Abstract
Background
Irritable bowel syndrome (IBS) reduces health related quality of life (HRQOL). It is unclear how having IBS modifies the impact of gastrointestinal (GI), psychosocial and somatic symptom variables on HRQOL compared to healthy controls (HCs).
Aims
1) Determine psychosocial, somatic and physical status variables most predictive of HRQOL in IBS and HCs and 2) Determine if IBS status modifies relationships between predictive factors and HRQOL.
Methods
IBS patients and HCs completed validated questionnaires measuring GI symptoms, psychosocial/somatic variables, and physical (PCS) and mental (MCS) HRQOL via the Short-Form-36. Associations between these variables and HRQOL were evaluated with multiple linear regressions. Variables were standardized to determine the strongest predictors of HRQOL. Statistical significance level was 0.01.
Results
Mean HRQOL was higher in 417 HCs vs 290 IBS subjects (PCS 55.6 vs 48.6 p<0.001, MCS 53.7 vs 44.8 p<0.001). GI symptom measures were negatively associated with PCS in IBS, but only usual severity was associated with MCS (p<0.01). In all subjects, psychosocial and somatic measures were associated with MCS and not PCS excluding GI symptom anxiety, which correlated with both (p<0.01). The strongest predictor of MCS was perceived stress in IBS and depression symptoms in HCs. GI symptom anxiety was the strongest predictor of PCS in both. Greater perceived stress and somatic symptom severity and less mindfulness was linked to larger depressions in HRQOL for IBS compared to HCs (p<0.01).
Conclusions
GI symptom severity and anxiety correlate with PCS while psychosocial/somatic measures parallel MCS. However, HRQOL is comparable in IBS and HCs when perceived stress, somatic symptom severity, and mindfulness are at optimal levels. These findings may have important implications.in the management of IBS.
Keywords: irritable bowel syndrome, health related quality of life, perceived stress, mindfulness, anxiety
Introduction
Irritable bowel syndrome (IBS) is a common and burdensome brain-gut disorder with an incidence of 10-22% in the general population;1 IBS is characterized by fluctuating abdominal pain and altered bowel habits with symptom intensity often related to poor illness coping, negative cognitions such as catastrophizing, and increased negative affect including anxiety and depression.2-4 The pathophysiology of IBS is often conceptualized via the biopsychosocial framework, which integrates the concepts of maladaptive thoughts, affective symptoms, cognitive change and vulnerable physiologic substrate to explain health outcomes and health related quality of life (HRQOL) in IBS.5
Disease burden in IBS can be measured by GI symptom intensity, healthcare resource utilization, productivity loss, and HRQOL. From the patient perspective, HRQOL serves as a principal gauge of physical and emotional disease burden. IBS lowers HRQOL to a similar degree as the flu or chronic renal disease.6,7 Significant research has been directed at identifying the drivers of diminished HRQOL to improve patient well-being, productivity and healthcare overutilization.8,9 HRQOL has physical and mental facets typically assessed in tandem to add insight and understanding to how well individuals function from an emotional or physical standpoint.
Studies have assessed factors associated with the mental and physical components of generic HRQOL in IBS patients. Known predictors of HRQOL in IBS include physical symptoms (i.e., pain, bloating, overall severity) and psychosocial variables (i.e., mindfulness, catastrophizing, anxiety, depression, illness specific fears) and somatic measures (presence of widespread symptoms). Interestingly, GI symptom intensity and frequency, core criteria for diagnosing and assessing IBS severity, are relevant but not the strongest predictors of HRQOL. GI symptom severity has minimal effect on the mental aspect of HRQOL;10-13 Spiegel et al. (2004) found that severe symptoms and predominantly painful symptoms were associated with physical HRQOL but all remaining predictors of physical and mental HRQOL were related to extraintestinal symptoms such as tiring easily, feeling nervous, tense, or hopeless. Lackner et al. (2014) reported only a modest relationship between IBS symptom severity and self-rated health in IBS, while psychosocial and extraintestinal factors accounted for the majority of variability. Unlike IBS GI severity, psychosocial and somatic variables are more predictive of mental quality of life.8,14-17 However, the most robust psychosocial and somatic symptom predictors of HRQOL are incompletely known and require additional investigation in order to optimize disease management.
Although IBS patients overall have a decreased HRQOL compared to healthy control subjects, there is a lack of studies which have compared predictors of HRQOL between IBS subjects and healthy controls (HCs). It is important to know if HRQOL is similarly affected in IBS patients and healthy controls or if there is a unique relationship between certain factors and HRQOL in IBS. Determining this information could promote more timely identification of at-risk IBS patients and facilitate targeted treatments of disease specific drivers of depressed HRQOL in IBS. Conceivably, optimizing these culprit physical and psychosocial variables could improve well-being to the level of healthy individuals.
Thus, the aims of our study are to: 1) Determine psychosocial and physical status measures most predictive of HRQOL in IBS and HCs and 2) Determine if IBS status modifies the relationship between predictive factors and HRQOL.
We hypothesize that both psychosocial variables and somatic symptoms will correlate closely with HRQOL, more so than physical GI symptoms. Furthermore we expect the strongest predictors of HRQOL to be distinct between IBS and HCs. Lastly we suspect IBS status will enhance the negative impact of various psychosocial and somatic variables on HRQOL compared to HCs.
Methods
Subjects and Clinical Characteristics
We recruited male and female participants at least 18 years old between June 2010 and June 2016. All subjects had a medical history and physical examination. The majority of IBS subjects (>90%) were recruited from community advertisement with the remaining minority recruited from GI clinics. A clinician with expertise in IBS confirmed the diagnosis of IBS and bowel habit subtype (i.e. IBS with constipation [IBS-C], IBS with diarrhea [IBS-D], IBS with mixed bowel habit pattern [IBS-M], and IBS unsubtyped [IBS-U]) based on the Rome III diagnostic criteria.18 HCs were recruited via community advertisement, did not have a history of IBS, other chronic GI conditions or pain disorders and were not taking psychotropic medications or participating in psychotherapy. Additional exclusion criteria for all subjects included history of infectious or inflammatory disorders, particularly those which can mimic IBS symptoms (e.g., inflammatory bowel disease, infectious gastroenteritis, diverticulitis, etc), other active chronic medical illnesses (e.g., chronic obstructive pulmonary disease, diabetes, chronic renal or cardiac disease, autoimmune disorders), active psychiatric illness over the past 6 months as assessed by structured clinical interview for the DSM-IV (MINI), and current tobacco or alcohol abuse. Compensation was provided for completion of questionnaires. All subjects completed the full array of survey tools. No previous publications including these participants have specifically examined the relationships or hypotheses of the current study.
GI Symptom Assessment
Bowel symptom Questionnaire (BSQ)
This questionnaire surveys Rome III IBS symptoms, and recent overall GI symptoms, abdominal pain, and bloating over the past week (rated on a 0-20 numeric rating scale anchored by “no symptoms” and “most intense symptoms imaginable”). The questionnaire also quantifies usual symptom severity (“How bad are your symptoms usually? 1=None: no symptoms, 2=Mild: can be ignored if I don’t think about it, 3=Moderate: cannot be ignored, but does not affect my lifestyle, 4=Severe: affects my lifestyle, 5=Very severe: markedly affects my lifestyle”).
Psychosocial and Somatic Symptom Measures
GI symptom-specific Anxiety
The validated Visceral Sensitivity Index (VSI) is a 15-item survey used to assess fear of GI symptoms.19 A 6-point Likert scale was employed to rate items and specify a negative consequence to experiencing GI-specific anxiety. High scores indicated greater GI symptom anxiety.
Somatic symptom severity
The Patient Health Questionnaire (PHQ-15) is a self-administered version of the PRIME-MD diagnostic instrument for common mental disorders. The tool comprises 15 somatic symptom questions scored from 0 (“not bothered at all”) to 2 (“bothered a lot”). The questionnaire contains 14 of the 15 most prevalent DSM-IV somatization disorder somatic symptoms.20 For the purpose of our study, we omitted GI-specific symptoms to prevent confounding with physical GI symptom data. This yields a PHQ-12 questionnaire devoid of GI-specific somatic complaints that has been employed to assess somatic symptom intensity without inflation by the three GI symptoms.21
Anxiety and Depression symptoms
The Hospital Anxiety and Depression Scale (HAD-A/D) is a 14-item questionnaire that is a well-validated, brief inventory for assessment of current symptoms pertaining to anxiety and depression that is widely employed for studies of medical subjects.22
Catastrophizing
Coping Strategies Questionnaire - Catastrophizing Subscale (CSQ) measures coping strategies in patients with chronic problems.23 It features eight subscales including diverting attention, reinterpreting pain sensations, coping self-statements, ignoring pain behaviors, praying or hoping, increasing activity level and catastrophizing. Our study utilized the catastrophizing subscale, which comprises six questions rated 0 (“never”) to 6 (“always”) regarding frequency of catastrophizing feelings about their symptoms such as “It’s terrible and I feel it’s never going to get better.”
Perceived Stress
The Perceived Stress Scale (PSS) is a 10-question Likert-type rating scale. It is one of the most widely employed scales for measuring perceived stress; the tool has been validated in studies examining severity of stressful situations, associations between stress and psychiatric or physical health and effectiveness of stress-reducing techniques. The scale measures the degree to which situations in one’s life are deemed stressful, where demands exceed a person’s ability to cope. Subjects are asked to report frequency of feelings in each question on a scale of 0 (never) to 4 (very often).24
Mindfulness
The Mindfulness Attention Awareness Scale (MAAS) is a 15-item scale detailing characteristics of dispositional mindfulness, specifically, open or receptive awareness of and attention to what is taking place in the present moment. This measure features robust psychometric properties and is validated in college, community, and cancer subjects. The MAAS reveals a state of consciousness that is correlated with and predictive of a variety of self-regulation and well-being constructs.25
Quality of Life Assessment
HRQOL
Generic HRQOL was assessed using the Short Form (SF-36) health survey composite scores of mental (MCS) and physical (PCS) well-being. Validated and widely employed to assess health outcome in a multitude of diseases, the SF health survey characterizes the effect of medical conditions and pain on physical and emotional well-being and limitation of day-to-day and pleasurable activities.26 The SF-12 MCS and PCS are scored from 0–100, with higher scores reflecting better HRQOL. The survey tool assesses eight subdomains of quality of life including general health, physical functioning, role functioning (physical), bodily pain, vitality, role functioning (emotional), mental health and social functioning.
Statistical Analysis
Our sample size was estimated a priori using effect size estimates provided by Lackner et al. (2014) where GI symptoms predicted an additional 14% of variability in physical quality of life (effect size f2 = 0.166) and 39.8% of variability in mental quality of life (f2 = 0.66) in IBS subjects beyond the variability explained by clinical characteristics.10 Using G*Power 3.1.9.2 and an F-test based on an α error rate of 5%, a range of 28 to 85 subjects was needed to detect these effect sizes (f2=0.166 and f2=0.66) with 80% power.
Multiple linear regression was used to examine relationships between HRQOL and GI/non-GI measures, IBS status, and the interaction of IBS status with psychosocial and somatic symptom measures, while controlling for age, sex, and education. Significance was set at p <0.01 due to two HRQOL outcomes and two predictor types (non-GI and GI) using a Bonferroni adjustment for multiple comparisons: 0.05/4 (rounded down). To ensure that bowel symptom intensity did not confound the outcomes, we controlled for GI usual severity in the regression models evaluating the individual psychological and somatic symptoms’ impact on quality of life among IBS subjects. Linear extrapolations of HRQOL at varying levels of GI/non-GI measures were produced for HC and IBS populations, with confidence intervals reflected in the shaded regions of each figure to indicate the precision of the prediction.
In a separate analysis to evaluate the strongest predictors of HRQOL, psychosocial and somatic symptom predictors were standardized (by subtracting the mean and dividing by the standard deviation) to assess their relative strengths predicting HRQOL. The strongest predictors based on the magnitude of the standardized coefficients are indicated by bold font.
Results
Clinical Characteristics
Subjects included 290 IBS patients (69% women, mean age 35 yrs, 23.8% IBS-C, 24.8% IB S-D, 47.2% IBS-M, and 4.1% IBS-U) and 417 HCs (74% women, mean age 30 yrs). As expected, HRQOL was higher in HCs compared to IBS (PCS 55.6 vs 48.6 p<0.001, MCS 53.7 vs 44.8 p<0.001). All psychosocial and somatic symptom measures significantly differed between HCs and IBS (Table 1).
Table 1.
Healthy control and IBS patient characteristics
| Variable | HC (n=417) | IBS (n=290) | p-value |
|---|---|---|---|
| Age (years) | 30.09 (10.57) | 35.32 (12.25) | p<0.001 |
| BMI | 24.48 (4.8) | 24.85 (4.91) | 0.41 |
| Female: n (%) | 288 (69) | 214 (74) | 0.201 |
| Education: n (%) | 0.003 | ||
| HS/HS Graduate | 19 (4.69) | 24 (8.54) | |
| Some College | 183 (45.19) | 90 (32.03) | |
| College Graduate | 127 (31.36) | 101 (35.94) | |
| Post College | 76 (18.77) | 66 (23.49) | |
| IBS Subtype: n (%) | |||
| IBS-C | 69 (23.79) | ||
| IBS-D | 72 (24.83) | ||
| IBS-U | 12(4.14) | ||
| IBS-M | 137 (47.24) | ||
| GI Symptom Measures | |||
| Overall Severity, 0-20 | 10.28 (4.31) | ||
| Abdominal Pain, 0-20 | 9.23 (4.92) | ||
| Bloating, 0-20 | 10.94 (5.33) | ||
| Usual Severity, 1-5 | 3.14 (0.71) | ||
| Psychosocial and Somatic Measures | |||
| VSI Score, 0-90 | 2.6 (4.88) | 35.33 (16.62) | p<0.001 |
| PHQ 12, 0-24 | 1.84 (1.86) | 5.75 (4.02) | p<0.001 |
| HAD Anxiety, 0-21 | 3.38 (2.8) | 7.48 (4.15) | p<0.001 |
| HAD Depression, 0-21 | 1.35 (1.88) | 3.78 (3.26) | p<0.001 |
| CSQ Score, 0-6, averaged | 0.38 (0.66) | 1.31 (1.19) | p<0.001 |
| PSS Score, 0-40 | 10.92 (6.58) | 16.59 (7.06) | p<0.001 |
| MAAS, 1-6, averaged | 4.60 (0.82) | 4.19 (0.91) | p<0.001 |
| SF12 MCS, 0-100 | 53.65 (7.24) | 44.85 (10.89) | p<0.001 |
| SF12 PCS, 0-100 | 55.55 (3.41) | 48.6 (8.89) | p<0.001 |
Mean values (standard deviation) are shown.
Abbreviations: HAD = Hospital Anxiety and Depression, CSQ = Coping Strategies Questionnaire (catastrophizing subscale), PSS = Perceived Stress Scale, VSI = visceral sensitivity index, MAAS = Mindfulness Awareness Assessment Scale, PHQ-12 = Patient Health Questionnaire-12 (Somatization Severity Scale without GI features), SF-12 = Short Form 12, PCS = Physical Component Score, MCS = Mental Component Score, IBS-C = IBS Constipation, IBS-D = IBS Diarrhea, IBS-U = IBS Unspecified, IBS-M = IBS Mixed
GI Symptom Burden and HRQOL
The individual impact of GI and psychological and somatic symptoms on HRQOL in IBS and HC subjects is reported in Table 2 (non-standardized coefficients and 95% confidence intervals). All GI symptom measures (usual severity, overall severity, bloating, abdominal pain) displayed a significant, inverse relationship with PCS (p<0.01). However, GI symptoms did not correlate with MCS, except for usual severity, which was significantly inversely related to MCS (p<0.01). Even though current abdominal pain rating negatively correlated with MCS, the results did not meet our significance threshold of p<0.01.
Table 2.
Estimated coefficients between predictors and HRQOL
| Physical QOL (PCS), β (95% CI) | Mental QOL (MCS), β (95% CI) | |||
|---|---|---|---|---|
| Psychosocial and Somatic Measures | HCs | IBS | HCs | IBS |
| HAD Anxiety | 0.12 (0,0.23) | -0.19 (-0.43,0.06) | -1.37 (-1.59,-1.15)** | -1.31 (-1.58,-1.04)** |
| HAD Depression | -0.08 (-0.26,0.1) | -0.57 (-0.87,-0.26)** | -2.24 (-2.55,-1.92)** | -1.97 (-2.29,-1.65)** |
| CSQ | -0.27 (-0.77,0.24) | -0.93 (-1.79,-0.07)* | -3.92 (-4.94,-2.89)** | -4.59 (-5.54,-3.64)** |
| PSS | 0.03 (-0.02,0.08) | -0.02 (-0.17,0.12) | -0.66 (-0.75,-0.58)** | -1 (-1.14,-0.86)** |
| VSI | -0.13 (-0.2,-0.06)** | -0.17 (-0.23,-0.11)** | -0.21 (-0.36,-0.05)** | -0.17 (-0.25,-0.1)** |
| MAAS | -0.28 (-0.72,0.16) | 0.16 (-1.09,1.41) | 3.13 (2.23,4.03)** | 6.73 (5.34,8.12)** |
| PHQ-12 | -0.2 (-0.38,-0.02)* | -0.74 (-0.98,-0.5)** | -1.56 (-1.94,-1.19)** | -0.95 (-1.26,-0.64)** |
| GI Symptoms | ||||
| Overall severity | -0.55 (-0.79,-0.32)** | -0.29 (-0.59,0.02) | ||
| Abdominal Pain | -0.34 (-0.55,-0.14)** | -0.29 (-0.55,-0.02)* | ||
| Bloating | -0.3 (-0.49,-0.1)** | -0.25 (-0.49,0.004) | ||
| Usual Severity | -3.15 (-4.58,-1.71)** | -2.46 (-4.31,-0.6)** | ||
adjusted p<0.05,
adjusted p<0.01
bolded terms are the strongest relative predictors
HAD = Hospital Anxiety and Depression
CSQ = Coping Strategies Questionnaire (catastrophizing subscale)
PSS = Perceived Stress Scale
VSI = visceral sensitivity index
MAAS = Mindfulness Awareness Assessment Scale
PHQ-12 = Patient Health Questionnaire – 12
Psychosocial and Somatic Symptom Assessment
In all subjects, psychosocial and somatic symptom measures were significantly associated with MCS (p<0.01) and not PCS excluding GI symptom anxiety (VSI), which correlated with both (p<0.01) (Table 2). VSI was the only significant predictor of PCS within both IBS and HC groups. HAD-depression and PHQ-12 showed significant correlations with PCS in IBS (p<0.01) but not HCs. When psychosocial and somatic symptom variables were standardized, the strongest predictor of MCS was PSS in IBS patients and HAD-depression in HCs. VSI was the strongest predictor of PCS in both IBS patients and HCs (Table 2). When adjusted for usual severity, a comprehensive measure of IBS GI symptom intensity, these findings were unchanged.
Modification of HRQOL predictors due to IBS
IBS status significantly altered the relationships of PSS and MAAS with MCS (Figure 1), and PHQ-12 with PCS (Figure 2). IBS subjects exhibited larger changes in QOL per unit change in PSS, MAAS or PHQ-12 compared to HCs (all p<0.01, Table 3). In other words, a similar degree of worsening in perceived stress, mindfulness or somatic symptom severity was associated with a greater decline in HRQOL in IBS vs. HCs. In IBS subjects, there was a significant correlation of MAAS scores and PSS (p<0.001, Figure 3). IBS status did not meaningfully augment HRQOL outcomes for the other psychosocial and somatic symptom factors.
Figure 1.
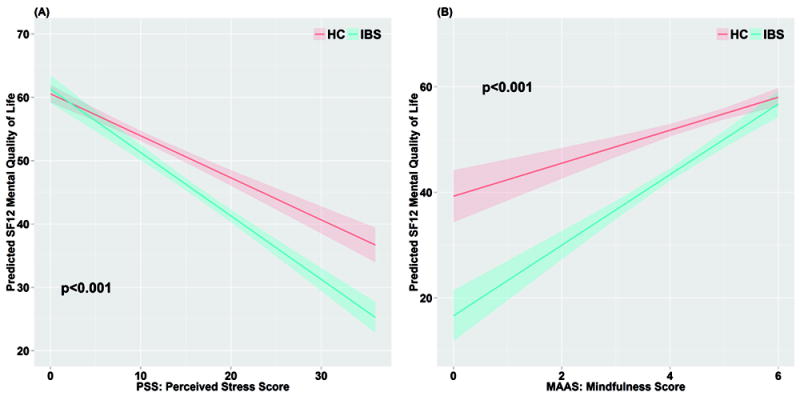
Regression model of IBS status moderating the effect of perceived stress score (PSS) (A) and mindfulness (MAAS) (B) on mental quality of life (MCS). There was a greater decline of MCS with worsening of PSS and MAAS scores in IBS compared to HCs (p<0.01). HCs = healthy controls, IBS = IBS population.
Figure 2.
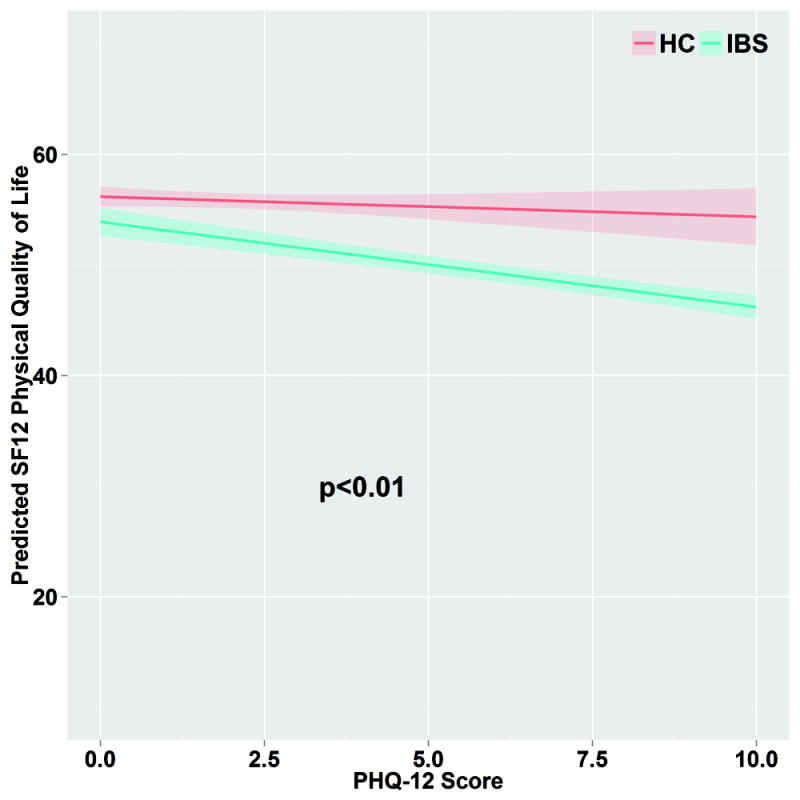
Regression model of IBS status moderating the effect of somatic symptom burden (PHQ-12) on physical quality of life (PCS). There was a greater decline of PCS with worsening PHQ-12 in IBS compared to HCs (p<0.01). HCs = healthy controls, IBS = IBS population.
Table 3.
Interaction p-value of IBS status and psychosocial/somatic measures on MCS/PCS QOL relationships
| Psychosocial and Somatic Symptom Measures | Physical QOL (PCS), p-value | Mental QOL (MCS), p-value |
|---|---|---|
| HAD-A | 0.036 | 0.808 |
| HAD-D | 0.011 | 0.196 |
| CSQ | 0.209 | 0.386 |
| PSS | 0.588 | <0.01 |
| VSI | 0.618 | 0.701 |
| MAAS | 0.820 | <0.01 |
| PHQ-12 | <0.01 | 0.011 |
HAD = Hospital Anxiety and Depression (A = anxiety) (D = depression)
CSQ = Coping Strategies Questionnaire (catastrophizing subscale)
PSS = Perceived Stress Scale
VSI = visceral sensitivity index
MAAS = Mindfulness Awareness Assessment Scale
PHQ-12 = Patient Health Questionnaire – Somatization Severity Scale
Figure 3.
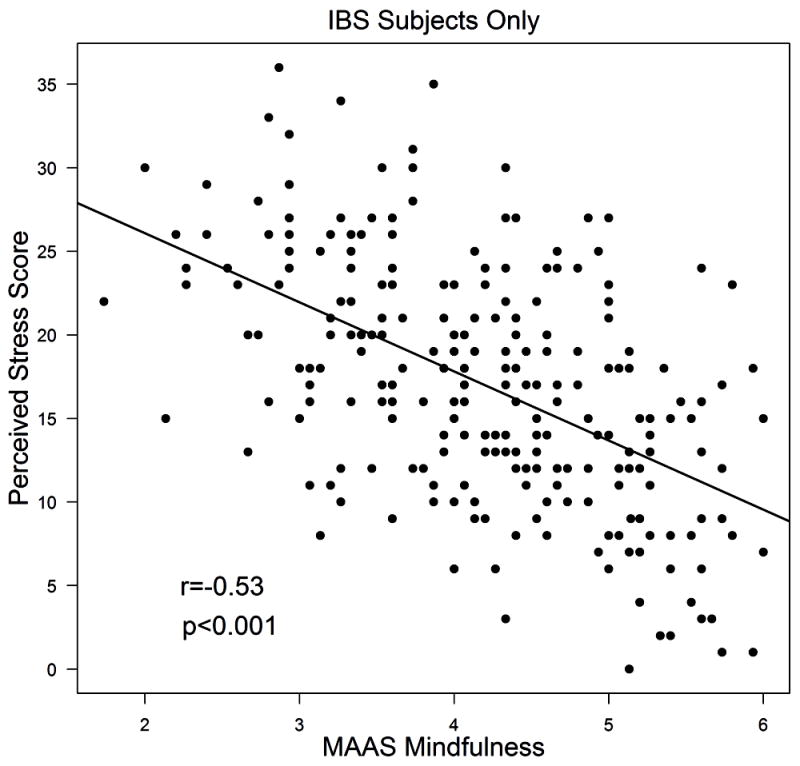
Scatter plot of mindfulness (MAAS) score versus perceived stress score (PSS) in IBS patients. Significant inverse relationship between MAAS and PSS (p<0.001).
Discussion
This study sought to identify relevant GI, psychosocial and somatic symptom predictors of HRQOL in IBS, and to analyze how IBS status modifies these relationships when compared to HCs. Our main findings were: 1) Mental and physical HRQOL were lower in IBS compared to HCs, 2) In IBS, GI symptom severity was significantly associated with physical, but not mental, HRQOL, 3) Psychosocial and somatic symptom measures correlated closely with mental HRQOL, but less so with physical HRQOL in IBS and HCs, 4) The strongest predictor of mental HRQOL differed between IBS and HCs with perceived stress (PSS) being the strongest predictor in IBS whereas current depression symptoms was the strongest predictor in HCs, 5) The strongest predictor of physical HRQOL in both IBS and HCs was GI symptom anxiety, and 6) IBS status modified the relationships between psychosocial and somatic symptom measures and HRQOL; in IBS and HCs with lower perceived stress or greater mindfulness, mental HRQOL in IBS equaled that of HCs. Likewise, in IBS and HCs with lower somatic symptom severity, physical HRQOL in IBS approached that of HCs.
Our findings reproduce previous findings that GI symptom severity (e.g., abdominal pain or bloating) have some predictive ability of physical HRQOL but are poor predictors of mental HRQOL compared to psychosocial and somatic symptom measures.10,13,14,17,21,24 However, GI symptom related anxiety, and not GI symptom severity, was the strongest predictor of physical HRQOL in IBS patients. Prior studies have noted the importance of GI symptom related anxiety as an independent and robust predictor of HRQOL in IBS,10-12 but it has not been well evaluated in HCs. While some IBS patients have a co-morbid anxiety disorder, many patients have anxiety symptoms related to their GI symptoms (i.e., GI symptom related anxiety) rather than a generalized anxiety disorder.28 Anxiety predominantly related to GI symptoms is understandable given the uncertainty and unpredictability associated with symptom occurrence that IBS patients report. Patients often do not know when, where or what will trigger symptoms, are uncertain what to eat and do not feel a sense of control over their symptoms.29 Differentiating GI symptom anxiety and a generalized anxiety disorder has potential clinical implications. For example, cognitive behavioral therapy (CBT) relieves IBS-related fear and avoidance behaviors in IBS regardless of comorbid psychological distress including generalized anxiety disorder; evidence suggests that maladaptive cognitions drive GI symptom anxiety. Thus GI symptom anxiety can occur independent of any generalized anxiety disorder and may require targeted or specialized therapy.30,31
Concordantly, we observed that in HCs, who did not have chronic or recurrent IBS symptoms, GI symptom anxiety was the strongest predictor of physical HRQOL of the measures tested including somatic symptom severity. GI symptoms are among the most common of bothersome symptoms among the general population. A large scale U.S. population survey of 13,568 participants found that 6 of the 26 most common and bothersome physical symptoms were abdominal pain, nausea, vomiting, gas, diarrhea, and constipation with lifetime prevalence rates ranging from 6% to 23.6%.32 A recent study by Cuenen and colleagues (2016) demonstrated that fear towards innocuous GI symptoms can develop in healthy individuals through an association with more painful GI symptoms.33 This associative learning has been shown to not only cause emotional distress but to increase perception of GI sensations.34 The VSI, a measure of GI symptom related anxiety and fear was developed to be sensitive to individuals’ degree of concern regarding typical GI symptoms. Thus, individuals without GI symptoms can have some level, albeit lower, of GI symptom anxiety that affects HRQOL.
Our data newly illustrates the importance of perceived stress as the strongest predictor of mental HRQOL in IBS patients, a relationship which has been studied to a limited degree in IBS. PSS is one of the most widely used instruments for measuring the degree to which an individual perceives situations to be stressful and has been used to predict objective biological markers of stress and increased risk for disease.24,35-38 Perceived stress, thought of as a patient’s appraisal of stress or cognitive perception of stress burden, exists as a summation of many diverse factors, conscious or subconscious, that contribute to total stress. Perceived stress has been shown to independently correlate with the presence of IBS,39 self-rated health,11 and HRQOL in IBS.40 Because IBS is a stress-sensitive disorder,41 we expected PSS, which serves as an appraisal of current stress, to have a robust impact on HRQOL. Stress is known to be associated with the onset and symptom flares of IBS.42 In addition, stress can affect the hypothalamic-pituitary-adrenal axis, autonomic nervous system, and GI motility, secretion, perception, and permeability, which have all been shown to be altered in IBS.43 In HCs, although PSS correlated with MCS, current depression symptoms was a stronger predictor.
Another main finding in our study is that the impact of PSS, MAAS and PHQ-12 on HRQOL was stronger for IBS patients compared to HCs. In IBS patients with high levels of mindfulness or low levels of perceived stress, mental HRQOL was similar to that of HCs. Physical HRQOL exhibited a similar trend in IBS and HCs when somatic symptom severity was lowest. Clearly these variables convey unique significance to HRQOL in IBS patients compared to healthy individuals. To explore why, one could consider perceived stress as a cumulative manifestation of the most relevant psychosocial and somatic symptom predictors of mental HRQOL; furthermore exhibiting low perceived stress appears to be linked with experiencing high levels of a protective quality, such as mindfulness,44 that promotes HRQOL.45 Mindfulness is a way of paying attention to the present moment (including bodily sensations, thoughts and emotions) in a non-judgmental way leading to less symptom rumination and catastrophizing.46-48 We found that those with higher levels of mindfulness had lower perceived stress. Evidence has shown that perceived stress and general health were significantly improved with mindfulness training.49 Mindfulness-based stress reduction training and mindfulness-based cognitive therapy are used to improve chronic pain, mental health disorders and maladaptive thought patterns50,51 and has been shown to be effective in IBS.52-58 Our data supports the notion that mindfulness facilitates lower perceived stress and therefore improves HRQOL; though this cross sectional analysis can only offer correlation and not causation. Furthermore, these findings are based upon a presumed linear relationship between predictor and HRQOL as yielded by an extrapolation analysis; thus alternative nonlinear or threshold associations were not considered.
Our observational findings also suggest that improving somatic symptoms, much like perceived stress, could conceivably produce HRQOL similar to that of HCs, but further studies are needed. IBS is considered to be a functional somatic syndrome, and somatic symptom severity is a significant driver of illness burden directly associated with increased IBS severity,59,4 decreased HRQOL27 and increased healthcare utilization.60 Our findings suggest that targeting IBS management efforts on reducing perceived stress and somatic symptom severity and enhancing mindfulness can potentially have a dramatic effect on HRQOL in IBS, although further studies are needed.
Limitations of this study stem from its cross-sectional nature, which confines interpretation to associative rather than causal. The populations studied were selected primarily from the Los Angeles community, which may limit the applicability of our findings. While we performed history and physical examinations on all subjects and excluded those with significant ongoing medical illnesses other than IBS, we assessed ‘functional’ comorbidities via the PHQ but there may have been some subjects with other illnesses that we were not aware of. We did not test for independence of psychosocial and somatic symptom variables with respect to HRQOL because of their inter-relatedness. Most of the characteristics described are well known to fluctuate in concordant directions when examined. However, we employed well-validated tools that are universally applied to describe these psychosocial and somatic symptom measures in the aim of investigating distinct concepts.
In conclusion, this study highlights the relevance of several psychosocial and somatic symptom measures that display unique significance to HRQOL in IBS patients when compared to HCs, which supports the unifying concept that IBS is a brain-gut disorder with a clinical presentation and overall well-being that represents the integration of perceived stress, symptom anxiety and widespread symptoms. IBS patient care encounters are often anchored around GI symptom burden (e.g., bowel pattern/frequency or abdominal pain) which are important to address, but overall well-being can be overlooked or difficult to conceptualize in the patient-provider encounter. To adequately assess and manage disease burden, timely appraisal of HRQOL and initiation of therapy when it is diminished should be prioritized, though many healthcare professionals overlook this metric.61 Our findings are helpful in highlighting potential therapeutic targets, such as perceived stress, mindfulness and somatic symptom severity, that when minimized (or maximized in the case of mindfulness) are associated with a HRQOL comparable to HCs.
Acknowledgments
Grant support: NIH/NIDDK P50 DK64539, R01 DK048351, P30 DK 41301
Footnotes
- Ray Addante: study concept and design, analysis and interpretation of data, drafting of the manuscript; critical revision of the manuscript for important intellectual content
- Bruce Naliboff: study concept and design, analysis and interpretation of data, critical revision of the manuscript for important intellectual content
- Wendy Shih: acquisition of data, analysis and interpretation of data, statistical analysis, critical review and editing of manuscript
- Angela P. Presson: analysis and interpretation of data, critical review and editing of the manuscript
- Kirsten Tillisch: critical revision and editing of the manuscript for important intellectual content
- Emeran Mayer: funding, critical revision of the manuscript for important intellectual content
- Lin Chang: study concept and design, analysis and interpretation of data, acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, funding, administrative and material support, study supervision
Disclosures: The authors have no relevant disclosures.
References
- 1.Lynn RB, Friedman LS. Irritable bowel syndrome. N Engl J Med. 1993;39:1940–1945. doi: 10.1056/NEJM199312233292608. [DOI] [PubMed] [Google Scholar]
- 2.Sherwin LB, Leary E, Henderson WA. The association of catastrophizing with quality-of-life outcomes in patients with irritable bowel syndrome. Qual Life Res. 2017;26(8):2161–2170. doi: 10.1007/s11136-017-1554-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grodzinsky E, Waster S, Victorsson L, et al. More negative self-esteem and inferior coping strategies among patients diagnosed with IBS compared with patients without IBS—a case-control study in primary care. BMC Fam Pract. 2015;16:6. doi: 10.1186/s12875-015-0225-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Tilburg MA, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J Psychosom Res. 2013;74:486–492. doi: 10.1016/j.jpsychores.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naliboff B, Lackner JM, Mayer E. Psychosocial factors in the care of patients with functional gastrointestinal disorders. In: Yamada T, editor. Principles of Clinical Gastroenterology. John Wiley & Sons; Hoboken, NJ: 2008. pp. P20–7. [Google Scholar]
- 6.Dapoigny M, Bellanger J, Bonaz B, et al. Irritable bowel syndrome in France: a common, debilitating and costly disorder. Eur J Gastro Hepatol. 2004;16:995–1001. doi: 10.1097/00042737-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Gralnek IM, Hays RD, Kilbourne A, et al. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119:654–60. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 8.Creed F. Health-related quality of life and health care costs in severe, refractory irritable bowel syndrome. Ann Intern Med. 2001;134(9 pt 2):860–8. doi: 10.7326/0003-4819-134-9_part_2-200105011-00010. [DOI] [PubMed] [Google Scholar]
- 9.Ballou S, Keefer L. The impact of irritable bowel syndrome on daily functioning: Characterizing and understanding daily consequences of IBS. Neurogastroenterol Motil. 2016:1–7. doi: 10.1111/nmo.12982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lackner JM, Gudleski GD, MA CX, et al. Fear of GI symptoms has an important impact on quality of life in patients with moderate-to-severe IBS. Am J of Gastro. 2014;109(11):1815–23. doi: 10.1038/ajg.2014.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lackner JM, Gudleski GD, Thakur ER, et al. The impact of physical complaints, social environment, and psychological functioning on IBS patients’ health perceptions: looking beyond GI symptom severity. Am J Gastroenterol. 2014;109(2):224–33. doi: 10.1038/ajg.2013.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jerndal P, Ringström G, Agerforz P, et al. Gastrointestinal-specific anxiety: an important factor for severity of GI symptoms and quality of life in IBS. Neurogastroenterol Motil. 2010;22(6):646–e179. doi: 10.1111/j.1365-2982.2010.01493.x. [DOI] [PubMed] [Google Scholar]
- 13.Michalsen VL, Vandvik PO, Farup PG. Predictors of health-related quality of life in patients with irritable bowel syndrome. A cross-sectional study in Norway Health and Quality of Life Outcomes. 2015;13:113. doi: 10.1186/s12955-015-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spiegel BM, Gralnek IM, Bolus R, et al. Clinical Determinants of health-related quality of life in patients with irritable bowel syndrome. Arch Intern Med. 2004;164(16):1773–1780. doi: 10.1001/archinte.164.16.1773. [DOI] [PubMed] [Google Scholar]
- 15.Whitehead WE, Burnett CK, Cook EW, III, et al. Impact of irritable bowel syndrome on quality of life. Dig Dis Sci. 1996;41:2248–2253. doi: 10.1007/BF02071408. [DOI] [PubMed] [Google Scholar]
- 16.Halder SL, Locke GR, III, Talley NJ, et al. Impact of functional gastrointestinal disorders on health-related quality of life: a population-based case-control study. Aliment Pharmacol Ther. 2004;19:233–242. doi: 10.1111/j.0269-2813.2004.01807.x. [DOI] [PubMed] [Google Scholar]
- 17.Rey E, Garcia-Alonso MO, Moreno-Ortega, et al. Determinants of quality of life in irritable bowel syndrome. J of Clin Gastro. 2008;42(9):1003–1009. doi: 10.1097/MCG.0b013e31815af9f1. [DOI] [PubMed] [Google Scholar]
- 18.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–91. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 19.Labus JS, Bolus R, Chang L, et al. The visceral sensitivity index: development and validation of a gastrointestinal symptom-specific anxiety scale. Aliment Pharmacol Ther. 2004;20:89–7. doi: 10.1111/j.1365-2036.2004.02007.x. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Vu J, Kushnir V, Casell B, et al. The impact of psychiatric and extraintestinal comorbidity on quality of life and bowel symptom burden in functional GI disorders. Neurogastroenterol Motil. 2014;26:1323–32. doi: 10.1111/nmo.12396. [DOI] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 24.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 25.Carlson LE, Brown KW. Validation of the mindful attention awareness scale in a cancer population. J Psychosom Res. 2005;58:29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- 26.McHorney CA, Ware JE, Jr, Lu JF, et al. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Koloski NA, Boyce PM, Jones MP, et al. What level of IBS symptoms drives impairment in health-related quality of life in community subjects with irritable bowel syndrome? Are current IBS symptom thresholds clinically meaningful? Qual Life Res. 2012 Jun;21(5):829–36. doi: 10.1007/s11136-011-9985-5. [DOI] [PubMed] [Google Scholar]
- 28.Labus JS, Mayer EA, Chang L, et al. The central role of gastrointestinal-specific anxiety in irritable bowel syndrome: further validation of the visceral sensitivity index. Psychosom Med. 2007;69(1):89–98. doi: 10.1097/PSY.0b013e31802e2f24. [DOI] [PubMed] [Google Scholar]
- 29.Drossman DA, Chang L, Schneck S, et al. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig Dis Sci. 2009;54(7):1532–41. doi: 10.1007/s10620-009-0792-6. [DOI] [PubMed] [Google Scholar]
- 30.Ljótsson B, Andersson E, Lindfors P, et al. Prediction of symptomatic improvement after exposure-based treatment for irritable bowel syndrome. BMC Gastroenterol. 2013;13:160. doi: 10.1186/1471-230X-13-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ljótsson B, Hedman E, Andersson E, et al. Internet-delivered exposure-based treatment vs. stress management for irritable bowel syndrome: a randomized trial. Am J Gastroenterol. 2011;106:1481–1491. doi: 10.1038/ajg.2011.139. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153(32):2474–80. [PubMed] [Google Scholar]
- 33.Ceunen E, Zaman J, Weltens N, et al. Learned fear of gastrointestinal sensations in healthy adults. Clin Gastroenterol Hepatol. 2016;14(11):1553–1558. doi: 10.1016/j.cgh.2016.04.035. [DOI] [PubMed] [Google Scholar]
- 34.Zaman J, Vlaeyen JW, Van Oudenhove L, et al. Influence of interoceptive fear learning on visceral perception. Psychosom Med. 2016;78:248–258. doi: 10.1097/PSY.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 35.Sibille KT, Langaee T, Burkley B, et al. Chronic pain, perceived stress, and cellular aging: an exploratory study. Mol Pain. 2012;8:12. doi: 10.1186/1744-8069-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schliep KC, Mumford SL, Vladutiu CJ, et al. Perceived stress, reproductive hormones and ovulatory function: a prospective cohort study. Epidemiology. 2015;26(2):177–84. doi: 10.1097/EDE.0000000000000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rehm KE, Elci Ou, Hahn K, et al. The impact of self-reported psychological stress levels on changes to peripheral blood immune biomarkers in recreational marathon runners during training and recovery. Neuroimmunomodulation. 2013;20(3):164–76. doi: 10.1159/000346795. [DOI] [PubMed] [Google Scholar]
- 38.Glei DA, Goldman N, Shkolnikov VM, et al. Perceived stress and biological risk: is the link stronger in Russians than in Taiwanese and Americans? Stress. 2013;16(4):411–20. doi: 10.3109/10253890.2013.789015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Althaus A, Broicher W, Wittkamp P, et al. Determinants and frequency of Irritable bowel syndrome in a German sample. Z Gastroenterol. 2016;54(3):217–25. doi: 10.1055/s-0041-106856. [DOI] [PubMed] [Google Scholar]
- 40.Edman JS, Greeson JM, Roberts RS, et al. Perceived stress in patients with common gastrointestinal disorders: associations with quality of life, symptoms and disease management. Explore (NY) 2017;13(2):124–128. doi: 10.1016/j.explore.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pellissier S, Bonaz B. The place of stress and emotions in the irritable bowel syndrome. Vitam Horm. 2017;103:327–354. doi: 10.1016/bs.vh.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 42.Whitehead WE, Crowell MD, Robinson JC, et al. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut. 1992;33(6):825–30. doi: 10.1136/gut.33.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chang L. The role of stress on physiological responses and clinical symptoms in irritable bowel syndrome. Gastroenterology. 2011;140(3):761–765. doi: 10.1053/j.gastro.2011.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bluth K, Eisenlohr-Moul TA. Response to a mindful self-compassion intervention in teens: A within-person association of mindfulness, self-compassion, and emotional well-being outcomes. J Adolesc. 2017;57:108–118. doi: 10.1016/j.adolescence.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reibel DK, Greseson JM, Brainard GC, et al. Mindfulness-based stress reduction and health-related quality of life in a heterogenous patient population. Gen Hosp Psychiatry. 2001;23(4):183–92. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- 46.Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10:144–156. [Google Scholar]
- 47.Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta. 1990 Print. [Google Scholar]
- 48.Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. 2011;31:1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Galla BM, O’Reilly GA, Kitil MJ, et al. Community-based mindfulness program for disease prevention and health promotion: Targeting stress reduction. Am J Health Promot. 2015;30(1):36–41. doi: 10.4278/ajhp.131107-QUAN-567. [DOI] [PubMed] [Google Scholar]
- 50.Baer R. Mindfulness Training as a clinical intervention: A conceptual and empirical review. Clin Psychology Science and Practice. 2003;10(n2):125–143. [Google Scholar]
- 51.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1983;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 52.Shaheen L, Schofield K. Mindfulness-based therapies in the treatment of somatization disorders: A systemic Review and Meta-Analysis. PLoS One. 2013;8(8):e71834. doi: 10.1371/journal.pone.0071834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zernicke KA, Campbell TS, Blustein PK, et al. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: a randomized wait-list controlled trial. Int J Behav Med. 2013;20(3):385–96. doi: 10.1007/s12529-012-9241-6. [DOI] [PubMed] [Google Scholar]
- 54.Zomorrodi S, Rasoulzadeh TSK, Azadfallah P, et al. Long Term Effects of Mindfulness on Quality of life in Irritable Bowel Syndrome. Iran J Psychiatry. 2015;10(2):100–5. [PMC free article] [PubMed] [Google Scholar]
- 55.Aucoin M, Lalonde-Parsi MJ, Cooley K. Mindfulness-based therapies in the treatment of functional gastrointestinal disorders: a meta-analysis. Evid Based Complement Alternat Med. 2014 doi: 10.1155/2014/140724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berrill JW, Sadlier M, Hood K, et al. Mindfulness-based therapy for inflammatory bowel disease patients with functional abdominal symptoms or high perceived stress levels. J Crohns Colitis. 2014;8(9):945–55. doi: 10.1016/j.crohns.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 57.Gaylord SA, Palsson OS, Garland EL, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am J Gastroenterol. 2011;106(9):1678–88. doi: 10.1038/ajg.2011.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kearney DJ, McDermott K, Martinez M, et al. Association of participation in a mindfulness programme with bowel symptoms, gastrointestinal symptom-specific anxiety and quality of life. Aliment Pharmacol Ther. 2011;34(3):363–73. doi: 10.1111/j.1365-2036.2011.04731.x. [DOI] [PubMed] [Google Scholar]
- 59.Spiller RC, Humes DJ, Campbell E, et al. The Patient Health Questionnaire 12 Somatic Symptom scale as a predictor of symptom severity and consulting behavior in patients with irritable bowel syndrome and symptomatic diverticular disease. Aliment Pharmacol Ther. 2010;32(6):811–20. doi: 10.1111/j.1365-2036.2010.04402.x. [DOI] [PubMed] [Google Scholar]
- 60.Shih YC, Barghout VE, Sandler RS, et al. Resource utilization associated with irritable bowel syndrome in the United States 1987-1997. Dig Dis Sci. 2002;47:1705–1715. doi: 10.1023/a:1016471923384. [DOI] [PubMed] [Google Scholar]
- 61.Hungin AP, Molloy-Bland M, Claes R, et al. Systematic review: the perceptions, diagnosis and management of irritable bowel syndrome in primary care – A Rome Foundation Working Team Report. Ailment Pharmacol Ther. 2014;40:1133–1145. doi: 10.1111/apt.12957. [DOI] [PubMed] [Google Scholar]


