Abstract
Background
To assess the current landscape of the heart failure (HF) epidemic and provide targets for future health policy interventions in Medicare, a contemporary appraisal of its epidemiology across inpatient and outpatient care settings is needed.
Methods and Results
In a national 5% sample of Medicare beneficiaries from 2002-2013, we identified a cohort of 2,331,939 unique fee-for-service Medicare beneficiaries ≥65-years-old followed for all inpatient and outpatient encounters over a 10-year period (2004-2013). Pre-existing HF was defined by any HF encounter during the first year, and incident HF with either one inpatient or two outpatient HF encounters. Mean age of the cohort was 72 years; 57% were women, and 86% and 8% were white and black, respectively. Within this cohort, 518,223 patients had pre-existing HF, and 349,826 had a new diagnosis of HF during the study-period. During 2004-2013, the rates of incident HF declined 32%, from 38.7 per 1000 (2004) to 26.2 per 1000 beneficiaries (2013). In contrast, prevalent HF increased during our study period from 162 per 1000 (2004) to 172 per 1000 beneficiaries (2013) (Ptrend<0.001 for both). Finally, the overall 1-year mortality among patients with incident HF is high (24.7%) with a 0.4% absolute decline annually during the study period, with a more pronounced decrease among those diagnosed in an inpatient vs outpatient setting (Pinteraction<.001)
Conclusions
In recent years, there have been substantial changes in the epidemiology of HF in Medicare beneficiaries, with a decline in incident HF and a decrease in 1-year HF mortality, while the overall burden of HF continues to increase.
Journal Subject Terms: Heart failure, Incidence, Prevalence, Cardiovascular Outcomes
Heart failure affects 6.5 million Americans and is associated with nearly $31 billion in healthcare costs annually.1 Given the high societal burden of heart failure, a clear understanding of epidemiological trends is critical for determining future workforce needs, focusing drug and device discovery investments, and prioritizing health care policy initiatives.
The epidemiology of heart failure has experienced substantial changes over time. Over a time period from the 1970’s to 1990’s when atherosclerotic cardiovascular disease rates were falling steadily, heart failure incidence increased annually, likely due to aging of the population and better survival with atherosclerotic cardiovascular disease.2 After stabilizing in the mid-1990s a trend towards declining HF incidence was reported over the next decade.3–5 For example, among fee-for-service Medicare beneficiaries, a 10% drop in the rates of new diagnosis of heart failure was reported from 1994-2003,.6 with similar trends reported from other Western countries.7 A more recent investigation from Olmstead County suggested that rates of incident heart failure declined in that community even more rapidly in the most recent decade, with a 37.5% decline from 2003-2013.8 A similar pattern has been observed in a nationwide Danish investigation which documented a 30-40% decline in heart failure incidence in the elderly during 1995-2012.9
However, it is unknown if the changes in heart failure epidemiology observed in the U.S. are driven by regionally-limited factors or represent a larger shift in heart failure epidemiology experienced by the health system. Recent investigations examining this question have focused solely on heart failure hospitalizations,10 which do not account for new cases diagnosed in an outpatient setting, something increasingly likely given the trend towards shifting care from inpatient to outpatient settings. In present study, using an administrative cohort of fee-for-service Medicare beneficiaries, we assessed calendar-year trends in heart failure incidence during the last decade, and elucidated annual rates of new heart failure cases in both inpatient and outpatient settings, as well as the burden of prevalent disease and 1-year heart failure mortality rates. Further, we elucidated trends in incident and prevalent heart failure in major demographic and regional subgroups.
METHODS
Data Sources
The 5% national Medicare limited data set for the years 2002-2013 was the data source for the study. The Medicare 5% dataset is an unbiased sample designed by the Center for Medicare and Medicaid Services (CMS) and represents a 5% sample of all Medicare beneficiaries in the US.6 Briefly, for every 100 new Medicare enrollees, based on a predetermined combination of beneficiary identification numbers, five are randomly selected into the sample and are represented in the datasets for all the subsequent years. The data for each year consists of information on Medicare eligibility classification (fee-for-service vs. managed care), and claims submitted to Medicare for reimbursement for all healthcare contacts across both inpatient (Medicare part A) and outpatient (Medicare part B) settings. Claim records are captured separately in inpatient and outpatient claims files, and claims submitted by individual physicians are captured in carrier files. Each of these Medicare claim-files includes information on dates of encounter (as calendar quarters) as well as up to 10 associated diagnosis and procedure codes (reported as International Classification of Diseases-9th edition [ICD-9] codes). Further, an accompanying annual record provides information on demographic characteristics, including patient age (in years), sex, race and the date of death for patients who died during that calendar year. The date of death was available as exact dates throughout the study period.
The Medicare data used in the study are proprietary and owned by the CMS. Therefore, while the authors cannot make them available to the public for purposes of reproducing the results, these can be obtained from the CMS directly.
Study population
We identified all fee-for-service Medicare beneficiaries ≥65 years of age with at least 1 year of continuous enrollment in both Medicare Parts A and B (eFigure 1 in the Online Supplement). Similar to prior studies,6 we selected fee-for-service enrollees with data on both Medicare Part A and B coverage since we wanted complete information on all potential inpatient and outpatient care encounters. Further, only elderly Medicare were included since those <65 years are not representative of the larger Medicare population. Of the total 3,915,899 unique Medicare beneficiaries in our sample, patients with missing identification numbers (n = 54), age <65 years (n=748,712, 19%), and overall enrollment period of <1 year (n = 270,993, 6.8%) were not included. For those with ≥1 year of enrollment, those who did not have even 1 calendar-year of continuous fee-for-service follow up in the cohort were also not included – i.e. those with 1 or more months of non-enrollment in parts A and B (n=234,506, 6%) or enrollment in Medicare managed care (n= 329,641, 8%) for every calendar year throughout the analysis period were not included. All patients were followed as a longitudinal cohort until their death, end of the study, or at their first transition out of Medicare fee-for-service coverage.
Study Variables and Outcomes
Medicare insurance claims records for beneficiaries selected into the cohort were reviewed for the entire period of follow-up. We identified heart failure encounters using a combination of International Classification of Diseases-9th edition (ICD-9) codes 428.x, 402.x1, 404.x1, and 404.x3 as any of the diagnosis codes on the claim record. These codes have been validated for identification of heart failure and are currently used by the American Heart Association’s Get With The Guidelines-Heart Failure registry as well as CMS to identify heart failure encounters.11–13 Further, we queried all healthcare claims files (inpatient and outpatient) for previously validated combinations of ICD-9 codes to identify both the number and the nature of comorbidities recorded for each patient for every calendar-year in the study, using the Charlson comorbidities:14 myocardial infarction (acute or prior), peripheral vascular disease, cerebrovascular disease, dementia, chronic lung disease, connective tissue disease, peptic ulcer disease, liver disease, diabetes with and without end-organ complications, hemiplegia, moderate or severe kidney disease, any malignancy, including leukemia and lymphoma, metastatic solid tumors, rheumatologic disease, and acquired immunodeficiency syndrome. We also included additional comorbidities that are relevant in the context of heart failure, specifically, hypertension, atrial fibrillation, obesity and valvular heart disease.
Statistical analyses
First, we identified patients with pre-existing heart failure for each calendar year. Patients with pre-existing heart failure were defined by any claim record in the inpatient, outpatient or carrier claim files with a diagnostic code for heart failure in any position (i.e. primary, secondary, etc.) during the first year of their entry into the analysis. Second, among patients without a diagnosis of heart failure within the first year, we identified patients who subsequently developed new-onset or incident heart failure, based on healthcare encounters for heart failure. Incident heart failure was defined by either one inpatient claim with a diagnosis code for heart failure or ≥2 outpatient or carrier claims with a heart failure code in two separate calendar quarters. The latter criterion to select outpatient heart failure was intentionally more stringent to ensure that at least 2 encounters separated in time were consistent with a heart failure diagnosis. Further, resolution of 2 outpatient encounters was set at calendar quarters since claims for the all years through 2008 were reported as calendar-quarters, as opposed to exact dates. We reorganized data for 2009 through 2013 when exact dates were reported into calendar quarters to maintain consistency over the study period. All encounters within a calendar-quarter were assigned to the first day of the quarter for the respective years (January 1 for the 1st calendar-quarter 1, April 1 for the 2nd quarter, July 1 for 3rd calendar, and October 1 for the 4th quarter, within respective calendar-years). Further, similar to prior studies,6 outpatient encounters for heart failure included any of the encounters that are represented in the outpatient/carrier files, including clinic visits, emergency department visits, observation care and urgent care.
We obtained rates of new heart failure diagnosis for each year for the 10-year period between 2004 and 2013, allowing for additional years (2002 and 2003) of lookback at the start of the analysis to exclude pre-existing heart failure. Next, we calculated age-adjusted rates of new heart failure diagnoses using Poisson regression, using age at the time of the diagnosis. Third, we examined differences in patient characteristics at the time of the diagnosis across calendar years, including patient demographics (age, sex and race) and comorbid conditions. Next, we examined trends in incident heart failure within major demographics groups, including age groups (65-69, 70-74, 75-79, 80-85, and over 85 years of age), sex (men vs. women) and racial groups (white, black, Hispanic and Asian), as well as across the 4 major U.S. Census regions (Midwest, Northeast, West, South). Next, prevalent heart failure for each calendar year was defined by the sum of the number of unique individuals with pre-existing and incident heart failure for the respective years as well as those with incident heart failure in preceding years. Finally, to assess changes in early mortality after a heart failure diagnosis, we calculated 1-year risk-adjusted hazard for mortality using Cox-proportional hazards model with calendar-year of diagnosis as the exposure, and the study start year (2004) as the reference year. Our risk-adjustment model accounted for age, sex, race and Charlson comorbidities enumerated above. The year 2004 was the reference year for these analyses, and population characteristics and observed mortality rates for patients with incident heart failure in this year represented the reference values for calendar-year trends in risk-adjusted mortality.
Sensitivity analyses
We conducted several sensitivity analyses to assess the robustness of our findings pertaining to the identification of incident heart failure. First, to examine the effect of missed prevalent disease in the 1 year look-back period that may have been miscategorized as incident heart failure, we considered an alternative look back period of 2 years. In this approach, any heart failure encounter within the first 2 years after the start of the analysis period for patients was considered prevalent disease, and incident heart failure was diagnosed in patients with at least 2 prior years of records without any heart failure claims. Second, we used alternative, more stringent definitions to identify a new diagnosis of heart failure, including using (i) only one inpatient encounter, (ii) one inpatient or two outpatient encounters, and (iii) one inpatient or three outpatient encounters for the diagnoses of heart failure to account for different methodologies suggested in published research using Medicare data.6
Analyses were performed using SAS 9.4 (Cary, NC). All statistical tests were two-sided, and the level of significance was set at an alpha of 0.05. The study was reviewed and approved by the institutional review board at the University of Texas Southwestern Medical Center, and since the data were de-identified, the requirement for informed consent was waived.
RESULTS
We identified 2,331,993 unique fee-for-service Medicare beneficiaries ≥65 years of age with at least one year of continuous study eligibility. There were a mean 1.3 million eligible patients in the study annually (eFigure 2 in the Online Supplement), with median follow up of 62 months (interquartile range: 29 to 120 months). The mean age of study participants at the beginning of the analysis period was 72 years, 57% were women, and 86% and 8% were white and black, respectively.
Within this cohort, 518,223 patients had pre-existing heart failure, defined by a heart failure encounter during the first year of eligibility for the analysis. Among patients without pre-existing heart failure, 349,826 patients had a new diagnosis of heart failure over the 10 years of follow-up. Of these, 207,687 (59.4%) were diagnosed in the inpatient setting and 142,139 (40.6%) in the outpatient setting. Trends in incident and prevalent heart failure across calendar years are presented in Figure 1A. The rates of incident heart failure, defined by either one inpatient or 2 distinct outpatient encounters (in two calendar quarters), declined 32% over the study period, from 38.7 per 1000 beneficiaries during 2004 to 26.2 per 1000 beneficiaries during 2013 (P-trend <0.001, Figure 1A and 1B). The decline was observed in both the inpatient and outpatient settings, though the decline in hospitalizations was most prominent (P for interaction, 0.003; Figure 1B), and the proportion of outpatient diagnoses of heart failure relative to the total increased from 36% in 2004 to 41% in 2013 (P for trend <0.001).
Figure 1.
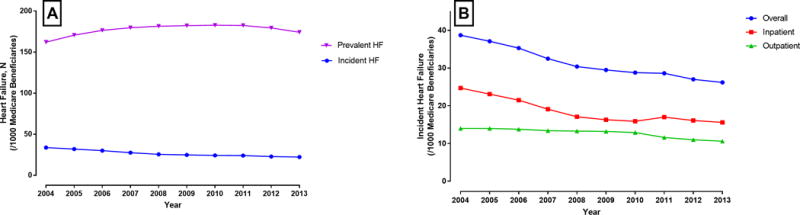
(A) Calendar-year trends in incidence and prevalence (pre-existing + incident) of heart failure in fee-for-service Medicare beneficiaries in a claims-based administrative cohort – defined in detail in Methods section. (B) Trends in incidence of overall, inpatient, and outpatient heart failure (P<.001 for all).
The mean age at diagnosis of heart failure was 80 years and this did not vary substantially across study years. Table 1 presents calendar-year trends in patient characteristics at the time of diagnosis of incident heart failure. Age-adjusted trends in new heart failure diagnosis closely follow the unadjusted trends (eFigure 3 in the Online Supplement). Throughout the study period, there was a modest increase in comorbid conditions including myocardial infarction, peripheral artery disease, cerebrovascular disease, and chronic obstructive pulmonary disease. There was also a near doubling in the rates of co-existing chronic kidney disease (18.9% to 37%). While there was a decline in incident heart failure, the proportion of prevalent heart failure increased during our study period from 162 per 1000 in 2004 to 172 per 1000 beneficiaries during 2013 (P-trend <0.001, Figure 1A).
Table 1.
Patient characteristics at the time of diagnosis of incident heart failure, by calendar-year of diagnosis.
| Characteristics at HF diagnosis | 2004–05 | 2006–2007 | 2008–09 | 2010–11 | 2012–13 | P-trend |
|---|---|---|---|---|---|---|
| N | 90617 | 77141 | 65055 | 60987 | 56026 | |
| Age in years (SD) | 79.7 (7.6) | 79.7 (7.6) | 80.1 (7.7) | 79.9 (8.0) | 79.9 (8.1) | <.001 |
| Men, % | 42.0 | 42.3 | 42.4 | 43.5 | 44.2 | <.001 |
| Race | 0.69 | |||||
| White, % | 87.5 | 87.8 | 87.8 | 87.7 | 88.2 | |
| Black, % | 8.4 | 8.0 | 7.7 | 7.8 | 7.4 | |
| Others, % | 3.9 | 4.1 | 4.4 | 4.4 | 4.4 | |
| Missing/Unknown, % | 0.2 | 0.1 | 0.1 | 0.1 | 0.2 | |
| Region* | <.001 | |||||
| Midwest, % | 26.4 | 26.0 | 25.2 | 24.7 | 24.6 | |
| Northeast, % | 19.7 | 20.3 | 20.2 | 20.0 | 20.1 | |
| South, % | 38.8 | 38.6 | 39.3 | 39.7 | 39.4 | |
| West, % | 14.1 | 14.6 | 14.9 | 15.2 | 15.5 | |
| Comorbid conditions | ||||||
| Any MI | 24.8 | 23.8 | 23.3 | 24.0 | 26.1 | <.001 |
| Atrial fibrillation | 14.3 | 11.2 | 9.2 | 7.9 | 7.3 | <.001 |
| Hypertension | 70.3 | 70.0 | 67.8 | 66.7 | 65.9 | <.001 |
| Obesity | 3.1 | 3.3 | 3.6 | 4.3 | 5.0 | <.001 |
| Peripheral Disease | 22.8 | 23.6 | 24.6 | 26.2 | 26.4 | <.001 |
| Cerebrovascular Disease | 33.3 | 34.5 | 34.6 | 34.6 | 34.5 | <.001 |
| Chronic Pulmonary Disease | 46.8 | 46.1 | 45.2 | 46.6 | 47.4 | 0.06 |
| Diabetes Mellitus without end-organ damage | 39.7 | 41.0 | 41.2 | 41.8 | 42.2 | <.001 |
| Diabetes with end-organ damage | 10.7 | 11.5 | 12.0 | 13.0 | 13.9 | <.001 |
| Moderate or Severe Renal Disease | 18.9 | 25.5 | 28.3 | 33.2 | 37.0 | <.001 |
| Connective Tissue Disease | 5.4 | 5.7 | 6.1 | 6.3 | 6.4 | <.001 |
| Leukemia/Metastatic Malignancy | 5.3 | 5.2 | 5.0 | 5.0 | 5.4 | 0.82 |
| Valvular Heart Disease | 15.4 | 13.9 | 12.8 | 11.9 | 11.3 | <.001 |
| Charlson Comorbidity Score | 4.3 (2.7) | 4.4 (2.8) | 4.5 (2.8) | 4.7 (2.8) | 4.8 (2.9) | <.001 |
The overall unadjusted 1-year mortality rate among patients with incident heart failure was 24.4%, with rates of 31.9% and 13.5% for heart failure diagnosed as inpatient and outpatient, respectively. Trends in observed mortality rates in subgroups based on age, sex, race/ethnicity, and US census regions are presented in eFigure 4 in the Online Supplement. Risk-adjusted mortality in patients within 1 year from diagnosis of heart failure improved from 25.7% to 23.0% during the study period (Figure 2A). The risk-adjusted 1-year mortality after incident heart failure in the inpatient setting declined between the years 2004 and 2010 (32.9% in 2004 to 27.8% in 2010, P for trend <.001), with a small increase between 2010 and 2012 (27.8% in 2010 to 31.1% in 2012). There was a modest, but statistically significant, decline in mortality following incident heart failure in the outpatient setting for the entire study period (13.0% in 2004 to 12.3% in 2012, P for trend =.02). While mortality declined for patients with both inpatient and outpatient diagnosis of heart failure, there was a more prominent decline among those with an inpatient diagnosis (P for diagnosis type and calendar-year interaction <.001), with an absolute decline in 1-year mortality by 0.36% per year in the inpatient compared with 0.15% per year in the outpatient setting (Figure 2B). Decline in mortality was observed consistently across demographic subgroups defined by sex and race (P for interaction > 0.10 for both).
Figure 2.
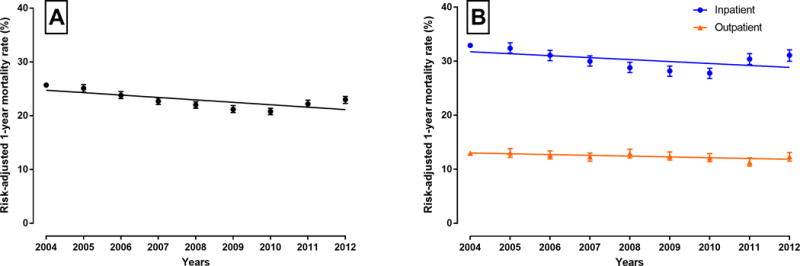
(A) Calendar-year trends in risk-adjusted 1-year mortality rate among patients with incident diagnosis of heart failure (reference year: 2004) (B) Calendar-year trends in risk-adjusted 1-year mortality rate among patients with inpatient and outpatient diagnoses of heart failure (reference year: 2004)
In subgroup analyses, rates of incident heart failure declined across age-groups with the greatest decline in the oldest age group (>85 years of age: 92.6/1000 in 2004 to 70.5/1000 in 2013) (Figure 3A). There were notable sex differences in rates of new heart failure diagnosis in Medicare, with higher rates in men compared with women throughout the study period (Figure 3B). There was a consistent decline in rates of incident heart failure in both men and women (P for calendar-year*sex interaction > 0.10). Among racial/ethnic groups, self-reported blacks had the highest rates of new heart failure diagnosis, followed by Hispanics, whites, and Asians (Figure 3C). Further, black patients were, on average, 2 years younger than the white patients at diagnosis (P<.001). Notably, racial/ethnic differences in heart failure incidence persisted across the years of our study with consistently higher heart failure incidence among blacks across study years (P for calendar-year*black-white race interaction > 0.10). Finally, in our pre-specified analysis by U.S. census regions, Western region had the lowest incidence of heart failure (P<.001, west vs other regions), with similar rates across the other three census regions (P=0.12) and a consistent decline in heart failure incidence over time seen across all four regions (Figure 3D, P for interaction for region > 0.10). Consistent with the overall population, prevalent heart failure increased across demographic subgroups of sex and race, as well as all four U.S. census regions (Figure 4A–C).
Figure 3.
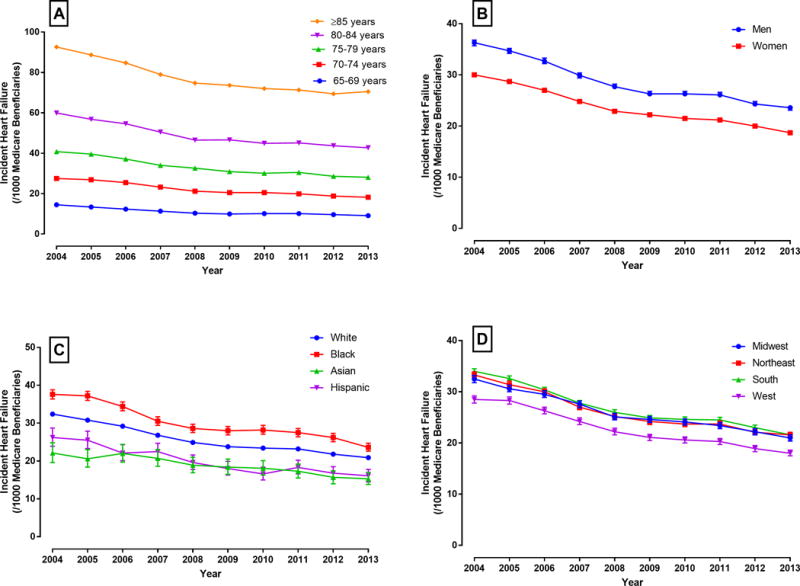
Trends in incidence of heart failure in subgroups of Medicare beneficiaries by (A) age, (B) Sex (age-adjusted), (C) Race (age-adjusted), and (D) US census regions (age-adjusted).
Figure 4.
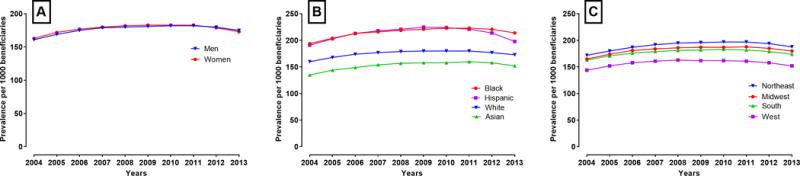
Trends in prevalence of heart failure in subgroups of Medicare beneficiaries by (A) Sex, (B) Race, and (C) US census regions.
In sensitivity analyses, based on longer period of look-back to define prevalent heart failure as well as 4 different definitions to identify incident heart failure (eFigures 5–8 in the Online Supplement) we found that the decline in rates of new heart failure diagnosis was consistent with our primary analysis.
DISCUSSION
In this large, national cohort study of fee-for-service Medicare beneficiaries followed for a decade, we made the following key observations. First, there has been a >30% decline in the rates of new heart failure diagnoses across inpatient and outpatient care settings over the 10-year study period between 2004 and 2013, though the decline in hospitalizations was most prominent. Second, rates of incident heart failure varied across demographic groups, with a higher incidence with advancing age and among men compared with women, and blacks compared with whites. Third, there has been a decline in 1-year mortality after a new diagnosis of heart failure across the study period, which was more prominent for diagnoses in the inpatient setting. Finally, in contrast to incident heart failure which has declined over time, there has been an increase in prevalent heart failure over the years of the present study, across demographic and geographic subgroups.
This is the first national-level study of U.S patients that demonstrates a decline in the number of new heart failure cases over the last decade. We observe a 30% decline in the rates of incident heart failure that is consistent with a declining trend in incident heart failure over the last two decades,2 and is qualitatively similar to the 37.5% decline observed in Olmstead County during the same period.8 A Danish study has recently also demonstrated a similar nationwide decline in incident heart failure among the elderly.9 Further, a prior study in the Medicare fee-for-service population demonstrated a decline in first heart failure hospitalizations from 28 per 1000 in 1998 to 20 per 1000 in 2008.10 Our study, which includes both inpatient and outpatient diagnoses of heart failure, provides evidence that the decline observed in the inpatient setting does not merely reflect transition of diagnosis and care from the inpatient to the outpatient setting, since a decline is observed in both settings. However, with an outpatient diagnosis representing an increasing proportion of all heart failure diagnoses, studies that rely solely on inpatient heart failure diagnoses are likely to provide only a partial assessment of the heart failure epidemic. The trend observed in our study is consistent across groups defined by sex, race, and U.S. census regions, suggesting that common factors underlie these temporal changes.
In contrast to the decline in incident heart failure cases, we found an increasing burden of both unique Medicare beneficiaries with prevalent heart failure each year, consistent with prior reports suggesting that the overall burden of the heart failure epidemic continues to rise.13 Our study suggests that the impact of heart failure on the healthcare system is being influenced by the decreasing mortality with heart failure, thereby resulting in an increasing number of patients surviving with heart failure. Therefore, from a resource utilization perspective, the declining incident heart failure is outweighed by declining mortality, with increasing current and future healthcare costs and expenditures for heart failure. Therefore, in addition to continued emphasis on heart failure prevention, further resources would need to be directed towards a potentially aging heart failure population with the associated resource-intensive care and need for advanced therapies. Future studies are needed to evaluate new strategies to mitigate the continued high burden of heart failure on the healthcare system.
The underlying cause of the observed decline in incident heart failure is unknown. Several improvements in the management of risk factors for heart failure may be implicated. These include improved management of both diabetes and hypertension,15–19 treatment of acute and chronic coronary disease with guideline directed therapy including statins and anti-platelet agents,20–23 and rapid revascularization in acute myocardial infarction and improvements in post-myocardial infarction care.24, 25 Additionally, some of the observed changes in the rates of incident heart failure across studies may represent better discrimination of heart failure from its mimics. The introduction of B-type natriuretic peptide testing has likely increased the specificity of heart failure diagnoses,26 as well as the more widespread use of echocardiography.27, 28 Thus, epidemiological changes may represent in part more accurate diagnosis of heart failure, with the reporting of fewer false positive cases.
Our study findings should be interpreted in the light of the following limitations. First, heart failure in our study is based on administrative records and has not been independently adjudicated. However, the combination of ICD-9 codes used in our study is consistent with those used by both CMS and heart failure registries,13, 29 and have been demonstrated to be both sensitive and specific for the identification of heart failure in large validation studies.11 Also, our findings are in agreement with other prior studies which demonstrate similar trends in regional U.S. cohorts and studies in other industrialized countries.3, 7–9 Further, the ascertainment of heart failure within an administrative record forms the basis for healthcare resource allocation as well as health policy interventions. Second, we do not have information on heart failure subtypes since the administrative codes for heart failure with reduced and preserved ejection fraction, and with acute decompensated heart failure have not been independently validated. Therefore, it is possible that the trends observed in our study do not apply to individual subtypes. Third, our study cannot make assumptions about the non-fee-for-service Medicare beneficiaries, represented by the Medicare managed-care population, since claim-level data are not available for these patients. However, differences in HMO participation are unlikely to explain differences in our study findings since Medicare studies during our study period have revealed that HMO rates have remained stable and represent a modest proportion of total Medicare beneficiaries.13 Fourth, we did not examine patterns of heart failure among patients below 65 years of age since the younger Medicare beneficiaries mostly reflect those with end stage renal disease and severe disability and are not representative of the general population. Future studies are needed to assess if trends in rates of new heart failure diagnosis vary in younger age groups. Finally, our assessment of heart failure only represents Medicare beneficiaries who sought medical care, and community-level assessment of prevalence and incidence of heart failure cannot be inferred. However, the care-seeking practices for heart failure within a closed insurance system is unlikely to be a function of time, and therefore, unlikely to account for our study findings.
In conclusion, while there has a been an increasing burden of prevalent heart failure in Medicare beneficiaries during 2004-2013, the number of unique fee-for-service Medicare beneficiaries with a new heart failure diagnosis has declined annually during the same period. This has been accompanied by an overall improvement in 1-year mortality after heart failure diagnosis. Our study suggests that along with emphasis on heart failure prevention and appropriate identification, health policy interventions should focus on the needs of an aging heart failure population.
Supplementary Material
Clinical Perspective.
What is new?
Between 2004-2013, the rate of new diagnosis of heart failure among elderly Medicare beneficiaries declined across both inpatient and outpatient healthcare settings. The 1-year mortality rate after a diagnosis of heart failure was high but improved during this period.
The prevalence of heart failure continued to increase throughout this period. Further, in more recent years, heart failure is increasingly being diagnosed in the outpatient setting, and patients with an outpatient diagnosis have a lower 1-year mortality after their diagnosis, compared with those for whom a hospitalization represents their first manifestation of heart failure.
What are the clinical implications?
Given the evolving landscape of heart failure among the elderly and the rising proportion of heart failure being diagnosed and managed in the outpatient setting, healthcare systems would need to focus on strengthening outpatient care services for heart failure.
Further, our observations suggest that while fewer patients are being diagnosed with heart failure, the mortality rates in the year following the diagnosis and the rising prevalence of heart failure continue to be major challenges.
Healthcare interventions would need to be aimed at understanding and improving the care patients receive in the period following their diagnosis of heart failure.
Acknowledgments
Funding Sources: Dr Berry receives funding from the American Heart Association prevention network (14SFRN20740000). Dr. Khera is supported by the National Heart, Lung, and Blood Institute (5T32HL125247-02) and the National Center for Advancing Translational Sciences (UL1TR001105) of the National Institutes of Health. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Disclosures: None.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Statistics C and Stroke Statistics S Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. doi: 10.1038/nrcardio.2010.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roger VL. Epidemiology of heart failure. Circ Res. 2013;113:646–59. doi: 10.1161/CIRCRESAHA.113.300268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–50. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 5.Croft JB, Giles WH, Pollard RA, Casper ML, Anda RF, Livengood JR. National trends in the initial hospitalization for heart failure. J Am Geriatr Soc. 1997;45:270–5. doi: 10.1111/j.1532-5415.1997.tb00939.x. [DOI] [PubMed] [Google Scholar]
- 6.Curtis LH, Whellan DJ, Hammill BG, Hernandez AF, Anstrom KJ, Shea AM, Schulman KA. Incidence and prevalence of heart failure in elderly persons, 1994-2003. Arch Intern Med. 2008;168:418–24. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 7.Jhund PS, Macintyre K, Simpson CR, Lewsey JD, Stewart S, Redpath A, Chalmers JW, Capewell S, McMurray JJ. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009;119:515–23. doi: 10.1161/CIRCULATIONAHA.108.812172. [DOI] [PubMed] [Google Scholar]
- 8.Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, Killian JM, Roger VL. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175:996–1004. doi: 10.1001/jamainternmed.2015.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christiansen MN, Kober L, Weeke P, Vasan RS, Jeppesen JL, Smith JG, Gislason GH, Torp-Pedersen C, Andersson C. Age-specific Trends in Incidence, Mortality and Comorbidities of Heart Failure in Denmark 1995-2012. Circulation. 2017;135:1214–1223. doi: 10.1161/CIRCULATIONAHA.116.025941. [DOI] [PubMed] [Google Scholar]
- 10.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306:1669–78. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kucharska-Newton AM, Heiss G, Ni H, Stearns SC, Puccinelli-Ortega N, Wruck LM, Chambless L. Identification of Heart Failure Events in Medicare Claims: The Atherosclerosis Risk in Communities (ARIC) Study. J Card Fail. 2016;22:48–55. doi: 10.1016/j.cardfail.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gage BF, Boechler M, Doggette AL, Fortune G, Flaker GC, Rich MW, Radford MJ. Adverse outcomes and predictors of underuse of antithrombotic therapy in medicare beneficiaries with chronic atrial fibrillation. Stroke. 2000;31:822–7. doi: 10.1161/01.str.31.4.822. [DOI] [PubMed] [Google Scholar]
- 13.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999-2011. Circulation. 2014;130:966–75. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. Journal of clinical epidemiology. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 15.Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–14. doi: 10.1161/CIRCULATIONAHA.112.096156. [DOI] [PubMed] [Google Scholar]
- 16.Gu Q, Paulose-Ram R, Dillon C, Burt V. Antihypertensive medication use among US adults with hypertension. Circulation. 2006;113:213–21. doi: 10.1161/CIRCULATIONAHA.105.542290. [DOI] [PubMed] [Google Scholar]
- 17.Yoon SS, Gu Q, Nwankwo T, Wright JD, Hong Y, Burt V. Trends in blood pressure among adults with hypertension: United States, 2003 to 2012. Hypertension. 2015;65:54–61. doi: 10.1161/HYPERTENSIONAHA.114.04012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander GC, Sehgal NL, Moloney RM, Stafford RS. National trends in treatment of type 2 diabetes mellitus, 1994-2007. Arch Intern Med. 2008;168:2088–94. doi: 10.1001/archinte.168.19.2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clemens KK, Shariff S, Liu K, Hramiak I, Mahon JL, McArthur E, Garg AX. Trends in Antihyperglycemic Medication Prescriptions and Hypoglycemia in Older Adults: 2002-2013. PLoS One. 2015;10:e0137596. doi: 10.1371/journal.pone.0137596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minard LV, Corkum A, Sketris I, Fisher J, Zhang Y, Saleh A. Trends in Statin Use in Seniors 1999 to 2013: Time Series Analysis. PLoS One. 2016;11:e0158608. doi: 10.1371/journal.pone.0158608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, Virani SS, Blankstein R, Khera A, Blaha MJ, Blumenthal RS, Lloyd-Jones D, Nasir K. National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013: Insights From the Medical Expenditure Panel Survey. JAMA Cardiol. 2017;2:56–65. doi: 10.1001/jamacardio.2016.4700. [DOI] [PubMed] [Google Scholar]
- 22.Weintraub WS. Perspective on Trends in Statin Use. JAMA Cardiol. 2017;2:11–12. doi: 10.1001/jamacardio.2016.4710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Keeffe AG, Nazareth I, Petersen I. Time trends in the prescription of statins for the primary prevention of cardiovascular disease in the United Kingdom: a cohort study using The Health Improvement Network primary care data. Clin Epidemiol. 2016;8:123–32. doi: 10.2147/CLEP.S104258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiomi H, Nakagawa Y, Morimoto T, Furukawa Y, Nakano A, Shirai S, Taniguchi R, Yamaji K, Nagao K, Suyama T, Mitsuoka H, Araki M, Takashima H, Mizoguchi T, Eisawa H, Sugiyama S, Kimura T, investigators CR-KA Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;344:e3257. doi: 10.1136/bmj.e3257. [DOI] [PubMed] [Google Scholar]
- 25.Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–9. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 26.Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, Omland T, Storrow AB, Abraham WT, Wu AH, Clopton P, Steg PG, Westheim A, Knudsen CW, Perez A, Kazanegra R, Herrmann HC, McCullough PA, Breathing Not Properly Multinational Study I Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347:161–7. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 27.Virnig BA, Shippee ND, O’Donnell B, Zeglin J, Parashuram S. Data Points Publication Series [Internet] Rockville (MD): Agency for Healthcare Research and Quality (US); 2011. Trends in the use of echocardiography, 2007 to 2011: Data Points #20. 2014 May 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK208663/. Accessed October 14, 2017. [PubMed] [Google Scholar]
- 28.Pearlman AS, Ryan T, Picard MH, Douglas PS. Evolving trends in the use of echocardiography: a study of Medicare beneficiaries. J Am Coll Cardiol. 2007;49:2283–91. doi: 10.1016/j.jacc.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 29.American Heart Association. Get With The Guidelines - Heart Failure Fact Sheet. http://www.heart.org/idc/groups/heart-public/@private/@wcm/@hcm/@gwtg/documents/downloadable/ucm_310967.pdf. Accessed June 6, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


