Abstract
Objectives:
Patient-centered medical home transformation initiatives for enhancing team-based, patient-centered primary care are widespread in the United States. However, there remain large gaps in our understanding of these efforts. This article reports findings from a contextual, whole system evaluation study of a transformation intervention at eight primary care teaching practice sites in Rhode Island. It provides a picture of system changes from the perspective of providers, staff, and patients in these practices.
Methods:
Quantitative/qualitative evaluation methods include patient, provider, and staff surveys and qualitative interviews; practice observations; and focus groups with the intervention facilitation team.
Results:
Patient satisfaction in the practices was high. Patients could describe observable elements of patient-centered medical home functioning, but they lacked explicit awareness of the patient-centered medical home model, and their activation decreased over time. Providers’ and staff’s emotional exhaustion and depersonalization increased slightly over the course of the intervention from baseline to follow-up, and personal accomplishment decreased slightly. Providers and staff expressed appreciation for the patient-centered medical home as an ideal model, variously implemented some important patient-centered medical home components, increased their understanding of patient-centered medical home as more than specific isolated parts, and recognized their evolving work roles in the medical home. However, frustration with implementation barriers and the added work burden they associated with patient-centered medical home persisted.
Conclusion:
Patient-centered medical home transformation is disruptive to practices, requiring enduring commitment of leadership and personnel at every level, yet the model continues to hold out promise for improved delivery of patient-centered primary care.
Keywords: Patient-centered medical home, primary care transformation, primary care, evaluation outcomes, quantitative and qualitative evaluation, health services delivery, health-care delivery
Introduction
The patient-centered medical home (PCMH) model of primary care delivery has taken hold throughout the United States,1 and practice transformation efforts have proliferated across the country, yet there remain significant gaps in our understanding of the processes, roles, and outcomes. Large numbers of practices have striven to transform their care delivery to implement efficient and effective team-based, patient-centered care, and it is essential that we have contextually based evaluation studies that include examination of work roles and processes for understanding how PCMHs develop and function.2–9 Some studies have found significant variability in how PCMH has been implemented,10 and others see concordance in steps toward increasing establishment of PCMH processes.11 For many who are concerned about the future of primary care, the PCMH model holds out the hope of aiding practices in achieving the Triple Aim12 of improved outcomes, better patient experience, and reduced costs. In recent years, this notion has been expanded to the proposed Quadruple Aim that recognizes provider satisfaction as an additional fundamental component of primary care practice.13 It has become clear over time that while PCMH core principles have evolved and there is no single way to achieve transformation,14 substantive PCMH transformation requires a values culture change, and even modification in the words used to discuss how primary care is delivered.15,16
Evaluation and outcomes investigations of PCMH and other practice transformation initiatives have been problematic for many reasons, including: (1) outcomes have been largely focused on relatively simple-to-capture “micro-measures” that provide a reductionist view of PCMH transformation, such as documentation of HgA1C and blood pressure, or provide limited understanding of what actually occurred, such as checking off that smoking cessation counseling was done;17,18 and (2) reported outcomes of PCMH initiatives have demonstrated varied efforts and results, with individual components creating successes or challenges. For example, a study of PCMH transformation in 30 practices across the United States documented successful work role innovations that enhanced team-based care.9 In California, a study of PCMH “concordant care” found that patients who experienced the three PCMH-related care components of continuity, coordination, and management, also received multi-faceted high-quality care. Patients who did not experience all three components received fewer aspects of care that constitute high-quality primary care.19 Health centers in New Orleans that undertook more significant PCMH transformation received higher scores from patients on care coordination.20 Furthermore, primary care settings that serve as teaching sites of various kinds may experience additional challenges and opportunities regarding PCMH transformation.21–23
Provider and staff burnout are frequently discussed in relation to increasing job satisfaction within primary care practice. Burnout is therefore important to consider in the context of the hard work of transformation in primary care.13,24 Findings have varied. In a survey of safety net clinic employees, staff and providers who perceived their site to include more PCMH components reported higher morale, and staff reported increased job satisfaction. However, providers reported decreased “freedom from burnout.”25 An earlier study comparing a PCMH site with controls found that a lower percentage of staff at the PCMH reported high emotional exhaustion at follow-up.26 Despite contradictory findings, it is clear that in addition to stress associated with the change process itself, stress resulting from insufficient resources to efficiently meet increasing demands for documentation, along with inadequacy of many electronic health records to produce the required data, is a significant contributor to burnout.27
The overarching research question for this article is: What are the evaluation outcomes that provide a picture of whole system changes from the perspective of patients, providers, and staff in a facilitated Rhode Island PCMH transformation intervention? This study was conducted by the Brown Primary Care Transformation Initiative (BPCTI) in the Department of Family Medicine at the Warren Alpert Medical School of Brown University. Our transformation facilitation team delivered in-depth, on-site facilitation, working closely with each practice to develop its unique PCMH transformation plan targeted to the conditions, needs, and goals of each practice.
New contribution
In an era where change initiatives for delivery of primary care are widespread, and evaluation is often limited to the measurement of micro markers of change, this study provides an example of an effort to obtain a more contextual understanding of whole system change. With increasing attention to PCMH as an expected primary care delivery model, findings from our evaluation study will expand our understanding of how practices transform and, further, how stakeholders respond to the change process. Our approach used quantitative and qualitative methods for the evaluation of varied primary care practice types. This approach is transferable to diverse practice settings, with potential for tailoring to address the particular needs of each transformation initiative.5,28
Methods
Study background
Overview
The BPCTI was a 5-year Health Resources and Services Administration (HRSA) grant (2010–2015), developed to facilitate PCMH transformation and training initiatives in the state of Rhode Island.28 Our aim was to facilitate and evaluate change at eight differing types of RI primary care teaching practices. Data collection for evaluation began 1 year into the study, with most of the first year having been dedicated to the development of the methodology, staff recruitment and training, and recruitment of the first practices. Our philosophy for the facilitation intervention was to prioritize the voice and experiences of patients in practice transformation, foster widespread practice engagement and identification of each practice’s most pressing transformation needs, and promote culture change within the practice.16 Given the design of this study, which did not offer monetary performance incentives to the practices, it was essential that participating practices express high interest at the outset in engaging with the hard work required to make changes in care delivery. Practices recruited into our study chose to participate due to their leadership’s interest in how the PCMH model could enhance the efficacy and efficiency of patient-centered care. We developed a project description and made it known across the state through various communication mechanisms that we were seeking interested practices with the following inclusion criteria: (1) being a primary care teaching site for residents and/or medical students; (2) having an electronic medical record (or being in the process of obtaining one); (3) identifying a physician champion for the PCMH transformation process; and (4) demonstrating motivation to engage providers and staff in transformation. Additional considerations for overall practice recruitment included selecting a diversity of primary care practice sizes, types, and locations in the state. Our project directors met with leadership of interested practices to gage their eligibility and commitment prior to inviting them to participate.
PCMH facilitation
The practice facilitation team lead was a family physician (co-author J.B.), and facilitation staff came to the project with varying educational and professional backgrounds, creating a dynamic team environment. To enhance PCMH transformation facilitation expertise among our team, a PCMH practice transformation expert was engaged as a consultant to train staff and guide development of the facilitation strategies. The BPCTI facilitation team met weekly throughout the project period to discuss progress in the practices, review literature and share PCMH tools, techniques, and innovations, and engage in ongoing training in a collaborative learning environment. While the approach to each practice was individualized, these team meetings fostered communication among facilitators and project leadership and standardized our project’s overall approach across practices. In addition, twice-yearly focus groups with the entire facilitation team (moderated by the project’s evaluation lead, co-author R.E.G.) added to our ability to explore how facilitation was progressing over time, and what changes needed to be made to our practice facilitation and project staff training plans.
Facilitation began at each practice site with a kickoff event to which all practice personnel and patient representatives were invited. The kickoff was designed and led in partnership with each practice’s PCMH champions. The event included explanation of the concepts associated in the literature with the PCMH model, practice leadership articulating their vision and goals for PCMH transformation, and invitation to the entire practice to brainstorm on further goals and collaborate on coordinated change initiatives. We encouraged patient involvement, and patients often were active participants right from the start at the kickoffs.
Facilitators visited the practices regularly throughout the study period, attended monthly PCMH practice meetings and were available by email and phone to provide support services, including assistance with operational innovations (e.g. instituting open-access scheduling where patients book same-day appointments), health information technology, PCMH recognition applications (i.e. National Committee for Quality Assurance—NCQA),29 communication processes, team-based care, patient engagement, workflow modification, and maintaining motivation for practice transformation. During particularly intensive periods, a facilitator may have been in contact with a practice daily, and at other times would communicate primarily at monthly meetings and when needed also by email or phone.
Data collection to foster transformation facilitation
Data were collected that served both to inform facilitation strategies and to evaluate the practices’ experiences with PCMH change processes. After the kickoff, extensive observation was conducted in each practice to develop iterative strategies to facilitate transformation and promote establishment of PCMH components in the practices. A baseline PCMH needs assessment using quantitative and qualitative methods was conducted, and findings were presented to each practice in a detailed report addressing the following categories: access to care, provider continuity, team-based care, adaptive reserve, care coordination, care management, patient centeredness, physical plant layout, health information technology, population management and workflow. Readiness to change was assessed with a survey designed by the BPCTI team and results of this formative, working survey were included in practice reports. Facilitators met with each practice to review the findings and assist practices in designing specific, staged action plans to address outstanding issues and devise projected timelines. Our facilitation team worked closely with each practice through observations, consultation and collaboration to determine strengths and needs and to engage leadership and staff in developing transformation plans suited to their unique circumstances.16
Conceptual framework
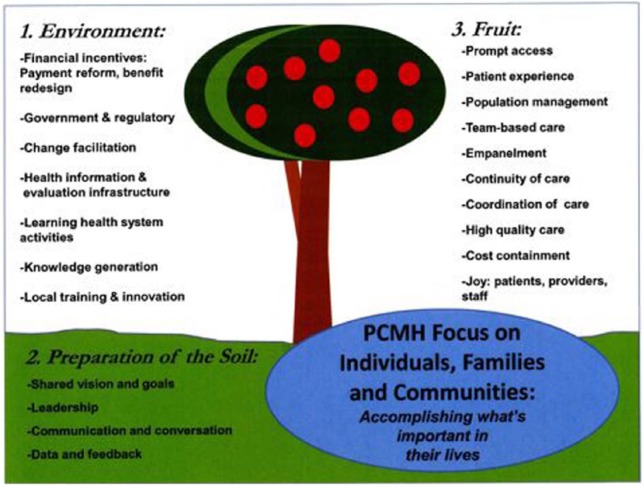
The assumptions underlying study design, data collection and analysis, and development of our final interpretation of the findings stem from insights gleaned from PCMH Evaluation and Transformation Think Tanks we convened at Brown University.5,28 The purpose of the Think Tanks was to bring together international experts on PCMH evaluation and transformation to identify the critical methods, tools, and concepts for understanding and implementing PCMH transformation from a holistic perspective. We convened the Evaluation Think Tank first in order to benefit from the findings prior to beginning our baseline evaluation work for the study, and to formulate the conceptual framework that would underlie the project. The resulting framework5 draws from the Think Tank discussions and literature on PCMH published at the time.30–34 The framework holds that in PCMH evaluation it is essential to obtain a conceptual understanding of not only what occurs through PCMH transformation, but also how it occurs and why, and a study design using both qualitative and quantitative methods must be implemented with multiple stakeholders to explore the transformation environment. Figure 1 illustrates the multiple components identified in the Think Tanks as underlying a comprehensive approach to transformation, including the need to consider inputs from the environment and prepare components of the “soil” to reap successful production of the “fruits” of PCMH. This article discusses a selection of the components that stood out as especially impactful in this project.
Figure 1.
Contextual model of PCMH evaluation components.
Evaluation methods overview
A baseline and follow-up evaluation study of the eight practices was conducted to understand how practice providers, staff and patients understood and experienced the transformation process, endeavoring to explore, as Crabtree et al.31 recommend, the “whole system changes.” Evaluation methods included practice observations; patient, provider, and practice staff qualitative interviews; surveys for patients, providers, and practice staff, and periodic focus groups with the facilitation team to discuss progress, barriers, and solutions. Patient instruments were in English and Spanish. Our evaluation team met weekly throughout the project period to develop the evaluation plan, choose methods and instruments, train data collection staff, monitor data collection, work through problems, and analyze the quantitative and qualitative data. Complete details of the evaluation design are described elsewhere.5,28 This article reports findings from one provider/staff survey, two patient surveys, qualitative interviews with providers, staff, and patients, and the facilitation team focus groups. Practice observation field notes were used to inform selection of surveys, development of interview guides, and practice facilitation plans. Observation data are not reported in this article. The Memorial Hospital of RI Institutional Review Board approved the study (#11-24), and informed consent was obtained for surveys and interviews.
Quantitative surveys
Samples, recruitment, data collection and measures
We included quantitative measurement tools that were feasible to implement, validated when possible, and that addressed multiple areas of practice functioning. Data were collected from providers, staff, and patients at each practice at baseline, aiming for a range of participant characteristics and then again at around one and a half years into the transformation process. Providers included family medicine and internal medicine residents, independently practicing MDs and DOs, nurse practitioners, and physician assistants. Practice provider/staff sample sizes for the total of the two assessment time points were calculated based on practice employee size. Only the smallest practices had universal samples, and so the N over the two time points ranged from 4 to 83. Practice employees were recruited for surveys in person and through email and completed the surveys either on paper or through an online platform. Patient survey sample sizes also ranged based on practice size, with a total of 58 to 220 for the two assessment time points. For several weeks over various times of the day and week, evaluation staff handed paper surveys directly to patients in practice waiting rooms. Also, practices made paper copies available to patients who deposited completed surveys in a locked collection box. All surveys for providers, staff and patients were completed and returned anonymously. We used the following survey instruments:
Practice clinician survey
The Maslach Burnout Inventory (MBI)35 is a 22-item instrument designed to assess three aspects of burnout: emotional exhaustion, depersonalization and decreased personal accomplishment. Questions are answered on a 7-point scale regarding how often respondents experience symptoms, from 0 = never to 6 = every day.
Patient surveys
The Patient Activation Measure (PAM)36 consists of 13 items that include statements regarding confidence, beliefs, knowledge and skills related to managing one’s health and healthcare. For each question, there are five possible responses on the PAM with four that range from strongly disagree to strongly agree and a fifth response—not applicable.37 The total score ranges from 13 to 52. Using Hibbard’s methodology,37,38 the raw scores are transformed into an activation score ranging between 0 and 100. A higher score corresponds to a higher level of patient activation.
The Patient Satisfaction Survey5 was developed by the U.S Department of Health and Human Services Health Resources and Services Administration and has 25 items with closed responses and three additional open-ended questions. For the first 23 questions, patients rate their care in multiple categories on a scale from 1 = poor to 5 = great; the final two questions have a yes/no response. Open-ended questions were included about what patients like best and least about the practice, and about their suggestions for improvements.
Statistical analysis
Simple frequencies and percentages were generated for practice level data. Data collected from respondents within each practice are often correlated with each other. To address this potential for correlation, these data collected from patients, staff and providers were analyzed using generalized linear mixed models (GLMMs) adjusting for practice. Since all surveys were collected anonymously, matching of data collected at baseline and follow-up assessments was not possible. Although this may introduce some bias in the analysis, the length of time between assessments (1.5 years) is long enough such that repeated testing bias is minimal, and respondent turnover would provide relatively independent samples at baseline and follow-up. To examine changes between baseline and follow-up responses, an assessment variable was included in the GLMM models in addition to adjusting for practice. No adjustments were made for missing data, since all values reported had <5% missing items, and most values had <2% missingness. All analyses were conducted using IBM SPSS Statistics for Windows v23.
Qualitative interviews and focus groups
Instruments, samples, recruitment and data collection
Qualitative in-depth, semi-structured individual interviews of approximately 30 min were conducted with PCMH champions, practice administrators, providers and staff who were involved in the PCMH process at each site, as well as with patients. Development of two open-ended question guides for practice employees and for patients was informed by the PCMH Evaluation Think Tank discussions, published literature, and observations in the medical practices. For practice employees, interviews focused on initial plans for becoming a PCMH; PCMH attitudes, knowledge and engagement; job roles; workflow communication; vision for practice transformation; and perceived barriers and facilitators to change. Patient interviews addressed patients’ perspectives on the nature and processes of care they received at the practice. All questions were pilot tested and modified as necessary.
Practice employees were purposively sampled39 to engage individuals in all practice roles and those who were involved in different aspects of the transformation endeavor. Employees were informed about the study at the initial kickoff event, through the facilitators’ presence at meetings and during observation, and through practice-wide emails to invite participation in interviews. Patients were purposively sampled in the clinic waiting rooms to include women and men of all adult ages, and parents of pediatric patients. Data collection staff approached patients/parents in waiting rooms at varying times of the day over several weeks to invite them to participate in an interview in English or Spanish. Patients who agreed signed the consent form, and an arrangement was made to meet the patient following conclusion of the medical visit to conduct the interview in a private room. Documentation monitored fulfillment of recruitment goals for participant characteristics. Interviews were audio-recorded, and interviewers listened to the recordings and wrote a detailed summary of each session.
Focus groups with the entire facilitation staff were conducted and recorded by the evaluation lead approximately every 6 months. An open-ended question guide was created to explore how the staff perceived their changing facilitation role over time, barriers they encountered at the practices, and solutions they devised.
Qualitative analysis
For qualitative data analysis, we used immersion/crystallization40 processes with our conceptual framework for understanding the multiple dimensions of PCMH transformation from the perspectives of different stakeholders. This involved: (1) two co-authors listening to the interview and focus group recordings and reading the summaries while taking further analytic notes to extract data and specific quotes relevant to discerning elements of the practice culture and other factors that might impact the transformation process; and (2) periodic larger project team group discussions of the data to discuss patterns that emerged from the individual analyses, identify variations in interpretation possibilities, and to arrive at final interpretation and selection of illustrative quotes for presentation of the findings. Insights from the interview analyses were included in the reports provided to each practice. Furthermore, findings from the focus groups with facilitation staff were used to adjust facilitation and on-going staff training strategies as we moved through the project.
Results
Provider and practice characteristics
The eight recruited practices were family medicine and internal medicine outpatient residency training sites at a Brown University-affiliated hospital, and six community-based RI primary care teaching practices that precepted medical students and/or residents for time-limited rotations: two community health centers, one micro-practice with two part-time family physicians, one single physician practice with a nurse, one multiple family physician practice with nursing and other staff, and one college health service. Table 1 presents characteristics of the providers and practices. The majority of providers (83%) were under 50 years of age and were female (73%). Of the practices, 25% were solo practices, 25% were residency training practices and the other practices included community health centers, multiple physician/staff, and collegiate health services.
Table 1.
Characteristics of providers and practices.
| Provider characteristics (n = 56) | Frequency (%) |
|---|---|
| Age (years) | |
| <50 | 46 (82.1) |
| >51 | 10 (17.9) |
| Gender | |
| Female | 41 (73.2) |
| Race/ethnicity | |
| White | 33 (58.9) |
| Other | 23 (41.1) |
| Practice information (n = 8) | Frequency (%) |
| Type of practice | |
| Solo or micro-practice | 2 (25.0) |
| Community health center or multiple physician/staff | 3 (37.5) |
| Residency training | 2 (25.0) |
| Collegiate health services | 1 (12.5) |
| Registries in use (diabetes, COPD, cancer) | 3 (37.5) |
| NCQA certified | 4 (50.0) |
| Open access | 5 (62.5) |
| Precept medical students/residents in the practice | 8 (100.0) |
COPD: chronic obstructive pulmonary disease; NCQA: National Committee for Quality Assurance.
Quantitative surveys
Patient demographics
Table 2 presents a summary of patient participant (n = 415) characteristics at baseline and follow-up. Mean age was 37 years, and about 77% of the independent samples of patients were female at both surveys. About 15% of the baseline population and 18% of the follow-up group were Hispanic. Whites comprised about 70% at both time points.
Table 2.
Patient survey respondent demographics*.
| Baseline (n = 415) | Follow-up (n = 415) | |
|---|---|---|
| Age (mean (SE); range = 18–92 years) | 37.3 (4.5) | 36.8 (4.6) |
| Female (n, %) | 320 (77.1) | 318 (76.6) |
| Race (n, %) | ||
| Asian | 18 (4.3) | 21 (5.1) |
| Black | 28 (6.7) | 31 (7.5) |
| White | 293 (70.6) | 274 (66.0) |
| Other | 76 (18.3) | 89 (21.4) |
| Hispanic (%) | 58 (14.0) | 73 (17.6) |
Values presented are adjusted for within practice correlation.
Patient satisfaction survey
The Patient Satisfaction Survey questions were grouped in categories, and results are presented as composites in each category5 (Table 3). Overall, patient satisfaction scores were high at baseline and follow-up. The survey categories with the lowest mean scores were “Waiting” and “Payment,” while the categories with the highest mean scores were “Confidentiality” and “Nurse and Medical Assistants.” Total satisfaction (composite score) on this survey increased (p = 0.04) and one of the nine subscales, “Satisfaction in the Facility”, demonstrated a statistically significant improvement (p = 0.03) from baseline to follow-up. Improvement in the subscale “Ease of Care” trended toward significance (p = 0.06).
Table 3.
Patient survey results—total scores and subscales.
| HRSA Patient Satisfaction Survey | Baseline (n = 415) |
Follow-up (n = 415) |
p value | ||
|---|---|---|---|---|---|
| Mean** | SE** | Mean** | SE** | ||
| Total satisfaction* (range = 7–49) | 33.21 | 0.40 | 34.03 | 0.51 | 0.04‡ |
| Ease of care | 4.14 | 0.09 | 4.24 | 0.08 | 0.06§ |
| Waiting | 3.81 | 0.11 | 3.87 | 0.14 | 0.49 |
| Provider | 4.45 | 0.07 | 4.48 | 0.08 | 0.67 |
| Nurse & medical assistants | 4.53 | 0.05 | 4.51 | 0.07 | 0.78 |
| Staff | 4.40 | 0.09 | 4.47 | 0.07 | 0.20 |
| Payment | 3.93 | 0.11 | 4.11 | 0.12 | 0.19 |
| Facility | 4.46 | 0.06 | 4.51 | 0.05 | 0.03‡ |
| Confidentiality | 4.60 | 0.05 | 4.64 | 0.05 | 0.29 |
| Patient Activation Measure (PAM) (range = 0–100; median = 63) |
65.68 | 1.35 | 63.12 | 1.74 | 0.01‡ |
HRSA: Health Resources and Services Administration.
Higher scores indicate greater satisfaction.
Values presented are adjusted for within practice correlation.
p ≤ 0.05.
p > 0.05 but less than 0.10.
PAM
Table 3, final row, shows an overall, statistically significant decrease from baseline to follow-up in patient activation (p = 0.01).36 When stratifying by type and size of practice, this change was statistically significant only for the college health service (p = 0.01).
MBI
Primary care providers, nurses and other clinical staff completed the MBI.35 Table 4 shows that in the three subscales of emotional exhaustion, depersonalization, and personal accomplishment, emotional exhaustion and depersonalization increased slightly and personal accomplishment decreased slightly, although it was not statistically significant. Clinical staff had slightly higher levels of emotional exhaustion than the national mean, lower levels of depersonalization, and higher levels of personal accomplishment. Stratifying by role, emotional exhaustion, and depersonalization were considerably higher at baseline and follow-up for providers compared to nurses and other clinical staff, and these differences between roles regardless of time point were statistically significant (p < 0.01). Personal accomplishment did not exhibit the same extent of difference by role. Compared to nurses and other clinical staff, providers had somewhat higher levels of personal accomplishment at both baseline and follow-up, but this difference was not statistically significant (p = 0.36).
Table 4.
Provider and staff burnout—Maslach Burnout Inventory (MBI) results*.
| MBI Scale | Personnel | Baseline (n = 161) |
Follow-up (n = 104) |
National |
|---|---|---|---|---|
| Mean (SE)*** | Mean (SE)*** | Mean | ||
| Emotional exhaustion | All clinical staff | 21.10 (1.79) | 21.58 (1.30) | 20.54 |
| By role** | ||||
| Nurse/staff | 18.97 (1.92) | 18.45 (0.75) | ||
| Provider | 24.41 (1.10) | 25.09 (1.22) | ||
| Depersonalization | All clinical staff | 5.74 (1.31) | 6.03 (0.97) | 7.18 |
| By role** | ||||
| Nurse/staff | 4.25 (0.56) | 3.79 (0.48) | ||
| Provider | 8.02 (1.24) | 8.54 (0.57) | ||
| Personal accomplishment | All clinical staff | 39.12 (0.56) | 38.45 (0.56) | 36.42 |
| By role** | ||||
| Nurse/staff | 38.87 (0.85) | 37.87 (0.70) | ||
| Provider | 39.50 (0.78) | 39.09 (0.98) | ||
MBI scales were not statistically different between assessments (baseline vs follow-up).
There were no differential changes over time by role (interaction between role and assessment). There is an overall significant difference by role for the emotional exhaustion (p < 0.01) and depersonalization scales (p < 0.01).
Values presented are adjusted for within practice correlation.
Qualitative interviews
In total, 95 interviews were conducted with patients; 78 with practice staff (including nurses, medical assistants, and administration and pharmacy staff); 42 with physicians (including residents at the family medicine and internal medicine residency practices); and 4 with nurse practitioners and 2 with physician assistants at the one practice that employed these types of clinicians.
Patient perceptions of their primary care practice
Satisfaction
Across the eight healthcare sites, patients expressed high satisfaction with their care and said they would recommend their primary care practice to others. As a patient commented, “I can switch at any time, but I’m comfortable here. The doctors here know about me. It’s nice.” A patient in another practice asserted, “This is the way healthcare should be, and you don’t find that everywhere.”
Recognition of PCMH components
While patients were not explicitly aware that their primary care practice was a PCMH, they described aspects of practice functioning that align with the PCMH model. Patients across practices expressed recognition of and appreciation for staff teamwork, for example: “They’re my own little team, they’re on the same page.” Another patient said she “saw the front desk working together” to make her appointment. Patients of the smaller practices in particular noticed team-based care: “It seems that work is seamless … I have put in volunteer time [at the practice] and seen them work together very well.”
Coordination of care with outside providers was variable across practices and appeared to function better in smaller practices:
I see [my primary care physician] less frequently than I see my [specialist] and I walk in here today, and she’s like, “I already have everything.” So I don’t have to track down blood lab results and tests. Everyone communicates really well.
In contrast, a patient from a larger practice expressed frustration about the communication between her psychiatrist and her primary care physician: “I think that would be a good idea if they were more in sync with each other … especially with what I went through with lost paperwork and stuff. It should all go into the computer.” Some patients were concerned about patient flow and communication with non-clinical staff. Long wait-time was a frequently mentioned source of frustration, except for patients at the micro-practice. Receptionists, often harried by the multiple tasks they simultaneously perform, were at times seen as unaccommodating and “not too friendly.” As one patient explained, “[I wish they were] showing a little more compassion, being in the medical fields. Just because you’re a receptionist doesn’t mean you’re just a receptionist.”
Continuity with providers is a PCMH component that patients appeared to value highly, though only some of the practices prioritized continuity. A patient who wished she had a doctor “assigned to her” felt that since her doctor changed “every six months,” her care was not as good as if she had one doctor who “knows all of your case because they are there with you all the time.” Another patient explained, “I don’t like being told that we’ll continue talking about an issue next time, only to have it be a different doctor next time.”
Communication with providers
Patients felt that they were able to communicate well with their primary care providers, and that their providers involved them in health-care decision-making. This was particularly so in the small practices where they felt they received high-level personalized care:
It’s great because the doctors here are very responsive. You never get a sense that they’re rushing or not spending enough time with you. [My doctor] is happy to answer all of my daughter’s questions and explain everything as she is going along.
I’m always involved in the decisions … They’re very receptive to that and I know I can always put forth how I feel about what I like to do care-wise.
I am treated as a person and not a number. I’ve been to other practices where it is like an assembly line and I don’t like that. [Here] I am not rushed.
Patients throughout the practices felt well-informed about the various implications of treatment options and were especially appreciative when they thought that the decisions were left up to them. One asserted, “[My doctor] asks me to do a lot of things, and I say “No.” She accepts it and tells me the pros and cons.” Another explained, “The doctor will tell you what they recommend, but will not demand it.”
Provider and practice staff perceptions of PCMH
Impact of participating in the PCMH initiative and receiving in-person transformation facilitation
Practice employees noted that as a result of the facilitation process, they have a “new mind-set,” and “it reinvigorated everyone.” The practices became “aware and awake” to issues that were long plaguing daily workflow, but that had not previously been adequately recognized, discussed and addressed. Some claimed that the facilitation process enabled the development of improved communication strategies, which in turn resulted in the formation of better relationships through all levels of the practice, as a medical assistant explained: “More communication on an even basis—not ‘Oh, you’re the doctor’.” In addition, practice employees claimed that through the transformation facilitation, more staff beyond the PCMH champions became “on board” with the PCMH initiative, new programs and policies were established, and a heightened focus was placed on establishing strategies for patient-centeredness. In contrast, some providers and staff were dismissive about the special nature of PCMH, for example: “This is a place that is always changing. If it’s not PCMH, it’s always something.”
Knowledge and recognition of PCMH transformation
Many providers and staff were familiar with the jargon and catch-phrases associated with the PCMH model but did not grasp the gestalt of what it means to be a PCMH. Even among those who valued PCMH, many still had doubts at the follow-up point about the overarching goals of the model:
PCMH feels sometimes so nebulous. Impossible to grasp or achieve. But I think the important thing is that you generally try to bring things up to speed in terms of meaningful use and using your [electronic] medical record. And take little pieces of [PCMH] and try to attack it … But when we rolled out the new health center we were able to brandish PCMH as something that we wanted to embody. And it’s not just idle words to be able to offer something to people and say, “We’re really current, and this is what we do.” (Physician)
Most providers and staff initially reduced the PCMH model to specific elements, such as hiring a nurse care manager, struggling to apply for and achieve NCQA recognition, and the on-going burden of documentation and outcomes reporting. In the follow-up interviews, many still associated PCMH with particular components, but at this later point these were process-oriented elements, such as having regularly scheduled PCMH meetings, creating mechanisms for team-based care, establishing the norm of morning team huddles, routinizing medication reconciliation, establishing an open-access appointment system, figuring out how to best integrate a nurse care manager in the practice, and using patient satisfaction data to drive practice improvements.
At some sites where implementation of PCMH features became routine over the course of the study period, providers and staff no longer identified these practice elements as PCMH innovations. This indicates that at least some components of PCMH were becoming institutionalized within the practices:
PCMH is rolled in. So when we had operations meetings today, many things on the agenda, I mentioned pods. I think that’s the way it should be. Because if you isolate it and say, “This is PCMH and this is the time we’re going to talk about it,” that’s okay when you’re starting, but now it has to encompass everything you’re doing. And I think it’s demonstrated very well in all of our meetings. (Practice manager)
I feel really lame that I don’t know precisely how PCMH is proceeding. My sense is that it’s almost been folded into PI [practice improvement]. And it’s now just a part of that bi-weekly PI and health leadership operations amalgam that we’re sort of doing, which I think maybe is good. Maybe that’s something PCMH is. Rather than being a specific meeting, it’s being sort of absorbed. (Nurse)
Leadership and staff involvement in PCMH transformation
Each practice differed in regard to how, in actuality, the transformation initiative went forward. Variations among practices included which roles in the practice the champion(s) held (e.g. physician owner/partner, physician employee, nurse, and office manager); how the champion(s) initially engaged and sustained engagement of other providers and staff; and to what extent and in what ways staff embraced the PCMH goals, were involved in the early stages of the transformation process, and remained involved. This was evident in the baseline interviews and persisted in follow-up interviews with little consistency within practices, as employees and even champions in the same practice expressed disparate views of which aspects of PCMH transformation were needed and had been accomplished.
Attitudes toward PCMH
Across sites, most of the providers and staff had at least partially positive attitudes toward PCMH, although most also harbored reservations about the model, and frustration with the extra work implementation involves. Concerns included the perception that a fully successful PCMH requires a tremendous amount of change that is impossible to achieve and conversely, that PCMH is a new name for what good primary care has always been. For some, confusion lingered, as they continued to view PCMH not as a transformative process, but as a concrete entity—the monthly meeting, or specific people associated with PCMH. For example, a nurse referring to the changes in membership on our facilitation team over the course of the project explained that her practice had difficulty keeping track of “who PCMH is.” Others equated PCMH with NCQA recognition and the accompanying burden of data reporting and establishing NCQA-required protocols. When providers reduced PCMH to specific, disjointed components and did not view them as contributing to a broader whole leading to an environment of enhanced patient care, they were discouraged. A physician wearily commented, “They tell us ‘This is the requirement: PCMH wants us to do this and this’.” Another expressed that PCMH is “jumping through the hoops” of NCQA. A physician who had recently completed the NCQA application and its required practice modifications asserted, “PCMH has been a distraction to the things we really would like to implement.”
Despite these many concerns, providers and staff in all of the practices felt that at least ideally, the PCMH model has positive potential.
Moving into [the PCMH] model is absolutely the way to go for patient satisfaction and efficiency. It makes sense for the same group of people to work with the same clientele. You get to know them and their needs more intimately. You’re able to huddle as a care team and look at what is coming up for the day and have everything ready to make the process as efficient as possible. (Physician)
Persisting challenges to PCMH implementation
Practice providers and staff described a variety of challenges that they grappled with throughout the study period and that persisted, at least to some extent, at the time of follow-up interviews. Even though all providers and staff were invited to the kickoff and subsequent regularly scheduled PCMH meetings, they did not equally internalize the PCMH model nor understand how it related to needed changes in their practice. Therefore, embracing the transformation goals and taking the time to work with their colleagues and our facilitators to develop strategies for transformation implementation and maintenance was uneven both across and within practices. At one large practice, multiple staff explained that some changes that were established by protocol modifications were not sufficiently communicated throughout the practice, and other changes that were tried simply fell by the wayside over time. In small practices, the PCMH principle of physician leadership6 was given, as there were few or no employees. In larger practices, PCMH leadership varied and was sometimes shared to include practice managers, an executive director, a quality improvement nurse, or a physician medical director. At a university health service, PCMH champions were designated from each clinical role at the site. Practice employees considered shared leadership to be beneficial, though it took concerted effort within the practices to maintain.
Despite efforts and intentions for inclusion, in the larger sites, it was more difficult for staff to understand and establish their roles in PCMH transformation. Reconfiguring long-held job roles was difficult at some sites where staff may have been excited by the new opportunities, yet concerned about taking on new responsibilities themselves or allowing others to do so. One nurse explained this difficulty, stating, “Nurses needed to find their niche in the PCMH.” A nurse who had encountered resistance noted, “People don’t want to change.” A physician champion stated that while leadership support is essential, he believed that it is easier to bring the non-physician staff into the change process first, and physicians will follow more agreeably once the change is somewhat established.
When practices instituted mechanisms to encourage all staff to “work to the top of their license,” as the frequently-heard PCMH concept for leveraging the potential of every member of the team is phrased, it meant, according to medical assistants, that they had to take on “extra work.” Chronic understaffing in larger sites complicated this process and also limited the time and energy that staff had to devote to PCMH activities. On the positive side, the PCMH model improved communication and promoted inclusiveness, as a medical assistant explained: “Instead of throwing directives, [the practice is] making [medical assistants] a part of the team and saying ‘Listen, this is what happens to a diabetic’s eye’.”
Incorporating patient engagement, another vital component of the PCMH model, was a challenge for all practices. One practice had a patient advisory board that periodically met through the year, all practices solicited patient satisfaction feedback through surveys (as is required by NCQA), but none felt that they were adequately engaging patients in their PCMH efforts. A nurse practitioner commented in the follow-up interview that she still hoped to enhance patient engagement in the future “to creatively address some things we haven’t thought about yet.”
Finally, structural and process components of transformation constituted persisting barriers to full implementation of desired innovations, such as finding ways to make the open-access system function well for both patients and practice workflow. Open access was considered one of the hallmark modifications associated with the PCMH model and some of the practices put in great effort to convert to this system. However, it was difficult to handle the volume of patient calls flooding the receptionists’ telephone lines first thing in the morning, and the available slots quickly filled up each day without accommodating all patients needing appointments. In addition, for those patients who needed language interpretation, the open-access system precluded the necessary pre-booking of interpreters who are external to the practices. One of the larger practices worked through the kinks in their open-access system over time and deemed it successful.
Practice achievements in PCMH transformation
Despite the barriers and difficulties encountered by practices in implementing practice changes consistent with the PCMH model, providers and staff described many areas of success. As one provider said of her practice after working on PCMH transformation, “We are prepared not only to meet the provider needs but also the patient needs.” The successful change components were not uniform across the eight study sites because the objective of our project was to facilitate the practices in identifying and implementing needed changes specific to their own practice conditions. Table 5 provides the types of PCMH-related changes achieved among the practices as a whole. Each practice accomplished a selection of these components.
Table 5.
Types of PCMH transformation components achieved among the practices*.
| • Enhanced team-based care • Establishment of daily morning huddles to discuss the day’s scheduled patients • Nurse follow-up of doctor visits • Nurse provision of patient education • “Boot camp” sessions to train medical assistants to take on more responsibilities and work to the top of their license • Restructure of a large practice into a pod system: proximity of all levels of clinicians improved both provider/staff communication and care • Deliberate empanelment which facilitated improved continuity of care and enhanced patient–physician relationships • Systematized, routinized medication reconciliation review • More effective use of the electronic health record, including for population health management • Creation of an electronic patient portal • Institution of online patient self-scheduling within an existing patient portal • Instituting an open access, same-day appointment system • Establishing and expanding behavioral health services within the practice • Redesign of waiting room to improve confidentiality • Redecoration of waiting room to improve inclusion of diverse ages, genders, races/ethnicities |
Each practice achieved some, but not all, of these PCMH components.
Facilitation staff perceptions of their role and their work
Over the course of periodic focus group discussions with the facilitation staff, they explained that their job required flexible role identities as they shifted between being participant observers of interactions within the practices, data collectors to understand how the practice functioned, and advisors. As one facilitator noted, “We’re kind of a reflector and also a resource.”
Facilitators saw themselves as variously information, resource, technology and conflict resolution specialists. They were teachers, problem solvers, organizational counselors and motivational coaches. Irrespective of background, age and amount or type of facilitation training received, all staff felt their confidence increased through on-the-job exposure and being initially paired with more experienced facilitators:
When I started as a facilitator … I had to meditate, or I had to really, really work on my own presence because I felt like I was jumping into this milieu where there was all this tension, and conflicts and background … As sort of a coaching figure I had to be together and supportive, no matter what. And it drew a lot [from me]. And then, as I got more comfortable, I don’t have to do that as much anymore. (Facilitator)
They cited persistence, patience, appreciation of site uniqueness, and the need to curb their tendency to prescribe an agenda as essential for gaining trust and meaningfully engaging busy practice providers and staff in the transformation effort:
What is my role? Am I taking the lead enough in the meetings that I have at [the practice]? Am I standing back too much? Am I letting them drive it? I should be, but I still feel like they’re not very straight drivers … (Facilitator)
Each facilitator worked with more than one practice, and because the practices had different goals and approached their change initiatives differently, varied facilitation techniques were used. Facilitators asserted that transparent communication, maintenance of relationships, and in-person interactions with PCMH champions from every practice role were critical for promoting progress and fostering movement of providers’ and staff’s focus away from the burdens of PCMH and toward embracing the potential of PCMH for enhancing patient care. As one facilitator explained later in the project period:
I can see sites thinking about how they can make their patient experience better, not just focusing on if their NCQA is up to date. There’s a patient at the other end of that measure, and I think a lot of our [practices] get that more and more. (Facilitator)
Discussion
Facilitation and transformation
While best practices for PCMH implementation have been promoted, it has also been recognized that a single facilitation design or PCMH content list will not suit all PCMH endeavors.41–45 Our evaluation of eight varying types and sizes of primary care practices, using both quantitative and qualitative methods, attempted to identify elements of PCMH transformation processes that were important to providers and staff and that may influence patients’ experiences. Providers and staff in our study described the effect of the on-site PCMH transformation facilitation process as both adding to and detracting from the essence of how they perceive their practice. For some staff, PCMH had such a concrete presence that it was associated with particular facilitation staff from our team or meetings those facilitators convened. For others, PCMH discussions and processes had become less tangible, as these became more integrated into normal practice functioning, and practice staff even wondered if enough explicit attention was still paid to PCMH. While a goal in PCMH is for change efforts to eventually become routinely implemented, transformation in thinking and transformation in action are necessarily iterative processes that must be re-evaluated as practice needs and the healthcare environment evolve. Consequently, a risk associated with complete routinization is that the on-going iterative process of PCMH transformation at the practice may stall, as special attention to PCMH is no longer considered necessary. Transformation goals gradually drop off the radar during everyday workflow and meetings, and providers and staff may not recognize that this has occurred.
Patients’ attitudes toward PCMH
Shifts in attitudes about PCMH were less dramatic among patients than among practice employees, possibly because the PCMH model promotes changes in care and operations that are less visible to patients46,47 and occur in the background of the care experience. A prime example is our finding that the two patient satisfaction survey subscales with significant increase regarded the more identifiable elements of “satisfaction in the facility” and “ease of care.” Patient satisfaction was high overall, which is similar to findings from a study by Hochman et al.48 who reported that a PCMH intervention model emphasizing continuity, coordination, and quality of care at a teaching clinic had favorable effects on patient satisfaction. Patient activation was found to decrease from baseline to follow-up in our study, although surveys were completed by different patients and this requires further investigation.
Provider and staff attitudes toward PCMH
Regarding providers and practice staff, our survey analyses identified changes in attitudes and perceptions about PCMH similar to findings from Solimeo et al.,49 where primary care providers were enthusiastic but still noted challenges in aligning PCMH ideals with clinical practice. Our participant providers and staff valued the PCMH concept in principle but were concerned about persistent barriers to implementation and the burden of PCMH recognition (i.e. NCQA) requirements. Our facilitation team worked closely with practice providers and staff to identify, think through, and formulate solutions to barriers, but for some barriers such as understaffing, successful solutions were not forthcoming. All of the practices in our study exhibited progress in some of the tenets associated with successful PCMHs, although each according to its particular circumstances had developed different subsets of these PCMH elements for their innovations.
A study in the Veterans’ Health Administration system found that while survey respondents had an overall positive attitude toward the PCMH, researchers identified multiple barriers including understaffing, low team efficacy, and stressful work environment contributing to higher feelings of burnout.50,51 Stress and burnout are commonplace among providers in the United States, with more than half of those surveyed in 2014 claiming burnout.52 While the PCMH aims to improve practice functioning, our MBI results and other studies demonstrate that the change process itself can wear on providers and staff, and perhaps more so on providers than staff. Designing and implementing PCMH components is hard work, involving modifications in practice culture as well as the mindsets and behaviors of those working in the practice.10,43,46
Using an electronic health record is a prerequisite for participation in PCMH initiatives to facilitate reporting and population health initiatives, and the clerical burden that technology has been shown to impose escalates provider burnout in the outpatient setting.53–55 It is unclear, therefore, if the increase in burnout in our study was less due to the transformation efforts associated with our PCMH initiative (which encouraged practices to identify their needs and choose their own areas for transformation work), than it was to the demands of electronic health records, other operational challenges, and several of the practices’ affiliating with more structurally demanding state-wide PCMH projects. During the course of our study, several of these practices joined Rhode Island’s all-payer PCMH initiative that provided payments for intensive documentation and reporting for specific patient outcome benchmarks. Other factors outside the scope of our intervention were staffing and workflow challenges which can diminish the positive benefits of implementing particular PCMH components, such as effective teamwork and morning huddles.56–58
The presence of engaged PCMH leaders within the practice is a basic necessity for achieving transformation,59 and as others have found,60 provider and staff engagement beyond the designated PCMH champions was a challenge to achieve and sustain in our larger practices. Some PCMH features such as routinized medication reconciliation or morning huddles were deemed by providers and staff in our study to enhance quality; while some requirements such as the process of NCQA application were seen as consuming time that could be better spent doing direct patient care. As Wagner et al.59 assert, PCMH transformation is necessarily disruptive to the work of providing patient care. Wagner’s study of three practices that successfully underwent transformation found that the primary motivator for engagement with the process was their desire to improve quality of care and patient or provider experience, rather than the financial incentive. Similarly, as the practices in our study received only a small, one-time payment, we sought to recruit practices inherently interested in enhancing patient-centered care to improve the experiences of receiving and delivering quality care.
PCMH in varying types of teaching practices
The practices in our study were teaching practices of several different types. Our transformation time-frame occurred relatively early on in PCMH adoption in the United States, and as Clay et al.61 note, teaching about PCMH while providers and staff are still learning about the concepts has substantial challenges. It is also essential to consider the impact of residency or medical student training on PCMH transformation62 and how hosting students and trainees in private teaching practices may impact the practices’ ability to engage in the labor and resource intensive process of PCMH implementation. What has become clear over time is that new educational models are required to adequately equip faculty and learners to practice effectively in medical homes, including the use of panel management and other population health strategies.63–69
Limitations
This study has several limitations. Evaluation of patient clinical outcomes was beyond the scope of this project. We did not document the specific doses of each aspect of the facilitation that individual practices received. Many of the providers and staff were the same at baseline and follow-up but not all were the same due to staff changeover. Patients who participated at baseline were not the same patients at the follow-up time point. Each practice underwent a unique transformation process, and the study design did not include providing recruited practices with per-member/per-month payment for achievement of clinical benchmarks. While provision of such payment is typical of many PCMH transformation efforts, a strength of our approach is that our study was not tied to an a priori set of outcomes. Each practice underwent a unique change process driven by its own needs and so progress among practices was not comparable; however, this strategy allowed our facilitation team to tailor their work with practices and focus on the PCMH components that each practice deemed to be critical. Finally, our quantitative findings are based on results obtained from eight practices; to increase the power of our findings will require a larger number of practices for further evaluation.
Conclusion
PCMH transformation in our participating practices took different routes and focused on different types of changes. Despite these differences, themes indicating both the on-going challenges and potential rewards of PCMH transformation endeavors emerged. Strong, practice-wide communication about on-going transformation plans and newly implemented protocols, as well as maintaining provider and staff engagement can be problematic but are essential for fostering sustained PCMH efforts. At the same time, when chronic understaffing occurs in primary care practices, the ability and interest of staff to “work to the top of their license” is impeded. Internalization of exactly what PCMH is remains difficult, as varying conceptualizations about the concept and its processes persist. In addition, patient engagement is an acknowledged component of importance that is challenging to implement adequately. At this time, PCMH initiatives and evaluation studies are widespread, yet objectives for the PCMH continue to evolve.7 With continuing development of PCMH facilitation, implementation and whole systems evaluation approaches, the benefits of PCMH may eventually come to outweigh the tribulations of transformation processes that have led to provider and staff burnout and persisting frustration with the concept of PCMH as a whole.
Supplemental Material
Supplemental material, Brown_Adult_patient_interview_questions for What matters in patient-centered medical home transformation: Whole system evaluation outcomes of the Brown Primary Care Transformation Initiative by Roberta E Goldman, Joanna Brown, Patricia Stebbins, Donna R Parker, Victoria Adewale, Renee Shield, Mary B Roberts, Charles B Eaton and Jeffrey M Borkan in SAGE Open Medicine
Supplemental Material
Supplemental material, Brown_Process_evaluation_focus_group_questions for What matters in patient-centered medical home transformation: Whole system evaluation outcomes of the Brown Primary Care Transformation Initiative by Roberta E Goldman, Joanna Brown, Patricia Stebbins, Donna R Parker, Victoria Adewale, Renee Shield, Mary B Roberts, Charles B Eaton and Jeffrey M Borkan in SAGE Open Medicine
Supplemental Material
Supplemental material, Brown_provider_and_staff_interview_questions.pdf for What matters in patient-centered medical home transformation: Whole system evaluation outcomes of the Brown Primary Care Transformation Initiative by Roberta E Goldman, Joanna Brown, Patricia Stebbins, Donna R Parker, Victoria Adewale, Renee Shield, Mary B Roberts, Charles B Eaton and Jeffrey M Borkan in SAGE Open Medicine
Acknowledgments
The authors would like to thank all of the providers, staff, and patients in the participating primary care practices who collaborated with them on this project, and who gave them access to the inner workings of their practices to understand their PCMHs in the context of change. They would also like to thank the attendees of the Brown Evaluation and Transformation Think Tanks for their contributions to the creative discussions that the authors considered as they designed this project.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Memorial Hospital of Rhode Island Institutional Review Board, approval #11-24.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Health Resources and Services Administration (HRSA), grant no. 1D54HP20675-01-00.
Informed consent: Written informed consent was obtained from all patients, providers, and staff prior to the qualitative interviews. The authors initially prepared written consents for the surveys as well, and submitted them to the IRB committee for review. The Memorial Hospital of Rhode Island, in its full board review, then deemed the de-identified surveys that also did not collect any protected health information, to not require written consent.
ORCID iD: Roberta E Goldman  https://orcid.org/0000-0001-7801-0530
https://orcid.org/0000-0001-7801-0530
References
- 1. Blubaugh S. The patient-centered medical home. Part I: a primer. J Med Pract Manage 2016; 31: 346–350. [PubMed] [Google Scholar]
- 2. Angelotti M, Bliss K, Schiffman D, et al. Transforming the primary care training clinic: New York State’s Hospital Medical Home demonstration pilot. J Grad Med Educ 2015; 7: 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Applequist J, Miller-Day M, Cronholm PF, et al. “In principle we have agreement, but in practice it is a bit more difficult”: obtaining organizational buy-in to patient-centered medical home transformation. Qual Health Res 2017; 27: 909–922. [DOI] [PubMed] [Google Scholar]
- 4. Flieger SP. Implementing the patient-centered medical home in complex adaptive systems: becoming a relationship-centered patient-centered medical home. Health Care Manage Rev 2017; 42: 112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goldman RE, Parker DR, Brown J. Recommendations for a mixed methods approach to evaluating the patient-centered medical home. Ann Fam Med 2015; 13: 168–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patient-Centered Primary Care Collaborative. Joint principles of the Patient-Centered Medical Home, http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf (2007, accessed 24 March 2016).
- 7. Patient-Centered Primary Care Collaborative. Shared principles of primary care, https://www.pcpcc.org/sites/default/files/Shared_Principles_of_Primary_Care.pdf (2017, accessed 10 September 2017).
- 8. Wagner EH, Coleman K, Reid RJ, et al. The changes involved in patient-centered medical home transformation. Prim Care 2012; 39: 241–259. [DOI] [PubMed] [Google Scholar]
- 9. Wagner EH, Flinter M, Hsu C, et al. Effective team-based primary care: observations from innovative practices. BMC Fam Pract 2017; 18: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lieberthal RD, Karagiannis T, Bilheimer E, et al. Exploring variation in transformation of primary care practices to patient-centered medical homes: a mixed methods approach. Popul Health Manag 2017; 20: 411–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Quigley DD, Predmore ZS, Chen AY, et al. Implementation and sequencing of practice transformation in urban practices with underserved patients. Qual Manag Health Care 2017; 26: 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff 2008; 27: 759–769. [DOI] [PubMed] [Google Scholar]
- 13. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014; 12: 573–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jabbarpour Y, DeMarchis E, Bazemore A, et al. The impact of primary care practice transformation on cost, quality, and utilization: a systematic review of research published in 2016. Patient Centered Primary Care Collaborative/The Robert Graham Center, https://www.pcpcc.org/sites/default/files/resources/pcmh_evidence_report_08-1-17%20FINAL.pdf (2017, accessed 5 October 2017).
- 15. Howard J, Etz RS, Crocker JB, et al. Maximizing the Patient-Centered Medical Home (PCMH) by choosing words wisely. J Am Board Fam Med 2016; 29: 248–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stout S, Weeg S. The practice perspective on transformation: experience and learning from the frontlines. Med Care 2014; 52(11 Suppl. 4): S23–S25. [DOI] [PubMed] [Google Scholar]
- 17. Alexander JA, Bae D. Does the patient-centred medical home work? A critical synthesis of research on patient-centred medical homes and patient-related outcomes. Health Serv Manage Res 2012; 25: 51–59. [DOI] [PubMed] [Google Scholar]
- 18. Hoff T. The patient-centered medical home: what we need to know more about. Med Care Res Rev 2010; 67: 383–392. [DOI] [PubMed] [Google Scholar]
- 19. Pourat N, Charles SA, Snyder S. Availability of care concordant with patient-centered medical home principles among those with chronic conditions: measuring care outcomes. Med Care 2016; 54: 262–268. [DOI] [PubMed] [Google Scholar]
- 20. Schmidt LA, Rittenhouse DR, Wu KJ, et al. Transforming primary care in the New Orleans safety-net: the patient experience. Med Care 2013; 51: 158–164. [DOI] [PubMed] [Google Scholar]
- 21. Doolittle BR, Tobin D, Genao I, et al. Implementing the patient-centered medical home in residency education. Educ Health 2015; 28: 74–78. [DOI] [PubMed] [Google Scholar]
- 22. Fernald DH, Deaner N, O’Neill C, et al. Overcoming early barriers to PCMH practice improvement in family medicine residencies. Fam Med 2011; 43: 503–509. [PubMed] [Google Scholar]
- 23. Weir SS, Page C, Newton WP. Continuity and access in an academic family medicine center. Fam Med 2016; 48: 100–107. [PubMed] [Google Scholar]
- 24. Rabatin J, Williams E, Baier Manwell L, et al. Predictors and outcomes of burnout in primary care physicians. J Prim Care Community Health 2016; 7: 41–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lewis SE, Nocon RS, Tang H, et al. Patient-centered medical home characteristics and staff morale in safety net clinics. Arch Intern Med 2012; 172: 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reid RJ, Fishman PA, Yu O, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care 2009; 15: e71–e87. [PubMed] [Google Scholar]
- 27. Arndt BG, Beasley JW, Watkinson D, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 15: 419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parker DR, Goldman RE, Brown J, et al. The Brown Primary Care Initiative design for strategies towards patient-centered medical home practice transformation. Prim Health Care 2014; 4: 173. [Google Scholar]
- 29. National Committee on Quality Assurance (NCQA). Patient-centered medical home recognition, http://www.ncqa.org/Programs/Recognition/Practices/PatientCenteredMedicalHomePCMH.aspx (accessed 19 March 2010).
- 30. Alexander JA, Paustian M, Wise CG, et al. Assessment and measurement of patient-centered medical home implementation: the BCBSM experience. Ann Fam Med 2013; 11(Suppl. 1): S74–S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Crabtree BF, Chase SM, Wise CG, et al. Evaluation of patient centered medical home practice transformation initiatives. Med Care 2011; 49: 10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosenthal MB, Beckman HB, Forrest DD, et al. Will the patient-centered medical home improve efficiency and reduce costs of care? A measurement and research agenda. Med Care Res Rev 2010; 67: 476–484. [DOI] [PubMed] [Google Scholar]
- 33. Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med 2010; 25: 601–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tomoaia-Cotisel A, Scammon DL, Waitzman NJ, et al. Context matters: the experience of 14 research teams in systematically reporting contextual factors important for practice change. Ann Fam Med 2013; 11(Suppl. 1): S115–S123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Maslach C, Jackson S, Leiter M. Maslach burnout inventory, http://www.mindgarden.com/products/mbi.htm (1996, accessed 29 October 2014).
- 36. Insignia Health. Patient activation measure (PAM), http://www.insigniahealth.com/solutions/patient-activation-measure (2016, accessed 12 September 2017).
- 37. Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the patient activation measure. Health Serv Res 2005; 40(6 Pt 1): 1918–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hibbard JH, Stockard J, Mahoney ER, et al. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004; 39(4 Pt 1): 1005–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kuzel A. Sampling for qualitative research. In: Crabtree BF, Miller WL. (eds) Doing qualitative research. 2nd ed. Thousand Oaks, CA: SAGE, 1999, pp. 33–45. [Google Scholar]
- 40. Borkan J. Immersion/crystallization. In: Crabtree BF, Miller WL. (eds) Doing qualitative research. 2nd ed. Thousand Oaks, CA: SAGE, 1999, pp. 179–194. [Google Scholar]
- 41. Harder VS, Long WE, Varni SE, et al. Pediatric-informed facilitation of patient-centered medical home transformation. Clin Pediatr 2017; 56: 564–570. [DOI] [PubMed] [Google Scholar]
- 42. Hoff T. Medical home implementation: a sensemaking taxonomy of hard and soft best practices. Milbank Q 2013; 91: 771–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hoff T, Scott S. The strategic nature of individual change behavior: how physicians and their staff implement medical home care. Health Care Manage Rev 2017; 42: 226–236. [DOI] [PubMed] [Google Scholar]
- 44. Mader EM, Fox CH, Epling JW, et al. A practice facilitation and academic detailing intervention can improve cancer screening rates in primary care safety net clinics. J Am Board Fam Med 2016; 29: 533–542. [DOI] [PubMed] [Google Scholar]
- 45. Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med 2010; 8(Suppl. 1): S33–S44; S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rissi JJ, Gelmon S, Saulino E, et al. Building the foundation for health system transformation: Oregon’s Patient-Centered Primary Care Home program. J Public Health Manag Pract 2015; 21: 34–41. [DOI] [PubMed] [Google Scholar]
- 47. Tung EL, Gao Y, Peek ME, et al. Patient experience of chronic illness care and medical home transformation in safety net clinics. Health Serv Res 2017; 53: 469–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hochman ME, Asch S, Jibilian A, et al. Patient-centered medical home intervention at an internal medicine resident safety-net clinic. JAMA Intern Med 2013; 173: 1694–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Solimeo SL, Stewart KR, Stewart GL, et al. Implementing a patient centered medical home in the Veterans Health Administration: perspectives of primary care providers. Healthcare 2014; 2: 245–250. [DOI] [PubMed] [Google Scholar]
- 50. Helfrich CD, Dolan ED, Simonetti J, et al. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. J Gen Intern Med 2014; 29(Suppl. 2): S659–S666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ladebue AC, Helfrich CD, Gerdes ZT, et al. The experience of Patient Aligned Care Team (PACT) members. Health Care Manage Rev 2016; 41: 2–10. [DOI] [PubMed] [Google Scholar]
- 52. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90: 1600–1613. [DOI] [PubMed] [Google Scholar]
- 53. Friedberg MW, Chen PG, Van Busum KR, et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy, https://www.rand.org/pubs/research_reports/RR439.html (2013, accessed 7 July 2017). [PMC free article] [PubMed]
- 54. Pelland KD, Baier RR, Gardner RL. “It’s like texting at the dinner table”: a qualitative analysis of the impact of electronic health records on patient-physician interaction in hospitals. J Innov Health Inform: 2017; 24: 894. [DOI] [PubMed] [Google Scholar]
- 55. Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA 2017; 317: 901–902. [DOI] [PubMed] [Google Scholar]
- 56. Helfrich CD, Dolan ED, Fihn SD, et al. Association of medical home team-based care functions and perceived improvements in patient-centered care at VHA primary care clinics. Healthcare 2014; 2: 238–244. [DOI] [PubMed] [Google Scholar]
- 57. Helfrich CD, Sylling PW, Gale RC, et al. The facilitators and barriers associated with implementation of a patient-centered medical home in VHA. Implement Sci 2016; 11: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Tuepker A, Kansagara D, Skaperdas E, et al. “We’ve not gotten even close to what we want to do”: a qualitative study of early patient-centered medical home implementation. J Gen Intern Med 2014; 29(Suppl. 2): S614–S622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wagner EH, Gupta R, Coleman K. Practice transformation in the safety net medical home initiative: a qualitative look. Med Care 2014; 52(11 Suppl. 4): S18–S22. [DOI] [PubMed] [Google Scholar]
- 60. Bleser WK, Miller-Day M, Naughton D, et al. Strategies for achieving whole-practice engagement and buy-in to the patient-centered medical home. Ann Fam Med 2014; 12: 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Clay MA, II, Sikon AL, Lypson ML, et al. Teaching while learning while practicing: reframing faculty development for the patient-centered medical home. Acad Med 2013; 88: 1215–1219. [DOI] [PubMed] [Google Scholar]
- 62. Reid A, Baxley E, Stanek M, et al. Practice transformation in teaching settings: lessons from the I3 PCMH collaborative. Fam Med 2011; 43: 487–494. [PubMed] [Google Scholar]
- 63. Anandarajah G, Furey C, Chandran R, et al. Effects of adding a new PCMH block rotation and resident team to existing longitudinal training within a certified PCMH: primary care residents’ attitudes, knowledge, and experience. Adv Med Educ Pract 2016; 7: 457–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bitton A, Pereira AG, Smith CS, et al. The EFECT framework for interprofessional education in the patient centered medical home. Healthcare 2013; 1: 63–68. [DOI] [PubMed] [Google Scholar]
- 65. Chandran R, Furey C, Goldberg A, et al. Training family medicine residents to build and remodel a patient centered medical home in Rhode Island: a team based approach to PCMH education. R I Med J 2014; 98: 35–41. [PubMed] [Google Scholar]
- 66. Eiff MP, Waller E, Fogarty CT, et al. Faculty development needs in residency redesign for practice in patient-centered medical homes: a P4 report. Fam Med 2012; 44: 387–395. [PubMed] [Google Scholar]
- 67. El Rayess F, Goldman R, Furey C, et al. Patient-centered medical home knowledge and attitudes of residents and faculty: certification is just the first step. J Grad Med Educ 2015; 7: 580–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kayingo G, Gilani O, Kidd VD, et al. Patient-centered medical home exposure and its impact on pa career intentions. Fam Med 2015; 48: 725–730. [PubMed] [Google Scholar]
- 69. Kozakowski SM, Eiff MP, Green LA, et al. Five key leadership actions needed to redesign family medicine residencies. J Grad Med Educ 2015; 7: 187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Brown_Adult_patient_interview_questions for What matters in patient-centered medical home transformation: Whole system evaluation outcomes of the Brown Primary Care Transformation Initiative by Roberta E Goldman, Joanna Brown, Patricia Stebbins, Donna R Parker, Victoria Adewale, Renee Shield, Mary B Roberts, Charles B Eaton and Jeffrey M Borkan in SAGE Open Medicine
Supplemental material, Brown_Process_evaluation_focus_group_questions for What matters in patient-centered medical home transformation: Whole system evaluation outcomes of the Brown Primary Care Transformation Initiative by Roberta E Goldman, Joanna Brown, Patricia Stebbins, Donna R Parker, Victoria Adewale, Renee Shield, Mary B Roberts, Charles B Eaton and Jeffrey M Borkan in SAGE Open Medicine
Supplemental material, Brown_provider_and_staff_interview_questions.pdf for What matters in patient-centered medical home transformation: Whole system evaluation outcomes of the Brown Primary Care Transformation Initiative by Roberta E Goldman, Joanna Brown, Patricia Stebbins, Donna R Parker, Victoria Adewale, Renee Shield, Mary B Roberts, Charles B Eaton and Jeffrey M Borkan in SAGE Open Medicine