Abstract
Background
Triple-drug regimens are the gold standard for HIV therapy. Nucleos(t)ide reverse transcriptase inhibitors (NRTIs) reducing regimens are used to decrease drugs toxicity, exposure and costs. Aim of our study was to evaluate trends of biochemical and inflammatory indices in patients switching to dual therapy (DT).
Methods
We included patients that a) switched to a DT from 2007 to 2015 from a tenofovir/abacavir-based triple regimen b) previously maintained a triple and c) subsequently a dual regimen for 12 months with virological suppression. We retrieved data measured at 5 points (at the switch, 6 and 12 months before and after switch). We used platelet-to-lymphocyte ratio (PLR), neutrophil-to-lymphocyte ratio (NLR) and CD4/CD8 ratio as inflammatory indices. We assessed temporal trends of viro-immunological, biochemical and inflammatory parameters.
Results
Overall, 364 and 65 patients switched from a tenofovir- and an abacavir-triple regimen, respectively.
In the tenofovir-reducing group, creatinine clearance and lipids raised after the switch. There was a significant increase in both CD4+ cells and CD4/CD8. CD8+ cells rose after the switch, while opposite trend was found for PLR.
In the abacavir-reducing group total lipids showed a decrease during the first 6 months after the switch and then stabilized. An increase of CD4+ and a decrease of CD8+ cells was observed during the study period, although not statistically significant. While CD4/CD8 remained stable after simplification, PLR decreased significantly after 6 months, then returning to baseline.
CD8+ cells increased in the tenofovir-reducing group despite a viro-immunological response. Intriguingly, PLR decreased, maintaining this trend for 12 and 6 months after tenofovir and abacavir interruption respectively.
Conclusions
Increased PLR has been linked to hypercholesterolemia and metabolic-syndrome, while high CD8+ cells count to increased risk of non-AIDS-related events regardless of CD4 T-cell recovery and to virological failure. Whether these findings may have clinical implications, and which role DT plays on the immune system and on inflammation should be further investigated.
Keywords: HIV, Switch, Dual-therapy, Inflammation, Antiretroviral therapy
Background
Since the start of the epidemic in the early eighties, huge efforts have been made in order to develop effective therapies against HIV virus [1]. Triple-drug regimens have proved their efficacy in controlling viral replication [2] and are now considered the gold standard for the treatment of HIV infection both in antiretroviral-naïve and in antiretroviral-experienced patients. These regimens normally include two nucleos(t)ide reverse transcriptase inhibitors (NRTIs) as a backbone, plus one core agent drug from another class: protease inhibitors (PIs), integrase inhibitors (INSTIs) or nucleoside reverse transcriptase inhibitors (NNRTIs) [3–5]. Thanks to these therapies, patients with HIV are now living longer, though experiencing a higher prevalence of aging-related comorbidities, such as metabolic disorders, renal, cardiovascular and liver diseases in addition to neurocognitive impairment [6]. Whether these events are due to adverse effects of long-term use of combined antiretroviral therapy (cART) remains a matter of concern [7]. Tenofovir disoproxil fumarate (TDF) and abacavir (ABC), respectively co-formulated with emtricitabine and lamivudine, have been the two NRTIs combinations most frequently used in clinical practice [5]. Both these NRTIs are well tolerated, although adverse effects often occur in patients who take them chronically. Indeed, TDF has been associated with acute and chronic renal impairment, small molecular weight proteinuria, nephrogenic diabetes insipidus, nephrotic syndrome, Fanconi syndrome [8, 9] and reduction in bone mineral density [10].
Moreover, yet still controversial [11, 12], ABC has been associated with an increased cardiovascular risk [13, 14]. Recently, NRTIs reducing regimens are used as an alternative approach in clinical practice to decrease drugs toxicities, exposure and costs in both cART-naïve and experienced patients [15–17].
Due to the different pharmacokinetic characteristics of each drug, triple drugs regimens offer more chances of an adequate tissue penetrance and distribution, in order to achieve a wider suppression of HIV replication [18]. The efficacy of simplified regimens needs to be addressed by further studies, and so the effects of reducing strategies on systemic inflammation and immunoactivation.
Given that certain dual therapy regimens have already proved to have good virological outcomes when compared to standard triple therapy in cART-experienced patient [19], aim of our study was to evaluate the trends of simplification to dual therapy in a cohort of patients coming from TDF or ABC-containing triple regimens, focusing on biochemical and inflammatory changes.
Methods
The Italian MASTER cohort is a hospital-based multicenter, open HIV cohort established in the mid-1990s, with retrospective patients enrollment from 1986 to 1997 and prospective recruitment subsequently. Patients are recruited from 8 HIV clinics in Italy. Inclusion criteria include a positive HIV-1 or HIV-2 antibody test, or a positive HIVRNA, and being in care in one of the participating centers. As long as the cohort first objective was to represent the epidemiological and clinical trend of HIV infection through the country, enrollment in MASTER is independent from the HIV disease stage, degree of immunosuppression or use of antiretroviral therapy. Clinical data are recorded for each patient in an electronic database every three/four months and a data check is performed at a central level every six months [20]. In the present study, we included all patients that a) switched to a dual therapy between January 2007 and June 2015 coming from a triple regimen that included tenofovir/emtricitabine (TDF/FTC) or abacavir/lamivudine (ABC/3TC) b) had been durably on a ABC/TDF-containing triple therapy for 12 months before switching and c) have maintained dual therapy for 12 months.
In the switch to dual therapy, those who were prescribed regimen 1 to 3 (Table 1) suspended TDF and ABC respectively co-formulated with emtricitabine and lamivudine. In these patients the PI was maintained and associated with 3TC. Those who were switched to regimen 4 suspended both the NRTIs, starting one INSTI and maintaining the PI.
Table 1.
Demographic and clinical features at switch to dual therapy
| Variables | From tenofovir/emtricitabine n (%) (n = 364) |
From abacavir/lamivudine n (%) (n = 65) |
p-valuea |
|---|---|---|---|
| Male | 249 (68.4) | 52 (80.0) | 0.060 |
| Age, in years, mean (SD) | 48.1 (10.2) | 51.0 (10.4) | |
| < 40 | 65 (17.9) | 5 (7.7) | 0.093 |
| 40–49 | 145 (39.8) | 26 (40.0) | |
| ≥ 50 | 154 (42.3) | 34 (52.3) | |
| Intravenous Drug Use | 85 (27.6) | 15 (25.9) | 0.953 |
| HCV co-infection | 134 (36.8) | 24 (36.9) | 0.987 |
| CD4 cell count, cell/mm3, mean (SD) | 631.6 (295.6) | 678.1 (342.2) | |
| < 200 | 15 (4.9) | 1 (1.8) | 0.674 |
| 200–349 | 35 (11.4) | 8 (14.6) | |
| 350–499 | 51 (16.7) | 8 (14.6) | |
| ≥ 500 | 205 (67.0) | 38 (69.1) | |
| Positive HIV-RNA, > 37 copies/mL | 37 (12.3) | 6 (11.3) | 0.835 |
| Time (months) in tenofovir/abacavir | 110.0 (68.3) | 110.4 (78.7) | 0.970 |
| Dual regimens: | |||
| Atazanavir/r + 3TC (regimen 1) | 121 (33.2) | 17 (26.2) | < 0.001 |
| Darunavir/r + 3TC (regimen 2) | 84 (23.1) | 14 (21.5) | |
| Lopinavir/r + 3TC (regimen 3) | 31 (8.5) | 1 (1.5) | |
| Raltegravir/dolutegravir+PI/r (regimen 4) | 128 (35.2) | 33 (50.8) | |
| Number of patients with at least one previous virological failure | 79 (21.7) | 25 (38.5) | 0.004 |
aWe used Student t-test for comparison of means Chi-squared test for comparition of proportions
We retrieved data on gender, age, date of enrollment, country of origin, HIV exposure risk and viral hepatitis C co-infection from the MASTER electronic database at the switchover date. The following parameters, measured at 5 different points of follow-up (12 months before, 6 months before, at the switch to dual therapy, 6 months after and 12 months after the switch), were also collected: HIV-RNA, CD4 cell count, CD8 cell count, neutrophils, lymphocytes and platelets counts, total cholesterol, high density lipoprotein (HDL) cholesterol, low density lipoprotein (LDL) cholesterol, triglycerides, serum creatinine and transaminases.
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and the principles of Good Clinical Practice. The study protocol was approved by the local ethics committees on the 4th of August, 2009, reference number 708. Written informed consent was obtained by all patients enrolled [20].
Outcomes
We evaluated temporal trends of virological and biochemical parameters and inflammatory indices, before and after the switch to dual therapy.
The creatinine clearance (CCr) was estimated from the serum creatinine, weight and height according to the Cockcroft Gault equation [21]. We used platelet-to-lymphocyte ratio (PLR), neutrophil-to-lymphocyte ratio (NLR) and CD4/CD8 ratio as inflammatory indices.
Statistical analysis
We performed a retrospective, multicenter, case cross-over study [22]. The study period for each subject went from 12 months before to 12 months after the switchover date. The parameters were expressed in means (standard deviations, SDs) or proportions as appropriate, according to the follow-up points (12 months before, 6 months before, at the switch to dual therapy, 6 months after and 12 months after the switch). We compared the characteristics at the moment of switchover between subjects coming from tenofovir-based regimens and those coming from abacavir-based regimens using common statistical tests for comparison of means (Student’s t-test) or proportions (Chi-squared test). We assessed temporal trends of HIV-RNA, CD4 cell count, CD8 cell count total, ALT, AST, cholesterol, HDL, LDL triglycerides, CCr, lymphocytes, neutrophils, platelets, PLR and NLR before and after the switch using mixed models for repeated measures. In the analysis we performed random effects mixed models in order to evaluate the role of time (in months) on the changes in biochemical parameters. These models had a random effect on subjects. Age, gender, previous AIDS event, HCV and HBV co-infection are not potential confounders because they are fixed over time. A sensitivity analysis by multiple imputation for missing data was performed. This method requires that the data are missing at random–not related to the missing values. If this assumption holds, resulting estimates (i.e., regression coefficients and standard errors) will be unbiased with no loss of power. We also stratified the analysis according to the regimens after switching (atazanavir, darunavir, lopinavir-ritonavir and integrase inhibitor regimens). The results of mixed models were expressed in terms of coefficients and their 95% confidence intervals (CIs). The coefficient should be interpreted as in a linear regression model: an increase in one unit in time leads to an increase in one unit in the outcome (biological parameters). We have used month as time unit.
All statistical tests were two-sided, where a level of significance of 0.05 has been assumed. Statistical tests were performed using Stata software version 12.0 (StataCorp, College Station, TX, USA).
Results
A total of 6067 subjects were followed in the Master Cohort between 2007 and 2015. TDF- and ABC- containing triple regimens were prescribed at least once to 1702 and 745 patients, respectively. Overall, simplification rate to dual therapy per 100 person-years was 8.83 (CI 95% 8.02–9.69) from both TDF- and ABC-containing triple regimens, while it was 7.50 (6.76–8.30) and 1.32 (1.02–1.68) for TDF- and ABC-containing triple regimens, respectively.
A total of 429 subjects (70.2% males) with a mean age of 49.8 years were included in this analysis. Demographic and clinical features are showed in Table 1. Overall, 364 patients switched from a TDF-containing triple regimen and 65 from an ABC-containing triple regimen to a dual therapy.
Patients that discontinued TDF, compared to those suspending ABC, had a lower prevalence of males (68.4% vs 80.0%), subjects with age ≥ 40 years (82.1% vs 92.3%) and experienced less virological failure (HIVRNA > 50 copies/ml) (21.7% vs 38.5%) before the simplification.
Dual regimens prescribed were categorized as follows: atazanavir/ritonavir (RTV) plus 3TC (regimen 1), darunavir/RTV plus 3TC (regimen 2), lopinavir-RTV plus 3TC (regimen 3), and raltegravir or dolutegravir plus ritonavir boosted protease inhibitor (regimen 4).
In the TDF reducing-group, when compared to the ABC reducing-group, there was a higher proportion of subjects that underwent regimen 1 (33.2% vs 26.2%) and regimen 3 (8.5% vs 1.5%), and a lower proportion of subjects in regimen 4 (35.2% vs 50.8%). The proportions of subjects in regimen 2 were similar in the two groups.
Biological parameters before and after switch in the TDF-reducing therapy group. Table 2
Table 2.
Parameters during the follow-up in the TDF-reducing therapy group (n = 364). Dual therapy (DT) Alanine transaminase (ALT) Aspartate transaminase (AST) High-density lipoprotein (HDL) Low-density lipoprotein (HDL) Creatinine clearance (CCr) platelet-to-lymphocyte ratio (PLR) neutrophil-to-lymphocyte ratio (NLR)
| Parameters | 12 months before Mean (SD) |
6 months before Mean (SD) |
Swicht to DT Mean (SD) |
6 months after switch Mean (SD) |
12 months after switch Mean (SD) |
From 12 months before to switcha Coef. (CI 95%) |
p-value | From switch to 12 months aftera Coef. (CI 95%) |
p-value |
|---|---|---|---|---|---|---|---|---|---|
| CD4 cell count, cell/mm3 | 611.1 (302.8) | 630.5 (300.5) | 631.6 (295.6) | 659.3 (295.9) | 699.2 (296.3) | 1.9 (0.3,3.5) | 0.023 | 6.8 (4.9,8.8) | < 0.001 |
| CD8 cell count, cell/mm3 | 900.1 (423.6) | 910.2 (439.7) | 872.3 (438.6) | 928.4 (475.8) | 919.2 (474.2) | −1.8 (− 4.9,1.4) | 0.272 | 4.2 (1.2, 7.6) | 0.007 |
| ALT (U/l) | 40.8 (46.8) | 38.4 (33.9) | 37.2 (30.4) | 38.4 (44.6) | 36.6 (35.6) | −0.3 (− 0.7,0.0) | 0.045 | − 0.0 (− 0.1,0.4) | 0.890 |
| AST (U/l) | 33.6 (37.4) | 30.3 (22.8) | 30.3 (24.3) | 29 (29.4) | 30.2 (26.6) | −0.3 (− 0.6–0.0) | 0.028 | −0.0 (− 0.3,0.2) | 0.760 |
| Total Cholesterol (mg/dl) | 184.9 (40.6) | 186.9 (40.6) | 186 (41.4) | 208.4 (45.9) | 199.7 (45.5) | 0.1 (−0.2,0.4) | 0.601 | 1.5 (1.1,1.9) | < 0.001 |
| HDL Cholesterol (mg/dl) | 44.7 (14.8) | 45.9 (16.4) | 46 (15.9) | 49.6 (15.4) | 48.9 (15.9) | 0.2 (0.0,0.3) | 0.009 | 0.3 (0.2,0.5) | < 0.001 |
| LDL Cholesterol (mg/dl) | 111.9 (35) | 113.1 (34.5) | 114.3 (34) | 125.1 (37.2) | 120 (38.2) | −0.1 (−0.2, 0.5) | 0.534 | 0.7 (0.2, 1.1) | 0.005 |
| Triglycerides (mg/dl) | 157.1 (90.9) | 160.5 (85.1) | 155.7 (105.2) | 174.3 (125.3) | 176.3 (141.2) | −0.2 (−1.2,0.7) | 0.629 | 1.3 (0.3,2.3) | 0.009 |
| CCr (ml/min) | 92.1 (25.2) | 91.1 (28.5) | 88.6 (30.2) | 93.2 (28.6) | 95.8 (29.7) | −0.4 (−0.5, − 0.2) | < 0.001 | 0.5 (0.3,0.6) | < 0.001 |
| Lymphocyte, 103/μL | 2087 (789) | 2100 (767) | 2062 (791) | 2202 (868) | 2236 (867) | −3.3 (−8.0, 3.3) | 0.259 | 16.9 (11.2,22.6) | < 0.001 |
| Neutrophils, 103/μL | 4230 (5825) | 3435 (1386) | 3422 (1344) | 3444 (1463) | 3560 (1610) | −65.4 (− 127.4–3.4) | 0.039 | 20.3 (− 1.8, 42.4) | 0.072 |
| Platelets, 103/μL | 216,359 (76022) | 216,525 (73144) | 218,494 (72903) | 214,413 (69168) | 214,286 (69895) | −10.9 (− 394.4, 372.96) | 0.955 | − 420.4 (− 810.2, − 30.5) | 0.035 |
| NLR | 1.9 (0.9) | 1.9 (0.9) | 2 (1.1) | 1.9 (1.2) | 1.9 (0.9) | 0.1 (0.0,0.2) | 0.067 | 0.0 (−0.0, 0.0) | 0.355 |
| PLR | 114.2 (51.5) | 113.4 (51.6) | 118.7 (59.5) | 109.4 (52.8) | 105.0 (46.0) | 0.3 (−0.1, 0.8) | 0.110 | −1.2 (−1.6,-0.7) | < 0.001 |
| CD4/CD8 | 0.79 (0.48) | 0.8 (0.5) | 0.84 (0.47) | 0.81 (0.42) | 0.88 (0.43) | 0.004 (0.001,0.008) | 0.008 | 0.003 (0.001,0.005) | 0.002 |
In the analysis we performed random effects mixed models in order to evaluate the role of time (in months) on the changes in biochemical parameters
aResults remained unchanged when sensitivity analysis by multiple imputation for missing data was performed
The CCr significantly decreased from 92.1 to 88.6 ml/min before the switch, and rose from 88.6 to 95.8 ml/min after the switch (p < 0.001 for both comparisons). CCr showed a significant biphasic trend with a decrease before the switch and an increase after the switch in all the regimens excluding regimen 1, where CCr was stable around 95 ml/min (p = 0.132). The best CCr recovery was observed after switching to the INSTI plus PI regimen (regimen 4) (p < 0.001) (Fig. 1).
Fig. 1.

Temporal trends of glomerular filtration rate (CCr) before and after switch in the TDF-reducing therapy group
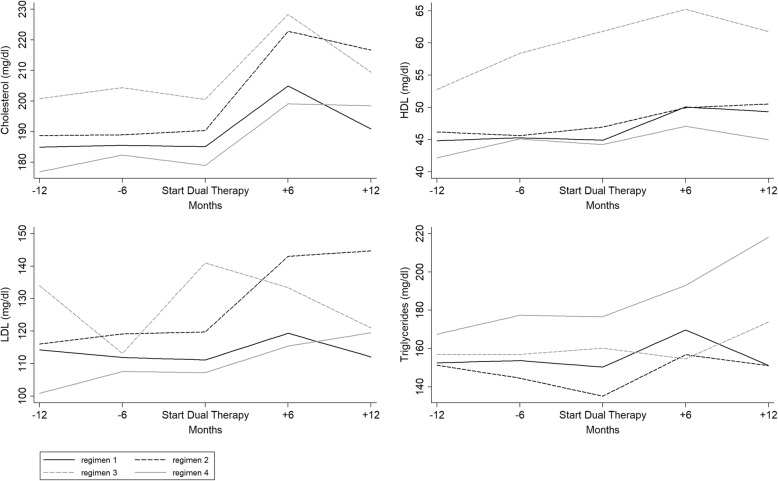
With regard to the lipid pattern, total, HDL and LDL cholesterol and triglycerides showed a fluctuation over time with an overall increase mainly during the first 6 months after the switchover to a dual therapy. After switching to dual therapy, the total cholesterol rose significantly in subjects undergoing regimens 1, 2 and 4 (p < 0.005 for all comparisons). HDL increased in regimen 1 (p < 0.001), whereas LDL rose significantly in regimens 2 and 4 (p < 0.001 for both). Triglycerides declined in the year before the switch in regimen 2 from 151.3 to 135.2 mg/ml (p = 0.045) and increased after the switch in regimen 4 from 176.7 to 218.2 mg/ml (p = 0.022) (Fig. 2).
Fig. 2.
Temporal trends of lipids before and after switch in the TDF-reducing therapy group
There was a significant increase in both CD4+ cell count and CD4/CD8 over the study period. On the contrary, the CD8+ cell count rose only after the switch from 872.3 to 919.2 cell mm3 (p = 0.007). When analyzing the different dual regimens, CD8+ cells trend showed a significant increase only for regimen 4 (p = 0.049) after the switch (Fig. 3).
Fig. 3.
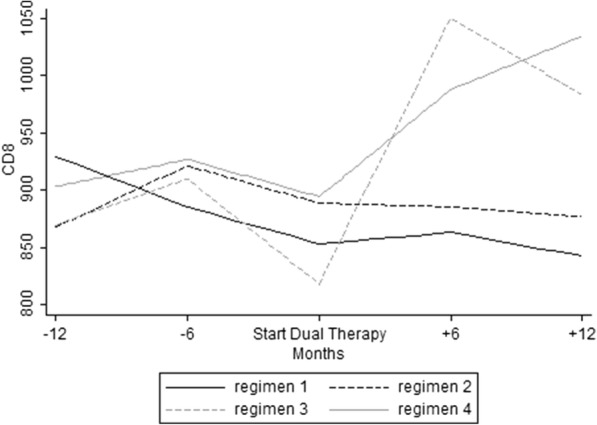
Temporal trends of CD8+ cells before and after switch in the TDF-reducing therapy group
Concerning CD4/CD8 ratio (Fig. 4), we observed a persistent rise before and after simplification only for regimens 1 and 2 (p < 0.001 for both).
Fig. 4.
Temporal trends of CD4/CD8 ratio and platelet/lymphocyte ratio (PLR) before and after switch in the TDF-reducing therapy group
We did not observe any variations of the NLR during the study period. PLR remained stable before and decreased after the switch to dual therapy (from 118.7 to 105.0, p < 0.001). When the 4 regimens were analyzed separately, there was a significant reduction of PLR after the switch for regimen 1 (from 133.4 to 116.7, p < 0.001), regimen 2 (117.3 to 103.4, p = 0.007) and regimen 4 (from 105.4 to 91.4, p = 0.038) (Fig. 4).
Biological parameters before and after switch in the ABC-reducing group. Table 3
Table 3.
Parameters during the follow-up in the ABC-reducing therapy group (n = 65). Dual therapy (DT) Alanine transaminase (ALT) Aspartate transaminase (AST) High-density lipoprotein (HDL) Low-density lipoprotein (HDL) Creatinine clearance (CCr) platelet-to-lymphocyte ratio (PLR) neutrophil-to-lymphocyte ratio (NLR)
| Parameters | 12 months before Mean (SD) |
6 months before Mean (SD) |
Swicht to DT Mean (SD) |
6 months after switch Mean (SD) |
12 months after switch Mean (SD) |
From 12 months before to switcha Coef. (CI 95%) |
p-value | From switch to 12 months aftera Coef. (CI 95%) |
p-value |
|---|---|---|---|---|---|---|---|---|---|
| CD4 cell count, cell/mm3 | 629.9 (327.7) | 656.6 (328) | 678.1 (342.2) | 677.4 (309.6) | 658.9 (265.4) | 1.3 (−2.3,4.9) | 0.481 | 1.6 (−2.4,5.5) | 0.435 |
| CD8 cell count, cell/mm3 | 1023.5 (473.3) | 1069.7 (664) | 982.6 (461) | 992.6 (526.1) | 970.7 (446.6) | −2.5 (− 10.5,5.5) | 0.541 | − 1.3 (− 7.3,4.6) | 0.658 |
| ALT (U/l) | 40.1 (41.6) | 43.5 (64.2) | 44.5 (47.7) | 45.9 (55.9) | 36.7 (34.8) | 0.4 (−0.9,1.6) | 0.580 | −0.2 (− 1.0,0.5) | 0.536 |
| AST (U/l) | 30.2 (28.8) | 31.2 (42) | 29.6 (30) | 32.7 (32.4) | 30.1 (21.4) | 0.1 (−0.8,0.9) | 0.860 | −0.1 (− 0.6,0.4) | 0.761 |
| Total Cholesterol (mg/dl) | 218.5 (44.3) | 220.8 (51.1) | 227.2 (48.8) | 218.4 (54.6) | 215.5 (39.2) | 0.6 (−0.3,1.5) | 0.218 | −1.6 (−2.6–0.6) | 0.003 |
| HDL Cholesterol (mg/dl) | 47.2 (17.4) | 53.5 (19.6) | 49.8 (14.1) | 53.9 (19.5) | 52.8 (19.7) | 0.1 (−0.2,0.4) | 0.604 | 0.2 (−0.1,0.4) | 0.168 |
| LDL Cholesterol (mg/dl) | 141.1 (38.3) | 133.4 (35.5) | 145.6 (42.4) | 138.4 (30.9) | 139.1 (27) | 0.2 (−0.9,1.3) | 0.742 | −0.7 (1.7,0.2) | 0.132 |
| Triglycerides (mg/dl) | 163.8 (92.2) | 180.8 (110.9) | 202.8 (115.5) | 194.2 (234.4) | 172.5 (161.1) | 2.4 (0.3,4.6) | 0.027 | −3.8 (−8.4,0.9) | 0.112 |
| CCr (ml/min) | 94.5 (31.5) | 97 (35.8) | 92.2 (26.8) | 91.6 (28.5) | 92.3 (30.9) | 0.0 (−0.4,0.3) | 0.852 | −0.4 (− 0.8–0.1) | 0.041 |
| Lymphocyte, 103 /μL | 2201 (662) | 2197 (838) | 2191 (663) | 2256 (686) | 2219 (655) | 0.2 (−13.7,14.2) | 0.972 | 6.5 (− 7.8,20.8) | 0.373 |
| Neutrophils, 103 /μL | 3227 (1354) | 3462 (1643) | 3851 (3336) | 3528 (1497) | 6059 (10610) | 40.7 (−32.7114.0) | 0.277 | 153.3 (−82.1388.7) | 0.202 |
| Platelets, 103 /μL | 216,173 (63378) | 213,125 (68580) | 211,927 (59231) | 198,250 (60544) | 217,611 (59716) | −665.6 (− 1486.0, 154.7) | 0.112 | 98.2 (− 781.3977.8) | 0.827 |
| NLR | 1.5 (0.6) | 1.7 (0.9) | 1.8 (1.3) | 1.7 (0.6) | 1.7 (0.7) | 0.2 (−0.2,0.5) | 0.367 | 0.0 (−0.02,0.03) | 0.840 |
| PLR | 106.9 (46.1) | 108.5 (47.7) | 104 (36.6) | 92.5 (31.2) | 107.5 (42.4) | −0.4 (−1.3,0.5) | 0.378 | −0.2 (− 1.1,0.7) | 0.645 |
| CD4/CD8 | 0.73 (0.42) | 0.76 (0.43) | 0.82 (0.47) | 0.81 (0.42) | 0.79 (0.38) | 0.005 (0.002,0.008) | 0.003 | 0.002 (−0.001,0.006) | 0.155 |
In the analysis we performed random effects mixed models in order to evaluate the role of time (in months) on the changes in biochemical parameters
aResults remained unchanged when sensitivity analysis by multiple imputation for missing data was performed
Total and LDL cholesterol and triglycerides showed a decrease during the first 6 months after the switch and then stabilized. Anyway, only the changes on total cholesterol were statistically significant. Overall there was an increase of the CD4+ cells and a decrease of CD8+ cells during the study period, although not statistically significant. Moreover, CD4/CD8 remained stable after simplification. There were no significant changes of NLR and PLR over the observational period. Intriguingly, PLR decreased significantly after 6 months from simplification (coeff. -2.07 95% CI -3.43, − 0.71; p = 0.003), returning then to baseline levels. Due to the low number of subjects in this group, we didn’t perform a stratified analysis for each regimen.
Discussion
An improvement in renal function and a worsening in the lipids profile were observed when TDF was removed from triple regimens, while ABC suspension was followed by a significant decrease in total cholesterol only. With regard to the immune reconstitution and to the inflammatory status, CD4+ cell counts and CD4/CD8 raised after simplification, especially in the TDF-reducing group. Intriguingly, CD8+ cells also increased, but only in the TDF-reducing group.
PLR, but not NLR level, decreased after NRTIs reduction. This trend was maintained for 12 months after TDF interruption and for only 6 months after the suspension of ABC.
During the study period, an overall simplification rate to dual therapy of 8.83/100 person-years has been observed. Simplification rate was higher from TDF- than from ABC-containing triple regimens (7.50/100 vs 1.32/100 person-year). Despite TDF-containing triple regimens were the preferred choice for most patients, physicians had suspended TDF more than ABC, as previously described in other studies focused on dual therapies [16]. This could reflect somehow the tendency to switch to a TDF-free dual-therapy regimen because of kidney or bone adverse effects, especially in an aging population. In the near future, this trend could be reverted thanks to the introduction of tenofovir alafenamide (TAF), which is thought to be safer in terms of renal and bone toxic effects [23].
Nowadays, the strategy of reducing the number of drugs in the cART regimen in order to reduce, or prevent, NRTIs-related toxicities and drug-to-drug interactions is not uncommon. Anyway, very few dual regimens are recommended by national and international guidelines [3–5]. Recently, in an Italian geriatrics cohort, it has been pointed out that around 25% of patients received unconventional dual regimens (mainly NRTIs-sparing), reaching an overall viral suppression in about 95% of patients [24]. NRTIs-sparing dual therapies were also the most frequent regimen used in our study (protease inhibitor plus integrase inhibitor). Although this regimen is not mentioned in the guidelines, enough information, from both trials [15, 16] and observational studies [25], have proved their efficacy and safety profile.
As previously observed in other studies [26–28], an improvement of kidney function and a disappearance of the lipid-lowering effect of TDF were shown after TDF discontinuation, while on the other hand, we observed an improvement of lipids profile after ABC suspension. To the best of our knowledge, no previous studies, apart from Di Giambenedetto and Fabbiani et al. [29, 30], specifically focused on the changes in renal function and lipids concentration during the switch from a triple to a dual cART regimen. Anyway, none of these two studies analyzed results from a TDF- or an ABC-stopping therapy separately. In the cohort from Di Giambenedetto, 82% of patients interrupted TDF, and the modifications observed in lipids and in the renal function were similar to ours.
Information on the impact of the various cART regimens on inflammation/immunoactivation remain very limited [31–35]. Actually, there is no consistent evidence about any differences in the reduction of inflammation and immune activation between protease and integrase inhibitors [33, 36, 37]. TAF and TDF (when included in a triple regimen) seem to have an equivalent impact on monocyte activation and on the reduction of systemic inflammation [38]. Moreover, no studies focused on the effects that NRTIs-reducing strategies may have on inflammatory markers in an overall virologically suppressed cART-experienced population.
Here we show that CD8+ cells increased in the group of patients stopping TDF, but not in those stopping ABC. The meaning of this trend in patients switching to a TDF-reducing therapy needs further studies and a longer follow-up in order to discover whether this finding could have clinical and/or virological implications.
Persistent inflammation is a predictor for clinical events and mortality in HIV-infected patients. Anyway, no agreement has been achieved about which one should be the best marker of inflammation in these cases [39, 40]. Persistently elevated CD8+ cells counts during long-term cART have been linked with increased risk of non-AIDS-related events in HIV-infected patients, regardless of CD4 T-cells recovery, and have been related with a chronic inflammation status, and with increased immuneactivation markers such as IL-6, soluble CD14 and d-dimer [39, 41, 42]. Higher CD8+ cells counts at cART initiation, or an increase in CD8+ cell count during cART, seem to be predictive of virological treatment failure [43–45]. In a study from Mussini et al. [46], a lower increase in CD4/CD8 ratio due to a raise in CD8+ cells was found in those switching to a mono/dual-therapy, when compared to those remaining on a standard triple regimen. Anyway, mono and dual therapies were not separated in this analysis, and the comparative group was composed by patients who remained on a triple regimen.
The persistence of HIV replication in sanctuary sites, despite undetectable viremia in plasma, could explain the persistence of systemic inflammation and immune activation, especially because cART penetration into viral reservoirs and sanctuary sites differs among different antiretroviral drugs. NRTIs-reducing strategies could alter the intracellular total cART concentrations when compared to plasma concentrations [20, 47, 48]. Very few data are available about what happens in HIV sanctuaries and reservoirs when simplified cART regimens are used in persistently HIV suppressed patients. ATLAS study showed that a simplification strategy had the same impact on the cellular viral reservoir when compared to triple regimen, but no data are available about immuno-inflammatory trends [49].
Recently, two biomarkers derived from common blood parameters, the neutrophil to lymphocyte ratio (NLR) and the platelet to lymphocyte ratio (PLR), have shown to be indicative of systemic inflammation [50, 51]. In previous studies from the MASTER cohort, we explored the role of NLR and PLR scores as predictors of cardiovascular events, prognosis of cancer and all-cause mortality, proving that they can have a role as positive predictors of these events [52–56].
In the present study, NLR and PLR levels were low throughout the follow-up period. Anyway, we observed a further significant decrease of PLR, but not of NLR levels, after NRTIs interruption. This trend was maintained for 12 months after TDF interruption, and for only 6 months after the discontinuation of ABC. More studies are needed to explore whether these fluctuations may have a clinical significance, or they are a casual feature. Data coming from either HIV-infected and -uninfected persons could explain this variation.
Previously, poor renal function [57] and low levels of vitamin D [58] have been associated with systemic inflammation during HIV infection. In HIV-uninfected people PLR was found to be an independent predictor of 25(OH)D levels along with PTH, calcium, sex and creatinine [59]. In our study, Vitamin D values were not available. Nevertheless, the impact of TDF on bone metabolism and loss of bone mass is known [60]. Whether the decrease of PLR is related with an improvement on the bone turnover and/or of the bone mass as a consequence of TDF interruption, must be deepened.
PLR was also found to be superior to NLR in predicting higher inflammation in end-stage renal disease in HIV-negative patients [61].
The PLR variation following ABC-reducing therapy could be mediated by the lipid profile improvement. Hypercholesterolemia has been linked to systemic and vascular inflammation through several cytokines [62, 63]. Increased PLR has been significantly associated with both presence and severity of metabolic syndrome in HIV-uninfected people [64]. Here, we observed a reduction on total cholesterol during the first 6 months after ABC suspension (maintained also after 12 months) and a concomitant significant decrease of PLR after 6 months, but not after 12 months from ABC suspension. More studies are needed in order to correlate the variations in the lipid profile with this simple and cheap indirect indicator of inflammation.
Obviously, several limitations are present in our study. They include the weakness of a retrospective study. Second, the sample size in the ABC-stopping group and in the several subgroups of dual therapies were relatively small and the results need to be confirmed in larger populations of patients. A further limitation is that associations between PLR and other inflammatory biomarkers were not measured and possible confounders of inflammation were not assessed.
This was not a prospective controlled study, so we cannot draw cause-and-effect relationships from our findings about inflammation. Despite the difficulties in using retrospective study results, strength of our study is the large sample size of a multicenter cohort.
Conclusions
To conclude, in our study we confirm the disappearance of the lipid-lowering effect and the positive impact on creatinine clearance in those discontinuing TDF, and we observed a decrease of total cholesterol after ABC suspension. Moreover, we found an increase in the CD8+ T-cells besides a PLR reduction in those patients who discontinued TDF and switched to a dual therapy.
Larger controlled studies are required to confirm our findings and to better elucidate the relationship between stopping NRTIs and PLR or- CD8 cells fluctuations. Moreover, a longer follow-up could elucidate whether these findings could correlate with specific clinical events.
Acknowledgements
The Italian MASTER Cohort includes the following collaborators: F. Castelli, G. Carosi, E. Quiros-Roldan, G. Paraninfo, E, Institute of Infectious and Tropical Diseases, University of Brescia, Brescia, Italy; C. Torti, Clinic of Infectious Diseases, Policlinico Universitario “Mater Domini”, Catanzaro, Italy; R. Cauda S. Di Giambenedetto, M. Fabbiani, M. Colafigli, Catholic University of Sacred Heart, Rome, Italy; F. Maggiolo Ospedali Riuniti, Bergamo, Italy; A. Scalzini, F. Castelnuovo, I. El Hamad, Spedali Civili di Brescia, Brescia, Italy; F. Mazzotta, S. Locaputo, N. Marino, P. Pierotti M. Di Pietro, C. Blè, F. Vichi, “S. Maria Annunziata” Hospital, Florence, Italy; L. Sighinolfi, “S. Anna” Hospital, Ferrara, Italy; G. Angarano, N. Ladisa, L. Monno, P. Maggi, Policlinico di Bari, Bari, Italy; A. Pan, S. Costarelli, Istituti Ospitalieri, Cremona, Italy; A. Gori, G. Lapadula, Ospedale S. Gerardo, Monza, Italy; M. Puoti, Ospedale Niguarda Cà Granda Milano, Italy; P. Viale, V. Colangeli, M. Borderi, Policlinico S. Orsola Malpighi, Bologna, Italy. We thank the Infectious Diseases and International Health (MISI) Fundation, Brescia (Italy) for sponsoring the Italian MASTER cohort.
Funding
The Italian MASTER cohort is sponsored by the Infectious Diseases and International Health (MISI) Foundation, Brescia, Italy. The data analysis included in this study were carried out thanks to an unrestricted grant from Gilead to MASTER. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The database used and analyzed for the current study is available from our statistician (Dr. Raffetti Elena: elena.raffetti@gmail.com) on reasonable request.
Abbreviations
- ALT
Alanine transaminase
- AST
Aspartate transaminase
- CART
Combined anti-retroviral therapy (cART).
- CCr
Creatinine clearance
- DT
Dual therapy
- HDL
High-density lipoprotein (HDL)
- HDL
Low-density lipoprotein
- INSTIs
Integrase inhibitors
- NLR
neutrophil-to-lymphocyte ratio
- NNRTIs
Nucleoside reverse transcriptase inhibitors
- NRTIs
Nucleos(t)ide reverse transcriptase inhibitors as a backbone, plus one core agent drug from another class
- PI
Protease inhibitors
- PLR
Platelet-to-lymphocyte ratio
Authors’ contributions
QRE, MP and RE conceived and designed the study. QRE, II, BA, LF, SA, MF and CF made substantial contributions to the acquisition of data. RE performed the statistical analysis. QRE and MP wrote the first version of the manuscript and interpreted data. All authors read, revised critically and approved the final version of the manuscript.
Ethics approval and consent to participate
The study protocol was approved by the Ethic Committee of the Azienda Ospedaliera Spedali Civili of Brescia on the 4th of August, 2009, reference number 708. Written informed consent was obtained by all patients enrolled.
Consent for publication
Not applicable.
Competing interests
EQR received travel grants from Bristol-Myers Squibb, Gilead, Bristol-Myers Squibb, Viiv and Janssen-Cilag; moreover received speaker’s honoraria from Gilead and MSD during the conduct of the study. PM received travel grants from Viiv and Gilead. ER declared no competing interests.
II declared no competing interests. BA reported grants from Bristol-Myers Squibb and Gilead, non-financial support from Bristol-Myers Squibb, Viiv and Janssen-Cilag during the conduct of the study. LF declared no competing interests. SA received travel grants from Bristol-Myers Squibb, Gilead, Bristol-Myers Squibb, Viiv and Janssen-Cilag; moreover received speaker’s honoraria from Bristol-Myers Squibb, Gilead, Bristol-Myers Squibb, Viiv and Janssen-Cilag during the conduct of the study and is currently acting as an Associate Editor for BMC Infectious Diseases. MF declared no competing interests. FC declared no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Eugenia Quiros-Roldan, Email: eugeniaquiros@yahoo.it.
Paola Magro, Email: p.magro@unibs.it.
Elena Raffetti, Email: elena.raffetti@gmail.com.
Ilaria Izzo, Email: izzo.ilaria@hotmail.it.
Alessandro Borghetti, Email: al.bor86@gmail.com.
Francesca Lombardi, Email: francesca.lombardi@gmail.com.
Annalisa Saracino, Email: annalisa.saracino@uniba.it.
Franco Maggiolo, Email: franco31556@hotmail.com.
Francesco Castelli, Email: francesco.castelli@unibs.it.
for the MASTER Cohort:
F. Castelli, G. Carosi, E. Quiros-Roldan, G. Paraninfo, C. Torti, R. Cauda, S. Di Giambenedetto, M. Fabbiani, M. Colafigli, F. Maggiolo Ospedali Riuniti, A. Scalzini, F. Castelnuovo, I. El Hamad, F. Mazzotta, S. Locaputo, N. Marino, P. Pierotti, M. Di Pietro, C. Blè, F. Vichi, L. Sighinolfi, G. Angarano, N. Ladisa, L. Monno, P. Maggi, A. Pan, S. Costarelli, A. Gori, G. Lapadula, M. Puoti, P. Viale, V. Colangeli, and M. Borderi
References
- 1.Vella S, Schwartländer B, Sow SP, Eholie SP, Murphy RL. The history of antiretroviral therapy and of its implementation in resource-limited areas of the world. AIDS. 2012;26(10):1231–1241. doi: 10.1097/QAD.0b013e32835521a3. [DOI] [PubMed] [Google Scholar]
- 2.Montaner JSG, Reiss P, Cooper D, Vella S, Harris M, Conway B, Wainberg MA, Smith D, Robinson P, Hall D, Myers M, Lange JMA, For the INCAS Study Group A randomized, double-blind trial comparing combinations of Nevirapine, Didanosine, and zidovudine for HIV-infected PatientsThe INCAS trial. JAMA. 1998;279(12):930–937. doi: 10.1001/jama.279.12.930. [DOI] [PubMed] [Google Scholar]
- 3.European AIDS Clinical Society Guidelines 2017. Version 8.2. Available: http://www.eacsociety.org/files/guidelines_8.2-english.pdf. Last accessed: 18 Aug 2017.
- 4.World Health Organization Consolidated Guidelines on the use of antiretroviral drugs for treating and preventing of HIV infection. Recomendations for a public approach. 2nd edition, 2016. Available: http://apps.who.int/iris/bitstream/10665/208825/1/9789241549684_eng.pdf Last accessed: 18 Aug 2017.
- 5.Società Italiana di Malattie Infettive e Tropicali (SIMIT). Linee guida italiane sull'utilizzo dei farmaci anti-retrovirali e sulla gestione diagnostico-clinica delle persone coinfezione da HIV. Available: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2545_allegato.pdf. Last accessed: 18 Aug 2017.
- 6.Wing EJ. HIV and aging. Int J Infect Dis. 2016;53:61–68. doi: 10.1016/j.ijid.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Cohen J, Torres C. HIV-associated cellular senescence: a contributor to accelerated aging. Ageing Res Rev. 2017;36:117–124. doi: 10.1016/j.arr.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011;57(5):773–780. doi: 10.1053/j.ajkd.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 9.Mocroft A, Kirk O, Reiss P, et al. Estimated glomerular filtration rate, chronic kidney disease and antiretroviral drug use in HIV-positive patients. AIDS. 2010;24:1667–1678. doi: 10.1097/QAD.0b013e328339fe53. [DOI] [PubMed] [Google Scholar]
- 10.Bedimo R, Maalouf NM, Zhang S, Drechsler H, Tebas P. Osteoporotic fracture risk associated with cumulative exposure to tenofovir and other antiretroviral agents. AIDS. 2012;26:825–831. doi: 10.1097/QAD.0b013e32835192ae. [DOI] [PubMed] [Google Scholar]
- 11.Cruciani M, Zanichelli V, Serpelloni G, Bosco O, Malena M, Mazzi R, et al. Abacavir use and cardiovascular disease events: a meta-analysis of published and unpublished data. AIDS. 2011;25:1993–2004. doi: 10.1097/QAD.0b013e328349c6ee. [DOI] [PubMed] [Google Scholar]
- 12.Bavinger C, Bendavid E, Niehaus K, Olshen RA, Olkin I, Sundaram V, et al. Risk of cardiovascular disease from antiretroviral therapy for HIV: a systematic review. PLoS One. 2013;8:e59551. doi: 10.1371/journal.pone.0059551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Worm SW, Sabin C, Weber R, et al. Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) study. J Infect Dis. 2010;201:318–333. doi: 10.1086/649897. [DOI] [PubMed] [Google Scholar]
- 14.Young J, Xiao Y, Moodie EE, et al. Effect of cumulating exposure to abacavir on the risk of cardiovascular disease events in patients from the Swiss HIV cohort study. J Acquir Immune Defic Syndr. 2015;69:413–421. doi: 10.1097/QAI.0000000000000662. [DOI] [PubMed] [Google Scholar]
- 15.Baril JG, Angel JB, Gill MJ, Gathe J, Cahn P, van Wyk J, et al. Dual therapy treatment strategies for the Management of Patients Infected with HIV: a systematic review of current evidence in ARV-naive or ARV-experienced, Virologically suppressed patients. PLoS One. 2016;11(2):e0148231. doi: 10.1371/journal.pone.0148231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Achhra AC, Mwasakifwa G, Amin J, Boyd MA. Efficacy and safety of contemporary dual-drug antiretroviral regimens as first-line treatment or as a simplification strategy: a systematic review and meta-analysis. Lancet HIV. 2016;3:e351–e360. doi: 10.1016/S2352-3018(16)30015-7. [DOI] [PubMed] [Google Scholar]
- 17.Orkin C, Llibre JM, Gallien S, Antinori A, Behrens G, Carr A. Nucleoside reverse transcriptase inhibitor-reducing strategies in HIV treatment: assessing the evidence. HIV Med. 2018;19(1):18-32. [DOI] [PubMed]
- 18.Else LJ, Taylor S, Back DJ, Khoo SH. Pharmacokinetics of antiretroviral drugs in anatomical sanctuary sites: the male and female genital tract. Antivir Ther. 2011;16:1149–1167. doi: 10.3851/IMP1919. [DOI] [PubMed] [Google Scholar]
- 19.Achhra AC, Boyd MA. Antiretroviral regimens sparing agents from the nucleoside(tide) reverse transcriptase inhibitor class: a review of the recent literature. AIDS Res Ther. 2013;10:33. doi: 10.1186/1742-6405-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torti C, Raffetti E, Donato F, Castelli F, Maggiolo F, Angarano G, Mazzotta F, Gori A, Sighinolfi L, Pan A, Cauda R, Scalzini A, Quiros-Roldan E, Nasta P, Gregis G, Benatti S, Digiambenedetto S, Ladisa N, Giralda M, Saracino A, Castelnuovo F, Di Pietro M, Lo Caputo S, Lapadula G, Costarelli S, Lorenzotti S, Mazzini N, Paraninfo G, Casari S, Focà E, Pezzoli C, Fabbiani M, Monno L, Pierotti P, Ble C, Leone S, Postorino MC, Fornabaio C, Zacchi F, Zoncada A, Carosi G. Cohort Profile: Standardized Management of Antiretroviral Therapy Cohort (MASTER cohort) Int J Epidemiol. 2017;46(2):e12. doi: 10.1093/ije/dyv192. [DOI] [PubMed] [Google Scholar]
- 21.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 22.Delaney JA, Suissa S. The case-crossover study design in pharmacoepidemiology. Stat Methods Med Res. 2009;18:53–65. doi: 10.1177/0962280208092346. [DOI] [PubMed] [Google Scholar]
- 23.Gallant JE, Daar ES, Raffi F, Brinson C, Ruane P, DeJesus E, Johnson M, Clumeck N, Osiyemi O, Ward D, Morales-Ramirez J, Yan M, Abram ME, Plummer A, Cheng AK, Rhee MS. Efficacy and safety of tenofovir alafenamide versus tenofovir disoproxil fumarate given as fixed-dose combinations containing emtricitabine as backbones for treatment of HIV-1 infection in virologically suppressed adults: a randomised, double-blind, active-controlled phase 3 trial. Lancet HIV. 2016;3(4):e158–e165. doi: 10.1016/S2352-3018(16)00024-2. [DOI] [PubMed] [Google Scholar]
- 24.Nozza S, Malagoli A, Maia L, Calcagno A, Focà E, De Socio G, Piconi S, Orofino G, Cattelan AM, Celesia BM, Gervasi E, Guaraldi G, GEPPO Study Group. Antiretroviral therapy in geriatric HIV patients: the GEPPO cohort study. J Antimicrob Chemother. 2017; 10.1093/jac/dkx169. [Epub ahead of print]. [DOI] [PubMed]
- 25.Jabłonowska E, Pulik P, Kalinowska A, Gąsiorowski J, Parczewski M, Bociąga-Jasik M, Pulik Ł, Siwak E, Wójcik K. Efficacy and safety of nucleoside-sparing regimen based on raltegravir and ritonavir-boosted darunavir in HIV-1-infected treatment-experienced patients. J Med Virol. 2017; 10.1002/jmv.24826. [Epub ahead of print]. [DOI] [PubMed]
- 26.Bonjoch A, Echeverría P, Perez-Alvarez N, Puig J, Estany C, Clotet B, Negredo E. High rate of reversibility of renal damage in a cohort of HIV-infected patients receiving tenofovir-containing antiretroviral therapy. Antivir Res. 2012;96:65–69. doi: 10.1016/j.antiviral.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Dubé MP, Cadden JJ. Lipid metabolism in treated HIV infection. Best Pract Res Clin Endocrinol Metab. 2011;25:429–442. doi: 10.1016/j.beem.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 28.Kurita T, Kitaichi T, Nagao T, Miura T, Kitazono Y. Safety analysis of Epzicom® (lamivudine/abacavir sulfate) in post-marketing surveillance in Japan. Pharmacoepidemiol Drug Saf. 2014;23(4):372–381. doi: 10.1002/pds.3588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Giambenedetto S, Fabbiani M, Quiros Roldan E, Latini A, D’Ettorre G, Antinori A, Castagna A, Orofino G, Francisci D, Chinello P, Madeddu G, Grima P, Rusconi S, Di Pietro M, Monsi A, Ciccarelli N, Borghetti A, Focà E, Colafigli M, De Luca A, Cauda R on behalf of the ATLAS-M Study Group. Treatment simplification to atazanavir/ritonavir + lamivudine versus mainteinance of atazanavir/ritonavir + two NRTIs in virologically suppressed HIV-1 infected patients: 48 week results from a randomized trial (ATLAS-M). J Antimicrob Chemoter 2017; 72: 1163–1171. [DOI] [PubMed]
- 30.Fabbiani M, Di Giambenedetto S, Poli A, Borghetti A, Castagna A, Mondi A, Galizzi N, Maillard M, Gori A, Cauda R, De Luca A, Gianotti N. Simplification to a dual regimen with darunavir/ritonavir plus lamivudine or emtricitabine in virologically-suppressed HIV-infected patients. J Infect. 2016;73(6):619–623. doi: 10.1016/j.jinf.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 31.Calza L, Magistrelli E, Danese I, Colangeli V, Borderi M, Bon I, Re MC, Mancini R, Conti M, Motta R, Viale P. Changes in serum markers of inflammation and endothelial activation in HIV-infected antiretroviral naive patients starting a treatment with Abacavir-lamivudine or Tenofovir-Emtricitabine plus Efavirenz. Curr HIV Res. 2016;14(1):61–70. doi: 10.2174/1570162X1401151102143222. [DOI] [PubMed] [Google Scholar]
- 32.Hileman CO, Funderburg NT. Inflammation, immune activation, and antiretroviral therapy in HIV. Curr HIV/AIDS Rep. 2017;14(3):93–100. doi: 10.1007/s11904-017-0356-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martinez E, D’Albuquerque PM, Llibre JM, Gutierrez F, Podzamczer D, Antela A, et al. Changes in cardiovascular biomarkers in HIV-infected patients switching from ritonavir-boosted protease inhibitors to raltegravir. AIDS. 2012;26(18):2315–2326. doi: 10.1097/QAD.0b013e328359f29c. [DOI] [PubMed] [Google Scholar]
- 34.McComsey GA, Kitch D, Daar ES, Tierney C, Jahed NC, Melbourne K, Ha B, Brown TT, Bloom A, Fedarko N, Sax PE. Inflammation markers after randomization to abacavir/lamivudine or tenofovir/emtricitabine with efavirenz or atazanavir/ritonavir. AIDS. 2012;26(11):1371–1385. doi: 10.1097/QAD.0b013e328354f4fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gandhi RT, McMahon DK, Bosch RJ, Lalama CM, Cyktor JC, Macatangay BJ, Rinaldo CR, Riddler SA, Hogg E, Godfrey C, Collier AC, Eron JJ, Mellors JW, ACTG A5321 Team Levels of HIV-1 persistence on antiretroviral therapy are not associated with markers of inflammation or activation. PLoS Pathog. 2017;13(4):e1006285. doi: 10.1371/journal.ppat.1006285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hileman CO, Kinley B, Scharen-Guivel V, Melbourne K, Szwarcberg J, Robinson J, Lederman MM, Mccomsey GA. Differential reduction in monocyte activation and vascular inflammation with integrase inhibitor-based initial antiretroviral therapy among HIV-infected individuals. J Infect Dis. 2015;212(3):345–354. doi: 10.1093/infdis/jiv004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelesidis T, Tran TT, Stein JH, Brown TT, Moser C, Ribaudo HJ, et al. Changes in inflammation and immune activation with atazanavir-, raltegravir-, darunavir-based initial antiviral therapy: ACTG 5260s. Clin Infect Dis. 2015;61(4):651–660. doi: 10.1093/cid/civ327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Funderburg NT, McComsey GA, Kulkarni M, Bannerman T, Mantini J, Thornton B, Liu HC, Zhang Y, Song Q, Fang L, Dinoso J, Cheng A, McCallister S, Fordyce MW, Das M. Equivalent decline in inflammation markers with Tenofovir Disoproxil fumarate vs. Tenofovir Alafenamide. EBioMedicine. 2016;13:321–327. doi: 10.1016/j.ebiom.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McComsey GA, et al. Associations of inflammatory markers with AIDS and non-AIDS clinical events after initiation of antiretroviral therapy: AIDS clinical trials group A5224s, a substudy of ACTG A5202. J Acquir Immune Defic Syndr. 2014;65(2):167–174. doi: 10.1097/01.qai.0000437171.00504.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.French MA, Cozzi-Lepri A, Arduino RC, Johnson M, Achhra AC, Landay A, et al. Plasma levels of cytokines and chemokines and the risk of mortality in HIV-infected individuals: a case-control analysis nested ina large clinical trial. AIDS. 2015;29(7):847–851. doi: 10.1097/QAD.0000000000000618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Serrano-Villar S, Sainz T, Lee SA, Hunt PW, Sinclair E, Shacklett BL, et al. HIV-infected individuals with low CD4/CD8 ratio despite effective antiretroviral therapy exhibit altered T cell subsets, heightened CD8+ T cell activation, and increased risk of non-AIDS morbidity and mortality. PLoS Pathog. 2014;10:e1004078. doi: 10.1371/journal.ppat.1004078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leon A, Leal L, Torres B, Lucero C, Inciarte A, Arnedo M, et al. Association of microbial translocation biomarkers with clinical outcome in controllers HIV-infected patients. AIDS. 2015;29(6):675–681. doi: 10.1097/QAD.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 43.Krantz EM, Hullsiek KH, Okulicz JF, Weintrob AC, Agan BK, Crum-Cianflone NF, et al. Elevated CD8 counts during HAART are associated with HIV virologic treatment failure. J Acquir Immune Defic Syndr. 2011;57:396–403. doi: 10.1097/QAI.0b013e318221c62a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lu W, Mehraj V, Vyboh K, Cao W, Li T, Routy J-P. CD4:CD8 ratio as a frontier marker for clinical outcome, immune dysfunction and viral reservoir size in virologically suppressed HIV-positive patients. J Int AIDS Soc. 2015;18:20052. doi: 10.7448/IAS.18.1.20052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Helleberg M, Kronborg G, Ullum H, Ryder LP, Obel N, Gerstoft J. Course and clinical significance of CD8+ T-cell counts in a large cohort of HIV-infected individuals. J Infect Dis. 2015;211(11):1726–1734. doi: 10.1093/infdis/jiu669. [DOI] [PubMed] [Google Scholar]
- 46.C. Mussini, P. Lorenzini, A. Cozzi-Lepri, G. Marchetti, S. Rusconi, A. Gori, S. Nozza, A. Antinori, A. d’Arminio Monforte, for the Icona Foundation Study Group CD4/CD8 ratio in patients who switch cART therapy: triple drug regimen could be better than mono/dual? 9th IAS Conference on HIV Science (IAS 2017), Abstract n° MOPEB0323. Abstract retrieved from http://www.ias2017.org/Portals/1/Files/IAS2017_LO.compressed.pdf?ver=2017-07-27-211231-197. Accessed 26 Oct 2017.
- 47.Huang Y, Hoque MT, Jenabian MA, Vyboh K, Whyte SK, Sheehan NL, Brassard P, Bélanger M, Chomont N, Fletcher CV, Routy JP, Bendayan R. Antiretroviral drug transporters and metabolic enzymes in human testicular tissue: potential contribution to HIV-1 sanctuary site. J Antimicrob Chemother. 2016;71(7):1954–1965. doi: 10.1093/jac/dkw046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martinez-Picado J, Deeks SG. Persistent HIV-1 replication during antiretroviral therapy. Curr Opin HIV AIDS. 2016;11(4):417–423. doi: 10.1097/COH.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lombardi F, Belmonti S, Quiros-Roldan E, Latini A, Castagna A, D'Ettorre G, Gagliardini R, Fabbiani M, Cauda R, De Luca A, Di Giambenedetto S, AtLaS-M Study Group. Evolution of blood-associated HIV-1 DNA levels after 48 weeks of switching to atazanavir/ritonavir+lamivudine dual therapy versus continuing triple therapy in the randomized AtLaS-M trial. J Antimicrob Chemother. 2017; 10.1093/jac/dkx068. [Epub ahead of print]. [DOI] [PubMed]
- 50.Azab B, Camacho-Rivera M, Taioli E. Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLoS One. 2014;9(11):e112361. doi: 10.1371/journal.pone.0112361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Acar G, Kalkan ME, Avci A, Alizade E, Tabakci MM, Toprak C, et al. The relation of platelet-lymphocyte ratio and coronary collateral circulation in patients with stable angina pectoris and chronic total occlusion. Clin Appl Thromb Hemost. 2015;21:462–468. doi: 10.1177/1076029613508599. [DOI] [PubMed] [Google Scholar]
- 52.Raffetti E, Donato F, Casari S, Castelnuovo F, Sighinolfi L, Bandera A, Maggiolo F, Ladisa N, di Pietro M, Fornabaio C, Digiambenedetto S, Quiros-Roldan E. Systemic inflammation-based scores and mortality for all causes in HIV-infected patients: a MASTER cohort study. BMC Infect Dis. 2017;17(1):193. doi: 10.1186/s12879-017-2280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Quiros-Roldan E, Raffetti E, Donato F, Magoni M, Pezzoli C, Ferraresi A, Brianese N, Castelnuovo F, Focà E, Castelli F. Neutrophil to Lymphocyte Ratio and Cardiovascular Disease Incidence in HIV-Infected Patients: A Population-Based Cohort Study. PLoS One. 2016;11(5):e0154900. doi: 10.1371/journal.pone.0154900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Raffetti E, Donato F, Castelli F, Maggiolo F, Carosi G, Quiros-Roldan E. The predictive role of NLR and PLR for solid non-AIDS defining cancer incidence in HIV-infected subjects: a MASTER cohort study. Infect Agent Cancer. 2015;10(34) 10.1186/s13027-015-0032-y. ECollection 2015. [DOI] [PMC free article] [PubMed]
- 55.Raffetti E, Donato F, Pezzoli C, Digiambenedetto S, Bandera A, Di Pietro M, Di Filippo E, Maggiolo F, Sighinolfi L, Fornabaio C, Castelnuovo F, Ladisa N, Castelli F, Quiros Roldan E. Systemic Inflammation-Based Biomarkers and Survival in HIV-Positive Subject With Solid Cancer in an Italian Multicenter Study. J Acquir Immune Defic Syndr. 2015;69(5):585–592. doi: 10.1097/QAI.0000000000000682. [DOI] [PubMed] [Google Scholar]
- 56.Raffetti E, Donato F, Castelnuovo F, Ladisa N, Paraninfo G, Di Filippo E, Segala D, Cologni G, Bandera A, Zacchi F, Digiambenedetto S, Di Pietro M, Castelli F, Quiros-Roldan E, Cohort MASTER. The prognostic role of systemic inflammatory markers on HIV-infected patients with non-Hodgkin lymphoma, a multicenter cohort study. J Transl Med. 2015;13:89. doi: 10.1186/s12967-015-0446-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gupta SK, Kitch D, Tierney C, Melbourne K, Ha B, McComsey GA. Markers of renal disease and function are associated with systemic inflammation in HIV infection. HIV Med. 2015;16(10):591–598. doi: 10.1111/hiv.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Manion M, Hullsiek KH, Wilson EMP, Rhame F, Kojic E, Gibson D, Hammer J, Patel P, Brooks JT, Baker JV, Sereti I. Study to understand the natural history of HIV/AIDS in the era of effective antiretroviral therapy (the ‘SUN study’) investigators. Vitamin D deficiency is associated with IL-6 levels and monocyte activation in HIV-infected persons. PLoS One. 2017;12(5):e0175517. doi: 10.1371/journal.pone.0175517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Akbas EM1, Gungor A2, Ozcicek A3, Akbas N4, Askin S4, Polat M5.Vitamin D and inflammation: evaluation with neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. Arch Med Sci 2016;12(4):721–727. 10.5114/aoms.2015.50625. Epub 2016 Jul 1. [DOI] [PMC free article] [PubMed]
- 60.Klassen KM, Kimlin MG, Fairley CK, Emery S, Anderson PH, Ebeling PR, STEAL Study Group Associations between vitamin D metabolites, antiretroviral therapy and bone mineral density in people with HIV. Osteoporos Int. 2016;27(5):1737–1745. doi: 10.1007/s00198-015-3432-3. [DOI] [PubMed] [Google Scholar]
- 61.Turkmen K, Erdur FM, Ozcicek F, et al. Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients. Hemodial Int. 2013;17:391–396. doi: 10.1111/hdi.12040. [DOI] [PubMed] [Google Scholar]
- 62.Ridker PM. From C-reactive protein to Interleukin-6 to Interleukin-1: moving upstream to identify novel targets for Atheroprotection. Circ Res. 2016;118(1):145–156. doi: 10.1161/CIRCRESAHA.115.306656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grebe A, Latz E. Cholesterol crystals and inflammation. Curr Rheumatol Rep. 2013;15:313. doi: 10.1007/s11926-012-0313-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Akboga MK, Canpolat U, Yuksel M, Yayla C, Yilmaz S, Turak O, Ozeke O, Topaloglu S, Aras D. Platelet to lymphocyte ratio as a novel indicator of inflammation is related with the severity of metabolic syndrome: a single center large-scale study. Platelets. 2016;27(2):178–183. doi: 10.3109/09537104.2015.1064518. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The database used and analyzed for the current study is available from our statistician (Dr. Raffetti Elena: elena.raffetti@gmail.com) on reasonable request.