Abstract
Objective
To investigate the impact of age and sex on 30-, 60- and 90-day hospital readmission after acute hospital discharge for individuals with traumatic brain injury (TBI).
Design
Retrospective cohort study.
Setting
Acute hospitals and post-acute discharge settings
Participants
From the 2013 Nationwide Readmissions Database, we retrieved information on 52,877 individuals with diagnosis-related group codes of TBI. We included only those alive at index acute discharge and excluded those discharged with same-day readmission. We divided our sample into four age groups: 18-40, 41-65, 66-75 and 76+ years old.
Interventions
NA.
Main Outcome Measure(s)
All-cause hospital readmission.
Results
Sex differences in 30-, 60- and 90-day hospital readmission were found for all age groups (all p<.05). The largest sex differences in hospital readmission were in the two oldest groups (66-75, 76+). For both sexes, the oldest group (76+) had the highest adjusted 90-day readmission risk [e.g., 90-day readmission: Odds Ratio (OR) = 2.32 (2.01-2.69) for males; OR=1.96 (1.59-2.43) for females]. Among those readmitted within 90 days, the youngest group (18-40 years) had the highest cumulative readmission percent (35% for both sexes) within the first week post-hospital discharge.
Conclusion
Age and sex were significantly associated with hospital readmission during the first 90 days post-discharge in our TBI sample. Specifically, those aged 66-75 or 76+ had the highest readmission risk over 90 days for both sexes. The findings suggest that clinicians should consider age and sex in discharge planning and for the entire episode of care for the TBI population.
Key words (MeSH terms): brain injuries, hospital readmission, patient age groups, long-term care
Graphical abstract
Introduction
Worldwide, nearly 10 million individuals experience traumatic brain injury (TBI) each year1,2. Brain injury can cause complex and chronic health conditions with high mortality and prolonged morbidity3,4. Furthermore, brain injury can lead to chronic physical, cognitive and psychological impairments that further worsen patients’ health and quality of life5. TBI is among the leading causes of emergency department visits and hospital admissions6,7. Patients with severe TBI or more underlying comorbidities have higher rates of hospital readmissions than those with less severe injury or fewer comorbidities8,9.
Since hospital readmissions are highly prevalent and costly10,11, identifying factors influencing hospital readmission could serve as a crucial first step to improving care outcomes in the TBI population10,11. Studies show that patients leaving hospitals against medical advice after TBI had higher rates of readmission12,13. Corrigan and colleagues (2014)14 pointed out that age-specific interventions are needed to reduce post-acute inpatient rehabilitation mortality in TBI. For patients with stroke, Slocum and colleagues (2006)15 found that age and functional status were better predictors of hospital readmission across nine years compared to medical comorbidities; however, such age-specific association remains unclear for the TBI population. In addition to age, recent studies have pointed out that sex-specific research in TBI is sparse and needed, to help improve emergency care and health outcomes for the TBI population16,17.
Most studies in the brain injury field include relatively small samples of patients (<100)18. In addition, most of the work related to hospital readmission has been conducted using a 30-day follow-up period. Only one recent Canadian population-based study examined the predictors of rehospitalization in a 3-year period post-TBI and identified the following significant predictors: male, older age, falls, greater injury severity, rural residence, greater comorbidity and psychiatric comorbidity19. To our knowledge, this study is the first to analyze the U.S. nationally representative TBI data for adults at all ages, covering all insurance plans across a 90-day follow-up period. Since patients with TBI often have underlying chronic conditions, continuous follow up after hospital discharge can help with continuous care planning and disease monitoring. Thus, this study aims to examine the impact of age and sex on 30-, 60- and 90-day all-cause hospital readmissions post-hospital discharge for the adult TBI population.
Methods
Data Source
The Nationwide Readmissions Database (NRD) 2013 is a population-based database managed by the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality (AHRQ)20. The NRD is drawn from the HCUP State Inpatient Databases (SID) and includes national readmission data from all types of payers (government, private and uninsured patients), across all ages. The NRD accounts for 49.3% of the US population and 49.1% of US hospitalizations as reported in the American Hospital Association (AHA) Annual Survey Database with more than 100 clinical and nonclinical variables. As the first database that includes hospitalizations in specialty and federal hospitals and community from 21 states, the NRD has data on approximately 15 million unweighted and 36 million weighted discharges annually20. Hospital readmission rates, readmission reasons and hospital costs for each hospital stay are the main outcomes in the NRD20. For this study, we used three files from the NRD: core file (clinical and nonclinical variables that support readmission analyses), severity file (diagnosis and procedure classifications variables) and hospital file (hospital-level variables). We obtained university Institutional Review Board approval (IRB# 16-0286) and an HCUP Data Use Agreement (DUA) prior to conducting this study.
Cohort Selection
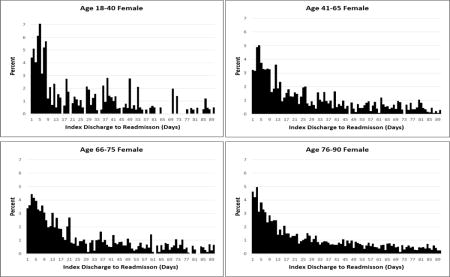
We used our conservative operational definition to identify patients with TBI based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)22 codes (800.XX, 802.XX, 803.XX, 804.XX and 851.XX-854.XX). In this study, we did not include 850.XX (concussion), as this code represents a wide spectrum of symptoms (from none, mild, to severe). Only individuals older than 18 years were included and we excluded those who died during the index hospitalization. Figure 1 provides the detailed cohort selection process. The final cohort of this study is 52,877 individuals with TBI. To examine the timing of readmission by age, we selected a sub-set of cases readmitted within 90 days.
Figure 1.
Cohort Selection
Figure 1 represents each step used in the cohort selection process. The final sample is 52,877.
Study Outcome
The primary outcome was any readmission that occurred within 90 days after hospital discharge. We used the Centers for Medicare and Medicaid Services (CMS) methodology to identify hospital-wide all-cause readmission22. We examined readmission at three time points: 30-, 60- and 90-days and included only the first (index) readmission at each time point. During the study period, 0.3% of the total NRD population had TB (using 15 million as the denominator), which was less than half the TBI prevalence of 0.7% reported by the CDC (numerator: 2.5 million, denominator: 323.1 million)22.
Primary Variable
We classified the sample into four age groups: 18-40, 41-65, 66-75 and 76+ years. The four age groups were determined based on (a) the data representation in the NRD (young, middle-aged, old and very old) and (b) the epidemiology literature report: adults with TBI aged 65 and older are responsible for more than 80,000 annual emergency department visits and those 76+ years have the highest rates of TBI-related hospitalization and death17,23.
Secondary Variables
Three secondary variables, severity of injury, discharge setting and hospital teaching status, were chosen because these three variables differed significantly by group readmission rate across time (Table 1). Based on all-patient-refined Diagnosis Related Group (AP-DRG) defined by the HCUP, we categorized severity of injury into four groups: minor, moderate, major and extreme severity, using the summed number of DRGs21. We also classified patients into three discharge-setting categories: home, Skilled Nursing Facility (SNF)/Intermediate Care Facility (ICF) and Home Health (HH). In addition, teaching status of the hospital was categorized as teaching-metropolitan, non-teaching-metropolitan and non-teaching-rural.
Table 1.
Person-level and Hospital-level Characteristics of Patients with Observed 30-, 60- and 90-Day Readmission.
| 30-day readmission (N=52,877) | 60-day readmission (N=48,300) | 90-day readmission (N=43,408) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Actual (n, %#) | Admitted (%**, SE)ˆ | p-value | Actual (n, %*) | Admitted (%**, SE) | p-value | Actual (n, %*) | Admitted (%**, SE) | p-value | |
| Patient Characteristics | |||||||||
|
| |||||||||
| Age group (yr) | <.0001* | <.0001* | <.0001* | ||||||
| 18–40 | 11,305(21.5) | 4.6(0.2) | 10,396(21.6) | 6.2(0.2) | 9,382(21.7) | 7.2(0.3) | |||
| 41–65 | 14,495(27.5) | 10.9(0.3) | 13,247(27.5) | 14.8(0.4) | 11,953(27.7) | 17.6(0.5) | |||
| 66–75 | 7,485(14.1) | 13.4(0.4) | 6,810(14.0) | 18.6(0.5) | 6,086(14.0) | 21.5(0.6) | |||
| 76+ | 19,592(37.0) | 14.6(0.3) | 17,847(36.8) | 20.1(0.4) | 15,987(36.7) | 24.0(0.4) | |||
| Sex | .0171* | .0009* | .0008* | ||||||
| Male | 31,363(59.1) | 11.7(0.2) | 28,743(59.3) | 14.9(0.3) | 25,830(59.3) | 17.6(0.3) | |||
| Female | 21,514(40.9) | 10.9(0.3) | 19,557(40.7) | 16.3(0.3) | 17,578(40.7) | 19.2(0.3) | |||
| Admission type | .0765 | .1516 | 0.2171 | ||||||
| Elective | 1,637(3.3) | 9.7(0.9) | 1,507(3.4) | 14.1(0.9) | 1,372(3.4) | 16.9(1.1) | |||
| Non Elective | 51,025(96.7) | 11.3(0.2) | 46,590(96.6) | 15.5(0.2) | 41,847(96.6) | 18.3(0.2) | |||
| ED Service | .0732 | .1599 | .0757 | ||||||
| No | 6,665(12.7) | 12.2(0.6) | 6,034(12.5) | 16.4(0.7) | 5,410(12.5) | 19.5(0.8) | |||
| Yes | 46,212(87.3) | 11.1(0.2) | 42,266(87.5) | 15.3(0.2) | 37,998(87.5) | 18.1(0.2) | |||
| Primary payer | <.0001* | <.0001* | .0001* | ||||||
| Medicare | 27,438(52.2) | 14.7(0.2) | 25,000(52.0) | 20.3(0.3) | 22,397(51.8) | 24.1(0.3) | |||
| Medicaid | 4,741(8.6) | 11.2(0.5) | 4,356(8.7) | 15.2(0.7) | 3,932(8.7) | 17.8(0.7) | |||
| Private | 11,229(21.6) | 6.9(0.3) | 10,265(21.6) | 9.4(0.3) | 9,276(21.8) | 11.0(0.4) | |||
| Self | 4,952(9.6) | 5.8(0.4) | 4,532(9.6) | 7.6(0.5) | 4,078(9.6) | 9.1(0.4) | |||
| Other | 4,517(8.1) | 7.0(0.4) | 4,147(8.1) | 10.0(0.6) | 3,725(8.1) | 11.6(0.6) | |||
| Severity | <.0001* | <.0001* | <.0001* | ||||||
| Minor | 14,401(26.9) | 7.3(0.3) | 13,181(27.0) | 9.7(0.3) | 11,909(27.2) | 11.4(0.4) | |||
| Moderate | 22,362(42.3) | 10.6(0.3) | 20,446(42.3) | 14.9(0.3) | 18,324(42.1) | 17.8(0.3) | |||
| Major | 12,367(23.5) | 15.4(0.4) | 11,272(23.5) | 20.8(0.5) | 10,121(23.5) | 24.2(0.6) | |||
| Extreme | 3,747(7.3) | 16.7(0.6) | 3,401(7.3) | 22.7(0.7) | 3,054(7.2) | 27.3(0.9) | |||
| Comorbidity | Mean (95% CI) | <.0001* | Mean (95% CI) | <.0001* | Mean (95% CI) | <.0001* | |||
| For admitted | 4.6(4.3, 2.8) | 4.6(4.4, 4.8) | 4.6(4.4,4.8) | ||||||
| Not admitted | 2.5(2.3, 2.6) | 2.5(2.4, 2.6) | 2.5(2.2,2.5) | ||||||
| Discharge destination | <.0001* | <.0001* | <.0001* | ||||||
| Home | 31,676(59.3) | 8.1(0.2) | 28,978(59.4) | 11.0(0.2) | 26,148(59.7) | 13.1(0.3) | |||
| SNF, ICF | 14,911(29.2) | 16.0(0.4) | 13,572(29.1) | 22.6(0.4) | 12,082(28.8) | 26.8(0.5) | |||
| Home Health | 6,290(11.4) | 15.5(0.6) | 5,750(11.4) | 20.3(0.6) | 5,178(11.4) | 23.7(0.7) | |||
| Residence | .0578 | .0011* | <.0001* | ||||||
| Central | 18,141(29.1) | 11.7(0.3) | 16,571(29.1) | 16.0(0.4) | 14,884(29.1) | 18.9(0.5) | |||
| Fringe | 11,980(24.0) | 11.6(0.4) | 10,936(24.0) | 16.3(0.4) | 9,819(24.0) | 19.2(0.5) | |||
| Counties (250K-1M) | 10,635(20.2) | 10.7(0.4) | 9,732(20.2) | 14.5(0.4) | 8,795(20.3) | 17.4(0.5) | |||
| Counties (50K-250K) | 4,744(9.8) | 11.9(0.8) | 4,339(9.8) | 16.5(0.9) | 3,899(9.9) | 19.4(0.9) | |||
| Counties (<50K) | 7,163(16.9) | 10.3(0.4) | 6,531(16.9) | 13.8(0.6) | 5,833(16.7) | 16.0(0.6) | |||
| Income(quartile) | .1826 | .5740 | 0.7473 | ||||||
| 1 | 14,388(28.2) | 10.9(0.3) | 13,182(28.3) | 15.2(0.4) | 11,872(28.3) | 18.1(0.3) | |||
| 2 | 13,342(26.4) | 11.8(0.3) | 12,140(26.3) | 15.9(0.4) | 10,872(26.2) | 18.6(0.4) | |||
| 3 | 12,908(24.1) | 11.1(0.3) | 11,814(24.1) | 15.3(0.4) | 10,609(24.1) | 18.0(0.4) | |||
| 4 | 12,239(21.3) | 11.2(0.3) | 11,164(21.3) | 15.4(0.3) | 10,055(21.4) | 18.4(0.4) | |||
|
| |||||||||
| Hospital characteristics | |||||||||
|
| |||||||||
| Hospital control | .3045 | .0293* | .0057* | ||||||
| Government | 9,821(16.3) | 10.6(0.5) | 9,000(16.3) | 14.1(0.5) | 8,116(16.4) | 16.7(0.5) | |||
| Private | 7,641(12.8) | 11.6(0.6) | 6,992(12.8) | 16.2(0.7) | 6,264(12.8) | 19.4(0.7) | |||
| Not-profit | 35,415(70.9) | 11.4(0.2) | 32,308(70.8) | 15.6(0.3) | 29,028(70.8) | 18.4(0.3) | |||
| Teaching status | .0180* | .0002* | .0004* | ||||||
| Teaching-metropolitan | 34,736(68.1) | 11.1(0.2) | 31,746(68.1) | 15.2(0.3) | 28,518(68.1) | 18.0(0.3) | |||
| Non-teach metropolitan | 16,811(28.4) | 11.9(0.3) | 15,343(28.4) | 16.5(0.4) | 13,806(28.4) | 19.3(0.4) | |||
| Non-teach rural | 1,330(3.5) | 9.2(0.9) | 1,211(3.5) | 12.0(1.0) | 1,084(3.4) | 14.5(1.1) | |||
| Hospital size | 0.1022 | .1209 | .2238 | ||||||
| Small | 2,172(4.6) | 11.3(0.7) | 1,970(4.6) | 16.5(1.0) | 1,795(4.6) | 19.9(1.2) | |||
| Medium | 9,708(18.3) | 10.4(0.5) | 8,874(18.4) | 14.5(0.6) | 8,011(18.5) | 17.6(0.6) | |||
| Large | 40,997(77.1) | 11.5(0.2) | 37,456(77.0) | 15.6(0.2) | 33,602(76.9) | 18.3(0.2) | |||
| Hospital volume (quartile) | 0.2879 | .0054* | .0021* | ||||||
| 1 | 13,412(25.5) | 11.8(0.3) | 12,230(25.5) | 16.6(0.3) | 10,974(25.5) | 19.9(0.5) | |||
| 2 | 13,119(24.5) | 11.4(0.3) | 11,951(24.4) | 15.7(0.4) | 10,078(24.5) | 18.2(0.5) | |||
| 3 | 13,239(24.5) | 11.2(0.4) | 12,142(24.5) | 15.2(0.5) | 10,896(24.5) | 18.0(0.5) | |||
| 4 | 13,107(25.5) | 10.7(0.5) | 11,977(25.5) | 14.2(0.6) | 10,754(25.5) | 16.9(0.7) | |||
weighted %,
weighted row % SE=Standard Error,
significant at p-value of 0.05;
denominator of readmission rate was based on the total sample in that specific age group at that admission period.
SE, standard error; CI, confidence interval; ED, emergency department; SNF, skilled nursing facility; ICF, intermediate care facility.
Covariates
We adjusted for the following covariates in all analytical models: sex (male/female), admission type (elective/non-elective), emergency room services (yes/no), primary payer (Medicare, Medicaid, private, self and other), Elixhauser comorbidity score24, county of residence by urban status (central, fringe, county population 250,000-1,000,000, population 50,000-250,000, population <50,000), income (zip-code level quartile), hospital ownership (e.g., government, private and non-profit), hospital bed size (small, medium and large) and hospital volume (quartile).
Primary 30-day Readmission Reasons
We identified the primary reasons for 30-day readmission by age, based on the ranked prevalence of each primary diagnosis assigned to each patient at 30-day readmission.
Statistical Analyses
We examined the time to first readmission using time-to-event analysis. Unadjusted readmission rates from day 1 to day 90 post-discharge were estimated using the Kaplan-Meier method, stratified by age groups. The follow-up period was censored at 12/31/2013 due to non-availability of 2014 data. Multivariate logistic regression was used to adjust for all the above-listed covariates to estimate the risk of 30-, 60-, or 90-day readmission associated with the primary variable (age), as well as the secondary variables (severity of injury and discharge setting). The denominators for ‘readmission rate’ were based on the total sample size of the specific readmission timeframe, age group and sex (e.g., 30-day readmission: the overall denominator is 52,877; for males, it is 31,363). All analyses were adjusted for NRD survey design (cluster, strata and weights) to allow for generalization of estimates. Analyses were conducted at three time points (30-, 60- and 90-day) on outcome (readmission) and also by sex (male vs. female) to examine the effect of time and sex on readmission. We also examined the interactions between sex/age and secondary variables. We used SAS 9.4 to perform all analyses25.
Results
Demographics
The largest cohorts of patients were 76+ years (37.0%), male (59.1%), discharged to home (59.3%), in the lowest quartile of income (28.2%) at baseline; had non-elective admissions (96.7%), an emergency department visit prior to the index hospitalization (87.3%), Medicare as the primary payer (52.2%), moderate severity of injury (42.3%) and resided in fringe counties (24.0%) (N=52,877) (Table 1).
Age and Sex Associated with Hospital Readmission
Unadjusted Hospital Readmission
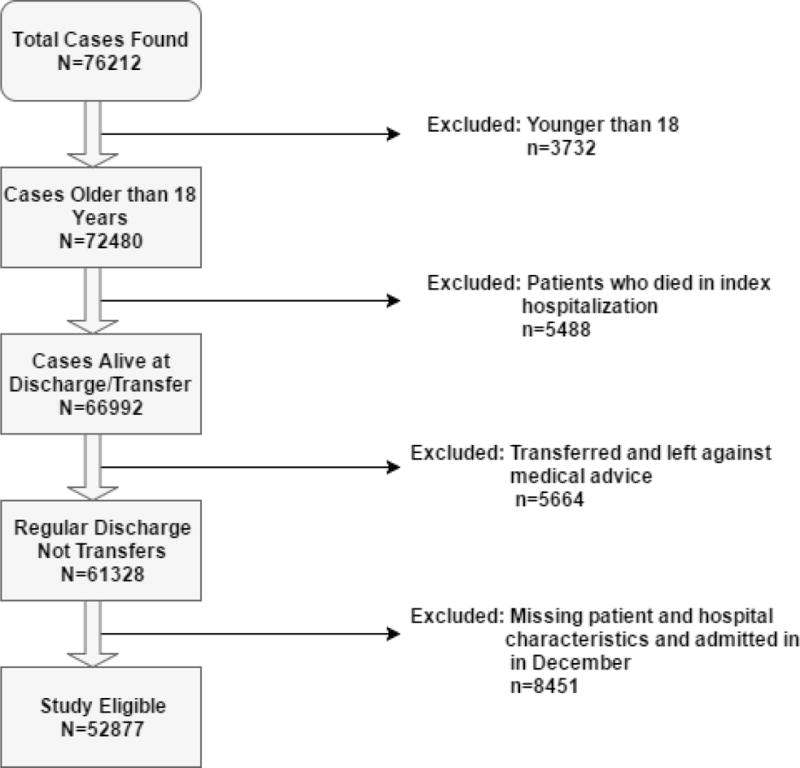
Table 1 shows significant sex differences in 30-, 60- and 90-day unadjusted hospital readmission among all age groups (all p< .05). Figure 2 presents the unadjusted hospital readmission trajectory by sex for all age groups across 90 days. Females 66-75 years had a very similar readmission pattern to females 76+ years. The youngest group (18-40 years) had the most distinct readmission pattern over 90 days compared to the other age groups, regardless of sex (Figure 2).
Figure 2.
Hospital Readmission Trajectory of Four Age Groups over 90 Days by Sex (Unadjusted Kaplan-Meier Censoring Method) (Sample size for male: 33,282; for female: 19,595).
X-axis represents time (days). Y-axis represents readmission rate.
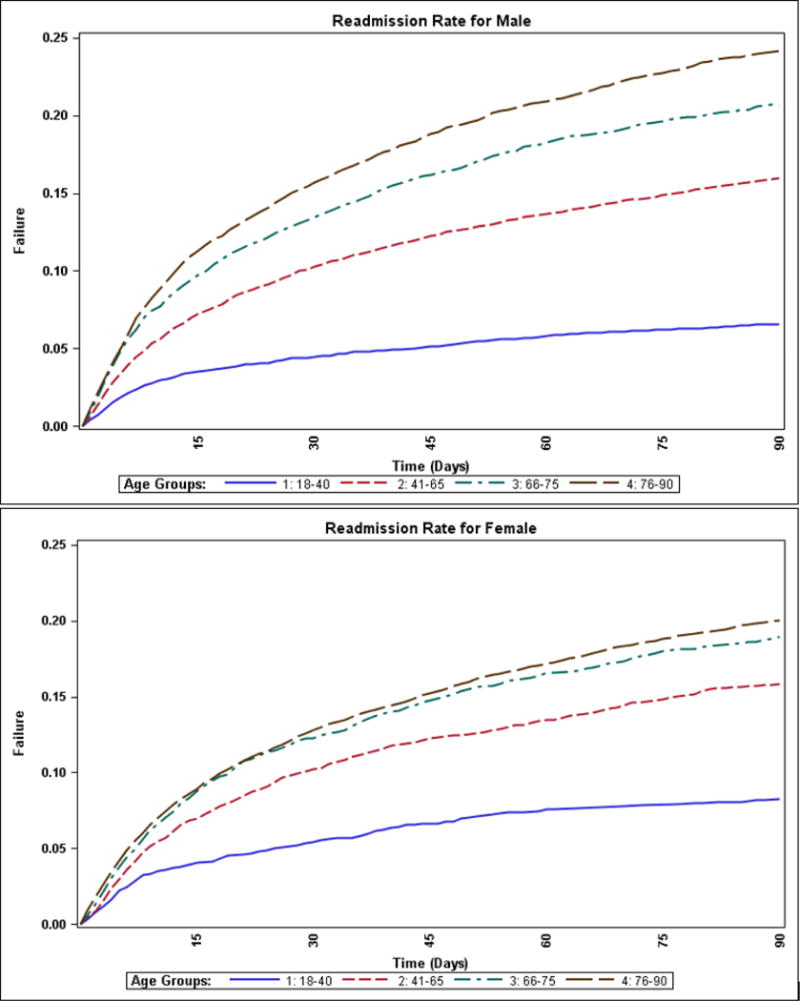
Cumulative Daily Unadjusted Readmission Percent
Figure 3 shows the daily readmission rate for all age groups by sex, among those with any readmission within 90 days from January 1st through September 30th. Table 2 summarizes the cumulative unadjusted readmission rate by sex weekly for the first five weeks. Overall, the youngest group (18-40 years) had the highest cumulative readmission rate during the first week post-discharge, regardless of sex (34.92% for males and 35.15% for females) (Table 2).
Figure 3.
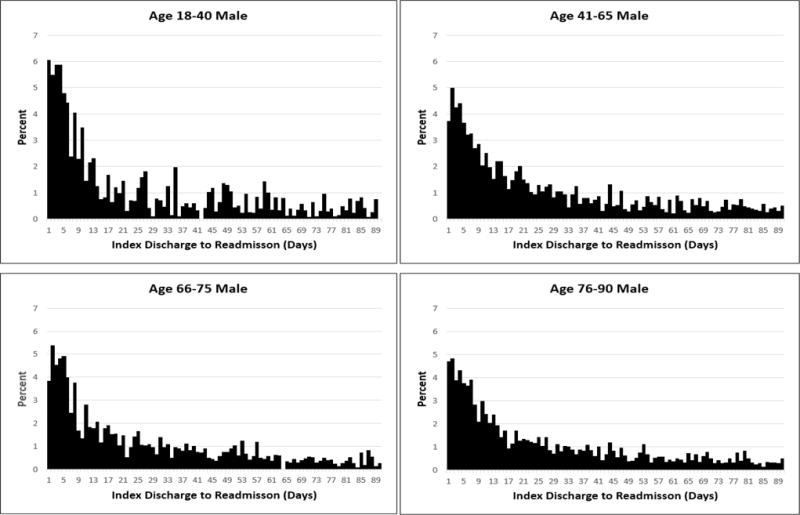
Daily Rate of Hospital Readmission Percentage for Four Age Groups by Sex.
X-axis represents time (days) from index discharge to readmission. Y-axis represents the readmission percent of each time point (day).
Table 2.
Percent of Unadjusted Hospital Readmissions across Age Groups by Sex (Per Week; January through September). (Sample size for males: 33,282; for females: 19,595).
| 1st wk* | 2nd wk | 3rd wk | 4th wk | 5th wk | |
|---|---|---|---|---|---|
| Age Group (years) | (1–7 days) | (8–14 days) | (15–21 days) | (22–28 days) | (29–35 days) |
| Male | |||||
|
| |||||
| 18–40 | 34.92(%)** | 17.01 | 7.56 | 6.76 | 5.45 |
| 41–65 | 27.56 | 15.78 | 11.81 | 8.20 | 6.53 |
| 66–75 | 29.91 | 15.29 | 10.46 | 7.75 | 6.49 |
| 76+ | 29.02 | 16.67 | 9.48 | 8.41 | 6.22 |
|
| |||||
| Female | |||||
|
| |||||
| 18–40 | 35.15 (%)** | 14.05 | 7.22 | 6.79 | 5.98 |
| 41–65 | 26.57 | 17.88 | 9.59 | 8.80 | 7.11 |
| 66–75 | 26.00 | 18.14 | 13.35 | 6.27 | 4.98 |
| 76+ | 27.12 | 15.80 | 10.31 | 8.16 | 6.61 |
wk=week.
All numbers are percentages. The denominator is the total sample size of each age group by sex.
Adjusted Hospital Readmission
Table 3 presents the adjusted Odds Ratio (OR) of readmission. The interactions between age/sex and injury severity level/discharge setting were not significant (p> .05). The main difference at three time-point in readmission rates was between the oldest group and the youngest group (for both males and females) [e.g., 90-day readmission: OR= 2.32 (95% CI: 2.01-2.69) for males vs. OR: 1.96 (95% CI: 1.59 – 2.43) for females] (Table 3). Using the 18-40 year group as a reference, the 76+ group had the highest risk of 30-, 60-, and 90-day readmission for both sexes (Table 3).
Table 3.
Age (by Sex), Severity and Discharge Location for Adjusted 30-, 60- and 90-Day Hospital Readmission.
| Patient characteristic | 30-day readmission | 60-day readmission | 90-day readmission |
|---|---|---|---|
| OR(95%CI)* | OR(95%CI) | OR(95%CI) | |
| Demographic characteristics | |||
| Age Group (years) | |||
| Male | |||
| Four groups | |||
| 18–40 | Ref. | Ref. | Ref. |
| 41–65 | 2.11(1.83, 2.43) | 2.15(1.89, 2.46) | 2.19(1.94, 2.46) |
| 66–75 | 2.07(1.73, 2.47) | 2.16(1.85, 2.52) | 2.09(1.81, 2.42) |
| 76+ | 2.24(1.90, 2.63) | 2.28(1.95, 2.67) | 2.32(2.01, 2.69) |
| Two groups | |||
| 18–40 | Ref. | Ref. | Ref. |
| 41+ | 2.17(1.90, 2.48) | 2.22(1.97, 2.50) | 2.31(2.08, 2.57) |
|
| |||
| Female | |||
| Four groups | |||
| 18–40 | Ref. | Ref. | Ref. |
| 41–65 | 1.48(1.15, 1.90) | 1.47(1.15, 1.89) | 1.65(1.33, 2.06) |
| 66–75 | 1.54(1.17, 2.02) | 1.59(1.22, 2.08) | 1.71(1.36, 2.15) |
| 76+ | 1.69(1.32, 2.17) | 1.76(1.37, 2.26) | 1.96(1.59, 2.43) |
| Two groups | |||
| 18–40 | Ref. | Ref. | Ref. |
| 41+ | 1.54(1.22, 1.94) | 1.51(1.21, 1.89) | 1.68(1.36, 2.08) |
|
| |||
| Severity of Injury | |||
| Minor | Ref. | Ref. | Ref. |
| Moderate | 1.16(1.07, 1.27) | 1.25(1.16, 1.35) | 1.30(1.20, 1.40) |
| Major | 1.40(1.25, 1.56) | 1.42(1.28, 1.58) | 1.43(1.29, 1.59) |
| Extreme | 1.21(1.04, 1.41) | 1.22(1.06, 1.40) | 1.29(1.11, 1.48) |
|
| |||
| Discharge Destination | |||
| SNF, ICF | Ref. | Ref. | Ref. |
| Home Health | 1.08(0.96, 1.21) | 0.97(0.99, 1.07) | 0.95(0.86, 1.06) |
| Home | 0.79(0.71, 0.87) | 0.74(0.68, 0.80) | 0.74(0.68, 0.80) |
|
| |||
| Teaching Status | |||
| Teaching-Metropolitan | Ref. | Ref. | Ref. |
| Non-Teaching-Metropolitan | 1.00(0.91, 1.10) | 0.99(0.92, 1.07) | 0.97(0.90, 1.05) |
| Non-Teaching-Rural | 0.78(0.62, 1.00) | 0.71(0.57, 0.88) | 0.74(0.61, 0.91) |
Adjusted for all covariates listed in Table 1 (sex, admission type, emergency room use, primary insurance payer, Elixhauser comorbidity score, county of residence, income, hospital ownership, hospital teaching status, hospital bed size, and hospital volume).
OR, odds ratio; CI, confidence interval; SNF, skilled nursing facility; ICF, intermediate care facility.
We also collapsed the four groups into two (18-40 vs. 41+ years) to conduct two-group comparisons. This categorical simplification was based on the unadjusted results in Figure 2 (i.e., the 18-40 group showed a distinct readmission pattern, regardless of sex). Using 18-40 as a reference, those 41 and above had significantly higher risk of 30-, 60- and 90-day readmission for both males and females (Table 3).
Characteristics of Multiple Readmissions
Among readmitted patients, about 68% (n=8,420) had only one readmission. For those with multiple readmissions (n=3,962), the average number of readmission was 2.7 (SD=1.3), total diagnoses was 9.9 (SD=5.8), total number of care procedures was 2.0 (SD=2.8) and the mean Elixhauser comorbidity score was 2.8 (SD=5.9). The majority of patients with multiple readmissions were female (63.6%), intracranially injured (69.1%), non-elective admitted (97.1%), Medicare covered (46.1%) and had emergency department visits (87.6%).
Primary 30-day Readmission Reasons by Age
We also examined the primary reason for 30-day readmission by age based on DRG. This study only reported the primary readmission reasons by age for study clarity. Poisoning/bodily injury was the most common reason for 30-day readmission across all ages, but other reasons varied by age. For those aged 18-40 and 41-65, the top three reasons included mental disorder; disease of the nervous system; and sense organs and disease of the circulatory/digestive system(s). For those aged 66-75 and older, the top three 30-day readmission reasons included disease of the circulatory system; disease of the respiratory system, infectious and parasitic disease; and disease of the genitourinary system (Appendix Table).
Secondary Variables and Hospital Readmission
Age group and sex showed no significant interaction with all three secondary variables. Individuals with the three most severe levels of injury (moderate, major and extreme) had significantly higher 30-, 60- and 90-day readmission risk than those with minor injury (Table 3). Those with major injury had the highest ORs of 30-. 60- and 90-day readmission. Using SNF/ICF as a reference, patients discharged to home had significantly lower readmission risk at 30-, 60- and 90-days (Table 3). Using teaching-metropolitan hospital as a reference, non-teaching rural hospital had significantly lower 60- and 90-day readmission risk (Table 3).
Discussion
This study examined the impact of age and sex on 30-day, 60-day and 90-day all-cause readmission for adults with TBI using a national representative dataset (NRD). Age and sex were significantly associated with readmission at three time points, severity of injury and types of post-acute discharge settings. The oldest group (76+ years) of males and females had the highest adjusted readmission risk of all age groups. Sex differences in readmission risk were significant across age groups. These findings suggest that early preventive strategies for readmission in patients with TBI should differ by age and sex.
Another significant finding is the timing of hospital readmission. Among those admitted within 90 days, the youngest group (18-40 years) had the highest cumulative readmission rate within the first week post-discharge, but the lowest readmission rate over 90 days, for both males and females. This study finding suggests that care continuity/monitoring during the first week after discharge is of utmost importance for younger and middle-aged patients with TBI. Providing early follow up may alleviate the risk of readmission in TBI26–28. Early intervention such as symptom management prior to discharge could also reduce the readmission risk for patients with TBI3.
Contradictorily, the Canadian population-based TBI study19 found no sex differences in the number of rehospitalizations for the first year, even though women between 15 and 49 years old had 15% more rehospitalizations than men at the 3-year follow-up. Such inconsistency may be due to the variety in study timeframe and national healthcare policies between this study and ours. However, our study agreed with Saverino et al.19 that those who were male, older, had more severe injury and more comorbidities had significantly higher readmission rates over time.
The primary causes of 30-day readmission in our sample were ‘poisoning/body injury’ and ‘circulatory system disease’ for those aged 41 or older. One study found self-poisoning to be the primary cause of suicidal deaths and attempts in a TBI sample29. Individuals with TBI tend to be in risky conditions that could lead to toxic or overdosing substance consumption and subsequent readmission. However, readmissions caused by poisoning/body injury are potentially preventable. Providing suicidal prevention, home care education, safety or environmental modification to remove unsafe triggers (e.g., drugs) may address such concerns. For ‘circulatory system disease,’ cardiac dysfunction in the first two weeks after TBI was found associated with higher rates of in-hospital mortality30. Consistently, our findings suggest that timely intervention in symptoms management and improved compliance with medication for cardiac disease may facilitate the hemodynamic management of TBI and further avoid follow up readmissions15.
We also suggest that younger and older patients with TBI (using 65 years as a cutoff) may require different protective mechanisms to maximize health outcomes. For example, psychosocial support may be more important for middle-aged patients with TBI, as Corrigan and colleagues13 found that individuals with TBI aged 30-59 years had poorer mental and emotional outcomes compared to older patients with TBI. Patients older than 65 years may benefit more than younger patients from medical management of chronic and comorbid conditions.
Patients with greater severity of injury had higher readmission risk within 90 days. Intiso and colleagues8 observed that readmitted patients with TBI were more disabled than those not readmitted. In addition, Hammond and colleagues31 found that TBI patients with higher motor functional status at admission were less likely to be readmitted to hospitals. While our study found that major loss of function (instead of extreme) was associated with a higher risk of readmission, we hypothesized that our result could be skewed due to a higher mortality rate for those with extreme severity of injury. However, additional data is not available to validate this assumption.
Selecting appropriate discharge setting could be crucial to optimize health outcomes. Patients discharged to SNF/ICF may be at greater risk of readmission than those discharged to home care. Hammond and colleagues30 also found discharge to institutional settings was associated with higher hospital readmission rates compared to discharge to home. Discharge to SNF also significantly increased the risk of depression in both men and women post-TBI31. Our and previous studies have shown the importance of monitoring quality of care and supporting psychosocial function across discharge settings in those with TBI.
Patients receiving services at non-teaching rural hospitals tend to have lower risk of hospital readmission at 60- and 90-day follow-up than those receiving services at teaching-metropolitan hospitals. In metropolitan areas, readmission rates were similar for teaching and non-teaching hospitals. Rural hospitals are less likely to treat patients with complex medical conditions due to limited capabilities, and rural hospitals have higher unplanned readmission rates when multiple-hospital patients are excluded from analysis32.
Brain injury often requires extensive rehabilitation and follow-up care. Understanding the factors associated with readmission risk thus helps guide strategies for effective care planning. We suggest future studies link the NRD with clinical data to provide additional clinical information and practical implementation.
Study Limitations
This study had several limitations. First, we did not address variations in brain injury types, levels of cognitive impairment or severity measures, as these data (e.g., the Glasgow Coma Scale) were not available. Second, varied diagnostic codes for brain injury may inherently have varied readmission risks. Future studies should investigate whether analyzing different ICD-9 diagnostic codes (e.g., bone fracture, intracranial nerve injury) affects the estimated readmission risk. Also, our conservative operational definition may underestimate hospital readmission rates and the results may not be comparable to other TBI studies. In addition, the NRD had a lower prevalence of TBI compared to the CDC report, which may under-represent the real TBI population. Lastly, this study utilized only one-year data, potentially limiting the implications and generalizability of the findings. For instance, we could not construct a look-back window or identify any previous brain injuries prior to the TBI diagnosis at the index date. NRD also lacks information on whether patients were readmitted to acute medical wards or mental health institutions.
Conclusion
We found that age and sex were significantly associated with 30-, 60- and 90-day hospital all-cause readmission in patients with TBI. Specifically, males were more at risk than females of 90-day readmission if they were 76+ years old. Females aged 66-75 and 76+ had similar readmission risk over 90 days. Recognizing age- and sex-related readmission patterns is the first step to developing strategies for preventive care for the TBI population. The rational next steps are to align resources and improve communication between all healthcare stakeholders. We also suggest early management of self-poisoning and cardiovascular diseases, and provision of psychosocial support to prevent subsequent readmission. This study provides evidence that adjusting treatment for those with TBI according to age and sex could optimize patients’ follow-up health outcomes.
Supplementary Material
Acknowledgments
Funding Source:
Dr. Ottenbacher is currently receiving a grant (90AR5009) from National Institute on Disability, Independent Living and Rehabilitation Research (NIDILRR), two grants (P2C HD065702 and R01HD069443) from National Center for Medical Rehabilitation Research (NICHD), National Institutes of Health (NIH). Dr. Karmarkar is currently receiving a grant (K01HD086290) from NICHD, NIH. For the remaining authors, none were declared.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- AHA
American Hospital Association
- CMS
Centers for Medicare and Medicaid Services
- DUA
Data Use Agreement
- DRG
Diagnosis Related Group
- HCUP
Healthcare Cost and Utilization Project
- HH
Home Health
- ICF
Intermediate Care Facility
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- NRD
Nationwide Readmissions Database
- OR
Odds Ratio
- SNF
Skilled Nursing Facility
- SID
State Inpatient Databases
- TBI
Traumatic Brain Injury
Footnotes
Reprints are not available
Conflict of Interest Disclaimer: All authors declare that they have no potential conflicts of interest with respect to publish this paper.
References
- 1.Humphreys I, Phillips CJ, Wood RL, Macey S. The costs of traumatic brain injury: A literature review. ClinicoEconomics and Outcomes Research. 2013;5(1):281–287. doi: 10.2147/CEOR.S44625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: A global perspective. NeuroRehabilitation. 2007;22(5):341–353. [PubMed] [Google Scholar]
- 3.Masel BE, DeWitt DS. Traumatic brain injury disease: Long-term consequences of traumatic brain injury. In: Levin HS, Shum DHK, Chan RCK, Levin HS, Shum DHK, Chan RCK, editors. New York, NY, US: Oxford University Press; 2014. pp. 28–53. http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2014-40048-003&site=eds-live&group=test. [Google Scholar]
- 4.Chauhan NB. Chronic neurodegenerative consequences of traumatic brain injury. Restor Neurol Neurosci. 2014;32(2):337–365. doi: 10.3233/RNN-130354. [DOI] [PubMed] [Google Scholar]
- 5.Stocchetti N, Zanier ER. Chronic impact of traumatic brain injury on outcome and quality of life: a narrative review. Crit Care. 2016;20:148. doi: 10.1186/s13054-016-1318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Report to Congress: traumatic brain injury in the United States: epidemiology and rehabilitation. doi: 10.1016/j.apmr.2015.07.001. Available at: http://www.cdc.gov/traumaticbraininjury/pdf/TBI_Report_to_Congress_Epi_and_Rehab-a.pdf. Accessed August 24, 2015. [DOI] [PubMed]
- 7.Coronado VG, McGuire LC, Sarmiento K, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995-2009. J Safety Res. 2012;43:299–307. doi: 10.1016/j.jsr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Intiso D, Fontana A, Maruzzi G, Tolfa M, Copetti M, Di Rienzo F. Readmission to the acute care unit and functional outcomes in patients with severe brain injury during rehabilitation. Eur J Phys Rehabil Med. 2016 Sep 1; doi: 10.23736/S1973-9087.16.04288-X. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Tuel SM, Presty SK, Meythaler JM, Heinemann AW, Katz RT. Functional improvement in severe head injury after readmission for rehabilitation. Brain Inj. 1992 Jul-Aug;6(4):363–72. doi: 10.3109/02699059209034951. [DOI] [PubMed] [Google Scholar]
- 10.Hubbard T, McNeil Ni. A NEHI Issue Brief. Improving medication adherence and reducing readmissions. 2012 Retried on 8/9/2016 from http://www.nacds.org/pdfs/pr/2012/nehi-readmissions.pdf.
- 11.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 12.Marcoux J, Alkutbi M, Lamoureux J, Feyz M, Saluja RS, de Guise E. Discharge against medical advice in traumatic brain injury: Follow-up and readmission rate. Can J Neurol Sci. 2016;26:1–7. doi: 10.1017/cjn.2016.241. [DOI] [PubMed] [Google Scholar]
- 13.Olufajo OA, Metcalfe D, Yorkgitis BK, Cooper Z, Askari R, Havens JM, Brat GA, Haider AH, Salim A. Whatever happens to trauma patients who leave against medical advice? Am J Surg. 2016 Apr;211(4):677–83. doi: 10.1016/j.amjsurg.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 14.Corrigan JD, Cuthbert JP, Harrison-Felix C, Whiteneck GG, Bell JM, Miller AC, Coronado VG, Pretz CR. US population estimates of health and social outcomes 5 years after rehabilitation for traumatic brain injury. J Head Trauma Rehabil. 2014;29(6):E1–9. doi: 10.1097/HTR.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 15.Slocum C, Gerrard P, Black-Schaffer R, Goldstein R, Singhal A, DiVita MA, Ryan C M, Mix J, Purohit M, Niewczyk P, Kazis L, Zafonte R, Schneider JC. Functional status predicts acute care readmissions from inpatient rehabilitation in the stroke population. PLoS One. 2015;10(11):e0142180. doi: 10.1371/journal.pone.0142180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sethuraman KN, Marcolini EG, McCunn M, Hansoti B, Vaca FE, Napolitano LM. Gender-specific issues in traumatic injury and resuscitation: consensus-based recommendations for future research. Acad Emerg Med. 2014 Dec;21(12):1386–94. doi: 10.1111/acem.12536. Epub 2014 Nov 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006 Oct;54(10):1590–5. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turner-Stokes L, Pick A, Nair A, Disler PB, Wade DT. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database of Systematic Reviews. 2015:2. doi: 10.1002/14651858.CD004170.pub3. Art. No.: CD004170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saverino C, Swaine B, Jaglal S, Lewko J, Vernich L, Voth J, Calzavara A, Colantonio A. Rehospitalization After Traumatic Brain Injury: A Population-Based Study. Arch Phys Med Rehabil. 2016 Feb;97(2 Suppl):S19–25. doi: 10.1016/j.apmr.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 20.Healthcare Cost and Utilization Project (HCUP) Overview of the Nationwide Readmissions Database (NRD) 2016 Retrieved on December 15, 2016 from https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
- 21.Averill RF, Goldfield N, Hughes JS, Bonazelli J, McCullough EC, Steinbeck BA, Mullin R, Tang AM, Muldoon J, Turner L, Gay J. All patient refined diagnosis related groups (APR-DRGs), Version 20.0: methodology overview. Wallingford: 3M Health Information Systems. 2003 Retrieved on November 12, 2016 from https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf.
- 22.Fingar KR, Weiss AJ, Barrett ML, Elixhauser A, Steiner CA, Guenter P, Brown MH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016. Dec, All-Cause Readmissions Following Hospital Stays for Patients With Malnutrition: Statistical Brief #218. 2006-2016. [PubMed] [Google Scholar]
- 23.Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. National Center for Injury Prevention and Control; Atlanta, GA: 2004. [Google Scholar]
- 24.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 25.SAS Institute Inc. SAS 9.4. Cary, NC: [Google Scholar]
- 26.Goodman D, Fisher E, Chang C. The revolving door: A report on US hospital readmissions. Princeton, NJ: Robert Wood Johnson Foundation; 2013. [Google Scholar]
- 27.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011 Oct 18;155(8):520–8. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 28.Dhawan P, Rose A, Krassioukov A, Miller WC. Early interventions for mild traumatic brain injury: Reflections on experience. BCMJ. 2006;48(9):442–446. [Google Scholar]
- 29.Simpson GK, Tate RL. Preventing suicide after traumatic brain injury: implications for general practice. Med J Aust. 2007;187(4):229–32. doi: 10.5694/j.1326-5377.2007.tb01206.x. [DOI] [PubMed] [Google Scholar]
- 30.Hammond FM, Horn SD, Smout RJ, Beaulieu CL, Barrett RS, Ryser DK, Sommerfeld T. Readmission to an acute care hospital during inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2015 Aug;96(8 Suppl):S293–303.e1. doi: 10.1016/j.apmr.2014.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Albrecht JS, Kiptanui Z, Tsang Y, Khokhar B, Liu X, Simoni-Wastila L, Zuckerman IH. Depression among older adults after traumatic brain injury: a national analysis. Am J Geriatr Psychiatry. 2015 Jun;23(6):607–14. doi: 10.1016/j.jagp.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jensen PH, Webster E, Witt J. Hospital type and patient outcomes: an empirical examination using AMI readmission and mortality records. Health Econ. 2009;18(12):1440–60. doi: 10.1002/hec.1435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


