Significance
In the past few years, references to the opioid epidemic, drug poisonings, and associated feelings of despair among Americans, primarily working-class whites, have flooded the media, and related patterns of mortality have been of increasing interest to social scientists. Yet, despite recurring references to distress or despair in journalistic accounts and academic studies, there has been little analysis of whether psychological health among American adults has worsened over the past two decades. Here, we use data from national samples of adults in the mid-1990s and early 2010s to demonstrate increasing distress and declining well-being that was concentrated among low-socioeconomic-status individuals but spanned the age range from young to older adults.
Keywords: despair, psychological distress, psychological well-being, mental health, socioeconomic status
Abstract
Although there is little dispute about the impact of the US opioid epidemic on recent mortality, there is less consensus about whether trends reflect increasing despair among American adults. The issue is complicated by the absence of established scales or definitions of despair as well as a paucity of studies examining changes in psychological health, especially well-being, since the 1990s. We contribute evidence using two cross-sectional waves of the Midlife in the United States (MIDUS) study to assess changes in measures of psychological distress and well-being. These measures capture negative emotions such as sadness, hopelessness, and worthlessness, and positive emotions such as happiness, fulfillment, and life satisfaction. Most of the measures reveal increasing distress and decreasing well-being across the age span for those of low relative socioeconomic position, in contrast to little decline or modest improvement for persons of high relative position.
Two interrelated recent trends among American adults have caught the attention of social scientists. One is the steady increase since the late 1990s in substance abuse epitomized by the opioid epidemic (1). This rise has been attributed to changes in prescription practices, aggressive marketing by pharmaceutical firms, nonmedical uses of opioids, and black market dissemination of drugs that are cheaper yet more toxic than prescription opioids (1, 2). The prevalence of alcohol use and related disorders appears to have increased substantially over a similar period, although the evidence is less consistent than for opioid use (3, 4). The second trend has been stagnation, or in some instances increases, in death rates among American adults since the late 1990s, particularly middle-aged whites and persons of low socioeconomic status (5–7). These changes in mortality likely resulted in no small part from the upsurge in substance abuse, as reflected by increases in deaths from drug and alcohol poisonings, suicide, and liver diseases over this timeframe.
Both of these trends have raised concerns about a potential deterioration in the mental health of Americans, as underscored by the now-popularized term “deaths of despair” to describe the upturn in drug- and alcohol-related deaths and suicide (8–10). Researchers have expended considerable effort to examine these worrisome patterns in cause-specific mortality and their social and economic underpinnings (6, 7, 11). However, scholars have failed to undertake a broad examination of the psychological health of Americans, one that goes beyond assessments of distress and depression, to determine whether “despair” has become more widespread in recent years. In this paper, we provide insights into this timely, yet underresearched, question.
The issue is admittedly complicated by the absence of established scales to measure despair or even an agreed-upon definition. [We are aware of only two attempts to measure despair. One measure was developed to capture regret and hopelessness at the end of life (12, 13) and the other, the “behavioral ‘despair’ test,” to identify potential antidepressants by forcing rats to remain afloat in a small space (14). Neither measure is appropriate for the present study.] Our approach is to assess changes since the mid-1990s in psychological measures that we believe relate to layman notions of despair and that are highly relevant to ongoing discussions about substance use and associated increases in mortality. Psychologists and other social scientists have increasingly recognized that mental health is far more than the absence of particular pathologies; positive and negative emotions are distinct and essential dimensions of mental well-being rather than simply polar opposites (15–17). Furthermore, there are two overlapping but distinct philosophies of well-being: The hedonic approach centers on happiness or pleasure, whereas the eudaimonic approach focuses on self-actualization (18, 19). Thus, we base our analysis on an extensive set of mental health measures that capture both psychological distress and well-being. Psychological distress is assessed by measures of negative affect and major depression. Well-being is evaluated by two measures of hedonic well-being (positive affect and life satisfaction) and two measures of eudaimonic well-being (psychological well-being and social well-being). Of particular importance for our examination of trends is that all measures derive from comparable sets of questions in two periods that cover the timeframe of interest.
Our objective is twofold. The first is to determine whether mental health has deteriorated since the mid-1990s. The second goal is to examine whether the observed changes are concentrated in the groups most likely to have experienced declines or stagnation in survival over this time span, namely non-Latino whites and persons of low income or little education (20, 21). Researchers have raised concerns that mortality increases among the less educated may simply reflect compositional changes: Individuals with low levels of schooling are a smaller and more disadvantaged group today than their counterparts were in the mid-1990s (22, 23). Because of this potential selection bias, we assess socioeconomic status (SES) with a composite measure that takes into account education, occupation, income, and wealth of the respondent as well as the spouse or partner if married; the measure is calculated as a percentile rank in the SES distribution, reflecting relative rather than absolute status.
We base our assessments on the two cross-sectional waves of the Midlife in the United States (MIDUS) study. Because MIDUS was developed to improve our understanding of factors that underlie the well-being of American adults, it collected an extensive set of measures of psychological and social health. MIDUS conducted interviews with independent national samples of adults in 1995 to 1996 and again in 2011 to 2014, spanning closely the period of rising substance abuse. We restrict the main analysis to non-Latino whites (n = 4,627 for the combined samples) not only because this group is most frequently implicated in concerns about rising premature mortality and despair but also because of sample size considerations.
Results
Descriptive statistics for the analysis variables indicate that respondents ranged in age between 24 and 76 and slightly below half of the sample was male (SI Appendix, Table S1). Mean values for the six mental health measures are very similar between the two waves, which, as shown later, is largely a result of counteracting changes at the low and high ends of the SES distribution.
Estimated coefficients from the regression models (logit models for the distress outcomes and linear models for the remaining outcomes) are presented in Table 1. Of central interest is the coefficient for survey wave, which reveals whether mental health worsened between 1995 to 1996 and 2011 to 2014 for those in the bottom percentile of the SES distribution. The interaction term between SES and survey wave, which captures the extent to which changes in mental health varied across the SES spectrum, is also of primary importance. Because of positive skewness in the distributions, we dichotomized the two outcomes of psychological distress so that the value of 1 denotes high distress for both negative affect and depressive symptoms. The remaining four outcomes are continuous standardized variables (mean 0, SD 1), with higher values denoting greater well-being.
Table 1.
Coefficients from models predicting psychological distress and well-being, pooled data from MIDUS wave 1 (1995 to 1996) and refresher cohort (2011 to 2014), non-Latino whites (n = 4,627)
| Outcome | High negative affect | Major depression | Positive affect† | Life satisfaction† | Psychological well-being† | Social well-being† |
| Male (ref., female) | −0.284** | −0.647*** | 0.069* | −0.053 | −0.016 | −0.027 |
| (−0.478, −0.090) | (−0.859, −0.436) | (0.002, 0.136) | (−0.118, 0.012) | (−0.082, 0.050) | (−0.091, 0.036) | |
| Age − 40 | −0.006 | −0.032** | 0.004 | 0.007* | −0.006 | 0.002 |
| (−0.024, 0.011) | (−0.051, −0.012) | (−0.003, 0.011) | (0.000, 0.013) | (−0.012, 0.000) | (−0.005, 0.009) | |
| (Age − 40)2 | −0.001** | −0.001** | 0.000*** | 0.001*** | 0.000*** | −0.000 |
| (−0.001, −0.000) | (−0.001, −0.000) | (0.000, 0.001) | (0.000, 0.001) | (0.000, 0.001) | (−0.000, 0.000) | |
| SES‡ | −1.551*** | −1.210*** | 0.432*** | 0.674*** | 1.046*** | 1.078*** |
| (−2.017, −1.085) | (−1.699, −0.722) | (0.268, 0.596) | (0.515, 0.832) | (0.888, 1.204) | (0.919, 1.238) | |
| SES‡ × (age − 40) | 0.005 | 0.028 | −0.009 | −0.011* | −0.003 | 0.005 |
| (−0.024, 0.034) | (−0.002, 0.059) | (−0.019, 0.000) | (−0.020, −0.002) | (−0.012, 0.006) | (−0.004, 0.015) | |
| 2011–2014 (ref., 1995–1996) | 0.655** | 0.335 | −0.317** | −0.338*** | −0.207* | −0.102 |
| (0.234, 1.076) | (−0.114, 0.784) | (−0.512, −0.122) | (−0.532, −0.143) | (−0.391, −0.024) | (−0.281, 0.078) | |
| 2011–2014 × (age − 40) | 0.000 | 0.009 | −0.001 | −0.004 | 0.004 | −0.001 |
| (−0.015, 0.015) | (−0.008, 0.025) | (−0.006, 0.005) | (−0.009, 0.001) | (−0.001, 0.009) | (−0.006, 0.005) | |
| 2011–2014 × SES‡ | −0.869* | −0.655 | 0.407** | 0.498*** | 0.132 | 0.169 |
| (−1.588, −0.150) | (−1.404, 0.094) | (0.142, 0.671) | (0.234, 0.762) | (−0.120, 0.383) | (−0.077, 0.415) | |
| Constant | −0.588*** | −0.699*** | −0.330*** | −0.406*** | −0.520*** | −0.551*** |
| (−0.873, −0.304) | (−0.993, −0.406) | (−0.443, −0.218) | (−0.520, −0.292) | (−0.630, −0.411) | (−0.657, −0.445) |
***P < 0.001, **P < 0.01, *P < 0.05.
Note: Models for binary outcomes (i.e., negative affect and major depression) are fit with logistic regression, while all other outcomes are fit using linear regression; 95% confidence intervals are shown in parentheses below the coefficient. ref, reference group.
Standardized (mean 0, SD 1) to better compare effect size.
SES represents percentile rank, which has been rescaled to range from 0 (1st percentile) to 1 (99th percentile). Thus, a one-unit effect represents the difference between a person in the bottom 1% and the top 1% of the SES continuum. The effects for any variables interacted with SES represent the effects for a person in the bottom 1% of SES.
We anticipate opposite signs in the regression coefficients between the two distress outcomes and the four well-being measures for SES, survey wave, and the interaction between SES and survey wave. The estimated coefficients for all six outcomes confirm this expectation. The coefficients for SES are always large, significant, and in the expected direction, signifying better mental health for those of higher SES. The main effects for survey wave consistently show a worsening of mental health for those at the lowest SES percentile, although coefficients are significant at P < 0.05 for only four of the outcomes (exceptions are depression and social well-being). The interaction term between SES and period is significant for negative affect, positive affect, and life satisfaction, indicating that deterioration in these mental health outcomes diminishes as SES increases.
Because of the inclusion of interaction terms, it is difficult to infer from the coefficients the extent to which mental health has declined over the 15+ y of interest, overall and by SES. In Table 2, we present the predicted values (proportions or Z scores) for relative SES at the 10th, 25th, 50th, 75th, and 90th percentiles in the two survey waves. The results highlight the social stratification of mental health: Higher SES is consistently associated with less distress and greater well-being. The effects are generally substantial. For example, at the second wave, 37% of low-SES individuals (10th percentile) are predicted to have high negative affect, in contrast to only 8% of high-SES individuals (90th percentile); for life satisfaction, psychological well-being, and social well-being, there is about a 1-SD difference between the low- and high-SES groups at the second wave (e.g., −0.55 − 0.38 = −0.93 for psychological well-being).
Table 2.
Predicted values for psychological distress and well-being, by SES percentile and survey wave, non-Latino whites
| Predicted proportion high | Predicted score | |||||||||||
| Negative affect | Major depression | Positive affect† | Life satisfaction† | Psychological well-being† | Social well-being† | |||||||
| SES percentile | 1995–1996 | 2011–2014 | 1995–1996 | 2011–2014 | 1995–1996 | 2011–2014 | 1995–1996 | 2011–2014 | 1995–1996 | 2011–2014 | 1995–1996 | 2011–2014 |
| 10th | 0.25 | 0.37 | 0.20 | 0.25 | −0.12 | −0.40 | −0.19 | −0.51 | −0.39 | −0.55 | −0.47 | −0.56 |
| 25th | 0.21 | 0.29 | 0.17 | 0.20 | −0.06 | −0.28 | −0.10 | −0.35 | −0.23 | −0.38 | −0.30 | −0.37 |
| 50th | 0.15 | 0.19 | 0.14 | 0.14 | 0.03 | −0.09 | 0.05 | −0.07 | 0.03 | −0.09 | −0.02 | −0.05 |
| 75th | 0.11 | 0.11 | 0.11 | 0.10 | 0.12 | 0.10 | 0.20 | 0.20 | 0.28 | 0.21 | 0.26 | 0.28 |
| 90th | 0.09 | 0.08 | 0.09 | 0.08 | 0.18 | 0.22 | 0.29 | 0.37 | 0.44 | 0.38 | 0.43 | 0.47 |
Note: based on coefficients from models shown in Table 1. Predicted values (probability for binary outcomes, Z score for continuous outcomes) are calculated by fixing survey wave (1995 to 1996, 2011 to 2014) and SES percentile (10th, 25th, 50th, 75th, 90th) at the specified values, while sex and age remain at the observed values in the sample.
Standardized (mean 0, SD 1) to better compare effect size.
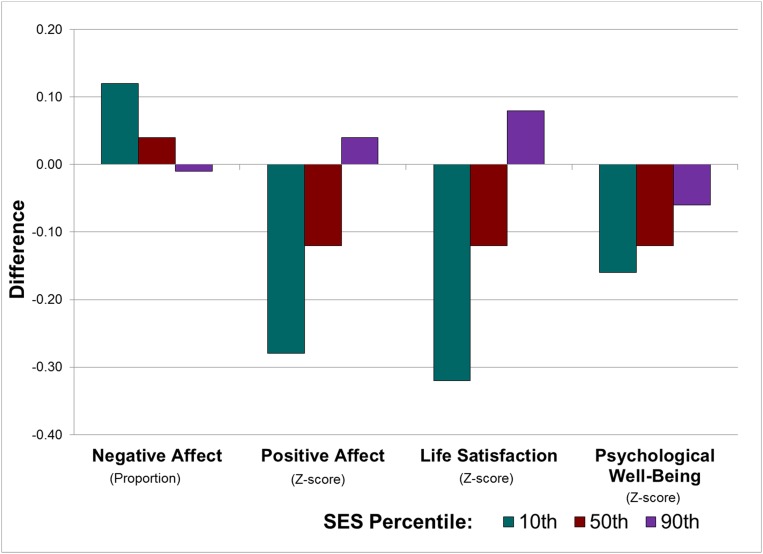
To further facilitate comparisons over time, the estimates in Table 2 are used to generate Fig. 1, which depicts the absolute difference in predicted values between the two waves for the 10th, 50th, and 90th percentiles of relative SES for the four outcomes with significant main effects for survey wave. The estimates underscore the substantial widening of SES disparities in mental health. For example, individuals at the 10th percentile experienced an increase in the probability of high negative affect of more than 0.10, a decrease in positive affect and life satisfaction of about 0.3 SD, and a decrease of 0.16 SD in psychological well-being between 1995 to 1996 and 2011 to 2014. By contrast, persons at the 90th percentile experienced virtually no change in negative affect, a small decline in psychological well-being, and improvements in positive affect and life satisfaction.
Fig. 1.
Difference (2011 to 2014 survey wave minus 1995 to 1996 survey wave) in predicted values, non-Latino whites. Note: based on predicted values shown in Table 2 (from models shown in Table 1). We subtract the predicted value for the survey wave fielded in 1995 to 1996 from the predicted value for the survey wave fielded in 2011 to 2014 to obtain the change (over time) in each outcome.
Because the models include interaction terms involving age, we estimated predictions for ages 30, 50, and 70 (SI Appendix, Fig. S1). The results for each age mirror those for the combined sample. That is, the estimated increases in distress and decreases in well-being have not been confined to those in midlife but instead appear to have been pervasive across the life course, a finding substantiated by the absence of significant interaction terms between period and age across all outcomes.
We repeated the analysis using the models in Table 1, except we replaced relative SES with the completed schooling categories used in many previous studies (5, 20, 22): high school graduate or lower, some college, and college graduate or higher (SI Appendix, Table S2). The estimates reveal similar patterns to those for the SES index. For example, the main effect for survey wave is significant (P < 0.05) for all outcomes except depression, and the predicted values (SI Appendix, Table S3) show the expected patterns by education and survey wave. However, only one outcome (life satisfaction) has a significant interaction term between survey wave and education, likely attributable to the crude categorization of education (e.g., the lowest category comprises 49% of the weighted sample in 1995 to 1996 and 39% in 2011 to 2014) in contrast to the fine gradation of relative SES (i.e., continuous values from the 1st to the 99th percentile).
The analysis so far has been restricted to non-Latino whites. We reestimated the models in Table 1 on the full sample of MIDUS respondents (n = 5,632), adding controls for race/ethnicity (SI Appendix, Table S4). The results remain essentially the same. Although no outcome is significantly different between Latinos and non-Latino whites, four outcomes (all but high negative affect and life satisfaction) indicate significantly better reported mental health for non-Latino blacks compared with non-Latino whites. Unfortunately, the sample sizes of these groups are too small to include interaction terms between race/ethnicity and survey wave (n = 196 for Latinos and n = 365 for non-Latino blacks in the pooled sample), a limitation which prevents us from examining whether the worsening of psychological health has indeed been most severe for whites.
Discussion
Despite a recent focus on widening socioeconomic disparities in life expectancy and associated trends in substance use and drug-related deaths, few scholars have explored whether these patterns are mirrored by changes in mental health (24). The few existing studies have focused on negative emotions, primarily distress and depression, and the findings have been inconsistent. Case and Deaton (5) used the Kessler (K6) questionnaire of psychological distress (equivalent to the measure of negative affect in MIDUS) and a simple question on “days mental health was not good” to suggest growing distress since the late 1990s, but their estimates were restricted to non-Latino whites aged 45 to 54. In a study that examined recent trends (2000 to 2015) in depression across a broad age range, Weinberger et al. (25) found an overall increase in the prevalence of depression among Americans, primarily at the youngest and oldest ages. In a separate study among adults 18 and older, which used both the K6 scale and a structured interview for depression, Mojtabai and Jorm (24) found little change in the prevalence of either psychological distress or depression over a similar timeframe (2001 to 2012).
In this paper, we address the issue more systematically and comprehensively, by drawing on a broader set of measures of psychological health derived from national samples of adults in the mid-1990s and the early 2010s. We go beyond measures of poor psychological health typically alluded to in discussions of deaths of despair to consider well-being alongside distress. The two measures of distress in this study (negative affect and depression) capture emotions such as sadness, hopelessness, worthlessness, loss of interest, and feeling down. By contrast, the two indexes of hedonic well-being (positive affect and life satisfaction) capture opposing emotions such as happiness, fulfillment, and satisfaction in life. The two measures of eudaimonic well-being (psychological and social well-being) were designed to examine meaning in life and self-realization, constructs that are often neglected in conventional measures but considered essential to an assessment of positive functioning (18, 26).
Overall, our results paint a picture of substantial social stratification in psychological health among American adults, one that has been widening as declines in mental health have occurred unevenly across the socioeconomic spectrum. Negative affect has increased among those of low SES with little change among those of high SES. In contrast, but consistent with earlier findings (24), we find no significant difference over time in depression. The two measures of hedonic well-being reveal the largest changes: substantial decreases since the late 1990s for persons of low SES, and modest improvements for those of high SES. Findings for psychological well-being show smaller decreases over time and a weaker differential by SES, whereas the estimates for social well-being are modest and insignificant. A possible explanation for the stronger findings for hedonic relative to eudaimonic well-being may be that hedonic measures more closely reflect the types of emotional setbacks, such as hopelessness, that have driven individuals to seek a drug-induced euphoria.
Previous studies and journalistic narratives have focused on despair in midlife in part because of the visibility of deaths of despair in age groups that typically experience low overall mortality. However, our findings do not suggest that heightened distress and diminished well-being are predominantly a midlife phenomenon. Rather, declines over time in mental health seem to have occurred throughout the age range evaluated here. These results are consistent with drug overdose death rates, which have been increasing among a broad age range, at least since the late 1990s (6, 27).
Despite our implicit linkage of these changes in mental health with time trends in opioid use and with discourse over deaths of despair, it is important to underscore that our findings are only suggestive of these relationships. We have not demonstrated a direct link between an individual experience of worsening mental health and increased substance use, nor could we do so with repeated cross-sectional data, because the direction of causality remains unclear. For example, it is plausible that the drug epidemic affected the psychological well-being of individuals as the epidemic ravaged families and friends and weakened the social and economic fabric of communities. The drug epidemic may also have reduced an individual’s income, assets, or occupational status, for example, as a result of loss of employment or a decline in earnings (28), because of high costs of drugs and treatment or through provision of support for loved ones.
As with all surveys, our findings may be biased by data problems. For example, information on income and assets was often missing from MIDUS, and such data are often plagued by response errors, owing to lack of knowledge, confusion among income categories, poor recall, and deliberate omission because of sensitivity of the information (29). It is also possible that respondents vary in their willingness to report mental health issues. What would be most problematic for this analysis is the occurrence of differential response over time by SES (e.g., if the threshold for acknowledging distress declined over time, perhaps in response to increased media attention to widening income inequality and other adverse conditions among the working class), but there is no way to evaluate whether this has occurred.
Future work could extend this study by examining whether—as the literature on deaths of despair suggests—these deleterious changes in mental health are most prevalent among non-Latino whites. Although small samples of minorities in MIDUS precluded such an analysis, we found that blacks fared significantly better than whites for four of six outcomes. Nevertheless, we are reluctant to conclude that blacks generally have better mental health than whites. Previous research underscores the absence of a simple ordering of racial and ethnic groups on overall mental health (30, 31). Moreover, many psychometric instruments have not been sufficiently validated across racial and ethnic populations, suggesting that racial differences may at least partly reflect variations in how individuals express feelings or perceive their mental state (31). We are also hesitant to suggest that mental health could account for the observed racial difference in drug use or drug-related mortality. Although the media have repeatedly called attention to the higher rates of opioid use among whites, drug-related mortality rates have surged since 2010 among non-Latino blacks (27, 32). Furthermore, the racial differential in substance abuse likely results at least in part from unequal access to drugs, a probable explanation for higher prescription opioid use among whites.
Another avenue for future research could be an exploration of sex differences in distress and well-being. Previous work has shown that drug overdose deaths have increased steadily for both men and women since the late 1990s, more so in absolute terms for men (6, 27). In addition, notable sex differences in cause-specific mortality trends among whites (6) may relate to sex-specific changes in mental health.
Researchers have been struggling to understand why Americans, particularly whites of low SES, have experienced rising rates of deaths of despair. Easier access to opioids may not be a sufficient explanation, although increased availability undoubtedly plays an important role. And the answer is unlikely to rest with simple economic explanations such as short-term declines in employment or wages. Researchers have speculated that the explanation involves complex social and economic transitions that have emerged over recent decades, including increasing income inequality and wage stagnation for the working class; long-term deterioration in employment opportunities that have led to intergenerational decline in economic security; reduction in stable marriages and cohabitating unions; increasing work–family strain; and weakening interactions within communities and associated social isolation (7, 33–35). Unfortunately, evaluation of these hypotheses has been largely limited to aggregate data that link trends in social and economic variables with information on drug use, pain, and mortality.
In exploratory analyses, we used the individual cross-sectional data from the present study to examine the potential influence of economic factors on mental health over this period. Specifically, we evaluated the degree to which inclusion of economic indicators measured at the two waves would reduce the coefficients for survey wave and for the interaction between survey wave and SES (from the values in Table 1). Inclusion of each of three measures of perceived economic distress—an index of perceived current financial strain and two measures of employment uncertainty (now and in the future)—generally resulted in large reductions in both of these coefficients. Inclusion of a broad set of objective economic indicators led to modest although still substantial reductions in these coefficients (SI Appendix, Table S5). While these analyses demonstrate a strong association between trends in economic variables and mental health, we cannot rule out potential reverse causality (e.g., the relationship between perceived economic distress and psychological distress is almost certainly bidirectional). Future analyses based on individual longitudinal data on psychological distress and well-being could provide a unique opportunity to deepen our understanding of these worrisome trends in mental health.
Materials and Methods
Data.
We use data from two cross-sectional waves of the Midlife in the United States study. In 1995 to 1996 (M1), MIDUS conducted phone interviews with a national sample of noninstitutionalized, English-speaking adults in the coterminous United States, targeted at ages 25 to 74. Persons were selected by random-digit dialing with an oversampling of older people and men (36). Among those who completed the phone interview (n = 3,487, 70% response rate), 3,034 (87%) also completed mail-in self-administered questionnaires (SAQs). In 2011 to 2014 (R1), a new refresher cohort of the same age range was sampled from the national population (the sampling frame included both landlines and cell phones) (37). Among those who completed the phone interview (n = 3,577, 59% response rate), 2,598 (73%) also completed the SAQ.
We restrict our analyses to respondents who completed the SAQ. We further limit the primary analyses to non-Latino whites (n = 2,513 from M1 and n = 2,114 from R1). Auxiliary analyses based on the full national sample (n = 3,034 from M1 and n = 2,598 from R1) are given in SI Appendix. All analyses used poststratification weights, which take into account age, sex, race, education, and marital status to ensure that the MIDUS samples show very similar distributions to the corresponding Current Population Survey.
The MIDUS data are publicly available from the Inter-university Consortium for Political and Social Research (https://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/2760; https://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/36532). We used poststratification weights and supplemental data on income sources for M1 that were obtained directly from MIDUS. Researchers can request these income data from Barry Radler (bradler@wisc.edu). Documentation for the construction of the poststratification weights and the Stata do-files used to perform the analyses are available by request from the corresponding author.
Outcome Measures.
We selected six established psychological summary measures as outcome variables: (i) two measures of psychological distress [the Kessler Psychological Distress scale (K6) of negative affect and the Composite International Diagnostic Interview Short Form (CIDI-SF) subscale for major depression]; (ii) two measures of hedonic well-being (an index of positive affect and a rating of life satisfaction); and (iii) two measures of eudaimonic well-being (indexes of psychological well-being and social well-being). More detailed descriptions of these outcomes are provided in SI Appendix. The CIDI-SF was administered during the phone interview, while all other outcomes come from the SAQ.
Socioeconomic Status.
To minimize selection biases that would result from use of educational attainment as an indicator of SES, we use a measure of relative socioeconomic status derived from six items: respondent’s (and spouse/partner’s) education, respondent’s (and spouse/partner’s) occupation, annual household income, and current assets of the respondent and spouse/partner (see SI Appendix for more details). We applied a square-root transformation to reduce skewness in income and asset data. Then, within each wave, we standardized the six items and computed the index as the average across relevant items (e.g., six items if married/partnered and both respondent and spouse/partner had ever been employed; Cronbach’s α = 0.75). We converted the resulting SES score to a percentile rank (1 to 100) based on the weighted distribution within each wave. Finally, we rescaled the rank to range from 0 (1st percentile) to 1 (99th percentile), so that a one-unit change represents the difference between a person in the bottom 1% and the top 1% of the SES continuum.
Analytical Strategy.
Because the two measures of distress are highly positively skewed, we dichotomized these outcomes and estimated logit models. We used a cutoff of four (out of seven) on the CIDI-SF subscale (14% of the weighted full sample), which defines major depression as at least 2 wk of either depressed mood or anhedonia (loss of interest in most things) nearly every day for most of the day, and includes at least four symptoms associated with depression (38). For negative affect, we used a cutoff greater than one (out of four), which corresponds to reporting the relevant symptoms, on average, more than “a little of the time” (18% of the weighted full sample). The other four outcomes were modeled using linear regression and have been standardized (mean 0, SD 1) to facilitate comparisons.
The models include controls for sex, age (specified as quadratic), SES, and survey wave. The models also include several interaction terms. Because some scholars have suggested that growing distress is most prominent in midlife or among working-age adults (5), we include an interaction term between age (linear term) and survey wave to allow changes in mental health to vary across the age range. In addition, in light of a large literature underscoring diminishing effects of SES on health and survival at older ages (39), we also include an interaction between age (linear term) and SES. A third interaction term—between SES and survey wave—reflects how changes in mental health differ by SES. The models are estimated on weighted data from the two pooled MIDUS waves and use robust SEs computed in Stata (40). Multiple imputation was used for missing values of variables in the analysis. The variables with the highest percentage of missing data were household income (18%), assets (13%), social well-being (7%), and psychological well-being (5%).
Supplementary Material
Acknowledgments
We thank Jennifer Dowd, Theresa Andrasfay, Peter Muennig, Carol D. Ryff, Barry Radler, and the anonymous referees for helpful comments. This work was supported by the National Institute on Aging (Grants P01 AG020166 and U19AG051426); Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant P2CHD047879); General Clinical Research Centers Program at the National Institutes of Health (Grants M01-RR023942 and M01-RR00865); National Center for Advancing Translational Sciences at the National Institutes of Health (Grant UL1TR000427); and Graduate School of Arts and Sciences, Georgetown University.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
See Commentary on page 7176.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1722023115/-/DCSupplemental.
References
- 1.Schuchat A, Houry D, Guy GP., Jr New data on opioid use and prescribing in the United States. JAMA. 2017;318:425–426. doi: 10.1001/jama.2017.8913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolodny A, et al. The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–574. doi: 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- 3.Grant BF, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74:911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Behavioral Health Statistics and Quality 2017 Results from the 2016 National Survey on Drug Use and Health: Detailed tables. Available at https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf. Accessed November 20, 2017.
- 5.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci USA. 2015;112:15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masters RK, Tilstra AM, Simon DH. Explaining recent mortality trends among younger and middle-aged white Americans. Int J Epidemiol. 2018;47:81–88. doi: 10.1093/ije/dyx127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Case A, Deaton A. Mortality and morbidity in the 21st century. In: Eberly J, Stock J, editors. Brookings Papers on Economic Activity. Brookings Institution; Washington, DC: 2017. pp. 397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khazan O. 2015 Middle-aged white Americans are dying of despair. Available at https://www.theatlantic.com/health/archive/2015/11/boomers-deaths-pnas/413971/. Accessed December 11, 2017.
- 9.Case A. 2015 “Deaths of despair” are killing America’s white working class. Available at https://qz.com/583595/deaths-of-despair-are-killing-americas-white-working-class/. Accessed December 11, 2017.
- 10.Monnat SM. Deaths of Despair and Support for Trump in the 2016 Presidential Election. The Pennsylvania State University Department of Agricultural Economics, Sociology, and Education Research Brief; State College, PA: 2016. [Google Scholar]
- 11.Masters RK, Tilstra AM, Simon DH. Mortality from suicide, chronic liver disease, and drug poisonings among middle-aged U.S. white men and women, 1980-2013. Biodemogr Soc Biol. 2017;63:31–37. doi: 10.1080/19485565.2016.1248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westerhof GJ, Bohlmeijer ET, McAdams DP. The relation of ego integrity and despair to personality traits and mental health. J Gerontol B Psychol Sci Soc Sci. 2017;72:400–407. doi: 10.1093/geronb/gbv062. [DOI] [PubMed] [Google Scholar]
- 13.Kleijn G, et al. Psychometric characteristics of a patient reported outcome measure on ego-integrity and despair among cancer patients. PLoS One. 2016;11:e0156003. doi: 10.1371/journal.pone.0156003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borsini F, Evangelista S, Meli A. Effect of GABAergic drugs in the behavioral ‘despair’ test in rats. Eur J Pharmacol. 1986;121:265–268. doi: 10.1016/0014-2999(86)90498-x. [DOI] [PubMed] [Google Scholar]
- 15.Westerhof GJ, Keyes CL. Mental illness and mental health: The two continua model across the lifespan. J Adult Dev. 2010;17:110–119. doi: 10.1007/s10804-009-9082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. [Google Scholar]
- 17.Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73:539–548. doi: 10.1037/0022-006X.73.3.539. [DOI] [PubMed] [Google Scholar]
- 18.Ryan RM, Deci EL. On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annu Rev Psychol. 2001;52:141–166. doi: 10.1146/annurev.psych.52.1.141. [DOI] [PubMed] [Google Scholar]
- 19.Ryff CD. Psychological well-being revisited: Advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83:10–28. doi: 10.1159/000353263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sasson I. Trends in life expectancy and lifespan variation by educational attainment: United States, 1990-2010. Demography. 2016;53:269–293. doi: 10.1007/s13524-015-0453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chetty R, et al. The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315:1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montez JK, Zajacova A. Why is life expectancy declining among low-educated women in the United States? Am J Public Health. 2014;104:e5–e7. doi: 10.2105/AJPH.2014.302146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dowd JB, Hamoudi A. Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. Int J Epidemiol. 2014;43:983–988. doi: 10.1093/ije/dyu120. [DOI] [PubMed] [Google Scholar]
- 24.Mojtabai R, Jorm AF. Trends in psychological distress, depressive episodes and mental health treatment-seeking in the United States: 2001-2012. J Affect Disord. 2015;174:556–561. doi: 10.1016/j.jad.2014.12.039. [DOI] [PubMed] [Google Scholar]
- 25.Weinberger AH, et al. Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychol Med. 2018;48:1308–1315. doi: 10.1017/S0033291717002781. [DOI] [PubMed] [Google Scholar]
- 26.Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 27.Hedegaard H, Warner M, Miniño AM. 2017. Drug overdose deaths in the United States, 1999–2015 (National Center for Health Statistics, Hyattsville, MD), NCHS Data Brief 273.
- 28.Krueger A. Brookings Papers on Economic Activity. Brookings Institution; Washington, DC: 2017. Where have all the workers gone? An inquiry into the decline of the U.S. labor force participation rate; pp. 1–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moore JC, Stinson LL, Welniak EJ., Jr Income measurement error in surveys: A review. J Off Stat. 2000;16:331–361. [Google Scholar]
- 30.Williams DR, Earl TR. Commentary: Race and mental health–More questions than answers. Int J Epidemiol. 2007;36:758–760. doi: 10.1093/ije/dym114. [DOI] [PubMed] [Google Scholar]
- 31.Perreira KM, Deeb-Sossa N, Harris KM, Bollen K. What are we measuring? An evaluation of the CES-D across race/ethnicity and immigrant generation. Soc Forces. 2005;83:1567–1601. [Google Scholar]
- 32.Shiels MS, Freedman ND, Thomas D, Berrington de Gonzalez A. Trends in U.S. drug overdose deaths in non-Hispanic black, Hispanic, and non-Hispanic white persons, 2000–2015. Ann Intern Med. 2018;168:453–455. doi: 10.7326/M17-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cherlin AJ. Labor’s Love Lost: The Rise and Fall of the Working Class Family in America. Russell Sage; New York: 2014. [Google Scholar]
- 34.Berkman LF, et al. Mothering alone: Cross-national comparisons of later-life disability and health among women who were single mothers. J Epidemiol Community Health. 2015;69:865–872. doi: 10.1136/jech-2014-205149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Montez JK, Sabbath E, Glymour MM, Berkman LF. Trends in work–family context among U.S. women by education level, 1976 to 2011. Popul Res Policy Rev. 2014;33:629–648. doi: 10.1007/s11113-013-9315-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brim OG, et al. 2016. National Survey of Midlife Development in the United States (MIDUS), 1995-1996. ICPSR02760-v11. Available at doi.org/10.3886/ICPSR02760.v11. Accessed December 20, 2016.
- 37.Ryff C, et al. 2016. Midlife in the United States (MIDUS Refresher), 2011-2014. ICPSR36532-v2. Available at doi.org/10.3886/ICPSR36532.v2. Accessed September 21, 2017.
- 38.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- 39.Lauderdale DS. Education and survival: Birth cohort, period, and age effects. Demography. 2001;38:551–561. doi: 10.1353/dem.2001.0035. [DOI] [PubMed] [Google Scholar]
- 40.StataCorp . Stata: Release 12. Statistical Software. StataCorp; College Station, TX: 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.