Abstract
Background
Although commonly prescribed, the evidence to support exercises therapy (ET) and conservative management for the treatment of full-thickness rotator cuff tears (FTT) is equivocal.
Purpose
The purpose of this systematic review of the literature was to determine the current level of evidence available for ET in the treatment of FTT and to provide a formal Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group of recommendation.
Methods
Five databases were systematically searched to evaluate the effectiveness of ET for FTT. Inclusion criteria: experimental or observational studies of adults clinically diagnosed with FTT, or massive, or inoperable tears that contained a treatment group that received ET for FTT. Exclusion criteria included: history of surgical repair, concurrent significant trauma, neurological impairment, and level V studies. Articles were assessed for quality, the level of evidence (I – V) and GRADE of recommendation (A to F) was determined. Data extraction included: demographics, specific interventions, and outcomes.
Results
One thousand, five-hundred and sixty-nine unique citations were identified, 35 studies were included: nine randomized controlled studies, six cohort studies, 15 case series and five case reports. There were 2010 shoulders in 1913 subjects with an average age of 64.2 years, 54% males, 73% of tears were > 1 cm and 37% were classified as massive. Based on studies that reported, >58% of tears were > 1 year and 73% were atraumatic. Of the non-operatively treated cohorts that reported the respective outcomes: 78% improved in pain (9/10 cohorts that reported statistically significant differences [stat-sig] p<0.05), 81% improved in ROM (14/14 cohorts that reported, met stat-sig), 85% improved in strength (7/8 cohorts that reported, met stat-sig), 84% improved in functional outcomes (17/17 cohorts that reported, met stat-sig). Dissatisfied outcomes occurred in 15% of patients, who then transitioned to surgery.
Conclusion
The current literature indicates GRADE B recommendation (moderate strength) to support the use of ET in the management of FTT. There is further need for well-designed randomized controlled trials.
Level of Evidence
2a
Keywords: Exercise therapy, full-thickness rotator cuff tear, non-operative management
INTRODUCTION
Rotator cuff tears (RCT) result in disability, poor quality of life, expensive utilization of healthcare resources1 and have been shown to affect 20-28% individuals between the ages of 60-69,2,3 31-40.7% in patients over the age of 70,2 51-62% in individuals over 80 years of age,4 with an increase of 2.69 odds of a RC tear for every decade of life (p = 0.005).5 Aggregate mean prevalence rates are estimated at 39% of asymptomatic individuals and 64% of symptomatic individuals,6 with the expectation that 50% of asymptomatic tears will become symptomatic at a mean of 2.8 years after the time of initial discovery.7,8 Though partial thickness rotator cuff tears (PTT) are more common than full-thickness rotator cuff tears (FTT),9,10 PTT tend to progress to FTT, developing pathological changes due to muscle retraction, fatty infiltration, and muscle atrophy and thus, are associated with greater disability.6,8,11-14 These facts are consistent with the prevalence of FTT in symptomatic patients progressing with age, with 28% of patients ≥ 60 years old, 50% of patients ≥ 70 years old, and 80% of ≥ 80 years old.5,7,9,15 Other potential predisposing factors besides age,2,4,5,7,11,16 include both non-modifiable factors (gender,17 hand dominance,18-20 pathology of the contralateral shoulder,21-23 family history,24 glenohumeral instability,25,26 coracoid and/or acromion anatomy25) and modifiable factors (smoking,27-29 posture,6,30,31 and poor or insufficient diet25,32-35).
Given the high prevalence, the substantial financial burden on both patients and society,9,36-40 and the associated disability associated with FTTs,41 determining effective management is of high priority for researchers and healthcare providers. Several reviews42-46 have compared the effectiveness of operative treatment to non-operative management, with some literature supporting surgical options47-50 and others demonstrating comparable outcomes between the two options.32,40,51,52 Similar ambiguity is seen with the surprising fact that of the 25 to 90% of surgical repairs that fail,40,53-61 the reported satisfaction levels and clinical outcomes scores are comparable to individuals with intact repairs.9,40 Given the discrepancies in finding between non-operative and operative management, as well as the unpredictable surgical re-tear rates, perhaps it is no surprise only 5% of the 5.7 million (as of 2010) patients over the age of 60 in the U.S. with RCTs in the U.S. were treated surgically.40 It is encouraging that exercise and physical therapy have been shown to be viable and alternative treatment option,9,32,40,45 especially in incidences where rotator cuff (RC) tendons have retracted beyond the glenoid rim,32,58,59 are massive in size ( ≥ 5 mm)62, and/or surgery is contraindicated due to comorbidities. However, researchers have had difficulty drawing strong conclusions as to the true comparative effectiveness of non-operative management of FTTs due to low-quality studies.32,42,43 This, in addition to the heterogeneity of conservative exercise programs, has made it difficult to synthesize and establish robust evidence-based rehabilitation programs. The limitations of this recent publication by Edwards et al9 was: (1) the fact that it was Level 5 evidence due to the lack of a systematic search to establish the protocol and (2) the proposed protocol was not specific to FTT.
Described conservative treatment of RCT are multimodal, ranging from exercise therapy, modalities (cryotherapy, thermal therapy, electrotherapy, acupuncture, ultrasound, and electrotherapy), taping, injection therapy, pharmacological management.9,32,42,63 However, as there is no consensus or gold standard exercise program of FTT, clinicians and researchers are left to use other shoulder pathology rehab programs40,63 or expert opinion9 to guide the clinical practice and clinical trials for the treatment of FTT. Though there have been a number of reviews on non-operative RCTs interventions in the last 15 years,32,43-46,64 these are either not specific to FTT,43 exercise therapy,44 or have focused on comparing surgical vs. non-surgical treatment rather than identifying and synthesizing the specific components of an optimal conservative management.45,64 The most recently published systematic review45 only identified three randomized control trials citations, which demonstrates the paucity of high-quality studies. This, in turn, makes it acceptable to conduct a systematic review including observational studies.65 The last systematic review32 to conduct a search of both randomized controlled trials and observational studies, specific to exercise therapy of FTT is over 10 years old and needs to be updated due to time elapsed,66 new evidence becoming available,67 and based on need or priority.68
The primary purpose of this systematic review is to: (1) update a prior review32 by synthesizing the available research on the effectiveness of exercise therapy for FTT, (2) use the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group criteria69 to evaluate the current level evidence of exercise therapy (with and without the addition of supplemental non-operative modalities and treatments) to provide a grade of recommendation.
METHODS
The PRISMA guidelines were employed in this systematic literature review.70 A formal research question was developed as is recommended by PRISMA guidelines:71
Population: skeletally mature human adults (greater than 18 years of age).
Intervention: exercise rehabilitation (in isolation or combination with other non-operative interventions).
Comparison: control, sham treatment, placebo, education, or other non-operative interventions
Outcome: change in pain, strength, range of motion, and function of the shoulder.
Time: not specified
Information sources and search parameters
The following databases have been searched until December 2016: Embase, Medline (PubMed), CINHAL Database, Cochrane Database of Systematic Reviews, PEDro, and Web of Science. Keywords used in the aforementioned review, Ainsworth et al 200732, as well as those derived from the research question were used. A medical school research librarian was consulted on formulated initial search for Medline (PubMed), as well as for translating the search to other databases utilizing the respective thesaurus for indexing articles and free entries. The search strategies for each of the respective databases can be found in Appendix A.
Study selection
Prior to conducting the search, inclusion and exclusion criteria for articles were defined. The inclusion and exclusion criteria were kept consistent with the original review,32 as is standard practice in updating systematic reviews.68 Identified studies were filtered by the following inclusion criteria: randomized clinical trials or observational studies, skeletally mature human adults with a clinical diagnosis of FTT, or massive, or inoperable RCTs. Additionally, it was required that studies explicitly state that at least one treatment group received exercise therapy, in isolation or in conjunction with other non-operative treatment, for FTT. The only criteria that differed from the original study32 were that only full-texts available in the English language were included due lack of translation resources42 and that included studies also needed to report one of the following outcomes: pain, ROM, strength, and/or functional outcome scores.
Though not ‘included’, prior systematic reviews pertinent to these inclusion criteria were identified, the quality assessment made, and conclusions comparisons made to those of the current review. This decision was made in order to capture the complete spectrum of conservative treatment FTT literature and to allow comparison of prior conclusions and synthesized data of such reviews.
Identified studies were also filtered by the following exclusion criteria: surgical repair at any previous time point, concurrent significant trauma or derangement to the shoulder (i.e. prior surgery, acromioclavicular joint separation, Hill-Sachs lesion of any kind, etc.), neurological diagnosis or impairment affecting the patients’ shoulder function (i.e. stroke, brachial plexus injury, spinal cord injury, etc.), inability to access full text article (i.e. exhausting all efforts and resources of medical school librarians and contacting the respective corresponding authors by email, social media, and/or phone), level 5 evidence such as, clinical commentaries, editorials, and grey literature.
All identified citations were filtered independently by two of the authors (M.J. and S.H.) based upon the title, then the title and abstract, and finally, by full text via the above inclusion and exclusion criteria. Any disagreements (n = 0) were resolved by consensus. The consensus was achieved on all publications included in the review without the need to resolved disagreements by a third independent reviewer (G.L.). Study design was determined by the ‘traditional’ classification method as described by Furlan et al.72
Assessment of trial quality
The quality of any identified systematic review was assessed using the Assessment of Methodological Quality of Systematic Reviews (AMSTAR) guidelines,73,74 as this has previously been demonstrated to be a valid and rigorous assessment of orthopedic literature.75 Prior to conducting our search, the methodological quality of any randomized control trial identified would be according to the Cochrane Collaboration's domain-based evaluation framework.76 The use of this assessment tool differs from the PEDro scale77 described in methods of the review32 being updated. However, much more recent and higher quality systematic reviews45,64 within the rotator cuff tear literature have used the Cochrane Collaboration's domain-based evaluation framework,76 and thus, for consistency this quality assessment tool was chosen. The included observational studies would be assessed using the guidance from the NHS Centre for Reviews and Dissemination tool.78 As more recent reviews within the shoulder have not considered observational studies this quality assessment tool was kept consistent with the original publication.
One reviewer (M.J.) assessed the methodological quality of included studies, and a second reviewer (S.H.) verified the data for accuracy and completeness. Reviewers resolved discrepancies by consensus, and thus, an independent third party was not required.
Level of evidence
The Level of Evidence of all included references was determined using criteria described by the Oxford Center of Evidence-Based Medicine (OCEBM), Oxford, United Kingdom (Table 1). Originally developed in 1998 and since modified in 2011, the OCEBM Levels of Evidence enables the appraisal on a scale from I to V based on study design, randomization, blinding, and the amount of bias, with a designation of I, being the highest level of evidence.79
Table 1.
Level of evidence modified from the Oxford Center of Evidence Based Medicine (OCEBM)96
| LEVEL OF EVIDENCE | STUDY CHARACTERISTICS |
|---|---|
| I | Evidence obtained from high-quality randomized controlled trials, prospective studies, or diagnostic studies. |
| II | Evidence obtained from lesser quality randomized control trials, prospective studies or diagnostic studies (e.g., improper randomization, no blinding, <80% follow-up) |
| III | Case controlled studies or retrospective studies. |
| IV | Case Series |
| V | Expert Opinion |
The overall Grade of Recommendation for exercise therapy (with or without other non-operative treatment) treating FTT as a whole, based off of the aggregate level of evidence, was determined using The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group. Initiated in 2000 The GRADE Working group has developed a hierarchal, alphabetical letter scale of A to F (Table 2) which takes into account the quality of evidence and strength of recommendations to aid in applying research to clinical decisions and judgments in healthcare.69
Table 2.
Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group Criteria86
| GRADE OF RECOMMENDATION | STRENGTH OF EVIDENCE | |
|---|---|---|
| A | Strong | A preponderance of level I and/or level II studies support the recommendation. Must include ≥ 1 level I study. |
| B | Moderate | A single high-quality randomized controlled trial or a preponderance of level II studies support the recommendation. |
| C | Weak | A single level II study or a preponderance of level III and level IV studies including statements of consensus by content experts support the recommendation. |
| D | Conflicting | Higher-quality studies conducted on this topic disagree with respect to their conclusions. The recommendation is based on these conflicting studies. |
| E | Theoretical/Foundational | A preponderance of evidence from animal or cadaver studies, from conceptual models/principles, or from basic sciences/bench research support this conclusion. |
| F | Expert Opinion | Best practice based on the clinical experience of the guidelines development team. |
The Investigators justified using the OCEBM Levels of Evidence and The GRADE Working Group criteria to determine the quality of evidence as both scales are endorsed by the American Physical Therapy Association (APTA) for grading Clinical Practice Guidelines.80
Data extraction
The methods and results sections of the included studies were to be reviewed and data regarding the study demographics, methodology were extracted and placed in table form. Individual outcomes for pain, range of motion, strength, and function were cataloged. Justification for extracting these specific outcomes is based on (1) remaining consistent with the original review32 and (2) these outcomes are synonymous with a comprehensive review considering exercise therapy in RC impingement.63 The effectiveness of these outcomes was assessed over time (intra-group evaluation) and when appropriate, across groups (between-group evaluation). When available, statistically significant differences (within and across cohorts) in pre- and post- outcomes were recorded. Clinical significance (when statistical significance was p < 0.05 and the intra-group or between group difference was ≥20%)63 was also reported when feasible to determine. The rationale to incorporate both statistical and clinical significance was (1) clinical significance is likely to be more valuable to practicing clinicians and (2) this is consistent with the methodology of the fore mentioned RC impingement review,63 which also set out to develop an evidence-based protocol from those results. Additionally, if no statistical significance was calculated or reported for the outcome of ‘function’ (includes shoulder specific disability outcomes) than the currently accepted minimally clinically important difference (MCID) (if previously established) of the outcome measure in question was used to determine the significance of the post-intervention change in the respective cohorts.
Synonymous with the methods of the data extraction, one reviewer (M.J.) extracted the methodology, the results, demographics, outcomes, and statistics of included studies, and a second reviewer (S.H.) verified the data for accuracy and completeness.
Heterogeneity of included studies
Due to inclusion criteria of accepting randomized and non-randomized clinical trials, calculation of heterogeneity across studies was deemed inappropriate on the basis of methodological heterogeneity and thus, a meta-analysis was not performed.
Statistical analysis
All numerical data was calculated by inputting the extracted data into Microsoft Excel (2016) spreadsheets and using the appropriate mathematical functions (i.e. ‘SUM’, ‘PERCENTILE’, etc.) to calculate the respective numerical values and results.
RESULTS
Study selection
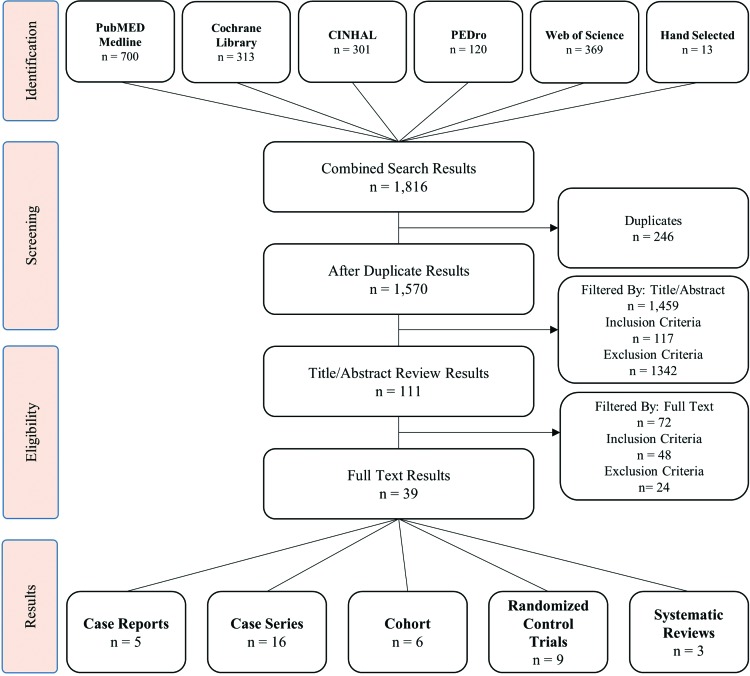
An aggregate total of 1570 citations was identified from the search after duplicates were removed (Figure 1). Based upon the number of identified studies, the search strategy was sufficiently comprehensive, returning more than our times the number results of previous reviews that investigated similar questions.32,45 After title and abstract screening 111 articles remained. Of the 72 articles excluded by full text, 48 were eliminated due to not meeting the inclusion criteria and 24 of them were eliminated due to meeting the exclusion criteria. Only one study81 was excluded due to not being able to find a full text version after exhausting all available resources (online databases previously mentioned, researchgate.com, Stanford University medical libraries and their network resources, attempting to contact the corresponding author). A total of 39 studies were included: five case reports,82-86 16 case series,1,87-101 six cohort studies (two retrospective102,103 and four prospective),40,104-106 and nine randomized control trials.47-49,52,107-111 Additionally, three relevant systematic reviews32,42,45 were identified. Details of included studies and patient demographics can be seen in Table 3.
Figure 1.
Flow diagram based on the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.
Table 3.
Patient Demographics
| First author (year) | Study design (Level of evidence)96 | Treatment groups (n = *) | Participants | Diagnosis€ | Diagnosis criterion | Traumatic or atraumatic (n = *) | Symptom Duration | Outcomes | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n = * | Mean age | Gender* | ||||||||
| Itoi (1992)109 | Case series (IV) | G0: Non-surgical (all pts) (62) G1: satisfied (15) G2: unsatisfied (8) |
Subject: 54 shoulder: 62 | 63 yr | M:F 32:22 (shoulder: M:F 36:26) | Full-thickness RC tear | Positive arthrogram | NR | NR | -Pain -Function -ROM -Strength |
| Bokor (1993)105 | Case series (IV) | G1: Non-surgical (53) | Subject: 53 | 62.2 yr | M:F 40:13 | Full-thickness RC tear | Positive arthrogram | Trauma: (40) Atraumatic: (13) | < 3 mo: 28 (53 %) 3-6 mo: 9 (17%) > 6 mo: 16 (30%) |
-ASES -UCLA score |
| Hawkins (1995)108 | Case series (IV) | G1: Non-surgical (19) G2: Not satisfied w/ non- surgical (14) (n=12 received surgery) |
Subject: 33 | 60 yr | M:F 27:6 | Full-thickness RC tear | Positive arthrogram | Trauma: (12) Atraumatic: (48) |
13.7 mo (82%) 22.5 yr (18%) |
-Strength -ROM -Constant-murley |
| Wirth (1997)114 | Case series (IV) | G1: Exercise therapy (60) | Subject: 60 | 64 yr | M:F 38:22 | Full-thickness RC tear | “Radiographically documented full thickness tears” |
NR | 19 mo | -ASES |
| Palmer (1998)101 | Case report (V) | Aquatic Therapy (1) | Subject: 1 | 78 yr | F: 1 | Full-thickness RC tear supra: 1 |
MRI | Traumatic: (1) | 2 wk | -Motion -Strength -Function: Overhead crawl (40 ft. x 2) |
| Yamada (2000)115 | Case series (V) | G1: Non-surgical (14) G2: Surgery (26) |
Subject: 40 | 70 yr | M:F G1: 9:5 G2: 23:3 |
Full-thickness RC tear supra, infra: NR |
Positive arthrogram | NR | Mean: 44 mo (12 mo – 11 yr) | - JOAS |
| Goldberg (2001)107 | Case series (V) | G1: Non-surgical (46) | Subject: 46 | 65 yr | M:F 22:24 | Full-thickness RC tear NR: 16 supra: 26 supra, infra: 2 supra, infra, subscap: 2 |
US, arthrogram, or MRI | NR | “None of the cuff tears were acute” |
-Simple shoulder test -SF-36 |
| Shibata (2001)126 | RCT (II) | G1: Sodium hyaluronate Injection (38) G2: Sodium hyaluronate & Dexamethasone (40) |
Subject: 78 | G1: 59.5 yr G2: 60.4 yr |
M:F 55:23 | Full thickness RC tear | MRI or Arthrogram | Traumatic: 42 Atraumatic: 36 |
G1: 5.8 mo G2: 4.7 mo |
-UCLA score -Unsatisfied (Surgery) |
| Vad (2002)120 | Cohort study (Retrospective) (III) | G1a: PT + meds (28) G1b: PT + meds + CS (12) G2: Failed G1a/b arthroscopy (32) G3: Primary surgery RCT repair (36) |
Subject: 108 | G1: 63.2 yr G2: 62.9 yr G3: 59.4 yr | M:F 50:58 | Full-thickness RC tear | MRI | Atraumatic | “Chronic” | -Shoulder rating questionnaire -ROM -Strength |
| Piccoli (2004)102 | Case report (V) | Multimodal (1) | Subject: 1 | 76 yr | F: 1 | Full-thickness RC tear supra: 1 |
MRI | Traumatic | 1 wk | -SPADI -SF-12 -ROM -Strength |
| Ainsworth (2006)104 | Case series (IV) | G1: Non-surgical (10) (Torbay rehabilitation program) | Subject: 10 | 75.6 yr | M:F 4:6 | Massive RC tear † | US | NR | NR | -OSDQ -SF 36 |
| Levy (2007)116 | Case series (IV) | G1: Non-surgical (17) | Subject: 17 | 80 yr | M:F 6:11 | Massive RC tear † supra, infra, subscap: 17 |
MRI (n=11) US (n=6) | Atraumatic | NR | -Constant-murley |
| Lunn (2007)119 | Cohort study (Retrospective) (III) | G1: Nonoperative (14) G2: Open repair (5) |
Subject: 19 | 47.7 yr | M:F 4:15 | Full-thickness infra: 14 |
MRI | Traumatic: 2 Atraumatic: 17 | 51.6 mo | -Strength -Constant-murley -MRI findings |
| Ainsworth (2009)127 | RCT (II) | G1: PT + Exercise (30) G2: Control (Placebo) (no exercise) (30) |
Subject: 54 | 78.2 yr | M:F 29:31 | Massive full thickness ( > 5 cm) | “Radiological diagnosed” | NR | < 12 mo: n = 26 >12 mo: n = 34 |
-OSS -SF-36 -MYMOP ROM |
| Baydar (2008)118 | Case series (IV) | G1: Non-surgical (20) | Subject: 20 | 60.9 yr | M:F 7:13 | Full-thickness RC tear (supraspinatus) small: 9 medium: 7 large: 3 |
MRI | NR | NR | -ASES -Constant-murley -SF 36 -Isokinetic strength -Patient satisfaction |
| Moosmayer (2010/2014)47,48 | RCT (II) | G1: Surgical (52) G2: PT (51) G2→G1 (9; 18%) |
Subject: 103 | G1: 59 yr G2: 61 yr | M:F G1: 37:15 G2: 36:15 | Full-thickness RC tear G1: supra: 37 supra, infra: 14 supra, subscap: 1 G2: supra: 40 supra, infra: 10 supra, subscap: 1 |
MRI US | Traumatic: G1: (24) G2: (16) Atraumatic: G1: (22) G2: (22) Inadequate trauma: G1: (6) G2: 13) |
G1: 12.3 mo G2: 9.8 mo |
-Constant-murley -ASES -SF 36 -Pain VAS -ROM -Strength -Patient satisfaction |
| Tanaka (2010)113 | Case series (IV) | G1: Non-surgical (Subject: 62 shoulders: 65) G2 Failed G1→surgery (Subjects: 56 shoulders: 58) |
Subject: 118 shoulder: 128 | 69 yr | M:F 67:61 | Full-thickness RC tear small: 41 medium: 64 large: 18 |
MRI | Traumatic: G1: (14, 21.5%) G2: (14, 24.1%) Atraumatic: G1: (51, 78.5%) G2: (44, 75.9%) |
NR | -Constant-murley -Night pain -ROM (FLX, ER) -Tear size -Surgical VZV just and weakness beginning |
| Gialanella (2011)128 | RCT (II) | G1: PT & CS (x1) (20) G2: PT & CS (x2) (20) G3: PT (20) |
Subject: 60 | G1: 78.7 yr G2: 77.3 yr G3: 79.4 yr |
M:F G1: 2:18 G2: 1:19 G3: 2:18 |
Full-thickness RC tear small: 31 medium: 18 large: 11 |
MRI US | NR | G1: 6.6 mo G2: 4.4 mo G3: 5.2 mo |
-Pain VAS -Shoulder functional status -Constant-murley |
| Merolla (2011)1 | Case series (IV) | G0: Conservative therapy (60) G1: ‘Successful’ (33) G2: G0→ surgery (27) |
Subject: 60 Shoulder: 60 | G0: 52 yr G1: 68 yr G2: 54 yr |
M:F 24:36 | RC tear G1: “complete tear” (33), (+) tear of LHB G2: RC tear (27) |
MRI | NR | NR | -Constant-murley -Pain VAS -ROM |
| Kijma (2012)110 | Case series (IV) | G1: Nonsurgical (43) | Subject: 43 | 62 yr | M:F 30:13 | “Rotator cuff tear” | MRI or MRA | NR | NR | -JOAS |
| Krischak (2013)124 | RCT (II) | G1: Standard OT (22) G2: Home exercises (16) |
Subject: 38 | 55.3 yr | M:F G1: 8:8 G2: 16:6 |
Full-thickness RC tear | MRI & physical exam | Atraumatic: (100%) | ≥3 mo | -Pain -Conastant- murley -EQ-5D -Strength -ROM |
| Kuhn (2013)40 | Cohort study (III) | G0: PT program‡ (422, 100%) G1: Cured (237, 62.2%) (no formal f/u scheduled) G2: Improved (continue PT) G3: No better (82, 29%) (offered surgery) |
Subject: 422 | 62.6 yr | M:F 206:194 | Full-thickness RC tear supra: 281 (70%) supra & infra: 83 (21%) supra, infra, teres: 3 (<1%) subscap: 2 (<1%) supra & subscap: 20 (5%) supra, infra, subscap: 7 (2%) unknown: 4 (1%) |
MRI | Atraumatic: (100%) | NR | -SF 12 -ASES -Shoulder activity score -SANE score |
| Benazzo (2014)99 | Case report (V) | Nonoperative: (1) | Subject: 1 | 23 yr | F: 1 | “Complete Lesion” supra: 1 |
MRI | Traumatic | 1 day | -SST -Constant-murley -ROM -Strength |
| Boorman (2014)123 | Cohort study (III) | G0: 3 mo supervised, non-operative§ G1: “Successful”(no surgery indicated) (70; 75%) G2: “failed” (underwent surgery) (23; 25%) |
Subject: 93 | 60 yr | M:F 54: 39 | “Full-thickness RC tear” (excluded full-thickness subscap & teres) |
MRI or US | Traumatic: (46, 49%) Atraumatic: (47, 51%) |
≥3 mo | -RC-QOL -ROM -Strength |
| Güzelant (2014)117 | Case series (Retrospective) (IV) | G1: “Conservative therapy” (33) | Subject: 33 | 71 yr | M:F 19:14 | “Massive retracted, irrepairable rotator cuff tears” (≥ 2 tendons) |
MRI | NR | 5.5 yr (66 mo) | -Pain VAS -ROM -Strength -ASES -UCLA score |
| Kukkonen (2014/2015)52,125 | RCT (II) | G1: PT (55) G2: Acromioplasty & PT (57) G3: RC repair, acromioplasty & PT (55) |
Subject: 171 Shoulder: 167 | G1: 65 yr G2: 65 yr G3: 65 yr |
M:F G1: 24:31 G2: 29:28 G3: 29:26 |
“Symptomatic supraspinatus tendon tear comprising <75% of tendon insertion” |
MRI | Atraumatic | G1: 26 mo G2: 28 mo G3: 28 mo |
-Constant-murley -Radiologic outcome -Cost -Patient satisfaction |
| Collin (2015)106 | Case series (IV) | G1: “Rehabilitation program” (45) (nonoperative) |
Subject: 45 | 67 yr | M:F 17:28 | Full thickness RC tear “of at least 2 tendons” Goutailler Stage: 3 - 4 Pseudoparalysis (<90 ° anterior elevation) |
NR | NR | NR | -Constant-murley |
| Lambers Heerspink (2015)49 | RCT (II) | G1: “Conservative Management” (31) G2: RC repair (25) |
Subject: 56 | G1: 60.5 G2: 60.8 |
M:F G1: 20:11 G2: 15:10 |
Full-thickness RC tear
-Supra: G1: 31; G2: 25 -Infra: G1: 1; G2: 0 -Subscap: G1: 4; G2: 1 |
MRI | Atraumatic | G1: 12.0 mo G2: 12.5 mo |
-Constant-murley -VAS Pain -Dutch simple shoulder test -Radiologic outcome |
| Baumer (2016)121 | Cohort Study (III) | G1: PT (25) G2: Healthy controls (25) |
Subject: 25 Shoulder: 50 |
G1: 60.2 G2: 59.0 |
M:F 7:18 | Full-thickness RC tear G1: “small” tears mean: 1.4 cm range: 0.8-2.6 cm G2: Tendinosis: 15 partial thickness: 4 full thickness: 3 mean size: 1 cm |
MRI or US | NR | NR | -Shoulder motion (radiography imaging system) -Strength -Pain VAS -WORC score |
| Christensen (2016)122 | Case series (IV) | G1: Non-operative(30) G2: Control (30)** |
Subject: 30 Shoulder: 60 |
70.4 | M:F 20:10 | “Irreparable RC tears” -Complete supra tear: 30 -Infra tear: 30 complete: 27 partial: 3 -Subscap tear: 6 |
US and MR or Arthroscopy |
Traumatic & atraumatic |
38.6 mo | -OSS -VAS Pain -EQ-5D -ROM -Strength |
| Miller (2016)111 | Case series (IV) | G1: “Exercise therapy” (5) | Subject: 5 | 60.2 | M:F 2:3 | “Symptomatic small, degenerative full-thickness RC tear” Supraspinatus (only) Goutallier grade ≤ 2 |
MRI | Degenerative | ≥3 mo | -Joint kinematics -ASES -WORC -DASH |
| Mischke (2016)100 | Case report (V) | “Conservative” therapy (1) | Subject: 1 | 57 | F: 1 | “Massive your parable rotator cuff tear” -Supraspinatus |
MRI | Insideous onset | 6 mo | -Pain -Quick DASH -GROC -ROM |
| Upadhyaya (2016)103 | Case report (V) | “Non-operative treatment” (1) | Subject: 1 | 49 | M: 1 | “Full thickness” -Supraspinatus |
MRI | Traumatic | “acute” | -MRI findings -Strength |
| Moosmayer (2017)112 | Case series (IV) | G1: Non-operative treatment (49) | Subject: 49 | 61 | M:F 30:19 | “Full-thickness RC”
- < 3 cm -Supra: 38 -Supras & infra: 11 |
MRI & US | Traumatic: 31 Atraumatic: 18 |
NR | -Tear size/progression -Muscle atrophy -Fatty degeneration -Constant score. -ASES -SF-36 -Pain VAS |
ASES, American shoulder and elbow surgeon's evaluation form; Constant-murley, constant murley shoulder outcome score; CS, cortical steroid injection; Con. Tx, conservative treatment; DASH, disabilities of the arm, shoulder, and hand outcome measure; ER, External rotation; EQ-5d, EuroQol questionnaire; Ft, feet; FLX, Flexion; G, group; GROC, global rating of change; HK Test, Hawkins Kennedy test; Infra, infraspinatus; JOAS, Japanese orthopedic association score; mo, month(s); LHB, long head of biceps tendon; MYMOP, measure yourself medical outcome profile; NR, not reported; OT, occupational therapy; OSS, Oxford shoulder score; Patte Classification, tears retracted past glenoid margin; PT, physical therapy; ROM, range of motion; RC, rotator cuff; RC-QOL; rotator cuff quality of life index instrument; RCT, randomized controlled trial; SF-12, short form–12 questionnaires; SF-36, short form–36 questionnaires; SPADI, shoulder pain and disability index; SST, shoulder short test score; Subscap, subscapularis; Supra, supraspinatus; Teres, teres minor; UCLA Score, University of California Los Angeles shoulder rating scale; VAS, visual analog score; WORC, Western Ontario rotator cuff index; Yr, year(s); *, numerical values given as number of subjects (unless otherwise specified); †, Grade 3 tearing; ‡, all subjects began a physical therapy program and were reevaluated at 6 and 12 weeks, at those times patient were assigned to G1, G2, or G3 based on findings. §, all subjects underwent a 3 mo supervised program of nonoperative treatment & with an evaluated by orthopedic surgeon and assigned to G1 or G2; **, subjects in G1 served as their own controls which composed G2.
It is important to note, there were two instances, Moosmayer et al 201047 and 201448 and with Kukkonen et al 201451 and 2015,52 in which consecutive, but separate studies (an original study and a long-term follow-up study) were published on the same patient cohort. To avoid the results of these studies having excessive weight during this investigation, the data extraction, and statistical analysis used the most current publication of these cohorts (Moosmayer et al 201448 and Kukkonen et al 201552). This justification has been used in previous RC intervention reviews.45,112
There were three systematic reviews after the filtering that exclusively included a cohort of studies that met the inclusion and exclusion criteria of this review. The earliest of these publications, Ainsworth et al (2007),32 is the systematic review that is being updated by this current investigation. Sieda et al64 included both surgically and conservatively treated RCT. However, the included studies specific to conservative management of RCT, as well as the means by which Sieda et al64 separated (compared) the surgical and non-operative results provided sufficient criteria to include the review in this investigation. Ryosa et al,45 the most recent review, was specific to randomized control trials.48,49,52 All three which have been included in this review as well. Further details regarding the scope of these systematic reviews are summarized in Appendix B.
The primary purpose for including pertinent systematic reviews was to: (1) provide a comprehensive view of the literature for other researchers and clinicians and (2) compare the comprehensiveness, methodology, and findings of this review to that of current systematic review literature on this topic. The results and conclusions of the reviews are summarized in Appendix C. The comparison of the results and conclusions of these reviews to the current investigation is elaborated on in the discussion section of this manuscript.
Patient demographics:
The aggregate number of shoulders was n = 2010, in 1913 subjects. There was an even distribution between males (53.8%, n = 1042) and females (46.2%, n = 896). Discrepancy (n = 25) in the total subjects and the sum of the number of men and women is due to 22 patients' gender not being recorded in Kuhn et al (2013)40 and Kukkonen et al (2015)52 not reporting the gender for 4 of 13 subjects who were lost to follow-up. Additionally, Moosmayer et al (2017)95 included 13 of 49 subjects from other included cohorts47,48 but the gender of these 13 subjects was not specified and thus, were unable to be adjusted for when calculating the aggregate total of males and females.
Of the total number of shoulders included in this current investigation (n = 2010), 1643 (82%) were treated non-operatively, 85 (4%) were controls or received no intervention, 256 (13%) shoulders were originally designated to a surgical cohort group, 292 (15%) were unsatisfied with non-operative treatment and went on to have surgery. Subject numbers were further broken down into a number of shoulders per study design. Randomized control trials accounted for 562 (28%) shoulders, cohort studies included 692 (34%) shoulders, case series included 751 (37%) shoulders, and case reports included 5 shoulders (<1%). Ages of the cohorts ranged from 23 to 80 years of age, the mean age for all included subject was 64.1 years old. (Table 3)
Diagnosis & Involved Muscles
All but three studies89,97,110 stated the specific advanced imaging (ultrasonography: nine studies, magnetic resonance imaging (MRI): 26 studies, arthrogram: seven studies, and/or arthroscopy: one study) that was used to confirm the diagnosis of FTT. Regarding the three studies in which the specific imaging study was not stated, Wirth et al97 and Ainsworth et al (2009)110 confirmed diagnosis by “radiographically documented full thickness tears” and in the third study, Collin et al,89 it is assumed that MRI was used as the authors identified the specific tendon(s) involved and stratified the stages of fatty infiltrate via the Goutallier classification.113 (Table 3).
The tendon(s) or number of tendons involved were reported in 1311 (65%) shoulders. Of those reported on, supraspinatus (848 shoulders, 65%) and infraspinatus (184 shoulders, 14%) were the most common tendons involved. This is consistent with prior reports of the junction between these two tendons (16 and 15 mm posterior to the long head of the biceps tendon) being the most prevalent location of tear initiation.114 Subscapularis tendon involvement occurred in only 44 (3%) shoulders and teres minor was reported in 3 (<1%) shoulders. (Table 3). Multiple tendons were involved in 232 shoulders (18% of those reported on).
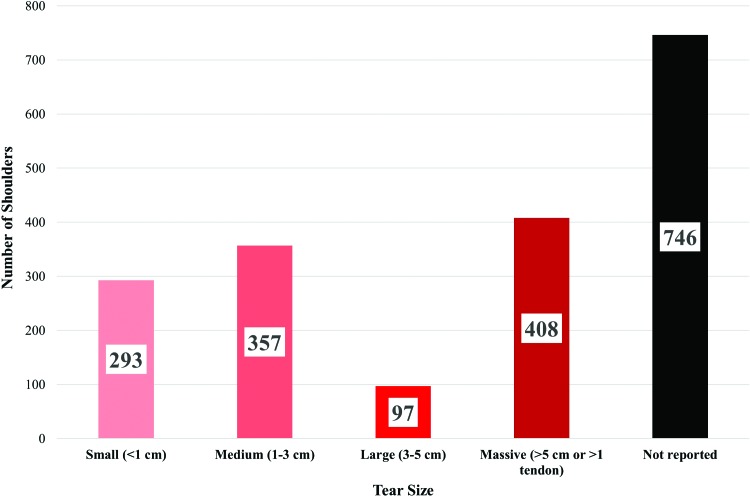
Tear size was reported in 1155 (57%) shoulders. Though there are multiple RCT classification systems,115,116 the one proposed by DeOrio and Cofield117 was most commonly reported in the included studies. Thus, this system was used to stratify the different sizes of tears reported. A graphical representation of these results can be seen in Figure 2.
Figure 2.
A graphical representation of the distribution of the rotator cuff tear sizes for the shoulders described in the included studies.
Mechanism and Duration of Symptoms
The mechanism of injury was classified into four groups: traumatic, atraumatic, “insufficient trauma”, or not reported. The mechanism of injury was reported in 1462 (73%) shoulders with atraumatic onset being the predominant mechanism of injury, occurring in 1192 (82%) shoulders. (Table 3)
The duration of shoulder symptoms prior to investigation ranged from one day to 5.5 years and was reported in 1133 (56%) shoulders. Given the variability in which the duration of symptoms was reported (i.e. “not-acute”, “chronic”, “greater than or equal to 3 mo.), this data was synthesized into <3 months, 3-6 months, 6-12 months, or > 12 months. (Table 3)
Study quality assessment
Observational studies
The evaluation of the quality of the included 27 observational studies (Table 4) revealed concerns in the methodology. Only one study106 met all criteria, however, the primary purpose of the study was identifying predictive baseline factors for failed conservative treatment and thus, no follow-up disability or impairment measurements were taken. All studies included relevant subjects, established ‘appropriate inclusion criteria’, and accounted for subjects lost to follow-up. Though, all but two case reports84,86 used ‘appropriate disability outcomes’ and 22 (65%) studies had an ‘appropriate impairment outcome.’ Only 12 (31%) observational studies explicitly stated that it was a prospective investigation, while 20 (74%) studies had an ‘adequate follow’ of ≥ one year. The criterion that was most often missed was the statement of a ‘blinded assessment.’ Only three studies,95,105,106 stated the blinded follow-up assessments were performed. The suspected reason for the lack of blinding was due to the high prevalence of case series. As there is most often only one cohort in these study designs, it may have seemed of lower importance for authors to blind the assessor.
Table 4.
Observation study methodology - methodological quality criteria for assessment of observational studies95
| First Author (Year) | Relevant subjects | Appropriate inclusion criteria | Prospective investigation (stated) | Adequate follow-up (1 year after final treatment) | Lost to follow-up accounted for | Blinded assessment (stated) | Appropriate impairment outcomes | Appropriate disability outcomes | Total Score |
|---|---|---|---|---|---|---|---|---|---|
| Itoi (1992)109 | ✔ | ✔ | ✗ | ✗ | ✔All present | ✗ | ✔ | ✔ | 5/8 |
| Bokor (1993)105 | ✔ | ✔ | ✗ | ✔ | ✔ | ✗ | ✔ | ✔ | 6/8 |
| Hawkins (1995)108 | ✔ | ✔ | ✔ | ✔ | ✔ | ✗ | ✔ | ✔ | 7/8 |
| Wirth (1997)114 | ✔ | ✔ | ✔ | ✔ | ✔ | ✗ | ✔ | ✔ | 5/8 |
| Palmer (1998)101 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | ✔ | None measured | 5/8 |
| Yamada (2000)115 | ✔ | ✔ | ✗ | ✔ | ✔ | ✗ | ✔ | ✔ | 6/8 |
| Goldberg (2001)107 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | None measured | ✔ | 5/8 |
| Vad (2002)120 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | None measured | ✔ | 5/8 |
| Piccoli (2004)102 | ✔ | ✔ | ✗ | ✗ | ✔ All present | ✗ | ✔ | ✔ | 5/8 |
| Ainsworth (2006)104 | ✔ | ✔ | ✗ | ✗ | ✔ All present | ✗ | None measured | ✔ | 4/8 |
| Levy (2007)116 | ✔ | ✔ | ✔ | ✗ | ✔ All present | ✗ | ✔ | ✔ | 6/8 |
| Lunn (2007)119 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | None measured | ✔ | 5/8 |
| Baydar (2009)118 | ✔ | ✔ | ✔ | ✔ | ✔ | ✗ | ✔ | ✔ | 7/8 |
| Tanaka (2010)113 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | ✔ | ✔ | 6/8 |
| Merolla (2011)1 | ✔ | ✔ | ✔ | ✔ | ✔ All present | ✗ | ✔ | ✔ | 7/8 |
| Kijma (2012)110 | ✔ | ✔ | ✔ | ✔ | ✔ | ✗ | None measured | ✔ | 7/8 |
| Kuhn (2013)40 | ✔ | ✔ | ✔ | ✔ | ✔ | ✗ | ✔ | ✔ | 7/8 |
| Benazzo (2014)99 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | ✔ | ✔ | 6/8 |
| Boorman (2014)123 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | 8/8 |
| Güzelant (2014)117 | ✔ | ✔ | ✗ | ✔ | ✔ | ✗ | ✔ | ✔ | 6/8 |
| Collin (2015)106 | ✔ | ✔ | ✔ | ✔ | ✔ | ✗ | ✔ | ✔ | 7/8 |
| Baumer (2016)121 | ✔ | ✔ | ✔ | ✗ | ✔ | ✗ | ✔ | ✔ | 6/8 |
| Christensen (2016)122 | ✔ | ✔ | ✔ | ✗ | ✔ | ✔ | ✔ | ✔ | 7/8 |
| Miller (2016)111 | ✔ | ✔ | ✔ | ✗ | ✔ All present | ✗ | ✔ | ✔ | 6/8 |
| Mischke (2016)100 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | ✔ | ✔ | 6/8 |
| Upadhyaya (2016)103 | ✔ | ✔ | ✗ | ✔ | ✔ All present | ✗ | ✔ | None measured | 5/8 |
| Moosmayer (2017)112 | ✔ | ✔ | ✗ | ✔ | ✔ | ✔ | ✔ | ✔ | 7/8 |
Randomized control trials
When considering the potential bias in the included randomized control trials, it was determined that all 8 revealed an aggregate ‘low’ risk of bias based on the seven criteria assessed by the Cochrane Collaboration's domain-based evaluation framework.76 However, all of the randomized control trials did demonstrate a ‘high’ risk of bias due to lack of blinding of participants, personnel, and outcome assessments. (Table 5).
Table 5.
Randomized control trial – Risk of bias93
| First Author (Year) | 1. Randomized sequence generation | 2. Allocation conceal moment | 3. Blinding of participants and personnel | 4. Blinding of outcome assessment | 5. Incomplete outcome data | 6. Selective reporting | 7. Other sources of bias | Total risk of bias |
|---|---|---|---|---|---|---|---|---|
| Shibata (2001)126 | Low | Low | High | High | Low | Low | Low | Low |
| Ainsworth (2009)127 | Low | Low | High | High | Low | Low | Low | Low |
| Moosmayer (2010/2014)47,48 | Low | Low | High | Low | Low | Low | Low | Low |
| Gialanella (2011)128 | Low | High | High | High | Low | Low | Low | Low |
| Kirschak (2013)124 | Low | Low | High | High | Low | Low | Low | Low |
| Kukkonen (2014/2015)52,125 | Low | Low | High | High | Low | Low | Low | Low |
| Lambers Heerspink (2015)49 | Low | Low | High | High | Low | Low | Low | Low |
Systematic reviews
The AMSTAR guidelines demonstrated sufficient rigor to identify flaws in the methodology of the identified systematic reviews. Though none of the three reviews met all criteria both Sieda et al64 and Ryosa et al45 demonstrated ‘Good’ methodology, meeting 10 and 9 out of the 11 methodology criteria, respectively. Ainsworth et al (2007)32 methodology was rated as ‘Fair’ as it met only 5 of the 11 methodology criteria. (Table 6)
Table 6.
| Criteria | Reviews: Author (year) | |||
|---|---|---|---|---|
| Ainsworth (2007)32 | Sieda (2010)81 | Ryosa (2016)45 | Jeanfavre (2017) | |
| 1. Was there ‘a priori’ design provided? | ✔ | ✔ | ✔ | ✔ |
| 2. Was there duplicate studies selection and data extraction? | ? | ✔ | ✔ | ✔ |
| 3. Was a comprehensive literature search performed? | ✔ | ✔ | ✔ | ✔ |
| 4. Was a status publication (i.e. gray literature) used as an inclusion criteria? | ✗ | ✗ | ✗ | ✗ |
| 5. Was a list of studies (included and excluded) provided? | ✗ | ✔ | ✗ | ✔ |
| 6. With the characteristics of the included studies provided? | ✔ | ✔ | ✔ | ✔ |
| 7. With a scientific quality of the included studies assessed and documented? | ✔ | ✔ | ✔ | ✔ |
| 8. Was a scientific quality of the included studies used appropriately in formulating conclusions? | ✔ | ✔ | ✔ | ✔ |
| 9. Was the methods used to combine the findings of studies appropriate? | NA | ✔ | ✔ | ✔ |
| 10. Was a likelihood of publication bias assessed? | ✗ | ✔ | ✔ | ✗ |
| 11. Was a conflict of interest included? | ✗ | ✔ | ✔ | ✔ |
| Total score: | 5/11 | 10/11 | 9/11 | 9/11 |
| Quality Rating: (good, fair, or poor) | Fair | Good | Good | Good |
NA, not applicable; ✔: yes; ✗: no; ?: cannot determine or not reported
Outcomes
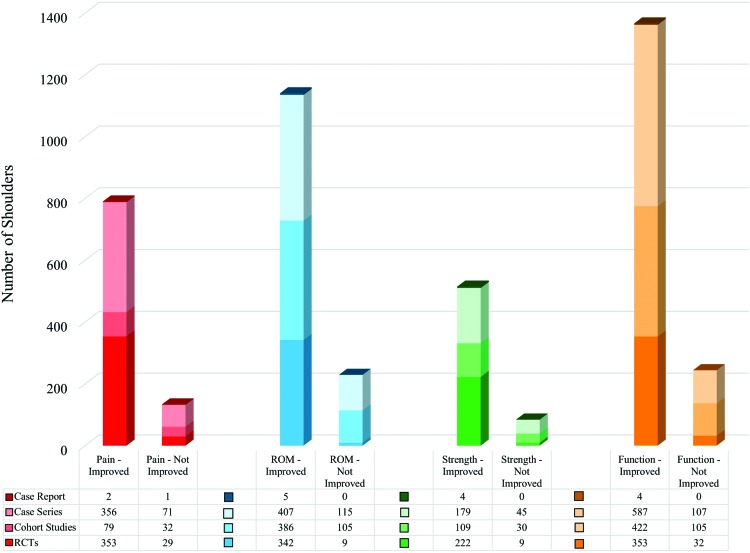
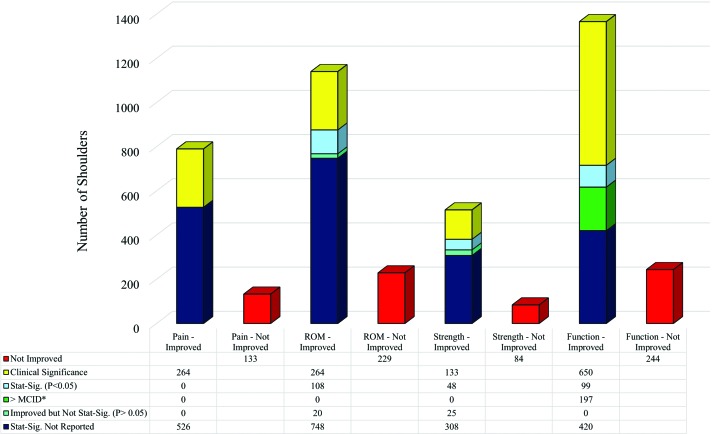
Individual outcomes of pain, range of motion, strength, and function were extracted from each of the studies. Each outcome is discussed below. The data extraction for the each of the outcomes can be found in Appendices D - G. Graphical representation of the outcomes are also provided in Figure 3 and Figure 4.
Figure 3.
A graphical representation and data table of the pain, range of motion (ROM), strength and function for the conservatively treated shoulders in the included studies. The shoulders from the different study designs are represented by the different color shades as noted in the legend.
Figure 4.
A graphical representation and data table of the pain, range of motion (ROM), strength and function for the conservatively treated shoulders in the included studies. The statistical and clinical significant differences are noted by the different color shades in the legend. Clinical significance, statistical significance (P < 0.05) and improves by > 20%; MCID, minimal clinical importance difference, Stat-Sig, statistical significance (P < 0.05); *, MCID was only used for functional outcome measures when no statistical significance was reported and when an accepted MCID had previously been established within the literature.
Pain
Pain was reported in 26 (79%) of the studies with an average follow-up time of 2.7 years (32.5 months). Over half of the studies (n = 16, 59%) measured pain through disability or impairment outcome measures, while the remaining 11 (41%) studies used a specific pain tool; either the visual analog scale (VAS) or the numerical rating pain scale (NRPS). Tanaka et al96 was the only study with a cross-sectional design, and thus, a change in pain outcome could not be determined. Pain outcomes improved in the remaining 26 (96%) studies with non-operative treatment. Statistical significance for within group change was reported in eight (29% of the 26) studies, all of which were statistically significantly different (p < 0.05; 95% CI) and clinically significant (improvement by ≥ 20%). The pain reported outcomes for all studies can be found in Appendix D.
When comparing across cohorts, two studies103,111 compared physical therapy with and without the addition of corticosteroid injection. Both studies favored physical therapy plus corticosteroid injection with a statistically significant difference (p<0.05). However, only in the short term (1 to 3 months) was this difference determined to be clinically significant (p<0.001).111 Additionally, there were four studies that compared non-operative treatment to surgical cohorts, and though all of these reported improvements in both groups, three of them demonstrated statistically significant improvements in pain (p < 0.05; 95% CI) in the surgical groups.48,49,52 None of these met clinical significance. The remaining study reported no statistical difference between the pain in the non-operative cohort and the operative cohort.96
There were nine cohorts (133 shoulders) in which pain did not improve enough for a ‘satisfactory’ result.1,48,91,92,95,96,103,111 Four of the cohorts converted to surgery.1,48,96,103 In another cohort,111 ‘physical therapy’ was the control and number of shoulder injections was the independent variable. Factors that differentiated the remaining ‘unsatisfied’ cohorts was ‘sleep loss due to night pain’ (p = 0.01 when compared to the ‘satisfied’ cohort in this study)91 and tear size progressing > 20 mm from initial measurement (p < 0.004).95
In summary, pain outcomes were reported for 40 non-operatively treated cohorts that included 923 shoulders. Of these, 31 (78%) cohorts, consisted of 790 (86%) shoulders that reported improvements in pain versus nine (22%) of cohorts consisting of 133 (14%) shoulders that did not improve or not to a ‘satisfactory’ level. Statistical significance was calculated in 10 (25%) cohorts consisting of 264 (29%) shoulders, all but one of these demonstrated both statistically (p < 0.05) and clinically significant improvements.
Range of motion
Range of motion (ROM) was reported in 28 (85%) studies as shown in Appendix E. The average follow-up for these reported outcomes was 2.4 years (29.2 months). A motion specific tool was used in 19 (68%) of these studies, while the remaining studies captured the ROM through disability and impairment outcomes. In the studies that specified the direction of motion, the most common ROM movements that were recorded were abduction (16 studies, 57%), flexion (15 studies; 54%), and external rotation (13 studies; 46%). Internal rotation (7 studies; 25%) and extension (one study; 4%) were much less common.
All of the studies that reported ROM demonstrated improvement in ROM post intervention in at least one cohort that received exercise therapy and conservative management. Of the nine studies1,92,94,98,100,101,103-105,109,111 that reported statistically significant within group change all nine demonstrated significant differences (p < 0.05; 95% CI) in at least one direction and in eight1,94,100,101,103-105,109 of these cohorts the improvement increased by ≥20% meeting clinical significance. There were only three select studies whose subjects’ ROM did not improve. Itoi et al92 identified a subset of patients who did not have ‘satisfied’ outcomes following conservative treatment and found that predictive factors were poor abduction ROM (108.0 ° vs 149.0 °; p < 0.05) and abduction weakness (3/5 on manual muscle testing (MMT)). Merolla et al1 developed a predictive score of 17 baseline variables and used a cutoff score of ≥13 out of 21 to identify patients who were likely to be ‘unsatisfied’ and opt for surgery within one year. The third cohort111 who did not demonstrate improvement was a control group who did not receive a corticosteroid injection in addition to physical therapy.
Statistically significant intragroup (pre and post rehab ET intervention) abduction ROM differences were demonstrated in nine studies (p < 0.05) and in seven (83%)1,94,101,103-105,109 of these studies the cohorts achieved clinically significant improvements. Likewise, significant intragroup flexion ROM differences were demonstrated in five studies (p < 0.05) with statistically significant differences in four (80%) studies1,100,101,104 and clinically significant differences in three (60%).1,100,104 Intragroup external rotation differences were reported in five studies and in three (60%) of these101,109,111 the improvements were both statistically (p < 0.05) and clinically different. Though it is likely of interest and benefit to clinicians and future researchers to identify which movements are most likely to significantly improve (both statistically and clinically) it should be noted that comparison across different planes of motion cannot be directly compared to one another from the above results due to the uneven distribution of different ROMs being reported.
Nine studies statistically examined intergroup differences. Three studies48,52,96 compared nonoperative cohorts to surgically treated cohorts, none of which found statistically significant difference between groups. Two studies compared conservative management with and without corticosteroid injections. One111 of these studies found no difference at six months, while the other study103 demonstrated no difference in the outcome but that the cohort that had received physical therapy plus corticosteroid injection took less time (5.3 months) to reach maximum abduction ROM (p < 0.05). The conclusions that can be drawn from other intergroup comparisons is that supervised occupation therapy (OT) and home exercise program demonstrates no difference in abduction, flexion, or external rotation ROM outcomes107 and that flexion and abduction ROM outcomes do not differ between cohorts whose tear progresses of tears by ≥20 mm or ≤ 20 mm.95
In summary, ROM outcomes were reported for 44 non-operatively treated cohorts that included 1369 shoulders. Of these, 36 (82%) cohorts, consisting of 1140 (83%) shoulders that reported improvements in ROM versus eight (19%) of cohorts consisting of 229 (17%) shoulders that did not improve or not to a ‘satisfactory’ level. Intra-group statistical differences were calculated in 14 (33%) cohorts, consisting of 272 (27%) shoulders, all of which demonstrated statistically significant differences in ROM (p < 0.05). Improvements in ROM were also clinically significant in 10 (23%) cohorts, 264 (19%) shoulders.
Strength
Strength was reported as an outcome in 21 (64%) studies with an average follow-up time of three years (35.5 months). See Appendix F for summarized strength outcomes and the specific tools and equipment used for measurement.
All studies that reported strength outcomes demonstrated improvement in at least one cohort that was treated with non-operative management. However, statistical comparisons for intragroup strength improvements was only reported in seven (33%) studies. Of these, six (75%) studies92,94,100,101,105,109 demonstrated statistically significant improvement (p < 0.05) and four (57%) studies the intragroup difference was also clinically significant.94,101,105,109
It is important to discuss the four instances in which a cohort's strength improvements were not statistically improved. In one study104 it was suspected that the lack of statistically significant change was due to too short of a follow-up time (nine weeks). It has been previously established that strength gains continue to progress well beyond the nine-week point of initiating resistance training.118 A second study109 that focused on the effects supplementing physical therapy with corticosteroid injections demonstrated both statistically and clinically significant strength gains at four weeks, but not at 24 weeks post-intervention, as there was a mild decline in each cohorts strength gains. This may speak to both, the transient effects that corticosteroid injections provide, as well as the necessity of a ‘maintenance’ program with rehab to ensure that strength gains are retained for the long term. Moreover, a case series by Hawkins et al91 demonstrated a subgroup of patients with ‘unsatisfied’ results that opted for surgery. Strength was measured in pounds using Constant-Murley score. Subjects in this subgroup reported average Constant-Murley strength score of 17.1 (equivalent to 15-18 lbs of abduction strength) as compared to the aggregate average Constant-Murley score of 23.2 (equivalent to 22-24 lbs of abduction strength). The difference between the groups was statistically (p = 0.008) and clinically significantly different. Similarly, Itio et al92 had a subgroup of subjects with an ‘unsatisfactory’ outcome (this is the same subgroup that was discussed previously in pain outcomes) who also failed meet statistically significant improvement in strength outcomes. This subgroup was retrospectively identified once outcomes were calculated to determine differences at baseline between the ‘satisfied’ and ‘unsatisfied’ cohorts. The variables that differentiated the ‘unsatisfied’ subgroup at baseline were poor abduction ROM (108.0 ° vs 149.0 °; p < 0.05) and abduction weakness (3/5 on manual muscle testing (MMT)). At post intervention follow-up (average of 3.4 years) only 63% of the ‘unsatisfied’ cohort had abduction strength that was ≥4/5 on MMT as compared to 87% of the ‘satisfied’ cohort. The intergroup difference was statistically (p < 0.05) and clinically significant.
When considering intergroup differences, seven studies reported statistically significant differences across cohorts. Hawkins et al91 and Itio et al92 both compared subgroups with ‘unsatisfied’ outcomes with that of a ‘satisfied’ cohort and, not surprisingly, found statistical (p = 0.008 and p < 0.05, respectively) and clinically significant differences favoring the ‘satisfied’ cohorts. Two studies compared the outcomes of non-operative treated cohorts to surgically treated cohorts. No difference was found at one year (p = 0.89),48 but statistically significant differences were found at two52 and five years.48 Neither of these differences were clinically significant. One study107 found no significant difference in any strength measurement in cohorts who received supervised occupational therapy versus a home program. Strength gains also proved to be statistically (p < 0.004) and clinically significant between a cohort who had tears that progressed by ≥20 mm over 8.8 years compared to subjects whose tears progressed <20 mm.95 The seventh article that compared across groups used the subjects’ contralateral shoulder as the control (did not receive any rehabilitation) and demonstrated a significant difference in post-intervention strength measures.104 However, a major flaw with this comparison was that the control limbs were only measured at time zero and thus, if a change in strength of the control limbs occurred post intervention it was not captured.
In summary, strength outcomes were reported for 28 non-operatively treated cohorts that included 598 shoulders. Of these, 23 (82%) cohorts, consisted of 514 (86%) shoulders that reported improvements in strength versus five (18%) cohorts consisting of 84 (14%) shoulders that did not improve or not to a ‘satisfactory’ level. Statistical differences were calculated in eight (29%) cohorts. Of these, seven cohorts consisting of 181 (30%) shoulders demonstrated statistically significant improvements (p < 0.05), while five (19%) cohorts, 133 (22%) shoulders, also made clinically significant gains for strength.
Function
Functional outcomes were reported in 33 (97%) studies with an average follow-up of 2.3 years (27.3 months). Thirty-one (97%) studies captured the function with a shoulder specific outcome measure, while one case report84 determined function by the patient's ability return to recreational swimming unrestricted. See Appendix G for details of the specific functional outcome measures used and the data extracted.
All 33 (100%) studies that reported on function demonstrated improvement in function with non-operative therapy. All 15 (45%) studies1,40,89,90,92,94,98,100-105,109,111 that reported intragroup differences (p < 0.05-0.0001) for shoulder specific outcomes demonstrated statistically significant differences and 11 (73%) of these studies1,40,90,92,94,98,100,101,103-105,109 demonstrated ≥ 20% improvement indicating clinically significant change.
Ten (30%) studies47,89,91,100,102,104,105,110,111 reported intergroup differences. Three studies91,95,106 denoted statistically (p = 0.038) and clinically significant differences between two conservatively managed cohorts, one with ‘satisfied’ results and another cohort. Hawkins et al91 demonstrated that poor response in Constant-Murley score following conservative therapy differentiated ‘satisfied’ (+7.1 points from baseline) from ‘unsatisfied’ (-1.1 points from baseline) at 3.8 years follow-up (p = 0.038). Similarly, Moosmayer et al (2017)95 showed that by dichotomizing subjects by tear progression ≥20 mm or < 20 mm over 8.8 years, that subjects with the <20 mm progression had better Constant-Murley scores (<20 mm progression: 81.0 vs > 20 mm progression: 58.5; p = 0.008), higher functioning ASES scores (<20 mm progression: 90.0 vs > 20 mm progression: 60.0; P = 0.02), but not significantly different SF-36 scores (p > 0.05). Boorman et al,106 on the other hand, sought to identify baseline predictive factors for subjects likely to ‘fail’ conservative therapy and opt for surgery. The authors found that baseline scores out of 100 (‘successful’ rehab cohort: 49 ± 21 vs. ‘failed’ rehab cohort: 33 ± 15; p = 0.017) on the Rotator Cuff Quality of Life Index (RC-QOL,as first described by Hollinshead et al119) was predictive for opting for surgery.
Three additional studies104,107,111 compared the intergroup difference between conservatively managed cohorts. Gialanella et al111 showed that there was no statistically significant difference (p>0.05) in Constant-Murley scores at three, six, or 12 months’ post-intervention between cohorts who received single or multiple shoulder injections plus physical therapy as compared to a cohort who only received physical therapy. Krischak et al107 compared a cohort who received ‘standard OT’ to a home exercise cohort and found that there was no difference in Constant-Murley score (p = 0.824) or EQ-5DL (p = 0.656) at two-month follow-up, but that there were statistically (p < 0.05) and clinically significant differences in the overall change in EQ-5DL health status subs-core, favoring the ‘standard OT’ cohort (+17.8 points vs home exercises group: + 3.2). The final study, Baumer et al104 demonstrated that despite a statistically (p < 0.01) and clinically significant change in the Western Ontario Rotator Cuff (WORC) score after nine months the intervention group score (70.3 ± 26) was significantly (p < 0.01) different than the baseline score of the healthy control group (98.2 ± 2.8). However, a limitation was that the healthy control group was only measured at baseline and thus, making the assumption that there was no change in the healthy control score.
Lastly, there were four studies48,49,52,102 that compared non-operative treatment to surgical RC repair. All of them used the Constant-Murley score as one of the region-specific outcomes. There was no statistically significant difference in total Constant-Murley score at 12 months (p > 0.05),49,52 24 months (p > 0.05),52 or four years (p = 0.61).102 One study48 did show a difference in the Constant-Murley score (p < 0.01) and American Shoulder and Elbow Surgeons Shoulder Score (ASES) (p < 0.001) after five years, favoring surgical treatment. However, these authors48 also showed that there was no significant difference in SF-36 scores (p = 0.38) between the conservative and surgical groups or in the Constant-Murley score (p = 0.02) between the cohort who opted for the initial repair at time zero and the cohort who attempted conservative therapy and then transitioned to surgical repair. This suggests that non-operative exercise therapy can be considered as first line treatment for 12 weeks without detriment to clinical outcomes. This is further corroborated by one study108 that found no statistically significant difference (p = 0.28) in patient satisfaction rates between conservative and surgically managed cohorts. Outcomes that did favor surgical repair cohorts were the Constant-Murley activity of daily living (ADL) subscore (p < 0.0001) at 12 and 24 months post-intervention108and the Disability visual analog scale (VAS) (p = 0.002) at 12 months.49
In summary, functional outcomes were reported for 45 non-operatively treated cohorts that included 1610 shoulders. Of these, 38 (84%) cohorts, consisting of 1366 (85%) shoulders that reported improvements in function versus seven (16%) cohorts consisting of 217 (15%) shoulders that did not improve or not to a ‘satisfactory’ level. When statistical differences were not calculated or reported, and when an accepted value was available for the respective outcome, the MCID was used to 11 (25%) cohorts consisting of 267 (17%) shoulders, of which eight (18%) cohorts including 142 (53%) shoulders met or surpassed MCID. Statistical differences were examined in 17 (38%) cohorts consisting of 749 (47%) shoulders all of which improved statistically (p < 0.05) and 13 (29%) cohorts, 650 (87%) shoulders, who also achieved clinically significant improvements for function.
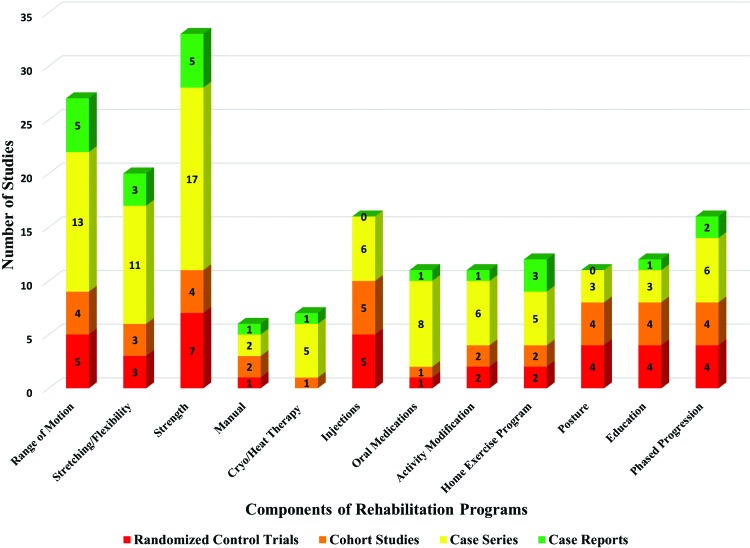
Components of programs
The components of the exercise and rehabilitation programs had considerable variation across the studies. However, consistent components of the programs included strengthening (97% of studies), ROM (79% of studies), stretching/flexibility (61% of studies), activity modification/education (57%), home exercise routine (explicitly stated in 32% of studies), manual therapy (18% of studies), heat or cold modalities (21% of studies), and postural interventions (24% of studies). Additional medical interventions that were used to supplement exercise therapy including medications (explicitly stated in 35% of studies) and/or corticosteroid injections (39% of studies) were also considered. Other components of the conservative management programs included scapula-thoracic specific interventions and reintegration into patient-specific activities. Phased progressions were specifically stated and described in 35% of studies and 57% of randomized control trials. (See Appendix H for details of the rehab programs for each included study. Refer to Figure 5 for a graphical representation of the prevalence of the most common rehab program components.)
Figure 5.
A graphical representation of prevalence of the different rehabilitation program components in the included studies. The different colors represent the different types of study designs as described in the legend below the graph.
Scope of prior systematic reviews
Two of the three prior systematic reviews identified by these search results were specific to non-operative rotator cuff tears. Ainsworth et al 200732 patient population nearly synonymous with the subjects and shoulders identified in this study, as this was the study that was being updated by this current review. The current review excluded two non-English studies120,121 that were included within Ainsworth et al 200732 that were excluded from the current review due to inability to accurately translate these texts. However, the current review included an additional 23 studies published after 2007. Ryosa et al45 studies were all included in this study, but the inclusion criteria were specific to randomized control trials and the purpose of the study was to compare non-operative therapy to surgical repair. Similarly, Sieda et al64 had a similar purpose as Ryosa et al45 with the exception of including controlled and uncontrolled studies, as well as investigating not only comparing nonoperative to operative RC repair, but also the effectiveness of different types of repairs.
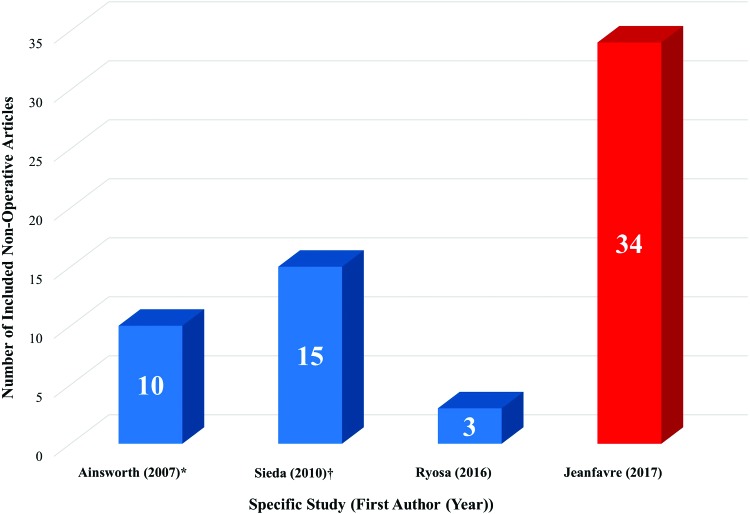
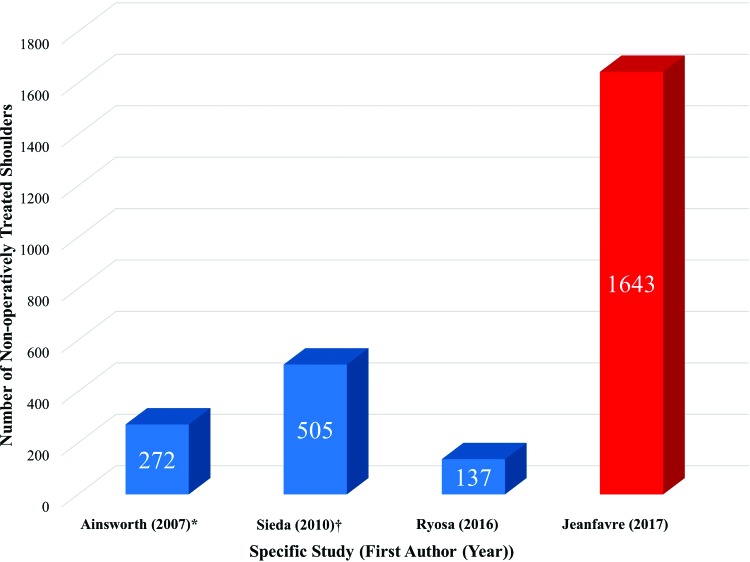
The number of studies included in the identified reviews varied from 345 to 13764 with the number of total subjects ranging from 25245 to 8,515.64 Though Sieda et al64 was the most comprehensive, including 137 studies and 8,515 subjects, of these only three controlled and seven uncontrolled studies were isolated to non-operative treatment and five studies compared non-operative management to surgical management. These 15 studies combined accounted for 178 non-operatively managed shoulders from controlled studies and 327 non-operatively treated shoulders from uncontrolled studies. A total of 505 subjects (37.5% the number of conservatively managed shoulders included in the current review). The other two reviews, Ainsworth et al (2007)32 and Ryosa et al45, included 10 studies (with 272 subjects) and three studies (with 252 subjects), respectively. Summaries of these reviews are provided in Appendix B and Appendix C. A graphical representation of the number of studies focusing on non-operative treatment for each review can be seen in Figure 6. While included non-operatively treated shoulders included in each review can be seen in Figure 7.
Figure 6.
The graph summarizes the number of non-operative shoulder treatment studies in each of the prior reviews and the current review. *, the review being updated; †, 137 total included articles but only 15 of these were specific to non-operative interventions.
Figure 7.
The graph summarizes the aggregate number of non-operative treated shoulders included in each of the prior reviews and the current review. *, the review being updated; †, 137 total included articles but only 15 of these were specific to non-operative interventions.
Conclusions of prior systematic reviews
All three prior systematic reviews demonstrated difficulty drawing conclusions regarding the effectiveness of non-operatively managed FTT stating that there is either “some” or “limited” and “inconclusive” evidence to support non-operative or exercise therapy alone or in comparison to that of surgical interventions. However, the most recent of these reviews was able to make an explicit recommendation that “a conservative approach is advocated as the initial treatment modality” in FTT.45 (See Appendix C for a summary of the conclusions of prior reviews).
GRADE of Recommendations
According to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group criteria69 exercise therapy, with and without supplementary physical therapy and non-surgical medical interventions, demonstrates Grade B – Moderate strength of recommendation. This is based on the multiple randomized control trials and the supplementary level III, level IV, and case report studies with consistent findings that demonstrate that non-operative interventions have on pain, ROM, strength, and function in FTT.
DISCUSSION
This systematic review identified both randomized control trials (nine studies47-49,52,107-111) and observation studies (four prospective cohort studies,40,104-106 two retrospective cohort studies,102,103 16 case series,1,87-101 and five case reports82-86) that, on the whole, demonstrate the consistent finding that exercise therapy is an effective treatment for the reduction of pain, improvement of ROM, strength, and most dramatically, function. Due to the lack of blinding, the highest level of randomized control trials included were level II studies. This, in combination with a predominant number of level III and IV studies reinforcing the findings of the randomized controls, provided the Grade B – Moderate strength for recommendation for using exercise therapy in the treatment of FTT.
One of the primary goals of this systematic review was to update the last systematic review by Ainsworth et al32 that included both randomized control trials and observational studies, specific to exercise therapy of FTT which is over 10 years old. According to previously established criteria for updating systematic reviews,67,68 it was apparent from those findings that an update was indicated by the amount of new evidence that has become available since its publication and with the profoundly increasing prevalence of RCT's in the setting of an aging population. As is convention, the inclusion and exclusion criteria, search strategy, and the analysis of quality assessment were all kept constant from the original review. No historic date restrictions were set on the search strategy for the current study as means to ensure that no studies were previously overlooked in the original search. Thus, the 10 observational studies84,85,87,88,90-92,97,98,103 included in the original review were also included in the current study. One study, a randomized trial by Shibata et al,109 that was published prior to Ainsworth et al (2007)32 was included in this review, as it met all pre-established criteria, but was not included in the original review. Despite an overlap in included studies, the results of the current review, were considerably different from those presented by Ainsworth et al (2007)32 in the total number of studies identified, the level of evidence identified, and the ability to provide a decisive GRADE of recommendation. This speaks to not only to the expansion of the amount of research being published on the conservative management of RCT but also to the overall improvement in the methodology of the more recent literature. This is further demonstrated by the improvement in quality of more recent studies. The average quality assessment score of observational studies since 2007 is 6.4 out of possible 8, compared an average score of 5.3 in the studies included in the initial review.
The second purpose of this review was to establish the effectiveness of the exercise therapy with and without additional physical therapy or medical management interventions. The primary outcomes that were looked at to determine this was pain, ROM, strength, and functional outcome measures. These metrics were chosen (1) because they were consistently reported across a large percentage of the included studies and (2) these have previously been established in similar reviews of shoulder rehabilitation.63 A significant percentage of conservatively treated shoulders demonstrated improvement in each of the outcomes. Of the non-operatively treated shoulders for which it was reported: pain was reduced in 86% of shoulders, ROM improved in 83% of shoulders, strength improved in 89% of shoulders, and functional reported outcomes improved in 85% of non-operatively treated shoulders. (Figures 3 and 4)
However, it is important to note that in several of these studies there was a cohort of patients who were unsatisfied with conservative treatment and opted for surgical intervention.1,40,48,49,103,106,108 This, in combination with the knowledge that performing a repair secondary to a trial of conservative therapy does not statistically change the patients’ outcomes, suggest that non-operative conservative therapy as a first line intervention for FTT should be considered.40,47,48 This is consistent with the conclusion a recent systematic review and meta-analysis by Ryosa et al,45 that directly compared non-operative treatment to surgery for FTT. Moreover, if individuals do not opt for surgical management within 12 weeks, they are unlikely to do so within the following two years.40,106
The average follow-up time frame for all of the outcomes ranged from 2.3 to 3.0 years. This is considered an adequate follow-up time period for RC literature as the longest follow-up for any randomized control trial included was five years. However, compared to the length of time that FTT can be symptomatic (conceivably decades, depending on a person's age of onset), two to three years is a relatively short time frame.
When considering long-term management of RC pathology, it is also important to acknowledge the risk of tear progression and fatty infiltration that can occur in the presence of FTT. Though a couple of studies found similar progression rates, with 23-52% experiencing > 5 mm tear size over two to three years with ‘non-operative’ treatment,122-124 fatty infiltrate and tear progression has not been shown to be significantly different between intact RC repairs, retorn rotator cuff repairs, and individuals who received non-operative treatment.49,108 This is also in contrast to PTT, in which only ∼10% will progress > 5 mm within the same time frame. It is also promising that a small percentage (8-18%) of FTT can show a radiological decrease in size with non-operative treatment.95,122 The proposed mechanism of how the healing occurs is referred to as ‘mechanotherapy’, in which cells respond to mechanical stimuli and resulting in a cellular response to promote tendon healing.9,125 Though serial imaging, either by ultrasound or MRI, can be used to monitor tear progression and fatty infiltration, tear progression can also be monitored through progression in pain intensity, as this has been correlated with tear size progression.9,95,122 Moosmayer et al (2017)95 noted that not all tear progressions have clinical implications and that ‘satisfied’ and ‘unsatisfied’ non-operative treated cohorts can be dichotomized by tears that progress by <20 mm and those that progress ≥20 mm, respectfully.
Another factor that can influence the decision for surgery vs non-operative management is the patient's respective demographic. The characteristics of the subjects included in this in this review, with an average age of 64 years and the majority of FTT being atraumatic and chronic degenerative tears, are consistent with the patient population and tear characteristics documented in the literature.126 The patient demographic, older age, degenerative tissue, and chronicity of tears have all been shown to negatively influence the success rates of surgically repaired FTT,127-130 providing further evidence for the consideration for initial non-operative, exercise therapy in this patient population. The consensus is that primary surgical repair is the more active and younger patient populations.126,129-132
Decisions for FTT management can be made by, not only by stratifying a patient's prognosis of surgical intervention but also by stratifying their prognosis to respond to non-operative treatment. Some variables that have been considered in identifying patients who are more likely to respond to surgical interventions include: age, activity level, history of trauma, severity of fatty atrophy, severity of pre-operative symptoms, and location or size of the tear.58,64,95,131,133-137 Individuals less likely to respond to non-operative treatment have lower baseline abduction ROM, abduction strength, younger age, lower BMI, lower RC-QoL, and lower WORC index (p > 0.05).92,106,131 One included study1 proposed a ‘Predictive Score’ that considered 17 baselines variables and a cut off of score 13 out of 21 (higher scores indicative of ‘unsatisfied’ outcomes with non-operative treatment and opting for surgical treatment within one year) to determine which patients are most likely to respond to conservative therapy.
Some variables in the literature have been shown to be inconsistent predictive factors of surgical or non-operative treatment include the extent of rotator cuff damage or degeneration on imaging studies.46,138,139 This aligns with the peculiar phenomenon RC injury being found in a large number of asymptomatic patients.139 Though several authors have been unable to fully explain the discrepancy between symptoms, functional limitations, and extent of RC pathology,3,19,40,106 a proposed hypothesis is that once a tear progresses to involve the posterior cuff musculature, there is an imbalance between the forces of the infraspinatus and the subscapularis, leading to a disruption of normal shoulder kinematics, GHJ stability, and loss of fulcrum for concentric rotation of the humeral head leading to a higher propensity of dysfunction and thus, disability and symptoms.9,140
Patient Demographics
The patient demographics of the subjects and shoulders within this review were consistent with the epidemiology of the RCTs. It is known that the incidence and prevalence of RCTs begin to increase in the sixth to seventh decade of life, which is consistent with the mean age of 64.2 years of age seen in the included subjects of this review.2,3 In regards to gender, there was nearly an even split between males (54%) and women (46%). Though epidemiology studies have found gender not to be a significant risk factor for RCT,18,19 there are large review reviews of RCT that demonstrate a slightly higher incidence in males than females.141
Considerations of the specific tendons of the RC involve is also important. It has been well documented that the supraspinatus tendon is the most commonly torn RC tendon.58,142-145 Proposed rationale for the supraspinatus being predisposed to injury, compared to the other RC tendons are said to be both intrinsic (age, genetics, comorbidities, vascularity of the tendon, anatomical shape of the acromion, etc.) and extrinsic (bursal and articular sided strain, frequency of shoulder use, and prior injury).146-149 A ‘degeneration microtrauma’ mechanism and cascade has been proposed by previous authors in which insufficient healing times between microtraumas to the tendon in combination with increased demand on remaining fibers, and inflammatory mediators and oxidative stress induces tenocyte apoptosis.9,150-153 This is synonymous with the ‘continuum model of tendon pathology’ which describes how the elevation of inflammatory cytokines in response to the cyclic loading of tenocytes can lead to ‘an alteration in tendon synthesis and degeneration’ and eventually a ‘reactive-on-degenerative tendinopathy’.154 These mechanisms are consistent with the supraspinatus tendon having been shown to have reduced healing capacity due to a control tendon, because of the increased degree of tenocyte apoptosis and the reduced production of type I collagen.153 Moreover, there have been additional in-vivo and cadaver studies that suggest there is a ‘critical zone’ within the supraspinatus tendon which can increase with age, impingement, and larger RC tears.112,155 Second to supraspinatus is the prevalence of infraspinatus tearing. This is not surprising given that the tendons of these muscles blend upon their insertion,156,157 that the most common location for tearing is at the junction of the two tendons,114 and that injury of the supraspinatus increases the strain and demand of the infraspinatus.149 These findings are consistent with the supraspinatus and infraspinatus having the highest prevalence in the included shoulders of this review.
However, as several of the included studies either did not report the specific tendon involved or listed the FTT as “massive”, there is a high risk of the prevalence of subscapularis and teres minor involvement being under reported. Recent studies have reported subscapularis involvement in RC tears as high as 31.5%, but only 6% in shoulders in which surgical repair was indicated.158 This is twice that of the 3% prevalence reported in this study. Similarly, teres minor tears have suggested to be rare in isolation159 and tend to be involved in “extensive FTT.”160 Despite 37% of tears being massive and/or involving > 1 tendon, teres minor involvement was only reported in three (<1%) of shoulders. One potential explanation for this, as mentioned above, is the most common location of FTT is at the junction of infraspinatus and supraspinatus and that teres minor is commonly preserved in the presence of massive FTT with degenerative RC changes and atrophy because the increased physical demand on the muscle can lead to hypertrophy of teres minor, especially in posterior-superior tears.160-162 This information is critical to acknowledge when devising a rehabilitation program that will be successful and strategically overcoming the ROM, strength, and functional deficits that exist in the presence of FTTs.
Included RCTs in this review were predominantly chronic and atraumatic in nature of onset. This is also consistent with the literature, As the literature suggests that traumatic and, therefore, more often acute RCTs are more likely to be considered for surgical management,45,163 the distributions of symptom duration and atraumatic onset should be viewed with caution. This is due to the risk of bias in the inclusion and selection criteria of the included studies being more likely to attract subjects who were not considered for a primary RC repair.
Comparison to Prior Reviews
There were three prior systematic reviews identified that had a similar scope, patient population, interventions, outcomes, and search strategies to the current review.32,45,64 A summary of the scope of these reviews is summarized in Appendix B and Appendix C.
It is apparent that an update of Ainsworth et al (2007)32 was warranted as another 25 pertinent publications regarding non-operative management of FTT have been added to the literature since 2007. Though Sieda et al64 and Ryosa et al45 are more recent, neither study was specific to non-operative management of FTT, as is apparent by the discrepancy in the number of included studies and the aggregate number of subjects. To the knowledge of the authors, the current review has three times the number of relevant studies and close to four times the number of shoulders compared to any prior review specific to the non-operative treatment of FTT. (Figures 6 and 7) However, the authors of the current review were unable to perform a meta-analysis which has been conducted by prior reviews,45,64 thus, the level of current evidence was summarized using a GRADE of Recommendation. This provided a distinct conclusion, in comparison to the language used in the conclusions prior reviews (i.e. ‘some evidence exists’,32 ‘inconclusive’,64 or ‘limited evidence’45).
It is also important to note the quality of the identified reviews. Based on The AMSTAR guidelines73,74 Sieda et al64 and Ryosa et al45 both demonstrated ‘Good’ quality, 10/11 and 9/11, respectively. Ainsworth et al (2007)32 on the other hand only demonstrated ‘Fair’ quality, 5/11. The quality of methodology assessment of the current review was determined to be ‘Good’ (9/11) as determined by the AMSTAR guidelines (Table 6).
A separate, but seminal, review and position statement that needs be discussed in light of the current findings is the American Academy of Orthopedic Surgeons (AAOS) 2012 Clinical Practice guidelines for “Optimizing the Management of Rotator Cuff Problems” states that there was ‘inconclusive evidence’ to provide a recommendation for exercise as a treatment for RCT.164 It is clear from the current results that since 2012 there is sufficient evidence to not only support the use of exercise therapy in the treatment of FTT but that this is effective in managing pain, improving range of motion, strength, and overall function. Simultaneously, the AAOS 2012 practice guidelines stated that surgery should not be performed for asymptomatic RCTs, and provided a limited recommendation on RCT repair as an option for patients with chronic, symptomatic FTT. Ironically this described demographic fits the majority of the 2,010 shoulders included in this review, demonstrating that given the aforementioned results, it would appear that conservative, non-operative treatment should be considered a viable alternative to surgical intervention.9 With the known risk of muscle wasting, fatty infiltration, further decline in disability and the potential for continual tear progression natural history progression, pharmacological management, activity modification, professional advice, and/or strategic neglect is not the best option for this patient demographic; exercise therapy through mechanotherapy mechanisms.9,125
Components of Exercise Therapy Rehabilitation of Full-Thickness Tears
The common aspects in the programs of the included studies were identified as: (1) range of motion, (2) flexibility/stretching, (3) strength/resistance exercise, (4) modalities, (5) supplementary pharmaceutical interventions including injections or oral medications, (6) postural and scapulothoracic exercises, and (7) education regarding the pathophysiology of the condition, the how exercise can help and goals of conservative management. Other aspects to consider are including a home exercise program, the specific parameters of the program (frequency, intensity, volume, duration), and whether or not to ‘phase’ the program. The prevalence of each of these interventions in the included articles is provided in Figure 5.
Despite the predictable and consistent deficits that need to be addressed in the rehabilitation of the patient with a RCT, there is considerable heterogeneity in the components and exercise prescription of the included rehabilitation programs. This variability amongst the intervention programs is a confounding variable and thus, may influence differences in outcomes. This has previously been identified as a source of performance bias in a systematic review in the related pathology of shoulder impingement syndrome.63 The argument for a ‘standardized accepted, evidence-based rehabilitation protocol’ is: (1) clinicians will ‘know that patients are receiving the best available rehabilitation program’, (2) a ‘standard rehabilitation protocol’ reduces confounding variables and performance bias, (3) it will allow for pooling and comparison of data across studies and different cohorts; (4) such a protocol can also serve as a control, allowing for the study and protocol modifications. It is apparent that the necessity of a synthesized protocol exists. However, it is important to note that a synthesized protocol is designed to serve as a guide for the rehabilitation process and not intended to supersede clinical judgment and decision making that is necessary to meet the unique needs of individual patients. Phased progression of any rehab protocol should be based not only on expected tissue healing timelines but also on clinical presentation and functional capabilities of each individual patient.
Limitations
There were limitations in the current review that are important to note. First, there is ambiguity in the literature between RCT and subacromial impingement syndrome (SIS). A number of articles that were excluded from this review discussed the effectiveness of exercise specific to SIS. However, patients with Stage III SIS are described as having key finding of a mechanical disruption of the rotator cuff tendon in the form of either partial or complete cuff tears defined as by Neer et al165 and Khan et al.166 However, certain studies failed to determine and/or state the stage of SIS of the respective subjects, these citations were excluded due to the extent, or lack thereof, of mechanical damage to the rotator cuff muscle(s) of the subjects described in these studies would not have definitively fit the inclusion criteria of this review (FTT).
Similarly, there is considerable heterogeneity in the classification systems used to describe RCTs.115,116 The discrepancies in classification systems used by included studies made it difficult at times to determine the full extent of tendons described. For instance, if it was stated that ‘<50% of the supraspinatus tendon was involved’ this very well could be describing a partial thickness tear in the superior to inferior direction or it could be interpreted as a FTT in the superior to inferior direction that only involved <50% of the tendon in the anterior to posterior direction. Though The International Society of Arthroscopy, Knee Surgery & Orthopedic Sports Medicine (ISAKOS) published a positional statement defining a synthesized classification system in 2013,116 all of the studies prior to this date (and some after) were using different classifications and thus, providing a risk of miss interpreting the full extent of the rotator cuff pathology. Note, in such cases when a study met all other inclusion criteria and there was ambiguity in the extent of the tear, the corresponding authors were contacted for clarification. This occurred in only three studies.1,86,93
This review was only specific to studies published in the English language. Sieda et al64 extended their search to English, French, and German studies and were able to identify four additional studies120,121,167,168 that otherwise would have been included in this review, but due to the pre-determined English language inclusion criteria and the lack of accessible (and accurate) translation resources, these studies were not included. As mentioned in the results section, there was another outlying study81 due to all available resources being exhausted and not being able to access a full text. Correspondence with the author(s) was attempted but no return response was received.
Another critique of the inclusion and exclusion criteria is the inclusion of case reports, observational studies, and randomized control trials. The lack of randomization and heterogeneity of the studies prevented a pooled analysis. Furthermore, the inclusion of case reports was not necessary as they made of <1% of the aggregate number of shoulders and commonly provide the most clinical utility in ‘recognition patterns’ for rare clinical conditions and reviews on certain topics related to the case.169 FTT are far from a ‘rare’ clinical condition and the topics (i.e. non-operative management) are certainly covered by other observational and randomized studies that were included. The rationale for including both observational and experimental studies and for inclusion criteria was due to the fact that the current review was an update of a prior review.32 As such, it is standard practice to keep inclusion and exclusion criteria as constant.
A final critique, outside of the control of the author, was the fact that there was a lack of reporting of statistical analysis in a large portion of the studies regardless of the outcome in question. When possible the MCID was applied to the functional outcome measure in an attempt to demonstrate a meaningful change in the absence of statistical significance. The lack of reporting of statistically significant differences limits impact and interpretation of the results. (Figure 4). Additionally, the lack of level I and II experimental design studies prevented assignment of a a GRADE A Recommendation for the use of exercise therapy in the treatment of FTT.
Despite these limitations, this is currently the most comprehensive search that has been conducted in regards to conservative management of FTT. Furthermore, the results have been used to substantiate and provide suggestions to the recently proposed ‘Edwards Protocol’ which can be used to guide clinical practice and provide a starting point for future high-quality randomized control trials.
CONCLUSION
The results of the current systematic review of the current literature provided few high-quality randomized control trials and a predominant number of observational studies, indicating GRADE B Recommendation (moderate strength) to support the use of ET in the management of FTT. There is substantial evidence to support the use of exercise therapy as first line management, especially in individuals >60 years of age with chronic, degenerative FTT. Future efforts should focus on coming to a consensus regarding exercises and interventions that are most effective in the conservative treatment of individuals with full thickness rotator cuff tears.
External Links
1. Video Presentation Summarizing Review and Results
Appendix A.
Search strategies
| PubMed Search (n = 711) | |||
|---|---|---|---|
| (“Physical Therapy Modalities”[MH] OR “Physical Therapy”[TIAB] OR Rehabilitation[MH] OR Rehabilitation[TIAB] OR Physiotherapy[TIAB] OR “Conservative”[TIAB] OR “Non-operative”[TIAB] OR “Non-surgical”[TIAB]) AND ((“Rotator Cuff”[MH] OR “Shoulder”[MH] OR “rotator”[TI] OR shoulder*) AND (ruptur*[TI] OR tear*[TI] OR injur*[TI])) |
| CINHAL (n = 301) | |||
|---|---|---|---|
| Search ID# | Search Term | Search Option | Results |
| S5 | (S2 OR S3) AND (S1 AND S4) |
Limiters – English Language; Peer Reviewed Search modes – Find all my search items |
301 |
| S4 | S2 OR S3 | Search modes – Find all my search items | 114,206 |
| S3 | (TI “non-surgical”) OR (AB “non-sugrical) OR (TI “Non-operative”) OR (AB “Non-operative) OR (AB Conservative) | Search modes – Find all my search items | 7,601 |
| S2 | (MM “Physical therapy+”) OR (MM “Rehabilization+) OR (MM “Therapeutic Exercise+”) | Search modes – Find all my search items | 107,091 |
| S1 | *MM “Rotator Cuff”) OR “Rotator Cuff” OR (MM “Rotator Cuff Injuries”) | Search modes – Find all my search items | 2,552 |
| Cochrane Library (n = 314) | ||
|---|---|---|
| ID | Search | Hits |
| #1 | MeSH descriptor: [Physical Therapy Modalities] explode all trees | 19634 |
| #2 | MeSH descriptor: [Rehabilitation] explode all trees | 19416 |
| #3 | MeSH descriptor: [Exercise] explode all trees | 17602 |
| #4 | MeSH descriptor: [Therapeutics] explode all trees | 274319 |
| #5 | “non-surgical” or “non-surgical” or “non-surgically” or “conservative” or “non-operative”:ti,ab,kw (Word variations have been searched) | 6216 |
| #6 | #1 or #2 or #3 or #4 or #5 | 288525 |
| #7 | MeSH descriptor: [Rotator Cuff] explode all trees | 371 |
| #8 | MeSH descriptor: [Shoulder] explode all trees | 420 |
| #9 | “rotator” or “shoulder”:ti,ab,kw (Word variations have been searched) | 5597 |
| #10 | injury or injure or tear or torn or rupture or ruptured:ti,ab,kw (Word variations have been searched) | 35767 |
| #11 | (#7 or #8 or #9) and (#10) | 928 |
| #12 | #6 and #11 | 314 |
| Web of Science (n = 369) | ||
|---|---|---|
| SearchID | Results | Search Strategy |
| #7 | 369 | (#6 AND #3) AND
LANGUAGE: (English) AND
DOCUMEN TYPES: (Article) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| #6 | 4,499 | #4 AND #5 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| #5 | 314,854 | (TI=(“Rotator cuff” OR Shoulder OR Shoulder*)) AND
LANGUAGE: (English) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| #4 | 61,903 | (TS=(“rotator cuff” OR “shoulder OR shoulder*) AND
LANGUAGE: (English) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| #3 | 2,189,473 | #2 OR #1 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| #2 | 709,765 | (TI=(conservative OR “non-operative” OR “non-surgical” OR rehabilitation OR therap*)) AND
LANGUAGE: (English) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| #1 | 2,127,290 | (TS=(“Physical Therapy” OR Physiotherapy OR Rehab OR Therp*)) AND
LANGUAGE: (English) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SS, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
Appendix B.
Summary table of scope of reviews
| Author (year) | Participants | Intervention | Comparison | Outcome | Search strategy |
Number of studies (n = ) |
Number of Shoulders (n = ) |
|---|---|---|---|---|---|---|---|
| Ainsworth (2007)32 | “Skeletally mature human adults who had a clinical diagnosis of full thickness, or massive, or inoperable rotator cuff tears.” |
“at least one treatment group received exercise therapy for the treatment of this condition” |
NR | “outcome measures” |
-MEDLINE (1950 – 7.31.06), AMED (1985-7.31.06), PEDro (-7.31.06), EMBASE (1974-7.31.06), CINAHL (1982-7.31.06 -Search terms provided -English only |
-Identified: 111 -Included: 10 observational |
-Total: 272 -M:116; F: 156 |
| Sieda (2010)81 | “Adults with confirmed rotator cuff tears” |
“Any nonoperative or operative treatment for postoperative rehabilitation” |
“Compare the benefits and harms of nonoperative and operative interventions” |
“clinically important outcomes” |
-MEDLIN < EMBASE, Evidence-Based Medicine Reviews, Cochrane Library, AMED, CINAHL, SPORTDiscus with Full Tex, Academic Search Elite, Health Source, Science citation Index Expanded (via Web of Science), Scopus, BIOSIS previews, CRISP, Current Controlled Trials, ClinicalTrials.gov, Netherlands Trial Register -Timeline: January 1990 – September 2009 -Search strategy provided -Operative studies: English only -Non-operative studies: English, German, French |
-Identified: 5677 Included: 137 66 controlled 71 uncontrolled |
Total: 8515 Controlled studies: -Operative: 3697 -Postoperative: 544 -Non-op: 178 -Op vs non-op: 243 Uncontrolled studies: -Operative: 3408 -Postoperative: 118 -Non-op: 327 |
| Ryosa (2016)45 | “Adults with rotator cuff tear” |
“Surgical repair of tendon tear” |
“Placebo, sham or other conservative treatment” |
“Change in pain, functioning level, quality of life and mobility of the shoulder” |
-Cochrane control trialed Registry (CENTRAL), MEDLINE, EMBASE, CINAHL, Web of science and physiotherapy evidence (PEDro) database -Timeline: Not specified – June 2015 -Search strategy provided -Randomized controlled trials (RCTs) -English only |
-Identified: 319 -Included: 3 RCTs |
Total: 252
-Cases: 123 -Controls: 129 -Non-op: 137 |
Non-op, nonoperative; NR, not reported; Op, operative;
Appendix C.
Results and conclusions of reviews
| Author (year) | Included studies | Results | Conclusion(s) |
|---|---|---|---|
| Ainsworth (2007)32 | -RCTs: 0 -Uncontrolled: 10 Case series: 8 Case studies: 2 |
-“Due to the heterogeneity of outcome measures used, it was not possible to combine results.” -“All studies improvement and outcome scores were reported.” |
-“Some evidence exists to support the use of exercises in the management of full thickness rotator cuff tears” |
| Sieda (2010)81 | -Included: 137 66 controlled 71 uncontrolled |
-Non-operative interventions:“ The strength of evidence was too low to make conclusions for any of the nonoperative interventions.” -Operative vs non-operative interventions: “The evidence was too limited to make conclusions regarding comparative effectiveness.” -Complications: “Because of low event rates, the benefits of receiving treatment for rotator cuff tears seems to outweigh the risks of associated harms.” -Prognostic factors: Older age, increased tear size, and greater preoperative symptoms were associated with recurrent tears |
-“Evidence on the operative effectiveness and harms a various operative and nonoperative treatments for rotator cuff tears is limited and inconclusive.” |
| Ryosa (2016)45 | -RCTs: 3 | -Constant score: 1 yr follow-up Effect size: 5.6 (95% CI; -0.41 to 11.62) favouring surgery (P > 0.05, NS) -Pain VAS: 1 yr follow-up 10 cm scale: -0.93 (95% CI -1.65 to -0.21) favouring surgery (P = 0.012; but below MCID) |
-“There is limited evidence that surgery is not more effective in treating rotator cuff tear then conservative treatment alone.” -“Conservative approaches abdicated as the initial treatment modality.” |
CI, confidence interval; Constant score; Constant-murley shoulder outcome score; MCID, minimal clinical important difference; NR, not reported; NS, not statistically significant; Pain VAS, pain visual analog scale; RCTs, randomized control trials; yr, year
Appendix D.
Outcomes for Pain
| First Author (Year) | Follow-up Period | Pain | Treatment groups (n = ) | Intragroup difference | Statistically significant (*clinical significance) |
Between group difference | Statistically significant (*clinical significance) |
|---|---|---|---|---|---|---|---|
| Itoi (1992)109 | 3.4 yr (1 – 9 yr) | Wolfgang criteria pain (0-4) | G0: All patients (62) G1: Satisfied (15) G2: Unsatisfied (8) |
(Pre→post) Motion pain (percent cohort): G0: 82%→45% Night pain (percent cohort): G0: NP: 55%→23% Wolfgang pain (points): ** G0: 2.0→ 3.0 G1: 2.2→3.3 G2: 2.4→2.1 |
(Post) Wolfgang pain: G0: P < 0.001* G1: P < 0.01* G2: P > 0.5 |
NR | NA |
| Bokor (1993)105 | 7.6 yr (3.7 – 12 yr) |
-ASES pain scale | G1: Non-surgical (53) | (Pre→post) ASES (n = ) None: 0→22 Slight: 2→17 Mild: 7→8 Moderate: 20→4 Severe: 24→2 |
NR | NA | NA |
| Hawkins (1995)108 | 3.8 yr | -Constant-murley pain score -‘Sleep loss due to NP’ |
G1: Non-surgical (19) G2: Not satisfied w/ non-surgical (14) |
(Pre→post) Constant-murley (score): G1: 9.3→10.9 G2: 7.3→10.3 Sleep loss (percent cohort): G1: 42% G2: 79% |
NR | (Post) Sleep loss (percent cohort): G1: 42% G2: 79% |
(Post) p = 0.01128* |
| Wirth (1997)114 | >/= 2 yr | ASES pain scale | G1: Exercise therapy (60) | NR | NR | NA | NA |
| Palmer (1998)101 | 2 yr | NR | Aquatic Therapy (1) | NR | NR | NR | NR |
| Yamada (2000)115 | 4 yr (12 mo – 19 yr) | -JOA pain score | G1: Non-surgical (14) G2: Surgery (26) |
(Post) (Percent improvement); G1: 57.7% G2: 70.9% |
(Post) G1: p=0.0012* G2: p<0.001* |
NR | NR |
| Goldberg (2001)107 | 6 mo Intervals 2.5 yr | NR | G1: Non-surgical (46) | NR | NR | NR | NR |
| Shibata (2001)126 | 24 wk | UCLA pain | G1: 25 mg sodium Hyaluronate & 3 mL 1% lidocaine (38) G2: 2mg Dexamethasone & 3 mL 1% lidocaine (40) |
(Pre→post) Pain score: G1: 2.37→ 5.31 G2: 2.5→5.14 |
NR | NR | NR |
| Vad (2002)120 | 3.1 yr (Range: 2-7 yr) |
-Shoulder Rating Questionnaire | G1a: PT + meds (28) G1b: PT + meds + CS (12) G2: Failed G1a/b arthroscopy (32) G3: Primary surgery RCT repair (36) |
(Pre→post) G1:20.8→30.7 G2: 20.7→39.5 G3: 16.3→40.5 |
(Post) G1: Pp<0.05* G2: p < 0.05* G3: p < 0.05* |
(Post) G1b greater ↓pain vs G1a (values NR) |
(Post) G1a vs G1b (p < 0.05) |
| Piccoli (2004)102 | 7 wk | -Pain VAS | Single case | (Pre→7 wk) 10/10 → 3/10 |
NA | NA | NA |
| Ainsworth (2006)104 | Avg: 10.8 mo (Range: 2-36 mo) | -SF36 pain score | G1: Non-surgical (10) (Torbay rehab program) |
(Post) (improvement) G1: 22 points |
NR | NR | NR |
| Levy (2007)116 | 9 mo | -Constant-murley pain score | G1: Non-surgical (17) | (Pre→≥9 mo) Constant-murley (score (range)): G1: 6 (0-9) → 12 (7-15) |
NR | NR | NR |
| Lunn (2007)119 | 50 mo | -Constant-murley pain score | G1: Nonoperative (14) G2: Open repair (5) |
(Pre→post) Constant-murley (score): G1: 4.9→9.5 G2: 5.1→9.3 |
NR | NR | NR |
| Ainsworth (2009)127 | 12 mo | SF-36 pain | G1: PT + Exercise (30) G2: Control (Placebo) (no exercise) (30) |
(3 mo→6 mo→12 mo) SF-36 pain (score change from baseline) G1: + 4.26→+3.65→+1.56 G2: (-)3.5→+4.58→+4.42 |
NR | (3 mo→6 mo→12 mo) SF-36 pain (score change from baseline) G1: + 4.26→+3.65→+1.56 G2: (-)3.5→+4.58→+4.42 |
(3 mo, 6 mo, 12 mo) SF-36 pain (score change from baseline) G1 vs G2: P > 0.05 (NS) -All time points |
| Baydar (2008)118 | 6 mo, 1 yr, 3 yr (Pt. report) | -ASES pain -SF-36 bodily pain |
G1: Non-surgical (20) | (Pre→ 6 mo) ASES pain (score): G1: 20.15→ 40.0 SF-36 bodily pain (score) G1: 36.1 → 73.6 |
(6 mo) ASES: P < 0.01* SF-36: P < 0.001* |
NA | NA |
| Moosmayer (2010/2014)47,48 ‡ |
6 mo, 1 yr, 2 yr, 5 yr |
-ASES pain scale | G1: Surgical (52) G2: PT (51) †G3: G2→G1 (9; 18%) †G4: PT only (39) |
(Pre→6 mo→12 mo→5 yr) ASES (cm): G1: 5.6→1.1→0.5→0.6 G2: 5.3→2.6→2.1 →1.6 G3: 6.3 G4: 5.0 |
NR | (Pre) G3: 6.3 G4: 5.0 (1 yr) G1: 0.5 cm G2: 2.1 cm (5 yr) G1: 1.6 cm G2: 0.6 cm |
(Pre) G3 vs G4: p<0.05 (1 yr) G1 vs G2: p < 0.0005 (5 yr) G1 vs G2: p < 0.05 |
| Tanaka (2010)113 | G1: 2.4 yr G2: 2.2 yr | -Time 0: Night pain | G1: Non-surgical (subjects: 62; shoulders: 65) G2 Failed G1→surgery (subjects: 56; shoulders: 58) |
(Post) (Percent of cohort): G1: 67.6% G2: 70.6% |
NR | (Post) (Percent of cohort): G1: 67.6% G2: 70.6% |
(Post) P = 0.719 (NS) |
| Gialanella (2011)128 | 6 mo | -Pain VAS | G1: PT & CS (x1) (20) G2: PT & CS (x2) (20) G3: PT (control) (20) |
(Pre→1 mo→3 mo→ 6 mo) Rest pain (cm): G1: 1.8→0.5→0.6→0.8 G2: 1.9→1.0→1.1→1.5 G3: 0.6→0.9→0.6→0.7 Activity pain (cm): G1: 7.1→3.8→3.7→5.4 G2: 7.3→3.9→4.0→5.4 G3: 6.9→6.7→6.5→6.8 Night pain (cm): G1: 5.8→2.1→2.7→3.5 G2: 5.5→1.8→1.9→2.9 G3: 4.6→ 4.5→4.6→4.6 |
(1 & 3 mo) Rest pain (cm): G1: P < 0.05* Activity pain (cm): G1 & G2: p < 0.001* Night pain (cm): G1 & G2: p < 0.001* (6 mo) Activity pain (cm): G1: p < 0.01* G2: Pp<0.001* Night pain (cm): G1 & G2: P < 0.001* |
(1 & 3 mo) Activity pain (cm): G1 & G2 lower than G3 Night pain (cm): G1 & G2 lower than G3 |
(1 & 3 mo) Activity pain (cm): G1 & G2 vs G3: p < 0.001* G1 vs G2 : NS Night pain (cm): G1 & G2 vs G3: p < 0.001* G1 vs G2 : NS |
| Merolla (2011)1 | 12 mo. | Pain VAS | G0: Conservative therapy (60) G1: ‘Successful’ (33) G2: G0→ surgery (27) |
(Pre→3 mo→6 mo→12 mo) Pain (mm): G1: 8.5→3.3→4.1→4.8 G2: 8.5→6.9→7.8→7.9 |
NR | (Pre→3 mo→6 mo→12mo) Pain (mm): G1: 8.5→3.3→4.1→4.8 G2: 8.5→6.9→7.8→7.9 |
NA |
| Kijma (2012)110 | 12.9 yr | -JOAS pain scale | G1: Nonsurgical (43) | (Post) JOAS (points): 25.4 No pain (n=): 24 (56%) Needed meds (n=): 5 (12%) |
NR | NR | NR |
| Krischak (2013)124 | 2 mo | Pain VAS | G1: Standard OT (22) G2: Home exercises (16) |
(Pre→2 mo) VAS (points): G1: 5.2→3.5 G2: 5.0→3.8 |
NR | (2 mo) G1: 3.5 G2: 3.8 |
(2 mo) G1 vs G2: P = 0.678 (NS) |
| Kuhn (2013)40 | 1 yr | NR | G0: PT program‡ (422, 100%) G1: Cured (237, 62.2%) (no formal f/u scheduled) G2: Improved (continue PT) G3: No better (82, 29%) (offered surgery) |
NR | NA | NR | NA |
| Benazzo (2014)99 | 29 mo | NR | Non-surgical: (1) | NR | NA | NA | NA |
| Boorman (2014)123 | 29 mo | NR | G0: 3 mo .supervised, non-operative§ G1: “Successful”(no surgery indicated) (70; 75%) G2: “failed” (underwent surgery) (23; 25%) |
NR | NA | NA | NA |
| Güzelant (2014)117 | 66 mo (mean) | -Pain VAS | G1: “Conservative therapy” (33) |
(Pre→post) Pain VAS (cm): 8.5→3.5 |
(Post) Pain VAS: P<0.05* P = 0.0378 |
NA | NA |
| Kukkonen (2014/2015)52,125 | 24 mo | -Constant-murley pain scale -Pain VAS |
G1: PT (55) G2: Acromioplasty & PT (58) G3: RC repair, acromioplasty & PT (54) |
(Pre→6 mo→12 mo→24 mo) Constant-Murley (score):** G1: 10.3→12.1→12.1 G2: 10.8→13.4→13.6 G3: 10.2→13.4→13.8 Pain VAS (cm): G1: 2.7→1.6→1.5→1.5 G2: 2.5→0.6→1.1 →1.0 G3: 2.6→0.9→1.0→0.6 |
NR | (12 mo; 24 mo) Constant-Murley (score):** G1: 12.1; 12.1 G2: 13.4; 13.6 G3: 13.4; 13.8 (Pre→24 mo) Pain VAS change (cm): G1: -1.3 G2: -1.8 G3: -2.0 |
(12 mo) Constant-Murley: G1 vs G2/G3: P<0.05 (p = 0.0321) (24 mo) Constant-murley: G1 vs G2/G3: P<0.05 (P = 0.01) (Pre→24 mo) Pain VAS change: G1 vs G2 vs G3: P = 0.45 (NS) |
| Collin (2015)106 | 24 mo | NR | G1: “Rehab program” (45) (nonoperative) |
NR | NA | NA | NA |
| Lambers Heerspink (2015)49 | 12 mo | Pain VAS | G1: “Conservative Management” (31) G2: RC repair (25) |
(Pre→12 mo) VAS (cm): G1: 6.3→3.2 G2: 6.2→2.2 |
NA | (12 mo) Change VAS (cm): G1: 2.9 G2: 4.0 |
(12 mo) VAS: G1 vs G2: P = 0.04 |
| Baumer (2016)121 | ≥9 wk | -Pain VAS | G1: PT (25) G2: Healthy controls (25) |
(Pre→≥9 wk) VAS (cm): G1: 3.8→1.7 G2: 6.2→NR |
(≥9 mo) G1: P < 0.01* |
(≥9 wk) VAS (cm): G1: 1.7; G2: 6.2 |
(>9 wk) VAS: G1 vs G2: P < 0.01* |
| Christensen (2016)122 | ≥5 mo | -Pain VAS -EQ-5D |
G1: Non-operative(30) G2: Control (30)†† |
(Pre→≥5 mo) VAS w/ Flx movement (cm): G1: 5.0→1.0 VAS w/ Abd movement (cm): G1: 5.0→2.0 VAS w/ ER movement (cm): G1: 4.0→0.5 EQ-5D (median score): G1: 60.0→80.0 |
(≥5 mo) VAS Flx: P = 0.001* VAS Abd: P < 0.001* VAS ER: P = 0.015* EQ-5D: P < 0.001* |
NR | NA |
| Miller (2016)111 | 12 wk | NR | G1: Exercise therapy | NR | NA | NR | NA |
| Mischke (2016)100 | 13 visits (time NR) | NPRS | Conservative therapy (1) | (Pre→visit 7→ visit 13) NPRS (0-10): 7→4→1 |
-Improved by MCID | NA | NA |
| Upadhyaya (2016)103 | 10 yr | -“Hawkin's test” -“Neer's test” |
Non-operative treatment (1) | (Pre → 10 yr) Hawkin's test (pain): (+) Pain → (+) Pain Neer's test (pain): (+) Pain → (+) Pain |
NR | NA | NA |
| Moosmayer (2017)112 | 8.8 yr | -Pain VAS | G1: Non-operative (49) G1a: Tear size < 9.9 mm (33) G1b: Tear size 10-19.9 mm (8) G1c: Tear Size ≥ 20 mm (8) |
(≥ 8.8 yr) VAS (score): G1a: 1.0 G1b: 2.0 G1c: 5.5 |
NR | (≥ 8.8 yr) VAS (score): G1a & G1b: 1.0 G1c: 5.5 |
(≥ 8.8 yr) VAS (score): G1a & G1b vs G1c: P < 0.004* |
AP, activity pain; ASES, American shoulder and elbow surgeon's evaluation form; Avg, average; Constant-murley, constant murley shoulder outcome score; CS, corticoid steroid; F/U, follow up; G, group; HEP, home exercise program; JOAS, Japanese orthopedic Association score; Mo, month; NA, not applicable; NP, night pain; NPRS, numerical pain rating scale; NR, not reported; NS, not statistically significant;; PROM, passive range of motion; PT, physical therapy; RP, resting pain; SPADI, shoulder pain and disability index; VAS, visual analog scale; Wk, week; Yr, year; *, clinical significance, indicates a statistical significant difference and a ≥20% difference; †, G3 and G4 are a subset of G2; ‡, all subjects began a physical therapy program and were reevaluated at 6 and 12 weeks, at those times patient were assigned to G1, G2, or G3 based on findings; §, all subjects underwent a 3 mo supervised program of nonoperative treatment & with an evaluated by orthopedic surgeon and assigned to G1 or G2; **, values estimated to nearest tenth based off graphical representation, as no specific numerical values reported with-in study; ††, subjects in G1 served as their own controls which composed G2.
Appendix E.
Outcomes for range of motion
| First Author (Year) | Follow-up Period | Outcome Scale | Treatment groups (n = ) | Intragroup difference | Statistically significant (*clinical significance) | Between group difference | Statistically significant |
|---|---|---|---|---|---|---|---|
| Itoi (1992)109 | 3.4 yr (1 – 9 yr) | -Goniometer -Wolfgang criteria |
G0: All patients (62) G1: Satisfied (15) G2: Unsatisfied (8) |
(Post) Abduction (°): G0: 153.0 ° (+12.7 °) External rotation (°): G0: 47.1 ° (+7.1 °) Wolfgang criteria (avg. score 0-4): ** G0: 2.5→3.2 G1: 3.4→3.6 G2: 2.5→1.8 |
(Post) Abd & ER: NR Wolfgang criteria: G0: P < 0.05 G1: P < 0.05 G2: P > 0.05 (NS) |
(Pre) Abduction (°): G1: 149.0 °; G2: 108.0 ° External rotation (°): G1: 55.0 ° G2: 50.0 ° |
(Pre) Abd: G1vs G2: p<0.05 ER: G1vs G2: p>0.05 (NS) |
| Bokor (1993)105 | 7.6 yr (3.7 – 12 yr) | -Goniometry | G1: Non-surgical (53) | (Avg ROM): ‘Elevation’: 121 °→149 ° |
NR | NA | NA |
| Hawkins (1995)108 | 3.8 yr | -Constant-murley mobility score | G1: Non-surgical (19) G2: Not satisfied w/ non- surgical (14) |
(Pre→post) G1: 34.7→36.5 G2: 33.9→30.3 |
NR | (Pre→post) G1: 34.7→36.5 G2: 33.9→30.3 |
NR |
| Wirth (1997)114 | >/= 2 yr | -NR | G1: Exercise therapy (60) | NR | NR | NA | NA |
| Palmer (1998)101 | 2 yr | -Goniometer | Aquatic Therapy (1) | (Pre→12 weeks) Flex: 90 °→160 ° Abd: 45 °→134 ° ER: NR→77 ° IR: NR°→60 ° Ext: 36 °→51 ° |
NR | NA | NA |
| Yamada (2000)115 | 4 yr (12 mo – 19 yr) | JOA Score | G1: Non-surgical (14) G2: Surgery (26) |
(Percent improvement): G1: 17.9% G2: 18.1% |
(Post) G1: P = 0.0501 G2: P < 0.001 |
NR | NR |
| Goldberg (2001)107 | 6 mo Intervals 2.5 yr | NR | G1: Non-surgical (46) | NR | NR | NR | NR |
| Shibata (2001)126 | 24 wk | -Goniometer | G1: 25 mg sodium Hyaluronate & 3 mL 1% lidocaine (38) G2: 2mg Dexamethasone & 3 mL 1% lidocaine (40) |
(Pre→4 wk→24 wk) Abduction (°): G1: 122.8 °→151.6 °→147.7 ° G2: 111 ° → 143.7 °→139.6 ° External rotation (°): G1: 43.8 °→52.2 °→49.6 ° G2: 37.3 °→45.3 °→46.5 ° Internal rotation (lumbar (Lsp) or thoracic (Tsp) vertebrae): G1: Tsp: 12.3→11.3→11.8 G2: Lsp: 1.1→Tsp: 12.5→ NR |
(4 wk) Abduction: G1: p<0.01* G2: p<0.01* External rotation: G1: p<0.001 G2: p<0.05* Internal rotation: G1: NS; G2: NS (24 wk) Abduction: G1: p<0.05* G2: p<0.05* External rotation: G1: p<0.05 G2: p<0.05* Internal rotation: G1: NS; G2: NS |
NR | NR |
| Vad (2002)120 | 3.1 yr (Range: 2-7 yr) |
Goniometer | G1a: PT + meds (28) G1b: PT + meds + CS (12) G2: Failed G1a/b arthroscopy (32) G3: Primary surgery RCT repair (36) |
(Pre→post) Abduction: G1: 68 °→108 ° (6.8 mo) G2: 74 °→110 ° (3.2 mo) G3: 72 °→116 ° (6.8 mo) |
(Post) G1: p < 0.05* G2: p < 0.05* G3: p < 0.05* |
(Post) G1b took less time (5.3 mo) than G1a (time NR) to reach maximum ADB ROM. |
(Post) G1b vs G1a: p < 0.05 |
| Piccoli (2004)102 | 7 wk | -Goniometer | Single case | (Pre→7 wk) Flexion: 90 °→150 ° Extension: 22 °→56 ° Abduction: 80 °→139 ° Internal rotation: 30 °→68 ° External rotation: 45 °→89 ° |
NA | NA | NA |
| Ainsworth (2006)104 | Avg: 10.8 mo (Range: 2-36 mo) | NR | G1: Non-surgical (10) (Torbay rehab program) |
NR | NR | NR | NR |
| Levy (2007)116 | 9 mo | -Constant-murley mobility score | G1: Non-surgical (17) | (Pre→≥9 mo) (Avg (range)): 12 (6-18) → 34 (24-40) |
NR | NR | NR |
| Lunn (2007)119 | 50 mo | -Constant-murley mobility score | G1: Nonoperative (14) G2: Open repair (5) |
(Pre→post) Constant-murley (score): G1: 30.3→34 G2: 32.8→34.8 |
NR | NR | NR |
| Ainsworth (2009)127 | 12 mo | -“Visual estimation” (Flexion) -Goniometer (ER) |
G1: PT + Exercise (30) G2: Control (Placebo) (no exercise) (30) |
(3 mo) Elevation AROM (percent of cohort) G1: 71% improved by > 5 ° G2: 53% improved by > 5 ° (3 mo→6 mo→12 mo) ER PROM G1: 1.88 °→8.75 °→7.43 ° G2: 5.36 °→(-)3.7 °→4.4 ° |
NR | (3 mo→6 mo→12 mo) Elevation AROM G1: Values NR G2: Values NR (3 mo→6 mo→12 mo) ER PROM G1: 1.88 °→8.75 °→7.43 ° G2: 5.36 °→(-)3.7 °→4.4 ° |
Elevation AROM: G1 vs G2: 3 mo: p = 0.015 6 mo: p = 0.051 12 mo: p = 0.374 (NS) ER PROM: G1 vs G2: 3 mo: p = 0.889 (NS) 6 mo: p = 0.009 12 mo: p = 0.029 |
| Baydar (2008)118 | 6 mo, 1 yr, 3 yr (Pt. report) | -Goniometer | G1: Non-surgical (20) | (Pre→6 mo) AROM: Flexion: 139 °→159.5 ° Abduction: 132.7 °→163.2 ° IR: 11.8 °→13.8 ° ER: 59.5 °→74.7 ° PROM: Flexion: 163 °→174 ° ER: 70.7 °→81.0 ° |
(6 mo) AROM: Flexion: p < 0.001 Abduction: p < 0.001* IR: p < 0.001 ER: p < 0.001* PROM: Flexion: p < 0.003 ER: p < 0.003 |
NA | NA |
| Moosmayer (2010/2014)47,48 ‡ | 6mo, 1yr, 2yr 5 yr | -Goniometer | G1: Surgical (52) G2: PT (51) †G3: G2→G1 (9; 18%) †G4: PT only (39) |
(Pre→6 mo→1 yr→ 5 yr) G1: Flexion: 87 °→147 °→166 °→171 ° Abd: 73.7 °→135 °→158 °→167 ° G2: Flexion: 89 °→147 °→156 °→164 ° Abd: 82 °→135 °→144 °→155 ° |
NR | (Post) Flx (°): G1: 171 °; G2: 164 ° Abd (°): G1: 167 °; G2: 155 ° |
(Post) Flx: G1 vs G2: p = 0.3 (NS) Abd: G1 vs G2: p = 0.15 (NS) |
| Tanaka (2010)113 | G1: 2.4 yr G2: 2.2 yr |
-Goniometer | G1: Non-surgical (subjects: 62 shoulders: 65) G2 Failed G1→surgery (subjects: 56 shoulders: 58) |
(Post) Flx (°): G1: 143 °; G2: 135 ° ER (°): G1: 52.2 °; G2: 35 ° |
NR | (Post) Flx (°): G1: 143 °; G2: 135 ° ER (°): G1: 52.2 °; G2: 35 ° |
(Post) Flx: G1 vs G2: p = 0.77 (NS) ER: G1 vs G2: p < 0.001* |
| Gialanella (2011)128 | 6 mo | -Constant-murley mobility score | G1: PT & CS (x1) (20) G2: PT & CS (x2) (20) G3: PT (control) (20) |
(Pre→3 mo→ 6 mo) AROM (score): G1: 14.0→17.0→14.8 G2: 15.3→20.1→16.7 G3: 16.6→17.0→16.4 |
(3 mo) AROM: G1: p < 0.01 G2: p < 0.001 (6 mo) AROM: G2: P < 0.05 |
(Pre→3 mo→ 6 mo) AROM (score): G1: 14.0→17.0→14.8 G2: 15.3→20.1→16.7 G3: 16.6→17.0→16.4 |
(6 mo) AROM: G1 vs G2 vs G3: p = NS |
| Merolla (2011)1 | 12 mo. | -Goniometer | G0: Conservative therapy (60) G1: ‘Successful’ (33) G2: G0→ surgery (27) |
(Pre→3 mo→6 mo→12 mo) Flx AROM (°): G0: 108 °→160 °→150 °→145 ° Abd AROM (°): G0: 92 °→150 °→145 °→140 ° ER AROM (°): G0: 45 °→42 °→47 °→46 ° IR AROM (°): G0: 50 °→52 °→48 °→54 ° |
(3 mo, 6 mo, 12 mo) Flx AROM: G0: P<0.01* Abd AROM: G0: P<0.01* ER AROM: G0: P>0.05 (NS) IR AROM: G0: P>0.05 (NS) |
NR | NA |
| Kijma (2012)110 | 12.9 yr | NR | G1: 43 | NR | NR | NR | NR |
| Krischak (2013)124 | 2 mo | -Goniometer | G1: Standard OT (22) G2: Home exercises (16) |
(Pre→2 mo) AROM (°): Abduction: G1: 131.7 ° →159.7 ° G2: 127.4 °→151.3 ° Flexion: G1: 155.1 ° →164.6 ° G2: 148.9 ° →161.1 ° External rotation: G1: 39.9 °→47.2 ° G2: 42.4 °→48.8 ° |
NR | (2 mo) AROM (°): Abd: G1: 159.7 °; G2: 151.3 ° Flx: G1: 164.6 °; G2: 161.1 ° ER: G1: 47.2 °; G2: 48.8 ° |
(2 mo) AROM (°): Abd: G1 vs G2: p = 0.66 (NS) Flx: G1 vs G2: p = 0.64 (NS) ER: G1 vs G2: p = 0. 92 (NS) |
| Kuhn (2013)40 | 1 yr | -Goniometer | G0: PT program‡ (422, 100%) G1: Cured (237, 62.2%) (no formal f/u scheduled) G2: Improved (continue PT) G3: No better (82, 29%) (offered surgery) |
(Pre→6 wk→12 wk) AROM (degrees): Flexion: G0: 149 °→163.3 °→162.9 ° Abduction: G0: 136.8 °→154.9 °→154.7 ° ER at 0 ° Abd: G0: 52.9 °→55.6 °→55.8 ° IR at 0 ° Abd: G0: 45.32 °→46.36 °→52.27 ° |
NR | NR | NA |
| Benazzo (2014)99 | 29 mo | NR | Non-surgical: (1) | (Pre→40 d→60 d) AROM (degrees): Flx: “unable”→100 °→”full ROM” Abd: “unable”→100 °→”full ROM” ER: “not impaired”→ ”full ROM” IR: “not impaired”→ ”full ROM” |
NA | NA | NA |
| Boorman (2014)123 | 29 mo | NR | G0: 3 mo supervised, non-operative§ G1: “Successful”(no surgery indicated) (70; 75%) G2: “failed” (underwent surgery) (23; 25%) |
(Baseline) Forward Elevation: G1: 154 ° G2: 153 ° |
NA | (Baseline) Forward Elevation: G1: 154 ° G2: 153 ° |
(Baseline) Forward Elevation: G1 vs G2: p = 0.618 (NS) |
| Güzelant (2014)117 | 66 mo (mean) | -Goniometer | G1: “Conservative therapy” (33) |
(Pre→Post) Flexion: 105 °→160 ° Abd-ER: 41 °→44 ° |
(Post) Flx: P<0.05 (p = 0.0272)* Abd-ER: p > 0.05 (NS) |
NA | NA |
| Kukkonen (2014/2015)52,125 | 24 mo | -Constant-murley mobility scale | G1: PT (55) G2: Acromioplasty & PT (58) G3: RC repair, acromioplasty & PT (54) |
(Pre→6 mo→12 mo→24 mo) Constant-murley (score):** G1: 29.1→36.1→36.1→ 37.0 G2: 31.2→35→36→36.2 G3: 30.0→34.1→36.0→36.0 |
NR | (24 mo) Constant-Murley (score):** G1: 37.0 G2: 36.2 G3: 36.0 |
(24 mo) Constant-Murley: G1 vs G2 vs G3: p>0.05 (NS) |
| Collin (2015)106 | 24 mo | -Anterior elevation -“ER with the elbow by the side” (ER1) |
G1: “Rehab program” (45) (nonoperative) |
(Pre→post) Anterior elevation > 160 ° (percent cohort): G1: NR→53% ER1 (percent cohort): G1: 31% →31% |
NR | NA | NA |
| Lambers Heerspink (2015)49 | 12 mo | -NR | G1: “Conservative Management” (31) G2: RC repair (25) |
NR | NA | NR | NA |
| Baumer (2016)121 | ≥9 wk | -Goniometer | G1: PT (25) G2: Healthy controls (25) |
(Pre→≥9 wk) AROM (°): Abd: G1:131.5 °→164.7 °; G2:180 ° Flx: G1: 140.7 °→169.4 °; G2: 180 ° ER: G1: 71.5 °→86.2 °; G2: 102.0 ° IR: G1: 40.2 °→55.4 °; G2: 64.7 ° PRROM (°): Abd: G1:135.2 °→164.3 °; G2:180 ° Flx: G1: 145.7 °→176.8 °; G2: 180 ° ER: G1: 74.3 °→88.4 °; G2: 103.6 ° IR: G1: 34.3 ° →43.8 °; G2: 57.3 ° |
(Pre→≥9 wk) AROM (°): Abd: G1: p = 0.01* Flx: G1: p < 0.01* ER: G1: p = 0.02* IR: G1: p = 0.03* PRROM (°): Abd: G1: p < 0.01* Flx: G1: p = 0.02* ER: G1: p = 0.01 IR: G1: p < 0.01* |
(≥9 wk) AROM (°): Abd: G1: 164.7; G2: 180 ° Flx: G1: 169.4 °; G2: 180 ° ER: G1: 86.2 °; G2: 102.0 ° IR: G1: 55.4 °; G2: 64.7 ° PRROM (°): Abd: G1: 164.3 °; G2: 180 ° Flx: G1: 176.8 °; G2: 180 ° ER: G1: 88.4 °; G2: 103.6 ° IR: G1: 43.8 °; G2: 57.3 ° |
(≥9 wk) AROM (°): Abd: G1 vs G2: p=0.03 Flx: G1 vs G2: p = 0.05 ER: G1 vs G2: p < 0.01 IR: G1 vs G2: p = 0.08 (NS) PRROM (°): Abd: G1 vs G2: p=0.03 Flx: G1 vs G2: p = 0.33 (NS) ER: G1 vs G2: p < 0.01 IR: G1 vs G2: p < 0.01 (NS) |
| Christensen (2016)122 | ≥5 mo | -Goniometer | G1: Non-operative(30) G2: Control (30)Δ |
(Pre→≥5 mo) AROM (°): Flx G1: 132.5 °→133.9 ° (+1.4 °) Abd G1: 93.7 °→133.9 ° (+34.4 °) ER G1: 27.9 °→31.7 ° (+3.8 °) |
(≥5 mo) Flx G1: p = 0.912 (NS) Abd G1: p = 0.005* ER: G1: p = 0.364 (NS) |
NR | NA |
| Miller (2016)111 | 12 wk | -Dynamic stereoradiography (DSX) | G1: Exercise therapy (5) | (Pre→12 wk) GH path length (percent of glenoid height): 67.2%→43.1% GH translation (percent of glenoid height): Superior-inferior: 17.1%→17.2% GH translation (percent of glenoid width): Anterior-posterior: 3.5%→3.2% Acromiohumaral distance (mm): Mean: 1.5 → 1.5 Minimum: 0.6 → 0.7 |
(12 wk) GH path length: P = 0.036* GH translation superior- inferior: p = 0.88 (NS) GH translation anterior- posterior: p = 0.89 (NS) Acromiohumaral distance: Mean: p = 0.81 (NS) Minimum: p = 0.31 (NS) |
NA | NA |
| Mischke (2016)100 | 13 visits (time NR) | Goniometer | Conservative therapy (1) | (Pre→visit 7→ visit 13) Shoulder Flx (°): 80 °→130 °→170 ° |
NA | NA | NA |
| Upadhyaya (2016)103 | 10 yr | -NR | Non-operative treatment (1) | (Pre → 10 yr) Range of motion: “full ROM”→ “P/AROM symmetry” |
NR | NA | NA |
| Moosmayer (2017)112 | 8.8 yr | -Constant-murley mobility scale | G1: Non-operative (49) G1a: Tear size < 9.9 mm (33) G1b: Tear size 10-19.9 mm (8) G1c: Tear Size ≥ 20 mm (8) |
(≥ 8.8 yr) Abduction (°): G1a: 180 ° G1b: 163 ° G1c: 160 ° Flexion (°): G1a: 180 ° G1b: 168 ° G1c: 170 ° |
NR | (≥ 8.8 yr) Abduction (°): G1a & G1b: 180 ° G1c: 160 ° Flexion (°): G1a & G1b: 180 ° G1c: 170 ° |
(≥ 8.8 yr) Abduction (°): G1a & G1b vs G1c: p = 0.13 (NS) Flexion (°): G1a & G1b vs G1c: p = 0.08 (NS) |
Abd, abduction; AROM, active range of motion; CS, corticosteroid; d, days; ER, external rotation; Flx, flexion; G, group; GH, glenohumeral; JOA, Japanese orthopedic association score; Mo, month; NA, not applicable; NR; not reported; NS; not statistically significant; PT, physical therapy; ROM, range of motion; Tsp ver, thoracic spine vertebrae, UCLA, University of California Los Angeles shoulder rating scale; wk, week; yr, year; *, clinical significance, indicates a statistical significant difference and a >20% difference; †, G3 and G4 are a subset of G2; Abd, abduction; ‡, all subjects began a physical therapy program and were reevaluated at 6 and 12 weeks, at those times patient were assigned to G1, G2, or G3 based on findings; §, all subjects underwent a 3 mo supervised program of nonoperative treatment & with an evaluated by orthopedic surgeon and assigned to G1 or G2; **, values estimated to nearest tenth based off graphical representation, as no specific numerical values reported with-in study.
Appendix F.
Outcomes for strength
| First Author (Year) | Follow-up Period | Outcome Scale | Treatment groups (n = ) | Intragroup difference | Statistically significant (*clinical significance) | Between group difference | Statistically significant |
|---|---|---|---|---|---|---|---|
| Itoi (1992)109 | 3.4 yr (1 – 9 yr) | -MMT | G0: All patients (62) G1: Satisfied (15) G2: Unsatisfied (8) |
(Pre→Post) (Percent of cohort ≥4/5): G0: Abd: 89.6%→87.1% ER: NR→87.1% G1: Abd: NR→87% G2: Abd: NR→63% |
(Post) (Percent of cohort ≥4/5): G0: p>0.05 (NS) G1: p<0.05 G2: p>0.05 (NS) |
(Post) G1: Abd: NR → 87% G2: Abd: NR → 63% |
(Post) (Percent of cohort ≥4/5): G1 vs G2: p < 0.05* |
| Bokor (1993)105 | 7.6 yr (3.7 – 12 yr) | -UCLA strength of flexion | G1: Non-surgical (53) | NR | NR | NA | NA |
| Hawkins (1995)108 | 3.8 yr | -Constant- Murley strength score | G1: Non-surgical (19) G2: Not satisfied w/ non-surgical (14) |
(Pre→ Post) Constant-Murley (score): G1: 21.2→23.2 G2: 18.6→17.1 |
NR | (Post) Constant-Murley (score): G1: 23.2 G2: 17.1 |
(Post) Constant-Murley (score): G1 vs G2: p = 0.008* |
| Wirth (1997)114 | >/= 2 yr | -ASES | G1: Exercise therapy (60) | NR | NR | NA | NA |
| Palmer (1998)101 | 2 yr | -Hand-held dynamometer | Aquatic Therapy (1) | (Pre→post) Supra: 0→7 lb Flex: 7→7lb Abd: 7→7lb ER: 8→17lb IR: NR→20lb Elbow Flex: 10→18lb Elbow Ext: 10→25lb |
NR | NA | NA |
| Yamada (2000)115 | 4 yr (12 mo – 19 yr) | -MMT | G1: Non-surgical (14) G2: Surgery (26) |
G1: Abd & ER 4/5 G2: Abd & ER 5/5 |
NR | NR | NR |
| Goldberg (2001)107 | 2.5 yr | -NR | G1: Non-surgical (46) | NR | NR | NR | NR |
| Shibata (2001)126 | 24 wk | -UCLA MMT | G1: 25 mg sodium Hyaluronate & 3 mL 1% lidocaine (38) G2: 2mg Dexamethasone & 3 mL 1% lidocaine (40) |
(Pre→4wk→24wk) UCLA MMT (score): G1: 3.4→4.8→4.6 G2: 3.0→4.0→3.9 |
(4 wk) UCLA MMT (score): G1: p<0.01* G2: p<0.01* (24 wk) UCLA MMT (score): G1: p>0.05 (NS) G2: p < 0.01 |
NR | NR |
| Vad (2002)120 | 3.1 yr (Range: 2-7 yr) |
-MMT | G1a: PT + meds (28) G1b: PT + meds + CS (12) G2: Failed G1a/b arthroscopy (32) G3: Primary surgery RCT repair (36) |
(Pre→post) (Percent of Cohort < 3/5 MMT): G1: 78% → NR G2: 83% → NR G3: 80% → NR |
NR | NR | NR |
| Piccoli (2004)102 | 7 wk | -MMT | Single case | (Pre→7 wk) Flexion: 3+/5 → 4+/5 Extension: 3+/5 → 4+/5 Abduction: 3+/5 → 4/5 Internal rotation: 3+/5 → 4+/5 External rotation: 3+/5 → 4+/5 |
NA | NA | NA |
| Ainsworth (2006)104 | Avg: 10.8 mo (Range: 2-36 mo) | -NR | G1: Non-surgical (10) (Torbay rehabilitation program) |
NR | NR | NR | NR |
| Levy (2007)116 | 9 mo | -Constant- murley strength score | G1: Non-surgical (17) | (Pre→≥9 mo) Constant (score): <1 (0-2 lb) → < 1 (0-2 lb) |
NR | NR | NR |
| Lunn (2007)119 | 50 mo | -Pre: MMT -Post: NR |
G1: Nonoperative (14) G2: Open repair (5) |
(Pre) ER at 0 ° ABD (grade): G1 & G2: 4/5 (n=13) G1 & G2: 3/5 (n=6) ER at 0 ° ABD (grade): G1 & G2: 5/5 (n=19) (Post) “Power in ER at 0 ° ABD” G1 & G2 injured arm: 3.2 kg G1 & G2 uninjured arm: 6.0 kg |
(Post) G1 & G2 Uninjured vs injured: p < 0.0001* |
NR | NR |
| Ainsworth (2009)127 | 12 mo | -NR | G1: PT + Exercise (30) G2: Control (Placebo) (no exercise) (30) |
NR | NR | NR | NR |
| Baydar (2008)118 | 6 mo, 1 yr, 3 yr (Pt. report) |
-Isokinetic strength measures | G1: Non-surgical (20) | (Pre→6 mo) (Peak torque (ft-lb)): ABD 60 °/s: 21.7→27.9 ABD 180 °/s: 19.45→22.4 ER 60 °/s: 3.95→7.70 ER 180 °/s: 3.95→6.85 IR 60 °/s: 15.75→22.7 IR 180 °/s: 12.6→19.5 |
(Post) ABD 60 °/s: p < 0.001* ABD 180 °/s: p < 0.001 ER 60 °/s: p < 0.001* ER 180 °/s: p < 0.001* IR 60 °/s: p < 0.001* IR 180 °/s: p < 0.001* |
NA | NA |
| Moosmayer (2010/2014)47,48 § | 6 mo, 1 yr, 5 yr | -Hand-held spring balance‡ | G1: Surgical (52) G2: PT (51) †G3: G2→G1 (9; 18%) †G4: PT only (39) |
(Pre→6 mo→1 yr→ 5 yr) G1: Scapular plane (kg) 7.5 →8.0 →11.1→12.1 G2: Scapular plane (kg) 8.1 →10.6 →11.9 →11.4 |
NR | (1 yr) G1: Scapular plane: 11.1 (kg) G2: Scapular plane: 11.9 (kg) (5 yr) G1: Scapular plane: 12.1 (kg) G2: Scapular plane: 11.4 (kg) |
(1 yr) G1 vs G2: p = 0.89 (5 yr) G1 vs G2: p < 0.001 |
| Tanaka (2010)113 | G1: 2.4 yr G2: 2.2 yr | -NR | G1: Non-surgical (Subjects: 62 Shoulders: 65) G2 Failed G1→surgery (subjects: 56 shoulders: 58) |
NR | NA | NR | NA |
| Gialanella (2011)128 | 6 mo | -NR | G1: PT & CS (x1) (20) G2: PT & CS (x2) (20) G3: PT (control) |
NR | NA | NR | NA |
| Merolla (2011)1 | 12 mo. | -NR | G0: Conservative therapy (60) G1: ‘Successful’ (33) G2: G0→ surgery (27) |
NR | NA | NR | NA |
| Kijma (2012)110 | 12.9 yr | NR | G1: 43 | NR | NA | NR | NA |
| Krischak (2013)124 | 2 mo | -Isokinetic dynamometer | G1: Standard OT (22) G2: Home exercises (16) |
(Pre→2 mo) Abd (Nm): 60 °/s G1: 31.6→38.1 G2: 39.9→41.6 Abd (Nm): 120 °/s G1: 33.7 →37.7 G2: 44.4 →44.8 ER (Nm): 60 °/s G1: 18.0 →20.3 G2: 20.8 →22.3 ER (Nm): 120 °/s G1: 17.0 →18.8 G2: 19.5 →20.9 |
NR | (2 mo) Abd (Nm): 60 °/s G1: 38.1 G2: 41.6 Abd (Nm): 120 °/s G1: 37.7 G2: 44.8 ER (Nm): 60 °/s G1: 20.3 G2: 22.3 ER (Nm): 120 °/s G1: 18.8 G2: 20.9 |
(2 mo) Abd (Nm): 60 °/s G1 vs G2: p = 0.359 (NS) Abd (Nm): 120 °/s G1 vs G2: p = 0.16 (NS) ER (Nm): 60 °/s G1 vs G2: p = 0.359 (NS) ER (Nm): 12 °/s G1 vs G2: p = 0.231 (NS) |
| Kuhn (2013)40 | 1 yr | -NR | G0: PT program§ (422, 100%) G1: Cured (237, 62.2%) (no formal f/u scheduled) G2: Improved (continue PT) G3: No better (82, 29%) (offered surgery) |
NR | NA | NR | NA |
| Benazzo (2014)99 | 29 mo | -NR | Non-surgical: (1) | (Pre→80 d) Strength (supraspinatus): NR→”normal” |
NA | NA | NA |
| Boorman (2014)123 | 29 mo | -NR | G0: 3 mo supervised, non-operative** G1: “Successful”(no surgery indicated) (70; 75%) G2: “failed” (underwent surgery) (23; 25%) |
(Baseline) ER full strength: (percent cohort) G1: 29% G2: 8% |
NA | (Baseline) ER full strength: (percent cohort) G1: 29% G2: 8% |
(Baseline) ER full strength: G1 vs G2: p = 0.966 (NS) |
| Güzelant (2014)117 | 66 mo | -“Horizontal hand scale” †† | G1: “Conservative therapy” (33) | (Pre→post) Infra: 3 (2-4)→ 3 (2-4+) Supra: 3 (2-4)→ 3 (2-4+) Deltoid: 3 (2-4)→ 4 (3-5) |
(Post) Infra: p > 0.05 (NS) Supra: p > 0.05 (NS) Deltoid: p < 0.05 (P = 0.0412) |
NA | NA |
| Kukkonen (2014/2015)52,125 | 24 mo | -Constant- Murley strength score | G1: PT (55) G2: Acromioplasty & PT (58) G3: RC repair, acromioplasty & PT (54) |
(Pre→6 mo→12 mo→24 mo) Constant-Murley (score):# G1: 8.5→11.2→11.5→11.5 G2: 8.1→10.1→10.9→12.0 G3: 8.1→9.0→10.8→12.0 |
NR | (24 mo) Constant-Murley (score):# G1: 11.5 G2: 12.0 G3: 12.0 |
(24 mo) Constant-Murley: G1 vs G2 vs G3: p>0.05 (NS) |
| Collin (2015)106 | 24 mo | -NR | G1: “Rehab program” (45) (nonoperative) |
NR | NA | NA | NA |
| Lambers Heerspink (2015)49 | 12 mo | -NR | G1: “Conservative Management” (31) G2: RC repair (25) |
NR | NA | NR | NA |
| Baumer (2016)121 | ≥9 wk | -Biodex system 2 | G1: PT (25) G2: Healthy controls (25) |
(Pre→≥9 wk) Normal strength (percentage): Abd: G1: 63.8%→59.7% G2: 96.8% Flx: G1: 78.3%→58.9% G2: 82.9% ER: G1: 69.3%→82.7% G2: 111.9% IR: G1: 78.3%→87.9% G2: 111.7% |
(Pre→≥9 wk) Normal strength: Abd: G1: p = 0.17 (NS) Flx: G1: p = 0.01 (NS) ER: G1: p = 0.09 (NS) IR: G1: p = 0.33 (NS) |
(≥9 wk) Normal strength (percentage): Abd: G1: 59.7%; G2: 96.8% Flx: G1: 78.3%; G2: 82.9% ER: G1: 69.3%; G2: 111.9% IR: G1: 78.3%; G2: 111.7% |
(≥9 wk) Normal strength (percentage): Abd: G1 vs G2: p < 0.01* Flx: G1 vs G2: p < 0.01 ER: G1 vs G2: p < 0.01* IR: G1 vs G2: p < 0.01* |
| Christensen (2016)122 | ≥5 mo | -Hand-held dynamometer | G1: Non-operative(30) G2: Control (30)Δ |
(Pre→≥5 mo) Force (N): Flx @ 45 ° G1: 23.5→33.7 Flx @ 90 ° G1: 17.6→24.6 Abd G1: 50.2→62.5 ER G1: 24.2→24.9 IR G1: 93.1→102.1 |
(≥5 mo) Strength (N): Flx @ 45 ° G1: p = 0.036* Flx @ 90 ° G1: p = 0.049* Abd G1: p = 0.009* ER G1: p = 0.363 (NS) IR G1: Pp = 0.102 (NS) |
NR | NA |
| Miller (2016)111 | 12 wk | -Hand-held dynamometer | G1: Exercise therapy (5) | (Pre→12 wk) Force (N): ER at 0 ° ABD: 54.2→83.9 (+54%) ER at 90 ° ABD: 46.7→81.2 ( + 74%) IR at 0 ° ABD: 93→121.8 (+31%) Scaption at 90 °: 40.1→61.9 (+54%) |
(12 wk) Force (N): ER at 0 ° ABD: p = 0.005* IR at 0 ° ABD: p = 0.036* ER at 90 ° ABD: p = 0.009* Scaption at 90 °: p = 0.024* |
NA | NA |
| Mischke (2016)100 | 13 visits (time NR) | NR | Conservative therapy (1) | NR | NA | NA | NA |
| Upadhyaya (2016)103 | 10 yr | -MMT | Non-operative treatment (1) | (Pre → 10 yr) MMT (grade 0-5): IR: 5/5 → 5/5 ER: 5/5 → 4/5 Abd: 4/5 → 4/5 |
NR | NA | NA |
| Moosmayer (2017)112 | 8.8 yr | -Constant- murley strength score | G1: Non-operative (49) G1a: Tear size < 9.9 mm (33) G1b: Tear size 10-19.9 mm (8) G1c: Tear Size ≥ 20 mm (8) |
(≥ 8.8 yr) Strength (kg): G1a: 12.0 G1b: 10.0 G1c: 6.0 |
NR | (≥ 8.8 yr) Strength (kg): G1a & G1b: 12.0 G1c: 6.0 |
(≥ 8.8 yr) Strength (kg): G1a & G1b vs G1c: 6.0: p < 0.004* |
Abd, abduction; CS, corticosteroid; Constant-murley, constant murley shoulder outcome score; ER, external rotation; G, group; infra, infraspinatus; IR, internal rotation; kg, kilogram; MMT, manual muscle test; Mo, month; NA, not applicable; NR; not reported; NS, not statistically significant; PT, physical therapy; supra, supraspinatus; UCLA, University of California Los Angeles shoulder rating scale; wk, week; yr, year; *, clinical significance, indicates a statistical significant difference and a ≥20% difference; †, G3 and G4 are a subset of G2; ‡, As described by the Constant-murley subscale for strength; §, all subjects began a physical therapy program and were reevaluated at 6 and 12 weeks, at those times patient were assigned to G1, G2, or G3 based on findings; **, all subjects underwent a 3 mo supervised program of nonoperative treatment & with an evaluated by orthopedic surgeon and assigned to G1 or G2; ††, assumed to be manual muscle testing; #, values estimated to nearest tenth based off graphical representation, as no specific numerical values reported with-in study.
Appendix G.
Outcomes for Function
| First Author (Year) | Follow-up Period | Outcome Scale | Treatment groups (n = ) | Intragroup difference | Statistically significant (*clinical significance) | Between group difference | Statistically significant |
|---|---|---|---|---|---|---|---|
| Itoi (1992)109 | 3.4 yr (1 – 9 yr) | -Wolfgang criteria | Groups based off symptom duration G1: < 3 wk (15) G2: 3 wk – 3 mo (19) G3: 3 mo – 12 mo (19) G4: 12 mo (9) |
(Pre→post) Wolfgang criteria (points): G1: 12.1 → 14.3 G2: 11.2 → 13.5 G3: 11.4 → 13.9 G4: 11.9 →12.5 |
(Post) G1: p<0.05 G2: p<0.01* G3: p<0.01* G4: p>0.05 (NS) |
NR | NR |
| Bokor (1993)105 | 7.6 yr (3.7 - 12 yr) | -ASES ADLs -UCLA |
G1: Non-surgical (53) | (Pre→post) ASES (Percent of cohort ‘mild or no compromise’ in ADLs): 24.8%→77.4 % UCLA (points; Avg score): 14.6 → 28.1 |
(Pre→Post) ASES (change in points) G1: + 52.6 > MCID: + 6.4202 UCLA (change in score) G1: (MCID NA) |
NA | NA |
| Hawkins (1995)108 | 3.8 yr | -Constant-Murley | G1: Non-surgical (19) G2: Not satisfied w/ non-surgical (14) |
(Post) Constant-Murley (score change): G1: + 7.2 G2: -1.1 |
(Post) G1: + 7.1 < MCID: + 10.4203 G2: -1.1 < MCID: + 10.4203 |
(Post) Constant-Murley (score): G1: 7.2; G2: -1.1 |
(Post) Constant-Murley: G1 vs G2: p = 0.038* |
| Wirth (1997)114 | >/= 2 yr | -UCLA | G1: Exercise therapy (60) | (Pre→post) UCLA (score): 13.4→29.4 |
NR (MCID NA) | NA | NA |
| Palmer (1998)101 | 2 yr | -Swimming | Aquatic Therapy (1) | Demonstrate front crawl 2x40 feet | NR | NA | NA |
| Yamada (2000)115 | 4 yr (12 mo-19 yr) | -JOAS | G1: Non-surgical (14) G2: Surgery (26) |
(Post) JOAS (Percent improvement): G1: 21.5% G2: 25.9% |
(Post) G1: p = 0.0060* G2: p < 0.0001* |
NR | NR |
| Goldberg (2001)107 | 2.5 yr | -SST -SF-36 |
G1: Non-surgical (46) | (Pre→2.5 yr) Simple shoulder test (points): 5.6 (+/-3.2)→7.0 (+/-3.8) Avg Improvement: 1.4(+/-3.6) SF-36 (points): Comfort: 48.3→58.5 (+10.1) Vitality: 60.0→49.6 (-10.4) Physical function: 60.4→48.3 (-12.2) General health: 76.4→60.8 (-15.7) |
(2.5 yr) Simple shoulder test: (p<0.01)* SF-36: Comfort: p=0.01* Vitality: p<0.01* Physical function: p<0.01* General health: p<0.01* |
NA | NA |
| Shibata (2001)126 | 24 wk | -UCLA | G1: 25 mg sodium Hyaluronate & 3 mL 1% lidocaine (38) G2: 2mg Dexamethasone & 3 mL 1% lidocaine (40) |
(Pre→4wk→24wk) UCLA (points): G1: 13.6→27.6→26.2 G2: 11.9→26.5→25.3 |
(24 wk) G1: 4 & 24 wk: p<0.0001* G2: 4 & 24 wk: p<0.0001* |
NR | NR |
| Vad (2002)120 | 3.1 yr (Range: 2-7 yr) |
-Shoulder rating questionnaire | G1a: PT + meds (28) G1b: PT + meds + CS (12) G2: Failed G1a/b arthroscopy (32) G3: Primary surgery RCT repair (36) |
(Pre→post) SRQ (score): G1a: 43/100 → 64/100 G1b: 44/100 → 75/100 G2: 44.5/100 →82/100 G3: 35/100 → 84/100 |
(Post) SRQ (score): G1a: p < 0.05* G1b: p < 0.05* G2: p < 0.05* G3: p < 0.05* |
(Post) SRQ (score): G1a: 64/100; G1b: 75/100 |
(Post) SRQ: G1b vs G1a: p < 0.05 |
| Piccoli (2004)102 | 7 wk | -SPADI -SF-12 |
Single case | (Pre→7 wk) SPADI (points): 76→17 SF-12 (points): PCS: 21.67 → 50.1 MCS: 56.28 → 58.49 |
(Pre→7 wk) SPADI (change in points) (-59) > MCID: + 8 points204 |
NA | NA |
| Ainsworth (2006)104 | Avg: 10.8 mo (Range: 2-36 mo) | -ODSQ -SF-36 |
G1: Non-surgical (10) (Torbay rehab program) | (Pre→3 mo.) ODSQ: (points) Avg Score: 34.2 → 23.6 SF-36 (points): Physical health: 25→35 Emotional health: 80→57 General health: 70→61 |
NR (MCID NA) | NA | NA |
| Levy (2007)116 | 9 mo | -Constant-Murley | G1: Non-surgical (17) | (Pre→≥9 mo) Constant Score (Avg score (range)): 26 (8-41)→63 (43-77) |
(Pre→≥9 mo) Constant Score (score change): G1: + 37 > MCID: + 10.4203 |
NA | NA |
| Lunn (2007)119 | 50 mo | -Constant-Murley | G1: Non-operative (14) G2: Open repair (5) |
(Pre→post) Constant-murley (points [percent]): G1: 51 [58.3%]→ 66.6 [75%] G2: 53.0 [58%]→ 69.5 [75.4%] |
(Post) G1: p = 0.009 G2: p = 0.009 |
(Post) Constant-murley (points [percent]): G1: 66.6 [75%] G2: 69.5% [75.4%] |
(Post) Constant-murley: G1 vs G2: p = 0.61 (NS) |
| Ainsworth (2009)127 | 12 mo | -OSS -SF-36 physical Function (PF) -MYMOP |
G1: PT + Exercise (30) G2: Control (Placebo) (no exercise) (30) |
(3 mo→6 mo→12 mo) OSS (score change time 0) G1: 8.19→9.42→8.96 G2: 3.0→4.43→6.27 SF-36 PF(score change time 0) G1: 7.78→4.42→5.21 G2: (-)3.5→(-)3.00→(-)3.17 MYMOP (score changed time 0) G1: 1.03→1.27→1.02 G2: 0.46→0.67→1.08 |
NR (MCID NA) | (3 mo→6 mo→12 mo) OSS (score change) G1: 8.19→9.42→8.96 G2: 3.0→4.43→6.27 SF-36 PF (score change) G1: 7.78→4.42→5.21 G2: (-)3.5→(-)3.00→(-)3.17 MYMOP (score changed) G1: 1.03→1.27→1.02 G2: 0.46→0.67→1.08 |
OSS: G1 vs G2: 3 mo: p = 0.002 6 mo: p = 0.008 12 mo: p = 0.16 (NS) SF-36 PF: G1 vs G2: 3 mo: p = 0.005 6 mo: p = 0.136 (NS) 12 mo: p = 0.049 MYMOP: G1 vs G2: 3 mo: p = 0.052 6 mo: p = 0.047 12 mo: p = 0.847 (NS) |
| Baydar (2008)118 | 6 mo, 1 yr, 3 yr (Pt. report) | -ASES -Constant- Murley -SF-36 |
G1: Non-surgical (20) | (Pre→6 mo→1 yr→ 3yr) ASES (points): 24.95→44.15→42.44→43.28 (Pre→ 6 mo) Constant-Murley (points): 52.10→ 76.35 SF-36 (points): Physical function: 48.75→82.5 Physical role: 11.25→78.75 Social functioning: 87.5→99.37 |
(All-time points) ASES: P < 0.01* (6 mo) Constant-Murley: p<0.01* SF-36: Physical function: p < 0.001* Physical role: p < 0.001* Social functioning: p < 0.044 |
NA | NA |
| Moosmayer (2010/2014)47,48 ‡ | 6mo, 1yr, 2yr 5 yr | -ASES -Constant-Murley -SF-36 |
G1: Surgical (52) G2: PT (51) †G3: G2→F1 (12) †G4: PT only (39) |
(Pre→6 mo→1 yr→ 5 yr) ASES (points): G1: 45.5→85.3→93.6→92.8 G2: 48.2 →35.4 →83.6 →85.4 G3: 40.3 G4: 50.6 Constant-Murley (points): G1: 35.3 →65.6 →77.7 →79.8 G2: 38.4 →63.9 →70.3 →74.2 SF-36 (points): G1: 38.2 →48.3 →51.2 →50.1 G2: 38.6 →47.3 →50.3 →48.4 |
(Pre→5 yr) ASES (point change): G1: + 47.3 > MCID: + 6.4202 G2: + 37.2 > MCID: + 6.4202 Constant (point change ): G1: + 44.5 > MCID: + 10.4203 G2: + 35.8 > MCID: + 10.4203 SF-36 (points): (MCID NA) |
(Pre) ASES (points): G3: 40.3; G4: 50.6 (5 yr) ASES (points): G1: 92.8; G2: 85.4 Constant-murley (points): G1: 79.8 G2: 74.2 G3: 73.3 G4: 70.1 SF-36 (points): G1: 50.1 G2: 48.4 |
(Pre) ASES: G4 vs G3: P < 0.05* (5 yr) ASES: G1 vs G2: P < 0.001 Constant-murley: G1 vs G2: p < 0.01 G4 vs G2: p < 0.01 G3 vs G2: p = 0.23 (NS) SF-36: G1 vs G2: p = 0.38 (NS) |
| Tanaka (2010)113 | G1: 2.4 yr G2: 2.2 yr | -Constant-Murley | G1: Non-surgical (subjects: 62 shoulders: 65) G2 Failed G1→surgery (subjects: 56 shoulders: 58) |
(Post) Constant-Murley Score > 75: G1: 100% of cohort G2: NR |
NR | NR | NR |
| Gialanella (2011)128 | 6 mo | -Constant-Murley | G1: PT & CS (x1) (20) G2: PT & CS (x2) (20) G3: PT (control) (20) |
(Pre→3 mo→ 6 mo) Constant-Murley (Total score): G1: 23.7 →34.7 →28.0 G2: 24.8 →35.6 →29.2 G3: 30.5 →30.7 →29.9 |
(3 mo) AROM sub-score: G1 & G2: P < 0.001 (6 mo) AROM sub-score: G1: p < 0.05 G2: p < 0.001 |
(Pre→3 mo→ 6 mo) Constant-Murley (Total score): G1: 23.7 →34.7 →28.0 G2: 24.8 →35.6 →29.2 G3: 30.5 →30.7 →29.9 |
(All time points) p = NS |
| Merolla (2011)1 | 12 mo. | -Constant-Murley -Prediction scale |
G0: Conservative therapy (60) G1: ‘Successful’ (33) G2: G0→ surgery (27) |
(Pre→3 mo→6 mo→12 mo) Constant-Murley (total score): G0: 46.3→62.3→60.2→ (G1) 61.9 Prediction score (out of 21): G1: range: 10.6 - 12.8/21 G2: range: 15.2-17.3/21 |
(3 mo, 6 mo, 12 mo) Constant-Murley (total score): G0: p<0.01* |
||
| Kijma (2012)110 | 12.9 yr | -JOAS | G1: 43 | (Post) JOAS (avg score): 9.4/10 No disturbance to ADLs (n = ): 31 (72%) |
NR | NR | NR |
| Krischak (2013)124 | 2 mo | -Constan-Murley -EQ-5D |
G1: Standard OT (22) G2: Home exercises (16) |
(Pre→2 mo) Constant-Murley (points): G1: 60.6→75.5 G2: 60.1→73.8 EQ-5D quality of life index (points): G1: 0.97 →0.926 G2: 0.885 →0.933 EQ-5D status of health (points:) G1: 53.8 →71.6 G2: 58.6 →61.8 |
(Pre→2 mo) Constant (score change): G1: + 14.9 > MCID: + 10.4203 G2: + 13.7 > MCID: + 10.4203 |
(2 mo) Constant-Murley (points): G1: 75.5; G2: 73.8 EQ-5D quality of life index (points): G1: 0.926; G2: 0.933 EQ-5D status of health (points): G1: 15.6; G2: 61.8 (Pre→2 mo) EQ-5D status of health (point difference): G1: 17.8; G2: 3.2 |
(2 mo) Constant-Murley G1 vs G2: p = 0.824 (NS) EQ-5D QOL index: G1 vs G2: p = 0.656 (NS) EQ-5D health status: G1 vs G2: p = 0.128 (NS) (Pre→2 mo) EQ-5D health status: G1 vs G2: p < 0.05* |
| Kuhn (2013)40 | 1 yr | -SF-12 MCS -SF-12 PCS -ASES -WORC score -SANE score -SA scale |
G0: PT program‡ (422, 100%) G1: Cured (237, 62.2%) (no formal f/u scheduled) G2: Improved (continue PT) G3: No better (82, 26%) (offered surgery) |
(Pre→6 wk→12 wk) SF-12 MCS: G0: 40.26→40.57→40.84 SF-12 PCS: G0: 35.34→35.64→36.01 ASES G0: 54.47→77.98→83.67 WORC scale: G0: 47.16→62.52→69.67 SANE scale: G0: 46.6→62.73→70.27 SA scale: G0: 9.89→10.15→10.01 |
(6 wk) SF-12 MCS: p = 0.36 (NS) SF-12 PCS: p<0.0001 ASES: p<0.0001* WORC scale: p<0.0001* SANE scale: p<0.0001* SA scale: p = 0.096 (NS) (12 wk) SF-12 MCS: p = 0.895 (NS) SF-12 PCS: p < 0.0001 ASES: p < 0.0001* WORC scale: p < 0.0001* SANE scale: p < 0.0001* SA scale: p = 0.47 (NS) |
NR | NA |
| Benazzo (2014)99 | 29 mo | -SST -Constant-Murley |
Non-surgical: (1) | (1 d→40 d→80 d) SST: 2→8→12 Constant-Murley: 44→57→100 |
(1 d→80 d) SST (Score change): - + 10 > MCID: + 2.0 Constant-Murley: (score change) - + 76 > MCID: + 10.4203 |
NA | NA |
| Boorman (2014)123 | 29 mo | -RC-QOL | G0: 3 mo supervised, non-operative§ G1: “Successful” (no surgery) (70; 75%) G2: “failed” (underwent surgery) (23; 25%) |
(Pre→3 mo→12 wk) RC-QOL score (0-100) G1: 49→82→80 G2: 33→38→NR |
NR (MCID NA) | (Pre) RC-QOL score (0-100): G1: 49 ± 21 (range: 0-84) G2: 33 ± 15 (range: 6-66) |
(Pre) RC-QOL: G1 vs G2: p<0.05 (P = 0.017*) |
| Güzelant (2014)117 | 66 mo (mean) | -ASES -UCLA |
G1: “Conservative therapy” (33) | (Pre→Post) ASES (score): 25.4→86.7 UCLA (score): 10.6→25.6 |
(Post) ASES: P < 0.05 (p = 0.0218*) UCLA: P < 0.05 (p = 0.0314*) |
NA | NA |
| Kukkonen (2014/2015)52,125 | 24 mo | -Constant-Murley -Constant-Murley ADL subscale -Satisfaction |
G1: PT (55) G2: Acromioplasty & PT (58) G3: RC repair, acromioplasty & PT (54) |
(Pre→12 mo→ 24 mo) Constant-Murley (score): G1: 57.8→74.1→76.2 G2: 59.6→77.2→80.1 G3: 58.0→77.9→80.6 Constant-Murley ADL subscale (score):* G1: 9.5→13.0→14.0→15.0 G2: 9.0→16.0→16.6→17.2 G3: 9.5→15.8→17.5→18.1 (24 mo) Satisfied (percent of cohort): G1: 89%; G2: 95%; G3: 94% |
(Pre→12 mo→ 24 mo) Constant-Murley (score): G1: + 18.4 > MCID: + 10.4203 G2: + 20.5 > MCID: + 10.4203 G3: + 22.6 > MCID: + 10.4203 |
(12 mo) Constant-Murley (score): G1: 74.1 G2: 77.2 G3: 77.9 (Pre→24 mo) Change in Constant-Murley (points): G1: 18.4; G2: 20.5; G3: 22.6 (12 mo; 24 mo) Constant-Murley ADLs (score):* G1: 14.0; 15.0 G2: 16.6; 17.2 G3: 17.5; 18.1 (24 mo) Satisfied (percent of cohort): G1: 89%; G2: 95%; G3: 94% |
(12 mo) Constant-Murley: G1 vs G2 vs G3: p = 0.34 (NS) (24 mo) Change in Constant-murley: G1 vs G2 vs G3: p>0.05 (NS) (12 mo) Constant-murley ADLs (score):* G1 vs G2/G3*: p<0.0001 (24 mo) Constant-murley ADLs (score):* G1 vs G2/G3*: p<0.01 (24 mo) Satisfaction: G1 vs G2 vs G3: p=0.28 (NS) |
| Collin (2015)106 | 24 mo | -Constant-Murley | G1: “Rehab program” (45) (nonoperative) |
(Pre→post) Constant-Murley (score): 43→56 |
(Post) p < 0.05 | NA | NA |
| Lambers Heerspink (2015)49 | 12 mo | -Constant-Murley -DSST -Disability VAS |
G1: “Conservative Management” (31) G2: RC repair (25) |
(Pre→12 mo) Constant-Murley (score): G1: 56.9→73.7 G2: 55.6→81.9 DSST (score): G1: 6.1→9.7 G2: 5.5→11.0 Disability VAS (cm): G1: 5.8→3.5 G2: 6.2→2.1 |
(Pre→12 mo) Constant (score change): G1: + 16.8 > MCID: + 10.4203 G2: + 26.3 > MCID: + 10.4203 DSST (score change): G1: + 3.6 > MCID: + 2.0203 G2: + 5.5 > MCID: + 2.0203 |
(12 mo) Constant-Murley (score): G1: 73.7; G2: 81.9 DSST (score): G1: 9.7; G2: 11.0 Disability VAS (cm): G1: 3.5; G2: 6.2→2.1 |
(12 mo) Constant-Murley: G1 vs G2: p > 0.05 (NS) DSST: G1 vs G2: p > 0.05 (NS) Disability VAS: G1 vs G2: p = 0.02* |
| Baumer (2016)121 | ≥9 wk | -WORC | G1: PT (25) G2: Healthy controls (25) |
(Pre→≥9 wk) WORC (score): G1: 40.6→70.3 G2: 98.2 |
(Pre→≥9 wk) WORC: G1: p<0.01* |
(≥9 wk) WORC (score): G1: 70.3; G2: 98.2 |
(≥9 wk) WORC: G1 vs G2: p < 0.01* |
| Christensen (2016)122 | ≥5 mo | -OSS -EQ-5D |
G1: Non-operative (30) G2: Control (30)Δ |
(Pre→3 mo→≥5 mo) OSS (score): G1: 26.0→34.2→37.7 (Pre→≥5 mo) EQ-5D (median score): G1: 0.671 → 0.755 |
(Pre→3 mo) OSS (score): G1: p < 0.05* (3 mo →5 mo) OSS (score): G1: p < 0.05* (Pre→≥5 mo) EQ-5D: G1: p = 0.009 |
NR | NA |
| Miller (2016)111 | 12 wk | -ASES -WORC -DASH |
G1: Exercise therapy (5) | (Pre→12 wk) ASES (score): 50.7→88.1 DASH (score): 35→5.6 WORC (score): 1198.8→344.8 |
(12 wk) ASES (score): p = 0.043* DASH (score): p = 0.047* WORC (score): p = 0.02* |
NA | NA |
| Mischke (2016)100 | 13 visits (time NR) | -GROC -Quick DASH |
Conservative therapy (1) | (Pre→visit 10→ visit 13) GROC (score): NR→+3→+5 Quick DASH (score): 65.9→43.2→31.8 |
(Pre→visit 10→ visit 13) GROC (score change): +2 = MCID + 2 Quick DASH (score change): +34.1 > MCID: 10.0203 |
NA | NA |
| Upadhyaya (2016)103 | 10 yr | -NR | Non-operative treatment (1) | NR | NR | NA | NA |
| Moosmayer (2017)112 | 8.8 yr | -Constant- Murley -ASES -SF-36 PHSS -SF-36 MHSS |
G1: Non-operative (49) G1a: Tear size < 9.9 mm (33) G1b: Tear size 10-19.9 mm (8) G1c: Tear Size ≥ 20 mm (8) |
(≥ 8.8 yr) Constant-Murley (score): G1a: 82.0; G1b: 81.0; G1c: 58.5 ASES (score): G1a: 90.0; G1b: 82.5; G1c: 60.0 SF-36 PHSS (score): G1a: 51.5; G1b: 50.5; G1c: 46.0 SF-36 MHSS (score): G1a: 59.8; G1b: 61.1; G1c: 58.5 |
NR | (≥ 8.8 yr) Constant-Murley (score): G1a & G1b: 81.0 G1c: 58.5 ASES (score): G1a & G1b: 90.0 G1c: 60.0 SF-36 PHSS (score): G1a & G1b: 51.5 G1c: 46.0 SF-36 MHSS (score:) G1a & G1b: 59.9 G1c: 58.5 |
(≥ 8.8 yr) Constant-Murley (score): G1a & G1b vs G1c: P = 0.008* ASES (score): G1a & G1b vs G1c: P = 0.02* SF-36 PHSS (score): G1a & G1b vs G1c: P = 0.14 (NS) SF-36 MHSS (score): G1a & G1b vs G1c: P = 0. 53 (NS) |
ASES, american shoulder and elbow surgeons index; ADLs, activities of daily living; Avg, average; Constant-murley, constant murley shoulder outcome score; CS, corticosteroid; DASH, disabilities of the arm, shoulder, and hand outcome measure; DSST, Dutch simple shoulder test; EQ-5D, EuroQol questionnaire; G, group; GROC, global rating of change; JOAS, Japanese orthopedic association score; MCID, minimally clinically important difference; MCS, mental component score; Mo, month; MYMOP, measure yourself medical outcome profile; NA, not applicable; NR; not reported; NS, not statistically significant; ODSQ, Oxford disability shoulder questionnaire; OSS, Oxford shoulder score; PCS, physical component score; PT, physical therapy; RC-QOL, rotator cuff quality of life index instrument; SA scale, shoulder activity scale; SANE score, single assessment numeric evaluation; SF-12, 12 item short form survey; SF-36, 36 item short form survey; SST, simple shoulder test score; UCLA, University of California Los Angeles shoulder rating scale; VAS, visual analog scale; wk, week; WORC, Western Ontario rotator cuff index; yr, year; *, clinical significance, indicates a statistical significant difference and a ≥20% difference; †, G3 and G4 are a subset of G2; ‡, all subjects began a physical therapy program and were reevaluated at 6 and 12 weeks, at those times patient were assigned to G1, G2, or G3 based on findings; §, all subjects underwent a 3 mo supervised program of non-operative treatment & with an evaluated by orthopedic surgeon and assigned to G1 or G2; *, values estimated to nearest tenth based off graphical representation, as no specific numerical values reported
Appendix H.
Components of conservative management interventions for included studies
| First author (Year) | Treatment duration (months) | Range of motion (ROM) | Stretching/flexibility | Strengthening | Joint mobilizations/manual therapy | Modalities | Pharmacological agents | Other |
|---|---|---|---|---|---|---|---|---|
| Itoi (1992)109 | 26 mo. (1 – 83 mo.) | 1. Active ROM 2. Passive ROM |
NR | 1. “muscle strengthening exercises” | NR | NR | 1. “anti-inflammatory agents” 2. injection (w/ & w/o CS) = ≤4x |
1. Rest (not specified) |
| Bokor (1993)105 | NR | NR | 1. “stretching” | 1. “strengthening” | NR | NR | 1. NSAIDs 2. CS (n=16) |
NR |
| Hawkins (1995)108 | 4 mo. | NR | NR | Weeks 1-10: 3x10; 1X/Day Weeks 10-16: 3x10: 3x/Week 6 Exercises: Add 1 every 2 wks 1. IR/ER “Rubber Tubing” 2. Short Arch FLX-EXT 3. Scapular retraction (Bilateral) 4. Supraspinatus drill (ABD arm from FLX & IR started position) 5. Long arc FLX/EXT 6. Diagonal PNF patterns with weights |
NR | NR | NR | NR |
| Wirth (1997)114 | ≥ 3 mo. |
Phase 1 1. Pendulum(s) 2. AAROM ER 3. Pulley system 4. Supine FLX & ER AROM 5. Wall Walks |
Phase 1 1. osterior capsule stretch 2. Overhead stretch using pull-up bar |
Phase 2A 2-3x/day; 1x5 reps; Band Color Progress 1x/2-3 weeks 1. IR/ER Therabands2. Scapular Retraction Theraband 3. Abduction (Elbow 90 °) Theraband4. Forward Press Theraband Phase 2B 2-3x/week 1. Wall Push-ups 2. Knee pushups 3. Shrug exercise 4. Shoulder press up from a chair 5. Scapular retraction (10 lbs; + 3lb/wk) Phase 3 2. Continue with exercises 2-3x/wk 3. Gradually reintegrate back into prior activities |
NR | 1. Hot shower 2. Heating pad 3. Cryotherapy post-exercise |
NR | 1. Activity modification 2. avoid the impingement arc >70 ° of elevation until symptoms improve 3. avoid “No Pain, No Gain” axiom of PT 4. Minimize and avoid pain |
| Palmer (1998)101* | 10 sessions (3.5 mo.) |
Phase 1 (AAROM – T-Bar) 1. FLX/EXT 2. Horizontal ABD 3. Scaption 4. ER 5. Unilateral shrugs 6. Arm circles |
NR |
Phase 2 1. Phase 1 – w/ ‘Light Resistance Band’ 2. Bicep Curl w/ gloves 3. Arm Circles w/ gloves 4. IR/IR w/ gloves 5. Breaststroke 6. Wall Push-ups 7. Functional Sweep Phase 3 1. Overhead crawl |
NR | NR | NR | NR |
| Yamada (2000)115 | NR |
PROM 1. Flexion 2. ER |
NR | 1. “Strengthening exercises as needed” | NR | 1. Hot Packs | 1. CS: 1-2x/wk (Avg: 15 x) | 1. Sling (1-3 weeks) |
| Goldberg (2001)107 | NR | NR | 1. Forward Elevation 2. ER 3. IR 4. Cross Body Stretch |
1. Supine Press 2. “RC Specific Exercises” 3. *Progress Exercise until 1lb wgt could be lifted 20x overhead in seated position |
NR | NR | NR | NR |
| Shibata (2001)126 | 24 wk | NR | NR | 1. ‘cuff strengthening’ | NR | heat | G1: 3 mL of 1% lidocaine G2: 2mg of dexamethasone + 3 mL of 1% Lidocaine |
1. If not satisfied at 4 wk, option for surgical rotator cuff repair |
| Vad (2002)120 | G1a: 8.2(1-22)wk G1b: 10.3(2-24) wk |
1. Not specified ("formal PT”) | 1. Not specified ("formal PT”) | 1. Not specified ("formal PT”) | 1. Not specified ("formal PT”) | 1. Not specified ("formal PT”) | 1. G1a: “Oral meds” 2. G1b: “Oral meds” & CS |
1. Not specified (“formal PT”) |
| Piccoli (2004)102 | 7 wk (19 visits) |
Phase 1 1. Wand exercises 2.FLX, ABD, ADD 2. Pendulums Phase 2 1. Wand exercises |
Phase 1 1. Manual stretching Phase 3 1. Manual resistance PNF (D1F & D2F) |
“Therapeutic exercise” Phase 1 1. Isometrics: flex, ER, IR 2. Scapula retraction (prone; 1 lb; 2x15) 3. UBE 5 min Phase 2 1. IR/ER “Rubber Tubing” 2. Short Arch FLX-EXT 3. Scapular retraction (Bilateral) 4. Supraspinatus drill (ABD arm from FLX & IR started position) 5. UBE 5 min → 7 min 6. Ball on wall (CW/CCW) Phase 3 1. Long arc FLX (5lb) 2. UBE 7 min → 10 min 3. Modified pushups (on knees) |
NR | - Ultrasound - Cryotherapy | Tylenol (w/ codeine) Aspirin | HEP |
| Ainsworth (2006)104 | 3 mo (12 wk) Wk1-4: 1x/wk Wk4-8: 1x/2-3wk | NR | 1. “Stretching” |
Progression of treatment program 1. Shoulder FLX to 90 ° (supine) 2. ER w/ yellow thera-band (supine) 3. 20 ° sways w/ arm straight (supine) 4. FLX w/ progressive weights (supine) 5. #1-4 (progressive incline of plinth) 6. Wall slides (eccentric control) (stand) 7. Elevation through elbow FLX (sit) 8. Raise/lower hand in elevation (sit) 9. ER w/ yellow thera-band (sit) 10. Proprioceptive activity (sit/stand) Improving proprioception 2. Close kinetic chain positions |
NR | NR | NR | 1. Patient education: 3. Pathophysiology 4. Goals of rehab program 2. Postural correction: 3. HEP (3 exercises; 2-3x/day) 4. Re-education of Muscle recruitment 5. Adaptation (activities improve function w/o increasing pain) |
| Levy (2007)116 | ≥12 wk | 1. Pendulums 2. AAROM FLX (supine) – 5 min |
NR | 1. FLX w/ 1-3lb (supine) – 5 min. 2. #1 w/ progressive incline (reclinesit) 3. FLX w/ elbow flexed using opposite arm for resistance (Stand/sit) – 10 reps |
NR | NR | 1. Pain meds (ibuprofen or other analgesic) | 1. Patient education - booklet with exercises and advice 2. Unsupervised HEP (3-5x/day) |
| Lunn (2007)119 | NR | NR | NR | NR | NR | NR | 1. CS injection | 1. Activity modification 2. “Physiotherapy conducted in a pool” |
| Ainsworth (2009)127 | 6 PT session | 1. “Exercises improve range of motion” |
1. “Stretching exercises to improve ROM of elevation, IR, & ER” |
1. Anterior deltoid strengthening program 2. IR & ER (TB) 3. Activities to improve proprioception |
1. Ultrasound (PRN) | 2. CS injection (PRN) | 1. “Advice” 2. Postural correction 3. Adaptation to functional activities |
|
| Baydar (2008)118 | 3 wk |
Phase 1 1. Wand exercises 3. FLX, EXT, ABD, ADD, IR, ER 2. Pendulums |
Phase 1 1. Posterior capsule stretch |
Phase 2 1. Thera-band & DB strengthening (IR, ER, FLX, EXT, ABD) 2. Scapula stabilization -Table push-ups -Shoulder shrugs -Shoulder press ups |
NR | 1. TEN 2. Ultrasound 3. Infrared radiation |
NR |
Phase 3 (Reintegration back to work/hobbies/sports) |
| Moosmayer (2010/2014)47,48† | 12 wk (≥40 min) | NR | NR | 1. ER/IR: isometric/concentric/eccentric 2. Scapulothoracic control/stability 3. GH joint control/stability (“centre humeral head in glenoid fossa”) |
NR | NR | NR | 1. Upper quarter posture 2. Exercise specific work, sport, leisure activities |
| Tanaka (2010)113 | 3.7 mo mo) | 1. “PROM” | 1. Stretching (RC & scapular muscles) | 1. “Muscle strengthening exercises” | 1. Tissue massage 2. “Manual therapy” |
1. TEN 2. Ultrasound |
1. NSAIDs 2. CS |
1. Rest |
| Gialanella (2011)128 | 6 mo (15x 20 min) | All groups: PROM | NR | All groups: “cuff strengthening exercises” |
All groups: “Passive GH joint mobilization” |
NR | G1: CS x1 G2: CS x2 (21-day interval) CS: (40 mg triamcinolone) |
NR |
| Merolla (2011)1 | 6 mo. | 1. AAROM (2 wk; 3x/wk)
-(scapulation, IR, ER) AROM (aquatic) (1 mo; 3x/wk) |
1. “soft tissue stretching” “stretching exercises” |
1. Anterior deltoid strengthening 2. IR/ER (TB) “Humeral positioners” |
NR | 1. Laser therapy (10 sessions) | 1. NSAIDS | 1. HEP |
| Kijma (2012)110 | NR | “Training to improve ROM” | NR | “Training to improve strength training from a physical therapist” |
NR | NR | 1. CS‡ 2. NSAIDs 3. Muscle Relaxors 4. Suppositories, & anxiety drugs, or sleep inducers§ |
NR |
| Krischak (2013)124 | 2 mo | G2: Home exercises 1. Pendulums: -(FLX/EXT, CW/CCW) 2.AROM: (FLX, ER) 3. breast stroke |
G2: Home exercises 1. Door stretch 2. Wall stretch (slides) |
G2: Home exercises 1. IR isometrics 2. TB resistance: -ADD, ABD, EXT, ER 3. Self-resisted FLX |
NR | NR | NR | 1. G1: “Standard OT” G2: Postural & breathing exercises |
| Kuhn (2013)40 *** | ≥ 6 wk | 1. Pendulums -(FLX, EXT, CW, CCW) 2. AAROM -FLX, EXT, IR, ER, ABD, 3. AROM 5. FLX (use of mirror to prevent shoulder shrug) |
1. Manual stretching: pectoralis minor, infraspinatus, teres minor, upper trapezius, sternocleidomastoid, and scalenes muscles 2. Sleeper stretch 3. Cross body stretch 4. Door/wall stretch |
1. Jackins exercise (anterior deltoid strengthening) 2. Posterior deltoid (prone horizontal abduction) 3. Pushup plus 4. Scapular punch 5. Shoulder elevation (shrug) 6. Seated row (TB) 7. Low trap row (TB 8. Upright row 9. Chair press (lat strength) 10. Side-lying (DB) or standing (TB) ER |
1. Maitland GH joint mobilizations: ** 2. Inferior glide 3. Anterior glide 4. Posterior glide 5. Long axis distraction 6. STM techniques†† |
NR | NR | 1. Postural exercises 6. Scapular retraction 7. Standing spinal extension |
| Benazzo (2014)99 | 80 days | 1. PROM 8. FLX, ABD, circumduction 2. AAROM |
NR | 1. Eccentric strengthening exercises | NR | NR | NR | 1. Sling & immobilization (duration NR) |
| Boorman (2014)123 | ≥3 mo | NR | 1. “Stretching exercises” |
1. “Strengthening exercises for the shoulder” | NR | NR | 1. Anti-inflammatory medications (optional) |
1. Education regarding physical condition and goals of the rehabilitation program |
| Güzelant (2014)117 ††† | ≥3 mo |
Phase 1 1. Pendulum(s) 2. AAROM ER 3. Pulley system 4. Supine FLX & ER AROM -Wall Walks |
Phase 1 1. Posterior Capsule Stretch 2. Overhead Stretch Using Pull-up Bar |
Phase 2A (2-3x/day; 1x5 reps) Band Color Progress 1x/2-3 weeks 1. IR/ER Therabands 2. Scapular Retraction Theraband 3. Abduction (Elbow 90 °) Theraband 4. Forward Press Theraband Phase 2B (2-3x/wk) 1. Wall Push-ups 2. Knee pushups 3. Shrug exercise 4. Shoulder press up from a chair 5. Scapular retraction (10 lbs; +3lb/wk) Phase 3 1. Continue with exercises (2-3x/wk) 2. Gradually reintegrate back into prior activities |
NR | 1. Hot Shower 2. Heating Pad Cryotherapy Post-Exercise |
1. NSAIDs (mean duration of use: 10 days; range: 5-10 d) |
1. Activity Modification 2. avoid the impingement arc >70 ° of elevation until symptoms improve 3. avoid “No Pain, No Gain” axiom of PT 4. Avoid & minimize pain |
| Kukkonen (2014/2015)52,125 | ≤ 6 mo (10 PT sessions) |
Phase 1: (0-6 wk) 1. “Improving glenohumeral motion and active scapular retraction” Phase 2: (6-12 wk) 1. “Static & dynamic exercises for the scapula & GH musculature were gradually increased” |
Phase 1: (0-6 wk) 1. “Improving GH motion & active scapular retraction” |
Phase 2: (6-12 wk) “Static & dynamic exercises for the scapula & GH musculature were gradually increased” Phase 3: (12 wk-6 mo) 1. “increased resistance & strength training up to 6 months” |
NR | NR | 1. Prior CS injection (G1: n = 39; 71%) (NOT administered as part of the study treatment) |
1. Written instructions 2. HEP |
| Collin (2015)106 | ≤24 mo (5 sessions) | 1. Relieve muscle tension | 1. “Relieve pain & muscle tension” muscles targeted:
-Pectoralis minor -Upper trapezius -Elevator scapulae |
1. “Strengthen muscles that stabilize & move the shoulder” 2. “Strength in the upper portion of the serratus anterior muscle” 3. “Strengthen intact rotator cuff muscles with special emphasis on the ER (teres minor) and coaptation of the deltoid” 4. “Ripped muscles that stabilize the GHJ but performing exercises with arm elevation” |
1. “Gentle manual recess entering techniques” |
NR | NR | 1. Recover proprioception and movement automaticity via neuro motor rehab targeting movement integration (emphasis on bilateral symmetrical movements & visualizing targets) |
| Lambers Heerspink (2015)49 | ≥ 12 wk |
Phase 1:(0-4 wk) 1. Maintain STJ mobility 2. PROM: -FLX/ABD -ER 3. circumduction Phase 2:(4-6 wk) 4. “Guided AROM” |
NR |
Phase 3:(6-12 wk) 1. AROM guided by pain 2. AROM coordination & stability training Phase 4: (>12 wk) 1. strength training 2. optimize mobility 3. coordination & stability training |
NR | NR | 1. CS Injection (≤ 3) 2. analgesic medication (optional) 4. NSAIDs 5. paracetamol 6. tramadol |
1. Education regarding physical condition & goals of the rehab program 2. Advice about ADLs 3. Postural correction |
| Baumer (2016)121 | 47.4 days (9.8 sessions) | 1. ROM (daily) | NR | 1. RC strengthening (daily) 2. STJ retraining (3x/wk) |
NR | NR | NR | 1. HEP |
| Christensen (2016)122 | 5 mo (12 PT sessions) | 3x/wk; ≤ 4x12 1. PROM: FLX (supine) 2. AAROM: FLX (supine) 3. AROM: ER (side-lying) |
NR | 3x/wk; ≤ 4x12 1. AAROM: FLX (semi-fowler's position) 2. AROM: FLX (standing) 3. AROM: ER (TB) |
NR | NR | NR | 1. Education: -physical condition -rationale of rehab program -how to manage pain related to exercise 2. HEP & training log |
| Miller (2016)111 | 12 wk |
Phase 1: 0-1 wk 1. PROM cane3 -ER & IR -supine FLX -standing EXT 2. AAROM cane -supine ER -standing ABD, FLX, EXT 3. wall walks |
Phase 2: 2-3 wk 1. cross body stretch 2. IR towel stretch 3. sleeper stretch |
Phase 1: 0-1 wk 1. isometric IR & ER at 0 ° 2. side-lying ER (pain-free ROM) 3. prone GH EXT with ER 4. scapular plane ABD 5. scapular retraction 6. manually resisted scapular movements Phase 2: 2-3 wk 1. ER & IR at 0 ° with TB 2. ER @90 ° with TB 3. subscapularis hug with TB 4. scapular plane ABD 5. prone Row into ER 6. prone T's (horizontal ABD at 90 °) 7. prone Y's (horizontal ABD at 120 °) 8. Serratus protraction with FLX 9. wall push-ups with plus 10. latissimus pull down 11. Rhythmic stabilization w/ manual resistance 12. bicep curl 13. triceps push down |
1. Cold therapy PRN | 1. HEP | ||
| Mischke (2016)100 | 13 PT sessions | 1. Shoulder (A)AROM | 1. Posterior GH stretch | 1. Rotator cuff isometrics 2. Rotator cuff isotonics 3. Scapular retraction 4. Bilateral GH ER 5. Dynamic hug 6. Pushup plus 7. PNF patterns (TB) |
1. Joint mobilizations -GH Joint -Spine CPAs (T1-6) -Sternoclavicular joint 2. Thoracic joint 3. mobilizations |
NR | NR | 1. “Functional retraining” 2. HEP 3. Education: Independent progression of strengthening exercises |
| Upadhyaya (2016)103 | NR | 1. “Supervised physical therapy” | 1. “Capsular stretching” | 1. “[Rotator] cuff strengthening” | NR | NR | NR | 1. HEP |
| Moosmayer (2017)112 | ≥ 3 mo. | “Physiotherapy” | “Physiotherapy” | “Physiotherapy” | “Physiotherapy” | NR | 1. “Analgesics” (n=1) 2. CS injection (n=1) |
1. Second bout of Physiotherapy with relapse of shoulder pain (n=7) |
AAROM, Active assisted range of motion; AROM, active range of motion; ABD, abduction; ADD, abduction; CPAs, central posterior to anterior joint mobilizations; CS, corticosteroid; CW, clockwise; CCW, counterclockwise; D1F, PNF D1 flexion (flexion, adduction, external rotation); D2F, PNF D2 flexion (flexion, abduction and external rotation); DB , dumbbell; EXT, extension; ER, external rotation; FLX, flexion; GH, glenohumeral; HEP, home exercise program; IR, internal rotation; min, minutes; mo, month; NSAID, non-steroid anti-inflammatory drug; NR, not reported; OT, occupational therapy; PT, physical therapy; PNF, proprioception neuromuscular facilitation; PRN, when necessary; PROM, Passive range of motion; reps, repetitions; RC, rotator cuff; STJ, scapulothoracic joint; STM, soft tissue mobilization; TB, thera-band; TENS, transcutaneous electrical nerve stimulation; wk, week(s); w/, with; w/o, without; *, aquatic therapy; †, non-surgical treatment was given on the basis of pre-established treatment goals in a non-standardized manner according to clinical findings and progress; ‡; included one of the following: Hyaluronic acid, 1% mepivacaine, or dexamethasone sodium phosphate; §, used together when night pain was intense; **, mobilizations parameters were 2-4 sets of 30 seconds with a frequency of 2-3 oscillations/second and a grade and specific direction of mobilization determined by the treating physical therapist; ††, soft tissue mobilization techniques were implemented at the discretion of the treating physical therapist and included muscle stretching, effleurage, friction and needing technique; ***, included supervised and/or home therapy: at 6 weeks follow-up subjects reported supervised therapy only (n=5), supervised and home therapy (n = 180) or home therapy only (n=41), average number of supervised visits: 7.99; †††, utilize the same rehabilitation program as Wirth (1997);
References
- 1.Merolla G Paladini P Saporito M Porcellini G. Conservative management of rotator cuff tears: literature review and proposal for a prognostic. Prediction Score. Muslec Lig Tendons J. 2011;1(1):12-19. [PMC free article] [PubMed] [Google Scholar]
- 2.Kim HM Teefey SA Zelig A Galatz LM Keener JD Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009;91(2):289-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sher JS Uribe JW Posada A Murphy BJ Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10-15. [DOI] [PubMed] [Google Scholar]
- 4.Teunis T Lubberts B Reilly BT Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg. 2014;23(12):1913-1921. [DOI] [PubMed] [Google Scholar]
- 5.Tempelhof S Rupp S Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8(4):296-299. [DOI] [PubMed] [Google Scholar]
- 6.Sambandam SN Khanna V Gul A Mounasamy V. Rotator cuff tears: An evidence based approach. World J Orthop. 2015;6(11):902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fehringer EV Sun J VanOeveren LS Keller BK Matsen FA 3rd. Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg. 2008;17(6):881-885. [DOI] [PubMed] [Google Scholar]
- 8.Yamaguchi K Tetro AM Blam O Evanoff BA Teefey SA Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199-203. [DOI] [PubMed] [Google Scholar]
- 9.Edwards P Ebert J Joss B Bhabra G Ackland T Wang A. Exercise rehabilitation in the non-operative management of rotator cuff tears: A review of the literature. Int J Sports Phys Ther. 2016;11(2):279-301. [PMC free article] [PubMed] [Google Scholar]
- 10.Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman's classic. J Shoulder Elbow Surg. 2000;9(2):163-168. [PubMed] [Google Scholar]
- 11.Lehman C Cuomo F Kummer FJ Zuckerman JD. The incidence of full thickness rotator cuff tears in a large cadaveric population. Bull Hosp Jt Dis. 1995;54(1):30-31. [PubMed] [Google Scholar]
- 12.Keener J Galatz L Stobbs-Cucchi G Patton R Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014;96(1):11-19. [DOI] [PubMed] [Google Scholar]
- 13.Hijioka A Suzuki K Nakamura T Hojo T. Degenerative change and rotator cuff tears. An anatomical study in 160 shoulders of 80 cadavers. Arch Orthop Trauma Surg. 1993;112(2):61-64. [DOI] [PubMed] [Google Scholar]
- 14.Gerber C Meyer DC Schneeberger AG Hoppeler H von Rechenberg B. Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: an experimental study in sheep. J Bone Joint Surg Am. 2004;86-A(9):1973-1982. [DOI] [PubMed] [Google Scholar]
- 15.Park JG Cho NS Song JH Baek JH Jeong HY Rhee YG. Rotator Cuff Repair in Patients over 75 Years of Age: Clinical Outcome and Repair Integrity. Clin Orthop Surg. 2016;8(4):420-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gumina S Carbone S Campagna V Candela V Sacchetti FM Giannicola G. The impact of aging on rotator cuff tear size. Musculoskelet Surg. 2013;97 Suppl 1:69-72. [DOI] [PubMed] [Google Scholar]
- 17.Abate M Schiavone C Di Carlo L Salini V. Prevalence of and risk factors for asymptomatic rotator cuff tears in postmenopausal women. Menopause. 2014;21(3):275-280. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto A Takagishi K Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116-120. [DOI] [PubMed] [Google Scholar]
- 19.Milgrom C Schaffler M Gilbert S van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77(2):296-298. [PubMed] [Google Scholar]
- 20.Brasseur JL Lucidarme O Tardieu M, et al. Ultrasonographic rotator-cuff changes in veteran tennis players: the effect of hand dominance and comparison with clinical findings. Eur Radiol. 2004;14(5):857-864. [DOI] [PubMed] [Google Scholar]
- 21.Liem D Buschmann VE Schmidt C, et al. The prevalence of rotator cuff tears: is the contralateral shoulder at risk? Am J Sports Med. 2014;42(4):826-830. [DOI] [PubMed] [Google Scholar]
- 22.Yamaguchi K Ditsios K Middleton WD Hildebolt CF Galatz LM Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699-1704. [DOI] [PubMed] [Google Scholar]
- 23.Ro KH Park JH Lee SH Song DI Jeong HJ Jeong WK. Status of the contralateral rotator cuff in patients undergoing rotator cuff repair. Am J Sports Med. 2015;43(5):1091-1098. [DOI] [PubMed] [Google Scholar]
- 24.Tashjian RZ Farnham JM Albright FS Teerlink CC Cannon-Albright LA. Evidence for an inherited predisposition contributing to the risk for rotator cuff disease. J Bone Joint Surg Am. 2009;91(5):1136-1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewis J Tennent T. How effective are diagnostic tests for the assessment of rotator cuff disease of the shoulder. Evidence Based Sports Med. 2007:327-360. [Google Scholar]
- 26.Gombera MM Sekiya JK. Rotator cuff tear and glenohumeral instability : a systematic review. Clin Orthop Relat Res. 2014;472(8):2448-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baumgarten KM Gerlach D Galatz LM, et al. Cigarette smoking increases the risk for rotator cuff tears. Clin Orthop Relat Res. 2010;468(6):1534-1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bishop JY Santiago-Torres JE Rimmke N Flanigan DC. Smoking Predisposes to Rotator Cuff Pathology and Shoulder Dysfunction: A Systematic Review. Arthroscopy. 2015;31(8):1598-1605. [DOI] [PubMed] [Google Scholar]
- 29.Carbone S Gumina S Arceri V Campagna V Fagnani C Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg. 2012;21(1):56-60. [DOI] [PubMed] [Google Scholar]
- 30.Yamamoto A Takagishi K Kobayashi T, et al. The impact of faulty posture on rotator cuff tears with and without symptoms. J Shoulder Elbow Surg. 2015;24(3):446-452. [DOI] [PubMed] [Google Scholar]
- 31.Gumina S Di Giorgio G Postacchini F Postacchini R. Subacromial space in adult patients with thoracic hyperkyphosis and in healthy volunteers. Chir Organi Mov. 2008;91(2):93-96. [DOI] [PubMed] [Google Scholar]
- 32.Ainsworth R Lewis JS. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br J Sports Med. 2007;41(4):200-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abboud JA Beason DP Soslowsky LJ. Emerging ideas: the effect of hypercholesterolemia on tendons. Clin Orthop Relat Res. 2012;470(1):317-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abboud JA Kim JS. The effect of hypercholesterolemia on rotator cuff disease. Clin Orthop Relat Res. 2010;468(6):1493-1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dougherty KA Dilisio MF Agrawal DK. Vitamin D and the immunomodulation of rotator cuff injury. J Inflamm Res. 2016;9:123-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mather RC 3rd Koenig L Acevedo D, et al. The societal and economic value of rotator cuff repair. J Bone Joint Surg Am. 2013;95(22):1993-2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bell JE. Repair of symptomatic rotator cuff tears after failed nonoperative treatment is cost-effective: commentary on an article by Richard C. Mather III, MD, et al. : “The societal and economic value of rotator cuff repair”. J Bone Joint Surg Am. 2013;95(22):e178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuye IO Jain NB Warner L Herndon JH Warner JJ. Economic evaluations in shoulder pathologies: a systematic review of the literature. J Shoulder Elbow Surg. 2012;21(3):367-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yeranosian MG Terrell RD Wang JC McAllister DR Petrigliano FA. The costs associated with the evaluation of rotator cuff tears before surgical repair. J Shoulder Elbow Surg. 2013;22(12):1662-1666. [DOI] [PubMed] [Google Scholar]
- 40.Kuhn J Dunn W Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22(10):1371-1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bunker T. Rotator cuff disease. Curr Orthop. 2002;16(3):223-233. [Google Scholar]
- 42.Seida JC le Blanc C Schouten JR, et al. Systematic review: nonoperative and operative treatments for rotator cuff tears [with consumer summary]. Ann Int Med. 2010;153(4):246-255. 2010. [DOI] [PubMed] [Google Scholar]
- 43.Huisstede BM Koes BW Gebremariam L Keijsers E Verhaar JA. Current evidence for effectiveness of interventions to treat rotator cuff tears. Man Ther. 2011;16(3):217-230. [DOI] [PubMed] [Google Scholar]
- 44.Downie BK Miller BS. Treatment of rotator cuff tears in older individuals: a systematic review. J Shoulder Elbow Surg. 2012;21(9):1255-1261. [DOI] [PubMed] [Google Scholar]
- 45.Ryosa A Laimi K Aarimaa V Lehtimaki K Kukkonen J Saltychev M. Surgery or conservative treatment for rotator cuff tear: a meta-analysis [with consumer summary]. Disabil Rehab. 2016;39(14):1357-1363. [DOI] [PubMed] [Google Scholar]
- 46.Grant HJ Arthur A Pichora DR. Evaluation of interventions for rotator cuff pathology: a systematic review. Journal of Hand Therapy. 2004;17(2):274-299. [DOI] [PubMed] [Google Scholar]
- 47.Moosmayer S Lund G Seljom U, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010;92(1):83-91. [DOI] [PubMed] [Google Scholar]
- 48.Moosmayer S Lund G Seljom U, et al. Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: a randomized controlled study in 103 cases with a five-year follow-up. J Bone Joint Surg Am. 2014;96(18):1504-1514. [DOI] [PubMed] [Google Scholar]
- 49.Lambers Heerspink FO van Raay J Koorevaar RCT, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015;24(8):1274-1281. [DOI] [PubMed] [Google Scholar]
- 50.Pedowitz RA Yamaguchi K Ahmad CS, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on: optimizing the management of rotator cuff problems. J Bone Joint Surg Am. 2012;94(2):163-167. [PubMed] [Google Scholar]
- 51.Kukkonen J Joukainen A Lehtinen J, et al. Treatment of non-traumatic rotator cuff tears: A randomised controlled trial with one-year clinical results. The bone & joint journal. 2014;96-b(1):75-81. [DOI] [PubMed] [Google Scholar]
- 52.Kukkonen J Joukainen A Lehtinen J, et al. Treatment of Nontraumatic Rotator Cuff Tears: A Randomized Controlled Trial with Two Years of Clinical and Imaging Follow-up. J Bone Joint Surg Am. 2015;97(21):1729-1737. [DOI] [PubMed] [Google Scholar]
- 53.Zanetti M Jost B Hodler J Gerber C. MR imaging after rotator cuff repair: full-thickness defects and bursitis-like subacromial abnormalities in asymptomatic subjects. Skeletal Radiol. 2000;29(6):314-319. [DOI] [PubMed] [Google Scholar]
- 54.Thomazeau H Boukobza E Morcet N Chaperon J Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997(344):275-283. [PubMed] [Google Scholar]
- 55.Mellado JM Calmet J Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. Am J Roentgenol. 2005;184(5):1456-1463. [DOI] [PubMed] [Google Scholar]
- 56.Bishop J Klepps S Lo IK Bird J Gladstone JN Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15(3):290-299. [DOI] [PubMed] [Google Scholar]
- 57.Klepps S Bishop J Lin J, et al. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32(7):1716-1722. [DOI] [PubMed] [Google Scholar]
- 58.Harryman DT 2nd Mack LA Wang KY Jackins SE Richardson ML Matsen FA 3rd. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73(7):982-989. [PubMed] [Google Scholar]
- 59.Gerber C Fuchs B Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505-515. [DOI] [PubMed] [Google Scholar]
- 60.Galatz LM Ball CM Teefey SA Middleton WD Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86A(2):219-224. [DOI] [PubMed] [Google Scholar]
- 61.Feng S Guo S Nobuhara K Hashimoto J Mimori K. Prognostic indicators for outcome following rotator cuff tear repair. J Orthop Surg (Hong Kong). 2003;11(2):110-116. [DOI] [PubMed] [Google Scholar]
- 62.Ladermann A Denard PJ Collin P. Massive rotator cuff tears: definition and treatment. Int Orthop. 2015;39(12):2403-2414. [DOI] [PubMed] [Google Scholar]
- 63.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Should Elb Surg. 2009;18(1):138-160. 2009. [DOI] [PubMed] [Google Scholar]
- 64.Seida JC LeBlanc C Schouten JR, et al. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010;153(4):246-255. [DOI] [PubMed] [Google Scholar]
- 65.Norris S Atkins D Bruening W, et al. Selecting Observational Studies for Comparing Medical Interventions. In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville (MD),2008. [PubMed] [Google Scholar]
- 66.Higgins JP Green S Scholten R. Maintaining reviews: updates, amendments and feedback. In: Wiley: Chichester, UK; 2008:31. [Google Scholar]
- 67.Chalmers I Enkin M Keirse MJ. Preparing and updating systematic reviews of randomized controlled trials of health care. Milbank Q. 1993;71(3):411-437. [PubMed] [Google Scholar]
- 68.Garner P Hopewell S Chandler J, et al. When and how to update systematic reviews: consensus and checklist. Br Med J. 2016;354:i3507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.The GRADE working group. Introduction: Grading the quality of evidence and the strength of recommendations. 2005; http://www.gradeworking group.org/intro.htm. Accessed July 3, 2015.
- 70.Moher D Liberati A Tetzlaff J Altman DG Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006-1012. [DOI] [PubMed] [Google Scholar]
- 71.Shamseer L Moher D Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Br Med J. 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- 72.Furlan AD Tomlinson G Jadad AA Bombardier C. Methodological quality and homogeneity influenced agreement between randomized trials and nonrandomized studies of the same intervention for back pain. J Clin Epidemiol. 2008;61(3):209-231. [DOI] [PubMed] [Google Scholar]
- 73.Shea BJ Bouter LM Peterson J, et al. External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS One. 2007;2(12):e1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shea BJ Grimshaw JM Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gagnier JJ Kellam PJ. Reporting and methodological quality of systematic reviews in the orthopaedic literature. J Bone Joint Surg Am. 2013;95(11):e771-777. [DOI] [PubMed] [Google Scholar]
- 76.Higgins JP Altman DG Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Maher CG Sherrington C Herbert RD Moseley AM Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713-721. [PubMed] [Google Scholar]
- 78.Khan KS Ter Riet G Glanville J Sowden AJ Kleinjnen J. Undertaking systematic reviews of research on effectiveness: CRD's guidance for carrying out or commissioning reviews. 2nd ed: NHS Centre for Reviews and Dissemination; 2001. [Google Scholar]
- 79.OCEBM Levels of Evidence Working Group. “The Oxford Levels of Evidence 2”. In: Oxford Centre for Evidence-Based Medicine.
- 80.American Physical Therapy Association. Clinical Practice Guidelines (CPGs): Getting Started. 2014; http://www.apta.org/EvidenceResearch/ImplementingEBP/CPGs/GettingStarted/. Accessed July 3, 2015.
- 81.Lenehan F Doody C. The benefit of physiotherapy in the conservative and surgical management of full-thickness rotator cuff tears: a systematic review. Irish Society of Chartered Physiotherapists (ISCP) Conference 2010. Physiotherapy Ireland. 2011;32(1):34-34. [Google Scholar]
- 82.Benazzo F Marullo M Pietrobono L. Supraspinatus rupture at the musculotendinous junction in a young woman. J Orthop Traumatol. 2014;15(3):231-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mischke JJ Emerson Kavchak AJ Courtney CA. Effect of sternoclavicular joint mobilization on pain and function in a patient with massive supraspinatus tear. Physiother Theory Pract. 2016;32(2):153-158. [DOI] [PubMed] [Google Scholar]
- 84.Palmer S. Aquatic physical therapy case report: Rehabilitation of a patient with a supraspinatus tear by aquatic therapeutic home exercises. J Aquatic Phys Ther. 1998;6(2):24-27. [Google Scholar]
- 85.Piccoli AS Hasson SM. Conservative management of a large rotator cuff tear to increase functional abilities: a case report. Physiotherapy Theory & Practice. 2004;20(3):201-208. [Google Scholar]
- 86.Upadhyaya S Pike AN Martin SD. 10-year follow-up of non-operatively treated full thickness rotator cuff tear. Sports Orthop Traumatol. 2016;32(1):67-72. [Google Scholar]
- 87.Ainsworth R. Physiotherapy rehabilitation in patients with massive, irreparable rotator cuff tears. Musculoskeletal Care. 2006;4(3):140-151. [DOI] [PubMed] [Google Scholar]
- 88.Bokor DJ Hawkins RJ Huckell GH Angelo RL Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993(294):103-110. [PubMed] [Google Scholar]
- 89.Collin PG Gain S Nguyen Huu F Ladermann A. Is rehabilitation effective in massive rotator cuff tears? Orthop Traumatol Surg Res. 2015;101(4 Suppl):S203-205. [DOI] [PubMed] [Google Scholar]
- 90.Goldberg BA Nowinski RJ Matsen FA 3rd. Outcome of nonoperative management of full-thickness rotator cuff tears. Clin Orthop Relat Res. 2001(382):99-107. [DOI] [PubMed] [Google Scholar]
- 91.Hawkins RH Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop Relat Res. 1995(321):178-188. [PubMed] [Google Scholar]
- 92.Itoi E Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1992(275):165-173. [PubMed] [Google Scholar]
- 93.Kijima H Minagawa H Nishi T Kikuchi K Shimada Y. Long-term follow-up of cases of rotator cuff tear treated conservatively. J Shoulder Elbow Surg. 2012;21(4):491-494. [DOI] [PubMed] [Google Scholar]
- 94.Miller RM Popchak A Vyas D, et al. Effects of exercise therapy for the treatment of symptomatic full-thickness supraspinatus tears on in vivo glenohumeral kinematics. J Shoulder Elbow Surg. 2016;25(4):641-649. [DOI] [PubMed] [Google Scholar]
- 95.Moosmayer S Gärtner AV Tariq R. The natural course of nonoperatively treated rotator cuff tears: an 8.8-year follow-up of tear anatomy and clinical outcome in 49 patients. J Shoulder Elbow Surg. 2017;26(4):627-634. [DOI] [PubMed] [Google Scholar]
- 96.Tanaka M Itoi E Sato K, et al. Factors related to successful outcome of conservative treatment for rotator cuff tears. Ups J Med Sci. 2010;115(3):193-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wirth MA Basamania C Rockwood CA Jr. Nonoperative management of full-thickness tears of the rotator cuff. Orthop Clin North Am. 1997;28(1):59-67. [DOI] [PubMed] [Google Scholar]
- 98.Yamada N Hamada K Nakajima T Kobayashi K Fukuda H. Comparison of conservative and operative treatments of massive rotator cuff tears. Tokai J Exp Clin Med. 2000;25(4-6):151-163. [PubMed] [Google Scholar]
- 99.Levy O Mullett H Roberts S Copeland S. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elbow Surg. 2008;17(6):863-870. [DOI] [PubMed] [Google Scholar]
- 100.Guzelant AY Sarifakioglu AB Gonen AK, et al. Massive retracted irreparable rotator cuff tears: what is the effect of conservative therapy? Turk J Geriatri. 2014;17(3):234-241. [Google Scholar]
- 101.Baydar M Akalin E El O, et al. The efficacy of conservative treatment in patients with full-thickness rotator cuff tears. Rheumatol Int. 2009;29(6):623-628. [DOI] [PubMed] [Google Scholar]
- 102.Lunn JV Castellanos-Rosas J Tavernier T Barthelemy R Walch G. A novel lesion of the infraspinatus characterized by musculotendinous disruption, edema, and late fatty infiltration. J Shoulder Elbow Surg. 2008;17(4):546-553. [DOI] [PubMed] [Google Scholar]
- 103.Vad VB Warren RF Altchek DW O'Brien SJ Rose HA Wickiewicz TL. Negative prognostic factors in managing massive rotator cuff tears. Clin J Sport Med. 2002;12(3):151-157. [DOI] [PubMed] [Google Scholar]
- 104.Baumer TG Chan D Mende V, et al. Effects of rotator cuff pathology and physical therapy on in vivo shoulder motion and clinical outcomes in patients with a symptomatic full-thickness rotator cuff tear. Orthop J Sports Med. 2016;4(9):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Christensen BH Andersen KS Rasmussen S Andreasen EL Nielsen LM Jensen SL. Enhanced function and quality of life following 5 months of exercise therapy for patients with irreparable rotator cuff tears - an intervention study. BMC Musculoskelet Disord. 2016;17:252-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Boorman RS More KD Hollinshead RM, et al. The rotator cuff quality-of-life index predicts the outcome of nonoperative treatment of patients with a chronic rotator cuff tear. J Bone Joint Surg Am. 2014;96(22):1883-1888. [DOI] [PubMed] [Google Scholar]
- 107.Krischak G Gebhard F Reichel H, et al. A prospective randomized controlled trial comparing occupational therapy with home-based exercises in conservative treatment of rotator cuff tears. J Shoulder Elbow Surg. 2013;22(9):1173-1179. [DOI] [PubMed] [Google Scholar]
- 108.Kukkonen J Joukainen A Lehtinen J, et al. Treatment of non-traumatic rotator cuff tears: A randomised controlled trial with one-year clinical results. Bone Joint J. 2014;96-b(1):75-81. [DOI] [PubMed] [Google Scholar]
- 109.Shibata Y Midorikawa K Emoto G Naito M. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. J Shoulder Elbow Surg. 2001;10(3):209-216. [DOI] [PubMed] [Google Scholar]
- 110.Ainsworth R Lewis J Conboy V. A prospective randomized placebo controlled clinical trial of a rehabilitation programme for patients with a diagnosis of massive rotator cuff tears of the shoulder. Shoulder & Elbow. 2009;1(1):55-60. [Google Scholar]
- 111.Gialanella B Prometti P. Effects of corticosteroids injection in rotator cuff tears. Pain medicine (Malden, Mass). 2011;12(10):1559-1565. [DOI] [PubMed] [Google Scholar]
- 112.Hegedus EJ Cook C Brennan M Wyland D Garrison JC Driesner D. Vascularity and tendon pathology in the rotator cuff: a review of literature and implications for rehabilitation and surgery. Br J Sports Med. 2010;44(12):838-847. [DOI] [PubMed] [Google Scholar]
- 113.Goutallier D Postel JM Bernageau J Lavau L Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994(304):78-83. [PubMed] [Google Scholar]
- 114.Kim HM Dahiya N Teefey SA, et al. Location and initiation of degenerative rotator cuff tears: an analysis of three hundred and sixty shoulders. J Bone Joint Surg Am. 2010;92(5):1088-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Belangero PS Ejnisman B Arce G. A review of rotator cuff classifications in current use. In: Shoulder Concepts 2013: Consensus and Concerns. Springer; 2013:5-13. [Google Scholar]
- 116.Calvo E. ISAKOS Classification System for Rotator Cuff Tears. In: Shoulder Concepts 2013: Consensus and Concerns. Springer; 2013:15-23. [Google Scholar]
- 117.DeOrio JK Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66(4):563-567. [PubMed] [Google Scholar]
- 118.Kraemer WJ Kent A Cafarelli E, et al. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687-708. [DOI] [PubMed] [Google Scholar]
- 119.Hollinshead RM Mohtadi NG Vande Guchte RA Wadey VM. Two 6-year follow-up studies of large and massive rotator cuff tears: comparison of outcome measures. J Shoulder Elbow Surg. 2000;9(5):373-381. [DOI] [PubMed] [Google Scholar]
- 120.Koubâa S Ben Salah FZ Lebib S Miri I Ghorbel S Dziri C. Traitement conservateur des ruptures transfixiantes de la coiffe des rotateurs. Étude prospective ouverte. À propos de 24 patients. Annales de Réadaptation et de Médecine Physique. 2006;49(2):62-67. [DOI] [PubMed] [Google Scholar]
- 121.Heers G Anders S Werther M Lerch K Hedtmann A Grifka J. [Efficacy of home exercises for symptomatic rotator cuff tears in correlation to the size of the defect]. Sportverletz Sportschaden. 2005;19(1):22-27. [DOI] [PubMed] [Google Scholar]
- 122.Maman E Harris C White L Tomlinson G Shashank M Boynton E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91(8):1898-1906. [DOI] [PubMed] [Google Scholar]
- 123.Harris JD Pedroza A Jones GL. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med. 2012;40(2):359-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Safran O Schroeder J Bloom R Weil Y Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39(4):710-714. [DOI] [PubMed] [Google Scholar]
- 125.Khan KM Scott A. Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43(4):247-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589-604. [DOI] [PubMed] [Google Scholar]
- 127.Kim IB Kim MW. Risk Factors for Retear After Arthroscopic Repair of Full-Thickness Rotator Cuff Tears Using the Suture Bridge Technique: Classification System. Arthroscopy. 2016;32(11):2191-2200. [DOI] [PubMed] [Google Scholar]
- 128.Lee YS Jeong JY Park CD Kang SG Yoo JC. Evaluation of the Risk Factors for a Rotator Cuff Retear After Repair Surgery. Am J Sports Med. 2017:363546517695234. [DOI] [PubMed] [Google Scholar]
- 129.Sherman SL Lyman S Koulouvaris P Willis A Marx RG. Risk factors for readmission and revision surgery following rotator cuff repair. Clin Orthop Relat Res. 2008;466(3):608-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Marx RG Koulouvaris P Chu SK Levy BA. Indications for surgery in clinical outcome studies of rotator cuff repair. Clin Orthop Relat Res. 2009;467(2):450-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kweon C Gagnier JJ Robbins CB Bedi A Carpenter JE Miller BS. Surgical Versus Nonsurgical Management of Rotator Cuff Tears: Predictors of Treatment Allocation. Am J Sports Med. 2015;43(10):2368-2372. [DOI] [PubMed] [Google Scholar]
- 132.Clement ND Nie YX McBirnie JM. Management of degenerative rotator cuff tears: a review and treatment strategy. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Boileau P Brassart N Watkinson DJ Carles M Hatzidakis AM Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J Bone Joint Surg Am. 2005;87A(6):1229-1240. [DOI] [PubMed] [Google Scholar]
- 134.Burkhart SS Barth JRH Richards DP Zlatkin MB Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(4):347-354. [DOI] [PubMed] [Google Scholar]
- 135.Beaudreuil J Bardin T Orcel P Goutallier D. Natural history or outcome with conservative treatment of degenerative rotator cuff tears. Joint Bone Spine. 2007;74(6):527-529. [DOI] [PubMed] [Google Scholar]
- 136.Lahteenmaki HE Hiltunen A Virolainen P Nelimarkka L. Repair of full-thickness rotator cuff tears is recommended regardless of tear size and age: A retrospective study of 2 patients. J Should Elbow Surg. 2007;16(5):586-590. [DOI] [PubMed] [Google Scholar]
- 137.Braun C Hanchard NC Batterham AM Handoll HH Betthäuser A. Prognostic Models in Adults Undergoing Physical Therapy for Rotator Cuff Disorders: Systematic Review. Phys Ther. 2016;96(7):961-971. [DOI] [PubMed] [Google Scholar]
- 138.Unruh KP Kuhn JE Sanders R, et al. The duration of symptoms does not correlate with rotator cuff tear severity or other patient-related features: a cross-sectional study of patients with atraumatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2014;23(7):1052-1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wolf BR Dunn WR Wright RW. Indications for repair of full-thickness rotator cuff tears. Am J Sports Med. 2007;35(6):1007-1016. [DOI] [PubMed] [Google Scholar]
- 140.Thompson WO Debski RE Boardman ND 3rd, et al. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24(3):286-292. [DOI] [PubMed] [Google Scholar]
- 141.Zhang AL Montgomery SR Ngo SS Hame SL Wang JC Gamradt SC. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29(4):623-629. [DOI] [PubMed] [Google Scholar]
- 142.Wheeless CR. Wheeless' textbook of orthopaedics. CR Wheeless, MD; 1996. [Google Scholar]
- 143.Minagawa H Yamamoto N Abe H, et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop. 2013;10(1):8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Garavaglia G Ufenast H Taverna E. The frequency of subscapularis tears in arthroscopic rotator cuff repairs: A retrospective study comparing magnetic resonance imaging and arthroscopic findings. Int J Should Surg. 2011;5(4):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Harryman DT 2nd Sidles JA Harris SL Matsen FA 3rd. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74(1):53-66. [PubMed] [Google Scholar]
- 146.Seitz AL McClure PW Finucane S Boardman ND Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clinical Biomech. 2011;26(1):1-12. [DOI] [PubMed] [Google Scholar]
- 147.Karas V Wang VM Dhawan A Cole BJ. Biomechanical factors in rotator cuff pathology. Sports Med Arthrosc. 2011;19(3):202-206. [DOI] [PubMed] [Google Scholar]
- 148.Longo UG Berton A Papapietro N Maffulli N Denaro V. Biomechanics of the rotator cuff: European perspective. In: Rotator Cuff Tear. Vol 57. Karger Publishers; 2012:10-17. [DOI] [PubMed] [Google Scholar]
- 149.Karas V Cole BJ Wang VM. Role of biomechanics in rotator cuff pathology: North American perspective. In: Rotator Cuff Tear. Vol 57. Karger Publishers; 2012:18-26. [DOI] [PubMed] [Google Scholar]
- 150.Via AG De Cupis M Spoliti M Oliva F. Clinical and biological aspects of rotator cuff tears. Muscl Lig Tendons J. 2013;3(2):70-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Nho SJ Yadav H Shindle MK Macgillivray JD. Rotator cuff degeneration: etiology and pathogenesis. Am J Sports Med. 2008;36(5):987-993. [DOI] [PubMed] [Google Scholar]
- 152.Morikawa D Itoigawa Y Nojiri H, et al. Contribution of oxidative stress to the degeneration of rotator cuff entheses. J Shoulder Elbow Surg. 2014;23(5):628-635. [DOI] [PubMed] [Google Scholar]
- 153.Yuan J Murrell GA Wei AQ Wang MX. Apoptosis in rotator cuff tendonopathy. J Orthop Res. 2002;20(6):1372-1379. [DOI] [PubMed] [Google Scholar]
- 154.Cook JL Rio E Purdam CR Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? Br J Sports Med. 2016;50(19):1187-1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Funakoshi T Iwasaki N Kamishima T, et al. In vivo visualization of vascular patterns of rotator cuff tears using contrast-enhanced ultrasound. Am J Sports Med. 2010;38(12):2464-2471. [DOI] [PubMed] [Google Scholar]
- 156.Clark JM Harryman DT 2nd. Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74(5):713-725. [PubMed] [Google Scholar]
- 157.Charousset C Grimberg J Duranthon LD Bellaiche L Petrover D Kalra K. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008;24(1):25-33. [DOI] [PubMed] [Google Scholar]
- 158.Narasimhan R Shamse K Nash C Dhingra D Kennedy S. Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. 2016;40(5):975-979. [DOI] [PubMed] [Google Scholar]
- 159.Zaman SU Syed HM. Arthroscopic Repair of an Isolated Teres Minor Tear. A Case Report. 2016;6(2):e40. [DOI] [PubMed] [Google Scholar]
- 160.Itoi E. Rotator cuff tear: physical examination and conservative treatment. J Orthop Sci. 2013;18(2):197-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kikukawa K Ide J. The appearance of the teres minor muscle in rotator cuff tears. J Shoulder Elbow Surg.23(5):603. [DOI] [PubMed] [Google Scholar]
- 162.Tokish JM Alexander TC Jr. Implementation of a Comprehensive Orthopaedic Registry System. Instr Course Lect. 2016;65:593-599. [PubMed] [Google Scholar]
- 163.Mall NA Lee AS Chahal J, et al. An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy. 2013;29(2):366-376. [DOI] [PubMed] [Google Scholar]
- 164.Pedowitz RA Yamaguchi K Ahmad CS, et al. Optimizing the management of rotator cuff problems. J Amer Acad Orthop Surgeons. 2011;19(6):368-379. [DOI] [PubMed] [Google Scholar]
- 165.Neer CS 2nd Craig EV Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65(9):1232-1244. [PubMed] [Google Scholar]
- 166.Khan Y Nagy MT Malal J Waseem M. The Painful Shoulder: Shoulder Impingement Syndrome. Open Orthop J. 2013;7:347-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Scheuermann R Behrens P Egbers H Havemann D. Early functional treatment of the injured shoulder supported by an active shoulder bandage. Aktuelle Traumatol. 1991;21(2):58-63. [PubMed] [Google Scholar]
- 168.Ghroubi S Chaari M Elleuch H Guermazi M Baklouti S Elleuch MH. [Functional and quality of life outcome of non-operated rotator cuff tears]. Ann Readapt Med Phys. 2008;51(9):714-721. [DOI] [PubMed] [Google Scholar]
- 169.Carleton HA Webb ML. The case report in context. Yale J Biol Med. 2012;85(1):93. [PMC free article] [PubMed] [Google Scholar]