Abstract
Health information technology (HIT) is increasingly adopted by nursing homes to improve safety, quality of care, and staff productivity. We examined processes of HIT implementation in nursing homes, impact on the nursing home workforce, and related evidence on quality of care. We conducted a literature review that yielded 46 research articles on nursing homes’ implementation of HIT. To provide additional contemporary context to our findings from the literature review, we also conducted semistructured interviews and small focus groups of nursing home staff (n = 15) in the United States. We found that nursing homes often do not employ a systematic process for HIT implementation, lack necessary technology support and infrastructure such as wireless connectivity, and underinvest in staff training, both for current and new hires. We found mixed evidence on whether HIT affects staff productivity and no evidence that HIT increases staff turnover. We found modest evidence that HIT may foster teamwork and communication. We found no evidence that the impact of HIT on staff or workflows improves quality of care or resident health outcomes. Without initial investment in implementation and training of their workforce, nursing homes are unlikely to realize potential HIT-related gains in productivity and quality of care. Policy makers should consider creating greater incentives for preparation, infrastructure, and training, with greater engagement of nursing home staff in design and implementation.
Keywords: nursing homes, information technology, nursing home staff, outcome and process assessment (health care)
-
What do we already know about this topic?
Nursing homes are increasingly adopting health information technology (HIT) for resident management and clinical support.
-
How does your research contribute to the field?
We found nursing homes often do not employ a systematic process for HIT implementation, lack necessary technology support and infrastructure, and underinvest in staff training, thereby limiting the potential to realize HIT-related gains in productivity and quality of care.
-
What are your research’s implications toward theory, practice, or policy?
Policy makers should consider creating greater incentives for preparation, infrastructure, and training, with greater engagement of nursing home staff in design and implementation.
Introduction
Health information technology (HIT) systems have the potential to improve safety, communication, and productivity in nursing homes (NHs). Early research suggests HIT can improve scores on NH quality indices1; resident outcomes such as maintenance of activities of daily living, range of motion, and bed mobility2; and clinical support to reduce rates of adverse drug events and increase identification of medication errors.3,4 The most recent survey of information technology (IT) in NHs reported that IT sophistication remains greatest for administrative support, such as billing functions, with growing incorporation in resident care functions such as bed availability and discharge management, and relatively slow uptake for clinical support functions such as documentation of vital signs, incident reporting, and medication administration.5 Furthermore, the early findings from that review suggest that current capabilities of HIT exceed its use.
The progression from HIT capability to integrated use depends on multiple factors, including staff training, skills, perceived value of HIT, and integration into organization workflows.1 Early research on HIT adoption in NHs has found that training and the need for culture change are important barriers to implementation.6 Greater satisfaction with HIT in NHs is associated with good training resources and effective implementation strategies, including carefully planned change management procedures, hiring adequately trained IT staff, and offering a system support plan.7,8 It is therefore critical to understand the experiences of frontline workers as the NH industry continues to move toward more sophisticated uses of technology.9,10 To date, little research has explored how use of HIT impacts NH staff and their work processes, communication, documentation, and clinical decision-making.
Conceptual Framework of Impact of HIT on NH Staff
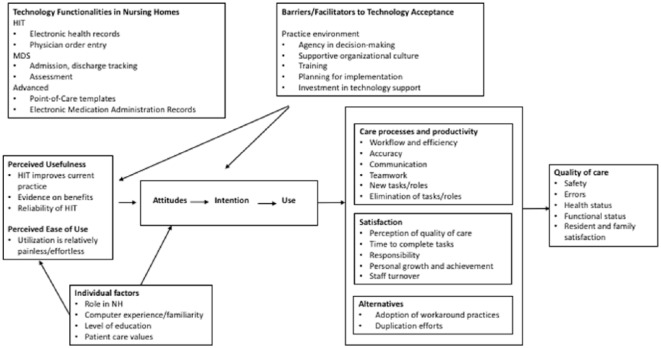
We synthesized and adapted existing frameworks on HIT use that have been developed for prior research and application (Figure 1). To identify the types and functionalities of HIT that are relevant to this study, we drew from the conceptual framework of HIT in NHs developed by Liu and Castle.11 The 3 concepts comprising the framework include (1) general HIT systems, eg, electronic health record, physician order entry; (2) Basic Minimum Data Set (MDS), ie, resident assessment data on health and functional abilities mandated for submission to the Centers for Medicare and Medicaid; and (3) Information systems (eg, billing, payroll, accounting, human resources). There are also 2 “Advanced Features” (eg, electronic medication administration records [eMAR] and point of care [POC] templates) within the framework that overlap with the 3 main concepts. Because the objective of this study was to examine impacts on staff engaged in resident and nursing care, we focused our research on the HIT and Basic MDS concepts and their overlap with Advanced Features, rather than nonclinical information systems functions.
Figure 1.
Conceptual framework for the impact of health information technologies on nursing home staff.
Note. HIT = health information technology; MDS = Minimum Data Set.
To explore potential impacts of HIT on NH staff, we adapted the Technology Acceptance Model (TAM) developed by Yarbrough for NHs.12 The Technology Acceptance Model posits that behavioral intention to use HIT arises from attitudes, perceived usefulness, perceived ease of use, and “external” barriers to technology acceptance such as time, costs, and system and organizational issues. Perceived usefulness includes whether HIT is perceived as improving current practice, showing evidence of benefits, and being both reliable and dependable. Perceived ease of use refers to whether use of HIT is considered relatively effortless. Both these factors in turn affect positive attitudes toward HIT and intention to use HIT. Furthermore, individual factors such as familiarity with computers and relative preferences for spending time on direct patient care (versus use of HIT) can affect perceptions and attitudes. Because the TAM was developed for physicians, other concepts are not developed for NH staff; for example, higher levels of education and practice ownership among physicians are proposed to influence perceived usefulness and ease of use, but NH staff have a range of educational levels, less likely to have NH ownership, and more likely to engage in team care. In this framework, perceptions and attitudes affect intent to use HIT, or pursuit of alternative behaviors, including work-arounds, duplication efforts, and staff exits.
In addition, the TAM addresses only perceptions and intent to use HIT and does not elaborate how HIT leads to productivity and quality of care outcomes, or how attitudes and behaviors moderate these impacts. We therefore draw from the model developed by Rouleau et al that outlines impacts of information and communication technology for nursing care.13 Rouleau et al describe how use of technology can affect nurses’ scope of practice, care processes, and productivity, including workflows, documentation accuracy, and changes in tasks/roles. Rouleau et al also identify how nurses’ experiences with HIT affect nurse satisfaction, with some concepts closely related to other model components such as perceived time to complete tasks (perceived ease of use, productivity, and workflows), and other concepts not previously identified, such as opportunities for personal growth and achievement. We use multiple arrows to indicate how several concepts affect nurses’ satisfaction. Care processes, productivity, and, in turn, nurses’ satisfaction contribute to quality of care and resident satisfaction. As with the TAM, the Rouleau model focuses on one category of HIT users (registered nurses) and does not account for potential differences due to education and responsibility levels seen in a NH.
Both models underemphasize the role of staff education, training, and planning for implementation as barriers/facilitators of technology adoption. These concepts may hold even greater relevance in NHs in which staff with fewer educational requirements (eg, certified nursing assistants [CNAs]) may have less familiarity with IT and require more formal training, and thus the NH’s pre-implementation planning process may be more complex.14 Both models acknowledge the importance of user agency in decision-making to subsequent outcomes in perceived usefulness and intention to use, including the involvement of users in choosing HIT, planning, and implementation.
Objectives
The purpose of this study was to examine the relationships between HIT implementation and NH workforce outcomes, including staff satisfaction, experiences with use, and overall effects on quality of care. We conducted a literature review to assess the current research evidence. Because of the time delay from peer-reviewed publication and synthesis into a literature review, we also conducted semistructured interviews and focus groups of NH staff to gain insights on current practice. By highlighting both gaps and promising practices, the findings can inform administrators and policy makers on how to engage and support staff through HIT implementation to ensure that quality benefits are realized. To examine the relationships between HIT implementation and the NH workforce, we posed the following questions:
How do NHs prepare their workforce for HIT implementation?
How has HIT implementation changed workflow and productivity in NHs?
How has HIT implementation changed staffing, roles, and teamwork?
Have changes in staffing, workflow, and/or productivity in NHs impacted quality of care?
Methods
We conducted both a review of the literature to understand both the evidence base and supplement our findings with key informant interviews and focus groups on current experiences of HIT in NHs.
Literature Review
Search strategy
We identified search terms that pertained to HIT, such as “electronic health record,” “computerized physician order entry,” “computerized patient record,” and “health information management.” These terms were then combined with terms related to the NH workforce: “nursing education,” “personnel management,” “job description,” “turnover,” and “staffing.” (See Online Appendix for the detailed search strategy.) Given that adoption of HIT in NHs is a relatively new phenomenon, we excluded studies published prior to 2004. We also excluded studies published in a language other than English.
Data sources
We conducted searches in the following databases: PubMed, CINAHL, PsycINFO, Google Scholar, and Web of Science. We used major subject headings that corresponded to pre-identified search terms for each database.
Eligibility criteria
We employed the following inclusion and exclusion criteria to identify and select studies: included if conducted in NHs or skilled nursing facilities, and excluded if focused on other settings such as residential care facilities, assisted living, or home health. We included only peer-reviewed original research and excluded reviews, commentaries, news articles, editorials, and unpublished reports. Last, we narrowed our search to studies that reported outcomes related to impact of HIT on the NH workforce, such as staff productivity and quality of care.
Study selection
Our search of electronic literature databases yielded 246 nonduplicate records. (See Online Appendix, Figure 1, for flow diagram of records and selection.) We identified an additional 2 unique records of studies by using SCOPUS to identify references listed in literature reviews. Two reviewers [MK, LW] then independently screened titles and abstracts for inclusion based on the study eligibility criteria. The 2 reviewers met and resolved discrepancies in selection, with refinement of the eligibility criteria. Following resolution, 103 records were selected for full text review. The reviewers again reviewed selections and resolved discrepancies to select 46 studies for inclusion in the final review.
Data abstraction
From the final 46 studies, we abstracted information on authors, date of publication, type of HIT studied, study design, setting, study population, workforce-related outcomes, and other outcomes.
Analysis
Most studies (39 out of 46) employed nonexperimental designs, and 3 of the 7 quasi-experimental designs did not employ statistical adjustment for nonequivalent comparison groups. Also, many studies employed qualitative methods such as focus groups, interviews, and direct observation. As a result, methods for evaluating literature quality [such as the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) system] were not applicable.15 Therefore, we analyzed the literature findings for major themes related to each of the primary research questions. Detailed descriptions of study designs and findings from the literature review are summarized in Online Appendix Table 1.
Key Informant Interviews and Focus Groups
In April and May 2016, investigators conducted nationwide telephone and in-person interviews and focus groups of NH employees to provide contemporary insights on how HIT impacts the workforce. Participants were interviewed from 5 different US regions (West, Southwest, Midwest, Northeast, South), employed in free-standing NHs, and representing a range of NH roles, from administrative (director of nursing [DON]), midlevel managerial (charge nurse), to CNAs. (Refer to Online Appendix Table 2 for a summary of participant roles and facility characteristics). For all participants, discussion questions were developed based on expert review (see Online Appendix Exhibits 3 and 4 for interview guides), with additional modifications based on literature review findings and participant roles. Discussions were recorded and transcribed; transcripts were analyzed with main themes triangulated with findings from the literature review. Study procedures were approved by the University of California, San Francisco Institutional Review Board.
Results
For each theme, we present the findings from the literature review, followed by qualitative interview findings to support that theme. Syntheses of main themes are summarized in Table 1.
Table 1.
Summary of Main Themes and Subthemes Identified From Literature Review.
| Theme | Main finding |
|---|---|
| Barriers/facilitators to technology adoption | |
| Planning and staff agency in decision-making | Little to no systematic processes are used for implementation of HIT |
| Training | NH leadership is concerned about staff lack of computer skills, fear of technology, and limited English proficiency to use HIT |
| NH staff report interest and enthusiasm for learning new HIT skills | |
| Initial training is inadequate and continuing training after implementation rarely provided | |
| Technology support | Staff are frustrated because IT support is insufficient, rarely on-site, and after hours is slow or nonexistent |
| Staff are dissatisfied due to poor quality equipment, unreliable systems, and limited Internet connectivity | |
| Care processes and productivity | |
| Workflow | Workflow efficiency may increase initially due to HIT implementation but eventually return to baseline |
| Workflows should be redesigned prior to implementation | |
| Accuracy and workarounds | Mixed evidence on accuracy of documentation: improvements related to legibility and errors due to workarounds |
| Changes in tasks and roles | No evidence that HIT reduced need for nursing home personnel |
| New roles as “super-users,” who are not necessarily compensated for additional skills or responsibilities | |
| Communication and teamwork | HIT implementation fosters staff communication and team cohesion |
| Staff satisfaction | Mixed evidence of both positive and negative effects of HIT on staff satisfaction |
| Limited evidence that HIT replaces staff roles or increases staff turnover | |
| Quality of care | No empirical evidence that HIT improves quality of care due to changes in staffing or productivity |
| NH staff perceive that HIT improves communication and documentation | |
Note. HIT = Health Information Technology; IT = information technology; NH = nursing home.
Barriers/Facilitators to Technology Adoption
We identified literature mapping to the following main themes regarding Barriers/Facilitators to Technology Adoption: Planning and Staff Agency in Decision-Making, Training, and Technology Support.
Planning and staff agency in decision-making
Little literature exists on planning and the involvement NH staff in preparing for HIT implementation, one aspect of staff agency in decision-making. Four studies referenced preparations, primarily to indicate that there was little or no systematic process for implementation, 16-19 with staff in 1 study characterizing HIT implementation as “trial and error.”16 Staff reported minimal communication prior to implementation17,19 and the motivations for HIT implementation not well understood.16,18,19 In 1 case, although administrators and DONs reported using multiple means of communication to prepare staff for introduction of a new HIT system, staff nurses and CNAs reported learning through word-of-mouth or having no advance notification.19 Only 2 studies described a deliberate effort to engage staff in selection of the HIT system or vendor20,21 and another 2 described design and pilot testing of the software with feedback from nurses.20,22 One study of Texas administrators and DONs reported those with higher leadership and employee readiness scores were more likely to have developed plans for implementation, but involvement of staff in those plans is not known.23 Two studies suggested that NHs had limited preparation for HIT implementation because leadership had poor understanding of HIT themselves.16,23
In interviews, participants reported a gradual phase-in with no apparent pattern or process for what component of HIT was implemented first. None of the participants reported participating in the initial vendor selection process. Participants employed by NHs within health systems perceived HIT decisions were driven by reimbursement policy with no staff input.
Training
Across multiple studies, administrators and DONs reported staff’s poor computer literacy,6,16,18,19,24-26 fear of technology,6,17,18,26 and limited English ability18,25,27 as barriers to implementation. In contrast, when interviewed or surveyed directly, nurses and CNAs reported trust in computer systems,28 curiosity about new HIT, and enthusiasm for opportunities to learn new skills.19 Few studies described training efforts to address either leadership concerns or to meet staff preparation needs and interest in HIT implementation. Three reported that inadequate investment and lack of clear expectations for training arose because NH leaders were unfamiliar with the technology and system capacities.16,18,19
Many studies found staff dissatisfaction due to insufficient time dedicated to training and sessions not tailored to staff needs.9,17,19,24,25,27 Of the studies that described training, many reported single sessions for nursing staff ranging from 30 minutes to 1 day, and single sessions for CNAs or personal care assistants (PCAs) of only 20 to 30 minutes.9,19,21,24,29-31 In one of the few studies in which staff reported satisfaction with training, they received more training than what was typically reported: multiple days for nurses and full days for CNAs.8 For new hires, training was often described as ad hoc, provided by other staff when available.24,30,32 Four studies described a “train-the-trainer” process, in which a few individuals typically received a 1-week training with the software vendor and then provided additional support to staff during implementation.19,21,24,33 Staff repeatedly identified the need for ongoing training and opportunities to practice.7,18,19,27 Two studies noted difficulties because training sessions were optional, not mandatory.17,32 All of the above studies concluded that HIT implementation challenges arose due to insufficient staff training. There were no studies that evaluated different training methods or quantified to what degree quality of care or productivity were attributable to training.
Interview responses were consistent with the literature, indicating limited training experiences and general dissatisfaction, although the sessions were slightly more extensive than what was reported in the literature. Nurses received 8 hours to 2 weeks of training, and CNAs received 30 minutes to 4 hours. Participants reported inconsistent training for system updates, receiving an email or endorsement about minor modifications. As noted in the literature, newly hired nurses and CNAs received fewer hours or no orientation at all.
Respondents suggested perceived computer simulation and 1:1 preceptor experience as superior to traditional in-service education sessions, though few reported receiving these training modalities. One participant noted the importance of involving clinical staff, and not only IT staff, in delivering training:
We hired a program manager from IT driving the process . . . Lesson learned, you really need to have a clinician as part of the program training otherwise I realize nurses will say “yes” and “yes” and not connect the dots. Nonclinicians don’t talk our language to be able to train the nurses.
Technology support
In conjunction with insufficient training, most studies found that NHs did not adequately invest in technology infrastructure or support personnel, and these deficiencies led to staff frustration. Staff frequently reported difficulties with HIT adoption due to too few computers, limited and/or slow Internet access, lack of wireless connectivity, and poor integration of systems.7,20,26,27,34-37 In multiple studies, staff also reported a need for greater IT support, ideally on-site.7,9,18,25-27,38 Several studies described help lines that were not available after hours and had slow response times.9,24,25,27 Two reported that on-site and intensive IT support available 24/7 were instrumental to HIT implementation.19,39
Our interviews provided greater detail into consequences of inadequate technology infrastructure and IT support. Participants most frequently identified poor Internet connectivity, and specifically wireless Internet dead zones throughout the facility, as the most substantive barrier to successful uptake of HIT. Participants reported access to 24-hour support lines, but during weekends and holidays staff could expect to wait 24 hours or receive no assistance until regular office hours. Only Administrators and DONs had staff access health records information off-site, and sometimes they assisted staff with technology concerns. Staff reported considerable frustration from insufficient support due to the frequency of technical difficulties:
In a 5-day work week, 3 days we have issues.
Care Processes and Productivity
Workflow
Staff perceptions of the influence of HIT on workflow were mixed: In some studies, staff described processes as more streamlined,6,9,19,24,40,41 and in others, processes were more cumbersome.7,16,18,25,27,30,32,42-44 In the quasi-experimental studies, staff in the intervention groups were more likely to report that documentation times and completeness improved.8,41,42 In the studies that used direct observation and process mapping of workflows, the number of steps and the time to complete tasks were either reduced or the same with the new HIT system.24,29-31,45 The studies with longer follow-up periods noted that staff efficiency decreased in the initial months following adoption, but that most processes had returned to baseline efficiency by 12 to 24 months.2,25,27,29,30 In some cases, this reflected greater familiarity with the HIT system,2 and in others, workflows were no more efficient because the staff had developed work-arounds or reverted to paper.24 Two studies concluded that evaluation and redesign of workflows should occur in the planning phase, prior to HIT implementation.18,36
Interview participants reported general improvements in workflow, with relatively few difficulties adapting to the new HIT system. Participants reported spending approximately half of each shift spent using HIT, with some improvements in efficiency:
If someone refuses their meds, I can do it as the incident is happening, I don’t have to wait until the end of the shift. It has helped. . . . Communication is faster in the event of a situation. My work does go by faster.
Accuracy and work-arounds
As noted with workflows, HIT appears to have mixed effects on documentation in NHs. In the one experimental study, a randomized controlled trial of a menu-driven incident reporting system for falls, the authors found that documentation of near-falls and fall circumstances in the intervention sites improved significantly relative to the control sites after 4 months.20 Two observational studies found that introduction of HIT led to improved accuracy and completeness of documentation,40,41 whereas another found the opposite.26 Studies of eMAR found alerts fostered proactive correction of medications.22,35 Others described work-around strategies that could negatively impact the quality of care, including skipping fields, “clicking” through fields that check vital signs prior to medication administration,36 documenting care before it was given,27 using paper documentation that was inconsistently entered in the HIT records,27,46 and avoiding checks in HIT systems due to log-on difficulties.43
Interview participants confirmed both favorable experiences with documentation quality but nearly all reported use of work-arounds to finish tasks quickly, increasing the potential for errors.
Almost all of them [do work-arounds]. . . . They give you a green, red, orange on the computer if you are late. . . . So they start charting ahead of time. . . . They started cheating.
Communication and teamwork
Administrators and staff frequently reported that HIT improved communication;19,20,24,25,27 with only 2 concluding no impact.42,47 In 1 study, nurses and managers described how HIT systems provided CNAs and PCAs with a consistent framework for alerts on resident care needs.42 When examined by direct observation, staff had fewer in-person or verbal interactions after HIT implementation but used a greater variety of communication methods.29,30,38,43,46 Other studies found that staff expressed a continued preference for verbal communication on issues deemed important.30,43,46
Some studies reported that HIT implementation fostered team cohesion.27,48,49 CNAs and PCAs reported mixed perceptions of the impact of HIT on their relationships with supervisors: On one hand, the value of their work may be more appreciated when it is visible in HIT;40 on the other hand, electronic tracking can convey a “Big Brother” impression of close monitoring.25,27
Interview participants perceived that HIT enhanced teamwork, as seasoned staff shared their clinical expertise with newer employees, while newer personnel assisted experienced workers with technology support. A chief nursing officer explained,
The older seasoned nurses did not feel intimidated because they got to share expertise and skills and that’s exactly why we were so successful.
Changes in tasks and roles
We found no studies that reported HIT implementation reduced the need for personnel. Instead, studies described a change in staff responsibilities; as noted above, some NHs created HIT “super user” roles. (“Super users” are typically staff from within the organization who receive additional training in new HIT systems to serve as technical support for their peers.)50 In some cases, super users were selected based on the results of an initial computer skills test;47 in others, the process was not well described and lack of transparency in the selection of super users fostered resentment.19,51 Staff members, and occasionally the super users themselves, did not know who was a designated super user.19 In all studies, super users were expected to assume the responsibility of training and assisting other staff without a change in their other work roles; they were compensated for extra hours but did not receive higher pay or other reward in recognition of their added skills or responsibilities.19 Two studies also referenced the use of “nurse mentors,” but there was no description of the selection, training, or deployment of mentors.7,27 On occasion, super users and mentors expressed frustration with their additional responsibilities and said they would prefer that colleagues use IT support.9 Three studies described positive benefits from engaging quality improvement nurses and teams with the HIT implementation process.22,27,49
Interviews were consistent with the literature, in that HIT systems did not reduce the need for personnel and instead created new roles. One DON noted the importance of having a staff nurse as a super user, because IT consultants were not as effective for ongoing support.
Staff Satisfaction
In addition to the findings related to satisfaction described above (eg, perceptions of training, technology support, teamwork), the literature also described impacts of HIT broadly on satisfaction and related staff turnover. We did not identify any literature that specifically addressed how HIT affected staff perceptions of responsibility, personal growth, or achievement in contributing to workplace satisfaction.
Staff satisfaction and turnover
Few studies reported an increase in staff turnover following HIT adoption. In 1 study of NHs in Texas, DONs reported that staff quit due to “information overload” and difficulty using computers.40 Two studies found increased absences, pulling out cables, and turning off systems due to staff dissatisfaction, but not staff exits.16,20 One quasi-experimental study found no significant differences in turnover between intervention (HIT) and comparison (no HIT) sites.2 The findings on turnover may be inconclusive because studies reported the impact of HIT on staff satisfaction as both positive6,8,9,17,42,52 and negative.7,8,16,18,24
Interviews also revealed that, despite difficulty with the new technology, few instances of technology-associated staff turnover occurred:
We had one or two CNAs who were resistant to change so those who were able to retired. However, nurses did not quit. Even the nurses who were here over 20 years stayed with the facility.
Quality of Care
We identified no studies that directly examined whether impacts of HIT on NH staff care processes or satisfaction affected the quality of resident care. We found 1 study that attempted to quantify the interrelationships between staffing, use of HIT for MDS, and quality of care.11 The authors concluded that the positive association between staffing and quality was both partly accounted for (mediated) by the higher use of HIT in more highly staffed NHs, and potentially amplified (moderated) by HIT. Quality gains from HIT are synergistic with staffing rather than via a direct pathway in which staff workflows are changed by HIT.
The remaining literature described staff perceptions of how HIT implementation may have impacted quality of care. Administrators and nurse managers believed HIT improved quality of care due to the capacity to monitor resident conditions, conduct oversight of care practices by frontline staff, and facilitate continuity of care.24,25,27,39,42,47,48,53,54 Nurses and CNAs reported that HIT improved the legibility of documentation and ease of access to needed information, and as a result they could deliver better quality of care to residents.7,9,30,47 However, CNAs and PCAs also expressed concern that use of HIT came at the expense of time spent on direct resident care, and some direct observation studies found that resident care time declined following HIT implementation.19,40,7,25,27,30 Both nursing and direct care staff perceived that HIT did not impact clinical decision-making.24,30
Interview participants did not report that HIT compromised resident care. A few noted that by making it easier to view medications and treatments, HIT allowed them to view patients more holistically. Participants reported quality of care improved due to increased efficiency and legibility of communications fostered by HIT.
Discussion
The adoption of HIT in NH settings is spreading rapidly,5 and HIT has the potential to improve quality of care in multiple ways. However, positive quality effects are contingent upon implementation and use by the end users—NH staff. Without engagement of the NH workforce, gains from HIT will be limited.
We found that despite over 10 years of research documenting staff needs for HIT implementation in NHs, training and preparation remain underinvested and inadequate. There is very little evidence that NHs engage in ongoing training after initial adoption to address changes in technology or provide comparable training for new hires, even though turnover is high in the long-term care workforce. Contributing factors include NH leaders’ own limitations in technology skills, time, perceptions of staff motivation to learn new HIT systems, and the disconnection between corporate and NH leadership in health systems. A review of the literature on physicians and nurses has also identified challenges due to training and technology support, but notes that hospitals are more likely to have these resources.55 Our findings suggest that failure to include staff in the planning process and to offer adequate training in NHs can result in several problems, including trainings that are brief and not appropriately tailored to care processes, unintended barriers in staff access to the new technology, insufficient IT support to troubleshoot problems, and slow, unreliable wireless Internet connections that impede staff ability to complete tasks.
Inadequate preparation and training for HIT may explain why we found mixed evidence for the impact of HIT on NH staff workflow and productivity. Our findings are consistent with literature on nurses and physicians, in which conflicting studies have shown both improvements and decrements in efficiency, time spent on documentation, and impacts on time spent on patient care.13,56 HIT has the potential to improve efficiency of tasks, but progress can be impeded by ongoing double-documentation with paper, work-arounds, and lack of training for system updates. These countertrends may partly explain why studies that used process observations found that HIT implementation produced little real change in efficiency or steps, despite staff perceptions otherwise. Furthermore, multiple studies and interviews noted work-arounds employed by NH staff that can lead to documentation errors and mistakes in clinical care.
However, literature and interviews indicated HIT can also foster teamwork and communication across roles and levels of seniority within NHs. This is similar to other studies that have reported improvements in interprofessional collaboration between nurses and physicians using information and communication technology.13 We found limited evidence of HIT impact on NH staff satisfaction, staffing, or turnover. Research on nurses and physicians has found mixed effects of HIT on satisfaction.13,55 The findings suggest that NHs are using HIT to supplement, not replace, existing staffing. Staff roles are evolving to fit the needs of HIT systems, particularly in the case of “super users.” “Super users” appear better positioned to train staff and provide ongoing HIT support, but it remains unclear whether they are appropriately compensated or allocated time for these new responsibilities. More investigation is needed on how super users are selected, trained, and roles defined in NHs. A recent examination of hospital nursing super users highlighted inconsistent processes for super user designation, training, and work expectations and, consequently, variability in the benefits of a super user. It also noted that super users reported physical and emotional exhaustion and that there were potential negative consequences of super users developing work-arounds and spreading negative opinions of HIT to other staff.57
The mix of negative evidence on training and productivity, versus positive evidence on staff communications and teamwork, may explain why we found no clear evidence that HIT enabled staff to improve quality of care. Alexander et al have found that higher HIT sophistication in NHs is associated with improved quality of resident care,1,39 but it is not clear if HIT led to improvements, versus if the types of NHs that invest in more sophisticated HIT are also more likely to have higher quality of care. If HIT-related benefits are seen only in NHs with higher levels of staffing, this suggests that HIT adoption by other NHs may not produce the desired results. Our findings suggest that without the initial investment in implementation—engaging staff with selection of the product, developing training and new workflows appropriate to the needs of the facility, and ensuring sufficient equipment and Internet connectivity—NHs are unlikely to realize potential gains in productivity and quality of care.
Limitations
There are several limitations to this study. First, the extant peer-reviewed research on the impact of HIT among the NHs workforce is limited, especially in the United States. However, there was consistency in many findings across studies, suggesting broad commonalities in the way staff interact with HIT across settings. Second, most studies utilized staff members’ self-reported experiences. These findings are subject to selection bias from voluntary participation in the study and staff may not be willing to disclose perspectives such as resistance to using technology. Third, given the lack of a systematic approach toward implementation across NHs, there was a vast heterogeneity in the types of HIT implemented; thus, it was not possible to compare each implementation’s impact on the NH workforce. Fourth, as is common in published research on technology adoption, there were temporal delays in the literature results compared with what is occurring “on the ground” in real time. At the same time, in this 10-year period of rapid innovation and adoption, the perspectives obtained from interviews suggest that the challenges are consistent between the older literature current conditions. Last, we obtained interviews from a range of participants across geography and roles, but with a small sample and little variation in implementation stage; a broader, more comprehensive staff perspective is needed.
Conclusion
Our findings support several recommendations to engage and prepare the NH workforce for HIT. First, stakeholders in NH care should develop a toolkit for the NH workforce on HIT implementation that includes a facility and staff readiness assessment20 and a technical needs assessment, given the numerous reported difficulties with wireless connectivity and technical support that negatively impact staff ability to use HIT successfully. Second, stakeholders should develop a framework to integrate quality improvement initiatives with HIT implementation. Third, policy makers and health systems should consider making incentives and other funds available for NHs to increase investments in training supported by clinical staff, and technology infrastructure.
Supplemental Material
Supplemental material, INQ-17-0300.Supplemental_Material.Revision for Nursing Home Implementation of Health Information Technology: Review of the Literature Finds Inadequate Investment in Preparation, Infrastructure, and Training by Michelle Ko, Laura Wagner and Joanne Spetz in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
We thank Onyinyechi Okwandu and Jessica Pessecow, RN, for their contributions in data collection and management for this study. We also thank Amy Markowitz, Lena Libatique, and Krista Chan for their contributions in editing and formatting for this article and its related presentations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS), Cooperative Agreement for a Regional Center for Health Workforce Studies (U81HP26494 to M.K., L.W., and J.S.).
ORCID iD: Michelle Ko  https://orcid.org/0000-0001-8859-0022
https://orcid.org/0000-0001-8859-0022
References
- 1. Alexander GL, Madsen RW. A report of information technology and health deficiencies in U.S. nursing homes. J Patient Saf. 2017. doi: 10.1097/PTS.0000000000000390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rantz MJ, Hicks L, Petroski GF, et al. Cost, staffing and quality impact of bedside electronic medical record (EMR) in nursing homes. J Am Med Dir Assoc. 2010;11(7):485-493. [DOI] [PubMed] [Google Scholar]
- 3. Resnick HE, Manard BB, Stone RI, Alwan M. Use of electronic information systems in nursing homes: United States, 2004. J Am Med Inform Assoc. 2009;16(2):179-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Handler SM, Sharkey SS, Hudak S, Ouslander JG. Incorporating INTERACT II clinical decision support tools into nursing home health information technology. Ann Longterm Care. 2011;19(11):23-26. [PMC free article] [PubMed] [Google Scholar]
- 5. Alexander GL, Madsen RW, Miller EL, et al. A national report of nursing home information technology: year 1 results. J Am Med Inform Assoc. 2017; 24 (1): 67-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cherry B, Carter M, Owen D, Lockhart C. Factors affecting electronic health record adoption in long-term care facilities. J Healthc Qual. 2008;30(2):37-47. [DOI] [PubMed] [Google Scholar]
- 7. Alexander GL, Rantz M, Flesner M, Diekemper M, Siem C. Clinical information systems in nursing homes: an evaluation of initial implementation strategies. Comput Inform Nurs. 2007;25(4):189-197. [DOI] [PubMed] [Google Scholar]
- 8. Yu P, Hailey D, Li H. Caregivers’ acceptance of electronic documentation in nursing homes. J Telemed Telecare. 2008;14(5):261-265. [DOI] [PubMed] [Google Scholar]
- 9. Meehan R. Electronic health records in long-term care: staff perspectives. J Appl Gerontol. 2017;36(10):1175-1196. [DOI] [PubMed] [Google Scholar]
- 10. Little MO, Rantz M, Lynn GA. Health information technology in long-term care: potential for the future. J Am Med Dir Assoc. 2016;17(5):379-380. [DOI] [PubMed] [Google Scholar]
- 11. Liu D, Castle NG. Health information technology in nursing homes. J Appl Gerontol. 2008; 28(1): 38-58. [Google Scholar]
- 12. Yarbrough AK, Smith TB. Technology acceptance among physicians: a new take on TAM. Med Care Res Rev. 2007;64(6):650-672. [DOI] [PubMed] [Google Scholar]
- 13. Rouleau G, Gagnon MP, Cote J, Payne-Gagnon J, Hudson E, Dubois CA. Impact of information and communication technologies on nursing care: results of an overview of systematic reviews. J Med Internet Res. 2017;19(4):e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. LeadingAge Center for Aging Services Technologies. Electronic Health Records (EHRs) for Long-term and Post-Acute Care: A Primer on Planning and Vendor Selection. Washington, DC: LeadingAge Center for Aging Services Technologies;2016. [Google Scholar]
- 15. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bezboruah KC, Paulson D, Smith J. Management attitudes and technology adoption in long-term care facilities. J Health Organ Manag. 2014;28(3):344-365. [DOI] [PubMed] [Google Scholar]
- 17. Fossum M, Ehnfors M, Fruhling A, Ehrenberg A. An evaluation of the usability of a computerized decision support system for nursing homes. Appl Clin Inform. 2011;2(4):420-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hudak S, Sharkey S. Health Information Technology: Are Long Term Care Providers Ready? California Healthcare Foundation;2007. Oakland, CA. [Google Scholar]
- 19. Schoville RR. Exploring the Implementation Process of Technology Adoption in Long-term Care Nursing Facilities. Ann Arbor: University of Michigan; 2015. [Google Scholar]
- 20. Wagner LM, Capezuti E, Taylor JA, Sattin RW, Ouslander JG. Impact of a falls menu-driven incident-reporting system on documentation and quality improvement in nursing homes. Gerontologist. 2005;45(6):835-842. [DOI] [PubMed] [Google Scholar]
- 21. Fossum M, Ehnfors M, Svensson E, Hansen LM, Ehrenberg A. Effects of a computerized decision support system on care planning for pressure ulcers and malnutrition in nursing homes: an intervention study. Int J Med Inform. 2013;82(10):911-921. [DOI] [PubMed] [Google Scholar]
- 22. Sharkey S, Hudak S, Horn SD, Barrett R, Spector W, Limcangco R. Exploratory study of nursing home factors associated with successful implementation of clinical decision support tools for pressure ulcer prevention. Adv Skin Wound Care. 2013;26(2):83-92;quiz 93-84. [DOI] [PubMed] [Google Scholar]
- 23. Cherry B. Assessing organizational readiness for electronic health record adoption in long-term care facilities. J Gerontol Nurs. 2011;37(10):14-19. [DOI] [PubMed] [Google Scholar]
- 24. Galani M. Factors Affecting Nursing Staff Use of Nursing Information Systems in Residential Aged Care Homes. 2015. Doctoral Thesis, University of Wollongong, Australia. Retrieved from ro.uow.edu/theses/4422
- 25. Rantz MJ, Alexander G, Galambos C, et al. The use of bedside electronic medical record to improve quality of care in nursing facilities: a qualitative analysis. Comput Inform Nurs. 2011;29(3):149-156. [DOI] [PubMed] [Google Scholar]
- 26. Wang T, Biedermann S. Adoption and utilization of electronic health record systems by long-term care facilities in Texas. Perspect Health Inf Manag. 2012;9(Spring):1g. [PMC free article] [PubMed] [Google Scholar]
- 27. Rantz M, Scott-Cawiezell J, Alexander G, et al. Evaluation of the Use of Bedside Technology to Improve Quality of Care in Nursing Facilities. Research Triangle Park, NC: RTI International; December 2006. [Google Scholar]
- 28. Yu P, Qiu Y, Crookes P. Computer-based nursing documentation in nursing homes: a feasibility study. Stud Health Technol Inform. 2006;122:570-574. [PubMed] [Google Scholar]
- 29. Munyisia E, Yu P, Hailey D. The effect of an electronic health record system on nursing staff time in a nursing home: a longitudinal cohort study. Australas Med J. 2014;7(7):285-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Munyisia EN, Yu P, Hailey D. Caregivers’ time utilization before and after the introduction of an electronic nursing documentation system in a residential aged care facility. Methods Inf Med. 2013;52(5):403-410. [DOI] [PubMed] [Google Scholar]
- 31. Qian S, Yu P, Hailey DM. The impact of electronic medication administration records in a residential aged care home. Int J Med Inform. 2015;84(11):966-973. [DOI] [PubMed] [Google Scholar]
- 32. Hustey FM, Palmer RM. Implementing an Internet-based communication network for use during skilled nursing facility to emergency department care transitions: challenges and opportunities for improvement. J Am Med Dir Assoc. 2012;13(3):249-253. [DOI] [PubMed] [Google Scholar]
- 33. Munyisia EN, Yu P, Hailey D. Does the introduction of an electronic nursing documentation system in a nursing home reduce time on documentation for the nursing staff? Int J Med Inform. 2011;80(11):782-792. [DOI] [PubMed] [Google Scholar]
- 34. Brandeis GH, Hogan M, Murphy M, Murray S. Electronic health record implementation in community nursing homes. J Am Med Dir Assoc. 2007;8(1):31-34. [DOI] [PubMed] [Google Scholar]
- 35. Lapane KL, Hiris J, Hughes CM, Feinberg J. Development and implementation of pharmaceutical care planning software for nursing homes based on the Fleetwood Model. Am J Health Syst Pharm. 2006;63(24):2483-2487. [DOI] [PubMed] [Google Scholar]
- 36. Vogelsmeier AA, Halbesleben JR, Scott-Cawiezell JR. Technology implementation and workarounds in the nursing home. J Am Med Dir Assoc. 2008;15(1):114-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zamora Z, McCall B, Patel L, et al. Implementation of a web-based system to improve the transitional care of older adults. Journal of Nursing Care Quality. 2012;27(2):182-189. [DOI] [PubMed] [Google Scholar]
- 38. Alexander GL, Rantz M, Galambos C, et al. Preparing nursing homes for the future of health information exchange. Appl Clin Inform. 2015;6(2):248-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Alexander GL, Madsen R. IT sophistication and quality measures in nursing homes. J Gerontol Nurs. 2009;35(7):22-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cherry BJ, Ford EW, Peterson LT. Experiences with electronic health records: early adopters in long-term care facilities. Health Care Manage Rev. 2011;36(3):265-274. [DOI] [PubMed] [Google Scholar]
- 41. Kruger K, Strand L, Geitung JT, Eide GE, Grimsmo A. Can electronic tools help improve nursing home quality? ISRN Nurs. 2011;2011:Article 208142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Engstrom M, Ljunggren B, Lindqvist R, Carlsson M. Staff perceptions of job satisfaction and life situation before and 6 and 12 months after increased information technology support in dementia care. J Telemed Telecare. 2005;11(6):304-309. [DOI] [PubMed] [Google Scholar]
- 43. Faxvaag A, Johansen TS, Heimly V, Melby L, Grimsmo A. Healthcare professionals’ experiences with EHR-system access control mechanisms. Stud Health Technol Inform. 2011;169:601-605. [PubMed] [Google Scholar]
- 44. Yu P, Zhang Y, Gong Y, Zhang J. Unintended adverse consequences of introducing electronic health records in residential aged care homes. Int J Med Inform. 2013;82(9):772-788. [DOI] [PubMed] [Google Scholar]
- 45. Cherry B, Carpenter K. Evaluating the effectiveness of electronic medical records in a long term care facility using process analysis. J Healthc Eng. 2011;2(1):75-86. [Google Scholar]
- 46. Qian S, Ping YU. Fitting clinical workflow: the case for wound care in a residential aged care home. Stud Health Technol Inform. 2014;204:130-136. [PubMed] [Google Scholar]
- 47. Munyisia EN, Yu P, Hailey D. The changes in caregivers’ perceptions about the quality of information and benefits of nursing documentation associated with the introduction of an electronic documentation system in a nursing home. Int J Med Inform. 2011;80(2):116-126. [DOI] [PubMed] [Google Scholar]
- 48. Alexander GL, Pasupathy KS, Steege LM, Strecker EB, Carley KM. Multi-disciplinary communication networks for skin risk assessment in nursing homes with high IT sophistication. Int J Med Inform. 2014;83(8):581-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Scott-Cawiezell J, Madsen RW, Pepper GA, Vogelsmeier A, Petroski G, Zellmer D. Medication safety teams’ guided implementation of electronic medication administration records in five nursing homes. Jt Comm J Qual Patient Saf. 2009;35(1):29-35. [DOI] [PubMed] [Google Scholar]
- 50. Boffa DP, Pawola LM. Identification and conceptualization of nurse super users. J Healthc Inf Manag. 2006;20(4):60-68. [PubMed] [Google Scholar]
- 51. Alexander GL, Rantz M, Flesner M, Diekemper M, Siem C. Clinical information systems in nursing homes: an evaluation of initial implementation strategies. Comput Inform Nurs. 2007;25(4):189-197. [DOI] [PubMed] [Google Scholar]
- 52. Alexander GL, Steege LM, Pasupathy KS, Wise K. Case studies of IT sophistication in nursing homes: a mixed method approach to examine communication strategies about pressure ulcer prevention practices. Int J Ind Ergon. 2015;49:156-166. [Google Scholar]
- 53. Colón-Emeric CS, Schmader KE, Twersky J, Kuchibhatla M, Kellum S, Weinberger M. Development and pilot testing of computerized order entry algorithms for geriatric problems in nursing homes. J Am Geriatr Soc. 2009;57(9):1644-1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Filipova AA. Electronic health records use and barriers and benefits to use in skilled nursing facilities. Comput Inform Nurs. 2013;31(7):305-318. [DOI] [PubMed] [Google Scholar]
- 55. Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood). 2011;30(3):464-471. [DOI] [PubMed] [Google Scholar]
- 56. Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12(5):505-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Yuan CT, Bradley EH, Nembhard IM. A mixed methods study of how clinician “super users” influence others during the implementation of electronic health records. BMC Med Inform Decis Mak. 2015;15:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, INQ-17-0300.Supplemental_Material.Revision for Nursing Home Implementation of Health Information Technology: Review of the Literature Finds Inadequate Investment in Preparation, Infrastructure, and Training by Michelle Ko, Laura Wagner and Joanne Spetz in INQUIRY: The Journal of Health Care Organization, Provision, and Financing