Abstract
Background
Community trends of acute decompensated heart failure (ADHF) in diverse populations may differ by race and sex.
Methods
The Atherosclerosis Risk in Communities (ARIC) Study sampled heart failure related hospitalizations (age ≥55 years) in four US communities from 2005-2014 using ICD-9-CM codes. ADHF hospitalizations were validated by standardized physician review and computer algorithm, yielding 40,173 events after accounting for sampling design (unweighted n=8746).
Results
Of the ADHF hospitalizations, 50% had reduced ejection fraction (HFrEF), 39% had preserved EF (HFpEF). HFrEF was more common in black men and white men, whereas HFpEF was most common in white women. Average age-adjusted rates of ADHF was highest in blacks (38.1 per 1000 black men, 30.5 per 1000 black women), with rates differing by HF type and sex. ADHF rates increased over the 10 years (average annual percent change, AAPC: black women +4.3%, black men +3.7%, white women +1.9%, white men +2.6%), mostly reflecting more acute HFpEF. Age-adjusted 28-day and 1-year case fatality proportions were approximately 10% and 30%, respectively, similar across race-sex groups and HF types. Only blacks showed decreased 1-year mortality over time (AAPC: black women −5.4%, black men −4.6%), with rates differing by HF type (AAPC: black women HFpEF −7.1%, black men HFrEF −4.7%).
Conclusions
Between 2005-2014, trends in ADHF hospitalizations increased in four US communities, primarily driven acute HFpEF. Survival at one year was poor regardless of EF, but improved over time for black women and black men.
Keywords: heart failure, epidemiology, mortality, race, ejection fraction
Journal Subject Codes: epidemiology, heart failure, race and ethnicity, mortality/survival
BACKGROUND
Understanding population-based trends in heart failure (HF) incidence and survival is important for planning and evaluating prevention and treatment strategies. The Institute of Medicine emphasized the importance of monitoring the cardiovascular health of the country and the value of timely, high-quality, population-based data on the incidence of heart disease and their risk factors1, 2. HF was estimated to affect 5.7 million American adults in 2012, with 915,000 incident cases3. Its prevalence is expected to rise to 8.4 million by 20304.
A recent population-based study in Olmsted County, MN suggested that the incidence of HF declined from 2000 to 2010, with HF with reduced ejection fraction (HFrEF) declining at a faster rate than HF with preserved ejection fraction (HFpEF)5. While HF survival has improved compared to >25 years ago6, median survival remains at approximately 5 years5, 7. Higher mortality was seen among those with HFrEF compared to HFpEF and among men compared to women8. However, these trends in HF incidence and survival were observed in homogenous populations comprised of >90% Caucasian Americans in a single US community, and included outpatient and chronic stable cases. Separating acute from chronic HF in more diverse US communities would enhance our understanding of trends of HF and its burden in the general population.
The Atherosclerosis Risk in Communities (ARIC) Study was the first to differentiate hospitalization rates of acute decompensated HF (ADHF) from chronic stable HF in a biracial community-based population9. We present here the 10-year trends of validated first and recurrent ADHF hospitalizations and case fatality from four U.S. communities.
METHODS
The data and study materials are available to other researchers for the purposes of reproducing the results, subject to completion of a data use agreement10.
Study Population
Beginning in 2005, the ARIC Study conducted continuous and comprehensive surveillance of hospitalized HF events for residents age ≥55 years in four US communities: Forsyth County, NC; Jackson, MS; Minneapolis suburbs, MN; and Washington County, MD. Because of small numbers, blacks in Minneapolis and Washington County and persons reported to be neither black nor white were excluded from these analyses. The population of eligible blacks and whites age 55 and older in the four communities was 225,395 persons in 2014 (56% women, 21% black).
Hospital Surveillance, Case Ascertainment and Event Classification
Methods of event ascertainment and classification have been described previously11. Briefly, a stratified random sample of eligible hospitalizations for HF in 2005-2014 was selected based on three criteria: (1) International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) discharge diagnosis codes for HF or HF-related condition (398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 415.0, 416.9, 425.4, 428.×, 518.4, 786.0×) in any position; (2) age ≥55 years at the time of hospital discharge; and (3) home address within boundaries of the ARIC communities. The sampling varied by ICD-9-CM discharge codes (428 and non-428), field center, sex, and race (by race in Forsyth County and Jackson only) to achieve similar standard errors across these groups12. Of note, unlike the cohort component of the ARIC Study, ARIC Study Community Surveillance samples hospitalizations across the 22 hospitals in the ARIC communities and cannot follow a specific patient to link the current with a past hospitalization, including past hospitalizations outside of these ARIC Study hospitals.
Medical records of eligible hospitalizations (unweighted n=23,410) were abstracted by trained abstractors if there was any evidence of decompensation or new onset of HF symptoms or any mention by a physician that HF was the reason for hospitalization. Abstracted cases (unweighted n=22,394) were independently classified by computer algorithm and/or 1-2 physicians of the ARIC Mortality and Morbidity Classification Committee (MMCC) into one of five categories11: definite ADHF, possible ADHF, chronic stable HF, HF unlikely, or unclassifiable. Disagreements were adjudicated by the chair of the MMCC (board certified HF specialist). Definite or possible ADHF required evidence either from symptoms, signs, imaging or treatment of an acute exacerbation, worsening or new onset of symptoms or other decompensated circulatory state. For the purpose of this report, definite and possible ADHF were combined. When available, imaging reports of LVEF within two years of the current hospitalization were abstracted; history of prior HF diagnosis and comorbidities was obtained from the index hospitalization. ADHF events were further classified as HFrEF (current [within 3 months or less of hospitalization] or most recent left ventricular ejection fraction [LVEF] less than 50%), HFpEF (all recorded LVEF 50% or greater), or HF with unknown LVEF (UHF). Patients with recovered HFrEF (subsequent LVEF ≥50%) or unknown LVEF (UHF) were excluded from analysis specific to HF type (HFrEF versus HFpEF) and trends, because of relatively small numbers (3.0% and 8.9% of all ADHF cases, respectively) and because the recovered HFrEF group is considered physiologically different from chronic HFrEF and HFpEF.
The focus of the ARIC Study has been to identify HF events that become serious enough to require hospitalization, and among these we look for “first hospitalizations” as a proxy for incident cases9, as we have done for other cardiovascular diseases13. Vital status within one year after admission was determined by linkage with the National Death Index. Institutional review boards approved the study protocol at all participating hospitals in the ARIC communities (no informed consent was required).
Statistical Analysis
After excluding non-ADHF hospitalizations (unweighted n=6202), a small number of non-black minorities (n=225), and blacks in two predominately white communities (Minneapolis and Washington County; n=168), the final sample included 8,746 (weighted n=40,173) validated ADHF hospitalizations for the years 2005-2014 (Figure 1). Supplemental Table 1 lists the number of eligible hospitalizations and ADHF events per year, stratified by first and recurrent hospitalized events. Inter- and post-censal sex- and race-specific population estimates for each study community were computed for 2005-2014 by interpolations or extrapolations from the 2000 and 2010 U.S. censuses. For example, in 2014, there were 27104 black women, 98441 white women, 19304 black men and 80546 white men age 55 years and older in these four communities; and the number of hospitalized ADHF occurring among these populations in 2014 were 6419, 14615, 5400, and 13738, respectively.
Figure 1.
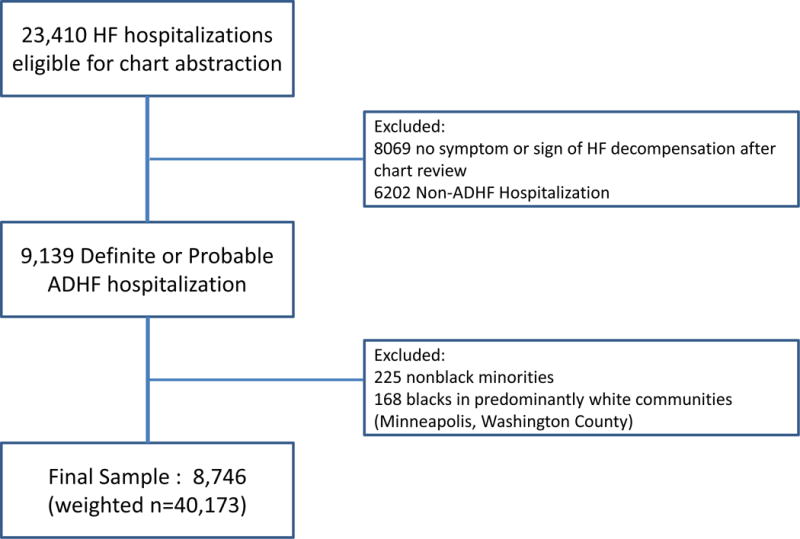
Flow diagram of eligible hospitalizations and the final study sample.
To account for the sampling design, all analyses were conducted using survey procedures and weighted by the inverse of the sampling probabilities. Differences by race and sex in probability of a hospitalization being first or in probability of HFrEF/HFpEF were tested using Wald tests based on logistic regression models. Sex and race-specific annual event rates per 1000 persons were computed based on population inter- and post-censal estimate denominators and adjusted for age by the direct method using the 2000 U.S. population estimates as the standard. Annual 28‐day and 365‐day (one‐year) case fatality percentages were computed based on denominators of those who were hospitalized with ADHF in the ARIC population and adjusted for age by the direct method using the ARIC combined hospitalized ADHF events as the standard. Case fatality analysis was available for all HF events hospitalized from 2005 through 2014 through National Death Index linkage data. Age‐adjusted trends are reported as average annual percent change (AAPC) by race and sex, using Poisson regression for first and recurrent hospitalization rates and using logistic regression for case fatality. Null hypotheses of no difference in the trends by race and sex were tested using Wald tests of the coefficients of interactions between main effects in these models.
All data analysis was performed using SAS version 9.1.3 (SAS Institute, Cary, North Carolina) or SUDAAN release 9.0.
RESULTS
Of the 40,173 validated hospitalized ADHF events from 2005 through 2014 in those age ≥55 years, 20,015 (50%) were HFrEF, 15,535 (39%) were HFpEF, 1,154 (2.9%) were recovered HFrEF (subsequent LVEF ≥50%), and 3,468 (8.6%) were HF with unknown LVEF (UHF) (Table 1). Approximately two-thirds (65%) of hospitalized ADHF events occurred in persons with no history of hospitalized HF, although 51% had a previous diagnosis of HF (without hospitalization). The percent of ADHF events that were first events was smaller among blacks (54%) as compared to whites (69%, p<0.0001), and among men (63%) compared to women (67%, p=0.0002). The proportion of ADHF events that were HFrEF was higher in men. Among first hospitalized ADHF, the distribution of HFrEF was 61% in black men, 53% in white men, 42% in black women, and 33% in white women. While there was no interaction between race and sex (p=0.24), first hospitalized events were more likely to be HFrEF in men (p<0.0001) and in blacks (p<0.0001). Recurrent hospitalized ADHF events were more commonly for HFrEF for all race-sex groups. Similarly, there was no interaction between race and sex (p=0.40), and recurrent events were more likely to be HFrEF in men (p<0.0001) and in blacks (p=0. 0007).
Table 1.
Baseline characteristics of 40,176 patients hospitalized for first and recurrent acute decompensated heart failure in 2005-2014, age 55 years and older, by race and sex: Atherosclerosis Risk in Communities Study Heart Failure Community Surveillance.
| All ADHF N= 40,173 |
First Hospitalized ADHF (N=26,028) |
Recurrent Hospitalized ADHF (N=14,144) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Black Women (N=3613) |
Black Men (N=2746) |
White Women (N=10393) |
White Men (N=9276) |
Black Women (N=2806) |
Black Men (N=2655) |
White Women (N=4221) |
White Men (N=4462) |
||
| Mean Age (year) | 75.8 (23.0) | 72.5 (20.8) | 69.2 (16.4) | 79.3 (23.5) | 76.3 (23.1) | 72.2 (22.7) | 68.1 (17.4) | 79.6 (23.1) | 76.8 (22.0) |
| Age groups (year) | |||||||||
| 55-64 | 7686 (19) | 1036 (29) | 1087 (40) | 1076 (10) | 1423 (15) | 839 (30) | 1225 (46) | 397 (9) | 602 (13) |
| 65-74 | 9595 (24) | 1021 (28) | 832 (30) | 1932 (19) | 2297 (25) | 811 (29) | 739 (28) | 880 (21) | 1082 (24) |
| 75+ | 22891 (57) | 1556 (43) | 826 (30) | 7386 (71) | 5555 (60) | 1155 (41) | 691 (26) | 2944 (70) | 2778 (62) |
| HF Type | |||||||||
| HFpEF | 15535 (39) | 1542 (43) | 791 (29) | 5646 (54) | 3251 (35) | 1018 (36) | 462 (17) | 1899 (45) | 926 (21) |
| HFrEF | 20015 (50) | 1531 (42) | 1683 (61) | 3431 (33) | 4941 (53) | 1425 (51) | 1971 (74) | 1841 (44) | 3192 (72) |
| Recovered HFrEF | 1154 (3) | 63 (2) | 71 (3) | 247 (2) | 286 (3) | 89 (3) | 76 (3) | 183 (4) | 139 (3) |
| UHF | 3468 (9) | 478 (13) | 200 (7) | 1070 (10) | 797 (9) | 274 (10) | 146 (5) | 298 (7) | 205 (5) |
| Comorbidities | |||||||||
| Prevalent CHD | 25324 (63) | 1607 (44) | 1441 (52) | 5591 (54) | 6518 (70) | 1779 (63) | 1844 (69) | 2780 (66) | 3765 (84) |
| Myocardial infarction | 10375 (26) | 454 (13) | 456 (17) | 2107 (20) | 2727 (29) | 664 (24) | 717 (27) | 1265 (30) | 1986 (45) |
| Angina | 5774 (14) | 340 (9) | 272 (10) | 1072 (10) | 1273 (14) | 460 (16) | 540 (20) | 708 (17) | 1109 (25) |
| Hypertension | 34476 (86) | 3296 (91) | 2469 (90) | 8709 (84) | 7529 (81) | 2584 (92) | 2418 (91) | 3643 (86) | 3827 (86) |
| Diabetes | 19158 (48) | 2080 (58) | 1381 (50) | 4223 (41) | 4072 (44) | 1773 (63) | 1421 (54) | 1862 (44) | 2346 (53) |
| Chronic kidney disease | 2711 (7) | 357 (10) | 371 (14) | 364 (4) | 457 (5) | 315 (11) | 225 (8) | 203 (5) | 419 (9) |
| Atrial fibrillation or flutter | 16129 (40) | 755 (21) | 566 (21) | 4297 (41) | 4102 (44) | 812 (29) | 709 (27) | 2448 (58) | 2439 (55) |
| Asthma/COPD | 15791 (39) | 1160 (32) | 808 (29) | 4158 (40) | 3611 (39) | 1120 (40) | 939 (35) | 2003 (47) | 1991 (45) |
| Obesity | 13183 (38) | 1545 (53) | 776 (35) | 3534 (38) | 3017 (36) | 1079 (50) | 789 (35) | 1351 (37) | 1089 (27) |
| Symptoms/ Signs | |||||||||
| Dyspnea/rales | 37419 (93) | 3250 (90) | 2489 (91) | 9615 (93) | 8647 (93) | 2646 (94) | 2496 (94) | 4025 (95) | 4251 (95) |
| Orthopnea | 13306 (33) | 1171 (32) | 1098 (40) | 2808 (27) | 2723 (29) | 1140 (41) | 1281 (48) | 1564 (37) | 1521 (34) |
| PND | 6209 (15) | 492 (14) | 534 (19) | 1169 (11) | 1314 (14) | 627 (22) | 737 (28) | 664 (16) | 671 (15) |
| Hypoxia | 18207 (45) | 1299 (36) | 844 (31) | 5686 (55) | 4486 (48) | 925 (33) | 722 (27) | 2259 (54) | 1985 (45) |
| Edema | 29640 (74) | 2545 (70) | 1987 (72) | 7274 (70) | 6886 (74) | 2190 (78) | 2064 (78) | 3156 (75) | 3539 (79) |
| Pulmonary edema (CXR) | 18581 (48) | 1753 (50) | 1286 (49) | 5099 (50) | 4006 (45) | 1441 (53) | 1136 (44) | 1933 (48) | 1927 (46) |
Values are presented as N (%) except for mean age where values are mean (SD). Percentages were rounded to the nearest integer.
Abbreviations: CHD = coronary heart disease; COPD = chronic obstructive pulmonary disease; CXR = chest x-ray; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; PND = paroxysmal nocturnal dyspnea; UHF = unknown subtype of heart failure (missing data for ejection fraction)
For those with first hospitalized ADHF, black patients compared to whites were younger, had fewer cardiac comorbidities (including prevalent coronary heart disease [CHD], myocardial infarction history, and atrial arrhythmias), but had more hypertension, diabetes and chronic kidney disease. Signs and symptoms of ADHF presentation were similar across all race-sex groups, with dyspnea and edema as the most common. Similar patterns of demographic and clinical characteristics were observed for those with recurrent ADHF hospitalizations.
Temporal trends in ADHF hospitalizations
Table 2 shows the age-adjusted average annual event rates of ADHF hospitalizations and average annual percentage changes (AAPC) by race-sex group, HF type, and HF history (first vs. recurrent). The highest event rates were in black men followed by black women, white men, and white women. ADHF rates increased over the 10 years (average annual percent change, AAPC: black women +4.3%, black men +3.7%, white women +1.9%, white men +2.6%), mostly reflecting more acute HFpEF. When stratified by HF type and HF history, the average annual rate of first hospitalized HFpEF was higher in blacks than in whites, and the average annual rate of first hospitalized HFrEF was higher in blacks than in whites.
Table 2.
Age-adjusted annual average event rates (AER) of hospitalized acute decompensated heart failure (ADHF) per 1000 persons in the population, and average annual percent change (AAPC), by heart failure type, race and sex: Atherosclerosis Risk in Communities Heart Failure Study Community Surveillance 2005-2014.
| Total (N=40,173) | HFpEF (N=15,535) | HFrEF (N=20,015) | ||||
|---|---|---|---|---|---|---|
| AER (per1000) | AAPC (%) | AER (per1000) | AAPC (%) | AER (per1000) | AAPC (%) | |
| All Hospitalized ADHF | ||||||
| Black Women | 30.5 (29.2, 31.8)*† | 4.3 (2.7, 5.9)* | 12.3 (11.4, 13.3)*† | 8.2 (5.2, 11.3) | 13.9 (12.8, 14.9)*† | 2.0 (−0.7, 4.7) |
| Black Men | 38.1 (36.6, 39.7) | 3.7 (2.3, 5.1) | 9.7 (8.7, 10.6) | 5.7 (2.1, 9.4) | 24.8 (23.5, 26.2) | 2.8 (0.8, 4.7) |
| White Women | 15.2 (14.7, 15.7) | 1.9 (0.7, 3.1) | 7.8 (7.4, 8.2) | 5.9 (4.0, 8.0) | 5.5 (5.2, 5.9) | −0.5 (−2.8, 1.9) |
| White Men | 20.7 (20.0, 21.4) | 2.6 (1.4, 3.8) | 6.3 (5.9, 6.8) | 4.6 (2.0, 7.3) | 12.3 (11.7, 12.9) | 2.6 (0.8, 4.4) |
| First Hospitalized ADHF | ||||||
| Black Women | 17.2 (16.1, 18.3)*† | 6.3 (3.8, 8.9)* | 7.4 (6.7, 8.1)*† | 10.0 (6.1, 14.1)* | 7.2 (6.5, 8.0)*† | 3.1 (−0.9, 7.4) |
| Black Men | 19.9 (18.6, 21.2) | 4.2 (1.9, 6.6) | 6.2 (5.5, 7.0) | 7.9 (3.4, 12.7) | 11.6 (10.6, 12.7) | 1.7 (−1.3, 4.8) |
| White Women | 10.8 (10.3, 11.3) | 1.8 (0.3, 3.4) | 5.9 (5.5, 6.2) | 5.3 (2.9, 7.7) | 3.6 (3.3, 3.9) | 0.7 (−2.3, 3.8) |
| White Men | 14.0 (13.3, 14.6) | 3.6 (2.0, 5.3) | 4.9 (4.5, 5.3) | 5.5 (2.5, 8.6) | 7.4 (6.9, 7.9) | 3.5 (1.1, 5.9) |
| Recurrent Hospitalized ADHF | ||||||
| Black Women | 13.3 (12.3, 14.3)*† | 1.7 (−0.9, 4.5) | 4.9 (4.3, 5.6)*† | 5.6 (0.5, 10.9) | 6.6 (5.9, 7.3)*† | 0.8 (−2.9, 4.7) |
| Black Men | 18.2 (17.0, 19.5) | 3.1 (0.7, 5.5) | 3.4 (2.8, 4.0) | 2.0 (−3.9, 8.3) | 13.2 (12.1, 14.3) | 3.7 (0.7, 6.7) |
| White Women | 4.4 (4.1, 4.7) | 2.0 (−0.6, 4.6) | 2.0 (1.7, 2.2) | 8.0 (3.9, 12.3) | 2.0 (1.7, 2.2) | −2.6 (−6.6, 1.5) |
| White Men | 6.8 (6.3, 7.2) | 0.5 (−2.1, 3.1) | 1.4 (1.2, 1.6) | 1.7 (−3.9, 7.7) | 4.9 (4.4, 5.3) | 1.2 (−1.9, 4.4) |
p<0.05 for comparison between race subgroups within the HF category.
p<0.05 for comparison between sex subgroups within the HF category.
Abbreviations:
AAPC = average annual percent change
AER = average event rates (number of ADHF events per year) per 1000 persons
HF = heart failure
HFpEF = heart failure with preserved ejection fraction
HFrEF = heart failure with reduced ejection fraction
Rates of first hospitalized ADHF increased each year for each race-sex group. The AAPC in the rates of all first ADHF hospitalizations was similar among all race-sex groups shown, ranging from an average 6.3% increase per year in black women to 1.8% in white women. Figure 2 depicts the age-adjusted first hospitalization rates per year by HF type and race-sex group. The increase in the rate of first hospitalized ADHF mostly reflected the increase in rates of HFpEF in each race-sex group over the 10-year time period. The age-adjusted average annual increases in first hospitalized HFpEF were at higher magnitude compared to the AAPC of all first hospitalized ADHF, with black women having the highest rise (an average 10.0% per year).
Figure 2.
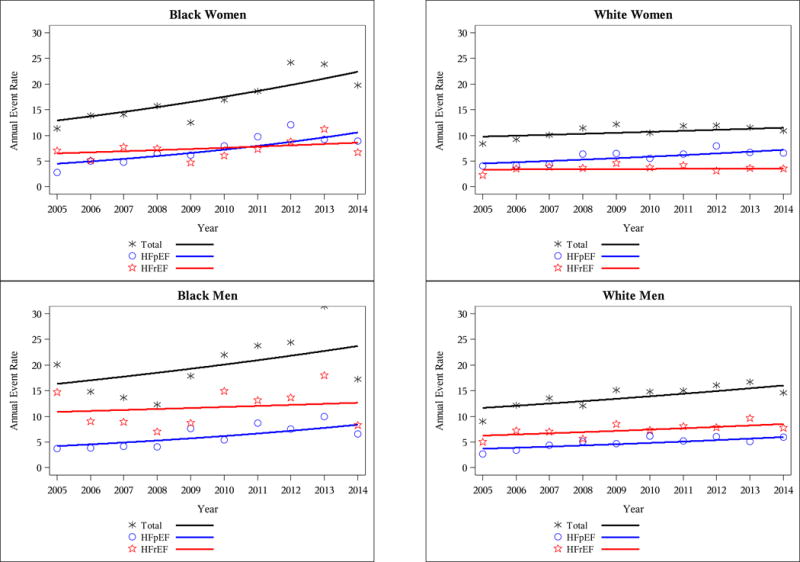
Age-adjusted annual event rates per 1000 for first hospitalized acute decompensated heart failure events, by heart failure type, race and sex: Atherosclerosis Risk in Communities Study Heart Failure Community Surveillance 2005-2014.
Changes in HFrEF rates were modest but showed different race-sex patterns. White men were the only race-sex group to have a rising rate of first hospitalized HFrEF. Changes in rates of first HFrEF were not statistically significant for blacks and white women.
Recurrent ADHF rates showed similar patterns as first ADHF hospitalizations, with blacks having higher average rates of recurrent ADHF hospitalizations regardless of HF type (Table 2). But the age-adjusted average annual increase in recurrent events was only statistically significant for women with HFpEF and black men with HFrEF.
Case Fatality
Table 3 displays the age-adjusted average annual 28-day and 1-year case fatality proportions by race-sex group, HF type, and HF history. For all ADHF hospitalizations, only blacks showed decreased 1-year mortality over time (AAPC: black women −5.4%, black men −4.6%), with rates differing by HF type (AAPC: black women HFpEF −7.1%, black men HFrEF −4.7%). For those with a first time hospitalization for ADHF, the age-adjusted average annual 28-day and 1-year case fatality proportions were higher among whites compared to blacks aggregated across HF type (p=0.02 and p=0.003, respectively) (Table 3). Figure 3 demonstrates the age-adjusted 1-year case fatality per year by HF type and race-sex group. In general, case fatality after a first ADHF hospitalization showed modest changes from 2005 through 2014, although 1-year case fatality significantly decreased by an average of 4.7% per year in black women. Among those with HFpEF, whites had higher 28-day and 1-year case fatality compared to blacks (p=0.01 and p=0.009, respectively). Changes in age-adjusted 28-day case fatality were not statistically significant for any race-sex group (Table 3 and Supplemental Figure 1).
Table 3.
Deaths within 28 days and 1 year of acute decompensated heart failure hospitalization, age-adjusted case fatality and average annual percent change (AAPC), by heart failure type, race and sex: Atherosclerosis Risk in Communities Study Heart Failure Community Surveillance 2005-2014.
| Total | HFpEF | HFrEF | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | 28-day CF (%) | AAPC (%) | N | 28-day CF (%) | AAPC (%) | N | 28-day CF (%) | AAPC (%) | |
| All Hospitalized ADHF | |||||||||
| Black Women | 570 | 10.2 (8.4,12.0)† | −6.0 (−13.3, 1.2) | 161 | 7.2 (4.9,9.4)† | 2.8 (−10.2, 15.9) | 302 | 11.6 (8.7,14.4) | −6.6 (−15.9, 2.8) |
| Black Men | 374 | 9.2 (7.5,10.9) | −3.2 (−9.1, 2.6) | 81 | 7.6 (4.6,10.5) | −0.6 (−14.6, 13.3) | 261 | 10.0 (7.8,12.3) | −3.5 (−10.4, 3.5) |
| White Women | 1805 | 11.7 (10.4,13.1) | −2.4 (−6.9, 2.1) | 825 | 10.1 (8.3,11.8) | −1.5 (−8.4, 5.4) | 651 | 12.2 (10.0,14.4) | −0.5 (−7.5, 6.4) |
| White Men | 1638 | 12.1 (10.7,13.5) | −0.7 (−5.3, 3.8) | 489 | 11.7 (9.3,14.2) | 0.5 (−7.4, 8.4) | 932 | 11.8 (10.1,13.6) | 2.5 (−3.1, 8.1) |
| First Hospitalized ADHF | |||||||||
| Black Women | 293 | 9.3 (7.0,11.5)† | −5.9 (−16.0, 4.2) | 85 | 6.2 (3.5,8.9)† | −5.7 (−24.0, 12.6) | 145 | 10.6 (6.8,14.3) | −3.9 (−17.7, 9.9) |
| Black Men | 159 | 7.3 (5.2,9.3) | 0.0 (−10.6, 10.7) | 37 | 5.4 (2.3,8.5) | 18.3 (−7.0, 43.6) | 115 | 9.0 (6.0,12.1) | −2.9 (−14.7, 9.0) |
| White Women | 1279 | 11.5 (9.9,13.1) | −4.1 (−9.5, 1.3) | 591 | 9.8 (7.7,11.8) | −1.6 (−9.8, 6.7) | 449 | 12.5 (9.8,15.3) | −1.0 (−9.5, 7.4) |
| White Men | 1065 | 11.8 (10.1,13.5) | −2.8 (−8.6, 3.0) | 371 | 11.4 (8.7,14.2) | −2.4 (−11.3, 6.6) | 545 | 11.6 (9.3,13.9) | 1.7 (−6.0, 9.4) |
| Recurrent Hospitalized ADHF | |||||||||
| Black Women | 277 | 11.5 (8.6,14.3) | −5.6 (−15.9, 4.6) | 76 | 8.7 (4.7,12.7) | 13.1 (−4.4, 30.6)* | 156 | 12.6 (8.5,16.8) | −9.3 (−22.3, 3.6) |
| Black Men | 215 | 11.6 (8.7,14.5) | −5.2 (−12.2, 1.7) | 43 | 11.6 (5.5,17.7) | −10.8 (−27.3, 5.6) | 145 | 11.0 (7.6,14.4) | −4.0 (−12.4, 4.3) |
| White Women | 525 | 12.3 (9.8,14.8) | 1.9 (−6.2, 10.0) | 233 | 10.9 (7.5,14.2) | −1.7 (−14.1, 10.7) | 202 | 11.6 (8.0,15.3) | 0.3 (−12.3, 13.0) |
| White Men | 572 | 12.8 (10.4,15.2) | 3.3 (−3.9, 10.5) | 118 | 12.8 (7.4,18.1) | 10.1 (−8.0, 28.2) | 387 | 12.0 (9.3,14.7) | 3.7 (−4.2, 11.6) |
|
| |||||||||
| N | 1-year CF (%) | AAPC (%) | N | 1-year CF (%) | AAPC (%) | N | 1-year CF (%) | AAPC (%) | |
|
| |||||||||
| All Hospitalized ADHF | |||||||||
| Black Women | 1783 | 30.9 (28.2,33.5)†‡ | −5.4 (−8.6, −2.2)† | 597 | 25.2 (21.4,29.0)†‡ | −7.1 (−13.1, −1.1)† | 888 | 34.0 (30.0,38.0) | −3.1 (−7.4, 1.1) |
| Black Men | 1456 | 33.7 (30.9,36.6) | −4.6 (−7.3, −1.8) | 299 | 27.5 (22.6,32.5) | −3.7 (−9.9, 2.6) | 1020 | 36.5 (32.7,40.4) | −4.7 (−8.0, −1.4) |
| White Women | 5014 | 33.8 (31.8,35.9) | −1.8 (−4.1, 0.5) | 2426 | 31.2 (28.5,34.0) | −2.1 (−5.3, 1.2) | 1827 | 34.4 (31.1,37.7) | 0.1 (−3.8, 3.9) |
| White Men | 5010 | 37.8 (35.7,39.8) | −1.3 (−3.4, 0.8) | 1506 | 37.0 (33.3,40.7) | 2.3 (−1.6, 6.3) | 2834 | 36.3 (33.6,39.0) | −1.9 (−4.7, 1.0) |
| First Hospitalized ADHF | |||||||||
| Black Women | 922 | 28.3 (25.0,31.7)† | −4.7 (−9.0, −0.3) | 347 | 24.5 (19.8,29.2)†‡ | −6.1 (−13.4, 1.3) | 402 | 29.2 (23.9,34.4) | −2.9 (−9.4, 3.6) |
| Black Men | 649 | 29.4 (25.7,33.2) | −1.7 (−6.0, 2.6) | 170 | 24.0 (18.2,29.7) | 1.3 (−7.6, 10.2) | 415 | 33.4 (28.1,38.8) | −3.2 (−8.6, 2.1) |
| White Women | 3444 | 32.3 (29.9,34.8) | −2.1 (−4.9, 0.7) | 1736 | 29.9 (26.7,33.0) | −1.9 (−5.9, 2.0) | 1161 | 32.9 (28.8,37.0) | 0.1 (−4.8, 5.1) |
| White Men | 3123 | 35.0 (32.5,37.5) | −1.2 (−4.0, 1.6) | 1114 | 34.9 (30.8,39.0) | 1.0 (−3.7, 5.7) | 1507 | 32.2 (28.8,35.5) | −0.5 (−4.6, 3.5) |
| Recurrent Hospitalized ADHF | |||||||||
| Black Women | 860 | 36.8 (32.2,41.4)†‡ | −5.8 (−10.4, −1.3)† | 250 | 26.4 (20.1,32.7)† | −8.1 (−17.8, 1.6)† | 485 | 39.5 (33.5,45.5) | −3.2 (−8.9, 2.5) |
| Black Men | 806 | 41.4 (36.3,46.4) | −6.6 (−10.2, −3.0) | 129 | 34.0 (25.0,43.0) | −8.4 (−17.4, 0.6) | 605 | 39.3 (33.9,44.8) | −5.8 (−9.9, −1.8) |
| White Women | 1569 | 38.4 (34.2,42.7) | −1.2 (−5.3, 2.8) | 690 | 35.3 (29.4,41.1) | −2.9 (−9.1, 3.2) | 665 | 37.3 (31.7,42.8) | 0.2 (−6.0, 6.4) |
| White Men | 1886 | 45.2 (41.0,49.5) | −1.0 (−4.3, 2.3) | 391 | 44.9 (36.7,53.2) | 6.4 (−0.9, 13.7) | 1326 | 42.5 (38.0,47.0) | −3.0 (−7.1, 1.1) |
N denotes the number of deaths.
p<0.05 for comparison between race-sex subgroups within the HF category.
p<0.05 for comparison between race subgroups within the HF category.
p<0.05 for comparison between sex subgroups within the HF category.
Abbreviations:
AAPC = average annual percent change
CF = average case fatality percentage
HF = heart failure
HFpEF = heart failure with preserved ejection fraction
HFrEF = heart failure with reduced ejection fraction
Figure 3.
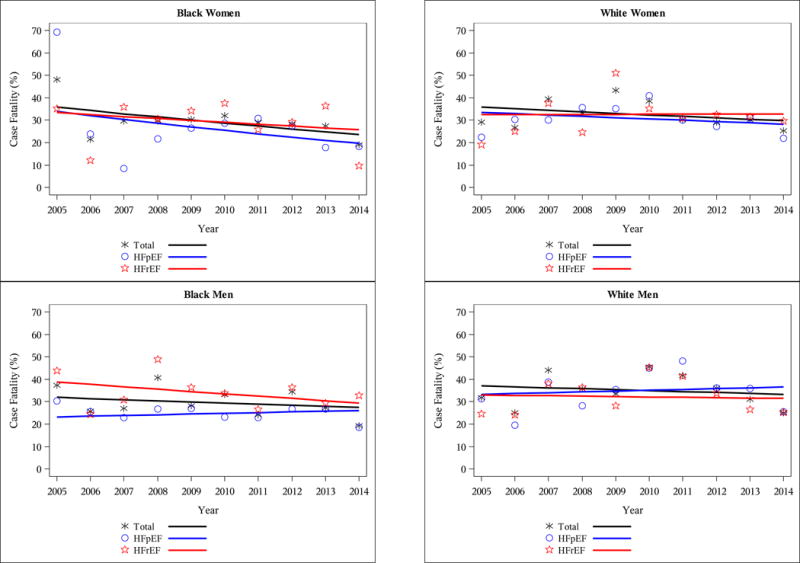
Age-adjusted 1-year case fatality for first hospitalized acute decompensated heart failure (ADHF) by heart failure type, race and sex: Atherosclerosis Risk in Communities Study Heart Failure Community Surveillance 2005-2014.
For patients with recurrent hospitalized ADHF, the average annual case fatality appeared higher in men than women (Table 3), but these sex-based differences were generally not statistically different. One-year mortality rates decreased by approximately 6% per year for both black women and black men over the 10 years, particularly black men with HFrEF.
Sensitivity analysis
The trends in HF incidence were sensitive to the definition of first hospitalization for ADHF. Sensitivity analyses were performed with first ADHF redefined more broadly as those with no history of HF diagnosis (regardless of presence of a hospitalization); this shifted the majority of hospitalized cases to recurrent ADHF. Demographic and clinical characteristics were similar to the population classified as an event with no previous hospitalization for HF (Supplemental Table 2). As expected, event rates were similarly shifted with significant trends seen primarily in the recurrent ADHF cases (Table 4 and Figure 4), and case fatality rates changed modestly for both first and recurrent ADHF cases, with at most a 5% absolute decrease in estimates (Table 5). Trends in 1-year case fatality were similar (decreases over time for black women with first ADHF, and both black women and black men with recurrent ADHF); however, 1-year case fatality increased over time for white women with first HFrEF (Table 5). These different trends in event rates and case fatality likely reflect differences in case-mix of ADHF created by changing the definition of a first event.
Table 4.
Age-adjusted annual average event rates (AER) of hospitalized acute decompensated heart failure (ADHF) per 1000 persons in the population, and average annual percent change (AAPC), by heart failure type*, race and sex: Atherosclerosis Risk in Communities Heart Failure Study Community Surveillance 2005-2014.
| Total (N=40,173) | HFpEF (N=15,535) | HFrEF (N=20,015) | ||||
|---|---|---|---|---|---|---|
| AER (per1000) | AAPC (%) | AER (per1000) | AAPC (%) | AER (per1000) | AAPC (%) | |
| FIrst ADHF* | ||||||
| Black Women | 7.5 (6.7, 8.2)†‡ | 1.8 (−1.7, 5.5) | 3.6 (3.0, 4.1)†‡ | 4.2 (−1.2, 9.8) | 3.0 (2.5, 3.5)†‡ | 0.8 (−4.8, 6.7) |
| Black Men | 8.5 (7.6, 9.3) | 1.2 (−2.3, 4.7) | 3.0 (2.4, 3.5) | 4.4 (−1.7, 10.8) | 4.6 (4.0, 5.3) | −1.0 (−5.7, 3.8) |
| White Women | 4.7 (4.4, 5.1) | −0.2 (−2.6, 2.3) | 2.9 (2.6, 3.1) | 2.1 (−1.3, 5.5) | 1.4 (1.2, 1.6) | −1.4 (−6.1, 3.5) |
| White Men | 5.8 (5.3, 6.2) | 3.3 (0.6, 6.1) | 2.4 (2.1, 2.7) | 7.2 (2.8, 11.7) | 2.7 (2.4, 3.0) | 1.3 (−2.6, 5.4) |
| Recurrent ADHF | ||||||
| Black Women | 23.0 (21.8, 24.2)†‡ | 5.1 (3.1, 7.1)† | 8.8 (7.9, 9.6)†‡ | 9.9 (6.1, 13.9)‡ | 10.8 (9.9, 11.7)†‡ | 2.3 (−0.8, 5.6) |
| Black Men | 29.7 (28.2, 31.2) | 4.4 (2.6, 6.2) | 6.7 (5.9, 7.5) | 6.3 (1.8, 11.0) | 20.2 (18.9, 21.5) | 3.7 (1.4, 6.0) |
| White Women | 10.5 (10.0, 10.9) | 2.8 (1.2, 4.5) | 5.0 (4.6, 5.3) | 8.3 (5.7, 11.0) | 4.1 (3.8, 4.4) | −0.1 (−2.9, 2.7) |
| White Men | 15.0 (14.3, 15.6) | 2.3 (0.7, 3.9) | 3.9 (3.5, 4.2) | 3.1 (−0.4, 6.7) | 9.5 (9.0, 10.1) | 3.0 (0.8, 5.2) |
First ADHF was defined as cases with no history of prior heart failure diagnosis.
p<0.05 for comparison between race subgroups within the HF category.
p<0.05 for comparison between sex subgroups within the HF category.
Abbreviations:
AAPC = average annual percent change
AER = average event rates (number of ADHF events per year) per 1000 persons
HF = heart failure
HFpEF = heart failure with preserved ejection fraction
HFrEF = heart failure with reduced ejection fraction
Figure 4.
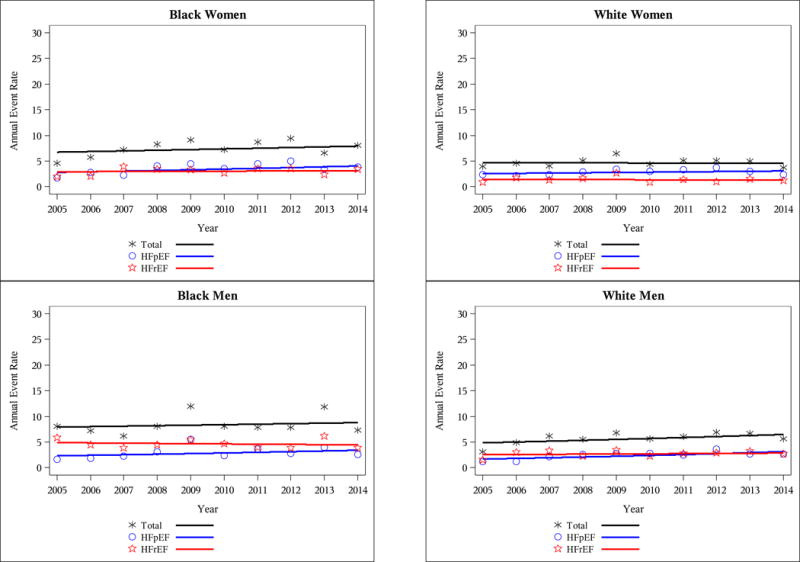
Age-adjusted annual event rates per 1000 for first hospitalized acute decompensated heart failure events (ADHF), by heart failure type, race and sex: Atherosclerosis Risk in Communities Study Heart Failure Community Surveillance 2005–2014. First ADHF was defined as cases with no history of prior heart failure diagnosis.
Table 5.
Deaths within 28 days and 1 year of acute decompensated heart failure hospitalization, age-adjusted case fatality and average annual percent change (AAPC), by heart failure type*, race and sex: Atherosclerosis Risk in Communities Study Heart Failure Community Surveillance 2005-2014.
| Total | HFpEF | HFrEF | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | 28-day CF (%) | AAPC (%) | N | 28-day CF (%) | AAPC (%) | N | 28-day CF (%) | AAPC (%) | |
| First ADHF* | |||||||||
| Black Women | 120 | 8.8 (5.4,12.2)† | −10.5 (−26.9, 6.0) | 34 | 5.2(1.5,8.9)† | −12.4 (−47.8, 23.1) | 50 | 9.9(4.5,15.2) | 5.7 (−13.2, 24.5) |
| Black Men | 60 | 6.2 (3.3,9.0) | 0.8 (−17.6, 19.3) | 18 | 5.0(0.6,9.5) | 40.7 (−10.7, 92.1) | 39 | 7.7(3.0,12.3) | −8.0 (−28.1, 12.2) |
| White Women | 566 | 11.8 (9.4,14.3) | −6.3 (−14.5, 1.8) | 277 | 9.6(6.7,12.5) | −6.4 (−18.7, 6.0) | 177 | 12.5(8.3,16.7) | −0.5 (−10.8, 9.9) |
| White Men | 461 | 12.5 (9.7,15.2) | −2.6 (−11.8, 6.6) | 177 | 11.0(7.2,14.9) | −2.3 (−16.3, 11.6) | 242 | 14.3(10.1,18.5) | −3.8 (−16.2, 8.6) |
| Recurrent ADHF | |||||||||
| Black Women | 449 | 10.7 (8.6,12.8) | −5.0 (−13.0, 3.0) | 127 | 8.0(5.1,10.9) | 6.9 (−5.8, 19.7) | 252 | 12.2(8.9,15.5) | −3.8 (−16.2, 8.6)† |
| Black Men | 313 | 10.1 (8.1,12.1) | −4.2 (−10.3, 1.9) | 63 | 8.6(4.8,12.3) | −8.7 (−22.3, 4.8) | 221 | 10.5(8.0,13.1) | −8.8 (−19.0, 1.5) |
| White Women | 1238 | 11.7 (10.1,13.3) | −0.6 (−6.2, 4.9) | 547 | 10.3(8.1,12.5) | 1.0 (−7.1, 9.1) | 474 | 12.0(9.5,14.6) | −3.0 (−10.3, 4.4) |
| White Men | 1177 | 12.0 (10.4,13.7) | −0.1 (−5.3, 5.2) | 312 | 12.2(9.0,15.3) | 2.0 (−7.6, 11.5) | 689 | 11.2(9.2,13.1) | −0.4 (−9.2, 8.4) |
|
| |||||||||
| N | 1-year CF (%) | AAPC (%) | N | 1-year CF (%) | AAPC (%) | N | 1-year CF (%) | AAPC (%) | |
|
| |||||||||
| First ADHF | |||||||||
| Black Women | 335 | 23.3 (18.7,28.0) | −8.7 (−16.5, −0.8) | 137 | 19.8 (13.7,25.9) | −6.6 (−20.1, 6.9) | 130 | 22.9 (15.6,30.2) | −6.8 (−19.2, 5.6) |
| Black Men | 261 | 28.8 (23.0,34.6) | −0.2 (−6.9, 6.5) | 80 | 22.7 (14.4,30.9) | 3.5 (−11.4, 18.5) | 152 | 32.8 (24.1,41.5) | −1.1 (−9.1, 7.0) |
| White Women | 1325 | 28.5 (25.0,31.9) | 0.1 (−4.7, 4.9) | 745 | 26.4 (22.2,30.7) | −2.2 (−8.6, 4.3) | 382 | 28.0 (21.7,34.3) | 8.6 (0.3, 16.9) |
| White Men | 1161 | 31.4 (27.7,35.1) | −0.1 (−4.9, 4.8) | 456 | 28.7 (23.3,34.2) | 2.5 (−5.6, 10.6) | 534 | 31.2 (25.8,36.5) | −0.0 (−6.9, 6.9) |
| Recurrent ADHF | |||||||||
| Black Women | 1447 | 33.4 (30.3,36.5)†‡ | −4.9 (−8.4, −1.5)† | 460 | 27.5 (22.9,32.2)†‡ | −7.7 (−14.4, −1.1)† | 757 | 37.5 (32.8,42.1) | −2.7 (−7.3, 1.8) |
| Black Men | 1194 | 35.2 (31.9,38.6) | −5.6 (−8.6, −2.6) | 218 | 29.5 (23.4,35.5) | −5.9 (−12.8, 1.0) | 868 | 37.6 (33.4,41.8) | −5.6 (−9.1, −2.0) |
| White Women | 3688 | 36.3 (33.8,38.8) | −2.7 (−5.3, −0.1) | 1681 | 34.1 (30.4,37.7) | −2.6 (−6.4, 1.2) | 1445 | 36.7 (32.9,40.6) | −2.2 (−6.5, 2.1) |
| White Men | 3849 | 40.4 (37.9,42.9) | −1.6 (−4.0, 0.9) | 1049 | 42.3 (37.4,47.2) | 2.8 (−1.6, 7.3) | 2300 | 38.0 (34.9,41.2) | −2.4 (−5.5, 0.8) |
First was defined as cases with no history of prior heart failure diagnosis.
p<0.05 for comparison between race subgroups within the HF category.
p<0.05 for comparison between sex subgroups within the HF category.
N denotes the number of deaths.
Abbreviations:
AAPC = average annual percent change
CF = average case fatality percentage
HF = heart failure
HFpEF = heart failure with preserved ejection fraction
HFrEF = heart failure with reduced ejection fraction
To enhance comparability with other community population studies (e.g., Olmsted County5,8), we defined HFrEF as EF as <50% since the beginning of ARIC HF Community Surveillance in 2005. Using other cut-points such as EF ≤40 or ≤45% resulted in higher event rates for HFpEF and lower event rates for HFrEF as expected, but did not substantially alter the trends observed using the original EF cut-point (Supplemental Table 3).
DISCUSSION
From 2005 to 2014, in the biracial ARIC Study communities, the average age-adjusted rates of first hospitalized HF were higher in blacks, with differences seen by HF type and sex. Over these 10 years, the rates of all first hospitalizations for ADHF increased in all race-sex subgroups, most notably for HFpEF. While the rate of first hospitalization for acute HFrEF was higher in black men, a significant, but modest, rise in first hospitalized acute HFrEF rate was seen in only white men; women and black men showed no statistically significant changes in HFrEF trends.
Reasons for the observed differences over time by sex, race and HF type may be related to temporal trends in coding hospital discharges and using biomarkers such as B-type natriuretic peptide for diagnosing HF. Whether increased recognition of HFpEF contributes to an increase in HFpEF diagnosis and thus its incidence is unknown. However, differences by race and sex may be related to different trends in comorbidities or etiologies of HF. For example, the incidence of acute myocardial infarction and rates of CHD deaths are decreasing14, 15; perhaps this trend may explain why there is no significant change in HFrEF incidence over time, since CHD is associated more with HFrEF than HFpEF. Common comorbidities related to HFpEF are on the rise and include atrial fibrillation16, hypertension, obesity, and diabetes17. There are well-recognized race and sex differences for these known risk factors for HF and other cardiovascular diseases; e.g., blacks have a higher prevalence of hypertension than whites, and black women have a higher prevalence of obesity compared to white women3. Black patients in the ARIC communities were more likely to have chronic kidney disease; but whether chronic kidney contributes to more ADHF is controversial18. Further investigation is needed to determine whether a specific comorbidity, compared to another, is more associated with first hospitalization for ADHF.
We report trends in the ARIC Study communities that are in contrast to the findings in other populations, where the incidence of heart failure among all ages declined in Olmsted County, MN, from 2000 to 20105, in the Clinical Practice Research Datalink (CPRD) cohort in the United Kingdom from 2002 to 201419, and in Medicare beneficiaries from 1994 to 200320 and 2002 to 201321, respectively. However, the trends in the ARIC communities are similar to older reports from Olmsted County (1987-2001)8 and recent preliminary findings in the Framingham cohort for which HFpEF incidence increased over 19 years22. The recurrent HF hospitalization trends in the ARIC Study are also in contrast to the 10-year trends seen in the Medicare population and in the National Inpatient Sample, which included both incident and recurrent hospitalizations and showed a decline in all HF hospitalization from 1998 to 2008 and from 2002 to 2013, respectively, with blacks having higher HF hospitalization rates than whites23, 24. The heterogeneity of findings across studies likely reflects differences in population demographics and definitions of HF. Notably, our ARIC community surveillance study population was restricted to white and black residents age ≥55 years, and our definition of HF incidence is based on first decompensation leading to hospitalization and did not include outpatient cases. The Olmsted County population sample and Framingham cohort are relatively homogenous with >90% of participants of white race/ethnicity, include both outpatient and inpatient HF cases (identified by ICD-9 codes and validated using the Framingham Study HF criteria), and did not differentiate between acute and chronic stable HF. The Framingham Study used a LVEF 45% cutoff to define HFpEF25; thus more HFpEF and less HFrEF were classified in their analyses. The U.K. CPRD cohort was also >95% white19. The Medicare population is restricted to age 65 years and older, whereas over 20% of the black population in the ARIC communities were age 55-64 years. HF cases in the National Inpatient Sample, the Medicare populations, and the U.K CPRD sample were classified using administrative claims data based on inpatient and/or outpatient ICD-9-CM or ICD-10 codes, defining incident HF as the initial HF hospitalization within the specified time period, and did not involve case adjudication. Of note, our previous reports suggest that HF hospitalization identified solely by ICD-9 codes may not accurately estimate the rates of ADHF9, missing up to 50% of cases26.
Despite the rise in the rate of first hospitalization for ADHF, especially for HFpEF, there were no consistent or significant changes in 28-day mortality after hospital discharge from 2005 to 2014, regardless of LVEF or HF type, or history of hospitalized HF. However, 1-year mortality decreased over the ten years, by 5-7% per year, in black women with first hospitalized ADHF and recurrent hospitalized ADHF, and in black men with recurrent ADHF. Yet, 1-year survival was similar for HFpEF and HFrEF for most race-sex groups regardless of history of hospitalized HF (except for black men with recurrent HFrEF whose 1–year mortality decreased 5.8% per year). This minimal change in survival by HF type is in contrast to reports from Olmsted County where the survival is better for HFpEF than HFrEF5, 8, and the trends where HF type was not specified15, 27. Our unique results may be related to the more diverse, biracial population of the ARIC population. Lower age-adjusted case fatality rates were observed in blacks in each sex group (particularly among blacks with HFpEF), despite higher first hospitalization rates of ADHF rates compared to whites. A similar racial difference was seen in the HFpEF cohort of the Get With The Guidelines-Heart Failure registry (linked to the Centers for Medicare & Medicaid Services administrative data) between 2006 and 201428. This racial difference may be related to younger age of HF onset in blacks and incomplete adjustment for other related factors.
Moreover, it is notable that the average age-adjusted 1-year mortality rates for first hospitalized ADHF, regardless of HF type, is approximately 30% for all race-sex groups, which is higher than estimates of approximately 20% based on populations from the Framingham Heart Study3 and Olmsted County5 (which included outpatient, presumably milder cases), but similar to estimates based on all acute HF hospitalizations from the Worchester Heart Failure Study27 and the Medicare population15. Particular to the ARIC Study is the ability to differentiate recurrent ADHF hospitalizations, which were associated with modestly higher 1-year mortality rates compared to first hospitalized cases, with no significant change over time and no demonstrable differences by race-sex groups. Reasons for these higher 1-year mortality estimates for both first and recurrent hospitalized ADHF events in the ARIC communities are most likely related to the definition of our hospitalized HF cases, as only hospitalized cases that were considered acute and decompensated were included, which would reflect a sicker patient population. Moreover, compared to the Olmsted County sample5, this ARIC population was older and included more patients with comorbidities such as CHD, hypertension, diabetes, and obesity. Evidence-based HF therapy may also be underprescribed in the ARIC communities (e.g., only 50% of HFrEF patients were on optimal medical therapy)29. Given the focus of providers, payors, and health care systems to decrease readmission rates for ADHF, seeing these survival trends in both first and recurrent hospitalized ADHF may translate to more attention on the medical management of hospitalized patients with HF.
Our study is not without limitations. A design limitation of community-wide, retrospective surveillance of hospitalizations that use survey sampling methods is that follow-up of individual patients beyond vital status is not routinely incorporated. Therefore details about the patient’s care beyond that sampled hospitalization are limited to only what is noted in the index hospital records, which may result in potential misclassification between “first” and “recurrent” ADHF hospitalizations. Because subsequent and prior hospitalizations cannot be linked to the index ADHF hospitalization, recurrent ADHF could have been misclassified in our study as a first hospitalization for ADHF. Furthermore, our definition of incident hospitalized HF is based on the lack of prior hospitalization for HF and includes patients with a prior diagnosis of HF (56%). Therefore, cases we classified as first hospitalized events may in fact include patients who experienced HF symptoms and received treatment outside the hospitalization setting. First hospitalization rates are also subject to misclassification bias with potential overestimation if prior HF hospitalizations were not noted in the abstracted medical records, especially in the early years before widespread use of electronic medical records. Therefore, these limitations could have led us to overestimate the rate of first hospitalization for ADHF. In a sensitivity analysis with an alternative definition of first ADHF, the pattern of increased event rates shifted from first to recurrent hospitalization for ADHF.
However, there is variation in the literature as to the optimal method for pinpointing the first onset of HF in population based studies. Since its inception, ARIC Community Surveillance has focused on identifying cardiovascular events that are serious enough to require hospitalization, as we have done for coronary heart disease since 198711. First hospitalization is a reasonable surrogate for HF incidence based on estimates from other studies. For example, most incident HF cases diagnosed in the outpatient setting in Olmsted County (74%) were hospitalized within 1.7±3.1 years of the diagnosis7.
Second, as with any observation study, this analysis was not powered to detect interactions between various subgroups (e.g., race-sex interaction by HF type). But we present the results stratified by race and sex and HF type, which would address potential significant subgroup interactions. Finally, the current study did not include outpatient HF events that did not eventually result in hospital admission. The goal and design of ARIC HF Community Surveillance was to assess the burden of hospitalized ADHF rather than the total burden of HF, which naturally restricts case identification. Nevertheless, the ARIC study has been the first to differentiate hospitalization rates of ADHF from chronic HF in a biracial community-based population, focusing on acute HF in order to provide better estimates of trends of the HF burden in the general population.
Other limitations of this study include that our study population originates from four U.S. communities, is restricted to those ≥55 years old, and therefore does not represent the total U.S. population. National trends will vary given the different proportions of different racial and ethnic groups across the country.
In summary, in this biracial population of four U.S. communities, trends in hospitalized ADHF from 2005 to 2014 differ by sex and race with an overall increase in first hospitalization events primarily due to HFpEF. Mortality rates from ADHF are higher than what has been previously reported in other U.S. population samples. The trends seen in this current study should be confirmed in other diverse population-based studies.
Supplementary Material
CLINICAL PERSPECTIVE.
What’s New
Ten-year rates and trends of hospitalized acute decompensated heart failure (ADHF) differ by race/sex and HF type (preserved versus reduced ejection fraction, HFpEF vs HFrEF) in the Atherosclerosis Risk in Communities (ARIC) Surveillance Study.
Acute HFrEF was more common in black men and white men; acute HFpEF was most common in white women.
Rates of hospitalized ADHF increased over time, with higher rates in blacks and rising cases of HFpEF.
Mortality rates were ~30% at 1 year, with a more pronounced decrease over time in blacks, but generally did not differ by HF type.
Clinical Implications
While overall national trends may vary by geographic region, blacks in the four ARIC communities had higher rates and trends of ADHF hospitalizations compared to whites, but also had lower age-adjusted 1-year case fatality in each sex group (particularly black women with HFpEF).
This racial difference may be related to younger age of HF onset, comorbidities, and other community-level and socioeconomic factors that may affect HF trends.
Given the national focus to decrease readmission rates for ADHF, more attention on the medical management of hospitalized patients with ADHF is also warranted.
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions, and particularly Dingyi Zhao, MS, Kim Ring, MPH, and Marina Bessell, MS for statistical support of this manuscript.
FUNDING SOURCES
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). The authors thank the staff and participants of the ARIC study for their important contributions.
Footnotes
DISCLOSURES
None.
References
- 1.Sidney S, Rosamond WD, Howard VJ, Luepker RV, National Forum for Heart D. Stroke P. The “heart disease and stroke statistics–2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013;127:21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine (US) Committee on a National Surveillance System for Cardiovascular and Select Chronic Diseases. A Nationwide Framework for Surveillance of Cardiovascular and Chronic Lung Diseases. Washington DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB, American Heart Association Statistics C and Stroke Statistics S Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG, American Heart Association Advocacy Coordinating C, Council on Arteriosclerosis T, Vascular B, Council on Cardiovascular R, Intervention, Council on Clinical C, Council on E Prevention. Stroke C. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, Killian JM, Roger VL. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175:996–1004. doi: 10.1001/jamainternmed.2015.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long-term trends in the incidence of and survival with heart failure. N Eng J Med. 2002;347:1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 7.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 8.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 9.Chang PP, Chambless LE, Shahar E, Bertoni AG, Russell SD, Ni H, He M, Mosley TH, Wagenknecht LE, Samdarshi TE, Wruck LM, Rosamond WD. Incidence and survival of hospitalized acute decompensated heart failure in four US communities (from the Atherosclerosis Risk in Communities Study) Am J Cardiol. 2014;113:504–510. doi: 10.1016/j.amjcard.2013.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Heart, Lung, and Bloof Institute. Atherosclerosis Risk in Communities Study (ARIC) 2017 Feb 3; https://biolincc.nhlbi.nih.gov/studies/aric/?q=aric.
- 11.Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni A, Shahar E, Deswal A, Heiss G, Chambless LE. Classification of Heart Failure in the Atherosclerosis Risk in Communities (ARIC) Study: A Comparison of Diagnostic Criteria. Circ Heart Fail. 2012;5:152–159. doi: 10.1161/CIRCHEARTFAILURE.111.963199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atherosclerosis Risk in Communities (ARIC) Manual 3A: Surveillance of Heart Failure Manual of Operations: Version 2.0. 2009 Feb; http://www.cscc.unc.edu/aric/visit/Surveillance_Procedures_-_Heart_Failure.6_3a.pdf.
- 13.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49:223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 14.Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-Two Year Trends in Incidence of Myocardial Infarction, CHD Mortality, and Case-Fatality in Four US Communities, 1987 to 2008. Circulation. 2012;125:1848–1857. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999-2011. Circulation. 2014;130:966–975. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piccini JP, Hammill BG, Sinner MF, Jensen PN, Hernandez AF, Heckbert SR, Benjamin EJ, Curtis LH. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries, 1993–2007. Circ Cardiovasc Qual Outcomes. 2012;5:85–93. doi: 10.1161/CIRCOUTCOMES.111.962688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Burden of Metabolic Risk Factors for Chronic Diseases C. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–647. doi: 10.1016/S2213-8587(14)70102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsushita K, Ballew SH, Coresh J. Influence of chronic kidney disease on cardiac structure and function. Curr Hypertens Rep. 2015;17:581-015–0581-x. doi: 10.1007/s11906-015-0581-x. [DOI] [PubMed] [Google Scholar]
- 19.Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, Allison M, Hemingway H, Cleland JG, McMurray JJV, Rahimi K. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. 2017 doi: 10.1016/S0140-6736(17)32520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curtis LH, Whellan DJ, Hammill BG, Hernandez AF, Anstrom KJ, Shea AM, Schulman KA. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008;168:418–24. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 21.Khera R, Pandey A, Ayers CR, Agusala V, Pruitt SL, Halm EA, Drazner MH, Das SR, de Lemos JA, Berry JD. Contemporary Epidemiology of Heart Failure in Fee-For-Service Medicare Beneficiaries Across Healthcare Settings. Circ Heart Fail. 2017;10 doi: 10.1161/CIRCHEARTFAILURE.117.004402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsao CW, Lyass A, Larson MG, Vasan RS. Divergent Temporal Trends in the Incidence of Heart Failure with Preserved and Reduced Ejection Fraction. Circulation. 2015;131:A23. doi: 10.1016/j.jchf.2018.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306:1669–1678. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National Differences in Trends for Heart Failure Hospitalizations by Sex and Race/Ethnicity. Circ Cardiovasc Qual Outcomes. 2017 Jul;10(7):e003552. doi: 10.1161/CIRCOUTCOMES.116.003552. pii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ho JE, Lyass A, Lee DS, Vasan RS, Kannel WB, Larson MG, Levy D. Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circ Heart Fail. 2013;6:279–286. doi: 10.1161/CIRCHEARTFAILURE.112.972828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agarwal SK, Wruck L, Quibrera M, Matsushita K, Loehr LR, Chang PP, Rosamond WD, Wright J, Heiss G, Coresh J. Temporal Trends in Hospitalization for Acute Decompensated Heart Failure in the United States, 1998-2011. Am J Epidemiol. 2016;183:462–470. doi: 10.1093/aje/kwv455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park D, McManus D, Darling C, Goldberg JH, Gore JM, Lessard D, Goldberg RJ. Recent trends in the characteristics and prognosis of patients hospitalized with acute heart failure. Clin Epidemiol. 2011;3:295–303. doi: 10.2147/CLEP.S25799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ziaeian B, Heidenreich PA, Xu H, DeVore AD, Matsouaka RA, Hernandez AF, Bhatt DL, Yancy CW, Fonarow GC. Race/Ethnic Differences in Outcomes Among Hospitalized Medicare Patients With Heart Failure and Preserved Ejection Fraction. JACC Heart Fail. 2017;5:483–493. doi: 10.1016/j.jchf.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang PP, Wruck LM, Kloss RA, Loehr LR, Russell SD, Punjabi NM, Bertoni AG, Miller ER, Shahar E, Rosamond WD. The Impact of Optimal Therapy on Survival of Hospitalized Acute Decompensated Heart Failure: The ARIC Study. Circulation. 2015;131:AP384. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


