Abstract
Background
Rising atmospheric carbon dioxide concentrations are anticipated to decrease the zinc and iron concentrations of crops. The associated disease burden and optimal mitigation strategies remain unknown. We sought to understand where and to what extent increasing carbon dioxide concentrations may increase the global burden of nutritional deficiencies through changes in crop nutrient concentrations, and the effects of potential mitigation strategies.
Methods and findings
For each of 137 countries, we incorporated estimates of climate change, crop nutrient concentrations, dietary patterns, and disease risk into a microsimulation model of zinc and iron deficiency. These estimates were obtained from the Intergovernmental Panel on Climate Change, US Department of Agriculture, Statistics Division of the Food and Agriculture Organization of the United Nations, and Global Burden of Disease Project, respectively. In the absence of increasing carbon dioxide concentrations, we estimated that zinc and iron deficiencies would induce 1,072.9 million disability-adjusted life years (DALYs) globally over the period 2015 to 2050 (95% credible interval [CrI]: 971.1–1,167.7). In the presence of increasing carbon dioxide concentrations, we estimated that decreasing zinc and iron concentrations of crops would induce an additional 125.8 million DALYs globally over the same period (95% CrI: 113.6–138.9). This carbon-dioxide-induced disease burden is projected to disproportionately affect nations in the World Health Organization’s South-East Asia and African Regions (44.0 and 28.5 million DALYs, respectively), which already have high existing disease burdens from zinc and iron deficiencies (364.3 and 299.5 million DALYs, respectively), increasing global nutritional inequalities. A climate mitigation strategy such as the Paris Agreement (an international agreement to keep global temperatures within 2°C of pre-industrial levels) would be expected to avert 48.2% of this burden (95% CrI: 47.8%–48.5%), while traditional public health interventions including nutrient supplementation and disease control programs would be expected to avert 26.6% of the burden (95% CrI: 23.8%–29.6%). Of the traditional public health interventions, zinc supplementation would be expected to avert 5.5%, iron supplementation 15.7%, malaria mitigation 3.2%, pneumonia mitigation 1.6%, and diarrhea mitigation 0.5%. The primary limitations of the analysis include uncertainty regarding how food consumption patterns may change with climate, how disease mortality rates will change over time, and how crop zinc and iron concentrations will decline from those at present to those in 2050.
Conclusions
Effects of increased carbon dioxide on crop nutrient concentrations are anticipated to exacerbate inequalities in zinc and iron deficiencies by 2050. Proposed Paris Agreement strategies are expected to be more effective than traditional public health measures to avert the increased inequality.
In a modeling study Christopher Weyant and colleagues predict reduced crop nutritional content and subsequent health disparities due to increased carbon dioxide levels caused by climate change.
Author summary
Why was this study done?
Increasing atmospheric carbon dioxide concentrations are anticipated to decrease the zinc and iron concentrations of some crops.
The disease burden induced by changes in zinc and iron concentrations in crops, and optimal mitigation strategies, are unknown.
What did the researchers do and find?
We developed a country-level microsimulation model of zinc and iron deficiency to project the health effects of zinc- and iron-deficiency-related diseases in terms of disability-adjusted life years accumulated over the period 2015 to 2050, worldwide.
We estimated that carbon-dioxide-induced reductions in the zinc and iron concentrations of crops would be expected to induce approximately 125.8 million disability-adjusted life years globally over the period from 2015 to 2050, disproportionately affecting South-East Asian and sub-Saharan African countries.
We also estimated that a climate mitigation strategy concordant with the Paris Agreement would avert a greater portion of this burden (approximately 48.2%) than traditional public health interventions (approximately 26.6%).
What do these findings mean?
The effects of increased carbon dioxide concentrations on crop nutrient concentrations may increase existing inequalities in nutritional deficiencies by 2050.
Climate mitigation strategies, such as the Paris Agreement, may be more effective than traditional public health interventions in averting this increased inequality.
Introduction
Increasing atmospheric carbon dioxide concentrations are anticipated to affect public health through increased unsafe weather events, extreme heat, air pollution, and allergen and disease vector exposure [1]. Increasing carbon dioxide concentrations are also anticipated to reduce the concentrations of zinc and iron in many agricultural crops, particularly C3 plants, which rely solely on C3 carbon fixation and include common rice and wheat varieties; C3 plants constitute 95% of terrestrial plants, account for over half of global caloric consumption, and serve as the primary source of dietary zinc and iron for populations at highest risk of nutritional deficiencies [2–5]. The empirical observation of lowered zinc and iron concentrations under elevated carbon dioxide is well established, although the mechanisms are not yet well understood and likely relate in part to changes in crop transpiration [2,5,6]. Zinc and iron deficiencies, in turn, increase the risk of infections, diarrhea, and anemia [7,8]. It remains unclear, however, where and to what degree increasing carbon dioxide concentrations may increase the global burden of nutritional deficiencies, and which strategies may best mitigate the increase. An active area of public health policy debate is whether direct climate change mitigation strategies, such as the Paris Agreement, will be sufficient or comparable to traditional public health measures to combat the complications of carbon-dioxide-induced zinc and iron deficiencies—particularly supplementation and disease control programs to combat the heightened risk of infections, diarrhea, and anemia [9].
The impact of increased carbon dioxide on nutritional deficiencies and their associated diseases depends on 5 related factors: the magnitude of increase in atmospheric carbon dioxide concentrations; the resultant changes in crop nutrient concentrations; current and future trends in consumption of crops and other dietary nutrient sources; the risks of deficiencies, given dietary consumption; and the risks of disease, given nutritional deficiencies.
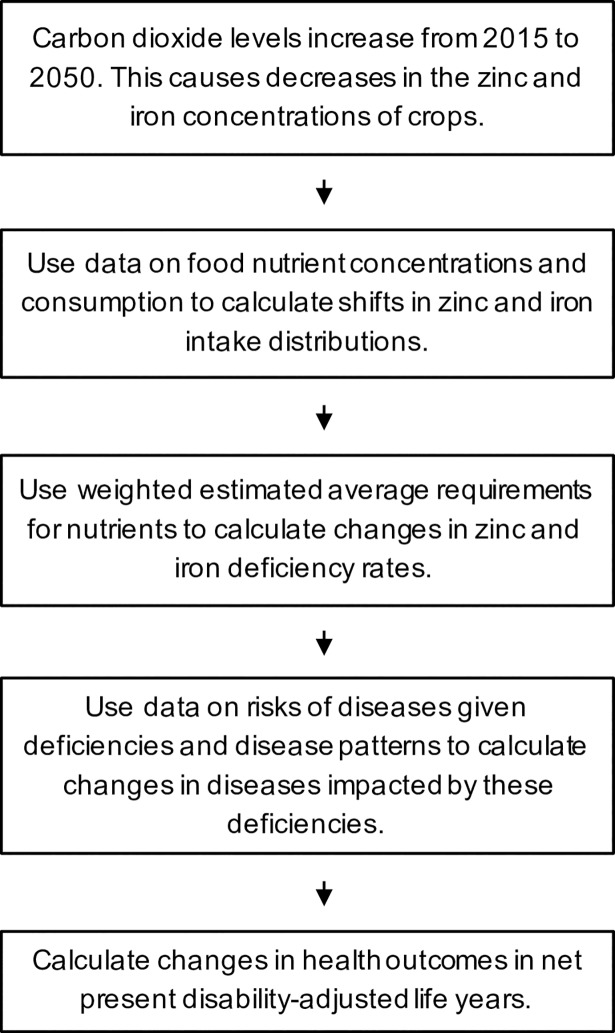
We developed a model (Fig 1) to estimate where and to what degree increasing carbon dioxide concentrations would be expected to increase the global burden of zinc and iron deficiencies and their associated diseases over the period 2015 to 2050. We used this model to evaluate which strategies may best mitigate the burden of disease attributable to increased carbon dioxide in the atmosphere. Specifically, we created a microsimulation in which demographically representative populations in each country were or were not exposed to carbon-dioxide-induced changes in the zinc and iron concentrations of crops, and experienced related disease burdens quantified in disability-adjusted life years (DALYs).
Fig 1. Model schematic.
In the model, increased atmospheric carbon dioxide concentrations decrease the zinc and iron concentrations of crops. Data on food nutrient concentrations and consumption are used to calculate changes in zinc and iron intake distributions. These distributions and weighted estimated average requirements (WtdEARs) for nutrients are used as inputs to a microsimulation, which projects health outcomes due to carbon-dioxide-induced declines in the zinc and iron concentrations of crops.
Methods
Data sources
To estimate the impact of increasing carbon dioxide concentrations on nutritional deficiencies and associated disease rates, we used 5 main data sources. We focused our analysis on country-level estimates of the following: carbon dioxide concentration changes from the Intergovernmental Panel on Climate Change [10], crop zinc and iron concentrations from the US Department of Agriculture (USDA) [11], changes in crop zinc and iron concentrations due to increasing carbon dioxide concentrations from Myers et al. [5], dietary supply from the Statistics Division of the Food and Agriculture Organization of the United Nations (FAOSTAT) [12], and disease prevalence among different populations globally from the Global Burden of Disease Project (GBD) [13]. Example values for Nigeria are shown in Table 1, with links to primary data for other countries in S1 and S2 Texts.
Table 1. Model inputs, with example values from Nigeria.
| Variable | Value | Units | Source |
|---|---|---|---|
| Nutritional requirements | |||
| Zinc required per day (WtdEAR) | 10.33 | mg/capita/day | [14] |
| Iron required per day (WtdEAR) | 18.91 | mg/capita/day | [8,12]* |
| Disease prevalence | |||
| Malaria prevalence | 3.80 × 10−2 | Fraction of population | [13,15]* |
| Pneumonia prevalence | 7.42 × 10−4 | Fraction of population | [13,15]* |
| Diarrhea prevalence | 5.50 × 10−2 | Fraction of population | [13,15]* |
| Disability weights | |||
| Malaria weight | 1.91 × 10−1 | NA | [15] |
| Pneumonia weight | 2.79 × 10−1 | NA | [15] |
| Diarrhea weight | 1.05 × 10−1 | NA | [15] |
| Iron deficiency anemia weight | 3.12 × 10−2 | NA | [8,13]* |
| Relative disease risks | |||
| RR malaria given zinc deficient | 1.56 | NA | [7] |
| RR pneumonia given zinc deficient | 1.52 | NA | [7] |
| RR diarrhea given zinc deficient | 1.28 | NA | [7] |
*Calculated value.
NA, not applicable; RR, relative risk; WtdEAR, weighted estimated average requirement.
Model structure
We incorporated the data into a microsimulation model (Fig 1) that simulates individuals within each country, reflecting the range of consumption of zinc and iron given the variations in dietary patterns in each country, and associated zinc and iron deficiency status and attendant risks for infections, diarrhea, and anemia. For each of 137 countries with data, we simulated 2 identical samples of 10,000 individuals demographically distributed to match country-specific age, sex, and secular birth/death trends. Each individual was probabilistically given values of zinc and iron consumption, morbidity risk, and mortality risk (Table 1; Fig 1). One population sample was subjected to carbon-dioxide-induced declines in the zinc and iron concentrations of crops while the other maintained current levels of zinc and iron concentrations. The primary model outcome was the difference between the 2 populations in DALYs per 1,000 persons. DALYs are the sum of years of life lost from disease and years of life lived with disability, weighted by the disability associated with each disease endpoint (Table 1).
In the simulation, we assumed that current dietary patterns (number of kilocalories/capita/day consumed of each food category) would remain the same despite increasing carbon dioxide concentrations, meaning that individuals would not adjust their total intake of food, or types of food eaten, based on reduction in nutrients in each crop. Average food consumption per capita in each country was determined from FAOSTAT data on approximately 100 mutually exclusive and collectively exhaustive food categories, such as potatoes, bovine meat, and beans [12]. The baseline zinc and iron contents per 100 grams and energy density of each food type were obtained from USDA data [11]. Country-specific zinc consumption distributions were constructed assuming normality and coefficients of variation (CVs) of 25% [16–18]. This method of constructing zinc consumption distributions from FAOSTAT and USDA data is similar to that used by Kumssa et al. [14]. Country-specific iron consumption distributions were also constructed assuming normality and CVs of 25% following prior literature [16]. An alternative assumption for iron consumption distributions, lognormality with CVs of 40% [19], was applied in sensitivity analysis (S4 Text). The annual crop-specific declines in zinc and iron concentrations due to increasing carbon dioxide were estimated from nutrient concentrations of crops grown under carbon dioxide concentrations expected by the year 2050 [5] with assumed linear declines in crop concentrations over the period from 2015 to 2050. The expected carbon dioxide concentrations by the year 2050 used in [5] are based on the Intergovernmental Panel on Climate Change’s assessment of carbon dioxide concentration projections [10], which are the same in all countries. Specifically, projected declines in the micronutrient concentrations of particular crops were extrapolated to broader crop categories, in keeping with previous studies (S1 Text) [9,20].
Given the annual level of zinc and iron consumed by each simulated individual, we determined whether an individual fell below a critical threshold level of zinc or iron intake that would be labeled “deficiency” and would predispose the individual to disease, using the estimated average requirement cut-point method [21–23], which compares a person’s average annual intake to the corresponding weighted estimated average requirement (WtdEAR). A WtdEAR is an average micronutrient requirement for a population and can be calculated by multiplying the requirement for each demographic group by the fraction of people in that demographic group and summing; the requirement for each demographic group is based on population-specific absorption factors [24].
The microsimulation model estimated the total morbidity and mortality burden associated with zinc and iron deficiencies per 1,000 people and for the overall population in each country. Zinc deficiency is associated with a heightened relative risk of morbidity and mortality from malaria, pneumonia, and diarrhea among children under 5 years, with no heightened disease risks among older persons [7]; the disability weights attributable to each of these conditions were obtained from prior assessments (Table 1) [8,13,15]. Prevalence rates, mortality rates, and trends over time for malaria, pneumonia, and diarrhea in each country were obtained from the GBD [13]. Mortality trends assumed continuation of the annual percent change in the per capita mortality for each disease as calculated by the GBD. The GBD calculated these values based on historical data from 1990 to 2013. Similarly, disease prevalence trends assumed continuation of the annual percent change in the prevalence rate for each disease from 1990 to 2013 as obtained from GBD data; in sensitivity analysis, disease prevalence rates were held constant (S8 Table). Iron deficiency was simulated as producing associated anemia, with disability weights, mortality rates, and mortality trends over time also from GBD data [8,13]. We note that iron deficiency and iron deficiency anemia (IDA) are not equivalent, but because IDA occurs when iron deficiency is sufficiently severe to reduce red blood cell production [25,26], the estimated average requirement cut-point method is a viable strategy for estimating the relative increase in IDA [27].
Model validation
Validity of model estimates was assessed by comparing model estimates to values reported in the literature [8,13,14] (S1–S3 Tables). Model estimates subjected to validation included current zinc and iron dietary supplies and percent deficiencies, current yearly disease burdens, and projected disease burdens from 2015 to 2050 (calculated from current yearly burdens and assuming continuation of secular trends in the scenario without climate change).
Comparative effectiveness
We considered alternative strategies to mitigate the disease burden from increased zinc and iron deficiencies attributable to increasing carbon dioxide concentrations. Specifically, we compared 5 traditional public health strategies to strategies consistent with the Paris Agreement to maintain global temperatures within 2°C of pre-industrial levels, adjusting each strategy for current anticipated feasibility and population reach. The 5 public health strategies were (i) zinc supplementation [28], in which zinc is administered daily to cover 80% of children under 5 years of age with random selection; (ii) iron supplementation [29], in which iron is administered weekly to cover 80% of females over 5 years of age; (iii) malaria mitigation [30], in which a previously described portfolio of interventions (e.g., long-lasting insecticide-treated nets, indoor residual spraying, and mass screening and treatment) is adopted at an 80% coverage level; (iv) pneumonia mitigation [31], in which a previously described portfolio of interventions (e.g., Haemophilus influenzae type b vaccine, pneumococcal vaccine, antibiotics for pneumonia, promotion of breastfeeding, vitamin A supplementation, and environmental improvements) is adopted at an 80% coverage level (except for the H. influenzae and pneumococcal vaccines, which are adopted at 90% coverage); and (v) diarrhea mitigation [31], in which a previously described portfolio of interventions (e.g., oral rehydration solution, rotavirus vaccine, antibiotics for dysentery, promotion of breastfeeding, vitamin A supplementation, and environmental improvements) is adopted at an 80% coverage level (except for the rotavirus vaccine, which is adopted at 90% coverage). Each strategy is detailed in S5 Text.
Sensitivity analyses
We performed 1-way sensitivity analysis, in which parameters were varied one at a time ± 10%, across all model inputs (S4 Text; S2–S8 Figs). In particular, we varied initial zinc and iron intake distributions across ranges to account for potential changes in dietary patterns and uncertainties in the quality of current measurements, initial disease prevalence rates to account for potential underreporting, and disease mortality rates conditional on deficiency to account for potential changes in healthcare availability. We also performed probabilistic sensitivity analysis by running the model 10,000 times per country while Monte Carlo sampling from probability distributions around each input parameter to compute uncertainty intervals for each outcome (S4 Text; S5–S8 Tables). Probability distributions for input parameters were determined based on previously reported probability distributions, uncertainty estimates, and natural bounds. The model was programmed in R version 3.2.2 [32], with input data and statistical code for replication and extension of our analysis published at https://purl.stanford.edu/tx325yy8269 concurrent with publication.
Results
Model validation
Our model-based estimates of nutrient supply, nutrient deficiency, and associated disease had a high degree of correspondence to current estimates from other sources (S1–S3 Tables). Specifically, our model-based estimates of global population-weighted zinc supply and deficiency were within 0.8% and 3.3% relative error from values in the literature, respectively [14]. Our estimate of global population-weighted iron deficiency was within 0.6% of values in the literature [8]. Our estimates of the 2015 DALY burdens due to malaria, pneumonia, diarrhea, and IDA were within 2.4%, 0.3%, 1.4%, and 0.2%, respectively, of values in the literature [13]. Estimated 2015 to 2050 DALY burdens due to malaria, pneumonia, diarrhea, and IDA globally were within 0.7%, 1.3%, 2.0%, and 2.7%, respectively, of values in the literature [13]. All other model-based results showed high concordance with prior estimates of current nutrient deficiency and disease (S1–S3 Tables).
Changes in zinc and iron deficiencies
In the absence of increasing carbon dioxide concentrations, zinc and iron deficiencies would be expected to induce 1,072.9 million DALYs globally over the period 2015 to 2050 according to our model. This global burden would represent approximately 2.0% of the expected DALYs due to all diseases of any kind over this period, which would make zinc and iron deficiencies the 13th leading risk factor for DALYs if the relative burdens attributable to other risk factors did not change [33].
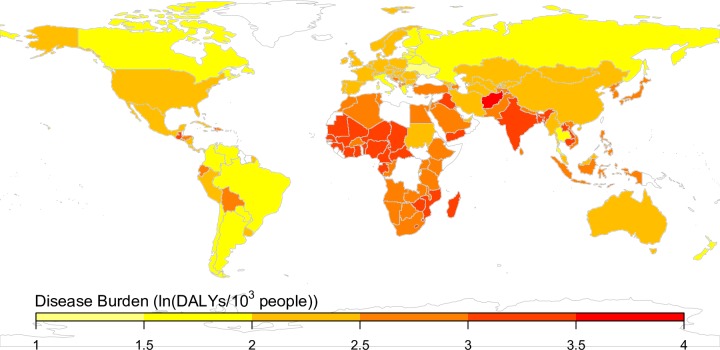
In the presence of increasing carbon dioxide concentrations, decreased zinc and iron concentrations of crops would be expected to lead to an additional 125.8 million DALYs globally over the period 2015 to 2050, with a disproportionate burden in the World Health Organization’s South-East Asia and African Regions (Fig 2). Countries in the study sample would be expected to experience increases in carbon dioxide concentration from approximately 400 ppm to 550 ppm (a 37.5% increase) from 2015 to 2050 and resultant declines in zinc and iron concentrations of C3 crops of approximately 5%–10% [5,9,10,34]. Given current consumption patterns, per our model, the nutrient concentration changes would induce an additional 8.2 percentage point increase in zinc deficiency (from the current baseline rate of 32.0% of the population deficient) and 6.1 percentage point increase in iron deficiency (from the baseline of 21.8% deficient) in the South-East Asia Region—the most highly affected region for zinc/iron deficiency—by 2050. The least-affected region, by contrast, would be the European Region, which would be anticipated to experience an additional 1.9 percentage point increase in zinc deficiency (from a baseline of 3.7% deficient) and 3.4 percentage point increase in iron deficiency (from a baseline of 11.1% deficient). The difference in the fraction of people placed at risk of zinc deficiency was not primarily due to a greater dependence on C3 crops in the South-East Asia Region for dietary zinc, but because a higher portion of the current population is only marginally above the threshold for zinc deficiency.
Fig 2. Per capita burden of disease attributed to carbon-dioxide-induced declines in the zinc and iron concentrations of crops, from 2015 to 2050.
The microsimulation was run 10,000 times for each country, and the natural logarithm of burden in disability-adjusted life years (DALYs)/103 people is shown. These values reflect the additional zinc and iron deficiency burden of disease due to increasing carbon dioxide, and background disease burdens are subtracted. Countries in white were those for which data were not available from the cited sources.
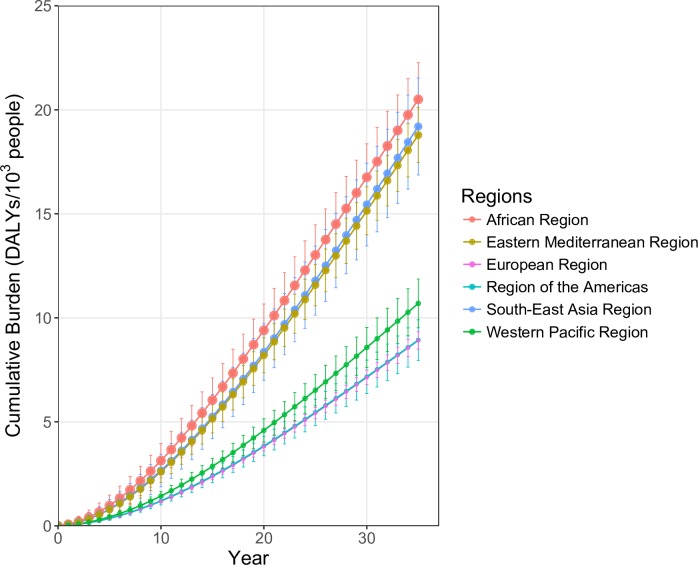
Model results suggested that carbon-dioxide-induced reductions in zinc and iron concentrations among crops would increase between-country and between-region inequalities in DALY burden per person (Fig 3). The regions with highest initial per capita burdens due to carbon-dioxide-induced zinc and iron reductions would also be expected to be the most affected over the 35-year period, with increased disparities over time. For example, the WHO African Region would be expected to experience approximately twice the per capita burden of other regions, such as the European Region, over the study period. Moreover, the regions with the highest per capita burdens due to carbon-dioxide-induced reductions (WHO African and South-East Asia Regions) are those with the highest current estimated burdens due to zinc and iron deficiencies (e.g., the current per capita burden of zinc and iron deficiencies in the African Region is approximately 4 times that of the European Region).
Fig 3. Cumulative per capita burden of disease attributed to carbon-dioxide-induced declines in the zinc and iron concentrations of crops, 2015 to 2050.
The points show mean cumulative disability-adjusted life years (DALYs) per 1,000 population, with error bars reflecting 1 standard deviation above and below the mean from 10,000 probabilistic simulations. The size of the points for each population is scaled to show initial DALY burden per 1,000 population in 2015 due to zinc and iron deficiencies. Regions are as defined by WHO.
Mitigation strategies
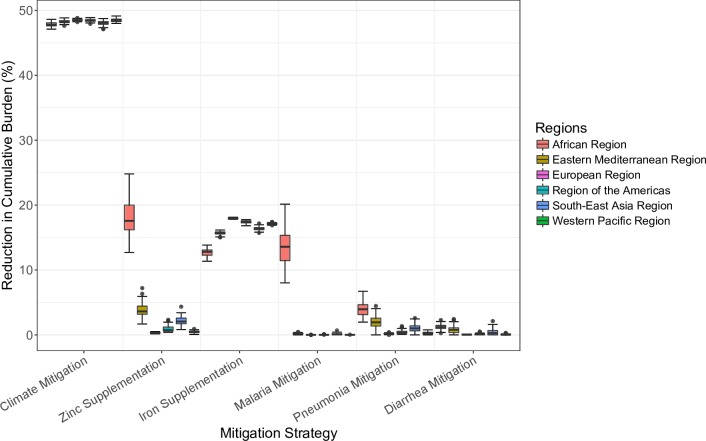
Compared with the 5 modeled traditional public health interventions, a climate mitigation strategy such as the Paris Agreement would be expected to avert the greatest portion of the cumulative projected burden of carbon-dioxide-attributable zinc and iron deficiencies between 2015 and 2050 (Fig 4). Even with 80% coverage with zinc and iron supplementation and with intensive disease control programs for malaria, pneumonia, and diarrhea, the sum total of the public health measures would be anticipated to reduce only 26.6% of the global carbon-dioxide-attributable zinc and iron deficiency burden of disease (95% credible interval [CrI]: 23.8%–29.6%). The countries that benefited most from the public health programs were those with high current zinc and iron deficiency DALY burdens (e.g., countries in the African Region), as these countries are expected to experience the greatest increases in deficiencies and highest disease rates over the study period.
Fig 4. Effect of mitigation strategies, 2015 to 2050.
Six mitigation strategies were considered for each of 137 countries. They included climate mitigation per the Paris Agreement to keep global temperatures below 2°C of pre-industrial levels; daily zinc supplementation for 80% of children under 5 years of age; weekly iron supplementation for 80% of women; and malaria, pneumonia, and diarrhea mitigation programs previously described in the literature adopted at 80% coverage levels (S5 Text). The microsimulation of 1 million people was run 100 times per country per strategy. The boxplots show median, interquartile, and outlier reductions in cumulative carbon-dioxide-induced disability-adjusted life year burdens from 2015 to 2050 for countries in each region by strategy. Of note, while there is considerable variation in carbon-dioxide-induced disease burden between iterations (Fig 3), there is relatively little variation in reduction in cumulative burden. This lack of variation is caused by the fact that all the mitigation strategies effectively reduce deficiencies or diseases on a percent basis (see Methods). Regions are as defined by WHO.
By contrast, interventions consistent with the Paris Agreement to keep global temperatures within 2°C of pre-industrial levels, which was previously anticipated to feasibly prevent approximately 47% of the increase in carbon dioxide concentrations by 2050 [35,36], would be expected to avert 48.2% of global carbon-dioxide-attributable zinc and iron deficiency burden of disease (95% CrI: 47.8%–48.5%). Since the 2015 carbon dioxide concentration was approximately 400 ppm and the 2050 carbon dioxide concentration is projected to be approximately 550 ppm [5,9,10,34], adhering to the Paris Agreement would be expected to result in a 2050 carbon dioxide concentration of approximately 480 ppm.
The greater effectiveness of the climate mitigation strategy relative to the public health measures was driven by the fact that it benefited the entire population, whereas the public health measures were targeted to subsets of the population with the highest per capita DALY burden, missing substantial populations with small per capita, but large aggregate, DALY burdens. Furthermore, the Paris Agreement reversed carbon-dioxide-induced deficiencies and related diseases, unlike the public health measures, which each addressed only a single form of deficiency or disease manifestation. The credible intervals for the percent reductions in disease burdens with the mitigation strategies were relatively small as all the mitigation strategies effectively reduce deficiencies or related diseases on a percent basis.
Sensitivity analyses
The relative benefits of the climate mitigation strategy versus the traditional public health strategies were unaltered by using a wide range of alternative literature-based input parameters (S2–S8 and S10 Figs; S7 and S8 Tables). In particular, the relative superiority of the climate mitigation strategy did not qualitatively change with alterations to baseline zinc and iron intakes, disease prevalence, or mortality rates. Model projections were generally most sensitive to changes in inputs related to iron (e.g., iron consumption, WtdEARs for iron, and IDA disability weights; S2–S8 Figs), but no scenario altered the comparative effectiveness of climate mitigation relative to traditional public health measures.
Discussion
Carbon-dioxide-induced reductions in zinc and iron concentrations among crops are anticipated, by our model, to lead to an additional 125.8 million DALYs globally over the period 2015 to 2050. A disproportionate burden of these DALYs is anticipated to affect countries with high existing burdens from zinc and iron deficiencies, thereby increasing existing global inequalities in nutritional deficiency by disproportionately affecting South-East Asia and Africa.
Our study suggests that climate mitigation strategies such as the Paris Agreement would be expected to avert a greater portion (approximately 48%) of the projected increase in zinc and iron deficiencies, about 1.8 times greater than the mitigation from traditional public health interventions including nutrient supplementation and disease control programs to counteract the heightened risk of diseases associated with zinc and iron deficiencies. A 48.2% reduction in DALY burden due to reduced zinc and iron concentrations of crops with the climate mitigation strategy is reasonable, as the climate mitigation strategy reduces the increase in 2050 carbon dioxide concentrations by approximately 47%, and a linear relationship between carbon dioxide concentrations and plant micronutrient concentrations was assumed. However, this linear relationship need not be the case and is not an obvious result due to potential nonlinearities created by relationships between micronutrient supplies, deficiencies, diseases, and resulting DALY burdens.
Our study extends prior work projecting changes in the zinc and iron concentrations of crops due to increasing carbon dioxide concentrations, changes in the prevalence of zinc deficiencies, and countries at risk from the changing iron concentrations of crops (by computing changes in iron supplies and cross-referencing them to estimates of the current prevalence of anemia) [2–5,9,20]. We extended this body of work by modeling diseases stemming from zinc and iron deficiencies using a microsimulation model to project disease burdens attributable to the nutrient concentration effects of increased atmospheric carbon dioxide and to evaluate potential mitigation strategies. Critically, this approach enabled us to understand this important health impact of climate change in the context of existing disease burdens and health inequalities between countries and regions.
Among the primary limitations of our analysis is our inability to anticipate what changes in dietary patterns might occur simultaneously with increasing carbon dioxide concentrations. We varied consumption parameters over wide ranges in sensitivity analysis and found that our findings of an overall increased inequality in disease burden between countries and the impact of climate mitigation relative to public health measures were consistent across a broad range of scenarios. This is an important area for further research. Another limitation is that we assumed that secular exponential trends in disease mortality rates would continue, reflecting economic development and health services improvement. Should recent trends not continue in positive directions, our projections may be viewed as optimistic, rendering our results conservative forecasts of the complications from zinc and iron deficiencies. A third limitation is that we assumed that crop zinc and iron concentrations decline linearly with increasing carbon dioxide concentrations. If the declines are convex, our disease burden projections are likely underestimates, while if they are concave, our disease burden projections are likely overestimates. Finally, because we used WtdEARs to project deficiencies, we felt that disaggregating results by gender and age group would imply a level of precision we cannot reliably provide at this point.
Future studies may directly experiment with interventions to induce higher zinc and iron concentrations in plants that can be grown in the most heavily affected countries. Further studies should also evaluate whether dietary changes may be directed to reduce the burden of disease associated with nutritional deficiency attributable to increased carbon dioxide in the atmosphere. Finally, subsequent studies might seek to evaluate the cost and cost-effectiveness of different mitigation strategies.
While such studies are underway, our findings indicate that rising atmospheric carbon dioxide concentrations and their impacts on nutrient concentrations in crops are likely to increase health inequalities from nutritional deficiencies by disproportionately impacting countries with the highest existing health burdens attributable to nutritional deficiencies. This projected increase in health inequalities is driven by differences in existing vulnerability of populations marginally above the threshold for deficiency and associated disease risk. Mitigation strategies concordant with the Paris Agreement, however, would be anticipated to substantially reduce the carbon-dioxide-induced rise in zinc and iron deficiency burdens, as compared to traditional public health measures, which may have a lesser effect even with optimistic degrees of population coverage and efficacy.
Supporting information
Modeled countries are shown in color corresponding to their WHO region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs globally are shown.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the African Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the Region of the Americas.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the South-East Asia Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the European Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the Eastern Mediterranean Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the Western Pacific Region.
(TIF)
The microsimulation was run 10,000 times for each country. The boxplots show median, interquartile, and outlier cumulative per capita carbon-dioxide-induced DALY burdens by decadal period for the countries in each region. These values reflect the additional zinc and iron deficiency burden of disease due to increasing carbon dioxide, and background disease burdens are subtracted.
(TIF)
The microsimulation of 1 million people was run 100 times per country per mitigation strategy. The boxplots show median, interquartile, and outlier reductions in cumulative DALY burdens from 2015 to 2050 for countries by region by strategy.
(TIF)
Results are shown as percent changes from literature values to model results. Iron supply could not be validated at the regional level as literature values were not available.
(DOCX)
Results are shown as percent changes from literature values to model results.
(DOCX)
Results are shown as percent changes from literature values to model results.
(DOCX)
The microsimulation of 10,000 people was run 10,000 times for each country. Projected raw and per capita DALY burdens due to carbon-dioxide-induced declines in the zinc and iron concentrations of crops from 2015 to 2050 are shown. Micronutrient supplies and percent deficiencies in 2015 are also shown.
(DOCX)
(DOCX)
(DOCX)
Iron consumption distributions were assumed to be lognormal with 40% CVs. The model was run 10,000 times with 10,000 people while sampling from distributions reflecting uncertainty in inputs.
(DOCX)
Malaria, pneumonia, and diarrhea prevalence rates in 2015 were assumed to continue over the model period. The model was run 10,000 times with 10,000 people while sampling from distributions reflecting uncertainty in inputs.
(DOCX)
The microsimulation of 1 million people was run 100 times per country per mitigation strategy. Six mitigation strategies were considered. They included climate mitigation per the Paris Agreement to keep global temperatures below 2°C of pre-industrial levels; daily zinc supplementation for 80% of children under 5 years of age; weekly iron supplementation for 80% of women; and malaria, pneumonia, and diarrhea mitigation programs previously described in the literature adopted at 80% coverage rates. The mean percent reductions in cumulative DALY burdens due to carbon-dioxide-induced declines in zinc and iron concentrations of crops from 2015 to 2050 are shown.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- CrI
credible interval
- CV
coefficient of variation
- DALY
disability-adjusted life year
- GBD
Global Burden of Disease Project
- IDA
iron deficiency anemia
- USDA
US Department of Agriculture
- WtdEAR
weighted estimated average requirement
Data Availability
Input data and statistical code for replication and extension of our analysis available at https://purl.stanford.edu/tx325yy8269
Funding Statement
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health (https://www.nimhd.nih.gov) under Award Numbers DP2MD010478 (SB), and U54MD010724 (EB, SB). CW was supported by a National Science Foundation Graduate Fellowship (https://www.nsf.gov, DGE-114747), and MB and EB were supported by a grant from the Woods Institute Environmental Ventures Program at Stanford University (https://woods.stanford.edu). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Smith KR, Woodward A, Campbell-Lendrum D, Chadee DD, Honda Y, Liu Q, et al. Human health: impacts, adaptation, and co-benefits In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al. , editors. Climate change 2014: impacts, adaptation, and vulnerability. Part A: global and sectoral aspects. Working Group II contribution to the fifth assessment report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2014. [Google Scholar]
- 2.Loladze I. Hidden shift of the ionome of plants exposed to elevated CO2 depletes minerals at the base of human nutrition. eLife. 2014;3:e02245 doi: 10.7554/eLife.02245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernando N, Panozzo J, Tausz M, Norton R, Fitzgerald G, Seneweera S. Rising atmospheric CO2 concentration affects mineral nutrient and protein concentration of wheat grain. Food Chem. 2012;133:1307–11. doi: 10.1016/j.foodchem.2012.01.105 [DOI] [PubMed] [Google Scholar]
- 4.Bowes G. Facing the inevitable: plants and increasing atmospheric CO2. Annu Rev Plant Physiol Plant Mol Biol. 1993;44:309–32. doi: 10.1146/annurev.pp.44.060193.001521 [Google Scholar]
- 5.Myers SS, Zanobetti A, Kloog I, Huybers P, Leakey ADB, Bloom AJ, et al. Increasing CO2 threatens human nutrition. Nature. 2014;510:139–42. doi: 10.1038/nature13179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGrath JM, Lobell DB. Reduction of transpiration and altered nutrient allocation contribute to nutrient decline of crops grown in elevated CO2 concentrations. Plant Cell Environ. 2013;36:697–705. doi: 10.1111/pce.12007 [DOI] [PubMed] [Google Scholar]
- 7.Caulfield LE, Black RE. Zinc deficiency In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Volume 1 Geneva: World Health Organization; 2004. [cited 2018 May 16]. pp. 257–279. Available from: https://books.google.com/books?hl=en&lr=&id=ACV1jEGx4AgC&oi=fnd&pg=PA257&dq=+Zinc+deficiency+Laura+E.+Caulfield+and+Robert+E.+Black&ots=tXEYvYvZW0&sig=KjRYgW2uv9kc9ROAZTSuuUTxaMo. [Google Scholar]
- 8.Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615–24. doi: 10.1182/blood-2013-06-508325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Myers SS, Wessells KR, Kloog I, Zanobetti A, Schwartz J. Effect of increased concentrations of atmospheric carbon dioxide on the global threat of zinc deficiency: a modelling study. Lancet Glob Health. 2015;3:e639–45. doi: 10.1016/S2214-109X(15)00093-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisher BS, Nakicenovic N, Alfsen K, Morlot JC, Chesnaye F, Hourcade J-C, et al. Issues related to mitigation in the long term context In: Metz B, Davidson OR, Bosch PR, Dave R, Meyer LA, editors. Climate change 2007: mitigation of climate change. Working Group III contribution to the fourth assessment report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- 11.US Department of Agriculture. USDA National Nutrient Database for Standard Reference, Release SR28 Washington (DC): US Department of Agriculture; 2016. [cited 2016 Sep 15]. Available from: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/nutrient-data-laboratory/docs/usda-national-nutrient-database-for-standard-reference/. [Google Scholar]
- 12.Food and Agriculture Organization of the United Nations. FAOSTAT: food balance sheets Rome: Food and Agriculture Organization of the United Nations; 2013. [cited 2016 Sep 15]. Available from: http://www.fao.org/faostat/en/#data/FBS. [Google Scholar]
- 13.Institute for Health Metrics and Evaluation. GHDx: GBD results tool Seattle: Institute for Health Metrics and Evaluation; 2013. [cited 2016 Sep 15]. Available from: http://ghdx.healthdata.org/gbd-results-tool. [Google Scholar]
- 14.Kumssa DB, Joy EJM, Ander EL, Watts MJ, Young SD, Walker S, et al. Dietary calcium and zinc deficiency risks are decreasing but remain prevalent. Sci Rep. 2015;5:10974 doi: 10.1038/srep10974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Global Burden of Disease 2004 update: disability weights for diseases and conditions Geneva: World Health Organization; 2008. [cited 2018 May 16]. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD2004_DisabilityWeights.pdf?ua=1. [Google Scholar]
- 16.Joy EJ, Ander EL, Young SD, Black CR, Watts MJ, Chilimba AD, et al. Dietary mineral supplies in Africa. Physiol Plant. 2014;151:208–29. doi: 10.1111/ppl.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wessells KR, Brown KH. Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting. PLoS ONE. 2012;7:e50568 doi: 10.1371/journal.pone.0050568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wessells KR, Singh GM, Brown KH. Estimating the global prevalence of inadequate zinc intake from national food balance sheets: effects of methodological assumptions. PLoS ONE. 2012;7:e50565 doi: 10.1371/journal.pone.0050565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beal T, Massiot E, Arsenault JE, Smith MR, Hijmans RJ. Global trends in dietary micronutrient supplies and estimated prevalence of inadequate intakes. PLoS ONE. 2017;12:e0175554 doi: 10.1371/journal.pone.0175554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith MR, Golden CD, Myers SS. Potential rise in iron deficiency due to future anthropogenic carbon dioxide emissions. GeoHealth. 2017;1:248–57. doi: 10.1002/2016GH000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carriquiry AL. Assessing the prevalence of nutrient inadequacy. Public Health Nutr. 1999;2:23–33. [DOI] [PubMed] [Google Scholar]
- 22.Stadlmayr B, Wijesinha-Bettoni R, Haytowitz D, Rittenschober D, Cunningham J, Sobolewski R, et al. FAO/INFOODS guidelines: guidelines for food matching. Version 1.2 Rome: Food and Agriculture Organization of the United Nations; 2012. [cited 2018 May 16]. Available from: http://www.fao.org/infoods/infoods/standards-guidelines/en/. [Google Scholar]
- 23.Wuehler SE, Peerson JM, Brown KH. Use of national food balance data to estimate the adequacy of zinc in national food supplies: methodology and regional estimates. Public Health Nutr. 2005;8:812–9. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization, Food and Agriculture Organization of the United Nations. Vitamin and mineral requirements in human nutrition 2nd edition Geneva: World Health Organization; 2004. [Google Scholar]
- 25.Bermejo F, García-López S. A guide to diagnosis of iron deficiency and iron deficiency anemia in digestive diseases. World J Gastroenterol. 2009;15:4638–43. doi: 10.3748/wjg.15.4638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372:1832–43. doi: 10.1056/NEJMra1401038 [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine Subcommittee on Interpretation and Uses of Dietary Reference Intakes, Institute of Medicine Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. DRI dietary reference intakes: applications in dietary assessment. Washington (DC): National Academies Press; 2000. [cited 2018 May 16]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222890/. [Google Scholar]
- 28.Yakoob MY, Theodoratou E, Jabeen A, Imdad A, Eisele TP, Ferguson J, et al. Preventive zinc supplementation in developing countries: impact on mortality and morbidity due to diarrhea, pneumonia and malaria. BMC Public Health. 2011;11(Suppl 3):S23 doi: 10.1186/1471-2458-11-S3-S23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pasricha S-R, Drakesmith H, Black J, Hipgrave D, Biggs B-A. Control of iron deficiency anemia in low- and middle-income countries. Blood. 2013;121:2607–17. doi: 10.1182/blood-2012-09-453522 [DOI] [PubMed] [Google Scholar]
- 30.Griffin JT, Hollingsworth TD, Okell LC, Churcher TS, White M, Hinsley W, et al. Reducing plasmodium falciparum malaria transmission in Africa: a model-based evaluation of intervention strategies. PLOS Med. 2010;7:e1000324 doi: 10.1371/journal.pmed.1000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhutta ZA, Das JK, Walker N, Rizvi A, Campbell H, Rudan I, et al. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013;381:1417–29. doi: 10.1016/S0140-6736(13)60648-0 [DOI] [PubMed] [Google Scholar]
- 32.R Core Team. R: a language and environment for statistical computing Vienna: R Foundation for Statistical Computing; 2015. [cited 2018 May 16]. Available from: https://www.R-project.org/. [Google Scholar]
- 33.World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks Geneva: World Health Organization; 2009. [Google Scholar]
- 34.Earth System Research Laboratory Global Monitoring Division. Global Greenhouse Gas Reference Network Trends in atmospheric carbon dioxide. Data: Mauna Loa CO2 annual mean data. Boulder: Earth System Research Laboratory; 2018. [cited 2018 Mar 24]. Available from: https://www.esrl.noaa.gov/gmd/ccgg/trends/data.html. [Google Scholar]
- 35.Meinshausen M, Smith SJ, Calvin K, Daniel JS, Kainuma MLT, Lamarque J-F, et al. The RCP greenhouse gas concentrations and their extensions from 1765 to 2300. Clim Change. 2011;109:213 doi: 10.1007/s10584-011-0156-z [Google Scholar]
- 36.Rogelj J, Meinshausen M, Knutti R. Global warming under old and new scenarios using IPCC climate sensitivity range estimates. Nat Clim Change. 2012;2:248–53. doi: 10.1038/nclimate1385 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Modeled countries are shown in color corresponding to their WHO region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs globally are shown.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the African Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the Region of the Americas.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the South-East Asia Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the European Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the Eastern Mediterranean Region.
(TIF)
One-way sensitivity analysis was performed across all model inputs. For each country, inputs were varied by plus and minus 10%, and the microsimulation was run 1,000 times. The 6 most influential inputs are shown for the Western Pacific Region.
(TIF)
The microsimulation was run 10,000 times for each country. The boxplots show median, interquartile, and outlier cumulative per capita carbon-dioxide-induced DALY burdens by decadal period for the countries in each region. These values reflect the additional zinc and iron deficiency burden of disease due to increasing carbon dioxide, and background disease burdens are subtracted.
(TIF)
The microsimulation of 1 million people was run 100 times per country per mitigation strategy. The boxplots show median, interquartile, and outlier reductions in cumulative DALY burdens from 2015 to 2050 for countries by region by strategy.
(TIF)
Results are shown as percent changes from literature values to model results. Iron supply could not be validated at the regional level as literature values were not available.
(DOCX)
Results are shown as percent changes from literature values to model results.
(DOCX)
Results are shown as percent changes from literature values to model results.
(DOCX)
The microsimulation of 10,000 people was run 10,000 times for each country. Projected raw and per capita DALY burdens due to carbon-dioxide-induced declines in the zinc and iron concentrations of crops from 2015 to 2050 are shown. Micronutrient supplies and percent deficiencies in 2015 are also shown.
(DOCX)
(DOCX)
(DOCX)
Iron consumption distributions were assumed to be lognormal with 40% CVs. The model was run 10,000 times with 10,000 people while sampling from distributions reflecting uncertainty in inputs.
(DOCX)
Malaria, pneumonia, and diarrhea prevalence rates in 2015 were assumed to continue over the model period. The model was run 10,000 times with 10,000 people while sampling from distributions reflecting uncertainty in inputs.
(DOCX)
The microsimulation of 1 million people was run 100 times per country per mitigation strategy. Six mitigation strategies were considered. They included climate mitigation per the Paris Agreement to keep global temperatures below 2°C of pre-industrial levels; daily zinc supplementation for 80% of children under 5 years of age; weekly iron supplementation for 80% of women; and malaria, pneumonia, and diarrhea mitigation programs previously described in the literature adopted at 80% coverage rates. The mean percent reductions in cumulative DALY burdens due to carbon-dioxide-induced declines in zinc and iron concentrations of crops from 2015 to 2050 are shown.
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Input data and statistical code for replication and extension of our analysis available at https://purl.stanford.edu/tx325yy8269