Abstract
Study Objectives
Earlier studies have linked neighborhood disadvantage with poor sleep outcomes. However, little is known about the association between changes in one’s neighborhood over time and night sleep and napping. In over 300000 middle-to-old aged Americans, we examined neighborhood socioeconomic status (SES) and change in neighborhood SES in relation to nocturnal sleep duration and napping.
Methods
Nocturnal sleep duration and daytime napping were self-reported at baseline (1995–1996). Participants also reported baseline residential addresses, which were linked to US censuses. We derived a neighborhood SES index using census variables and calculated the baseline level and change (1990–2000) in neighborhood SES. Multinomial logistic regression was used to estimate the associations between neighborhood SES over time and nocturnal sleep and napping.
Results
Lower baseline neighborhood SES was associated with short sleep, long sleep, and napping. When compared with the highest quintile of neighborhood SES, the lowest was associated with 46% and 72% increase in relative risk (RR) of reporting very short (< 5 hours) sleep, 28% and 19% higher RR of long (≥9 hours) sleep and 95% and 85% increase in long (≥1 hours) nap in men and women, respectively. Moreover, a decrease in neighborhood SES was associated with higher RR of reporting very short sleep in women; while an improvement in neighborhood SES was associated with an increase in RR of long sleep in men.
Conclusions
Neighborhood disadvantage and worsening neighborhood conditions were associated with unhealthy sleep behaviors. These results reinforce a growing literature on the potential importance of neighborhood context for understanding sleep health.
Keywords: sleep, napping, neighborhood socioeconomic status, social determinants of sleep, sleep health, neighborhood effects, health, sleep duration, total sleep time
Statement of Significance
Neighborhood environment may impact sleep behavior. However, there has been limited research on the link between change in neighborhoods over time and sleep duration. We examined neighborhood socioeconomic status (SES) in relation to night sleep and napping behavior in over 300 000 middle-to-old aged US adults. We found that a lower neighborhood SES at baseline was associated with short and long night sleep and daytime napping. Worsening neighborhood conditions were associated with short night sleep in women and improving conditions associated with long sleep in men. More research, especially prospective or natural experimental investigations, are needed to elucidate the associations between neighborhood environments over time and sleep health.
Introduction
Sleep deficiency is an important risk factor for a wide range of adverse health outcomes, including higher risks of cardiometabolic diseases, mental disorders, cancer, and all-cause mortality [1–4]. The American Academy of Sleep Medicine and the National Sleep Foundation have each issued consensus statements recommending a minimum of 7 hours of sleep for healthy adults [5, 6]. However, despite the well-established evidence supporting an important role of sleep in maintaining good health, about one-third of the US population fail to meet this guideline [7–9]. In addition to nighttime sleep deficiency, daytime naps (especially those >1 hour), have also been linked to various conditions, such as diabetes, cardiovascular disease, and higher all-cause mortality [10, 11]. Given the health implications of sleep, it is important to identify factors that are associated with higher risk of unhealthy sleep patterns.
Like many other health behaviors such as diet and physical activity, sleep and napping are shaped not only by biological and individual factors, but also by characteristics of the larger macroenvironment [12]. Recent studies have found that physical and social aspects of the neighborhood environment are associated with sleep deficiency. For example, exposure to ambient light and noise have an adverse effect on sleep [13, 14]. In addition, neighborhood disadvantage, including low social cohesion, poor safety, and high poverty, is associated with sleep deficiency [15–24]. Although these research findings support an association between neighborhood characteristics and sleep, all of the previous studies used one-time measurement of neighborhood environment and therefore were not able to capture dynamic neighborhood circumstances that may also influence health behaviors such as sleep. However, many neighborhoods are not static, and even neighborhoods that are similar in socioeconomic status (SES) at a single point in time may have had different histories and SES trajectories, which may have an important and independent impact on the health behavior and outcomes among residents. Although studies examining health effects of longitudinal trends of neighborhood conditions are rare, some earlier studies suggested that longitudinal neighborhood measures are stronger predictors of health disparities than single-time measures [25, 26]. In addition, studies focusing on changing neighborhood conditions may also provide evidence supporting the need for designing interventions that aim at improving disadvantaged neighborhoods. Finally, despite the growing body of evidence on adverse effects of excessive napping in the aging population, little is known about the differences in daytime napping behaviors across neighborhood characteristics.
To address these limitations in existing literature, we examined neighborhood SES in relation to nocturnal sleep and daytime napping in more than 300000 middle-to-old-aged Americans. Specifically, we tested the hypothesis that a lower neighborhood SES and a secular trend of worsening neighborhood SES are positively associated with unhealthy sleep behaviors, including insufficient sleep at night as well as long napping during the day. Conversely, we hypothesized that a high level of neighborhood SES and improvement in neighborhood SES over time are both negatively associated with insufficient and long napping.
Methods
Study population
The NIH-AARP Diet and Health Study is a large cohort study that recruited AARP members (age 50–71) in six US states (California, Florida, Louisiana, New Jersey, North Carolina, and Pennsylvania) and two metropolitan areas (Atlanta, Georgia, and Detroit, Michigan). Details of the study were reported previously [27]. In 1995–1996, 566399 participants completed the baseline questionnaire, in which they reported their residential address. Within 6 months of the baseline, a risk-factor questionnaire was mailed to the cohort and collected additional lifestyle information, including habitual sleep duration and napping. Of the 334905 participants who satisfactorily completed both questionnaires, we excluded those with no information on sleep or napping (N = 2678) or missing residential address (N = 1788). To avoid reverse causation in which the prior health history is a source of short sleep duration, we also excluded participants who reported a history or heart disease (N = 46352), stroke (N = 4270) and cancer (N = 67252), as well as those who rated their health as poor (N = 1918) at baseline. The final analytic cohort included 97890 women and 110647 men. The study was approved by the National Cancer Institute Special Studies Institutional Review Board.
Neighborhood SES
Baseline addresses were geocoded into geographical coordinates and linked to the 1990 and 2000 US Census at the census tract level. We applied an adapted version of the method developed by Messer et al [14]. and Major et al [28]. to generate an empirical index for neighborhood SES for both 1990 and 2000. In brief, we selected 14 census tract-variables (% total with less than high school education, % total unemployed, % unemployed men, % renter occupied housing units, % housing units vacant, median value of all owner occupied housing units, % household with income below poverty, % female headed HH with dependent children, % households with an income <$22500 [1990 census] or <$30000 [2000 census], % households on public assistance, and % households with no car, % non-Hispanic blacks, % residents 65 and above, and % in same residence since 1985 [1990 census] or 1995 [2000 census]). We performed principal component analysis (PCA) on these variables, stratified by state. We then assessed variables for inclusion using the two-step procedure: (1) a variable was first retained if it had a loading above 0.33 (cut-off point for the top 20% of all loadings) in any state; (2) a retained variable in step (1) was excluded if it had a loading in any state lower than 0.19 (cut-off point for the bottom 20% of all loadings). In total, we retained six variables: % total with less than high school education, % total unemployed, % households with income below poverty, % households with an income <$22500 (1990) or <$30000 (2000), % households on public assistance, and % households with no car. We re-ran the PCA for the whole baseline cohort using the retained variables alone and derived the SES index for each census tract by summarizing the PCA scores of the six variables for 1990 and 2000 separately. Distribution and loadings of census variables by tertiles of SES index are presented in Supplementary Table 1. We then calculated percentile rankings for the SES index in 1990 and 2000. Finally, neighborhood SES at baseline was measured by averaging the 1990 and 2000 percentiles, while change in neighborhood SES was measured by the difference in percentiles between the two time points.
Assessment of nocturnal sleep duration and napping
In the risk-factor questionnaire, participants were asked to report how many hours they spent “sleeping at night” or “napping during the day” in a “typical 24-hour period over the past 12 months”. They were asked to choose from “less than 5 hours”, “5 to 6 hours”, “7 to 8 hours” and “9 or more hours” for nocturnal sleep and from “none”, “less than 1 hour”, “1 to 2 hours”, “3 to 4 hours” and “5 or more hours” for napping. We combined the highest three categories of napping into one group (≥1 hours) to preserve statistical power.
Statistical analysis
Participants were divided in quintiles based on their baseline neighborhood SES (first quintile indicates the lowest SES while the fifth quintile indicates the highest [reference]). For change in neighborhood SES, we grouped participants into five categories based on percentile differences between 1990 and 2000: increase in SES by more than 10 percentile points, increase in SES by more than 2.5 but no more than 10 percentile points, increase or decrease in SES by 2.5 percentile points or less (reference), decrease in SES by more than 2.5 but no more than 10 percentile points, decrease in SES by more than 10 percentile points. To examine the association of nocturnal sleep duration and day napping with baseline or change in neighborhood SES, we used multinomial logistic regression models to calculate the relative risk ratios (RRR) and 95% confidence interval (CI). The models contained a four-category outcome variable for sleep duration (<5 hours, 5–6 hours, 7–8 hours [reference], ≥9 hours) or a three-category outcome variable for napping (none [reference], <1 hour, ≥1 hours). We adjusted several covariates as potential confounders, including age (50–54, 55–59, 60–64, 65–71), education (less than high school, high school, some college, college and higher), race and ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian, Pacific Islander, and American Indian, other), marital status (married, widowed, divorced or separated, never married) and state of residence (CA, FL, LA, NJ, NC, PA, GA, MI). Because nocturnal sleep and day napping can influence each other and may act as mediators for the associations with neighborhood SES, we additionally adjusted for napping (for analysis of sleep) and napping (for analysis of napping) in separate models. To assess the independent effects of baseline neighborhood SES and change in neighborhood SES between 1990 and 2000, we mutually adjusted these two variables for their respective analysis. Robust variance estimation is used for standard error estimation to account for clustering across census tracts [29]. In total, there were 17850 census tracts in our study and the median number of participants in each tract is 11 (interquartile range: 5–20). All analysis were performed using SAS 9.3 (SAS Institute, Cary, NC).
Results
Study characteristics by quintiles of baseline neighborhood SES index are presented in Table 1. When compared to participants in the highest quintile of neighborhood SES, those living in neighborhoods with lower SES were more likely to be female, but less likely to be white, have a college education, or be married. In general, higher neighborhood SES was associated with a healthier lifestyle, characterized by less current smoking, higher levels of physical activity, less TV viewing, higher score for Healthy Eating Index and lower body mass index (BMI). The prevalence of 7–8 hours of sleep and no napping was also higher among participants in high SES neighborhoods.
Table 1.
Study characteristics according to quintiles of baseline neighborhood SES (1995–1996) among participants in the National Institutes of Health-AARP Diet and Health Study
| Study characteristics | Baseline neighborhood SES, 1990–2000 | P-value | ||||
|---|---|---|---|---|---|---|
| Q1 (low SES) | Q2 | Q3 | Q4 | Q5 (high SES) | ||
| Age, mean (SD) | 61.9 (5.3) | 62.0 (5.4) | 61.9 (5.4) | 61.5 (5.4) | 61.2 (5.4) | <.0001* |
| Female, % | 52.8 | 48.6 | 46.9 | 44.1 | 39.8 | <.0001† |
| White, non-Hispanic, % | 84.5 | 94.2 | 95.5 | 95.6 | 96.1 | <.0001† |
| College and postcollege, % | 39.9 | 33.4 | 39.0 | 46.4 | 60.2 | <.0001† |
| Married, % | 57.7 | 64.3 | 66.1 | 69.9 | 75.9 | <.0001† |
| Current smoker, % | 13.2 | 11.7 | 10.9 | 9.5 | 7.4 | <.0001† |
| Physical activity ≥5 times/week, % | 18.8 | 19.6 | 19.5 | 20.2 | 20.8 | <.0001† |
| TV viewing ≤2 hour/day, % | 32.2 | 33.0 | 35.5 | 38.6 | 45.2 | <.0001† |
| Body mass index, kg/m2, mean (SD) | 27.4 (5.5) | 27.0 (5.2) | 26.8 (5.0) | 26.6 (4.9) | 26.2 (4.5) | <.0001* |
| alcohol consumption, g/day, median (IQR) | 1.1 (0, 7.1) | 1.4 (0, 9.9) | 1.9 (0.2, 11.5) | 2.5 (0.5, 12.8) | 3.7 (0.7, 15.1) | <.0001‡ |
| HEI-2005 total score, mean (SD) | 66.2 (11.7) | 66.8 (11.5) | 67.0 (11.4) | 67.3 (11.2) | 68.2 (10.7) | <.0001* |
| Self-reported health, excellent, % | 15.8 | 18.0 | 20.1 | 22.6 | 26.7 | <.0001† |
| Sleep duration, % | <.0001† | |||||
| <5 hours | 3.9 | 3.1 | 2.7 | 2.4 | 1.8 | |
| 5–6 hours | 35.0 | 31.9 | 31.6 | 30.9 | 29.0 | |
| 7–8 hours | 57.6 | 61.7 | 62.5 | 63.6 | 66.1 | |
| ≥9 hours | 3.5 | 3.4 | 3.2 | 3.1 | 3.1 | |
| Napping, % | <.0001† | |||||
| None | 47.5 | 49.9 | 52.3 | 55.4 | 59.7 | |
| <1 hour | 41.3 | 40.9 | 39.9 | 37.7 | 34.9 | |
| ≥1 hours | 11.3 | 9.2 | 7.8 | 6.9 | 5.4 | |
IQR, interquartile range.
*p-value was derived from one way ANOVA.
† p-value was derived from Chi-square test.
‡ p-value was derived from Kruskal–Wallis test.
We first examined the associations between individual-level sociodemographic factors, including race/ethnicity, education, and marital status and nocturnal sleep duration (Supplementary Table 2) and day napping (Supplementary Table 3). In both men and women, minority race and ethnicity, lower education levels and non-married status were associated with a higher relative risk of reporting short (<5 hours or 5–6 hours) versus normal (7–8 hours) sleep and long (≥1 hours) versus no napping. Long sleep (≥9 hours) was positively associated with being never married in women, and having a high school or lower education, as well as being divorced or separated, or never married in men.
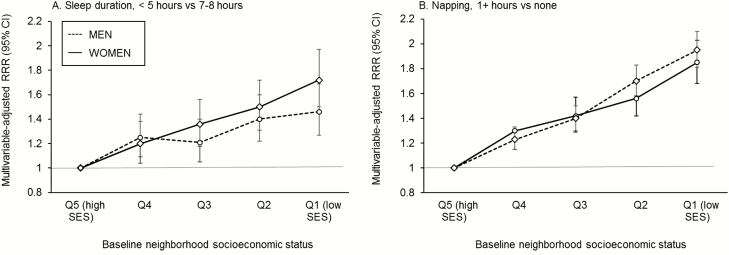
Next, we investigated baseline neighborhood SES in relation to nocturnal sleep duration (Figure 1, Supplementary Table 4) and day napping (Figure 1, Supplementary Table 5). After adjusting for multiple variables, lower neighborhood SES was associated with higher relative risk of reporting very short sleep, short sleep, long sleep, and napping in both men and women. When compared with the highest quintile of neighborhood SES, the lowest quintile was associated with 46% and 72% increase in relative risk of reporting very short (<5 hours) sleep in men and women, respectively (RRRQ1 vs Q5 [95% CI], 1.46 [1.27, 1.69] for men and 1.72 [1.50, 1.97] for women), 28% and 19% higher relative risk of long (≥9 hours) sleep (RRRQ1 vs Q5 [95% CI], 1.28 [1.14, 1.44] for men and 1.19 [1.06, 1.34] for women) and almost twofold increase in reporting long nap (RRRQ1 vs Q5 [95% CI], 1.95 [1.81, 2.10] for men and 1.85 [1.68, 2.03] for women). Results from models additionally adjusted for napping (for analysis on sleep) and sleep (for analysis on napping) had minimal impact on the results (Model 2 in Supplementary Tables 4 and 5).
Figure 1.
Multivariate association between baseline (1995–1996) neighborhood SES and (A) sleep duration and (B) napping. Baseline neighborhood SES is measured by average percentile rankings of neighborhood SES index between 1990 and 2000. Models were adjusted for age, race and ethnicity, education, marital status, state of residence and change in neighborhood SES.
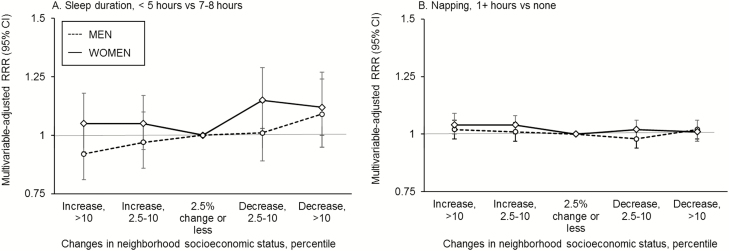
Finally, we examined the association between change in neighborhood SES and nocturnal sleep duration (Figure 2A, Supplementary Table 6) and day napping (Figure 2B, Supplementary Table 7). We found that when compared to women whose neighborhoods experienced little change in SES (less than 2.5 percentile points increase or decrease), a decrease in neighborhood SES of 2.5 percentile points or more between 1990 and 2000 was associated with a higher relative risk of reporting <5 hours sleep in women (RRR Q1 vs Q5 [95% CI], 1.15 [1.03, 1.29] for 2.5–10 percentile decrease and 1.12 [1.00, 1.27] for ≥10 percentile decrease). In men, this association was not statistically significant. Interestingly, an improvement in neighborhood SES was associated with 11% increase in relative risk of long sleep in men, but not in women. Change in neighborhood SES was not associated with napping. Again, additional adjustment for napping or sleep had little impact on the results.
Figure 2.
Multivariate association between changes in neighborhood socioeconomic status (1990–2000) and (A) sleep duration and (B) napping. Changes in neighborhood SES is expressed in difference in percentile ranking between 1990 and 2000. Increase in percentile indicates improved neighborhood SES, while decrease in ranking indicates worsened neighborhood SES. Models were adjusted for age, race and ethnicity, education, marital status, state of residence, and baseline neighborhood SES.
Discussion
In this large population of older US men and women, we found that lower baseline neighborhood SES was associated with short and long sleep at night as well as long napping during the day. Moreover, we found evidence suggesting that worsening neighborhood SES was associated with very short sleep duration in women while an increase in neighborhood SES was associated with long sleep duration in men.
Several earlier studies examined the relationship between various neighborhood characteristics and sleep in diverse populations. The majority of the studies focused on the neighborhood social environment, particularly neighborhood safety. A cross-sectional study in US Hispanic adults linked unsafe neighborhoods to short sleep, low sleep efficiency, and late sleep timing [18]. Similarly, among African Americans in the Jackson Heart Study, high neighborhood violence was also associated with shorter sleep duration and poorer sleep quality [21]. An international study using data from Mexico, Ghana, South Africa, India, China, and Russia found that respondents who felt safe in their neighborhoods reported better sleep outcomes [22]. Two recent cross-sectional studies in the Multi-Ethnic Study of Atherosclerosis Study (MESA) examined multiple aspects of the neighborhood social environment, and found that neighborhood disorder, low safety, and low social cohesion were associated with both self-reported and objectively-measured short sleep duration [16, 17]. Using the 2004 Survey of Texas Adults, a statewide probability sample of Texas adults, two studies reported that a higher perception of neighborhood disorder was associated with poor sleep quality [23, 24]. Studies on other aspects of neighborhood characteristics, including the physical environment and socioeconomic conditions were less consistent. An investigation of predominantly white adults in Wisconsin reported a poorer perception of neighborhood quality was correlated with worse sleep quality [15]. In the MESA study, DeSantis et al [16]. did not find an association between sleep and the physical environment and neighborhood SES after adjusting for multiple covariates. In addition, three studies used composite measures of neighborhood SES similar to that in our study and examined the relationship with sleep [16, 20, 21], but none of them reported a significant association, even in the Jackson Heart Study, in which social environment was significantly associated with sleep outcomes [21]. Finally, two recent studies of predominantly Hispanic populations did not find a relationship between various neighborhood characteristics and different sleep outcomes [30, 31]. The evidence suggests that the relationship between neighborhood SES and sleep is weaker, and most of the earlier studies only included hundreds to thousands of participants. With a much larger sample size, our study supplied new evidence supporting a role of disadvantaged neighborhood environment in sleep deficiencies.
Our study is the first to explore the relationship between neighborhood trajectories and sleep. Our findings suggest that the trajectories of neighborhood SES may have an additional association with sleep duration: even after adjusting for baseline SES, women who lived in a neighborhood with a deteriorating trajectory were more likely to report very short sleep (<5 hours) when compared to women living in more stable neighborhoods. Interestingly, an upward trajectory in neighborhood SES seemed to be associated with longer sleep in men. Although there has been limited research on change in neighborhood conditions and health, emerging evidence suggests that improvement in neighborhood conditions may lead to health benefits while worsening conditions are linked to adverse health outcomes. For example, a recent study by Powell-Wiley et al. found that an increase in neighborhood-level safety between 2003–2005 and 2010–2012 was associated with decreasing BMI over the same period in MESA participants [32], and an earlier investigation in the same population also reported a relationship between increase in neighborhood development and decrease or lower increase in BMI and waist circumference [33]. Our study supports a potentially important relationship between neighborhood change and health behaviors such as sleep. In addition, the potential impact of change in neighborhood SES was independent of the overall level of neighborhood SES, suggesting that neighborhood decline may have a unique impact on sleep. One of the potential mechanisms is through loss of social capital in neighborhoods with unstable, particularly worsening, conditions. As neighborhood conditions worsen, residence with more resources tend to move out, further contributing to lower neighborhood SES. Previous studies suggested that population loss and high resident turnover rate are linked to impaired social cohesion, informal social control, and increase in neighborhood crime [34], which can create a stressful environment that may lead to sleep deficiencies. However, due to the cross-sectional nature of our study and lack of information on residential histories, we were not able to directly examine the impact of neighborhood change over a period of time on sleep outcomes at a later time point. More prospective or natural experimental studies are needed to examine the role of neighborhood change on various health behaviors and outcomes. Findings from such research could provide valuable information for public health professionals to evaluate the potential of neighborhood interventions aimed at improving community health.
We found a strong positive association between low neighborhood SES and daytime napping, particularly long napping. A long period of daytime napping (>1 hour) is a well-established risk factor for multiple cardiometabolic conditions and premature death [10, 11], and the relationship is particularly strong in the older population [35]. Although the underlying mechanisms that link napping with adverse health outcomes remain unclear, some researchers postulated that napping, especially long napping, may be a marker of insufficient sleep and/or existing chronic conditions, particularly those associated with fatigue and inflammation [36, 37]. In the US population, napping is usually not a cultural habit but instead caused by daytime sleepiness and fatigue. Therefore, the relationship between neighborhood and napping in our study could be driven by nighttime sleep deficiency or underlying health problems. However, adjusting for sleep duration had little impact on the associations between neighborhood SES and napping, suggesting that sleep duration was unlikely to play a major role in this association. Regardless of the causes of long napping during daytime, given the role of napping as a predictor of morbidity and mortality, our results suggest that more attention is needed to monitor sleep, napping and health problems in disadvantaged neighborhoods.
Our study has several limitations. First, we used 1990 and 2000 census data to estimate neighborhood SES at baseline (1995/1996) as well as the trajectory of neighborhood SES between 1990 and baseline. Because neighborhood change may not be linear, our estimation may deviate from the actual neighborhood conditions experienced by the study participants. Second, we did not have the residential history of study participants and we were unable to examine whether length of residency played a role in the relationship between neighborhood SES and sleep. Third, sleep duration and napping were self-reported, and a previous study found that self-reported and measured sleep duration are only moderately correlated (correlation coefficient, 0.47) [38]. Interestingly, the study also found that people with short sleep were more likely to overestimate their sleep when compared to people with longer sleep. Together, these problems may result in misclassification of exposure and differential bias in observed results. However, the direction of the bias is towards the null and the real association could be larger than what was reported here. Moreover, we did not have information on other important aspects of sleep behavior, including sleep quality, sleep timing, and sleep disorders. For our napping variable, the questionnaire did not distinguish between daily nappers and occasional nappers, and therefore we were not able to assess whether they were differently associated with neighborhood environment. In addition, the Study did not collect information on income and other variables related to socioeconomic positions, and we had to rely on education level as the only measure on individual SES. As a result, the results could be affected by residual confounding due to incomplete control for individual-level factors. Finally, our study population was predominantly white and from a relatively high SES background. Therefore, the results may not be generalizable to other populations.
In conclusion, we found a consistent relationship between adverse neighborhood conditions and unhealthy sleep behaviors. Our study provides new evidence to the expanding literature supporting a role of neighborhood conditions in health behaviors and potentially health outcomes. We encourage more prospective or experimental design investigations on the potential effects of changing neighborhood conditions and sleep health, as they may provide stronger evidence to help establish a causal relationship as well as guide potential public health interventions.
Supplementary Material
Supplementary material is available at SLEEP online.
Funding
Partial salary support for L.H. was provided by the National Heart, Lung, and Blood Institute (NHLBI), R01-HL122460-01A1. Q.X. received no funding support for this study.
Notes
Conflict of interest statement. None declared.
References
- 1. Rangaraj VR, et al. . Association between sleep deficiency and cardiometabolic disease: implications for health disparities. Sleep Med. 2016;18:19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lo JC, et al. . Self-reported sleep duration and cognitive performance in older adults: a systematic review and meta-analysis. Sleep Med. 2016;17:87–98. [DOI] [PubMed] [Google Scholar]
- 3. Zhao H, et al. . Sleep duration and cancer risk: a systematic review and meta-analysis of prospective studies. Asian Pac J Cancer Prev. 2013;14(12):7509–7515. [DOI] [PubMed] [Google Scholar]
- 4. Cappuccio FP, et al. . Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Watson NF, et al. . Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hirshkowitz M, et al. . National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. [DOI] [PubMed] [Google Scholar]
- 7. Bin YS, et al. . Sleeping at the limits: the changing prevalence of short and long sleep durations in 10 countries. Am J Epidemiol. 2013;177(8):826–833. [DOI] [PubMed] [Google Scholar]
- 8. Ford ES, et al. . Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep. 2015;38(5):829–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liu Y, et al. . Prevalence of healthy sleep duration among adults–United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. [DOI] [PubMed] [Google Scholar]
- 10. Yamada T, et al. . Daytime napping and the risk of cardiovascular disease and all-cause mortality: a prospective study and dose-response meta-analysis. Sleep. 2015;38(12):1945–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hublin C, et al. . Napping and the risk of type 2 diabetes: a population-based prospective study. Sleep Med. 2016;17:144–148. [DOI] [PubMed] [Google Scholar]
- 12. Grandner MA. Sleep, health, and society. Sleep Med Clin. 2017;12(1):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chepesiuk R. Missing the dark: health effects of light pollution. Environ Health Perspect. 2009;117(1):A20–A27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Muzet A. Environmental noise, sleep and health. Sleep Med Rev. 2007;11(2):135–142. [DOI] [PubMed] [Google Scholar]
- 15. Hale L, et al. . Perceived neighborhood quality, sleep quality, and health status: evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Desantis AS, et al. . Associations of neighborhood characteristics with sleep timing and quality: the Multi-Ethnic Study of Atherosclerosis. Sleep. 2013;36(10):1543–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Johnson DA, et al. . The neighborhood social environment and objective measures of sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2017January 1;40(1): zsw016. doi:10.1093/sleep/zsw016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Simonelli G, et al. . Neighborhood factors as predictors of poor sleep in the Sueno Ancillary Study of the Hispanic community health study/study of Latinos. Sleep. 2017 January 1; 40(1): zsw025. doi:10.1093/sleep/zsw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Troxel WM, et al. . Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health Place. 2017;45:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fuller-Rowell TE, et al. . Racial disparities in sleep: the role of neighborhood disadvantage. Sleep Med. 2016;27–28:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnson DA, et al. . The social patterning of sleep in African Americans: associations of socioeconomic position and neighborhood characteristics with sleep in the Jackson Heart Study. Sleep. 2016;39(9):1749–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hill TD, et al. . Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med. 2016;18:56–60. [DOI] [PubMed] [Google Scholar]
- 23. Hale L, et al. . Does sleep quality mediate the association between neighborhood disorder and self-rated physical health?Prev Med. 2010;51(3–4):275–278. [DOI] [PubMed] [Google Scholar]
- 24. Hill TD, et al. . Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place. 2009;15(4):1006–1013. [DOI] [PubMed] [Google Scholar]
- 25. Do DP. The dynamics of income and neighborhood context for population health: do long-term measures of socioeconomic status explain more of the black/white health disparity than single-point-in-time measures?Soc Sci Med. 2009;68(8):1368–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sheehan CM, et al. . Long-term neighborhood poverty trajectories and obesity in a sample of California mothers. Health Place. 2017;46:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schatzkin A, et al. . Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125. [DOI] [PubMed] [Google Scholar]
- 28. Major JM, et al. . Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PLoS One. 2010;5(11):e15538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hosmer DW, et al. . Applied Logistic Regression. 2nd ed New York: Wiley; 2000. [Google Scholar]
- 30. Johnson DA, et al. . The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Health. 2015;1(3):148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chambers EC, et al. . Sleep and the housing and neighborhood environment of urban Latino adults living in low-income housing: The AHOME Study. Behav Sleep Med. 2016;14(2):169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Powell-Wiley TM, et al. . Associations of neighborhood crime and safety and with changes in body mass index and waist circumference: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2017;186(3):280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hirsch JA, et al. . Built environment change and change in BMI and waist circumference: Multi-ethnic Study of Atherosclerosis. Obesity (Silver Spring). 2014;22(11):2450–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kirk DS, et al. . Neighborhood change and crime in the modern metropolis. Crime Justice. 2010;39:441–502. [Google Scholar]
- 35. Leng Y, et al. . Daytime napping and the risk of all-cause and cause-specific mortality: a 13-year follow-up of a British population. Am J Epidemiol. 2014;179(9):1115–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Faraut B, et al. . Napping: a public health issue. From epidemiological to laboratory studies. Sleep Med Rev. 2017;35:85–100. [DOI] [PubMed] [Google Scholar]
- 37. Mantua J, et al. . Exploring the nap paradox: are mid-day sleep bouts a friend or foe?Sleep Med. 2017;37:88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lauderdale DS, et al. . Self-reported and measured sleep duration: how similar are they?Epidemiology. 2008;19(6):838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.