Abstract
Objective
To determine the trends, prevalence and risk factors of overweight and obesity among Bangladeshi women of reproductive age from 1999 to 2014.
Design
We analysed nationally representative data from the 1999, 2004, 2007, 2011 and 2014 cross-sectional Bangladesh Demographic and Health Surveys.
Setting
Bangladesh.
Participants
Women aged 15–49 years.
Primary outcome
Overweight/obesity.
Results
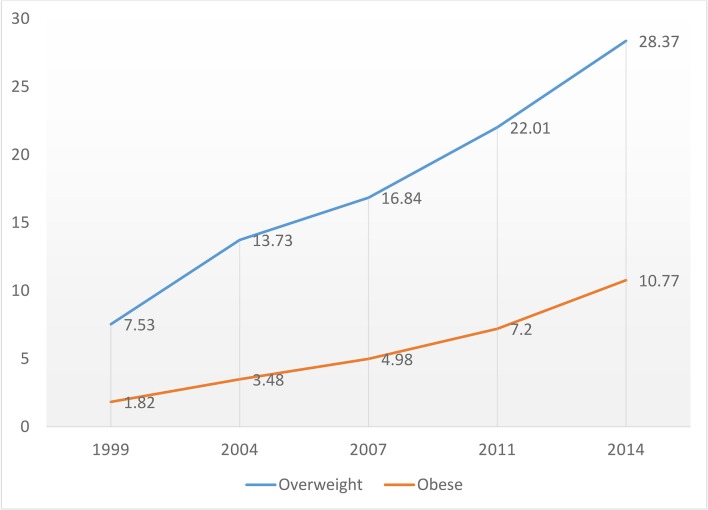
A total of 58 192 women were included in the analysis. The prevalence of overweight and obesity among women of reproductive age increased significantly from 7.53% (95% CI 6.83 to 8.29) and 1.82% (95% CI 1.48 to 2.24) in 1999 to 28.37% (95% CI 27.49 to 29.28) and 10.77% (95% CI 10.22 to 11.35) in 2014, respectively. Age, education, wealth index, watching television and contraceptive use were associated with overweight and obesity in both urban and rural areas.
Conclusions
Overweight and obesity prevalence increased significantly among Bangladeshi women of reproductive age between 1999 and 2014. Development of effective low-cost strategies to address the increasing burden of obesity should be a high priority.
Keywords: body mass index (BMI), overweight, obesity, trends, BDHS, Bangladesh
Strengths and limitations of this study.
To our knowledge, this is the first study in Bangladesh to compare longitudinal (15 years) trends in the prevalence and risk factors associated with overweight/obesity in women using nationally representative data.
The analysis accounted for a complex survey design (clustering, stratification, sample weights), which gives accurate estimates of the population.
Importantly, survey year was used as a predictor, which highlights incremental changes in overweight/obesity over time.
The surveys did not include responses on diet, fruit or vegetable intake, or physical activity, which are important predictors of overweight and obesity.
The surveys collected body mass index of women of reproductive age (15–49 years); therefore, the results may not be generalisable to women older than 49 years or to men.
Introduction
Obesity is a growing global public health concern.1 An estimated two billion adults were reported to have overweight or obesity in 2014, with a worldwide prevalence of 39%.1 2 Obesity increases the risk of many serious chronic health conditions, such as hypertension, pre-diabetes, type 2 diabetes, dyslipidaemia, cardiovascular diseases, certain cancers and metabolic syndrome.2–4 With a J-shaped (slight upward trend with a low body mass index (BMI) and steep increase with higher BMI relationship between BMI and mortality, obesity is associated with a high risk of mortality.5
While the impact of the overweight and obesity epidemic in developed countries has been highlighted,6 recent studies demonstrate that the prevalence of obesity has increased significantly in many low-income and middle-income countries.7 This trend of increasing overweight and obesity will likely continue to rise in low-income and middle-income countries.8 Bangladesh, a low-income country in South East Asia, has also observed an increasing prevalence of overweight and obesity. Like many low-income and middle-income countries, Bangladesh has experienced demographic and nutritional changes among its population, such as changing lifestyle (eg, high-calorie food intake, sedentary lifestyle) and urbanisation. The rate of serious chronic health conditions in Bangladesh has increased steadily, and death attributable to chronic conditions climbed from 8% in 1986 to 68% in 2006.6 Traditionally, infectious diseases9 and undernutrition10 were major public health problems in the country, and little attention was focused on overweight and obesity by public health officials.
Data on the overweight and obesity trend in Bangladesh are sparse. Few studies that reported the prevalence of obesity were cross-sectional, and data were limited to 1 year or less11 and included only specific participants (eg, patients with diabetes, schoolchildren and so on).12 Further, sociodemographic trends associated with the rising incidence of overweight and obesity in Bangladesh have not been well studied. Further, the scale to determine BMI categories varied widely in prior studies, and most used scales other than the WHO-recommended Asian standard BMI classification.
Women of reproductive age have higher rates of overweight and obesity and are more adversely affected by obesity-related complications than men.13 This gender difference is mainly due to general weight gain during childbearing years, gestational weight gain and/or weight retention, adverse lifestyle, or risk factors associated with pregnancy and the postpartum period.14 Maternal obesity increases the risk of numerous complications including pregnancy, labour and birth for both the mother and the child, diabetes and hypertensive disorders etc.13 15 Compared with normal weight, maternal overweight is associated with a higher risk of caesarean delivery and a higher incidence of anaesthetic and postoperative complications.16 17 Low Apgar scores, macrosomia and neural tube defects are also more frequent in infants of obese mothers compared with infants of normal-weight mothers.16 17
Understanding the obesity trend and identifying modifiable sociodemographic factors responsible for overweight and obesity among this high-risk group may help inform the development of feasible public health interventions to reduce the burden of obesity and associated adverse health outcomes. We used nationally representative data from the Bangladesh Demographic and Health Survey (BDHS) to estimate the trends in overweight and obesity and to identify sociodemographic factors associated with overweight and obesity among women of reproductive age in Bangladesh between 1999 and 2014.
Methods
Data sources
We analysed publicly available data from the 1999, 2004, 2007, 2011 and 2014 BDHS. The BDHS is a nationally representative cross-sectional survey of the non-institutionalised Bangladeshi population. It was developed over decades, progressively adopting standardised demographic and health survey items designed to provide data for monitoring population health in Bangladesh. The Bangladesh Ministry of Health and Family Welfare and the National Institute of Population Research and Training (NIPORT) have been conducting the survey at 3-year intervals since 1993.18
Sampling design and sample size
All BDHS surveys use a two-stage stratified sampling procedure. In the first stage, enumeration areas are selected with a probability proportional to population size. Population size is based on the master sampling frame of the 2001 and 2011 population and housing census prepared by the Bangladesh Bureau of Statistics.19 In the second stage, systematic household sampling is conducted from each sampling unit to provide a statistically reliable estimate of key demographic and health-related variables. Details on the BDHS methods are available elsewhere.18 The surveys include 10 544, 11 440, 10 996, 17 842 and 17 863 women, from 1999, 2004, 2007, 2011 and 2014, respectively. We excluded participants below 15 years of age, participants with missing values for measured height and weight, and women who were pregnant at the time of the survey. After applying the exclusion criteria, the total sample consisted of 58 192 women.
Outcome
The primary outcome variable of this study was BMI, calculated as weight in kilograms divided by height in metres squared. In the analysis, we used BMI classifications recommended by the WHO for the Asian population: normal weight (18.5 to <23.0), moderate risk or overweight (23.0 to <27.5), and high risk or obese (≥27.5).20 We also conducted analyses using the WHO and National Institutes of Health BMI classification for the general population: underweight (<18.5), normal weight (18.5 to <25.0), overweight (25.0 to <30.0) and obese (≥30.0).21
Covariates
We choose covariates associated with overweight and obesity based on literature review.11 22 Sociodemographic characteristics included age (15–24, 25–34, 35–44 and 45+), marital status (married, not married), education (no education, primary, secondary and higher), place of residence (rural, urban), geographical region (south (Barishal), south-east (Chittagong), central (Dhaka), west (Khulna), mid-western (Rajshahi), north-west (Rangpur) and east (Sylhet)), wealth index (poorest, poorer, middle, rich and richest), employment status (yes, no), watching television (TV) at least once a week (yes or no), number of living children (0, 1–2, 3–4 and ≥5), number of household members (1–2, 3–4 and ≥5), contraceptive use (not using any method, using pill and other methods) and survey year. Survey year was treated as a categorical variable. The BDHS provides a household wealth index estimated using multiple household and asset variables. The principal component analysis was used for estimation. The household-level variables include having electricity, type and source of drinking water, access to a sanitation facility, availability of cooking fuel, main roof material, main wall material and floor material. The asset variables are having wardrobe, table, chair or bench, watch or clock, radio, TV, bicycle, motorcycle, sewing machine, telephone, and land ownership.
Statistical analysis
Descriptive statistics (eg, mean, frequencies) were calculated to define the characteristics of survey participants. All five surveys were appended given that a similar survey protocol in terms of design, scope, coverage, sampling, data collection, coding and weighting was used across surveys. This approach simplified the reporting estimates and improved the statistical power of the analyses. The distributions of BMI at each survey year were compared between rural and urban populations using kernel density plots. The BMI trend over the 15-year period was assessed by linear regression with survey year as the primary predictor. The nature, strength and direction of the association between women’s sociodemographic characteristics and BMI categories were assessed using multinomial logistic regression models with adjusted risk ratios (ARR) and 95% CI for urban and rural study participants separately. All analyses were performed using the statistical software Stata/MP V.13.0. We used the ‘svy’ procedures to adjust for the sample stratification and clustering effect in all further analyses at the time of each survey. We used forward, backward and stepwise model selection procedures to select the best predicting model. Variance inflation factor was calculated to check the collinearity of the predictor variables and the outcome for both urban and rural sample (online supplementary table S1).
bmjopen-2017-018468supp001.pdf (261KB, pdf)
Patient and public involvement
The BDHS questionnaires were based on the MEASURE DHS model questionnaires. These model questionnaires were adapted for use in Bangladesh during a series of meetings with a technical working group (TWG) that consisted of representatives from NIPORT, Mitra and Associates, International Centre for Diarrhoeal Disease Research, Bangladesh, United States Agency for International Development/Bangladesh, and MEASURE DHS. Patients were not directly involved in the study. However, the TWG involved representatives from government and non-governmental organisations, the Ministry of Health and Family Welfare, and donor organisations. All of these groups were involved in the study design and questionnaire development. The results will be used by the health researchers and policy makers of the country.
Results
Sociodemographic characteristics
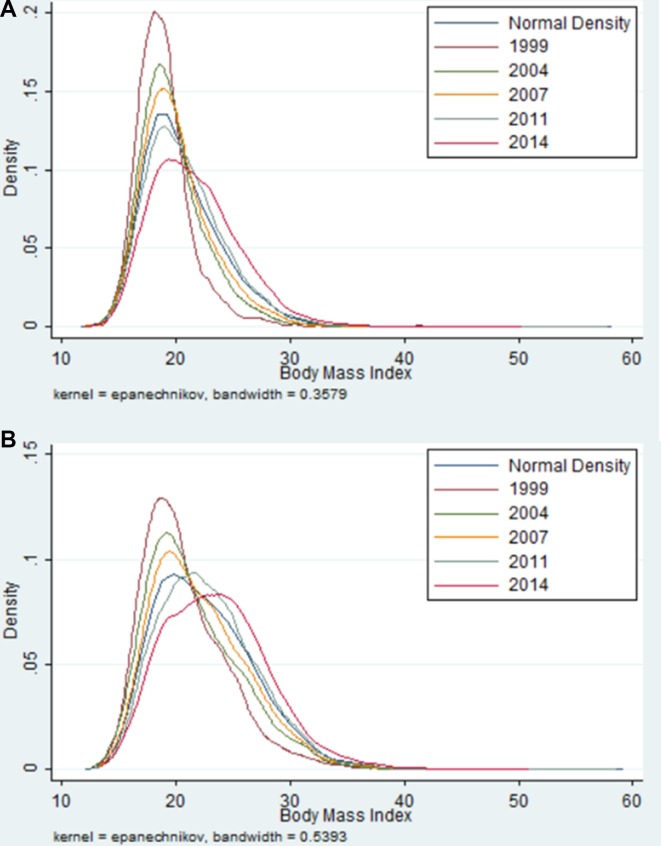
A total of 68 685 women participated across the five surveys. BMI data were available for 62 059 study participants, and the survey response rates ranged between 96.9% and 98.6% from 1999 to 2014 (online supplementary table S2). We examined the changes in the shape of BMI distributions among Bangladeshi women of reproductive age in 1999, 2004, 2007, 2011 and 2014 using the kernel density plot by urban and rural areas (figure 1). Both urban and rural BMI distribution curves appear to be skewed to the right over the 15-year period, indicating a gradual increase in BMI. Table 1 shows the socioeconomic and demographic characteristics of study participants across survey years. Over time, the mean age of study participants increased from 25 (±6.63) to 32 (±9.12) years. There was a significant reduction in the proportion of women with no education from 45% to 26% (p<0.001) between 1999 and 2014. Similarly, the proportion of women with higher education increased almost twofold (from 4.19% to 8.32%). The frequency of watching TV increased approximately 1.6 times and the proportion of working women almost doubled (18.81% vs 34.15%) over the study period. There was a significant change in the family structure during the study period. Five or more living children per women dropped from 12.63% to 8.11%.
Figure 1.
Kernel density plot of the distribution of body mass index of women of reproductive age in 1999, 2004, 2007, 2011 and 2014. A, Rural; B, Urban.
Table 1.
Sociodemographic characteristics of the study participants by survey year, BDHS 1999–2014
| Variables | 1999 | 2004 | 2007 | 2011 | 2014 | P values |
| Age, mean (SD) | 25.88 (6.63) | 30.56 (9.36) | 30.94 (9.3) | 31.23 (9.22) | 31.37 (9.12) | <0.001 |
| Age group, n (%) | <0.001 | |||||
| 15–24 | 2148 (47.05) | 3303 (31.82) | 2996 (30.29) | 4557 (28.72) | 4433 (27.04) | |
| 25–34 | 2007 (41.52) | 3533 (33.77) | 3344 (33.13) | 5603 (34.19) | 5969 (36.44) | |
| 35–44 | 486 (10.61) | 2598 (24.39) | 2747 (26.69) | 4321 (26.2) | 4435 (26.05) | |
| 45+ | 38 (0.81) | 1055 (10.02) | 1040 (9.89) | 1792 (10.89) | 1787 (10.47) | |
| Educational level, n (%) | <0.001 | |||||
| No education | 2002 (44.62) | 4158 (42.44) | 3326 (34.85) | 4386 (28.59) | 4039 (25.68) | |
| Primary | 1364 (29.14) | 3070 (29.07) | 3014 (29.67) | 4857 (30.04) | 4875 (29.24) | |
| Secondary | 1072 (22.05) | 2629 (23.52) | 2983 (29.52) | 5731 (34.3) | 6153 (36.76) | |
| Higher | 241 (4.19) | 632 (4.97) | 801 (5.96) | 1299 (7.07) | 1557 (8.32) | |
| Place of residence, n (%) | <0.001 | |||||
| Urban | 1275 (17.76) | 3593 (22.58) | 3858 (22.81) | 5709 (26.1) | 5764 (28.41) | |
| Rural | 3404 (82.24) | 6896 (77.42) | 6269 (77.19) | 11 000 (73.9) | 11 000 (71.59) | |
| Geographical region, n (%) | <0.001 | |||||
| Barishal | 434 (6.48) | 1252 (6.33) | 1327 (6.01) | 1819 (5.45) | 1982 (6.19) | |
| Chittagong | 937 (20.08) | 1869 (17.56) | 1775 (18.23) | 2616 (18) | 2639 (18.29) | |
| Dhaka | 1123 (31.05) | 2376 (31.27) | 2178 (31.5) | 2795 (32.18) | 2893 (34.96) | |
| Khulna | 760 (11.42) | 1583 (12.32) | 1589 (12.77) | 2488 (12.4) | 2460 (10.51) | |
| Rajshahi | 889 (24.48) | 2374 (26.35) | 1933 (25.31) | 4703 (26.73) | 4769 (23.56) | |
| Sylhet | 536 (6.49) | 1035 (6.17) | 1325 (6.18) | 1852 (5.25) | 1881 (6.49) | |
| Marital status, n (%) | <0.001 | |||||
| Not married | 130 (2.71) | 859 (7.93) | 822 (7.7) | 1091 (6.6) | 1014 (5.95) | |
| Married | 4549 (97.29) | 9630 (92.07) | 9305 (92.3) | 15 000 (93.4) | 16 000 (94.05) | |
| Urban | ||||||
| BMI, kg/m2 | <0.001 | |||||
| Mean (SD) | 20.78 (4.51) | 21.52 (5.06) | 22.24 (5.44) | 23 (4.87) | 23.7 (5.06) | |
| BMI categories, n (%) | <0.001 | |||||
| Underweight | 385 (29.74) | 903 (24.84) | 787 (19.54) | 879 (13.46) | 738 (12.21) | |
| Normal weight | 585 (45.65) | 1573 (44.47) | 1629 (41.73) | 2298 (41.4) | 1996 (34.73) | |
| Overweight | 237 (19.09) | 801 (21.87) | 1010 (26.88) | 1729 (30.62) | 1971 (33.74) | |
| Obese | 68 (5.53) | 316 (8.81) | 432 (11.85) | 803 (14.52) | 1059 (19.32) | |
| Overweight or obese | 305 (24.61) | 1117 (30.68) | 1442 (38.73) | 2532 (45.14) | 3030 (53.06) | |
| Rural | ||||||
| BMI, kg/m2 | <0.001 | |||||
| Mean (SD) | 18.97 (2.42) | 19.76 (2.72) | 20.18 (2.83) | 20.82 (3.29) | 21.71 (3.62) | |
| BMI categories, n (%) | <0.001 | |||||
| Underweight | 1636 (48.19) | 2581 (36.9) | 2107 (32.45) | 2940 (27.83) | 2353 (21.09) | |
| Normal weight | 1560 (45.76) | 3422 (49.82) | 3135 (50.72) | 5138 (48.59) | 4926 (45.3) | |
| Overweight | 174 (5.03) | 762 (11.36) | 851 (13.88) | 1997 (18.97) | 2780 (26.24) | |
| Obese | 34 (1.02) | 131 (1.92) | 176 (2.96) | 489 (4.62) | 801 (7.38) | |
| Overweight or obese | 208 (6.05) | 893 (13.28) | 1027 (16.83) | 2486 (23.58) | 3581 (33.62) | |
| Wealth index, n (%) | 0.1665 | |||||
| Poorest | NA | 1865 (19.85) | 1636 (19.19) | 2811 (18.29) | 2999 (18.55) | |
| Poorer | NA | 1880 (19.92) | 1822 (19.35) | 2995 (19.47) | 3102 (18.95) | |
| Middle | NA | 1960 (19.77) | 1910 (19.72) | 3129 (20.07) | 3382 (20.04) | |
| Richer | NA | 2098 (20.38) | 2043 (20.85) | 3472 (20.83) | 3534 (21.21) | |
| Richest | NA | 2686 (20.08) | 2716 (20.88) | 3866 (21.34) | 3607 (21.24) | |
| Watch television (once a week), n (%) | <0.001 | |||||
| No | 2946 (66.99) | 5459 (54.5) | 5138 (53.2) | 8149 (51.61) | 7997 (48.83) | |
| Yes | 1732 (33.01) | 5027 (45.5) | 4985 (46.8) | 8120 (48.39) | 8626 (51.17) | |
| Currently working, n (%) | ||||||
| No | 3839 (81.19) | 8098 (76.85) | 7068 (67.12) | 14 000 (86.62) | 11 000 (65.85) | |
| Yes | 840 (18.81) | 2390 (23.15) | 3055 (32.88) | 2216 (13.38) | 5398 (34.15) | |
| Number of living children, n (%) | <0.001 | |||||
| 0 | 67 (1.46) | 1017 (9.39) | 930 (8.78) | 1371 (8.53) | 1385 (7.96) | |
| 1–2 | 2669 (56.66) | 4590 (43.15) | 4769 (47.11) | 8236 (50.09) | 8857 (53.48) | |
| 3–4 | 1358 (29.25) | 3312 (32.45) | 3111 (31.61) | 5102 (31.64) | 5013 (30.45) | |
| >5 | 585 (12.63) | 1570 (15.01) | 1317 (12.5) | 1564 (9.74) | 1369 (8.11) | |
| Number of household member, n (%) | <0.001 | |||||
| 1–2 | 46 (1.03) | 382 (3.71) | 405 (4.11) | 694 (4.46) | 834 (5.27) | |
| 3–4 | 1208 (26.22) | 3079 (30.31) | 3171 (32.63) | 5633 (34.65) | 6224 (37.36) | |
| >5 | 3425 (72.75) | 7028 (65.99) | 6551 (63.25) | 9946 (60.89) | 9566 (57.36) | |
| Contraceptive use, n (%) | <0.001 | |||||
| Not using | 2060 (44.71) | 4422 (41.76) | 4555 (44.02) | 6260 (38.76) | 6227 (37.19) | |
| Pills | 1352 (2.904) | 2641 (2.606) | 2734 (2.835) | 4385 (2.725) | 4476 (2.717) | |
| Other | 1267 (26.25) | 3426 (32.18) | 2838 (27.63) | 5628 (33.99) | 5921 (35.64) | |
| Husband’s education, n (%) | <0.001 | |||||
| No education | 1851 (42.48) | 3818 (39.16) | 3342 (35.92) | 4833 (31.73) | 4764 (29.5) | |
| Primary | 1102 (24.24) | 2629 (25.34) | 2610 (25.78) | 4362 (26.89) | 4503 (27.1) | |
| Secondary | 1098 (23.05) | 2691 (24.43) | 2660 (25.94) | 4680 (27.93) | 4884 (29.71) | |
| Higher | 549 (10.23) | 1342 (11.07) | 1501 (12.37) | 2390 (13.46) | 2471 (13.69) | |
BDHS, Bangladesh Demographic and Health Survey; BMI, body mass index; NA, not available.
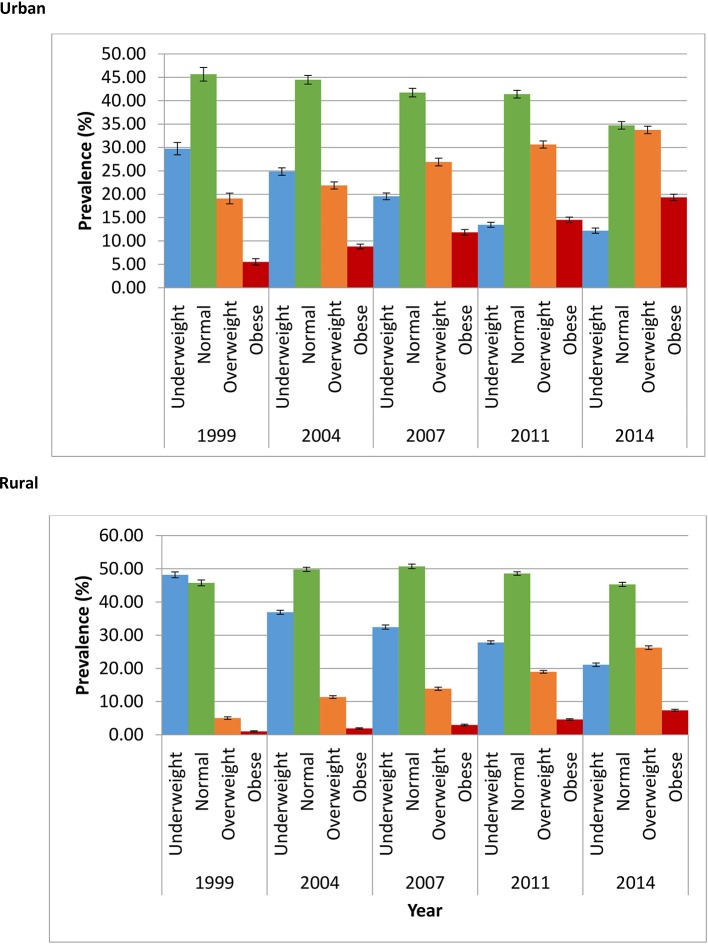
Trends in overweight and obesity
We present the trends in overweight and obesity prevalence over the study period in figure 2. The overall prevalence of overweight increased almost fourfold (from 7.53% to 28.37%) and the prevalence of obesity increased almost fivefold (from 1.82% to 10.77%)%) over the 15-year period. Figure 3 demonstrates the prevalence of BMI categories by place of residence. There was a 1.76-fold and 3.5-fold increase and 5.12-fold and 7.23-fold increase in the prevalence of overweight and obesity in urban and rural areas, respectively (figure 3).
Figure 2.
Prevalence of overweight and obesity by survey year, Bangladesh Demographic and Health Survey 1999–2014.
Figure 3.
Prevalence of underweight, normal, overweight and obesity by year and place of residence, Bangladesh Demographic and Health Survey 1999–2014.
Prevalence of overweight and obesity
Online supplementary table S3 shows the overall prevalence of BMI categories by age groups and place of residence. The prevalence of individuals with overweight and obesity increased across the five survey years for women residing in both urban and rural areas across all age groups. The prevalence of underweight and normal weight decreased in both rural and urban areas. Based on the Asian BMI cut-offs, the overall prevalence of overweight in rural and urban women increased from 19.08% (95% CI 16.95 to 21.42) and 5.02% (95% CI 4.33 to 5.83) in 1999 to 33.74% (95% CI 32.19 to 35.32) and 26.24% (95% CI 25.17 to 27.34) in 2014, respectively. Similarly, the prevalence of obesity increased from 5.52% (95% CI 4.32 to 7.04) and 1.02% (95% CI 0.72 to 1.44) in 1999 to 19.32% (95% CI 18.01 to 20.69) and 7.37% (95% CI 6.82 to 7.97) in 2014 in urban and rural areas, respectively. The steepest increase of overweight was observed among women aged 35–44 years, from 15.79% and 6.10% in 1999 to 37.62% and 30.09% in 2014 in urban and rural areas, respectively. The prevalence of obesity increased almost threefold among women aged 25–34 years, from 7.47% and 1.37% in 1999 to 21.23% and 8.28% in 2014 in urban and rural areas, respectively. The prevalence estimates of BMI for urban and rural women differed when the international BMI cut-offs were used (online supplementary table S4). A sharp decline was also observed in underweight women (urban: from 29.73% to 12.2%; rural: from 48.18% to 21.08%) from 1999 to 2014 applying the international BMI standard. Across urban and rural and all survey years, the prevalence of overweight and obesity using the Asian-specific guidelines was 2.10–2.5 times higher than the prevalence estimates based on the international guidelines (online supplementary figures S1 and S2).
Risk factors of overweight or obesity
The adjusted association of overweight and obesity is presented in table 2. Overall, the risk factors of overweight and obesity differed between urban and rural women. Increasing age was associated with higher overweight and obesity risk among both rural and urban residents, although the association was stronger among urban residents. The highest overweight (ARR: 3.14, 95% CI 2.74 to 3.59) and obesity (ARR: 6.77, 95% CI 5.56 to 8.24) risk were for the urban women in the age group 35–44 years compared with women 15–24 years of age. The risk of overweight and obesity was high for urban women with higher educational level, married women and women whose husband had a higher educational level. In terms of wealth index, there was a significant risk variation between urban and rural study participants. The middle, richer and richest rural women had 1.63, 2.55 and 5.85 higher odds of being overweight compared with women in the lowest wealth index group. The odds of being obese were 2.30, 3.94 and 7.88 times higher for middle, richer and richest rural women, respectively. Married women in urban areas had a 27% (ARR: 1.27, 95% CI 1.04 to 1.56) higher risk of being overweight and 41% (ARR: 1.41, 95% CI 1.07 to 1.86) higher risk of being obese compared with unmarried women. Marital status was not significantly associated with overweight or obesity in rural women. Watching TV at least once a week was an independent risk factor for overweight and obesity among both urban and rural women, and the risk was stronger among urban women. In the adjusted model, women who watched TV at least once a week had 28% (ARR: 1.28, 95% CI 1.13 to 1.45) and 72% (ARR: 1.72, 95% CI 1.43 to 2.07) higher risk of being overweight and obese, respectively, compared with women who do not watch TV at least once a week.
Table 2.
Association of overweight and obesity with sociodemographic characteristics by place of residence, BDHS 1999–2014
| Urban | Rural | |||||||
| Overweight vs healthy | Obese vs healthy | Overweight vs healthy | Obese vs healthy | |||||
| RR (95% CI) | P values | RR (95% CI) | P values | RR (95% CI) | P values | RR (95% CI) | P values | |
| Age group | ||||||||
| 15–24 | Ref | Ref | Ref | Ref | ||||
| 25–34 | 2.39 (2.11 to 2.70) | 0.000 | 4.04 (3.34 to 4.87) | 0.00 | 2.09 (1.9 to 2.31) | 0.000 | 3.23 (2.67 to 3.91) | 0.000 |
| 35–44 | 3.14 (2.74 to 3.59) | 0.000 | 6.77 (5.56 to 8.24) | 0.00 | 2.45 (2.2 to 2.73) | 0.000 | 4.06 (3.30 to 4.99) | 0.000 |
| 45+ | 2.59 (2.15 to 3.12) | 0.000 | 6.22 (4.88 to 7.92) | 0.00 | 2.47 (2.14 to 2.86) | 0.000 | 3.69 (2.87 to 4.74) | 0.000 |
| Educational level | ||||||||
| No education | Ref | Ref | Ref | Ref | ||||
| Primary | 1.22 (1.06 to 1.41) | 0.006 | 1.25 (1.01 to 1.54) | 0.03 | 1.11 (1.01 to 1.23) | 0.023 | 1.22 (1.02 to 1.46) | 0.026 |
| Secondary | 1.41 (1.20 to 1.65) | 0.000 | 1.61 (1.29 to 2.02) | 0.00 | 1.15 (1.03 to 1.30) | 0.014 | 1.27 (1.04 to 1.55) | 0.019 |
| Higher | 1.61 (1.30 to 1.99) | 0.000 | 1.42 (1.07 to 1.90) | 0.02 | 1.12 (0.92 to 1.36) | 0.238 | 0.92 (0.67 to 1.27) | 0.649 |
| Marital status | ||||||||
| Not married | Ref | |||||||
| Married | 1.27 (1.04 to 1.56) | 0.018 | 1.41 (1.07 to 1.86) | 0.01 | NA | NA | NA | NA |
| Wealth index | ||||||||
| Poorest | Ref | Ref | Ref | Ref | ||||
| Poorer | 1.15 (0.87 to 1.52) | 0.317 | 0.99 (0.58 to 1.70) | 0.99 | 1.32 (1.17 to 1.49) | 0.000 | 1.45 (1.11 to 1.90) | 0.006 |
| Middle | 1.65 (1.29 to 2.11) | 0.000 | 1.63 (1.02 to 2.61) | 0.04 | 1.65 (1.46 to 1.87) | 0.000 | 2.30 (1.78 to 2.97) | 0.000 |
| Richer | 1.88 (1.49 to 2.37) | 0.000 | 2.55 (1.64 to 3.96) | 0.00 | 2.46 (2.16 to 2.8) | 0.000 | 3.94 (3.05 to 5.10) | 0.000 |
| Richest | 2.83 (2.24 to 3.57) | 0.000 | 5.58 (3.6 to 8.63) | 0.00 | 3.38 (2.9 to 3.94) | 0.000 | 7.88 (5.93 to 10.46) | 0.000 |
| Watch television (once a week) | ||||||||
| No | Ref | Ref | Ref | Ref | ||||
| Yes | 1.28 (1.13 to 1.45) | 0.000 | 1.72 (1.43 to 2.07) | 0.00 | 1.25 (1.15 to 1.35) | 0.000 | 1.4 (1.22 to 1.62) | 0.000 |
| Currently working | ||||||||
| No | Ref | Ref | ||||||
| Yes | 0.79 (0.71 to 0.89) | 0.000 | 0.54 (0.46 to 0.64) | 0.00 | NA | NA | NA | NA |
| Number of household member | ||||||||
| 1–2 | Ref | Ref | ||||||
| 3–4 | NA | NA | NA | NA | 0.86 (0.72 to 1.02) | 0.093 | 0.86 (0.64 to 1.16) | 0.353 |
| >5 | NA | NA | NA | NA | 0.71 (0.60 to 0.84) | 0.000 | 0.61 (0.45 to 0.81) | 0.001 |
| Contraceptive use | ||||||||
| Not using | Ref | Ref | Ref | |||||
| Pills | 0.96 (0.85 to 1.09) | 0.605 | 0.79 (0.67 to 0.94) | 0.01 | 1.06 (0.98 to 1.16) | 0.130 | 0.83 (0.70 to 0.97) | 0.022 |
| Other | 1.07 (0.95 to 1.20) | 0.237 | 1.04 (0.9 to 1.20) | 0.55 | 1.08 (0.99 to 1.18) | 0.053 | 0.94 (0.82 to 1.09) | 0.459 |
| Husband’s education | ||||||||
| No education | Ref | Ref | Ref | Ref | ||||
| Primary | 1.11 (0.95 to 1.29) | 0.164 | 1.12 (0.89 to 1.4) | 0.32 | 1.07 (0.97 to 1.18) | 0.132 | 1.22 (1.01 to 1.47) | 0.037 |
| Secondary | 1.18 (1.01 to 1.37) | 0.031 | 1.32 (1.05 to 1.65) | 0.02 | 1.2 (1.08 to 1.34) | 0.001 | 1.51 (1.25 to 1.82) | 0.000 |
| Higher | 1.55 (1.28 to 1.88) | 0.000 | 1.94 (1.49 to 2.52) | 0.00 | 1.46 (1.25 to 1.69) | 0.000 | 1.98 (1.55 to 2.53) | 0.000 |
| Survey year | ||||||||
| 2004 | Ref | Ref | Ref | Ref | ||||
| 2007 | 1.23 (1.07 to 1.42) | 0.003 | 1.35 (1.11 to 1.64) | 0.00 | 1.19 (1.06 to 1.35) | 0.004 | 1.49 (1.15 to 1.93) | 0.002 |
| 2011 | 1.43 (1.26 to 1.63) | 0.000 | 1.68 (1.40 to 2.00) | 0.00 | 1.71 (1.54 to 1.90) | 0.000 | 2.50 (2.00 to 3.13) | 0.000 |
| 2014 | 2.07 (1.81 to 2.37) | 0.000 | 3.23 (2.71 to 3.86) | 0.00 | 2.60 (2.33 to 2.89) | 0.000 | 4.47 (3.59 to 5.57) | 0.000 |
BDHS, Bangladesh Demographic and Health Survey; NA, not available; ref, reference; RR, risk ratio.
Women’s employment status was only associated with overweight or obesity for urban residents. Working urban women had a lower probability of being overweight (ARR: 0.79, 95% CI 0.71 to 0.89) or obese (ARR: 0.54, 95% CI 0.46 to 0.64) compared with those who do not work. Women in rural areas with five or more household members had a lower probability of being overweight (ARR: 0.71, 95% CI 0.60 to 0.84) and obese (ARR: 0.61, 95% CI 0.45 to 0.81) compared with women with two or fewer household members. Compared with the 2004 survey, the risk of being overweight significantly increased with each subsequent survey period in urban and rural areas. For the increase of one survey period, the risk of overweight and obesity was much stronger in rural areas compared with urban areas after adjusting for all predictors. For example, in the most recent 2014 survey, the odds of being overweight were 2.60 (95% CI 2.33 to 2.89) and 2.07 (95% CI 1.18 to 2.37) times higher among rural and urban women, respectively, as compared with the 2004 survey year. Similarly, the odds of being obese were 4.47 (95% CI 3.59 to 5.57) and 3.23 (95% CI 2.71 to 3.86) times higher for rural and urban women, respectively, as of the 2004 survey year.
Discussion
We identified an increasing trend of overweight and obesity among Bangladeshi women of reproductive age, with a fivefold increase of obesity between 1999 and 2014. Overweight and obesity put women at increased risk of many adverse health outcomes, including cardiovascular disease, diabetes, kidney disease and obesity-related cancers.3 4 23 These women are also more likely to develop pregnancy complications, such as gestational diabetes, hypertensive disorders of pregnancy, caesarean section delivery and adverse fetal outcome.13 15 Although Bangladesh has made substantial progress in reducing death from pregnancy-related complications in the last several decades, pregnancy-associated risks remain high. The increasing trend of obesity among women of reproductive age may create new challenges.24 25
Our findings of an increasing longitudinal prevalence of overweight and obesity are consistent with findings from neighbouring countries, current trends in most low-income and middle-income countries, as well as across the globe.2 This trend could be explained by substantial lifestyle changes, including changes in eating habits with more energy-dense food intake and sedentary lifestyles with reduced physical activity patterns.26 These changes have been observed in Bangladesh with rapid economic growth, urbanisation, modernisation and globalisation of the food market.27
We found the highest increase in the prevalence of overweight and obesity among women aged 35–44 years. Studies from other low-income countries showed that older women (aged 45–49) are at greatest risk of overweight and obesity.28 Because we did not include women older than 49 years of age, the actual number of obese women might be much higher in Bangladesh. Our study also showed that the increasing rate of overweight and obesity was more marked in rural areas than urban areas, whereas the rate of decline of undernutrition was much higher in urban areas. This disparity may be the result of multiple factors. Our study also showed that the increasing overweight and obesity rates were more marked in rural areas than urban areas, and the decline of the undernutrition rate was much higher in urban areas. This disparity between rural and urban areas may be the result of multiple factors, such as a reduction in poverty and increased per capita income. Bangladesh’s per capita income has been growing around 5% per year in the 2000s. This increased per capita income at the household level has improved nutritional status. However, this growth was not equal among the rich and the poor. The upward trend of income inequality also exists at all levels: national, rural and urban. The Gini coefficient, a commonly used measure of income inequality, shows an increase from 0.432 in 1995 to 0.458 in 2010. Moreover, urban inequality has increased faster than rural inequality, likely explaining the slow reduction of the number of underweight women in urban areas.
Our data showed that over the last 15 years, the number of educated and employed urban women increased significantly in Bangladesh. Because educational status and employment are both negatively associated with obesity, this might explain the variation in overweight and obesity between urban and rural women.29
We determined that educational status including the husband’s educational status, marital status, wealth index, self-reported hours of watching TV and employment status were significantly associated with overweight and obesity. Our study showed that compared with women who have no education, women with higher educational status were at an increased risk of overweight and obesity. Highly educated women are more likely to have a sedentary job requiring less physical activity and hence have an increased risk of weight gain. Studies from other low-income and middle-income countries also demonstrate a positive association between the level of education and obesity22 30; however, a negative association between the two variables has been observed primarily in developed countries.29 Our findings that wealthier women are more likely to be overweight or obese are consistent with studies done in other low-income and middle-income countries.22 31 This is likely due to the fact that increasing wealth in lower income countries results in greater access to food, an escape from physical labour and a higher risk of obesity.
We found that watching TV was an independent predictor of overweight and obesity. TV viewing has been used as a proxy for sitting time, and studies that follow participants over long periods of time have consistently found that people who spend more time watching TV are more likely to gain weight.32 Unemployed Bangladeshi women spend a significant amount of time watching TV as a leisure activity. Moreover, with the economic growth increasing access to TV suggests that TV viewing may further increase, which may further contribute to obesity of this group.
Because geographical, ethnic and cultural variations have large impacts on trends of overweight and obesity, we used the Asian BMI standard instead of international guidelines. The prevalence estimate of overweight and obesity using the Asian BMI category across all survey years was 2.10–2.50 times higher compared with estimates based on international guidelines. Evidence has shown that Asian populations are at an increased risk of cardiometabolic disorders at lower BMI levels than other ethnic groups, attributed to a considerably higher body fat percentage.33 For this reason, in 2004 the WHO recommended lowering the BMI cut-offs for Asian adults from 25 to 23 kg/m2 for overweight and from 30 to 27.5 kg/m2 for obesity.20 Previous reports that used international BMI classification in estimating overweight and obesity prevalence in Asians may have underestimated adverse health risks.
Our analysis has several limitations. We used secondary cross-sectional data, limiting our ability to identify a causal relationship between predictors and overweight and obesity. Moreover, the data set lacks some key variables, including eating habits, physical activity and smoking. Evidence showed that these factors strongly influence weight gain and may interact with other predictors of obesity, such as wealth and education. However, the study included representative sample across Bangladesh, including both urban and rural women, and used the Asian BMI category for the analysis, strengthening our evidence base.
Conclusion
Overweight and obesity increased among Bangladeshi women of reproductive age between 1999 and 2014. Sociodemographic factors including age, education, wealth index, marital status, watching TV and employment status were associated with the increased trend of overweight and obesity. The prevalence and risk factors of overweight and obesity varied between urban and rural women. Further research should focus on identifying other behavioural risk factors associated with overweight and obesity and identify feasible interventions for those most at risk.
Supplementary Material
Acknowledgments
We gratefully acknowledge the DHS for allowing us to use the data. We also would like to thank Dr. Donna L Carden, Professor of Emergency Medicine, University of Florida for her invaluable suggestions in the revision and copyediting.
Footnotes
Contributors: MABC conceptualised the study and designed the analytical approach, performed the data analyses and interpreted the findings, and led the writing of the article. MMA was involved in the literature search and drafting of the manuscript. MZH helped conceptualise the study literature, variable selection, edited and drafted the manuscript, revised the manuscript critically for important intellectual content, and helped in the final approval of the version to be submitted. All authors helped write the manuscript. All authors read and approved the final manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: All BDHS surveys received ethical approval from the ICF Macro Institutional Review Board, Maryland, USA, and the National Research Ethics Committee of the Bangladesh Medical Research Council (BMRC), Dhaka, Bangladesh. Informed consent was obtained from each participant of the survey before enrolling in the survey by using the Introduction and Consent form of the survey. It was also explained that the information will be kept strictly confidential and will not be shared with anyone except with the members of the survey team.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data sets used for the current study are publicly available at http://dhsprogram.com/data/available-datasets.cfm.
References
- 1. World Health Organization. Obesity and overweight. 2016. http://www.who.int/mediacentre/factsheets/fs311/en/ (Accessed March 24, 2017).
- 2. Ng M, Fleming T, Robinson M, et al. . Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chowdhury MA, Uddin MJ, Haque MR, et al. . Hypertension among adults in Bangladesh: evidence from a national cross-sectional survey. BMC Cardiovasc Disord 2016;16:22 10.1186/s12872-016-0197-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chowdhury MA, Uddin MJ, Khan HM, et al. . Type 2 diabetes and its correlates among adults in Bangladesh: a population based study. BMC Public Health 2015;15:1070 10.1186/s12889-015-2413-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Organization WH. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia, 2000. [Google Scholar]
- 6. Swinburn BA, Sacks G, Hall KD, et al. . The global obesity pandemic: shaped by global drivers and local environments. Lancet 2011;378:804–14. 10.1016/S0140-6736(11)60813-1 [DOI] [PubMed] [Google Scholar]
- 7. Cohen E, Boetsch G, Palstra FP, et al. . Social valorisation of stoutness as a determinant of obesity in the context of nutritional transition in Cameroon: the Bamiléké case. Soc Sci Med 2013;96:24–32. 10.1016/j.socscimed.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 8. Ziraba AK, Fotso JC, Ochako R. Overweight and obesity in urban Africa: A problem of the rich or the poor? BMC Public Health 2009;9:465 10.1186/1471-2458-9-465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Snyder JD, Merson MH. The magnitude of the global problem of acute diarrhoeal disease: a review of active surveillance data. Bull World Health Organ 1982;60:605. [PMC free article] [PubMed] [Google Scholar]
- 10. Müller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ 2005;173:279–86. 10.1503/cmaj.050342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sarma H, Saquib N, Hasan MM, et al. . Determinants of overweight or obesity among ever-married adult women in Bangladesh. BMC Obes 2016;3:13 10.1186/s40608-016-0093-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Akter J, Shahjahan M, Hossain S, et al. . Determinants of overweight and obesity among Bangladeshi diabetic women of reproductive age. BMC Res Notes 2014;7:513 10.1186/1756-0500-7-513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol 2004;103:219–24. 10.1097/01.AOG.0000107291.46159.00 [DOI] [PubMed] [Google Scholar]
- 14. Gunderson EP. Childbearing and obesity in women: weight before, during, and after pregnancy. Obstet Gynecol Clin North Am 2009;36:317–32. 10.1016/j.ogc.2009.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health 2001;91:436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Galtier-Dereure F, Boegner C, Bringer J. Obesity and pregnancy: complications and cost. Am J Clin Nutr 2000;71:1242S–8. 10.1093/ajcn/71.5.1242s [DOI] [PubMed] [Google Scholar]
- 17. Triunfo S, Lanzone A. Impact of overweight and obesity on obstetric outcomes. J Endocrinol Invest 2014;37:323–9. 10.1007/s40618-014-0058-9 [DOI] [PubMed] [Google Scholar]
- 18. NIPORT NIoPRaT, Associates Ma, International I. Bangladesh Demographic and Health Survey 2011. Dhaka, 2013. [Google Scholar]
- 19. (BBS) BBoS. Bangladesh Population and Housing Census 2011. Dhaka: Government of the People’s Republic of Bangladesh, 2012. [Google Scholar]
- 20. Barba C, Cavalli-Sforza T, Cutter J, et al. . Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 21. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res 1998;6(Suppl 2):51s–209. [PubMed] [Google Scholar]
- 22. Mkuu RS, Epnere K, Chowdhury MAB. Prevalence and Predictors of Overweight and Obesity Among Kenyan Women. Prev Chronic Dis 2018;15:E44 10.5888/pcd15.170401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Flegal KM, Graubard BI, Williamson DF, et al. . Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007;298:2028–37. 10.1001/jama.298.17.2028 [DOI] [PubMed] [Google Scholar]
- 24. Koblinsky M, Anwar I, Mridha MK, et al. . Reducing maternal mortality and improving maternal health: Bangladesh and MDG 5. J Health Popul Nutr 2008;26:280–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chowdhury AM, Bhuiya A, Chowdhury ME, et al. . The Bangladesh paradox: exceptional health achievement despite economic poverty. Lancet 2013;382:1734–45. 10.1016/S0140-6736(13)62148-0 [DOI] [PubMed] [Google Scholar]
- 26. Malik VS, Willett WC, Hu FB, Fb H. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol 2013;9:13–27. 10.1038/nrendo.2012.199 [DOI] [PubMed] [Google Scholar]
- 27. Vlismas K, Stavrinos V, Panagiotakos DB. Socio-economic status, dietary habits and health-related outcomes in various parts of the world: a review. Cent Eur J Public Health 2009;17:55. [DOI] [PubMed] [Google Scholar]
- 28. Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? Am J Clin Nutr 2009;90:369–76. 10.3945/ajcn.2009.27487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Martín AR, Nieto JM, Ruiz JP, et al. . Overweight and obesity: the role of education, employment and income in Spanish adults. Appetite 2008;51:266–72. 10.1016/j.appet.2008.02.021 [DOI] [PubMed] [Google Scholar]
- 30. Chowdhury MAB, Mkuu RS, Epnere K, et al. . 2017. Risk factors for hypertension in early to mid-life Kenyans: The Kenya Demographic and Health Survey. Paper presented at: 38th Annual Meeting and Scientific Sessions of the Society of Behavioral Medicine, San Diego, CA:The Hilton San Diego Bayfront in San Diego; [Google Scholar]
- 31. Dinsa GD, Goryakin Y, Fumagalli E, et al. . Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev 2012;13:1067–79. 10.1111/j.1467-789X.2012.01017.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Al-Ghamdi SH. The association between watching television and obesity in children of school-age in Saudi Arabia. J Family Community Med 2013;20:83 10.4103/2230-8229.114767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Deurenberg-Yap M, Chew SK, Lin VF, et al. . Relationships between indices of obesity and its co-morbidities in multi-ethnic Singapore. Int J Obes Relat Metab Disord 2001;25:1554–62. 10.1038/sj.ijo.0801739 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018468supp001.pdf (261KB, pdf)