532-2149.2012.00234.x. [DOI] [PubMed] [Google Scholar]
- 61.Liu Y., Qian C., Yang M. Treatment patterns associated with ACR-recommended medications in the management of fibromyalgia in the United States. J Manag Care Spec Pharm. 2016;22(3):263–271. doi: 10.18553/jmcp.2016.22.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bernardy K., Klose P., Busch AJ., Choy EH., Hauser W. Cognitive behavioural therapies for fibromyalgia. Cochrane Database Syst Rev. CD009796. 2013;(9) doi: 10.1002/14651858.CD009796.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Egle UT., Egloff N., von Kanel R. Stress-induced hyperalgesia (SIH) as a consequence of emotional deprivation and psychosocial traumatization in childhood: implications for the treatment of chronic pain. Schmerz. 2016;30(6):526–536. doi: 10.1007/s00482-016-0107-8. [DOI] [PubMed] [Google Scholar]
- 64.Scheidt CE., Waller E., Endorf, et al. Is brief psychodynamic psychotherapy in primary fibromyalgia syndrome with concurrent depression an effective treatment? A randomized controlled trial. Gen. Hosp Psychiatry. 2013;35(2):160–167. doi: 10.1016/j.genhosppsych.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 65.Üçeyler N., Burgmer M., Friedel E., et al. Etiology and pathophysiology of fibromyalgia syndrome: updated guidelines 2017, overview of systematic review articles and overview of studies on small fiber neuropathy in FMS subgroups [in German], Schmerz. 2017;31(3):239–245. doi: 10.1007/s00482-017-0202-5. [DOI] [PubMed] [Google Scholar]
- 66.Hadler NM. “Fibromyalgia” and the medicalization of misery. J Rheumatol. 2003;30(8):1668–1670. [PubMed] [Google Scholar]