A young female and her sister presented with similar complaints of persistent erythema of the face associated with burning sensation for the past few months. On further inquiring, both of them acknowledged the use of topical clobetasol propionate on their face for past one year. On examination, hypertrichosis along with telangiectasias on an erythematous background were found to be present. [Figure 1a and b]. Dermoscopy (Dinolite AM413ZT; polarizing) revealed the presence of irregularly dilated, branched tortuous vessels almost interconnecting with each other giving a “polygonal pattern.” Between the larger interconnecting vessels, there were nonlinear smaller vessels and red dots. White structureless areas and yellowish areas were also visible [Figure 2a and b]. Coarse terminal hairs were also noticed over these areas.
Figure 1.
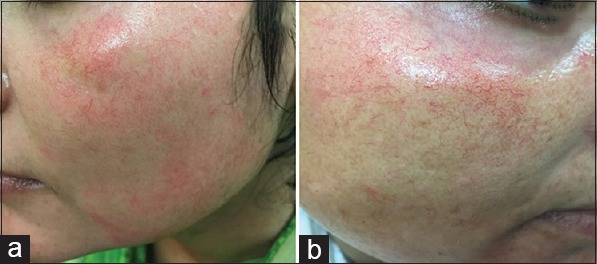
(a and b) Topical steroid damaged face of the two sisters
Figure 2.
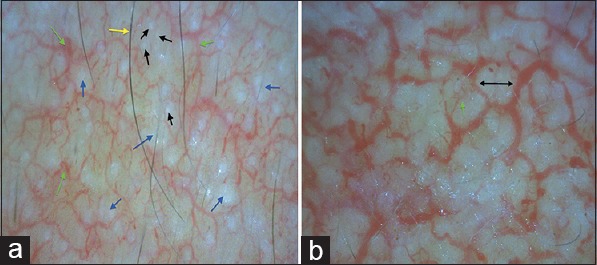
(a) Polarising dermoscopy at a lower magnification showing dilated tortuous branched vessels (green arrow) with inter winning structureless white areas (blue arrow) and terminal hairs (yellow arrow). Openings of sebaceous glands have been marked as black arrows. [Dinolite AM413ZT; 50X; Polarising]. (b) Polarising dermoscopy at a higher magnification showing almost interconnected vessels giving a ‘polygonal appearance’ (black double arrow) and smaller non-linear vessels (green arrow). [Dinolite AM413ZT; 200X; Polarising]
Topical steroid damaged/dependent face (TSDF) has been defined as a semi-permanent or permanent damage to the skin of the face precipitated by the irrational, indiscriminate, unsupervised, or prolonged use of topical corticosteroids (TC) resulting in a plethora of cutaneous signs and symptoms and psychological dependence on the drug.[1] Facial skin is thinner, and hence, not only percutaneous absorption of drugs is increased but the side effects are also early and severe as compared to other sites like back and abdomen.[2] The clinical picture of TSDF appears due to a combination of dermal atrophy (TC inhibit collagen and hyaluronic acid synthesis by fibroblasts),[2] local immunosuppression, and inhibition of action of nitric oxide (NO).[3,4] On withdrawal of TC, endothelial NO is released causing vasodilation and erythema.[3] On dermoscopy, dilated vessels as a result of vasodilation are observed. The tortuosity of these vessels is due to the lack of support to vasculature as a result of steroid induced dermal atrophy. Dermal atrophy is visible as white structureless areas. Yellowish areas may correspond with increased skin transparency due to epidermal atrophy. One important differential of TSDF is erythematotelangiectatic rosacea (ER). Dermoscopic features of ER include polygonal vessels, superficial scales, follicular plugs, and features related to demodicidosis.[5] Except for polygonal vessels these features are not seen in TSDF. To conclude, dermoscopy of TSDF can help in diagnosis as well as in monitoring patient's adherence to management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lahiri K, Coondoo A. Topical steroid damaged/dependent face (TSDF): An entity of cutaneous pharmaco dependence. Indian J Dermatol. 2016;61:265–72. doi: 10.4103/0019-5154.182417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnes L, Kaya G, Rollason V. Topical corticosteroid-induced skin atrophy: A comprehensive review. Drug Saf. 2015;38:493–509. doi: 10.1007/s40264-015-0287-7. [DOI] [PubMed] [Google Scholar]
- 3.Rapaport MJ, Rapaport V. The Red Skin Syndromes: Corticosteroid addiction and withdrawal. Expert Rev Dermatol. 2006;1:547–61. [Google Scholar]
- 4.Fisher M. Steroid-induced rosacea like dermatitis: Case report and review of the literature. Cutis. 2009;83:198–204. [PubMed] [Google Scholar]
- 5.Lallas A, Argenziano G, Longo C, Moscarella E, Apalla Z, Koteli C, et al. Polygonal vessels of rosacea are highlighted by dermoscopy. Int J Dermatol. 2014;53:e325–7. doi: 10.1111/ijd.12270. [DOI] [PubMed] [Google Scholar]


