Abstract
Over the last two decades, the understanding of adipose tissue has undergone radical change. The perception has evolved from an inert energy storage tissue to that of an active endocrine organ. Adipose tissue releases a cluster of active molecules named adipokines. The severity of obesity-related diseases does not necessarily correlate with the extent of body fat accumulation but is closely related to body fat distribution, particularly to visceral localization. There is a distinction between the metabolic function of central obesity (visceral abdominal) and peripheral obesity (subcutaneous) in the production of adipokines. Visceral fat accumulation, linked with levels of some adipokines, induces chronic inflammation and metabolic disorders, including glucose intolerance, hyperlipidaemia, and arterial hypertension. Together, these conditions contribute to a diagnosis of metabolic syndrome, directly associated with the onset of cardiovascular disease. If it is well known that adipokines contribute to the inflammatory profile and appetite regulation, this review is novel in synthesising the current state of knowledge of the role of visceral adipose tissue and its secretion of adipokines in cardiovascular risk.
Keywords: Metabolic syndrome, central obesity, adipokines, visceral adipose tissue, cardiovascular disease, appetite, inflammation
Introduction
The high and sustained prevalence of metabolic syndrome (MetS) is among the most significant public health problems of the 21st century.1 MetS prevalence has been exponentially increasing globally for the past two decades,1 and the understanding of adipose tissue has also undergone a dramatic change from an inert energy storage tissue to an active endocrine organ. The severity of obesity-related diseases is not directly linked to the accumulation of total body fat but rather to its distribution, and particularly to visceral localization. In the early 1980s, a distinction between the metabolic function of central obesity (visceral abdominal) and peripheral obesity (subcutaneous) was proposed.2,3 Visceral adipose tissue (VAT) is the adipose tissue that is stored within the abdominal cavity around internal organs (viscera), such as the kidneys and intestines. VAT communicates with other central and peripheral organs by synthesis and secretion of a host of molecules that are generally referred to as adipokines. VAT accumulation, linked with levels of some adipokines, induces chronic inflammation and metabolic disorders, including glucose intolerance,4,5 hyperlipidaemia,6–9 and arterial hypertension.7 Together, these conditions contribute to a diagnosis of MetS, and consequently, VAT accumulation leads to the onset of MetS and is directly linked with cardiovascular disease (CVD) development.10–13 Along with contributing to inflammatory profiles, adipokines are implicated in appetite regulation and therefore, through energy balance, directly contribute to abdominal obesity.8,14,15 The strength of the relationship between VAT and adipokines was so apparent that a “visceral fat syndrome” was regarded as more appropriate than MetS.16 Here, we present a review and synthesis of existing literature regarding the roles of adipokines secreted from VAT and the implications for inflammation and cardiovascular risk.
Definition and importance of VAT
The concept of MetS has evolved through several committees14,15,17,18 but not without a certain amount of disagreement regarding the specific diagnostic criteria linked to MetS. Each iteration of the definition of MetS has essentially described the clustering of multiple metabolic and cardiovascular risk factors.15 The first formalised concept of MetS was proposed by the World Health Organisation in 1999 as a high cardiovascular risk entity, incorporating multiple risk factors for CVD.17 Within this syndrome, the World Health Organisation highlighted the importance of insulin resistance defined as type 2 diabetes, impaired fasting glucose, impaired glucose tolerance, or elevated glucose uptake. Insulin resistance had to be associated with at least two of the following criteria: obesity (body mass index >30 kg/m2 or an estimation of central obesity assessed by waist-to-hip ratio), arterial hypertension, or dyslipidaemia (hypertriglyceridaemia or low high-density lipoprotein [HDL] levels). In 2001, the National Cholesterol Education Program-Adult Treatment Panel then proposed an updated definition of MetS that recommended the estimation of abdominal obesity (via waist circumference instead of body mass index or waist-to-hip ratio) as one of the five factors.18 The other factors included elevated triglycerides, decreased HDL cholesterol, arterial hypertension, and elevated fasting blood glucose levels. The main evolution of this new definition was therefore that insulin resistance ceased being an essential diagnostic factor, and instead, the important role of VAT emerged, estimated via a simple waist circumference measurement. Nevertheless, none of the five factors were essential criteria for diagnosis using the National Cholesterol Education Program-Adult Treatment Panel definition; MetS was diagnosed if any three of the five factors were present. It was not until 2005, and largely due to several publications emerging at the start of the decade that highlighted the importance of VAT, that the definition was updated. In 2005, the International Diabetes Federation reinforced the role of VAT in the definition of MetS: abdominal obesity became an essential factor necessary for diagnosis that needed to be associated with at least two of the other four factors (elevated triglycerides, reduced HDL cholesterol, hypertension, and elevated blood glucose). This definition maintained waist circumference as the preferred measure because of its simplicity.14 The more recent (2009) joint harmonizing statement identified central obesity as one of the cluster of risk factors associated with both CVD and type 2 diabetes.15 Despite ongoing discussion regarding the waist circumference ‘cut-off’ used for defining MetS, a general acceptance was reached concerning the important role of VAT. MetS is defined as a constellation of metabolic anomalies induced by abdominal (visceral) obesity.15
VAT: A metabolically active organ – adipokines
Over the last two decades, the understanding of adipose tissue has undergone radical change. The perception of adipose tissue has evolved from an inert energy storage tissue, primarily storing triglycerides,19 to an active endocrine organ. Historically, it was possible to assign an endocrine function to adipose tissue via the conversion of androgens to oestrogens by aromatase, resulting in a decrease in circulating testosterone levels and, reciprocally, in the production of oestrogens.20 However, this could not be described as an adipokine, because the secretion was not specific to adipose tissue.
Adipose tissue communicates with other organs via the synthesis and secretion of a multitude of molecules typically referred to as adipokines. A growing number of adipokines are known to intervene directly with metabolic homeostasis,21,22 highlighting the central role of adipose tissue in regulating energy homeostasis of the entire body. The primary adipokines secreted by VAT that play a role in inflammation, metabolism, or CVD include: tumour necrosis factor alpha (TNF-α),23 interleukin-6 (IL-6),24 interleukin-1-beta, adiponectin,25 resistin,26 serum amyloid A-3 (SAA3),27 alpha 1-acid glycoprotein, pentraxin-3, interleukin-1 receptor antagonist, macrophage migration inhibitory factor 28, plasminogen activator inhibitor-1 (PAI-1),29 visfatin,30 and vascular endothelial growth factor (VEGF).31 Overviews of all productions/secretions originating from adipose tissue can be found in various recent reviews,32,33 but those not listed above are implicated in the extracellular matrix without a further role yet described in the pathophysiology of metabolic syndrome, inflammation, or CVD. The pathophysiology of metabolic syndrome includes: insulin resistance, dysregulation of appetite and obesity, chronic inflammation, and its final complication, CVD. We therefore want to clarify the role of each adipokine involved in the pathophysiology of metabolic syndrome.
VAT, insulin resistance, and adipokines
Individuals with obesity characteristically have an imbalance in their adipokine profile, increasing their potential to develop metabolic disturbances (MetS) and more specifically altered insulin sensitivity.34 The key adipokines involved in insulin resistance are resistin, adiponectin, TNF-α, IL-6, visfatin, SAA3, and PAI-1.
Resistin derives its name from insulin resistance and the reactive hyperinsulinaemia it induces by fixing itself to insulin receptors on adipocytes, liver, and muscles.35 Resistin levels increase in the presence of obesity and may play a causal role in type 2 diabetes development.26
Adiponectin is only secreted by adipose tissue.25,36 Contrary to other adipokines, concentrations of adiponectin are reduced in obese individuals,37 potentially due to glucocorticoids and TNF-α.38 Augmentation of adiposity engenders a retro-inhibition of adiponectin production.37 Adiponectin synthesis is regulated by insulin and insulin-like growth factor-1, leading to an increased concentration of this adipokine.38 Adiponectin plays an anti-diabetic role within the liver and skeletal muscles by increasing insulin sensitivity at these sites. It acts by raising cytoplasmic GLUT4 transporters towards the plasma membrane, therefore facilitating glucose uptake by the tissues. Weight loss-derived reductions in VAT also increase adiponectin concentrations, which may further increase insulin sensitivity,39,40 despite the weight loss-related lower insulin production. Hence, elevated levels of adiponectin may decrease the risk of type 2 diabetes.41
Insulin resistance is characterised by increased concentrations of free fatty acids in the plasma and muscles, which contribute to impaired insulin signal transduction. Adiponectin may enable better fatty acid oxidation, as well as help reduce muscle and liver triglycerides, contributing to its anti-diabetic action.
The secretion of TNF-α by adipose tissue is increased in overweight individuals23 and is correlated with the percentage of adipose tissue and the severity of insulin resistance.42 TNF-α acts locally through paracrine mechanisms, inducing adipocyte insulin resistance by deactivating the insulin receptor as well as its substrate (IRS-1).43 The same mechanism is apparent in skeletal muscle, because TNF-α is also produced by adipose tissue macrophages situated between myocytes.24 However, obese mice with a genetic deletion of the TNF-α code or its receptors experienced only minor protective effects from weight gain, hyperglycaemia, or insulin resistance.44,45 This may indicate that TNF-α has only a limited role in the pathogenesis of insulin resistance.
Within the adipose tissue, IL-6 is secreted by both the adipocytes and the macrophages.24 IL-6 is an endocrine cytokine acting distally from the secretion site. Its concentrations correlate well with VAT46 and hepatic insulin resistance.47 Organs primarily targeted by this adipokine are liver, bone marrow, and the vascular endothelium.46 In mouse models, chronic exposure to IL-6 caused hepatic insulin resistance.48,49
Visfatin is primarily produced by VAT. An increase in visfatin levels in obesity is related to the preservation of insulin sensitivity, enhanced glucose uptake by adipocytes, and inhibition of hepatocyte glucose release.50
Although not as well investigated as other adipokines, the SAA3 protein is also produced by VAT, and its plasmatic concentrations have been found to correlate well with insulin resistance.27 Furthermore, PAI-1-deficient mice are reportedly protected from the development of insulin resistance,51 with numerous studies confirming the physiological implications of PAI-1 in insulin resistance.52
VAT, energy balance, appetite, and adipokines
Individuals with MetS typically have elevated circulating leptin levels. However, these patients appear to resist the hypothalamic action of leptin.53 Leptin is a peptide hormone secreted by adipose tissue. Leptin secretion rates are two to three times higher in subcutaneous than omental fat tissue in both obese and non-obese women.54 This adipokine plays a major role in long-term energy homeostasis. Circulating concentrations of leptin decrease during periods of fasting, triggering different energy-saving adaptive mechanisms. These include increased appetite via stimulation of neuronal hypothalamic pathways,55 decreased production of thyroid hormones,56 inhibition of the reproductive axis,57 and depression of the immune system.58 The energy cost of maintaining optimal efficiency of the immune system is estimated to be approximately 15% of total energy expenditure of the organism59 and may play an integral part in the regulation of energy balance. Leptin resistance impairs the catabolic pathway that normally reduces appetite and increases energy consumption and results in excess weight being maintained. Therefore, leptin resistance is likely to be highly prevalent among individuals with MetS.
Although the central effect of adiponectin on energy homeostasis remains unclear and controversial,60 it is well established that adiponectin regulates energy balance in peripheral tissues through modulation of glucose and fatty acid metabolism.61 In the short term, high doses of adiponectin supplementation may reduce caloric intake in spontaneously hypertensive rats.62 However, it is apparent through animal models that supplementation with adiponectin does not induce long-term caloric restriction.63 Despite this, adiponectin supplementation is protective of body mass gains in rats, even when fed high-fat diets, by decreasing visceral fat accumulation.63
Decreased levels of IL-6 may trigger weight gain.64 It has been found that genetically modified mice without IL-6 develop obesity, which suggests an important role of IL-6 in the regulation of energy balance. Therefore, elevated circulating IL-6 concentrations in individuals with MetS may indicate, as with insulin and leptin, the development of resistance to IL-6.
In contrast to IL-6, PAI-1-deficient mice are protected from the development of obesity, suggesting that PAI-1 is implicated in the regulation of energy balance.51
It has been hypothesised that resistance to visfatin may be important in the regulation of body weight,65 and this is supported by rare polymorphisms of the visfatin gene conferring protection from obesity.66,67 Visfatin could be orexigenic68,69 and promote cell survival during starvation.70 In obesity, visfatin concentrations are increased in blood50 but decreased in cerebrospinal fluid.65 Further studies are needed to clarify visfatin’s role in appetite regulation.71
VAT, low-grade chronic inflammation, and adipokines
Adipokines secreted from VAT can contribute to inflammation by both promoting (pro-inflammatory) and inhibiting (anti-inflammatory) the process.
Resistin is considered an inflammatory marker,72 and its gene expression is regulated by pro-inflammatory agents, such as TNF-α, PAI-1, and IL-6. A probable link exists between blood levels of resistin and obesity as well as a positive association between resistinaemia and PAI-1.72
Adiponectin has anti-atherogenic and anti-inflammatory properties via its effects on TNF-α and C-reactive protein (CRP). Adiponectin either directly or indirectly modulates the inflammatory cascade by modifying the action and production of inflammatory cytokines, thus possibly playing an important role in the pathophysiology of atherosclerosis.25
IL-6 plasma concentration is the most important factor in the mediation of the hepatic response to acute stress (tissue damage, infection, etc.). It acts by coordinating the defence mechanisms of the organism (inflammation) to eliminate damaged cells and pathogenic agents and initiate tissue repair.73 During the inflammatory response, CRP is synthesised by the liver and stimulated by IL-6 to bind to the plasma membrane of damaged cells and activate cascading of the complement, which leads to cellular death.74 Therefore, CRP is a strong marker of metabolic risk. Adipose tissue in an important contributor to a state of chronic systemic inflammation, characteristic of MetS, by secreting large volumes of IL-6 into the plasma, which results in CRP production.74 Systemic inflammation provoked by increased IL-6 concentrations and the subsequent synthesis of CRP may be a side effect of an initially normal physiological response that becomes deleterious with the development of IL-6 resistance.
Visfatin mediates a complex cellular signalling process stimulated by oxidative stress resulting in vascular endothelial inflammation. The exact role of visfatin in inflammation is unclear with increased concentrations associated with an augmentation in both pro- and anti-inflammatory blood cytokines.75
The SAA3 protein is a component of the acute inflammatory phase. However, its role as an independent predictor of MetS is unclear.76
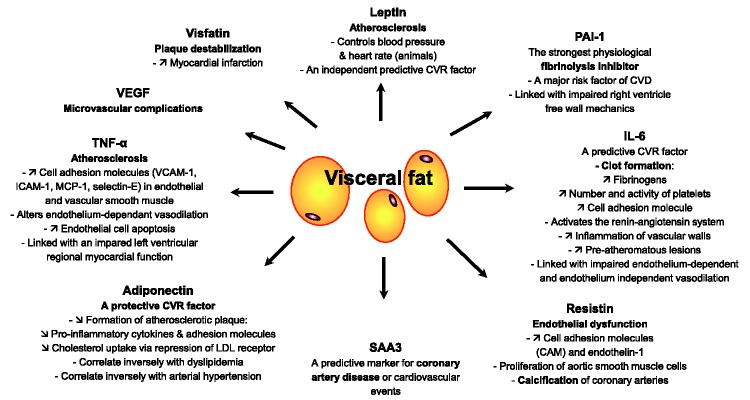
VAT, cardiovascular risk, and adipokines (Figure 1)
Figure 1.
Cardiovascular risk of adipokines.
Deregulation of numerous adipokines has been implicated in obesity, type 2 diabetes, arterial hypertension, CVD, and an increasing list of other pathologies.33 If the increase in circulating concentrations of leptin resulting from an inflammatory response is beneficial in controlling acute infection,77 the opposite is true in the case of chronic inflammation, such as in MetS. Genetically modified obese mice deficient in leptin are protected from atherogenic pathology, despite the accumulation of other cardiovascular risk factors, thus suggesting that leptin may be directly involved in the development of CVD.78 It also appears that leptin may be a key driver of blood pressure and heart rate responses in animals, although these effects have not been replicated in humans to date.79 Additionally, a prospective study in humans revealed that increased circulating leptin concentration is a predictive risk factor for CVD, independent of other factors.80
Resistin is also involved in cardiovascular risk via its role in promoting endothelial dysfunction. It does so by inducing the secretion of cell adhesion molecules (CAM) and endothelin-1 by the endothelial cells81 or through proliferation of aortic smooth muscle cells.82 Calcification of coronary arteries, an index of atherosclerosis, is also associated with increased resistin levels.72 Resistin has a negative association with HDL.72
Plasma concentrations of adiponectin are decreased in obese patients and patients with diabetes, as well as patients with coronary artery disease.83 Adiponectin inhibits the formation of atherosclerotic plaque via two mechanisms.84 First, it inhibits atheromatous formation on the intima by repressing the expression of pro-inflammatory cytokines and adhesion molecules. Second, it inhibits cholesterol uptake via repression of low-density lipoprotein receptor expression.85 Adiponectin has also been shown to correlate inversely with dyslipidaemia and arterial hypertension,85 as well as with other components of MetS.85
TNF-α accelerates atherosclerosis by inducing expression of adhesion molecules (vascular CAM-1, intercellular CAM-1, monocyte chemotactic protein-1, and selectin-E) in the endothelial and vascular smooth muscle cells86 and by altering endothelium-dependant vasodilation87–89 or promoting endothelial cell apoptosis.90,91 TNF-α was also linked with impaired left ventricular regional myocardial function.92,93
IL-6 triggers an increase in fibrinogens and the number and activity of platelets, leading to increased risk of clot formation.94 Additionally, vascular endothelial and smooth muscle cells are also targets of the IL-6 adipokine. IL-6 produces an increase in adhesion molecule expression and activation of the renin-angiotensin system, leading to inflammation of vascular walls and the development of pre-atheromatous lesions.95 IL-6 has been linked with impaired endothelium-dependent and -independent vasodilation89 and with insulin-dependent vasodilation.96 Moreover, IL-6 induces CRP production, which is a predictive risk factor for CVD and evolution towards type 2 diabetes.97,98
The pro-inflammatory and pro-atheromatous SAA3 protein has been identified as a predictive marker for coronary artery disease or cardiovascular events.76
Fibrinolysis is an anti-thrombotic physiological process that dissolves blood clots once they are no longer needed for haemostasis. Augmentation of the strongest physiological fibrinolysis inhibitor, PAI-1, is considered a major risk factor for CVD.99 PAI-1 is secreted by the liver (hepatocytes), vascular vessels (endothelial cells), and adipose tissue.100 An increase in circulating PAI-1 concentrations is frequently observed in abdominal obesity.101 PAI-1 is also increased (mRNA and secretion) in VAT.29 The association between PAI-1, cardiovascular events, and metabolic disorders is well established.52 Moreover, PAI-1 was also linked with impaired right ventricle free wall mechanics.102
VEGF is produced by many types of cells, including fibroblasts, macrophages, neutrophils, endothelial cells, and T cells.103 VEGF is also secreted by the adipose tissue. Although not normalized for adipocyte number, VEGF protein expression and secretion may be fat-deposit dependent and highest in the omental fat deposits.31 VEGF is necessary to initiate the formation of immature vessels and to maintain vessel homeostasis.104 However, elevated circulating VEGF levels are believed to play a role in type 2 diabetes microvascular complications even if the link between VEGF and type 2 diabetes and its complications might be indirect and more complex than expected.105
Visfatin appears to be associated with a greater risk of cardiovascular disease than benefit. While visfatin is positively correlated with HDL cholesterol, it is also expressed by plaque macrophages and has a role in plaque destabilization.75 In addition, elevated plasma visfatin levels increase the risk of myocardial infarction.106
Adipokines in chronic inflammatory diseases and the influence of TNF-blockade on the adipokine profile
Lastly, we want to acknowledge that some chronic inflammatory diseases, such as rheumatoid arthritis, spondyloarthritis, or psoriasis, are associated with the development of MetS and a higher risk of CVD. Rheumatoid arthritis (RA) is the prototype of chronic inflammatory disease associated with metabolic syndrome and accelerated atherosclerosis. In patients with RA undergoing anti-TNF-α therapy because of severe disease refractory to conventional therapy, a positive correlation between body mass index of the patients and serum leptin levels was observed.107 In these patients there was a correlation between leptin levels and VCAM-1.107 This is of potential relevance, because biomarkers of endothelial cell activation were elevated in patients with RA. Furthermore, anti-TNF blockade improved endothelial function in these patients108 and decreased the levels of endothelial cell activation biomarkers.109 Additionally, in patients with RA undergoing anti-TNF-α infliximab therapy because of severe disease, high-grade inflammation was independently and negatively correlated with circulating adiponectin concentrations. In contrast, low adiponectin levels clustered with MetS features, such as dyslipidaemia and high plasma glucose levels, that have been reported to contribute to atherogenesis in RA.110 However, the interaction of high-grade inflammation with low circulating adiponectin concentrations was not mediated by TNF-α in these patients.110 Moreover, in patients with RA undergoing anti-TNF-α therapy, a strong association between serum resistin levels and laboratory markers of inflammation, particularly CRP, was observed.111 A positive association between parameters of disease activity in psoriasis and resistin concentrations was also reported in patients with moderate-to-severe psoriasis.112 Finally, in a study that included patients with RA with severe disease undergoing anti-TNF-α-infliximab therapy, visfatin levels were not associated with inflammation or metabolic syndrome.113 However, in patients with ankylosing spondylitis undergoing anti-TNF-α therapy, visfatin concentration correlated with insulin resistance.114
Summary
This review synthesised the current literature on the role of key adipokines associated with cardiovascular risk in MetS. Since the identification of leptin in 1994, the discovery of additional adipokines has enhanced the understanding of the role of visceral adipose tissue in metabolic and cardiovascular pathology. It has been shown that visceral adipose tissue is a highly active endocrine organ that secretes numerous adipokines that have both pro- and anti-inflammatory properties contributing to inflammation, appetite regulation, insulin resistance, and cardiovascular risk, all implicated in metabolic syndrome.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 2005; 365: 1415–1428. [DOI] [PubMed] [Google Scholar]
- 2.Bjorntorp P. Classification of obese patients and complications related to the distribution of surplus fat. Am. J. Clin. Nutr 1987; 45(5 Suppl): 1120–1125. [DOI] [PubMed] [Google Scholar]
- 3.Kissebah AH, Vydelingum N, Murray R, et al. Relation of body fat distribution to metabolic complications of obesity. J. Clin. Endocrinol. Metab 1982; 54: 254–260. [DOI] [PubMed] [Google Scholar]
- 4.Nagaretani H, Nakamura T, Funahashi T, et al. Visceral fat is a major contributor for multiple risk factor clustering in Japanese men with impaired glucose tolerance. Diabetes Care 2001; 24: 2127–2133. [DOI] [PubMed] [Google Scholar]
- 5.Yamashita S, Nakamura T, Shimomura I, et al. Insulin resistance and body fat distribution. Diabetes Care 1996; 19: 287–291. [DOI] [PubMed] [Google Scholar]
- 6.Fujioka S, Matsuzawa Y, Tokunaga K, et al. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism 1987; 36: 54–59. [DOI] [PubMed] [Google Scholar]
- 7.Kanai H, Matsuzawa Y, Kotani K, et al. Close correlation of intra-abdominal fat accumulation to hypertension in obese women. Hypertension 1990; 16: 484–490. [DOI] [PubMed] [Google Scholar]
- 8.Dutheil F, Lesourd B, Courteix D, et al. Blood lipids and adipokines concentrations during a 6-month nutritional and physical activity intervention for metabolic syndrome treatment. Lipids Health Dis 2010; 9: 148–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dutheil F, Walther G, Chapier R, et al. Atherogenic subfractions of lipoproteins in the treatment of metabolic syndrome by physical activity and diet - the RESOLVE Trial. Lipids Health Dis 2014; 13: 112–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakajima T, Fujioka S, Tokunaga K, et al. Correlation of intraabdominal fat accumulation and left ventricular performance in obesity. Am. J. Cardiol 1989; 64: 369–373. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura T, Tokunaga K, Shimomura I, et al. Contribution of visceral fat accumulation to the development of coronary artery disease in non-obese men. Atherosclerosis 1994; 107: 239–246. [DOI] [PubMed] [Google Scholar]
- 12.Dutheil F, Lac G, Lesourd B, et al. Different modalities of exercise to reduce visceral fat mass and cardiovascular risk in metabolic syndrome: the RESOLVE randomized trial. Int. J. Cardiol 2013; 168: 3634–3642. [DOI] [PubMed] [Google Scholar]
- 13.Boudet G, Walther G, Courteix D, et al. Paradoxical dissociation between heart rate and heart rate variability following different modalities of exercise in individuals with metabolic syndrome: The RESOLVE study. Eur J Prev Cardiol 2017; 24: 281–296. [DOI] [PubMed] [Google Scholar]
- 14.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome–a new worldwide definition. Lancet 2005; 366: 1059–1062. [DOI] [PubMed] [Google Scholar]
- 15.Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 2009; 120: 1640–1645. [DOI] [PubMed] [Google Scholar]
- 16.Matsuzawa Y, Funahashi T, Nakamura T. The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism. J Atheroscler Thromb 2011; 18: 629–639. [DOI] [PubMed] [Google Scholar]
- 17.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med 1998; 15: 539–553. [DOI] [PubMed] [Google Scholar]
- 18.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002; 106: 3143–3421. [PubMed] [Google Scholar]
- 19.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 2004; 89: 2548–2556. [DOI] [PubMed] [Google Scholar]
- 20.Schindler AE, Ebert A, Friedrich E. Conversion of androstenedione to estrone by human tissue. J. Clin. Endocrinol. Metab 1972; 35: 627–630. [DOI] [PubMed] [Google Scholar]
- 21.Hauner H. Secretory factors from human adipose tissue and their functional role. Proc. Nutr. Soc 2005; 64: 163–169. [DOI] [PubMed] [Google Scholar]
- 22.Halberg N, Wernstedt-Asterholm I, Scherer PE. The adipocyte as an endocrine cell. Endocrinol. Metab. Clin. North Am 2008; 37: 753–768, x–xi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hotamisligil GS, Arner P, Caro JF, et al. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J. Clin. Invest 1995; 95: 2409–2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weisberg SP, McCann D, Desai M, et al. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest 2003; 112: 1796–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whitehead JP, Richards AA, Hickman IJ, et al. Adiponectin–a key adipokine in the metabolic syndrome. Diabetes Obes Metab 2006; 8: 264–280. [DOI] [PubMed] [Google Scholar]
- 26.Azuma K, Katsukawa F, Oguchi S, et al. Correlation between serum resistin level and adiposity in obese individuals. Obes. Res 2003; 11: 997–1001. [DOI] [PubMed] [Google Scholar]
- 27.Leinonen E, Hurt-Camejo E, Wiklund O, et al. Insulin resistance and adiposity correlate with acute-phase reaction and soluble cell adhesion molecules in type 2 diabetes. Atherosclerosis 2003; 166: 387–394. [DOI] [PubMed] [Google Scholar]
- 28.Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J. Am. Soc. Nephrol 2004; 15: 2792–2800. [DOI] [PubMed] [Google Scholar]
- 29.Alessi MC, Peiretti F, Morange P, et al. Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease. Diabetes 1997; 46: 860–867. [DOI] [PubMed] [Google Scholar]
- 30.Fukuhara A, Matsuda M, Nishizawa M, et al. Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science 2005; 307: 426–430. [DOI] [PubMed] [Google Scholar]
- 31.Zhang QX, Magovern CJ, Mack CA, et al. Vascular endothelial growth factor is the major angiogenic factor in omentum: mechanism of the omentum-mediated angiogenesis. J. Surg. Res 1997; 67: 147–154. [DOI] [PubMed] [Google Scholar]
- 32.Lafontan M. Historical perspectives in fat cell biology: the fat cell as a model for the investigation of hormonal and metabolic pathways. Am J Physiol Cell Physiol 2012; 302: C327–C359. [DOI] [PubMed] [Google Scholar]
- 33.Deng Y, Scherer PE. Adipokines as novel biomarkers and regulators of the metabolic syndrome. Ann. N. Y. Acad. Sci 2010; 1212: E1–E19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pacholczyk M, Ferenc T, Kowalski J. [The metabolic syndrome. Part II: its mechanisms of development and its complications]. Postepy Hig Med Dosw (Online) 2008; 62: 543–558. [in Polish, English Abstract]. [PubMed] [Google Scholar]
- 35.Steppan CM, Bailey ST, Bhat S, et al. The hormone resistin links obesity to diabetes. Nature 2001; 409: 307–312. [DOI] [PubMed] [Google Scholar]
- 36.Chandran M, Phillips SA, Ciaraldi T, et al. Adiponectin: more than just another fat cell hormone? Diabetes Care 2003; 26: 2442–2450. [DOI] [PubMed] [Google Scholar]
- 37.Lafontan M, Viguerie N. Role of adipokines in the control of energy metabolism: focus on adiponectin. Curr Opin Pharmacol 2006; 6: 580–585. [DOI] [PubMed] [Google Scholar]
- 38.Stefan N, Stumvoll M. Adiponectin–its role in metabolism and beyond. Horm. Metab. Res 2002; 34: 469–474. [DOI] [PubMed] [Google Scholar]
- 39.Trujillo ME, Scherer PE. Adiponectin–journey from an adipocyte secretory protein to biomarker of the metabolic syndrome. J. Intern. Med 2005; 257: 167–175. [DOI] [PubMed] [Google Scholar]
- 40.Pajvani UB, Scherer PE. Adiponectin: systemic contributor to insulin sensitivity. Curr Diab Rep 2003; 3: 207–213. [DOI] [PubMed] [Google Scholar]
- 41.Li S, Shin HJ, Ding EL, et al. Adiponectin levels and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 2009; 302: 179–188. [DOI] [PubMed] [Google Scholar]
- 42.Tsigos C, Kyrou I, Chala E, et al. Circulating tumor necrosis factor alpha concentrations are higher in abdominal versus peripheral obesity. Metabolism 1999; 48: 1332–1335. [DOI] [PubMed] [Google Scholar]
- 43.Hotamisligil GS, Murray DL, Choy LN, et al. Tumor necrosis factor alpha inhibits signaling from the insulin receptor. Proc. Natl. Acad. Sci. U. S. A 1994; 91: 4854–4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Uysal KT, Wiesbrock SM, Marino MW, et al. Protection from obesity-induced insulin resistance in mice lacking TNF-alpha function. Nature 1997; 389: 610–614. [DOI] [PubMed] [Google Scholar]
- 45.Ventre J, Doebber T, Wu M, et al. Targeted disruption of the tumor necrosis factor-alpha gene: metabolic consequences in obese and nonobese mice. Diabetes 1997; 46: 1526–1531. [DOI] [PubMed] [Google Scholar]
- 46.Fried SK, Bunkin DA, Greenberg AS. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: depot difference and regulation by glucocorticoid. J. Clin. Endocrinol. Metab 1998; 83: 847–850. [DOI] [PubMed] [Google Scholar]
- 47.Bastard JP, Jardel C, Bruckert E, et al. Elevated levels of interleukin 6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss. J. Clin. Endocrinol. Metab 2000; 85: 3338–3342. [DOI] [PubMed] [Google Scholar]
- 48.Klover PJ, Zimmers TA, Koniaris LG, et al. Chronic exposure to interleukin-6 causes hepatic insulin resistance in mice. Diabetes 2003; 52: 2784–2789. [DOI] [PubMed] [Google Scholar]
- 49.Kim JH, Kim JE, Liu HY, et al. Regulation of interleukin-6-induced hepatic insulin resistance by mammalian target of rapamycin through the STAT3-SOCS3 pathway. J. Biol. Chem 2008; 283: 708–715. [DOI] [PubMed] [Google Scholar]
- 50.Al-Dokhi LM. Adipokines and etiopathology of metabolic disorders. Saudi Med J 2009; 30: 1123–1132. [PubMed] [Google Scholar]
- 51.Ma LJ, Mao SL, Taylor KL, et al. Prevention of obesity and insulin resistance in mice lacking plasminogen activator inhibitor 1. Diabetes 2004; 53: 336–346. [DOI] [PubMed] [Google Scholar]
- 52.Alessi MC, Juhan-Vague I. PAI-1 and the metabolic syndrome: links, causes, and consequences. Arterioscler. Thromb. Vac. Biol 2006; 26: 2200–2207. [DOI] [PubMed] [Google Scholar]
- 53.Flier JS. Obesity wars: molecular progress confronts an expanding epidemic. Cell 2004; 116: 337–350. [DOI] [PubMed] [Google Scholar]
- 54.Van Harmelen V, Reynisdottir S, Eriksson P, et al. Leptin secretion from subcutaneous and visceral adipose tissue in women. Diabetes 1998; 47: 913–917. [DOI] [PubMed] [Google Scholar]
- 55.Schwartz MW, Woods SC, Porte D, Jr., et al. Central nervous system control of food intake. Nature 2000; 404: 661–671. [DOI] [PubMed] [Google Scholar]
- 56.Legradi G, Emerson CH, Ahima RS, et al. Leptin prevents fasting-induced suppression of prothyrotropin-releasing hormone messenger ribonucleic acid in neurons of the hypothalamic paraventricular nucleus. Endocrinology 1997; 138: 2569–2576. [DOI] [PubMed] [Google Scholar]
- 57.Ahima RS, Prabakaran D, Mantzoros C, et al. Role of leptin in the neuroendocrine response to fasting. Nature 1996; 382: 250–252. [DOI] [PubMed] [Google Scholar]
- 58.Howard JK, Lord GM, Matarese G, et al. Leptin protects mice from starvation-induced lymphoid atrophy and increases thymic cellularity in ob/ob mice. J. Clin. Invest 1999; 104: 1051–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Buttgereit F, Burmester GR, Brand MD. Bioenergetics of immune functions: fundamental and therapeutic aspects. Immunol. Today 2000; 21: 192–199. [DOI] [PubMed] [Google Scholar]
- 60.Thundyil J, Pavlovski D, Sobey CG, et al. Adiponectin receptor signalling in the brain. Br. J. Pharmacol 2012; 165: 313–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dridi S, Taouis M. Adiponectin and energy homeostasis: consensus and controversy. J Nutr Biochem 2009; 20: 831–839. [DOI] [PubMed] [Google Scholar]
- 62.Bassi M, do Carmo JM, Hall JE, et al. Chronic effects of centrally administered adiponectin on appetite, metabolism and blood pressure regulation in normotensive and hypertensive rats. Peptides 2012; 37: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shklyaev S, Aslanidi G, Tennant M, et al. Sustained peripheral expression of transgene adiponectin offsets the development of diet-induced obesity in rats. Proc. Natl. Acad. Sci. U. S. A 2003; 100: 14217–14222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wallenius V, Wallenius K, Ahren B, et al. Interleukin-6-deficient mice develop mature-onset obesity. Nat. Med 2002; 8: 75–79. [DOI] [PubMed] [Google Scholar]
- 65.Hallschmid M, Randeva H, Tan BK, et al. Relationship between cerebrospinal fluid visfatin (PBEF/Nampt) levels and adiposity in humans. Diabetes 2009; 58: 637–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bottcher Y, Teupser D, Enigk B, et al. Genetic variation in the visfatin gene (PBEF1) and its relation to glucose metabolism and fat-depot-specific messenger ribonucleic acid expression in humans. J. Clin. Endocrinol. Metab 2006; 91: 2725–2731. [DOI] [PubMed] [Google Scholar]
- 67.Blakemore AI, Meyre D, Delplanque J, et al. A rare variant in the visfatin gene (NAMPT/PBEF1) is associated with protection from obesity. Obesity (Silver Spring) 2009; 17: 1549–1553. [DOI] [PubMed] [Google Scholar]
- 68.Cline MA, Nandar W, Prall BC, et al. Central visfatin causes orexigenic effects in chicks. Behav. Brain Res 2008; 186: 293–297. [DOI] [PubMed] [Google Scholar]
- 69.Sun G, Bishop J, Khalili S, et al. Serum visfatin concentrations are positively correlated with serum triacylglycerols and down-regulated by overfeeding in healthy young men. Am. J. Clin. Nutr 2007; 85: 399–404. [DOI] [PubMed] [Google Scholar]
- 70.Yang H, Yang T, Baur JA, et al. Nutrient-sensitive mitochondrial NAD+ levels dictate cell survival. Cell 2007; 130: 1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Carrero JJ, Witasp A, Stenvinkel P, et al. Visfatin is increased in chronic kidney disease patients with poor appetite and correlates negatively with fasting serum amino acids and triglyceride levels. Nephrol. Dial. Transplant 2010; 25: 901–906. [DOI] [PubMed] [Google Scholar]
- 72.Reilly MP, Lehrke M, Wolfe ML, et al. Resistin is an inflammatory marker of atherosclerosis in humans. Circulation 2005; 111: 932–939. [DOI] [PubMed] [Google Scholar]
- 73.Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochem. J 1990; 265: 621–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J. Clin. Invest 2003; 111: 1805–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mattu HS, Randeva HS. Role of adipokines in cardiovascular disease. J. Endocrinol 2013; 216: T17–36. [DOI] [PubMed] [Google Scholar]
- 76.Johnson BD, Kip KE, Marroquin OC, et al. Serum amyloid A as a predictor of coronary artery disease and cardiovascular outcome in women: the national heart, lung, and blood institute-sponsored women’s ischemia syndrome evaluation (WISE). Circulation 2004; 109: 726–732. [DOI] [PubMed] [Google Scholar]
- 77.Bornstein SR, Licinio J, Tauchnitz R, et al. Plasma leptin levels are increased in survivors of acute sepsis: associated loss of diurnal rhythm, in cortisol and leptin secretion. J. Clin. Endocrinol. Metab 1998; 83: 280–283. [DOI] [PubMed] [Google Scholar]
- 78.Hasty AH, Shimano H, Osuga J, et al. Severe hypercholesterolemia, hypertriglyceridemia, and atherosclerosis in mice lacking both leptin and the low density lipoprotein receptor. J. Biol. Chem 2001; 276: 37402–37408. [DOI] [PubMed] [Google Scholar]
- 79.Simonds SE, Pryor JT, Ravussin E, et al. Leptin mediates the increase in blood pressure associated with obesity. Cell 2014; 159: 1404–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wallace AM, McMahon AD, Packard CJ, et al. Plasma leptin and the risk of cardiovascular disease in the west of Scotland coronary prevention study (WOSCOPS). Circulation 2001; 104: 3052–3056. [DOI] [PubMed] [Google Scholar]
- 81.Verma S, Li SH, Wang CH, et al. Resistin promotes endothelial cell activation: further evidence of adipokine-endothelial interaction. Circulation 2003; 108: 736–740. [DOI] [PubMed] [Google Scholar]
- 82.Calabro P, Samudio I, Willerson JT, et al. Resistin promotes smooth muscle cell proliferation through activation of extracellular signal-regulated kinase 1/2 and phosphatidylinositol 3-kinase pathways. Circulation 2004; 110: 3335–3340. [DOI] [PubMed] [Google Scholar]
- 83.Matsuzawa Y. The metabolic syndrome and adipocytokines. FEBS Lett 2006; 580: 2917–2921. [DOI] [PubMed] [Google Scholar]
- 84.Kadowaki T, Yamauchi T. Adiponectin and adiponectin receptors. Endocr. Rev 2005; 26: 439–451. [DOI] [PubMed] [Google Scholar]
- 85.Hopkins TA, Ouchi N, Shibata R, et al. Adiponectin actions in the cardiovascular system. Cardiovasc. Res 2007; 74: 11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ouchi N, Kihara S, Arita Y, et al. Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein adiponectin. Circulation 1999; 100: 2473–2476. [DOI] [PubMed] [Google Scholar]
- 87.Bhagat K, Vallance P. Inflammatory cytokines impair endothelium-dependent dilatation in human veins in vivo. Circulation 1997; 96: 3042–3047. [DOI] [PubMed] [Google Scholar]
- 88.Wang P, Ba ZF, Chaudry IH. Administration of tumor necrosis factor-alpha in vivo depresses endothelium-dependent relaxation. Am. J. Physiol 1994; 266(6 Pt 2): H2535–H2541. [DOI] [PubMed] [Google Scholar]
- 89.Walther G, Obert P, Dutheil F, et al. Metabolic syndrome individuals with and without type 2 diabetes mellitus present generalized vascular dysfunction: cross-sectional study. Arterioscler. Thromb. Vac. Biol 2015; 35: 1022–1029. [DOI] [PubMed] [Google Scholar]
- 90.Choy JC, Granville DJ, Hunt DW, et al. Endothelial cell apoptosis: biochemical characteristics and potential implications for atherosclerosis. J. Mol. Cell. Cardiol 2001; 33: 1673–1690. [DOI] [PubMed] [Google Scholar]
- 91.Hermann C, Assmus B, Urbich C, et al. Insulin-mediated stimulation of protein kinase Akt: A potent survival signaling cascade for endothelial cells. Arterioscler. Thromb. Vac. Biol 2000; 20: 402–409. [DOI] [PubMed] [Google Scholar]
- 92.Serrano-Ferrer J, Crendal E, Walther G, et al. Effects of lifestyle intervention on left ventricular regional myocardial function in metabolic syndrome patients from the RESOLVE randomized trial. Metabolism 2016; 65: 1350–1360. [DOI] [PubMed] [Google Scholar]
- 93.Crendal E, Walther G, Vinet A, et al. Myocardial deformation and twist mechanics in adults with metabolic syndrome: Impact of cumulative metabolic burden. Obesity (Silver Spring) 2013; 21: E679–E686. [DOI] [PubMed] [Google Scholar]
- 94.Burstein SA, Peng J, Friese P, et al. Cytokine-induced alteration of platelet and hemostatic function. Stem Cells 1996; 14(Suppl 1): 154–162. [DOI] [PubMed] [Google Scholar]
- 95.Wassmann S, Stumpf M, Strehlow K, et al. Interleukin-6 induces oxidative stress and endothelial dysfunction by overexpression of the angiotensin II type 1 receptor. Circ. Res 2004; 94: 534–541. [DOI] [PubMed] [Google Scholar]
- 96.Vinet A, Obert P, Dutheil F, et al. Impact of a lifestyle program on vascular insulin resistance in metabolic syndrome subjects: the RESOLVE study. J. Clin. Endocrinol. Metab 2015; 100: 442–450. [DOI] [PubMed] [Google Scholar]
- 97.Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N. Engl. J. Med 2000; 342: 836–843. [DOI] [PubMed] [Google Scholar]
- 98.Ridker PM, Morrow DA. C-reactive protein, inflammation, and coronary risk. Cardiol. Clin 2003; 21: 315–325. [DOI] [PubMed] [Google Scholar]
- 99.Juhan-Vague I, Alessi MC, Vague P. Increased plasma plasminogen activator inhibitor 1 levels. A possible link between insulin resistance and atherothrombosis. Diabetologia 1991; 34: 457–462. [DOI] [PubMed] [Google Scholar]
- 100.Fain JN, Madan AK, Hiler ML, et al. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology 2004; 145: 2273–2282. [DOI] [PubMed] [Google Scholar]
- 101.Bastard JP, Pieroni L, Hainque B. Relationship between plasma plasminogen activator inhibitor 1 and insulin resistance. Diabetes. Metab. Res. Rev 2000; 16: 192–201. [DOI] [PubMed] [Google Scholar]
- 102.Serrano-Ferrer J, Walther G, Crendal E, et al. Right ventricle free wall mechanics in metabolic syndrome without type-2 diabetes: effects of a 3-month lifestyle intervention program. Cardiovasc Diabetol 2014; 13: 116–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kiriakidis S, Andreakos E, Monaco C, et al. VEGF expression in human macrophages is NF-kappaB-dependent: studies using adenoviruses expressing the endogenous NF-kappaB inhibitor IkappaBalpha and a kinase-defective form of the IkappaB kinase 2. J. Cell Sci 2003; 116(Pt 4): 665–674. [DOI] [PubMed] [Google Scholar]
- 104.Hausman GJ, Richardson RL. Adipose tissue angiogenesis. J. Anim. Sci 2004; 82: 925–934. [DOI] [PubMed] [Google Scholar]
- 105.Bonnefond A, Saulnier PJ, Stathopoulou MG, et al. What is the contribution of two genetic variants regulating VEGF levels to type 2 diabetes risk and to microvascular complications? PLoS One 2013; 8: e55921–e55921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yang Y, Li Z, Tao HF, et al. An elevated plasma level of visfatin increases the risk of myocardial infarction. Genet Mol Res 2014; 13: 8586–8595. [DOI] [PubMed] [Google Scholar]
- 107.Gonzalez-Gay MA, Garcia-Unzueta MT, Berja A, et al. Anti-TNF-alpha therapy does not modulate leptin in patients with severe rheumatoid arthritis. Clin. Exp. Rheumatol 2009; 27: 222–228. [PubMed] [Google Scholar]
- 108.Gonzalez-Juanatey C, Llorca J, Sanchez-Andrade A, et al. Short-term adalimumab therapy improves endo-thelial function in patients with rheumatoid arthritis refractory to infliximab. Clin. Exp. Rheumatol 2006; 24: 309–312. [PubMed] [Google Scholar]
- 109.Gonzalez-Gay MA, Garcia-Unzueta MT, De Matias JM, et al. Influence of anti-TNF-alpha infliximab therapy on adhesion molecules associated with atherogenesis in patients with rheumatoid arthritis. Clin. Exp. Rheumatol 2006; 24: 373–379. [PubMed] [Google Scholar]
- 110.Gonzalez-Gay MA, Llorca J, Garcia-Unzueta MT, et al. High-grade inflammation, circulating adiponectin concentrations and cardiovascular risk factors in severe rheumatoid arthritis. Clin. Exp. Rheumatol 2008; 26: 596–603. [PubMed] [Google Scholar]
- 111.Gonzalez-Gay MA, Garcia-Unzueta MT, Gonzalez-Juanatey C, et al. Anti-TNF-alpha therapy modulates resistin in patients with rheumatoid arthritis. Clin. Exp. Rheumatol 2008; 26: 311–316. [PubMed] [Google Scholar]
- 112.Pina T, Genre F, Lopez-Mejias R, et al. Relationship of leptin with adiposity and inflammation and resistin with disease severity in psoriatic patients undergoing anti-TNF-alpha therapy. J. Eur. Acad. Dermatol. Venereol 2015; 29: 1995–2001. [DOI] [PubMed] [Google Scholar]
- 113.Gonzalez-Gay MA, Vazquez-Rodriguez TR, Garcia-Unzueta MT, et al. Visfatin is not associated with inflammation or metabolic syndrome in patients with severe rheumatoid arthritis undergoing anti-TNF-alpha therapy. Clin. Exp. Rheumatol 2010; 28: 56–62. [PubMed] [Google Scholar]
- 114.Miranda-Filloy JA, Lopez-Mejias R, Genre F, et al. Leptin and visfatin serum levels in non-diabetic ankylosing spondylitis patients undergoing TNF-alpha antagonist therapy. Clin. Exp. Rheumatol 2013; 31: 538–545. [PubMed] [Google Scholar]