Abstract
Background:
An anterior cruciate ligament (ACL) rupture is a serious injury that can be career-ending in collegiate athletics. A rerupture after primary ACL reconstruction occurs in 1% to 11% of all athletes.
Purpose:
To describe the epidemiology of recurrent ACL ruptures in the 25 National Collegiate Athletic Association (NCAA) sports in the NCAA Injury Surveillance Program (ISP) and to identify and compare sport-specific risk factors for a recurrent ACL rupture.
Study Design:
Descriptive epidemiology study.
Methods:
Athletes who experienced a primary or recurrent ACL rupture between 2004 and 2014 were identified using data from the NCAA ISP. ACL ruptures occurred in 12 of 25 sports during the study period. We assessed the rates and patterns of primary and recurrent ACL ruptures and reported them as events per 10,000 athlete-exposures (AEs). Sex-comparable sports were compared using rate ratios. Rupture rates were compared using odds ratios, with P values <.05 indicating significance. Regular-season and postseason data were combined because of low counts of postseason events.
Results:
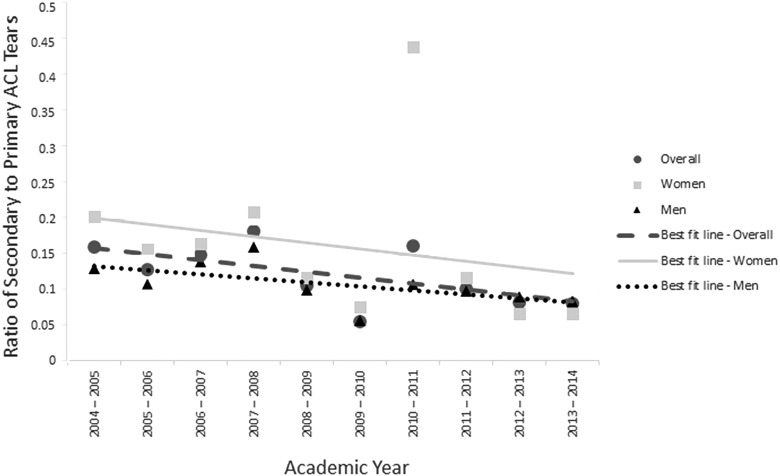
Of 350,416 AEs, there were 1105 ACL ruptures, 126 of which were recurrent. The highest rates of recurrent ACL ruptures (per 10,000 AEs) were among male football players (15), female gymnasts (8.2), and female soccer players (5.2). Of sports played by athletes of both sexes, women’s soccer had a significantly higher rate of recurrent ACL ruptures than men’s soccer (rate ratio, 3.8 [95% CI, 1.3-15]). Among all sports, men had a significantly higher rate of recurrent ACL ruptures (4.3) than women (3.0) (P = .04). Overall, the ratio of recurrent to primary ACL ruptures decreased over the 10-year study period. Both women and men had a decreasing trend of recurrent to primary ACL ruptures, although women had a steeper decrease.
Conclusion:
These data can help identify athletes who are most at risk of recurrent ACL ruptures after ACL reconstruction and who may benefit from injury prevention programs.
Keywords: anterior cruciate ligament, Injury Surveillance Program, National Collegiate Athletic Association, primary rupture, recurrent rupture
Anterior cruciate ligament (ACL) ruptures are among the most commonly studied injuries in orthopaedic research. The incidence of ACL ruptures is estimated to range from 30 to 78 per 100,000 person-years.5,13,15,18,27,28,37 After ACL reconstruction, 61% to 89% of athletes successfully return to sports,8,26,30,39 typically at 8 to 18 months after reconstruction, depending on the level of play.26,29,30 An analysis of National Collegiate Athletic Association (NCAA) Injury Surveillance Program (ISP) data from 1988 to 2004 showed that the highest rates of ACL ruptures occurred in women’s gymnastics, women’s basketball, women’s soccer, and men’s football.17 Using ISP data, a recent study compared the rate of ACL ruptures during the period 1988-2004 with 2004-2013; the authors found an 88% decrease in ACL ruptures among female gymnasts, a 64% decrease among female soccer players, and modest decreases among male football players and female basketball players.1
After primary ACL reconstruction, a rerupture can be devastating. The reported rate of ACL reruptures range from 1% to 11%.§ Reruptures may be caused by traumatic reinjuries, biologic graft failure, or technical surgical errors.9,36 A large prospective multicenter study showed that the most common cause of a rerupture is a noncontact injury to the ACL graft, which constitutes 55% of reruptures treated with revision ACL reconstruction.9 Because of the high costs of surgery and rehabilitation and the substantial time needed for rehabilitation, primary and recurrent ACL ruptures represent a major economic burden10,16 and may end the careers of college athletes. Compared with NCAA athletes who begin their collegiate careers with surgery-naïve knees, those who have undergone knee surgery before college matriculation have a significantly higher rate of repeat ipsilateral knee surgery during their collegiate athletic careers, but this rate has not been previously analyzed by sex or sport.21,43
Despite the physical and economic burdens of ACL reruptures, there are few current epidemiological data on such injuries among college athletes. The aim of this study was to describe the epidemiology of recurrent ACL ruptures in NCAA championship sports using data from the ISP and to compare the risk factors for a recurrent ACL rupture by sport, player sex, event type (practice vs competition), and season (preseason vs regular season/postseason).
Methods
This study was deemed exempt from institutional review board approval.
Data Collection
ACL rupture data were obtained from the ISP database for the 2004-2005 to 2013-2014 academic years for 25 men’s and women’s collegiate sports.22 The ISP data collection methods have been described.22 The ISP includes 25 sports from each of 3 competitive divisions. Athletic trainers log the number of student-athletes participating in each school-sanctioned practice or competition as well as injuries sustained. This does not include injuries sustained outside of sanctioned events, practices, and competitions. Data are reported using an electronic health record application by the medical staff throughout the academic year as part of daily clinical practice. Data are then transferred to the Datalys Center for Sports Injury Research and Prevention’s server, where identifying information is removed and relevant variables and values are retained and released.22
Deidentified common data elements are extracted and subjected to an automated verification process. Data that are flagged as inconsistent or invalid are reassessed by the athletic trainers and quality-assurance staff, who work together to resolve all issues. A reportable injury is defined as one resulting from participation in an organized intercollegiate practice or competition that required attention from a physician or athletic trainer. A reportable athlete-exposure (AE) is defined as 1 athlete participating in 1 NCAA-sanctioned practice or competition in which the athlete was exposed to the possibility of an injury, regardless of the duration of the athlete’s participation. Only athletes with playing time during a competition are included in competition exposures.22
Primary ACL ruptures were defined as those occurring in knees with no history of ACL ruptures. Recurrent ACL ruptures were defined as those occurring in the same knee as a previously treated ACL rupture.
Statistical Analysis
The rates and patterns of ACL ruptures during sanctioned collegiate sporting events were analyzed. The numbers of primary and recurrent ACL ruptures per 10,000 AEs were stratified by sport, event (practice vs competition), and season (preseason, regular season, or postseason). Because of low postseason event counts, rate ratios (RRs) comparing rates between the preseason and the combined regular season and postseason were assessed. RRs (with 95% CIs) were calculated to compare primary versus recurrent ACL rupture rates, preseason versus regular-season/postseason rates, practice versus competition rates, and rates by sport. The rate was calculated using the number of ACL ruptures and number of AEs by sport and is reported as number per 10,000 AEs. For sex-comparable sports (eg, men’s and women’s basketball), rates were compared between sexes by calculating RRs and using odds ratios (ORs) to examine differences between primary versus recurrent ACL ruptures. We were unable to make this comparison using preseason ice hockey and soccer data because of the absence of recurrent ACL ruptures among female ice hockey players and male soccer players during the preseason.
Data on primary and recurrent ACL ruptures were stratified by academic year and sex. The ratio of recurrent to primary ACL ruptures among men’s and women’s sports was also calculated by year, and a linear regression best-fit model was used to determine the trend of change in the ratio of recurrent to primary ACL ruptures during the 10-year study period.
We evaluated the risk factors for a recurrent ACL rupture among NCAA athletes and calculated ORs to assess whether season (preseason vs regular season/postseason) or event type (practice vs competition) was associated with a recurrent ACL rupture. These data were further stratified by sex.
All 95% CIs not containing 1.0 were considered statistically significant. ORs were considered significant if P < .05. Data were analyzed using MedCalc software (version 17.5.5; MedCalc Software).
Results
Overall Frequencies and Rates
The following 12 sports had athletes who sustained ACL ruptures: men’s and women’s basketball, ice hockey, lacrosse, and soccer; men’s football; and women’s field hockey, gymnastics, and volleyball. During the study period, 1105 ACL ruptures (979 primary and 126 recurrent) and 350,416 AEs were reported, for a rupture rate of 32 per 10,000 AEs. One athlete was excluded because of a lack of ACL injury data. Of all ACL injuries, 126 (11%) were recurrent. Most of the recurrent ACL ruptures occurred in men’s football (41%, n = 52), women’s soccer (15%, n = 19), and women’s basketball (13%, n = 17). The highest rates (per 10,000 AEs) of recurrent ACL ruptures were in men’s football (15), women’s gymnastics (8.2), and women’s soccer (5.2) (Table 1).
TABLE 1.
Rate of Anterior Cruciate Ligament Ruptures by Sporta
| Sport | All Rupture | Primary Rupture | Recurrent Rupture |
|---|---|---|---|
| Basketball | |||
| Men’s | 11 (8.6-14) | 9.6 (7.4-12) | 1.4 (0.7-2.6) |
| Women’s | 27 (23-31) | 24 (21-29) | 2.6 (1.6-4.1) |
| Gymnastics (women’s) | 34 (23-50) | 26 (16-40) | 8.2 (3.3-17) |
| Ice hockey | |||
| Men’s | 8.3 (5.2-13) | 7.4 (4.5-12) | 0.9 (0.1-3.2) |
| Women’s | 4.5 (1.7-10) | 4.5 (1.7-10) | 0.0 (0.0-0.0) |
| Field hockey (women’s) | 21 (13-31) | 16 (9.8-26) | 4.1 (1.3-9.9) |
| Football (men’s) | 152 (139-165) | 137 (125-149) | 15 (11-19) |
| Lacrosse | |||
| Men’s | 42 (31-55) | 39 (29-52) | 2.6 (0.7-7.1) |
| Women’s | 44 (34-56) | 39 (30-51) | 3.6 (1.3-8.1) |
| Soccer | |||
| Men’s | 9.5 (6.4-14) | 8.1 (5.3-12) | 1.4 (0.4-3.3) |
| Women’s | 22 (18-28) | 17 (13-22) | 5.2 (3.2-7.9) |
| Volleyball (women’s) | 8.3 (5.9-11) | 7.4 (5.2-10) | 0.9 (0.3-2.2) |
aData are shown as number of ruptures per 10,000 athlete-exposures (95% CI).
During the study period, the ratio of recurrent to primary ACL ruptures decreased by 0.85% per year (Figure 1). This decrease was steeper among women than among men, but this difference was not statistically significant (P = .814).
Figure 1.
Ratio of recurrent to primary anterior cruciate ligament (ACL) tears by player sex.
Sport-Specific Analyses
Men’s and Women’s Basketball
There was no significant difference in the rate of recurrent ACL ruptures by sex (P = .12) (Table 2) or in the rate of ACL ruptures by competition versus practice or preseason versus regular season/postseason. Both women and men were more likely to sustain ACL ruptures during competition than during practice, with no significant differences in the rupture rate during the preseason versus regular season/postseason (Table 3).
TABLE 2.
Rate Ratio of Anterior Cruciate Ligament Ruptures in Women Versus Men
| Sport | Primary Rupture | Recurrent Rupture | ||
|---|---|---|---|---|
| Rate Ratio (95% CI) | P Value | Rate Ratio (95% CI) | P Value | |
| Basketball | 2.6 (1.9-3.4) | <.0001a | 1.9 (0.8-4.3) | .12 |
| Ice hockey | 0.6 (0.2-1.7) | .33 | 0.0 (0.0-8.6) | .57 |
| Lacrosse | 1.0 (0.7-1.5) | .99 | 1.4 (0.3-5.8) | .66 |
| Soccer | 2.1 (1.3-3.4) | .0016a | 3.8 (1.3-15) | .02a |
aAchieved statistical significance.
TABLE 3.
Rate of Anterior Cruciate Ligament Ruptures per 10,000 Athlete-Exposures and Odds Ratio of a Rupture Occurring During Competition Versus Practice and Regular Season/Postseason Versus Preseasona
| Sport | Competition vs Practice Rate | Regular Season/Postseason vs Preseason Rate | ||||||
|---|---|---|---|---|---|---|---|---|
| Competition | Practice | OR (95% CI) | P Value | Regular Season/Postseason | Preseason | OR (95% CI) | P Value | |
| Basketball | ||||||||
| Men’s | 25 | 6.3 | 4.0 (2.5-6.5) | <.0001b | 6.3 | 11 | 1.0 (0.6-1.7) | .86 |
| Women’s | 64 | 15 | 4.4 (3.2-5.9) | <.0001b | 15 | 29 | 0.9 (0.6-1.3) | .58 |
| Field hockey (women’s) | 34 | 16 | 2.2 (0.9-5.2) | .09 | 16 | 33 | 0.5 (0.2-1.2) | .13 |
| Football (men’s) | 568 | 88 | 6.8 (5.7-8.1) | <.0001b | 158 | 151 | 1.1 (0.9-1.3) | .61 |
| Gymnastics (women’s) | 129 | 22 | 6.1 (2.7-13.4) | <.0001b | 48 | 19 | 2.5 (1.0-6.0) | .04b |
| Ice hockey | ||||||||
| Men’s | 25 | 1.8 | 14 (4.0-48) | <.0001b | 1.8 | 4.3 | 0.2 (0.1-0.4) | <.0001b |
| Women’s | 10 | 2.5 | 4.1 (0.7-24) | .12 | 2.5 | 0 | 1.7 (0.1-30) | .73 |
| Lacrosse | ||||||||
| Men’s | 94 | 30 | 6.2 (3.5-11) | <.0001b | 30 | 38 | 1.2 (0.6-2.2) | .63 |
| Women’s | 111 | 25 | 4.5 (2.9-7.5) | <.0001b | 25 | 26 | 2.0 (1.1-3.8) | .03b |
| Soccer | ||||||||
| Men’s | 25 | 3.7 | 6.9 (3.0-16) | <.0001b | 3.7 | 2.7 | 7.9 (3.0-21) | <.0001b |
| Women’s | 48 | 13 | 3.8 (2.4-5.8) | <.0001b | 13 | 23 | 1.0 (0.6-1.6) | .88 |
| Volleyball (women’s) | 15 | 6.4 | 2.3 (1.2-4.5) | <.0001b | 6.4 | 9.7 | 0.8 (0.4-1.7) | .58 |
aOR, odds ratio.
bAchieved statistical significance.
Men’s and Women’s Ice Hockey
Among ice hockey players, there were no significant differences between men and women in primary or recurrent ACL ruptures (Table 2). Both women and men were more likely to sustain ACL ruptures during competition versus practice and during the regular season/postseason versus preseason (Table 3).
Men’s and Women’s Lacrosse
Among lacrosse players, there were no significant differences in the rate of primary or recurrent ACL ruptures between men and women (Table 2). Both women and men were more likely to sustain ruptures during competition versus practice, and women were more likely to sustain ruptures during the regular season/postseason versus preseason (Table 3).
Men’s and Women’s Soccer
Women were more likely than men to sustain recurrent ACL ruptures (RR, 3.8 [95% CI, 1.3-15]) (Table 2). Women were also more likely to sustain recurrent ACL ruptures during practice (RR, 11 [95% CI, 1.6-447]) but not during competition, the preseason, or the regular season/postseason. Both women and men were more likely to sustain ACL ruptures during competition than during practice, and men were more likely to sustain ACL ruptures during the regular season/postseason versus preseason (Table 3).
Men’s Football
The overall rate of ACL ruptures was 152 (95% CI, 139-165) per 10,000 AEs, of which there were 15 recurrent ACL ruptures (95% CI, 11-19) per 10,000 AEs. During competition, there were 568 ACL ruptures (95% CI, 503-640) per 10,000 AEs, which was much higher than the practice rate (88/10,000 AEs [95% CI, 78-99]) (OR, 6.8 [95% CI, 5.7-8.1]; P < .0001). The ACL rupture rate was similar during the preseason (151/10,000 AEs [95% CI, 129-176]) versus regular season/postseason (158/10,000 AEs [95% CI, 143-175]) (OR, 1.1 [95% CI, 0.9-1.3]; P = .61) (Table 3).
Women’s Field Hockey
The overall rate of ACL ruptures was 21 (95% CI, 13-31) per 10,000 AEs, of which there were 4.1 recurrent ACL ruptures (95% CI, 1.3-9.9) per 10,000 AEs. The rate of ACL ruptures during competition (34/10,000 AEs [95% CI, 17-62]) was more than double the rate during practice (16/10,000 AEs [95% CI, 8.2-27]) (OR, 2.2 [95% CI, 0.9-5.2]; P = .09). The rate of ACL ruptures during the preseason (33/10,000 AEs [95% CI, 15-62]) was approximately double the rate during the regular season/postseason (16/10,000 AEs [95% CI, 8.9-23]) (OR, 0.5 [95% CI, 0.2-1.2]; P = .13) (Table 3).
Women’s Gymnastics
There were 25 ACL ruptures in women’s gymnastics (19 primary, 6 recurrent) during the 10-year study period. The overall rate of ACL ruptures was 34 (95% CI, 23-50) per 10,000 AEs, of which there were 8.2 recurrent ruptures (95% CI, 3.3-17) per 10,000 AEs. The rate of ACL ruptures during competition (129/10,000 AEs [95% CI, 58-225]) was much higher than the rate during practice (22/10,000 AEs [95% CI, 12-35]) (OR, 6.1 [95% CI, 2.7-13.4] ; P < .0001). The rate of ACL ruptures during the regular season/postseason (48/10,000 AEs [95% CI, 30-75]) was more than double the rate during the preseason (19/10,000 AEs [95% CI, 8.5-38]) (OR, 2.5 [95% CI, 1.0-6.0]; P = .04) (Table 3).
Women’s Volleyball
There were 36 ACL ruptures in women’s volleyball (32 primary, 4 recurrent) during the 10-year study period. The overall rate of ACL ruptures was 8.3 (95% CI, 5.9-11) per 10,000 AEs, of which there were 0.9 recurrent ruptures (95% CI, 0.3-2.2) per 10,000 AEs. The rate of ACL ruptures during competition (15/10,000 AEs [95% CI, 9.7-23]) was more than twice the rate during practice (6.4/10,000 AEs [95% CI, 3.7-11]) (OR, 2.3 [95% CI, 1.2-4.5]; P < .0001). The rate of ACL ruptures did not differ significantly during the preseason versus regular season/postseason (Table 3).
Discussion
We examined the epidemiology of recurrent ACL ruptures in 25 NCAA sports, of which 12 had reported ACL injuries. We found that from the 2004-2005 to 2013-2014 academic years, the rate of recurrent ACL ruptures in many sports (men’s football, women’s gymnastics, and women’s field hockey ) remained high, with women’s soccer players having a significantly higher rate of recurrent ACL ruptures compared with men’s soccer players.
Studies have reported a high incidence of ACL ruptures,5,13,15,18,27,28,37 and recurrent ACL ruptures are potentially career ending. Of professional athletes in the United States who underwent ACL reconstruction, 87% successfully returned to play at a mean 1 year after surgery; however, of the 3.5% who had recurrent ACL ruptures requiring revision surgery, the return-to-play rate was only 50%.8 Okoroha et al31 reported on National Football League (NFL) players who underwent revision ACL reconstruction between 2007 and 2014. They found that of 24 players who underwent surgery, 19 returned to regular-season NFL play at an average of 1 year after surgery. Those who returned to play in the NFL played in significantly fewer games and seasons after surgery than before their recurrent injury.31 Using data from the prospective French ACL Study (FAST), Lefevre et al23 compared return to sport after primary and revision ACL reconstruction. In this cohort, functional scores at 1 year were significantly better in the primary reconstruction group than in the revision reconstruction group. The return-to-sport rate was similar between the 2 groups; however, those who had undergone revision ACL reconstruction were significantly less likely to return to their usual preoperative sport than those who had undergone primary ACL reconstruction.
In addition to the lower rate of return to sports, recurrent ACL injuries carry a risk of long-term functional deficits. A report of ACL ruptures in an orthopaedic sports medicine practice found that at 12 years after revision reconstruction, approximately 28% of patients had sustained a recurrent rupture of the ACL graft.2 Those who had recurrent ACL ruptures had worse International Knee Documentation Committee scores than those with primary ACL reconstructions, with a greater severity of degenerative radiographic changes in the group whose revised ACL reconstructions had reruptured.2
In our study, the highest rates of recurrent ACL ruptures occurred in men’s football, women’s gymnastics, and women’s soccer, whereas the highest rates of primary ACL ruptures occurred in men’s football, men’s and women’s lacrosse, and women’s gymnastics. Previously reported factors associated with a higher risk of recurrent ACL ruptures include higher level of play/level of activity, graft type, and female sex.20,24,38 Our study focused on collegiate athletes; in our study, 1 of 9 ACL ruptures was recurrent. Recurrent ACL ruptures accounted for 14% of ACL ruptures in women and 10% of ACL ruptures in men. All analyzed sports in our study had a higher rate of injuries during competition, except women’s ice hockey and women’s field hockey in which there were no differences in the rupture rate between competition and practice. This propensity toward ACL ruptures during competition has been reported previously,11,12 and it may in part be because of the less predictable environment, greater speed, and greater intensity of competition settings.
Athletes are at greatest risk of sustaining a recurrent ACL rupture at 1 to 2 years after primary surgery.3,25,33,35 The Multicenter ACL Revision Study (MARS) found that 55% of those undergoing revision ACL reconstruction for an ACL rerupture had experienced noncontact mechanisms of an ACL rerupture.9 Research has shown that female athletes have a higher risk of noncontact ACL ruptures than male athletes, with data from the 2004-2014 NCAA ISP cohort indicating that 60% of ACL ruptures in female athletes were caused by a noncontact injury, versus 41% in male athletes.1 Compared with their male counterparts, female athletes tend to have insufficiency in neuromuscular control, with an imbalance of flexibility, coordination, and muscle strength that may predispose them to ACL ruptures7 as well as reruptures of an ACL graft suggesting the potential need for targeted prevention in return-to-play guidelines.
Within sex-comparable sports, we found a 3.8 times higher rate of recurrent ACL ruptures among women’s soccer players compared with men’s soccer players. This may be attributable, in part, to a higher rate of primary ruptures among women than among men either during previous seasons or during high school play before collegiate sport participation.1,19 Allen et al3 described ACL injury recurrence among a cohort of female soccer players, in which 11% of athletes of any level of play presenting to their clinic with an ACL rupture had recurrent ACL tears. Furthermore, significantly more athletes who returned to playing soccer had graft tears compared with those who did not return to the sport.3
Overall, our data provide an approximation that from 2004 to 2014, there was a decreasing trend in the ratio of recurrent to primary ACL ruptures. This may be caused by several factors, including data variations in the methods used to calculate this approximation, improvements in surgical fixation techniques, improved surgical indications, the higher baseline ratio of recurrent to primary ACL ruptures among women than men at the beginning of our study period, and the possible effect of injury prevention programs targeting female athletes.14,34,41,42 The American Academy of Orthopaedic Surgeons recently published appropriate use criteria for ACL injury prevention programs, stating that for appropriate patients, a supervised rehabilitation program can aid in ACL injury prevention.42 Although not studied, it is possible that the implementation of such programs during the 2004-2014 study period may partially account for the decreasing trend observed in the ratio of recurrent to primary ACL ruptures in female athletes compared with male athletes. Further studies on athletes with prior ACL reconstruction should be performed to help determine who may derive the most benefit from injury prevention programs.
Our study has several limitations. The incidence of ACL ruptures during the study period was relatively low, limiting our ability to examine sport-specific differences. Because these are population-level surveillance data, we were unable to account for risk factors that were unrecorded in the data set. We present estimates of rerupture rates because the ISP data did not allow us to follow individual athletes for rupture recurrence. Additionally, athletes whose primary ACL ruptures occurred during their last season of competition could not be followed for recurrent ACL ruptures. However, these estimates allow us to compare sports and risk factors for a recurrent ACL rupture during play in the NCAA.
To calculate the rupture rate, we used AEs, which are defined in independent units without controlling for duration, intensity, or type of sport exposure. Okoroha et al32 showed that among National Basketball Association athletes, the number of exposures and the amount of time played made equal contributions to ACL injury rates. Because the NCAA ISP data set does not identify all athletes with a history of ACL ruptures but only comments on whether an ACL rupture is primary or recurrent, we used AE data for the entire population in calculating the rate of ACL reruptures. Therefore, we may have underestimated rerupture rates. Unfortunately, no individual identifiers are available in the database, so we were unable to assess the rate of contralateral ACL ruptures in patients with previous ACL ruptures.
Athletes with previous ACL ruptures may not perform at the same level or have the same number of AEs as those with injury-naïve knees, adding to the underestimation of rerupture rates. In population surveys, exposure data are useful because they represent the injury risk according to activity. For example, in our data set, an equal incidence of ACL ruptures occurred during men’s football competition and practice; however, based on exposure, there was a significantly higher rupture rate during competition than practice because football players have more practice scenarios than game scenarios during their seasons.
The use of the NCAA ISP database has the inherent limitation of a voluntary, trainer-driven reporting system with no confirmation of data. Last, the ISP data set did not report all injury-specific characteristics such as team-specific attributes (eg, participation in ACL injury prevention programs). If prevention programs were introduced during the study period, they could have influenced injury rates.
Conclusion
Our results indicate that the rate of recurrent ACL ruptures for many sports, including men’s football, women’s gymnastics, and women’s field hockey, remained high. Women’s soccer players had a significantly higher rate of recurrent ACL ruptures compared with men’s soccer players. These data can help identify athletes who are most at risk of recurrent ACL ruptures after ACL reconstruction and who may benefit from injury prevention programs. Further studies are needed to identify the causes of and modifiable risk factors for a recurrent ACL rupture.
Acknowledgment
The NCAA ISP data were provided by the Datalys Center for Sports Injury Research and Prevention. The ISP was funded by the NCAA. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Datalys Center or the NCAA.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval was waived for the present study.
References
- 1. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: National Collegiate Athletic Association Injury Surveillance System data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 2. Ahmed I, Salmon L, Roe J, Pinczewski L. The long-term clinical and radiological outcomes in patients who suffer recurrent injuries to the anterior cruciate ligament after reconstruction. Bone Joint J. 2017;99-B(3):337–343. [DOI] [PubMed] [Google Scholar]
- 3. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 4. Andernord D, Desai N, Bjornsson H, et al. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. [DOI] [PubMed] [Google Scholar]
- 5. Bollen S. Epidemiology of knee injuries: diagnosis and triage. Br J Sports Med. 2000;34(3):227–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. [DOI] [PubMed] [Google Scholar]
- 7. Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med. 2010;44(10):694–697. [DOI] [PubMed] [Google Scholar]
- 8. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen JL, Allen CR, Stephens TE, et al. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med. 2013;41(7):1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. de Loes M, Dahlstedt LJ, Thomee R. A 7-year study on risks and costs of knee injuries in male and female youth participants in 12 sports. Scand J Med Sci Sports. 2000;10(2):90–97. [DOI] [PubMed] [Google Scholar]
- 11. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221–233. [PMC free article] [PubMed] [Google Scholar]
- 12. Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004-2005 through 2008-2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med. 2012;40(5):990–995. [DOI] [PubMed] [Google Scholar]
- 13. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12(6):622–627. [DOI] [PubMed] [Google Scholar]
- 14. Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. [DOI] [PubMed] [Google Scholar]
- 15. Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop. 2009;80(5):563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Herzog MM, Marshall SW, Lund JL, Pate V, Spang JT. Cost of outpatient arthroscopic anterior cruciate ligament reconstruction among commercially insured patients in the United States, 2005-2013. Orthop J Sports Med. 2017;5(1):2325967116684776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 18. Janssen KW, Orchard JW, Driscoll TR, van Mechelen W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003-2004 to 2007-2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports. 2012;22(4):495–501. [DOI] [PubMed] [Google Scholar]
- 19. Joseph AM, Collins CL, Henke NM, et al. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kamath GV, Murphy T, Creighton RA, et al. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42(7):1638–1643. [DOI] [PubMed] [Google Scholar]
- 22. Kerr ZY, Dompier TP, Snook EM, et al. National Collegiate Athletic Association Injury Surveillance System: review of methods for 2004-2005 through 2013-2014 data collection. J Athl Train. 2014;49(4):552–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lefevre N, Klouche S, Mirouse G, et al. Return to sport after primary and revision anterior cruciate ligament reconstruction: a prospective comparative study of 552 patients from the FAST cohort. Am J Sports Med. 2017;45(1):34–41. [DOI] [PubMed] [Google Scholar]
- 24. Liechti DJ, Chahla J, Dean CS, et al. Outcomes and risk factors of rerevision anterior cruciate ligament reconstruction: a systematic review. Arthroscopy. 2016;32(10):2151–2159. [DOI] [PubMed] [Google Scholar]
- 25. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40(7):1551–1557. [DOI] [PubMed] [Google Scholar]
- 26. Mai HT, Chun DS, Schneider AD, et al. Performance-based outcomes after anterior cruciate ligament reconstruction in professional athletes differ between sports. Am J Sports Med. 2017;45(10):2226–2232. [DOI] [PubMed] [Google Scholar]
- 27. Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31(12):1644–1648. [DOI] [PubMed] [Google Scholar]
- 28. Nordenvall R, Bahmanyar S, Adami J, et al. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40(8):1808–1813. [DOI] [PubMed] [Google Scholar]
- 29. Notarnicola A, Maccagnano G, Barletta F, et al. Returning to sport after anterior cruciate ligament reconstruction in amateur sports men: a retrospective study. Muscles Ligaments Tendons J. 2016;6(4):486–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nwachukwu BU, Voleti PB, Berkanish P, et al. Return to play and patient satisfaction after ACL reconstruction: study with minimum 2-year follow-up. J Bone Joint Surg Am. 2017;99(9):720–725. [DOI] [PubMed] [Google Scholar]
- 31. Okoroha KR, Kadri O, Keller RA, et al. Return to play after revision anterior cruciate ligament reconstruction in National Football League players. Orthop J Sports Med. 2017;5(4):2325967117698788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Okoroha KR, Marfo K, Meta F, et al. Amount of minutes played does not contribute to anterior cruciate ligament injury in National Basketball Association athletes. Orthopedics. 2017;40(4):e658–e662. [DOI] [PubMed] [Google Scholar]
- 33. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pfile KR, Curioz B. Coach-led prevention programs are effective in reducing anterior cruciate ligament injury risk in female athletes: a number-needed-to-treat analysis. Scand J Med Sci Sports. 2017;27(12):1950–1958. [DOI] [PubMed] [Google Scholar]
- 35. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. [DOI] [PubMed] [Google Scholar]
- 36. Samitier G, Marcano AI, Alentorn-Geli E, et al. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015;3(4):220–240. [PMC free article] [PubMed] [Google Scholar]
- 37. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 38. Schilaty ND, Bates NA, Sanders TL, et al. Incidence of second anterior cruciate ligament tears (1990-2000) and associated factors in a specific geographic locale. Am J Sports Med. 2017;45(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sepulveda F, Sanchez L, Amy E, Micheo W. Anterior cruciate ligament injury: return to play, function and long-term considerations. Curr Sports Med Rep. 2017;16(3):172–178. [DOI] [PubMed] [Google Scholar]
- 40. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 41. Sugimoto D, Myer GD, Barber Foss KD, et al. Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis. Br J Sports Med. 2016;50(20):1259–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vincent KR, Herman DC. AAOS appropriate use criteria: anterior cruciate ligament injury prevention programs. J Am Acad Orthop Surg. 2017;25(4):e83–e86. [DOI] [PubMed] [Google Scholar]
- 43. Wang D, Rugg CM, Mayer E, et al. Precollegiate knee surgery predicts subsequent injury requiring surgery in NCAA athletes. Am J Sports Med. 2016;44(8):2023–2029. [DOI] [PubMed] [Google Scholar]
- 44. Wasserstein D, Khoshbin A, Dwyer T, et al. Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med. 2013;41(9):2099–2107. [DOI] [PubMed] [Google Scholar]