Abstract
Objective
Continuity of care is a long-standing feature of healthcare, especially of general practice. It is associated with increased patient satisfaction, increased take-up of health promotion, greater adherence to medical advice and decreased use of hospital services. This review aims to examine whether there is a relationship between the receipt of continuity of doctor care and mortality.
Design
Systematic review without meta-analysis.
Data sources
MEDLINE, Embase and the Web of Science, from 1996 to 2017.
Eligibility criteria for selecting studies
Peer-reviewed primary research articles, published in English which reported measured continuity of care received by patients from any kind of doctor, in any setting, in any country, related to measured mortality of those patients.
Results
Of the 726 articles identified in searches, 22 fulfilled the eligibility criteria. The studies were all cohort or cross-sectional and most adjusted for multiple potential confounding factors. These studies came from nine countries with very different cultures and health systems. We found such heterogeneity of continuity and mortality measurement methods and time frames that it was not possible to combine the results of studies. However, 18 (81.8%) high-quality studies reported statistically significant reductions in mortality, with increased continuity of care. 16 of these were with all-cause mortality. Three others showed no association and one demonstrated mixed results. These significant protective effects occurred with both generalist and specialist doctors.
Conclusions
This first systematic review reveals that increased continuity of care by doctors is associated with lower mortality rates. Although all the evidence is observational, patients across cultural boundaries appear to benefit from continuity of care with both generalist and specialist doctors. Many of these articles called for continuity to be given a higher priority in healthcare planning. Despite substantial, successive, technical advances in medicine, interpersonal factors remain important.
PROSPERO registration number
CRD42016042091.
Keywords: continuity of care, mortality, systematic review, doctors, doctor patient relationship
Strengths and limitations of this study.
The first systematic review of continuity of care and mortality.
We included studies working with patients with all conditions, of all ages and of all stages of conditions.
We included articles investigating continuity with all kinds of doctors in any health system.
We included articles using any clearly defined measure of continuity of care.
A meta-analysis was not possible due to heterogeneity of continuity and mortality measures.
Introduction
Medical science has advanced rapidly since the early 19th century. Major advances from the germ theory to the sequencing of the human genome have together generated much deeper understanding of the pathophysiology of disease with improved prevention and treatment. However, all these advances are mostly related to physical factors. Research on human aspects of medical care has lagged.
Internationally, there has been a decrease in the perceived value of personal contact between patients and doctors. An editorial in the New England Journal of Medicine 1 suggested that non-personal care should become the ‘default option’ in medicine.
One way to study interpersonal care is by measuring continuity of care. The definition of continuity of care that we have used previously2 is repeated contact between an individual patient and a doctor. Such repeated contact gives patients and doctors the opportunity for improved understanding of each other’s views and priorities. Continuity of care can be considered to be a proxy measure for the strength of patient–doctor relationships.3
There have been a variety of approaches to measure continuity and so far only three randomised controlled trials have been completed.4–6 These all showed continuity to be beneficial for patients over relatively short periods. However, RCTs are problematic with pre-existing long-term human relationships, like marriage and parent–child relationships, as prospective randomisation is almost impossible. Some doctor–patient relationships last for decades and become highly personal, and therefore RCTs are unethical or impractical. Observational studies have inherent limitations, and investigating continuity of care has certain problems, in particular that of reverse causality; poor health or death early in the study leading to a low measured level of continuity.7 However, study teams are increasingly aware of this and use study designs and analytical methods to reduce and account for it.
There is a clear rationale for the effectiveness of continuity of care as doctors collect ‘accumulated knowledge’8 about an individual patient which they then use in subsequent consultations to tailor advice.
Continuity of care in general practice is associated with greater patient satisfaction,9 improved health promotion,10 increased adherence to medication11 and reduced hospital use.12 Given all these separate benefits, the question arises whether these extend to mortality rates. Death is clearly the most important and serious of all outcomes.
Since 2010, individual studies have emerged investigating whether continuity of care is associated with reduced mortality, including some with specialists.13–35 These reports represent a new development, underlining the interpersonal component of medical care.
Research question
Are higher levels of continuity of doctor care, in any setting, with any patient group, associated with changed mortality?
Methods
Search strategy and selection criteria
For inclusion in this systematic review (without meta-analysis), articles must have been published in the peer-reviewed literature, in the last 21 years, in English. We searched the databases of MEDLINE, Embase and the Web of Science from 1996 to 2017 by searching for ‘continuity’ OR ‘continuity of care’ together with terms for a medical doctor/physician and terms indicating death or mortality in the title or abstract (see online supplementary information—example search strategy). In addition, references of articles selected were hand-searched for additional relevant citations.
bmjopen-2017-021161supp001.pdf (191.1KB, pdf)
Experimental and observational study designs were considered including controlled trials, cohort studies (prospective and retrospective) and case–control studies. Systematic reviews and meta-analyses were excluded. Study participants could include any patient group, including entire populations or groups of patients with a specific disease or other feature.
Articles must have compared measured degrees of continuity of care with doctors (of any kind) to mortality rates. Any valid measure of continuity was considered, including continuity being lost or absent and articles where the continuity measure was a single appointment or visit by a general practitioner/family physician during a hospital stay. Articles about organisational continuity and general staffing numbers were excluded.
As an outcome measure, any measure of mortality was accepted, that is, all-cause, time/age-limited or cause-specific. When complications or hospital admissions were combined with death rates, we sought a separate measure of mortality alone. If this was not available, studies were excluded.
Two pairs of reviewers checked the search results and decided independently whether papers met the eligibility criteria. Initially, the title and abstract of each citation was screened. The full texts of selected articles were then examined. Disagreements were resolved by discussion, and PHE independently had the deciding vote.
Data items
The variables and outcomes extracted included basic information: authors, date and country. We also extracted study design, study population (any particular condition, setting, age group, any other inclusion or exclusion criteria and selection method), numbers of patients, measure of continuity, length of continuity measurement and doctor type (generalist doctor including general practitioner, family physician and primary care physician or specialist). We extracted the period of time for the mortality measurement, and any overlap with or interval between mortality and continuity measurement periods. We also extracted whether mortality was all-cause or a disease-specific cause or limited to a particular group, how mortality was assessed and confounding factors tested or accounted for. We also extracted an estimation of any association found, with risk ratio or OR where possible and whether higher continuity was linked to an increased or decreased mortality risk. Data were extracted independently by two reviewers (of DJPG, EW, AT and KSL), using the data-extraction table designed for this review. Disagreements were resolved as described previously.
Risk of bias
The quality and risk of bias were assessed independently for individual studies by two reviewers using the Newcastle-Ottawa Scale.36 We also assessed relevant areas of bias in terms of the timing of continuity and mortality measurement and confounding factors considered. For continuity of care and mortality, there is a particular potential for bias in that the worsening of health status before death may cause either decreased or increased continuity of care (reverse causality),7 so we noted whether this had been considered and adjusted for in study design. In terms of bias across studies, we considered publication bias and reporting bias in terms of whether mortality was the primary outcome.
Data analysis
Studies were analysed for a relationship between continuity of care and mortality rates, and whether this relationship was an inverse one (ie, greater continuity of care led to lower mortality rates) or not. For each study, we sought a risk metric (ie, relative risk ratio, HR or OR) from an adjusted model of data analysis in order to minimise the risk of selection bias and confounding. Where these statistical metrics were not reported, we provided any other available comparison measure.
Patient involvement statement
DJPG is a member of the St Leonard’s Practice Patient Participation Group as well as the Patron of the National Association for Patient Participation. As such, he is a patient representative as well as an author. The research question and outcomes were therefore conceived by a patient from the practice based on the priorities, experience and preferences stated by patients at successive national patient conferences.
Results
Study selection
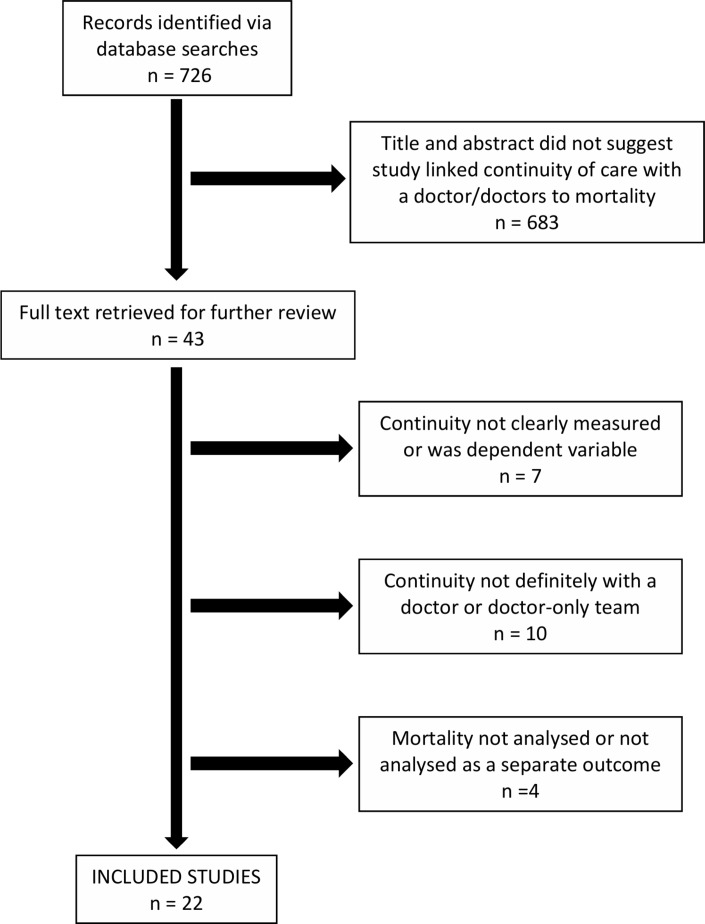
After removal of duplicate results, 726 peer-reviewed publications were identified. No previous systematic reviews or trials on this subject were found. Of the 726 papers identified, 43 papers were selected for full-text review (figure 1). Articles were then excluded if continuity was not clearly measured or was the dependent variable,37–42 if the continuity of care measure was not clearly with a doctor or doctors only35 43–49 and if mortality was not analysed or not analysed separately at any point50–52 (eg, if it was expressed only as a composite outcome with hospitalisation). This left 22 studies for inclusion.
Figure 1.
Study selection flow diagram.
Study characteristics
As shown in table 1, the majority of included reports (15, 68.2%) were of retrospective cohort studies, often using insurance data. There were four prospective cohort and three cross-sectional studies. No randomised controlled trials were found. A number of cohort studies included large numbers of patients (median 16 855). All of the reports were published since 2010. The studies were carried out in nine different countries; the majority were from North America (Canada 6, USA 5). Seven were from Europe (England 3, France 2, Croatia 1 and the Netherlands 1). There were two from Taiwan and one each from Israel and South Korea.
Table 1.
Studies investigating the link between continuity and mortality that meet the inclusion criteria, ordered by study design
| First author and year of publication | Country of origin | Patients | Study design | Number of patients if cohort study | Continuity measure | Continuity with | Length of time continuity measured | Confounding factors checked and/or adjusted for | Mortality measure | Quality score (mean (of two reviewers) |
Mortality primary outcome? | Length of time mortality counted |
| Bentler 201413 | USA | 65 years+, community residing Medicare beneficiaries who completed NHHSUQ survey, not in managed care, not in MMC plan. | PC | 1219 | 1, 2, 3, 5, 8 | Physician | 1–2 years | A,B,C,D,E,F,G, H,I,K,M,N,O |
All-cause time to death | 9 | Yes | Up to 5 years |
| Cerovečki 201314 | Croatia | With opioid dependence, treated with methadone in family medicine setting. | PC | 287 | 7 | Family physician | 12 years | A,B,M,O,S | All cause | 8.5 | Yes | 12 years |
| Spatz 201415 | USA | 18 years+, hospitalised with acute myocardial infarction. | PC | 2454 | 8 | Doctor | N/A | A,B,C,D,E,F,G, I,J,M,O,T |
All cause | 9 | Yes | 12 months |
| van Walraven 201016 | Canada | 18 years+, discharged into community from medical or surgical services of 11 Ontario hospitals. | PC | 3876 | 1 | Physician who saw patient before, during and/or after hospital stay | 6 months | A,B,H,L,N,O | All cause | 9 | Yes | 6 months |
| Blecker 201417 | USA | 18 years+, hospitalised at least 2 days including at least one at weekend. | RC | 3391 | 1 | Discharge physician | 2 days | A,B,C,K,N,O,T | In hospital | 8 | No | Length of hospital stay |
| Brener 201618 | Canada | 18 years+, discharged from hospital into community, family physician has history of hospital visits. | RC | 164 059 | 9 | Family physician | N/A | A,B,D,L,O,Q | All cause | 9 | Yes | 90 days postdischarge |
| Hoertel 201419 | France | In CNAMTS insurance fund, saw a psychiatrist regularly. | RC | 14 515 | 2 | Psychiatrist | 3.5 years | A,B,D,K,N,O | All cause | 8.5 | Yes | 3 years |
| Justiniano 201720 | USA | 18 years+, underwent colorectal resection and readmitted within 30 days of DC. | RC | 20 016 | 0 | Surgeon | N/A | A,B,C,I,K,O, P,Q,T,U |
All cause, colorectal cancer | 9 | Yes | 1 year |
| Leleu 201321 | France | NHI reimbursement patients, >2 visits in 6 months. | RC | 325 742 | 1, 2 | Primary care physician/GP | 3 years | A,B,D,K | All cause | 9 | Yes | 3 years |
| Liao 201522 | Taiwan | 31–99 years, with type 2 diabetes. | RC | 89 428 | 6 | Any physician | 1 year | A,B,H,K,N, O,P,U |
All cause | 8.5 | No | 4–9 years |
| Lustman 201523 | Israel | 40–75 years, with type 2 diabetes, remained in area, saw primary care provider >3x. | RC | 23 679 | 1 | Primary care physician/GP | 2 years | A,D,H,K,M, N,O |
All cause, diabetes related causes | 8.5 | Yes | 2 years |
| Maarsingh 201624 | The Netherlands | 55–85 years, data available. | RC | 1712 | 3 | GP | 17 years | A,B,D,E,F,G, K,M,Q,O |
All cause | 9 | Yes | 21 years |
| McAlister 201325 | Canada | 20 years+, DC from hospital with 1st time heart failure. | RC | 16 855 | 0, 1 | Physician who saw patient x2 in year before or 1x during admission | N/A | D,K,O,P,Q,R | All cause | 9 | Composite | 3 months/6 months |
| McAlister 201626 | Canada | 20 years+, DC from hospital with 1st time heart failure. | RC | 39 249 | 0,1 | Any physician | N/A | A,B,Q,K,M, O,H |
All cause | 8 | Composite | 30 days |
| Pan 201727 | Taiwan | 35 years+, diagnosed with type 2 diabetes, in Taiwan NHI database. | RC | 396 838 | 2 | Any physician | 8 years | A,B,D,K,O, P,Q |
All cause | 8.5 | Yes | Up to 8 years |
| Shin 201428 | South Korea | 20 years+, in Korean National Health Insurance, new diagnosis of hypertension, diabetes, hypercholesterolaemia or their complications. | RC | 47 433 | 2, 4, 5 | Physician | 2 years | A,B,D,F,K, N,Q,U |
All cause | 9 | Yes | Up to 5 years |
| Sidhu 201429 | Canada | ‘Adults’ treated and released from 93 emergency departments with first-time diagnosis of heart failure. | RC | 12 285 | 0, 1 | Physician who saw patient x2 in year before or 1x during admission | 30 days | A,B,G,K,O, P,Q,N |
All cause | 8.5 | Composite | 12 months but only give separate data for deaths for 30 days |
| Weir 201630 | USA | 20 years+, with incident diabetes and at least 2 years insurance. | RC | 285 231 | 1 | Physician who saw patient the most | 2 years | A,B,D,G, H,K,O |
All cause | 8.5 | Composite | 1 year |
| Worrall 201131 | Canada | 65 years+, with diabetes, 2+ fee-for-service family physician visits. | RC | 305 | 1 | Family physician | 3 years | A,B,N | All cause | 7 | Yes | 3 years |
| Baker 201632 | England | Registered with 7858 general practices, with complete data, in England. | CS | N/A | 8 | GP | N/A | C,D,F,G,J,P | Premature- ratio observed to expected, age <75 | 8 | Yes | N/A |
| Honeyford 201333 | England | Registered with 229 general practices in the East Midlands between April 2006 and March 2009. | CS | N/A | 8 | GP | N/A | A,B,C,D,F, G,P,U |
CHD under 75 and all age. | 8 | Yes | 3 years |
| Levene 201234 | England | 18 years+, registered with GP for at least 6/12 months of the year. | CS | N/A | 8 | GP | N/A | A,B,C,D, F,O,P |
All cause, COPD, all cancer, CHD | 9 | Yes | 2 years |
Continuity measures: 1, usual provider of care index; 2, continuity of care index; 3, Herfindahl-Hirschmann Index; 4, Modified, Modified Continuity Index; 5, most frequent provider; 6, % consistency to physician; 7, loss of contact with family physician; 8, patient survey; 9, family physician visited patient in hospital; 0, follow-up by familiar doctor.
Confounding factors: A, age; B, sex; C, race; D, deprivation/social status/income; E, education; F, smoking; G, chronic conditions; H, prior hospitalisation; I, insurance; J, acute conditions; K, co-morbidity (including Charlston Index); L, LACE Index (risk of 30-day readmission or death after hospital discharge); M, marital/relationship status; N, number of healthcare visits/service intensity; O, other healthcare history; P, practice, hospital or doctor characteristics; Q, location; R, length of hospital stay; S, treatment plan; T, timing of admission; U, other.
CS, cross-sectional; CHD, Coronary heart disease; CNAMTS, Caisse Nationale de l’Assurance Maladie des Travailleurs Salariés; COPD, Chronic Obstructive Pulmonary Disease; DC, discharged; GP, general practitioner; MMC, Medicare Managed Care; N/A, Not Applicable; NHHSUQ, National Health and Health Services Use Questionnaire; NHI, National Health Insurance; PC, prospective cohort; RC, retrospective cohort.
Nine (40.9%) of the studies investigated continuity with a general practitioner/family physician/primary care physician, 3 were with specialists only17 19 20 and 10 included continuity with doctors of any kind. Eight studies (34.8%) selected patients during or following an index hospitalisation.15–18 20 25 26 29. Five studies studied patients with diabetes22 23 27 30 31 and three studies focused on older patients.13 24 31
The continuity measures used are reported in table 1. The most common measure used was the Usual Provider of Care (UPC) index which was used in 10 studies (45.5%).13 16 17 21 23 25 26 29–31 Six studies used more than one measure, some only for sensitivity analysis.13 21 25 26 28 29 One study13 was designed to compare the association of different continuity measures with outcomes, including mortality. One article18 used the occurrence of a supportive visit by a family physician to a patient in hospital and another14 simply took loss of contact as meaning loss of continuity. Three studies32–34 used the results of a question or questions from the annual UK national General Practice Patient Survey.
The length of time over which continuity was measured (when not a survey response or hospital visit indicating a relationship) varied greatly between studies, from a single weekend in hospital17 up to 17 years.24 The median length of continuity measurement was 2 years (IQR 3.75).
Most studies (20, 90.9%) reported all-cause mortality. One study32 investigated premature mortality; under the age of 75. Another33 used premature coronary heart disease mortality as the primary outcome. The length of time for recording deaths also showed a large variation between studies, from 30 days to up to 21 years. The median follow-up time was 2.5 years (IQR 4.4).
Most of the studies investigated a large number of potential confounding factors (table 1). All studies working at the level of individual patients included some measure of health status including LACE index, comorbidities, previous healthcare usage and other measures. Most studies looked at age and sex and 14 (63.6%) used a measure of deprivation, social status or income.
Results of individual studies
Of the 22 studies, 18 (81.8%) showed that greater continuity of care was significantly associated with lower mortality. Of these, 16 (72.7% of the 22) were with lower all-cause mortality (table 2). Two studies found no association of greater continuity of care with subsequent mortality during17 or following16 a hospital stay. One study found that continuity was not significantly associated with mortality except in general practices in the least deprived areas.32 One study13 investigated a range of continuity measures. They found that all insurance claims-based measures showed that higher levels of continuity were associated with higher mortality rates but greater continuity as reported by patients was associated with reduced mortality. This is the only study showing any association of increased continuity with increased mortality.
Table 2.
Outcome measures of studies investigating the association of continuity of care with mortality
| First author and year of publication | Ratio (if available) | Other result | 95% CI | For measure | Continuity associated with mortality? | Results summary |
| Bentler 201413 | 2.25† | 1.33 to 3.81 | AHR above vs below mean patient-reported care site continuity. | Yes | Patient-reported duration continuity had significant, protective association with time to death. Seven claims-based continuity of care indicators and one patient-reported measure (site continuity) showed higher continuity associated with increased death hazard. | |
| 0.54* | 0.37 to 0.8 | AHR, highest vs lowest tertile patient-reported duration continuity. | ||||
| 2.3† | 1.56 to 3.38 | AHR, highest vs lowest tertile, UPC. | ||||
| 1.8† | 1.12 to 2.88 | AHR, highest vs lowest tertile, inverse number of providers. | ||||
| 1.69† | 1.13 to 2.52 | AHR, highest vs lowest tertile, MMCI. | ||||
| 1.7† | 1.12 to 2.59 | AHR, highest vs lowest tertile, Ejlertsson’s Index K. | ||||
| 2.33† | 1.56 to 3.49 | AHR, highest vs lowest tertile, Bice-Boxerman CoC. | ||||
| 1.98† | 1.23 to 3.21 | AHR, highest vs lowest tertile, MCI. | ||||
| 2.35† | 1.59 to 3.49 | AHR, highest vs lowest tertile, sequential continuity. | ||||
| Cerovečki 201314 | 12.6* | 3.001 to 53.253 | OR, loss of CoC. | Yes | Loss of continuity of care one predictor of fatal outcome. | |
| Spatz 201415 | 1.92* | 1.19 to 3.12 | AHR, no usual source of care vs strong USOC relationship. | Yes | In multivariable analysis, having no USOC associated with higher 12-month mortality. | |
| van Walraven 201016 | 1.03 | 0.95 to 1.12 | AHR, increase of 0.1 in continuity score, preadmission physician. | No | No significant association found for death risk with continuity with any doctor type studied. | |
| 0.87 | 0.74 to 1.02 | AHR, increase of 0.1 in continuity score, hospital physician. | ||||
| 0.97 | 0.89 to 1.06 | AHR, increase of 0.1 in continuity score, postdischarge physician. | ||||
| Blecker 201417 | 0.72 | 0.29 to 1.8 | AOR, UPC 1 (complete continuity) vs 0, no continuity. | No | Increased weekend UPC was significantly associated with decreased mortality in unadjusted analysis. No association after multivariate adjustment. | |
| Brener 201618 | 0.87* | 0.82 to 0.93 | AOR, visited vs not, 90-day postdischarge. | Yes | In unadjusted model, visited patients more likely to die at 90 days. In unadjusted model, visited patients less likely to die at 90 days. | |
| 0.88* | 0.81 to 0.86 | AOR, visited vs not, 30-day postdischarge. | ||||
| Hoertel 201419 | 0.83* | 0.83 to 0.83 | AHR, 0.1% increase in CoC index. | Yes | 0.1 increase in CoC index associated with decreased likelihood of death. | |
| 0.53* | 0.52 to 0.54 | AHR, perfect continuity vs imperfect continuity. | ||||
| Justiniano 201720 | 2.33 | 2.10 to 2.60 | AHR, readmitted to original hospital but with different surgeon vs same hospital, same surgeon. | Yes | In comparison with patients readmitted to the same hospital and managed by the same surgeon, patients managed at the same hospital but by a different surgeon had > twofold risk of 1-year mortality. | |
| Leleu 201321 | 0.96* | 0.95 to 0.96 | HR, 0.1 increase in CoC. | Yes | Increase in the CoC index associated with decrease in death risk. | |
| Liao 201522 | * | Significant trend (p<0.001, test for monotonic trend) | Decreasing consistency in medical care-seeking behaviour with decreasing adjusted survival. | Yes | A significant monotonic trend was observed between decreasing consistency in medical care-seeking behaviour (from high consistency to low consistency) and decreasing multivariate-adjusted survival. | |
| Lustman 201623 | 0.59* | 0.5 to 0.7 | OR, high vs low UPC, measured at the same time. | Yes | Patients with a high UPC had lower risk of mortality. Not affected on adjusting for background characteristics. | |
| 0.7* | 0.56 to 0.88 | OR, high vs low UPC, measured in successive years. | ||||
| Maarsingh 201624 | 1.2* | 1.01 to 1.42 | HR, lowest vs highest CoC. | Yes | In final model, participants in lowest CoC category showed greater mortality than those in maximum. | |
| McAlister 201325 | 0.86 | HR, familiar vs unfamiliar (our calculation, CI not available). | Yes | After 6 months, death HR for familiar Dr 0.66 (95% CI 0.61 to 0.71) and 0.77 (0.68 to 0.88) with unfamiliar vs no follow-up. At 3 months, 1.6% of those who had a visit with a familiar Dr died, 3.3% who only saw an unfamiliar Dr, p<0.001. | ||
| McAlister 201626 | * | 3.1% vs 2.0%, p<0.0001 | % mortality: follow-up by unfamiliar or familiar physician. | Yes | More died with follow-up with unfamiliar physician compared with those with at least one visit with familiar physician. | |
| Pan 201727 | 0.47* | 0.46 to 0.48 | AHR high (>50%) vs low (≤50%) CoC score. | Yes | Patients with diabetes with higher physician continuity had a lower risk of mortality. | |
| Shin 201428 | 1.13* | 1.05 to 1.21 | AHR, below vs above median most frequent provider. | Yes | Above median continuity associated with lower all-cause mortality using three different measures. | |
| 1.13* | 1.05 to 1.21 | AHR, below vs above median MMCI. | ||||
| 1.12* | 1.04 to 1.21 | AHR, below vs above median CoC. | ||||
| Sidhu 201429 | * | 1.9% vs 1.4%, p<0.0001 | % mortality: follow-up by unfamiliar or familiar physician. | Yes | More died with follow-up with unfamiliar physician compared with those with at least one visit with familiar physician. | |
| Weir 201630 | 0.75* | 0.61 to 0.94 | AOR, high vs low UPC. | Yes | High UPC associated with decreased mortality. | |
| Worrall 201131 | * | 9.0% vs 18.1%, (p=0.025, χ²) | % mortality: high vs low continuity group. | Yes | Proportion of people dying significantly lower in high-continuity group. | |
| Baker 201632 | 21 deaths | −16 to 63 | Potential reduction in premature deaths in England in 1 year if there is a change of 1 percentile of patients expressing trust in their doctor. | No | Continuity not associated with mortality (except in less deprived practices in a separate subgroup analysis). | |
| −49 deaths | −250 to 156 | Potential reduction in premature deaths in England in 1 year if there is a change of 1 percentile of patients able to get an appointment in advance. | ||||
| Honeyford 201333 | 0.994* | 0.989 to 1 | IRR, 1% change in survey response. | Yes | An increase in % of patients recalling being able to see their preferred GP was associated with decreased mortality. | |
| Levene 201234 | 0.999 | 0.997 to 1.01 | IRR, all-cause mortality. | Depends on mortality measure | No significant association with all-cause mortality. An increase in the % of patients recalling being better able to see their preferred doctor was associated with decreases in COPD mortality and in all-cancer mortality. | |
| 0.997* | 0.995 to 0.999 | IRR, all-cancer mortality. | ||||
| 0.999 | 0.995 to 1.07 | IRR, coronary heart disease mortality. | ||||
| 1.0002 | 0.99 to 1.01 | IRR, stroke mortality. | ||||
| 0.993* | 0.98 to 0.998 | IRR, COPD mortality. |
*Significant result showing higher levels of continuity associated with lower mortality.
†Significant result showing higher levels of continuity associated with higher mortality.
AHR, adjusted HR; AOR, adjusted GP, general practitioner; OR; CoC, Continuity of Care Index; IRR, incident rate ratio; MCI, modified continuity index; MMCI, Modified Modified Continuity Index; UPC, Usual Provider of Care Index; USOC, usual source of care.
Due to the heterogeneity of study continuity and mortality measurements, it was not possible to combine them to produce an estimate of effect size; however, table 2 shows the risk ratio, OR or HR from individual studies where available.
Risk of bias within studies
Using the Newcastle-Ottawa Scale,36 all 22 studies were rated as high quality, with nine 10 studies (40.9%) gaining maximum scores from both reviewers independently (table 1, supplementary table). No study was scored less than 7 out of 9 by any reviewer. As all these studies were cohort or cross-sectional studies, they tested for associations only. However, most involved statistical analyses for a wide range of potential confounding factors (table 1).
The specific bias of reverse causality between the healthcare-related events that might occur before death was discussed in 14 (63.6%) of the studies. Four cohort studies did not discuss reverse causality.14 24 27 31 However, all of the studies included some measure of health/disease status as a potential confounding factor and some included several detailed measures of these in their models.
Five of the studies had a design which meant there was no overlap between the time for continuity measurement and the period during which deaths were counted.13 20 22 28 30 Seven studies have complete14 16 21 23 28 29 31 and four partial overlap of these periods.17 19 24 25 Five studies included additional analyses which either eliminated the overlap23 or introduced a lag time19 21 26 28 between continuity and mortality measurement periods. In each of these additional analyses, continuity was still found to be significantly associated with mortality. One long-term study24 calculated survival from the date of the last continuity measurement and stratified by the length of time in the study. Five studies19 21 25 28 29 used their continuity score as a time-dependent variable in the model.
Risk of bias across studies
There is a risk of publication bias. It may be that reports showing no effect are less likely to be published. However, two showed no association. In two, mortality was not the primary outcome and in six, it was part of a composite outcome. For 13 studies, mortality was not the only outcome. In 10 studies, the association of two or more factors, including doctor continuity of care, with outcomes was tested. Continuity and mortality as exposure and outcome, respectively, are reported in a range of studies, including where testing this association was not the primary aim.
Discussion
Principal findings
In a substantial majority of studies (18, 81.8%) meeting the selection criteria, higher levels of continuity of care with doctors were associated with lower mortality rates. Two others, finding no significant association, had very short timescales for measurement of continuity, to the extent that the strength of any patient–doctor relationship was potentially questionable. Another study showing no significant association with all-cause mortality was cross-sectional, and the measurement methods related to questions on a national survey about seeing a particular general practitioner, again not necessarily indicative of a strong patient–doctor relationship.
One study8 found that for claims-based measures of continuity, increased mortality was associated with higher levels of continuity of care. However in the same study, higher levels of patient-reported continuity were associated with lower mortality rates. This emphasises the interpersonal relationship between patient and doctor as claims-based measures only give numbers of contacts and do not directly measure the quality of the relationship.
The effect sizes were generally small (table 2) but these were in the same range as some treatment effects, as very large, repeatable effects on mortality are rare.53 In addition, for some studies included in this review, effect sizes were calculated using very small increments in the continuity measure.
Strengths and weaknesses of the evidence
All the studies found investigating the association of continuity of care with mortality were observational in nature, although the majority were high-quality cohort studies including three prospective cohort studies. The issue of reverse causality applies to all the evidence presented here. This could bias an association between continuity of care and mortality in either direction. As patient health worsens when approaching death, continuity of care may deteriorate for many reasons, for example, patients moving areas to accommodate increased health needs, the need to see more specialists or a loss of ability to obtain and attend appointments. Alternatively, deterioration of health could lead to a concerned doctor ensuring that the patient receives more continuity of care. For the cross-sectional studies, there is also a potential for confounding due to practice-level factors.
There have been randomised controlled trials into continuity of care but none on existing relationships or lasting longer than a year and none with mortality as an outcome.4–6 Observational studies which control rigorously for confounding factors and have a design aimed at limiting the impact of reverse causality are the best evidence available.
Of the 16 cohort studies finding an association of higher continuity with lower mortality, most studies attempt to at least partially account or control for reverse causality in their study design or analysis. Most controlled for differences in health status and risk factors. Some carried out analyses measuring continuity and mortality in separate years, or with a lag. This method, particularly the lag between measurements, should help to minimise bias caused by rapid worsening prior to death. However, four cohort studies showing this association14 24 27 31 did not discuss this kind of reverse causality although one24 nevertheless made several adjustments for health status and calculated survival from the date of the last continuity measurement. Measuring continuity and mortality over separate time periods is also one way of eliminating the potential bias caused by those who survived longer having more time to accrue continuity (time-dependent bias). Another way of reducing this is to model continuity as a time-dependent variable which was the case in five studies.19 21 25 28 29
All studies included were rated as high quality, using the Newcastle-Ottawa Scale.
Several of the articles reported on studies using very large cohorts. The studies came from a number of different countries with different healthcare systems and cultures. Continuity of care in the studies included that received from specialist as well as generalist doctors, showing that the effect is not limited to one branch of medicine or health system.
As continuity research is an emerging field, no consensus on the best way to measure it has been reached. The measure used most was the UPC Index which does not take into account the total number, frequency or sequence of visits.54
Doctors have been studied as a discrete category in numerous studies, and data systems usually allow them to be separately studied. The group studied included family doctors/general practitioners, physicians and psychiatrists so was already heterogeneous so expanding this to other professional groups would have complicated interpretation. As doctors are the most highly trained health professionals with the most influence over decisions, it is reasonable to assume that if interpersonal contact affects mortality, it is most likely to occur with doctors. Therefore, we eliminated articles, some with significant reductions in mortality, that measured continuity in relation to mixed profession teams or to other health professionals.35 43–49 This is the first systematic review investigating whether continuity of doctor care is associated with reduced mortality. We expect this to encourage studies with different selection criteria; for example, for continuity with other healthcare professionals.
Possible mechanisms and implications
This review, finding that increased receipt of continuity of care is associated with reduced mortality, comes after it has been shown that continuity of care is associated with multiple benefits for patients.9–12 It therefore fits well with such earlier work. It is only recently that large databases and long-term cohort studies have made effective investigation into the links between continuity and mortality possible.
These known associations suggest possible mechanisms in that greater uptake of evidence-based preventative medicine such as immunisations as well as better concordance with treatments is likely to reduce mortality. Continuity of care is associated with patients perceiving that the doctor has become more responsive.55Patients then disclose more and medical management is more likely to be tailored to the needs of the patient as a person. The increased patient satisfaction may also be associated with an ‘optimism’ boost to health.56 We have previously suggested that ‘doctors tend to overestimate their effectiveness when consulting with patients they do not know, and underestimate their effectiveness when consulting with patients they know’.57
The cumulative impact of these multiple gains may then be reflected in reduced mortality.
Historically, continuity of care has been considered a feature of the practice of medical generalists and featured in the job descriptions of the general practitioner.58 59 Recent studies included in this review found that continuity was associated with reduced mortality with specialist physicians,22 28 psychiatrists19 and surgeons20 too.
Although this evidence is observational, with 18 of the 22 studies showing significant reductions in mortality with continuity of doctor care, the clear preponderance of evidence is in favour of the association. Three studies showed no significant association and one13 had mixed results but no study exclusively showed an association of higher continuity of care with higher mortality rates. Although there are difficulties in carrying out controlled trials on this subject, a few, with interventions to increase continuity of care, have been successful,4–6 and this could be attempted more widely. The presence of this association in nine countries, across three continents, and in very different populations and healthcare systems implies a basic human effect.60 The policy implication as many studies noted is prioritising continuity of care.
For 200 years, medical advances have been mainly technical and impersonal which has reduced attention to the human side of medicine. This systematic review reveals that despite numerous technical advances, continuity of care is an important feature of medical practice, and potentially a matter of life and death.
Supplementary Material
Acknowledgments
The authors thank Professor Rod Taylor of the University of Exeter Medical School for providing useful comments on the draft manuscript. We acknowledge the Royal Society of Medicine Library for carrying out some literature searches for us. The authors are grateful to the University of Exeter Medical School Collaboration for Academic Primary Care for reimbursing the publication costs.
Footnotes
Contributors: DJPG conceived the idea for the systematic review. KS-L wrote the protocol with input from other authors and submitted it to PROSPERO. AT, EW and KS-L carried out database searches. DJPG, KS-L, AT and EW carried out article selection, data extraction and assessing article quality. PHE had the deciding vote in article selection, data extraction and assessing article quality. KS-L carried out data analysis. All authors wrote and edited the manuscript. All authors approved the manuscript for publication.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional unpublished data are available.
References
- 1. Duffy S, Lee TH. In-person health care as option B. N Engl J Med 2018;378:104–6. 10.1056/NEJMp1710735 [DOI] [PubMed] [Google Scholar]
- 2. Pereira Gray D, Evans P, Sweeney K, et al. Towards a theory of continuity of care. J R Soc Med 2003;96:160–6. 10.1177/014107680309600402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adler R, Vasiliadis A, Bickell N. The relationship between continuity and patient satisfaction: a systematic review. Fam Pract 2010;27:171–8. 10.1093/fampra/cmp099 [DOI] [PubMed] [Google Scholar]
- 4. Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA 1984;252:2413–7. [PubMed] [Google Scholar]
- 5. Flint C, Poulengeris P, Grant A. The ’Know Your Midwife' scheme–a randomised trial of continuity of care by a team of midwives. Midwifery 1989;5:11–16. 10.1016/S0266-6138(89)80059-2 [DOI] [PubMed] [Google Scholar]
- 6. Tracy SK, Hartz D, Hall B, et al. A randomised controlled trial of caseload midwifery care: M@NGO (Midwives @ New Group practice Options). BMC Pregnancy Childbirth 2011;11:82 10.1186/1471-2393-11-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Walraven C, Oake N, Jennings A, et al. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract 2010;16:947–56. 10.1111/j.1365-2753.2009.01235.x [DOI] [PubMed] [Google Scholar]
- 8. Hjortdahl P. Continuity of care: general practitioners' knowledge about, and sense of responsibility toward their patients. Fam Pract 1992;9:3–8. 10.1093/fampra/9.1.3 [DOI] [PubMed] [Google Scholar]
- 9. Baker R, Streatfield J. What type of general practice do patients prefer? Exploration of practice characteristics influencing patient satisfaction. Br J Gen Pract 1995;45:654–9. [PMC free article] [PubMed] [Google Scholar]
- 10. Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract 2004;53:974–80. [PubMed] [Google Scholar]
- 11. Chen CC, Tseng CH, Cheng SH. Continuity of care, medication adherence, and health care outcomes among patients with newly diagnosed type 2 diabetes: a longitudinal analysis. Med Care 2013;51:231–7. 10.1097/MLR.0b013e31827da5b9 [DOI] [PubMed] [Google Scholar]
- 12. Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ 2017;356:j84 10.1136/bmj.j84 [DOI] [PubMed] [Google Scholar]
- 13. Bentler SE, Morgan RO, Virnig BA, et al. The association of longitudinal and interpersonal continuity of care with emergency department use, hospitalization, and mortality among Medicare beneficiaries. PLoS One 2014;9:e115088 10.1371/journal.pone.0115088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cerovečki V, Tiljak H, Ožvačić Adžić Z, et al. Risk factors for fatal outcome in patients with opioid dependence treated with methadone in a family medicine setting in Croatia. Croat Med J 2013;54:42–8. 10.3325/cmj.2013.54.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Spatz ES, Sheth SD, Gosch KL, et al. Usual source of care and outcomes following acute myocardial infarction. J Gen Intern Med 2014;29:862–9. 10.1007/s11606-014-2794-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Walraven C, Taljaard M, Etchells E, et al. The independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists. J Hosp Med 2010;5:398–405. 10.1002/jhm.716 [DOI] [PubMed] [Google Scholar]
- 17. Blecker S, Shine D, Park N, et al. Association of weekend continuity of care with hospital length of stay. Int J Qual Health Care 2014;26:530–7. 10.1093/intqhc/mzu065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brener SS, Bronksill SE, Comrie R, et al. Association between in-hospital supportive visits by primary care physicians and patient outcomes: A population-based cohort study. J Hosp Med 2016;11:418–24. 10.1002/jhm.2561 [DOI] [PubMed] [Google Scholar]
- 19. Hoertel N, Limosin F, Leleu H. Poor longitudinal continuity of care is associated with an increased mortality rate among patients with mental disorders: results from the French National Health Insurance Reimbursement Database. Eur Psychiatry 2014;29:358–64. 10.1016/j.eurpsy.2013.12.001 [DOI] [PubMed] [Google Scholar]
- 20. Justiniano CF, Xu Z, Becerra AZ, et al. Long-term deleterious impact of surgeon care fragmentation after colorectal surgery on survival: continuity of care continues to count. Dis Colon Rectum 2017;60:1147–54. 10.1097/DCR.0000000000000919 [DOI] [PubMed] [Google Scholar]
- 21. Leleu H, Minvielle E. Relationship between longitudinal continuity of primary care and likelihood of death: analysis of national insurance data. PLoS One 2013;8:e71669 10.1371/journal.pone.0071669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liao PJ, Lin ZY, Huang JC, et al. The relationship between type 2 diabetic patients' early medical care-seeking consistency to the same clinician and health care system and their clinical outcomes. Medicine 2015;94:e554 10.1097/MD.0000000000000554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lustman A, Comaneshter D, Vinker S. Interpersonal continuity of care and type two diabetes. Prim Care Diabetes 2016;10:165–70. 10.1016/j.pcd.2015.10.001 [DOI] [PubMed] [Google Scholar]
- 24. Maarsingh OR, Henry Y, van de Ven PM, et al. Continuity of care in primary care and association with survival in older people: a 17-year prospective cohort study. Br J Gen Pract 2016;66:e531–e539. 10.3399/bjgp16X686101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McAlister FA, Youngson E, Bakal JA, et al. Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. Can Med Assoc J 2013;185:E681–E689. 10.1503/cmaj.130048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McAlister FA, Youngson E, Kaul P, et al. Early Follow-Up After a Heart Failure Exacerbation: The Importance of Continuity. Circ Heart Fail 2016;9:e003194 10.1161/CIRCHEARTFAILURE.116.003194 [DOI] [PubMed] [Google Scholar]
- 27. Pan CC, Kung PT, Chiu LT, et al. Patients with diabetes in pay-for-performance programs have better physician continuity of care and survival. Am J Manag Care 2017;23:e57–e66. [PubMed] [Google Scholar]
- 28. Shin DW, Cho J, Yang HK, et al. Impact of continuity of care on mortality and health care costs: a nationwide cohort study in Korea. Ann Fam Med 2014;12:534–41. 10.1370/afm.1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sidhu RS, Youngson E, McAlister FA. Physician continuity improves outcomes for heart failure patients treated and released from the emergency department. JACC Heart Fail 2014;2:368–76. 10.1016/j.jchf.2014.03.006 [DOI] [PubMed] [Google Scholar]
- 30. Weir DL, McAlister FA, Majumdar SR, et al. The Interplay Between Continuity of Care, Multimorbidity, and Adverse Events in Patients With Diabetes. Med Care 2016;54:386–93. 10.1097/MLR.0000000000000493 [DOI] [PubMed] [Google Scholar]
- 31. Worrall G, Knight J. Continuity of care is good for elderly people with diabetes: retrospective cohort study of mortality and hospitalization. Can Fam Physician 2011;57:e16–20. [PMC free article] [PubMed] [Google Scholar]
- 32. Baker R, Honeyford K, Levene LS, et al. Population characteristics, mechanisms of primary care and premature mortality in England: a cross-sectional study. BMJ Open 2016;6:e009981 10.1136/bmjopen-2015-009981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Honeyford K, Baker R, Bankart MJ, et al. Modelling factors in primary care quality improvement: a cross-sectional study of premature CHD mortality. BMJ Open 2013;3:e003391 10.1136/bmjopen-2013-003391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Levene LS, Bankart J, Khunti K, et al. Association of primary care characteristics with variations in mortality rates in England: an observational study. PLoS One 2012;7:e47800 10.1371/journal.pone.0047800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wolinsky FD, Bentler SE, Liu L, et al. Continuity of care with a primary care physician and mortality in older adults. J Gerontol A Biol Sci Med Sci 2010;65:421–8. 10.1093/gerona/glp188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp accessed May 18th 2017.
- 37. Wolinsky FD, Miller TR, An H, et al. Dual use of medicare and the veterans health administration: are there adverse health outcomes? BMC Health Serv Res 2006;6:131 10.1186/1472-6963-6-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wolinsky FD, An H, Liu L, et al. Exploring the association of dual use of the VHA and Medicare with mortality: separating the contributions of inpatient and outpatient services. BMC Health Serv Res 2007;7:70 10.1186/1472-6963-7-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Damiani G, Federico B, Venditti A, et al. Hospital discharge planning and continuity of care for aged people in an Italian local health unit: does the care-home model reduce hospital readmission and mortality rates? BMC Health Serv Res 2009;9:22 10.1186/1472-6963-9-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jacobs DG, Sarafin JL, Head KE, et al. Trauma attending physician continuity: does it make a difference? Am Surg 2010;76:48–54. [PubMed] [Google Scholar]
- 41. Ali NA, Hammersley J, Hoffmann SP, et al. Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med 2011;184:803–8. 10.1164/rccm.201103-0555OC [DOI] [PubMed] [Google Scholar]
- 42. Laksman ZW, Krahn AD, Dorian P, et al. Greater mortality risk among patients with delayed follow-up after implantable cardioverter defibrillator procedures. Can J Cardiol 2014;30:598–605. 10.1016/j.cjca.2014.03.028 [DOI] [PubMed] [Google Scholar]
- 43. Desai RA, Dausey DJ, Rosenheck RA. Mental health service delivery and suicide risk: the role of individual patient and facility factors. Am J Psychiatry 2005;162:311–8. 10.1176/appi.ajp.162.2.311 [DOI] [PubMed] [Google Scholar]
- 44. Ho PM, Luther SA, Masoudi FA, et al. Inpatient and follow-up cardiology care and mortality for acute coronary syndrome patients in the Veterans Health Administration. Am Heart J 2007;154:489–94. 10.1016/j.ahj.2007.05.018 [DOI] [PubMed] [Google Scholar]
- 45. Hong JS, Kang HC. Continuity of ambulatory care and health outcomes in adult patients with type 2 diabetes in Korea. Health Policy 2013;109:158–65. 10.1016/j.healthpol.2012.09.009 [DOI] [PubMed] [Google Scholar]
- 46. Nyweide DJ, Anthony DL, Bynum JP, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med 2013;173:1879–85. 10.1001/jamainternmed.2013.10059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nelson K, Sun H, Dolan E, et al. Elements of the patient-centered medical home associated with health outcomes among veterans: the role of primary care continuity, expanded access, and care coordination. J Ambul Care Manage 2014;37:331–8. 10.1097/JAC.0000000000000032 [DOI] [PubMed] [Google Scholar]
- 48. Cho KH, Kim YS, Nam CM, et al. The association between continuity of care and all-cause mortality in patients with newly diagnosed obstructive pulmonary disease: a population-based retrospective cohort study, 2005-2012. PLoS One 2015;10:e0141465 10.1371/journal.pone.0141465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Harris AH, Gupta S, Bowe T, et al. Predictive validity of two process-of-care quality measures for residential substance use disorder treatment. Addict Sci Clin Pract 2015;10:22 10.1186/s13722-015-0042-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McKinley RK, Stokes T, Exley C, et al. Care of people dying with malignant and cardiorespiratory disease in general practice. Br J Gen Pract 2004;54:909–13. [PMC free article] [PubMed] [Google Scholar]
- 51. van Walraven C, Mamdani M, Fang J, et al. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med 2004;19:624–31. 10.1111/j.1525-1497.2004.30082.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tsai HY, Chou YJ, Pu C. Continuity of care trajectories and emergency room use among patients with diabetes. Int J Public Health 2015;60:505–13. 10.1007/s00038-015-0671-1 [DOI] [PubMed] [Google Scholar]
- 53. Pereira TV, Horwitz RI, Ioannidis JP. Empirical evaluation of very large treatment effects of medical interventions. JAMA 2012;308:1676–84. 10.1001/jama.2012.13444 [DOI] [PubMed] [Google Scholar]
- 54. Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev 2006;63:158–88. 10.1177/1077558705285294 [DOI] [PubMed] [Google Scholar]
- 55. Reis HT, Clark MS, Pereira Gray D, et al. Measuring responsiveness in the therapeutic relationship: a patient perspective. Basic Appl Soc Psych 2008;30:339–48. 10.1080/01973530802502275 [DOI] [Google Scholar]
- 56. Ayling K, Fairclough L, Tighe P, et al. Positive mood on the day of influenza vaccination predicts vaccine effectiveness: A prospective observational cohort study. Brain Behav Immun 2018;67:314–23. 10.1016/j.bbi.2017.09.008 [DOI] [PubMed] [Google Scholar]
- 57. Pereira Gray D, Sidaway-Lee K, White E, et al. Improving continuity: The clinical challenge. InnovAiT: Education and inspiration for general practice 2016;9:635–45. 10.1177/1755738016654504 [DOI] [Google Scholar]
- 58. Royal College of General Practitioners. The future general practitioner—learning and teaching. J R Coll Gen Pract 1972;22:581–2. [PMC free article] [PubMed] [Google Scholar]
- 59. Party LW. The Work of the General Practitioner in Europe. J R Coll Gen Pract 1977;27:117. [Google Scholar]
- 60. Bradford Hill A. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-021161supp001.pdf (191.1KB, pdf)