Abstract
Identifying oneself as being overweight may be associated with adverse health outcomes, yet prospective tests of this possibility are lacking. Over 7 years, we examined associations between perceptions of being overweight and subsequent health in a sample of 3,582 U.S. adults. Perceiving oneself as being overweight predicted longitudinal declines in subjective health (d = −0.22, p < .001), increases in depressive symptoms (d = 0.09, p < .05), and raised levels of physiological dysregulation (d = 0.24, p < .001), as gauged by clinical indicators of cardiovascular, inflammatory, and metabolic functioning. These associations remained after controlling for a range of potential confounders and were observed irrespective of whether perceptions of being overweight were accurate or inaccurate. This research highlights the possibility that identifying oneself as overweight may act independently of body mass index to contribute to unhealthy profiles of physiological functioning and impaired health over time. These findings underscore the importance of evaluating whether weight-feedback interventions may have unforeseen adverse consequences.
Keywords: obesity, body image, weight stigma, health, well-being, open data, open materials
People who are objectively overweight (i.e., those with a body mass index, or BMI ≥ 25 kg/m2) often do not identify themselves as such; instead, they view their bodies as being of normal weight (Johnson, Beeken, Croker, & Wardle, 2014; Robinson & Oldham, 2016). Traditionally, this has been considered a cause for concern because identifying oneself as being overweight has been presumed to be a necessary prerequisite to healthy behavior change: If individuals identify themselves as being overweight, rather than normal weight, they should be more motivated to seek treatment, initiate lifestyle changes, or attempt weight loss (Duncan et al., 2011; Johnson et al., 2014). In keeping with this rationale, large-scale personalized weight feedback programs have been designed to increase people’s awareness of their own overweight status and prompt weight loss (Ikeda, Crawford, & Woodward-Lopez, 2006).
However, adiposity is stigmatized and derogated in modern society; overweight individuals face negative stereotypes from the general public and health-care professionals, negative portrayals in the media, and prejudice across a range of life domains (Heuer, McClure, & Puhl, 2011; Teachman & Brownell, 2001). Because the stigmatization of adiposity is widely recognized, individuals who identify as being overweight may fear negative evaluation from other people; this sort of judgment is likely to be stressful and damaging to psychological well-being (Blodorn, Major, Hunger, & Miller, 2016; Hunger, Major, Blodorn, & Miller, 2015). Longitudinal studies have shown that people who experience weight discrimination show diminished self-worth, impaired well-being, and increased weight gain over time (Robinson, Sutin, & Daly, 2017; Sutin & Terracciano, 2013). This evidence suggests that identifying oneself as being overweight may be detrimental rather than beneficial to health.
Indeed, self-identification as overweight, rather than normal weight, has been shown to prospectively predict greater weight gain over time in adults in the United States and the United Kingdom, a finding that was explained in part by the stress associated with perceiving oneself as overweight (Robinson, Hunger, & Daly, 2015). This weight gain could not be attributed to differences in initial BMI, and perceiving oneself as overweight had consequences for weight gain that were observed irrespective of whether this perception was accurate or inaccurate. Furthermore, recent evidence from a quasiexperimental evaluation of a large-scale weight-feedback program suggests that informing girls that they are overweight may produce unintended weight gain (Almond, Lee, & Schwartz, 2016).
The weight gain associated with personally identifying oneself as being overweight is likely to have implications for psychological health and physiological functioning. Obesity is a well-established risk factor for depression (Faith et al., 2011), and weight changes are known to produce corresponding changes in blood pressure, inflammation, glucose tolerance, and lipids, such as cholesterol and triglycerides (e.g., Dattilo & Kris-Etherton, 1992; Neter, Stam, Kok, Grobbee, & Geleijnse, 2003). Further, we anticipate that the psychosocial experience attached to identifying as an overweight person may have mental and physical health consequences that occur independently of weight gain.
For example, a series of cross-sectional studies has shown that people who identify themselves as being overweight are more likely to suffer from depression and impaired well-being and to have an increased risk of suicidal behavior irrespective of their current weight (Atlantis & Baker, 2008; Hayward, Millar, Petersen, Swinburn, & Lewis, 2014; Swahn et al., 2009). Weight-based discrimination has been conceptualized as a social-evaluative threat with likely downstream physiological and psychological effects (Tomiyama, 2014). Prior research on racial and health inequalities, for example, has documented the physiological impact of social denigration; such stress can activate the sympathetic nervous system and induce sustained neuroendocrine responses with potentially deleterious health consequences (Daly, Boyce, & Wood, 2015; Williams & Mohammed, 2009). Likewise, weight discrimination could activate the fight-or-flight response, which is adaptive in times of acute physical threat but is maladaptive if chronically activated in response to social threat. This could lead to cortisol secretion and stress-induced eating, thus detrimentally affecting metabolic and cardiovascular-system functioning (Epel, Lapidus, McEwen, & Brownell, 2001; Tomiyama, 2014).
Recent well-designed experimental studies support this notion. They show that experimental manipulations that aim to induce experiences of weight stigma lead to behavioral and physiological changes, including increased unhealthy eating (Incollingo Rodriguez, Heldreth, & Tomiyama, 2016) and cortisol secretion (Himmelstein, Incollingo Belsky, & Tomiyama, 2015), both of which in the long term could promote physiological dysregulation. Further, the stress-induced physiological consequences of weight stigma may be most pronounced among people who perceive themselves as heavy (Himmelstein et al., 2015). Taken together, this emerging evidence suggests that the psychosocial experience attached to identifying oneself as overweight may be stressful, leading to weight gain and potentially to broader, more far-reaching health consequences, such as physiological dysfunction (Sutin, Stephan, Carretta, & Terracciano, 2015).
The current study examines whether perceiving oneself as overweight predicts subsequent impairments to health status 7 years later. We hypothesized that self-identification as overweight in early adulthood would be associated with increased physiological dysregulation, decreased subjective health, and increased depression levels, after controlling for baseline BMI and a range of sociodemographic characteristics. We further hypothesized that weight gain may act as a key pathway between perceiving oneself as overweight and subsequent health impairments.
Method
Participants
In this study, we used data from Wave 3 (2001–2002) and Wave 4 (2008–2009) of the National Longitudinal Study of Adolescent Health (Add Health; Harris et al., 2009). We used the public-domain Add Health data set, which is composed of a randomly selected sample of half of the core study sample and half of the African American oversample. The Add Health sample was drawn from a nationally representative sample of 144 schools selected using stratified random sampling. Add Health obtained informed consent at each study wave in accordance with guidelines set out by the institutional review board at the University of North Carolina School of Public Health. The current study includes participants who completed the Wave 3 (baseline) and Wave 4 (follow-up) in-home interviews and provided data on all key variables: perceived weight, BMI, self-rated health, depressive symptoms, and physiological dysregulation.
Of the 4,882 participants who completed the baseline assessment, 3,582 (2,017 women and 1,565 men) provided sufficient follow-up data to be included in the current analyses (see Table 1 for characteristics of the sample). Participants included in the analyses were more likely to be female (p < .001), to be White (p < .001), and to have a limiting chronic condition (p < .01) than were those who were excluded; they also tended to have a higher BMI ( p < .01). Weighting the analyses to account for selective attrition did not produce different results; therefore, we report unweighted regression results here. Participants included in the analysis were, on average, 21.80 years old (SD = 1.81) at baseline and 28.80 years old (SD = 1.78) at follow-up.
Table 1.
Participants’ Characteristics
| Characteristic | Statistic |
|---|---|
| Perception of self as overweight (%) | 41.82 |
| Age (years) | |
| Baseline | M = 21.80, SD = 1.81 |
| Follow-up | M = 28.80, SD = 1.78 |
| Sex (% female) | 56.31 |
| White (%) | 72.30 |
| Educationa | M = 13.23, SD = 1.98 |
| Income (U.S. dollars) | M = 12,949.39, SD = 11,817.93 |
| Limiting condition (%)b | 18.29 |
| Body mass index (kg/m2) | |
| Baseline | M = 26.62, SD = 6.24 |
| Follow-up | M = 29.17, SD = 7.33 |
| Self-rated healthc | |
| Baseline | M = 4.00, SD = 0.87 |
| Follow-up | M = 3.64, SD = 0.92 |
| Depressive symptomsd | |
| Baseline | M = 4.51, SD = 4.07 |
| Follow-up | M = 5.17, SD = 4.09 |
Education was scored on a scale from 6 (6th grade) to 22 (5 or more years of graduate school) and indicates the highest level of education achieved at the Wave 3 (baseline) assessment. bPhysical conditions that limited activity and lasted for more than 1 year were considered to be limiting conditions. cSelf-rated health was scored on a scale from 1 (poor) to 5 (excellent). dDepressive symptoms were assessed using nine items from the Center for Epidemiological Studies Depression Scale (Radloff, 1977); the possible score ranged from 0 to 27.
Measures
Perceived weight
Self-perceived weight was assessed at baseline using the item “How do you think of yourself in terms of weight?” Participants rated their perceived weight on a scale from 1 (very underweight) to 5 (very overweight), with a midpoint of 3 (about the right weight). Participants were classified as perceiving themselves as being overweight if they scored 4 (slightly overweight) or 5 (very overweight). This group was contrasted with the remainder of the sample, who scored 1 (very underweight), 2 (slightly underweight), or 3 (about the right weight) on this measure.
Body mass index
Height and weight measurements were taken by trained interviewers at baseline and follow-up assessments according to a standardized protocol (see Entzel et al., 2009). A steel tape measure was used to measure standing height to the nearest 0.5 cm; participants stood against a smooth wall without shoes or hats. Weight was measured to the nearest 0.1 kg using a high-capacity digital bathroom scale. These readings were used to calculate BMI. A quality-control study in which participants were tested and then retested 1 to 2 weeks later showed that the assessment methods used produced highly reliable height, weight, and BMI measures (intraclass correlation coefficients from .98 to 1.00; Hussey et al., 2015).
Physiological dysregulation
As part of the Add Health Wave 4 follow-up, participants were examined by qualified staff who collected measures of cardiovascular, inflammatory, and metabolic health. Interviewers followed standardized step-by-step procedures to measure participants’ resting, seated blood pressure from the right arm using an electronic oscillometric blood pressure monitor (Entzel et al., 2009). Three assessments were taken at 30-s intervals; the last two readings were recorded and averaged as the measure of resting systolic and diastolic blood pressure. A measure of waist circumference was taken at the superior border of the iliac crest using a tape measure (Entzel et al., 2009). Interviewers also used a finger-prick test to collect whole-blood spots, which were dried and sent to the lab for analysis.
Drawing on these measures, we followed prior studies (e.g., Hampson, Edmonds, Goldberg, Dubanoski, & Hillier, 2013) to produce a composite indicator of physiological dysregulation composed of biomarkers of cardiovascular, inflammatory, and metabolic system func-tioning considered to capture cumulative biological risk (Seeman, McEwen, Rowe, & Singer, 2001). Specifically, systolic and diastolic blood pressure provided an index of cardiovascular functioning. Inflammation levels were assessed using a high-sensitivity C-reactive protein test. Waist circumference provided an index of body fat. Metabolic risk factors were assessed using the ratio of total blood cholesterol to levels of high-density lipoprotein cholesterol, total triglycerides, glucose, and glycated hemoglobin (hemoglobin A1c). Each measure was converted to deciles and summed to produce a normally distributed overall physiological dysregulation score. This composite measure was then standardized to have a mean of 0 and standard deviation of 1.
Self-rated health
General self-rated health was assessed at baseline and follow-up using the item “In general, how is your health?” Participants’ health status was scored on a scale from 1 (poor) to 5 (excellent), with a midpoint of 3 (good). This single-item measure summarizes global health information and has been shown to be a stronger predictor of all-cause mortality than individual health markers derived from blood assays, physical measurements, or medical histories (Ganna & Ingelsson, 2015). Predictions regarding hospitalizations, health-care use, and mortality based on this measure have been shown to be comparable with those identified using multi-item self-reported health measures (DeSalvo, Fan, McDonell, & Fihn, 2005).
Depressive symptoms
Depressive symptoms experienced over the previous week were assessed at baseline and follow-up using nine items from the Center for Epidemiological Studies Depression Scale (Radloff, 1977). The items assessed a range of depressive symptoms including depressed affect (feeling blue, sad, depressed), positive affect (feeling as good as other people, enjoying life), somatic symptoms (bothered by things, tired, trouble concentrating), and interpersonal symptoms (feeling disliked by other people). The frequency of depressive symptoms in the week preceding the screening was rated on a scale from 0 (never/rarely) to 3 (most of the time/all of the time), and the nine items were summed so that higher scores indicated greater depressive symptoms (range = 0–27; Cronbach’s α = .81 in both waves).
Analytical strategy
We first predicted self-rated health and depressive symptoms at follow-up (T) controlling for these variables at baseline (T – 1) to capture residualized changes in health and avoid issues associated with regression toward the mean (e.g., Linn & Slinde, 1977). The main explanatory variable was whether the participant perceived him- or herself as overweight at baseline. We controlled for potential confounds, including baseline BMI, and age, sex, race, education, income, and the presence of a limiting health condition. We then tested the relation between perceiving oneself as overweight at baseline and physiological dysregulation assessed 7 years later:
Next, we conducted two robustness tests. First, we tested whether each predicted association was also observed if we used a continuous measure of perceived weight—from 1 (very underweight) to 5 (very overweight)—rather than our main dichotomous indicator of whether participants perceived themselves as overweight. We then tested whether the anticipated links between participants’ perception of being overweight and the health outcomes examined were moderated by overweight status or gender. We predicted that participants who perceived themselves as being overweight would have poorer subsequent health than those who did not, irrespective of whether these perceptions were accurate or whether participants were male or female.
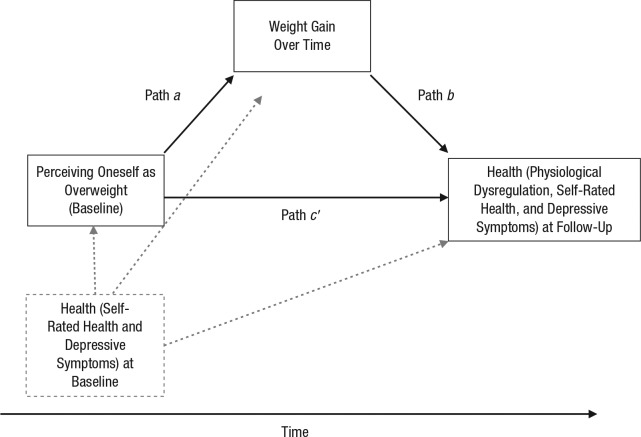
Finally, we tested whether weight gain attributable to the perception of being overweight (path a in Fig. 1) predicted subsequent health (path b) and mediated the associations between the perception of being overweight and subsequent physiological dysregulation, self-rated health, and depressive symptoms (whether the a × b effect was statistically different from zero as indicated by a 95% confidence interval for the indirect effect not containing zero). Because baseline health could influence weight perceptions, weight gain, and subsequent health (see the dashed lines in Fig. 1), we adjusted our models for initial self-rated health and depressive symptoms when examining these outcomes. To test this mediation hypothesis, we used the SPSS PROCESS macro (Hayes, 2013) and created 10,000 bootstrap samples to estimate bias-corrected and accelerated 95% confidence intervals (BCa 95% CIs) and to establish the significance levels of the indirect effects.
Fig. 1.
Conceptual model of the hypothesized effect of perceiving oneself as overweight at baseline on health at follow-up, as mediated by weight gain over time. The effect of health at baseline is indicated by the dashed lines.
Because data on physiological dysregulation were available only at follow-up in Add Health, we could not rule out the possibility that unobserved baseline dysregulation acted as a “third variable” (note its absence from the baseline health variable in in Fig. 1) that influenced both baseline weight perceptions and subsequent physiological dysregulation, accounting for the link between these variables. However, using additional data sets (for details, see Section 2 of the Supplemental Material available online), it was possible to estimate the impact of including or excluding a control for baseline physiological dysregulation on the portion of the link between the perception of being overweight and follow-up dysregulation that was due to weight gain over time (i.e., the indirect effect, a × b). We first tested whether controlling for baseline dysregulation influenced the strength of path a (from perception of being overweight to weight gain) over an 11-year period. Next, we tested whether including a control for baseline physiological dysregulation affected the association between weight gain (over 4 years) and dysregulation at follow-up (path b).
Results
Of the 3,582 participants, 41.82% perceived themselves as being overweight at baseline, whereas the remaining 58.18% did not, as shown in Table 1. The correlation between perception of being overweight (dichotomous) and actually being overweight (BMI ≥ 25 kg/m2) was .57 (p < .001), which confirms the substantial discrepancy between being objectively overweight and perceiving oneself as being overweight (Duncan et al., 2011; Johnson et al., 2014). Self-rated health decreased over the course of the study (baseline: M = 4.00, SD = 0.87; follow-up: M = 3.64, SD = 0.92), t(3581) = −21.46, p < .001, and depressive symptoms increased (baseline: M = 4.51, SD = 4.07; follow-up: M = 5.17, SD = 4.09), t(3581) = 9.24, p < .001. Participants’ BMI also increased, by 2.55 kg/m2, over the 7-year period between the baseline and follow-up assessments, t(3581) = 36.30, p < .001.
Health outcomes at the 7-year follow-up
The results of the regression analyses are summarized in Table 2. Between baseline and follow-up, participants who perceived themselves to be overweight showed a decline of 0.22 SD in self-rated health, p < .001. Perceiving oneself as overweight also predicted a small increase in depressive symptoms over the study period, d = 0.09, p < .05. In addition to these changes in self-rated health and depressive symptoms, perceiving oneself as overweight predicted physiological dysregulation 7 years later. Participants who perceived themselves as being overweight had dysregulation scores 0.24 SD higher than the scores of participants who did not perceive themselves as being overweight, p < .001. These associations were independent of baseline BMI and the potential confounding sociodemographic factors measured (i.e., age, gender, ethnicity, education, income, and the presence of a limiting condition). Further, we observed a very similar pattern of results when a continuous measure of perceived weight was used (see Section 1 in the Supplemental Material).
Table 2.
Results of the Regression Analysis: Perception of Oneself as Overweight as a Predictor of Subsequent Physiological Dysregulation, Self-Rated Health, and Depressive Symptoms
| Predictor | Physiological
dysregulation |
Self-rated health |
Depressive symptoms |
|||
|---|---|---|---|---|---|---|
| Weight gain not included | Weight gain included | Weight gain not included | Weight gain included | Weight gain not included | Weight gain included | |
| Perception of self as overweight | 0.24*** (0.04) | 0.13*** (0.03) | −0.22*** (0.04) | −0.18*** (0.04) | 0.09* (0.04) | 0.09* (0.04) |
| Age | 0.03*** (0.01) | 0.04*** (0.01) | −0.02* (0.01) | −0.02** (0.01) | 0.03*** (0.01) | 0.03** (0.01) |
| Sex (female) | −0.52*** (0.03) | −0.49*** (0.03) | −0.06 (0.03) | −0.07* (0.03) | 0.16*** (0.03) | 0.16*** (0.03) |
| White | 0.01 (0.03) | 0.06* (0.03) | 0.18*** (0.03) | 0.16*** (0.03) | −0.12*** (0.04) | −0.12*** (0.04) |
| Education | −0.04*** (0.01) | −0.03*** (0.01) | 0.07*** (0.01) | 0.07*** (0.01) | −0.07*** (0.01) | −0.07*** (0.01) |
| Income | −0.00 (0.00) | 0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| Limiting condition | 0.07* (0.04) | 0.09** (0.03) | −0.05 (0.04) | −0.06 (0.04) | 0.07 (0.04) | 0.06 (0.04) |
| Body mass index at baseline | 0.07*** (0.00) | 0.07*** (0.00) | −0.01*** (0.00) | −0.02*** (0.00) | −0.00 (0.00) | −0.00 (0.00) |
| Weight gaina | — | 0.10*** (0.00) | — | −0.04*** (0.00) | — | −0.00 (0.00) |
| Self-rated health | — | — | 0.39*** (0.02) | 0.38*** (0.02) | — | — |
| Depressive symptoms | — | — | — | — | 0.10*** (0.00) | 0.10*** (0.00) |
Note: The table presents z scores, with standard errors in parentheses.
Weight gain was calculated by subtracting body mass index (BMI) at baseline from BMI at follow-up.
p < .05. **p < .01. ***p < .001.
We also investigated whether the link between perceiving oneself as overweight and the health outcomes examined was dependent on whether participants accurately perceived themselves as overweight (BMI ≥ 25.0 at baseline) or overestimated their weight status (BMI < 25 at baseline). When included in the fully adjusted model, the interaction term between perceiving oneself as overweight and the accuracy of that perception (i.e., whether the participant was objectively overweight or not overweight at baseline) was nonsignificant for changes in self-rated health, b = 0.02, SE = 0.08, t(3570) = 0.24, p = .81, and depressive symptoms, b = 0.24, SE = 0.32, t(3570) = 0.74, p = .46. Further, the inclusion of the interaction term did not produce any increase in model fit, which confirms that the effect that perceiving oneself as overweight had on self-rated health and depression was not dependent on the accuracy of weight perceptions.
There was a significant negative interaction between perceiving oneself as overweight and the accuracy of that perception in predicting physiological dysregulation, b = −0.17, SE = 0.07, t(3571) = −2.29, p < .05: Perceiving oneself as overweight was more strongly associated with dysregulation when this perception was inaccurate (BMI < 25 at baseline). However, perceiving oneself as being overweight was predictive of future physiological dysregulation among both participants who were overweight at baseline, b = 0.15, SE = 0.05, t(1801) = 3.00, p < .005, and participants with BMI levels less than 25 who overestimated their weight at baseline, b = 0.26, SE = 0.06, t(1761) = 4.36, p < .001. Taken together, these findings suggest that perceiving oneself as being overweight is an important predictor of subsequent health, irrespective of the accuracy of weight perceptions.
Finally, we tested whether the association between perceiving oneself as being overweight and health was moderated by sex. Across the three outcomes (i.e., self-rated health, self-rated depressive symptoms, and physiological dysregulation), there was no evidence that gender interacted with baseline perceptions of oneself as overweight as opposed to not overweight (all ps > .05), which indicates that perceiving oneself as being overweight has a similar effect on health in both male and female adults.
Mediation through weight gain
There was substantial evidence that weight gain may explain why perceiving oneself as being overweight is predictive of subsequent health ratings and physiological dysregulation. Perceiving oneself as being overweight predicted increased weight gain between baseline and follow-up, b = 1.08, SE = 0.19, t(3573) = 5.79, p < .001, as shown previously (Robinson et al., 2015). Weight gain was unrelated to changes in depressive symptoms, and formal mediation analysis confirmed that there was no evidence that perceiving oneself as being overweight had an indirect effect on depressive symptoms through weight gain, b = 0.00, BCa 95% CI = [−0.01, 0.01]. However, weight gain was associated with a decline in self-rated health, b = −0.04, SE = 0.00, t(3571) = −11.75, p < .001, and with higher levels of physiological dysregulation at follow-up, b = 0.10, SE = 0.00, t(3572) = 33.59, p < .001, in a model adjusted for baseline BMI and covariates.
Including weight gain in our main regression model diminished the strength of the associations between perceiving oneself as being overweight and self-rated health—model without weight gain: b = −0.22, SE = 0.04, p < .001; model with weight gain: b = −0.18, SE = 0.04, p < .001—and between perceiving oneself as being overweight and physiological dysregulation—model without weight gain: b = 0.24, SE = 0.04, p < .001; model with weight gain: b = 0.13, SE = 0.03, p < .001—as shown in Table 2. Formal mediation analyses confirmed that weight gain mediated the association between perceived overweight and declines in self-rated health, b = −0.04, BCa 95% CI = [−0.06, −0.03], and increased physiological dysregulation, b = 0.11, BCa 95% CI = [0.07, 0.14]. Finally, our additional analyses of two separate data sets indicated that the latter mediation channel may not be markedly affected by the absence of a control for baseline physiological dysregulation (which was not available in Add Health).
Specifically, this additional data showed that adjusting for initial dysregulation did not diminish the association between perceiving oneself as being overweight and subsequent weight gain—path a without adjustment: b = 0.67, SE = 0.12, p < .001; path a with adjustment: b = 0.66, SE = 0.12, p < .001—or the association between weight gain and dysregulation at follow-up—path b without adjustment: b = 0.10, SE = 0.01, p < .001; path b with adjustment: b = 0.11, SE = 0.01, p < .001 (see Section 2 in the Supplemental Material).
In the context of the current study, these analyses provide indirect evidence that the portion of the link between perceiving oneself as being overweight and follow-up dysregulation that is due to weight gain (i.e., the mediation channel a × b) is unlikely to be attributable to unobserved variation in baseline physiological dysregulation.
In summary, the mediation analyses demonstrated the association between perceiving oneself as being overweight and physiological dysregulation was partially indirect; 46% of this relation was mediated by weight gain. A similar pattern emerged for self-rated health: A smaller portion (18%) of the role of perceiving oneself as being overweight was explained by weight gain. Weight gain did not explain why perceiving oneself as being overweight was linked to increased depressive symptoms.
Discussion
There is now evidence linking perceptions of weight to weight gain throughout life. Children viewed as overweight by their parents tend to gain more weight across childhood irrespective of their initial BMI (Robinson & Sutin, 2016). In the teenage years, normal-weight adolescents who perceive themselves as overweight appear to be at increased risk of unhealthy eating, weight gain, and obesity (Cuypers et al., 2012; Martin et al., 2014; Sutin & Terracciano, 2015). Further, BMI report cards labeling girls as “outside a healthy weight” have been shown to inadvertently promote a small level of weight gain (Almond et al., 2016). In adulthood, perceiving oneself as being overweight has been found to be associated with promoting stress-related eating and weight gain (Robinson et al., 2015). Together, these findings suggest that psychologically identifying oneself as a member of the socially stigmatized “overweight” group is likely to be associated with weight gain and eating patterns conducive to obesity.
In the current study, we aimed to test whether there might be other consequential downstream health and well-being effects of weight perceptions. We capitalized on the natural differentiation between medically defined adiposity and perceiving oneself as being overweight to show that such a perception predicted poor health in a large sample of U.S. adults. Specifically, perceiving oneself as being overweight was prospectively associated with physiological dysregulation, declines in subjective health, and increases in depressive symptoms over a 7-year follow-up period. These associations were independent of initial BMI levels and sociodemographic characteristics, were not significantly different for men and women, and were meaningful in magnitude. For example, the longitudinal link between perceiving oneself as being overweight and decreased subjective health (d = −0.22) was equivalent in magnitude to an additional 3 years of education, a key predictor of self-rated health (e.g., Kunst et al., 2005) and the link to physiological dysregulation corresponded to an increase in baseline BMI of more than 3 kg/m2 (d = 0.24). These findings are compatible with the idea that perceiving oneself as being overweight is likely to be stressful and as a result may have adverse health effects (Sutin & Terracciano, 2015).
Indeed, there is rapidly growing evidence that weight-based social stigmatization is linked to daily stress, negative feelings, unhealthy eating, weight gain, and declines in physical and mental health (Robinson et al., 2017; Sutin, Robinson, Daly, & Terracciano, 2016; Sutin et al., 2015; Sutin, Stephan, et al., 2016). These findings suggests that weight stigma may trigger a cycle of stress, maladaptive coping responses, further weight gain, and poor health (Blodorn et al., 2016; Brewis, 2014; Hunger et al., 2015; Sikorski, Luppa, Luck, & Riedel-Heller, 2015; Tomiyama, 2014). However, it has not been clear whether, given the current social climate, simply recognizing oneself as being overweight might set in motion this negative cycle that leads to weight gain and poor health.
Our mediation analyses provided some initial evidence that this might be the case. Weight gain mediated a large portion of the long-term prospective association between perceiving oneself as being overweight and health status as gauged by multiple biomarkers of cardiovascular, metabolic, and immune-system functioning and participant perceptions of physical health. In contrast, although the psychological experience attached to being overweight was predictive of increased depressive symptoms over time, this could not be explained by changes in body weight over time. It may be that such mechanisms as reduced self-esteem or negative body image explained this association.
The assumption has been that the failure of individuals who are objectively overweight to accurately identify their weight status may be a major public-health concern (Duncan et al., 2011; Johnson et al., 2014); however, our results point to a need for further examination of this assumption. Rather than increasing the likelihood that individuals will effectively manage their body weight, the stress and stigma associated with adiposity may render perceiving oneself as being overweight more detrimental than beneficial to health. If this is the case, well-intended attempts by health-care professionals and public-health officials to ensure that people in the medically defined overweight category identify as such could lead to unforeseen consequences in the long run. Our findings provide initial evidence that such consequences could include physiological dysregulation, depressive symptoms, and poor health. This possibility now warrants close examination using multiwave observational studies along with experimental and quasiexperimental designs with large samples and lengthy periods of follow-up (e.g., Almond et al., 2016).
This further work is necessary because our observational findings are limited in two key respects. First, although we could show that perceiving oneself as being overweight preceded declines in subjective health and increases in depressive symptoms, our measure of physiological dysregulation was available only at follow-up. We therefore cannot rule out the possibility of reverse causality, whereby the link between perceiving oneself as being overweight and subsequent dysregulation reflects the unobserved influence of baseline physiological dysregulation (see Fig. 1). Our mediation analyses partially mitigate this possibility: We have shown that weight gain over 7 years explains a large portion of the link between perceiving oneself as being overweight and subsequent dysregulation. Further, our additional analyses drawing on two further data sets found little evidence that controlling for initial dysregulation was likely to alter this mediation effect. However, additional waves of data are needed to definitively test whether perceived overweight prospectively predicts physiological dysfunction.
A second form of reverse causality that our data cannot directly address is the possibility that current weight perceptions partially reflect the human capacity to imagine future outcomes and anticipate weight gain and health changes. In this scenario, perceiving oneself as being overweight may not influence health; rather, such perceptions may simply reflect self-knowledge of the eventual effects of one’s diet and exercise patterns or of a family or genetic propensity for weight gain. To overcome this potential limitation, future studies could control for the perceived probability of future weight gain. Further, an examination of the mediating pathways from perceived overweight to the emergence of poor health (e.g., through discrimination experiences, stigma concerns, perceived stress, eating behavior) would help articulate the mechanisms underlying these links. Finally, using long-form measures of reported health coupled with latent change models would help ensure effect-size estimates are not attenuated by measurement error.
This study also has several important strengths. Using longitudinal analyses allowed us to examine how perceiving oneself as being overweight predicts changes in health and well-being over time. Further, by examining physiological dysregulation, a measure comprising objectively assessed clinical indicators, we could rule out the possibility that the link between perceived overweight and future health was due to differences in answering style (e.g., where people who tend to say negative things about their weight also do so about their health). Finally, we could show that weight gain explained a large portion of the link between perceiving oneself as being overweight and physiological dysregulation. This finding is notable because it supports a cyclical model whereby identifying with a stigmatized group may have a range of deleterious social-psychological consequences that perpetuate weight gain and lead to poor health (Tomiyama, 2014). Further, this finding also suggests that psychosocial and psychobiological pathways unrelated to weight gain must be examined to fully explain how perceiving oneself as being overweight may “get under the skin.” In conclusion, the current research provides initial evidence that perceiving oneself as being overweight may contribute to future health and sets the scene for studies exploring the psychosocial processes linking weight perceptions and subsequent ill health.
Supplementary Material
Acknowledgments
This research used data from the National Longitudinal Study of Adolescent Health (Add Health), which was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations.
Footnotes
Action Editor: Wendy Berry Mendes served as action editor for this article.
Declaration of Conflicting Interests: The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
Funding: E. Robinson was funded by the Medical Research Council and the Economic Research Council. A. R. Sutin was supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development Grant 1R15-HD083947.
Supplemental Material: Additional supporting information can be found at http://journals.sagepub.com/doi/suppl/10.1177/0956797617696311
Open Practices:

 All data and
materials have been made publicly available via Data Sharing for Demographic
Research and can be accessed at http://doi.org/10.3886/ICPSR21600.v17. The complete Open
Practices Disclosure for this article can be found at http://journals.sagepub.com/doi/suppl/10.1177/0956797617696311.
This article has received the badges for Open Data and Open Materials. More
information about the Open Practices badges can be found at https://www.psychologicalscience.org/publications/badges.
All data and
materials have been made publicly available via Data Sharing for Demographic
Research and can be accessed at http://doi.org/10.3886/ICPSR21600.v17. The complete Open
Practices Disclosure for this article can be found at http://journals.sagepub.com/doi/suppl/10.1177/0956797617696311.
This article has received the badges for Open Data and Open Materials. More
information about the Open Practices badges can be found at https://www.psychologicalscience.org/publications/badges.
References
- Almond D., Lee A., Schwartz A. E. (2016). Impacts of classifying New York City students as overweight. Proceedings of the National Academy of Sciences, USA, 113, 3488–3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atlantis E., Baker M. (2008). Obesity effects on depression: Systematic review of epidemiological studies. International Journal of Obesity, 32, 881–891. [DOI] [PubMed] [Google Scholar]
- Blodorn A., Major B., Hunger J. M., Miller C. (2016). Unpacking the psychological weight of weight stigma: A rejection-expectation pathway. Journal of Experimental Social Psychology, 63, 69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewis A. A. (2014). Stigma and the perpetuation of obesity. Social Science & Medicine, 118, 152–158. [DOI] [PubMed] [Google Scholar]
- Cuypers K., Kvaløy K., Bratberg G., Midthjell K., Holmen J., Holmen T. L. (2012). Being normal weight but feeling overweight in adolescence may affect weight development into young adulthood—an 11-year followup: The HUNT study, Norway. Journal of Obesity, 2012, Article 601872. doi: 10.1155/2012/601872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Boyce C. J., Wood A. M. (2015). A social rank explanation of how money influences health. Health Psy-chology, 34, 222–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dattilo A. M., Kris-Etherton P. M. (1992). Effects of weight reduction on blood lipids and lipoproteins: A meta-analysis. The American Journal of Clinical Nutrition, 56, 320–328. [DOI] [PubMed] [Google Scholar]
- DeSalvo K. B., Fan V. S., McDonell M. B., Fihn S. D. (2005). Predicting mortality and healthcare utilization with a single question. Health Services Research, 40, 1234–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan D. T., Wolin K. Y., Scharoun-Lee M., Ding E. L., Warner E. T., Bennett G. G. (2011). Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. International Journal of Behavioral Nutrition and Physical Activity, 8, 20. doi: 10.1186/1479-5868-8-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entzel P., Whitsel E. A., Richardson A., Tabor J., Hallquist S., Hussey J. M., Harris K. M. (2009). Add Health Wave IV documentation: Cardiovascular and anthropometric mea-sures. Retrieved from http://www.cpc.unc.edu/projects/addhealth/data/guides/WaveIVcardiovascularandanthropometricdocumentation110209.pdf
- Epel E. S., Lapidus R., McEwen B., Brownell K. (2001). Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psycho-neuroendocrinology, 26, 37–49. [DOI] [PubMed] [Google Scholar]
- Faith M. S., Butryn M., Wadden T. A., Fabricatore A., Nguyen A. M., Heymsfield S. B. (2011). Evidence for prospective associations among depression and obesity in population-based studies. Obesity Reviews, 12, e438–e453. doi: 10.1111/j.1467-789X.2010.00843.x [DOI] [PubMed] [Google Scholar]
- Ganna A., Ingelsson E. (2015). 5 year mortality predictors in 498 103 UK Biobank participants: A prospective population-based study. The Lancet, 386, 533–540. [DOI] [PubMed] [Google Scholar]
- Hampson S. E., Edmonds G. W., Goldberg L. R., Dubanoski J. P., Hillier T. A. (2013). Childhood conscientiousness relates to objectively measured adult physical health four decades later. Health Psychology, 32, 925–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K. M., Halpern C. T., Whitsel E., Hussey J., Tabor J., Entzel P., Udry J. R. (2009). The National Longitudinal Study of Adolescent to Adult Health: Research design.Retrieved from http://www.cpc.unc.edu/projects/addhealth/design
- Hayes A. F. (2013). An introduction to mediation, moderation, and conditional process modeling: A regression-based approach. New York, NY: Guilford Press. [Google Scholar]
- Hayward J., Millar L., Petersen S., Swinburn B., Lewis A. J. (2014). When ignorance is bliss: Weight perception, body mass index and quality of life in adolescents. International Journal of Obesity, 38, 1328–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuer C. A., McClure K. J., Puhl R. M. (2011). Obesity stigma in online news: A visual content analysis. Journal of Health Communication, 16, 976–987. [DOI] [PubMed] [Google Scholar]
- Himmelstein M. S., Incollingo Belsky A. C., Tomiyama A. J. (2015). The weight of stigma: Cortisol reactivity to manipulated weight stigma. Obesity, 23, 368–374. [DOI] [PubMed] [Google Scholar]
- Hunger J. M., Major B., Blodorn A., Miller C. (2015). Weighed down by stigma: How weight-based social identity threat influences weight gain and health. Social and Personality Psychology Compass, 9, 255–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussey J. M., Nguyen Q. C., Whitsel E. A., Richardson L. J., Halpern C. T., Gordon-Larsen P., Harris K. M. (2015). The reliability of in-home measures of height and weight in large cohort studies: Evidence from add health. Demographic Research, 32, 1081–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda J. P., Crawford P. B., Woodward-Lopez G. (2006). BMI screening in schools: Helpful or harmful. Health Education Research, 21, 761–769. [DOI] [PubMed] [Google Scholar]
- Incollingo Rodriguez A. C., Heldreth C. M., Tomiyama A. J. (2016). Putting on weight stigma: A randomized study of the effects of wearing a fat suit on eating, well-being, and cortisol. Obesity, 24, 1892–1898. [DOI] [PubMed] [Google Scholar]
- Johnson F., Beeken R. J., Croker H., Wardle J. (2014). Do weight perceptions among obese adults in Great Britain match clinical definitions? Analysis of cross-sectional surveys from 2007 and 2012. BMJ Open, 4, Article e005561. doi: 10.1136/bmjopen-2014-005561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunst A. E., Bos V., Lahelma E., Bartley M., Lissau I., Regidor E., Helmert U. (2005). Trends in socioeconomic inequalities in self-assessed health in 10 European countries. International Journal of Epidemiology, 34, 295–305. [DOI] [PubMed] [Google Scholar]
- Linn R. L., Slinde J. A. (1977). The determination of the significance of change between pre- and posttesting periods. Review of Educational Research, 47, 121–150. [Google Scholar]
- Martin B. C., Dalton W. T., Williams S. L., Slawson D. L., Dunn M. S., Johns-Wommack R. (2014). Weight status misperception as related to selected health risk behaviors among middle school students. Journal of School Health, 84, 116–123. [DOI] [PubMed] [Google Scholar]
- Neter J. E., Stam B. E., Kok F. J., Grobbee D. E., Geleijnse J. M. (2003). Influence of weight reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension, 42, 878–884. [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Robinson E., Hunger J. M., Daly M. (2015). Perceived weight status and risk of weight gain across life in US and UK adults. International Journal of Obesity, 12, 1721–1726. [DOI] [PubMed] [Google Scholar]
- Robinson E., Oldham M. (2016). Weight status misperceptions among UK adults: The use of self-reported vs. measured BMI. BMC Obesity, 3, Article 21. doi: 10.1186/s40608-016-0102-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Sutin A. (2016). Parental perception of weight status and weight gain across childhood. Pediatrics, 137(5), Article e20153957. doi: 10.1542/peds.2015-3957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Sutin A. R., Daly M. (2017). Perceived weight discrimination mediates the longitudinal relation between obesity and depressive symptoms in US and UK adults. Health Psychology, 36, 112–121. doi: 10.1037/hea0000426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T. E., McEwen B. S., Rowe J. W., Singer B. H. (2001). Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences, USA, 98, 4770–4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikorski C., Luppa M., Luck T., Riedel-Heller S. G. (2015). Weight stigma “gets under the skin”—evidence for an adapted psychological mediation framework—a systematic review. Obesity, 23, 266–276. [DOI] [PubMed] [Google Scholar]
- Sutin A. R., Robinson E., Daly M., Terracciano A. (2016). Weight discrimination and unhealthy eating-related behaviors. Appetite, 102, 83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Stephan Y., Carretta H., Terracciano A. (2015). Perceived discrimination and physical, cognitive, and emotional health in older adulthood. The American Journal of Geriatric Psychiatry, 23, 171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Stephan Y., Grzywacz J. G., Robinson E., Daly M., Terracciano A. (2016). Perceived weight discrimination, changes in health, and daily stressors. Obesity, 24, 2202–2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Terracciano A. (2013). Perceived weight discrimination and obesity. PLoS ONE, 8, Article e70048. doi: 10.1371/journal.pone.0070048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Terracciano A. (2015). Body weight misperception in adolescence and incident obesity in young adulthood. Psychological Science, 26, 507–511. [DOI] [PubMed] [Google Scholar]
- Swahn M. H., Reynolds M. R., Tice M., Miranda-Pierangeli M. C., Jones C. R., Jones I. R. (2009). Perceived overweight, BMI, and risk for suicide attempts: Findings from the 2007 Youth Risk Behavior Survey. Journal of Adolescent Health, 45, 292–295. [DOI] [PubMed] [Google Scholar]
- Teachman B. A., Brownell K. D. (2001). Implicit anti-fat bias among health professionals: Is anyone immune? International Journal of Obesity & Related Metabolic Disorders, 25, 1525–1531. [DOI] [PubMed] [Google Scholar]
- Tomiyama A. J. (2014). Weight stigma is stressful: A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite, 82, 8–15. [DOI] [PubMed] [Google Scholar]
- Williams D. R., Mohammed S. A. (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32, 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.