Abstract
Objectives:
To determine the diagnostic accuracy of Focused Assessment with Sonography for Trauma (FAST) in blunt abdominal trauma caused by motor vehicle accidents at our Hospital in Dhahran city.
Methods:
This descriptive, observational study was conducted in the Radiology Department at King Fahad Military Medical Complex Dhahran, Saudi Arabia between September 2016 and September 2017. All adult patients (n=105) involved in motor vehicle accidents with blunt abdominal injury on presentation were retrospectively reviewed for FAST and CT scans for detection of free fluid. Focused assessment with sonography for trauma studies were conducted or supervised by senior registrar of general surgery (trauma team leader). Computed tomography findings were reviewed by 2 experienced radiologists. High and low-grade solid abdominal visceral (liver, spleen, kidney) injuries were identified on CT scans. Focused assessment with sonography for trauma and CT scan findings were identified as ‘positive’ and ‘negative’ for presence and absence of free fluid respectively. Outcomes of FAST were presented on a 2x2 contingency table.
Results:
Sensitivity of FAST in detecting intraperitoneal free fluid was calculated as 76.1% (95% confidence interval [CI], 64.14-85.69%), specificity 84.2% (95% CI, 68.75-93.98%) and accuracy 79% (95% CI, 70.01-86.38%). Focused assessment with sonography for trauma detected free fluid in most cases of high-grade solid visceral injuries. Nearly half of true-negative cases were having low grade visceral or other injuries.
Conclusion:
Focused assessment with sonography for trauma is an important tool in initial assessment of suspected blunt abdominal injury patients with high sensitivity and specificity. A negative FAST does not exclude low grade solid visceral or other injuries.
Motor vehicle accidents (MVAs) are a major health concern in the Kingdom of Saudi Arabia.1 Blunt abdominal trauma resulting from these accidents has contributed towards high morbidity and mortality.2,3 Rapid diagnosis and treatment are vital, leading to the development of focused assessment with sonography in trauma (FAST) in 1997, which reached worldwide importance through its incorporation into algorithms of Advanced Trauma Life Support (ATLS). It is used to identify presence of free fluid in the peritoneal cavity, which may represent hemoperitoneum, and enables for an early referral to further imaging and/ or surgery.4 In original FAST, detection of free fluid is made at upper right quadrant (perihepatic area, hepatorenal recess, or Morrison pouch), upper left quadrant (peri-splenic view), suprapubic (pouch of Douglas), and sub-xiphoid region (pericardial view).5,6 Recently, ‘extended FAST’ (eFAST) has been introduced to scan the lower chest area, revealing pneumothorax.7 Despite the apparent ease of use and accessibility, the accuracy of a FAST scan is found to be related and influenced by injury severity, patient built (obesity) and condition (hemodynamic stability), machine characteristics and resolution, and the level of experience and training of the operator. Unfortunately, FAST has the potential for limitations, misinterpretation, or misdiagnosis. Additionally, the detection of blunt mesenteric, bowel, diaphragmatic, or retroperitoneal injuries can be difficult and often missed by FAST.8
Computed tomography has become the gold standard for the investigation of blunt abdominal injuries.5,9 With the development of multi-detector CT scanners, imaging time has been significantly reduced, improving its diagnostic capabilities with high sensitivity and specificity of more than 95% in detection of intra-abdominal injuries and a high negative predictive value of nearly 100%.9 However, the need to transfer the patient to the scanner from the emergency department makes it unsuitable for hemodynamically unstable patients. Also, radiation risks and contrast related concerns can delay or limit CT evaluation in some patients. Therefore, in trauma patients, where time is critical, ultrasound is still useful as it is quick and can be performed at bedside. Several studies have shown its utility as a screening test in this setting; however, very few studies have correlated its diagnostic capability with underlying severity or grading of solid abdominal visceral injuries.10,11
The primary objective of this study is to determine the diagnostic accuracy of FAST in MVA patients in a trauma team setting. The secondary objective is to correlate FAST findings with different grades of solid abdominal visceral injuries identified on CT scan.
Methods
This descriptive observational study was conducted in the Radiology Department at King Fahad Military Medical Complex (KFMMC), Dhahran, Saudi Arabia over a period of one year, from September 2016 to September 2017.
Our Hospital is situated in the Northern area of Dhahran city in the Eastern Province of Saudi Arabia. It is a tertiary care military hospital, providing immediate care for all emergency trauma patients including motor vehicle accident victims. Trauma team activation in the emergency department ensures quick assessment of trauma patients by a trauma team lead by a trauma team leader (usually a senior registrar general surgery), followed by FAST and subsequently a CT study (when deemed necessary). Most CT scans are performed within 1-2 hours. The CT scan room is in close proximity to the emergency department and its service is available 24-hour a day.
All adult patients (aged more than 14 years) with a clinically-suspected blunt abdominal injury on presentation at Hospital Emergency within a few (1-3) hours of motor vehicle accident and who underwent FAST in the emergency room (ER) and subsequently a CT scan in the radiology department were retrospectively reviewed for the presence of free fluid. Children (aged less than 15 years), pregnant women, and patients with penetrating abdominal injuries were excluded. Only patients for whom FAST studies were performed within half an hour of presentation in the ER were selected. Only patients for whom FAST was conducted or supervised by the senior registrar trauma team were included. Patients with inconclusive or limited FAST studies were excluded. Patients for whom CT scans were performed within 2 hours of arrival in the ER were selected. Hemodynamically unstable patients who were directly shifted to the operating room (OR) after FAST without an intervening CT were excluded.
The research protocol was approved by the Hospital Research and Ethics Committee, and study was conducted in accordance with the Helsinki Declaration. Informed written consents for the CT scans were assessed and approached through patients’ files and records. All clinical and radiological data were kept strictly confidential. Findings of FAST were acquired from clinical notes (trauma management forms in patient files from medical records) and the Hospital Information System (HIS). Focused assessment with sonography in trauma scans were carried out in the ER by a portable ultrasound machine (GE LOGICe, General Electric, Asia) using a 3.75-MHz curvilinear probe. Radiologic (CT scan) data was retrieved from the Radiology Information System-Picture Archiving and Communication System (RIS-PACS). Computed tomography scans were requested by the trauma team leader and were performed on a 128-slice scanner (Siemens SOMATOM definition flash 2010, Munich Germany), acquiring a routine contrast-enhanced study (using non-ionic water-soluble contrast) of the abdomen and pelvis from the xiphisternum to the pubic symphysis. Indications for an abdominal CT scan, whether selected regional abdominal imaging or a pan-scanning (whole-body CT), were based on hospital-approved criteria (including clinical information about a high-risk mechanism of injury, and clinical condition of polytrauma patient like compromising vitals or conscious level), injury severity assessment and clinical judgement. Computed tomography scans were reviewed by 2 experienced (general) radiologists (having more than 7 years of experience in body imaging) who were blinded of the initial FAST results and radiology reports. Final documentation of findings was mutually agreed upon between the 2 radiologists. Although no major discrepancies arose; however, in the event of a disagreement a third senior radiologist was consulted in establishing a consensus.
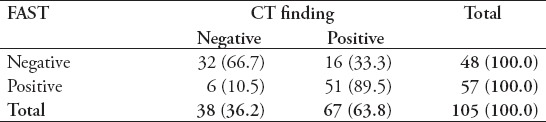
Findings of both FAST and CT scan were considered either ‘positive’ or ‘negative’ for the presence or absence of free fluid respectively. Computerized tomography scan was considered the gold standard for detection of free fluid. Outcomes of FAST were categorized as either true positive (TP; FAST correctly identified presence of free fluid), true negative (TN; FAST correctly identified absence of free fluid), false positive (FP; FAST incorrectly identified presence of free fluid), or false negative (FN; FAST incorrectly identified absence of free fluid). A 2x2 contingency table was used to represent these outcomes.
Clinical information recorded for all patients included their age, gender, seating (whether driver, front seat passenger, or back seat passenger), safety (whether seat-belted/ restrained or not), and mechanism of injury (roll-over, frontal collision, side-impact, or rear-impact).
The scale devised by the Organ Injury Scaling Committee of the American Association for the Surgery of Trauma was used to grade commonly-involved solid visceral injuries, namely those of the liver, spleen, or kidney.12,13 Abdominal injuries as seen on CT scans were categorized as high-grade solid visceral injuries (HGSVIs; grade III or more), low-grade solid visceral injuries (LGSVIs; grades I or II), other (retroperitoneal, extraperitoneal, bowel, or bladder injuries), only mild free fluid (OMFF), or no detectable visceral injuries (NDVI).
All data from selected patients, including those from FAST studies and CT scans, were collected and analyzed using Statistical Package for Social Sciences, Version 22 (Armonk, NY: IBM Corp.). Sensitivity, specificity, and diagnostic accuracy of FAST were determined. Injuries and outcomes were assessed to evaluate FAST utility.
Results
Of 105 motor vehicle accident patients, 87 were men, 18 were women, and the mean age was 32.3 years (range 15-56 years, standard deviation/ SD- 9). Most of the victims were drivers (n=71, 67%), and most were found unrestrained (n=95, 90.5%). The most common mechanism of injury was roll-over (n=77, 73.3%) followed by frontal collision (n=22, 21%), side-impact (n=4, 3.8%), and rear-impact (n=2, 1.9%). Outcomes of FAST results were presented on a 2x2 contingency table (Table 1). Sensitivity of FAST in detecting intraperitoneal free fluid were calculated as 76.1% (95% confidence interval [CI], 64.14- 85.69%), specificity 84.2% (95% CI, 68.75- 93.98%) and accuracy 79% (95% CI, 70.01- 86.38%).
Table 1.
Outcomes of focused assessment with sonography for trauma (FAST) for detection of free fluid.
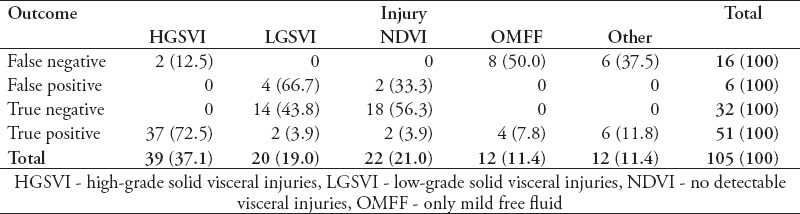
Focused assessment with sonography for trauma detected free fluid in most of high-grade solid abdominal visceral injuries (37 of 39 patients). However, nearly half the true negatives (14 of 32, 43%) were having low grade solid abdominal visceral injuries (Table 2). Unfortunately, FAST could not detect small amount of free fluid (8 of 12 patients) and those with other injuries (6 of 12).
Table 2.
Outcomes of focused assessment with sonography for trauma (FAST) and underlying abdominal injuries.
Discussion
The clinical application of FAST in emergency departments has been increasing for the initial screening of blunt abdominal trauma due to its non-invasiveness, non-ionizing imaging capabilities, easy availability and usage, and quick diagnostic yield in most of the patients.7 However, various studies have shown its limitations to detect severity and extent of injuries that are of particular concern in hemodynamically unstable patients usually requiring immediate surgery or intervention.5 Therefore, diagnosis of abdominal injuries now relies exclusively on a timely and adequately performed CT examinations.8 In our study, we found FAST to have fairly reasonable sensitivity (76%), specificity (84%), and accuracy (79%) in a trauma team setting. Tabassum et al found greater values (84%, 92%, and 88%, respectively) in 167 trauma patients over a 6-month period.14 We included only MVA patients and excluded hemodynamically unstable patients who underwent immediate surgery (laparotomy) without CT scans that might have contributed to a small sample size. Some studies in the literature have determined the diagnostic accuracy of FAST as performed by emergency and radiology residents. Ala et al,15 for example, reported greater sensitivity, but the operators were radiology residents. In our study, as being our standard practice, the most experienced and available person (senior registrar general surgery) of the trauma team performed the ultrasound.
Though a few studies have also observed a higher sensitivity of FAST by using either serial FAST or including inter-loop (bowel) free fluid in the abdomen (Rajabzadeh Kanafi et al16), we chose traditional FAST because it was practiced the same way in our emergency department and also our study was retrospective in nature. Adding a search for inter-loop fluid would have been time-consuming, difficult, and at times limited (because of the obscuration of bowel gases) and would be possible in a prospective study. Even delayed or serial FAST was not routinely performed in our study and was not considered practical in every patient. We noted that most of the false negatives (8 of 12) were found to have ‘only minimal free fluid’ on CT scans that shows limitation of ultrasound in the detection of minimal (less than 50 mL) pelvic free fluid in the supine position as documented earlier in the literature,5,7,10 We also found that many of the false negatives were related to ‘other injuries’ (retro- or extra-peritoneal bladder injuries involving pelvic fractures), that also show limitation of ultrasound in such regions due to obscuration of bowel gases and limited resolution. Very few studies have correlated the severity of solid organ injuries with the sensitivity of FAST. For example, Cheung et al10 observed an increased sensitivity with higher injury grade and also highlighted that staff training affected the outcome. Our study showed similar results with FAST detection of free fluid in most of the high grade visceral injuries. However, we observed that many (46%) of true negatives were having low grade visceral injuries. It should be noted that the underlying organ-specific severity might not correlate well with clinical severity. Also, severity grade is difficult to define for hollow-viscous (stomach and bowel), mesenteric, and retroperitoneal injuries. Therefore, we recommend a period of monitoring, serial FAST, or further investigation.
Other studies17-19 with different levels of operators contributed towards varied diagnostic accuracies of FAST. Our study, being based on trauma team setting under a trauma team leader, assumed FAST operators to be more experienced with same level of expertise utilizing same ultrasound machine, thereby minimizing any bias towards observation and results. However, regular practice and periodic assessments are suggested for the FAST operators to have good yield from FAST studies as highlighted.10
Focused assessment with sonography for trauma was performed for every trauma patient having suspicion of abdominal injury at presentation to our Hospital Emergency, and indication for a CT scan was not based solely upon clinical injury severity score (ISS), therefore, initial ISS was not documented in our study. However, most of patients who underwent pan-scanning (whole-body CT) were having an ISS score of 12 or above, and scores below these were usually directed to selected regional (abdominal) imaging. Correlation of initial ISS with FAST findings could have been interesting but it was not possible for every patient in our study. The time interval or lag between actual trauma and FAST, and also between FAST and the subsequent CT were not recorded, but these could have influenced the development and detection of free fluid (considering time delays and intervening resuscitation by fluids). It would be of interest to evaluate accuracy of FAST overcoming these limitations. Also, the incorporation of extended FAST (eFAST) would be of interest in future studies.
In conclusion, FAST is a rapid and reliable tool in a trauma team setting for initial assessment of suspected blunt abdominal injury in motor vehicle accident patients. It can readily detect free fluid in most of high grade solid visceral injuries. A negative FAST does not exclude low grade solid visceral or other (hollow viscus, retroperitoneal) injuries.
Footnotes
References
- 1.DeNicola E, Aburizaize OS, Siddique A, Khwaja H, Carpenter DO. Road Traffic Injury as a Major Public Health Issue in the Kingdom of Saudi Arabia: A Review. Front Public Health. 2016;4:215. doi: 10.3389/fpubh.2016.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mansuri FA, Al-Zalabani AH, Zalat MM, Qabshawi RI. Road safety and road traffic accidents in Saudi Arabia. A systematic review of existing evidence. Saudi Med J. 2015;36:418–424. doi: 10.15537/smj.2015.4.10003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Saudi Arabia (Factsheet) 2014. Available from: http://www.who.int/violence_injury_prevention/road_safety_status/2013/country_profiles/saudi_arabia.pdf .
- 4.Michalke JA. An overview of emergency ultrasound in the United States. World J Emerg Med. 2012;3:85–90. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheng AY, Dalziel P, Liteplo AS, Fagenholz P, Noble VE. Focused assessment with sonography in trauma and abdominal computed tomography utilization in adult trauma patients: Trends over the last decade. Emerg Med Int. 2013;2013:678380. doi: 10.1155/2013/678380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richards JR, McGahan JP. Focused Assessment with Sonography in Trauma (FAST) in 2017: What Radiologists Can Learn. Radiology. 2017;283:30–48. doi: 10.1148/radiol.2017160107. [DOI] [PubMed] [Google Scholar]
- 7.Montoya J, Stawicki SP, Evans DC, Bahner DP, Sparks S, Sharpe RP, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42:119–126. doi: 10.1007/s00068-015-0512-1. [DOI] [PubMed] [Google Scholar]
- 8.Fleming S, Bird R, Ratnasingham K, Sarker SJ, Walsh M, Patel B. Accuracy of FAST scan in blunt abdominal trauma in a major London trauma centre. Int J Surg. 2012;10:470–474. doi: 10.1016/j.ijsu.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Stengel D, Ottersbach C, Matthes G, Weigeldt M, Grundei S, Rademacher G, et al. Accuracy of single-pass whole-body computed tomography for detection of injuries in patients with major blunt trauma. CMAJ. 2012;184:869–876. doi: 10.1503/cmaj.111420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung KS, Wong HT, Leung LP, Tsang TC, Leung GK. Diagnostic accuracy of Focused Abdominal Sonography for Trauma in blunt abdominal trauma patients in a trauma centre of Hong Kong. Chin J Traumatol. 2012;15:273–278. [PubMed] [Google Scholar]
- 11.Soult MC, Weireter LJ, Britt RC, Collins JN, Novosel TJ, Reed SF, et al. Can routine trauma bay chest x-ray be bypassed with an extended focused assessment with sonography for trauma examination? Am Surg. 2015;81:336–340. [PubMed] [Google Scholar]
- 12.Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision) J Trauma. 1995;38:323–324. doi: 10.1097/00005373-199503000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Tinkoff G, Esposito TJ, Reed J, Kilgo P, Fildes J, Pasquale M, et al. American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg. 2008;207:646–655. doi: 10.1016/j.jamcollsurg.2008.06.342. [DOI] [PubMed] [Google Scholar]
- 14.Tabassum HM, Akhtar N, Mehmood A, Sultan A. Diagnostic accuracy of Surgeon-performed Focused Assessment Sonography in Trauma patients with blunt abdominal injury. JSZMC. 2016;7:1020–1023. [Google Scholar]
- 15.Ala AR, Pouraghaei M, Shams Vahdati S, Taghizadieh A, Moharamzadeh P, Arjmandi H. Diagnostic Accuracy of Focused Assessment with Sonography for Trauma in the Emergency Department. Trauma Mon. 2016;21:e21122. doi: 10.5812/traumamon.21122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajabzadeh Kanafi A, Giti M, Gharavi MH, Alizadeh A, Pourghorban R, Shekarchi B. Diagnostic accuracy of secondary ultrasound exam in blunt abdominal trauma. Indian J Raiol. 2014:11. doi: 10.5812/iranjradiol.21010. doi.org/10.5812/iranjradiol.21010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mushtaq S, Rauf Khan MU, Akbar A, Bodla MA. Diagnostic accuracy of Focused Abdominal Sonography in Trauma (FAST) in patients with blunt abdominal trauma. PJMHS. 2014;8:299–302. [Google Scholar]
- 18.Kumar S, Bansal VK, Muduly DK, Sharma P, Misra MC, Chumber S, et al. Accuracy of Focused Assessment with Sonography for Trauma (FAST) in Blunt Trauma Abdomen-A Prospective Study. Indian J Surg. 2015;77(S2 Suppl 2):393–397. doi: 10.1007/s12262-013-0851-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghafouri HB, Zare M, Bazrafshan A, Modirian E, Farahmand S, Abazarian N. Diagnostic accuracy of emergency-performed focused assessment with sonography for trauma (FAST) in blunt abdominal trauma. Electron Physician. 2016;8:2950–2953. doi: 10.19082/2950. [DOI] [PMC free article] [PubMed] [Google Scholar]


