Abstract
In this editorial we propose a condition that we refer to as ‘diabetes fatigue syndrome’ (DFS), which is commonly encountered in clinical practice. We define DFS as a multifactorial syndrome of fatigue or easy fatigability that occurs in persons with diabetes. It may be caused by a variety of lifestyle, nutritional, medical, psychological, glycemia/diabetes-related, and endocrine and iatrogenic factors. The authors share clinical pearls which can help the diabetes healthcare provider diagnose DFS, identify its etiologic factors and manage the syndrome. The editorial highlights the need to focus on symptomatic well-being in diabetes, along with efforts to achieve numerical targets.
Keywords: Adrenal, Anemia, Fatigue syndrome, Lifestyle modification, Pituitary, Thyroid, Vascular complications, Vitamin D deficiency
Introduction
Fatigue is a condition which interests researchers, clinicians, and public health specialists alike [1]. Most of the published discussion on fatigue has revolved around its description and measurement, its psychological pathogenesis and impact, and its influence on occupational and industrial health [2, 3]. Yet, a consensus on its definition has not yet been reached, and its quantification is still not standardized [1]. Fatigue is a common symptom of diabetes that is not limited to uncontrolled diabetes. Persons may complain of fatigue along with a variety of symptoms, which may together herald comorbid psychological, medical, metabolic or endocrine, and acute or chronic complications. For the diabetes healthcare professional, the debates on fatigue are a distraction from the ultimate clinical challenge, namely, to identify fatigue, diagnose the cause(s) of the fatigue, manage the condition, and prevent worsening of the morbidity.
In this editorial we seek to achieve a working definition of ‘diabetes fatigue syndrome’ (DFS), provide a clinical rubric with which to evaluate this condition, and focus attention on this relatively neglected aspect of diabetes care. Much of the discussion in this article should be relevant to general clinical care as well.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
The Importance of Symptoms
Modern diabetes care is characterized by a strong focus on evidence-based, number-driven targets and outcomes. While this approach does have its benefits, it has shortcomings and limitations as well, one of which is that little attention is paid to the symptomatic well-being of the persons with diabetes. At times, in fact, complaints may be neglected, and symptoms sacrificed, to justify the use of particular therapeutic strategies or tools. A casual reading of modern guidelines suggests that the end-target (e.g., a specific glycated hemoglobin value, or cardiovascular outcome) is more important than the means (a drug which causes gastrointestinal or genitourinary discomfort). Understandably, such clinical judgment is bound to be met with patient dissatisfaction. One symptom which may be ignored in the quest for optimal numerical end-targets, is fatigue.
Fatigue
Fatigue is defined as physical and/or mental exhaustion [4] that can be triggered by stress, medication, overwork, or mental and physical illness or disease. Fatigability is a term used to assess how fast someone gets exhausted. Easy fatigability implies the occurrence of physical and/or mental exhaustion at a level of work or stress that should ordinarily not cause such exhaustion. Fatigue impairs physical as well as mental functioning, and it reduces the quality of life. Thus, a person presenting with complaints of fatigue deserves a focused endocrine and medical checkup.
Fatigue in diabetes: a vicious cycle
Fatigue is a frequently encountered symptom in the general practice management of diabetes. Fatigue may be the presenting symptom of diabetes, or it may present as one of a constellation of complaints. It may even persist after glycemic control is achieved. All of these clinical situations, irrespective of causality or association, may be grouped together as DFS. Fatigue has been reported to be prevalent in patients with type 1 diabetes or type 2 diabetes [5, 6]. Its association with inflammation, body mass index, insulin treatment, and depression has also been studied [7–9]. The lack of correlation between fatigue on the one hand and hyperglycemia and glycemic variability on the other is also known [10]. The unique features of fatigue in persons with diabetes have also been recognized, prompting the development of disease-specific diagnostic tools [11], as opposed to generic ones [12, 13].
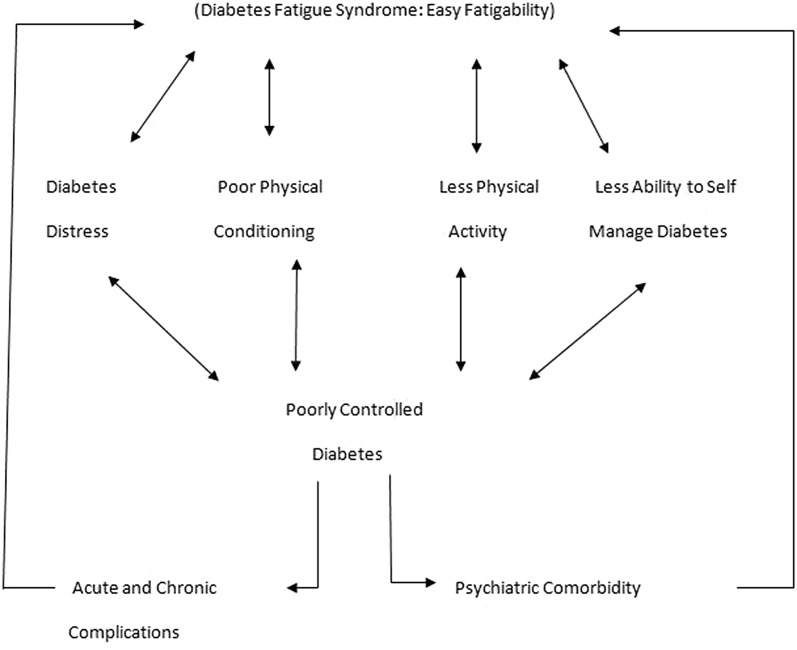
Diabetes and fatigue seem to have a bidirectional relationship, both feeding and worsening each other, thereby creating a vicious cycle of DFS (Fig. 1). This relationship is strengthened by biochemical, psychological, and lifestyle factors.
Fig. 1.
The vicious cycle of diabetes fatigue syndrome
The biochemistry of diabetes fatigue
The pathophysiology of fatigue centers around biochemical and ionic changes which occur in muscle and subsequently impact the electrical and contractile properties of this organ. Substrate depletion, high levels of hydrogen ions, and the presence of inorganic phosphate and potassium have been implicated in the pathogenesis of fatigue. Evidence suggests, however, that calcium ion availability at the sarcoplasmic reticulum of the mitochondria, which is linked to a decrease in ATP synthesis, may lead to fatigue [14].
In persons with diabetes, lack of insulin (relative to the body’s needs) may shift the energy substrate from carbohydrate to fat. When this occurs (once glycogen stores are exhausted), the ADP phosphorylation rate falls and ATP resynthesis slows down. This process may explain the occurrence of fatigue in diabetes.
The Psychology of Fatigue
Fatigue also has a strong psychological component [1]. The inability to self-manage diabetes may lead to a sense of fatiguability, which in turn may hamper efforts to manage the condition. Thus, there is a bidirectional relationship between easy fatiguability and diabetes distress, with each feeding on the other, creating a vicious cycle which ultimately leads to DFS.
Diabetes Fatigue Syndrome
We define DFS as a multifactorial syndrome of fatigue or easy fatigability that occurs in persons with diabetes. It may be caused by a variety of lifestyle, nutritional, medical, psychological, glycemic/diabetes-related, endocrine, and iatrogenic factors.
In this section we discuss the common forms of DFS that are encountered in clinical practice and describe the neuropsychiatric, musculoskeletal, and general symptoms and signs that facilitate the diabetes healthcare provider in making the differential diagnosis of DFS (Tables 1, 2). We also list ‘clinical pearls’ which help the healthcare provider to diagnose and manage DFS (Tables 2, 3). Chronic fatigue syndrome is extreme fatigue which persists unabated for at least 6 months and which is not the result of a diagnosed disease or illness. It is just one cause (out of many) of fatigue and does not fall within the range of the subject discussed here.
Table 1.
Causes of fatigue in persons with diabetes
| Non-endocrine causes | Endocrine causes |
|---|---|
| Lifestyle related | Glycemic related |
| Lack of physical conditioning/exercise | High HbA1c in spite of normal glucose levels |
| Poor sleep hygiene | Postprandial hyperglycemia with normal fasting glucose |
| Excessive caffeine, alcohol intake | Recurrent hypoglycemia |
| Substance abuse | High glycemic variability |
| Drug withdrawal | Complications of diabetes |
| Diet related | Nephropathy |
| Excessive caloric intake | Heart failure |
| Excessive caloric restriction | Myopathy |
| Protein malnutrition | Neuropathy |
| Starvation ketosis | Concomitant endocrinopathy |
| Medical | Hypothyroidism |
| Anemia | Cushing’s syndrome |
| Dyselectrolytemia | Hypogonadism |
| Vitamin deficiency | Addison’s disease |
| Diabetes distress | Iatrogenic |
| Chronic corticosteroid use | |
| Statins | |
| Diuretics | |
| Beta blockers |
HbA1c Glycated hemoglobin
Table 2.
Fatigue and depression: differential diagnosis
| Parameter | Fatigue | Depressive disorder |
|---|---|---|
| Definition | Used to refer to loss of energy with complaints of increased fatigue after mental effort, often associated with some decrease in occupational performance or coping efficiency in daily tasks. Mental fatiguability is typically described as an unpleasant intrusion of distracting associations or recollections, difficulty in concentrating, and generally inefficient thinking | A mood disorder characterized by depressed mood, loss of interest and enjoyment, and reduced energy leading to increased fatiguability and diminished activity |
| Symptoms |
Physical symptoms: reduced activity, low energy, tiredness, decreased physical endurance, increased effort to do physical tasks, general weakness, heaviness, slowness or sluggishness, nonrestorative sleep, and sleepiness. Cognitive symptoms: decreased concentration, decreased attention, decreased mental endurance, and slowed thinking. Emotional symptoms: decreased motivation or initiative (apathy), decreased interest, feeling overwhelmed, feeling bored, aversion to effort, and feeling low |
Depressed mood, loss of interest and enjoyment, and reduced energy leading to increased fatiguability and diminished activity |
| Definite diagnosis |
Definite diagnosis requires the following: (1) Either persistent and distressing complaints of increased fatigue after mental effort, or persistent and distressing complaints of bodily weakness and exhaustion after minimal effort; (2) At least two of the following: - Feelings of muscular aches and pains - Dizziness - Tension headaches - Sleep disturbance - Inability to relax - Irritability - Dyspepsia (3) Any autonomic or depressive symptoms present that are not sufficiently persistent and severe to fulfil the criteria for any other disorders, including depressive disorders |
Definitive diagnosis requires that the individual usually suffers from (1) depressed mood, (2) loss of interest and enjoyment, and (3) reduced energy leading to increased fatiguability and diminished activity. Marked tiredness after only slight effort is common. Other common symptoms are: - Reduced concentration and attention - Reduced self-esteem and self-confidence - Ideas of guilt and unworthiness (even in a mild type of episode) - Bleak and pessimistic views of the future - Ideas or acts of self-harm or suicide - Disturbed sleep - Diminished appetite Mild: at least two of three main symptoms and at least two of the other common symptoms Moderate: at least two of the three main symptoms and at least three of the other common symptoms Severe: all of the three main symptoms and at least four of the other common symptoms |
| Associated morbidity | Associated with decrease in occupational performance or coping efficiency in daily tasks | Associated with significant distress and/or dysfunction |
| Instruments for severity rating | Fatigue Questionnaire and the Fatigue Associated with Depression scales (FasD) | Beck’s Depression inventory, Hamilton Depression Rating Scale |
Table 3.
Pragmatic suggestions
| Pragmatic suggestions |
|---|
| Every person with diabetes must be asked about fatigue at each clinical encounter |
| Every person with DFS should be screened clinically for lifestyle, drug intake, and medical and endocrine factors, and by history taking and physical examination |
| Every person with a suggestive history or physical examination findings should be assessed for specific medical conditions and endocrinopathies |
| Relevant investigations for DFS must be prescribed based upon index of clinical suspicion and economic considerations |
| A therapeutic trial of vitamin D and calcium may be considered in South Asian persons with fatigue, taking the ubiquitous occurrence of vitamin D deficiency into consideration |
| Hormone replacement or supplementation should be not initiated as a treatment for DFS without documentation of endocrine deficiency or insufficiency |
DFS Diabetes fatigue syndrome
Etiology and Presentation
The possible causes of DFS may be classified as non-endocrine and endocrine factors, respectively.
Non-Endocrine DFS
Lifestyle-Related Causes
Non-endocrine factors that may contribute to DFS include an unhealthy lifestyle, inappropriate diet, and suboptimal mental health. Lack of physical conditioning, poor sleep hygiene, substance abuse (including excessive alcohol, caffeine), and drug withdrawal may lead to DFS. These factors are usually identified though history taking. Validated questionnaires may be used to screen for some of these conditions [15, 16]. The treating physician should also be aware of locally prevalent substances of abuse (such as betel quid, khat, opium) and culture-linked syndromes (e.g., Dhat syndrome) that may contribute to DFS.
Nutritional Causes
Unhealthy diets, which may lead to macronutrient or micronutrient malnutrition or starvation ketosis, can also precipitate DFS. Again, a history taking, with a detailed dietary recall, helps establish the diagnosis.
Medical Causes
Common medical conditions, such as anemia, dyselectrolytemia, and multiple vitamin deficiencies, are also characterized by fatigue. Such morbidities are as plausible in persons with diabetes as in those without. Specific symptoms and signs may point towards these comorbid causative factors of DFS. Many of these conditions coexist with dietary inadequacy. A history of breathlessness on exertion, excessive blood loss, worm infestation, and pallor on examination suggest anemia. Dyselectrolytemia usually leads to neurological symptoms and signs. Proximal muscle weakness, together with musculoskeletal aches, pains, and easy fatigability, implies vitamin D deficiency.
Psychological Causes
At times, DFS may be worsened by psychological impairment. Diabetes distress is defined as an emotional response, characterized by extreme apprehension, discomfort, or dejection due to a prescribed inability to cope with the challenges and demands of living with diabetes. This adjustment disorder is characterized by a discomfort disorder that in turn is characterized by discomfort, and it may be reported as fatigue, possibly contributing to, overlapping with, or mimicking DFS. Yet another differential diagnosis of fatigue may be major depressive disorder. The differences between fatigue and depression are highlighted in Table 2 [17, 18].
Endocrine DFS
If lifestyle, nutritional, and medical causes are ruled out, a targeted gluco-endocrine evaluation must be done to pinpoint the cause of DFS.
Diabetes-Related Causes
Diabetes-related causes include poor glycemic control, diabetic complications, and concomitant endocrinopathies. A suboptimal gluco-phenotype, involving any or all of the glycemic hexad (hyperglycemia, hypoglycemia, excessive glycemic variability), can lead to DFS. Similarly, fatigue may be the presenting symptom, or it may herald an insidious onset of vascular complications, such as heart failure and nephropathy. Lesser known comorbidities of diabetes, including chronic venous disease and Alzheimer’s disease, may also present with fatigue.
Endocrine Causes
Persons with diabetes, especially type 1 diabetes, are more prone to endocrinopathy. Diseases such as hypothyroidism, Addison’s disease, Cushing‘s syndrome, and hypothyroidism, if left unrecognized and/or untreated, may worsen DFS. The symptoms, sign, and laboratory anomalies specific to these diseases, coupled with a high index of clinical suspicion, help in their identification.
Iatrogenic Causes
At times, DFS may be iatrogenic. Drugs such as corticosteroids, beta blockers, diuretics, and statins are known to cause fatigue. Their use must be looked into during the evaluation of DFS.
Clinical Approach
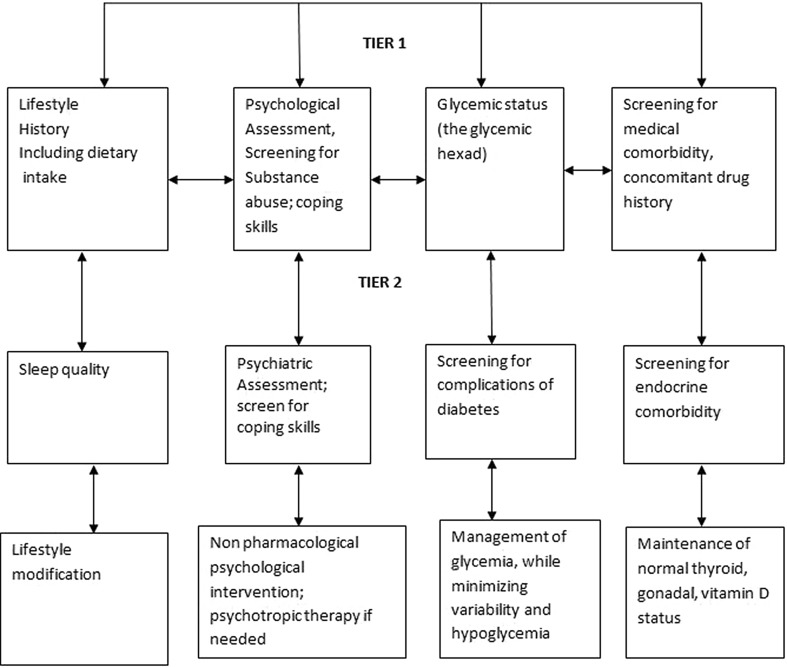
Diabetes fatigue syndrome is a multifactorial multifaceted condition which should not be evaluated from a purely gluco-centered or endocrine-oriented prism. The appropriate strategy to addressing DFS should follow a simple hierarchy (Table 2; Fig. 2) which evaluates the biomedical and psychosocial causative factors in parallel. Lifestyle- and diet-related factors are evaluated prior to factors related to medical and endocrine dysfunction. Deficiencies of macronutrients, micronutrients, electrolytes, sleep, and exercise, solely or in combination, must be ruled out before further evaluation. While glycemic control is assessed along with screening for diabetic complications, a detailed drug history must be taken to rule out iatrogenic causes of fatigue, such as statins, beta blockers, centrally acting antihypertensives, and diuretics. Fatigue corrected by eating food indicates hypoglycemia, and early morning headache or fatigue may indicate nocturnal hypoglycemia.
Fig. 2.
Approach to diagnosing diabetes fatigue syndrome
A careful history and physical examination may reveal clues which can help in choosing focused investigations to confirm common medical and endocrine diagnoses. Sudden onset fatigue in persons with well-controlled diabetes, accompanied by pallor, and reduction in anti-diabetic drug requirements should prompt investigation for nephropathy and hypothyroidism. Fatigue with breathlessness and inability to exercise in diabetes should prompt investigation for heart failure. Proximal muscular symptoms should prompt assessment for vitamin D deficiency, osteomalacia and Cushing’s syndrome, while predominant neuropathic symptoms suggest a diagnosis of diabetic neuropathy, hypothyroidism or hypoparathyroidism. Fatigue with predominant skeletal symptoms suggests a diagnosis of hyperparathyroidism, osteomalacia or osteoporosis.
Fatigue with periodicity suggests a diagnosis of dyselectrolytemia or premenstrual syndrome. Fatigue with loss of libido or other sexual dysfunction may suggest a diagnosis of hypogonadism, including menopause or andropause. Psychological morbidity, such as diabetes distress, should be ruled out prior to diagnosing psychiatric conditions.
The astute physician should be able to correlate the patient’s symptoms and sign and apply ‘good clinical sense’ to order relevant investigations. At the same time, DFS is multi-etiologic, and the treating physician must take the opportunity to optimize lifestyle, nutritional intake psychological status, and medication usage in persons with fatigue. Table 3 lists some pragmatic suggestions which reinforce this clinical approach.
Management of DFS
The psychological aspect of DFS can be minimized by effective management of diabetes distress. Diabetes distress occurs due to the person’s inability to cope with the demands of life with diabetes. Therefore, its management is best done by following a four pronged strategy: enhancing self-perception, enhancing coping skills, minimizing the discomfort of change, and utilizing external support. An effective coping adjustment with diabetes may help mitigate not only psychological distress, but also psychosomatic symptoms such as fatigue as well.
Lifestyle optimization, including a healthy diet, physical activity regimen, stress control, and a good sleep pattern, will help mitigate fatigue precipitated by unhealthy living habits.
Effective and safe glycemic control, along with maintenance of optimal endocrine, medical, and metabolic function, is necessary to tackle the physical component of DFS. A focus on euglycemia, with minimal hypoglycemia and glycemic variability, is required to ensure efficient mitochondrial function and achieve maximal musculoskeletal efficiency.
Summary
Diabetes fatigue syndrome is defined as a multifactorial syndrome of fatigue or easy fatigability, occurring in persons with diabetes, which may be caused by a variety of lifestyle, nutritional, medical, psychological, glycemia/diabetes-related, endocrine, and iatrogenic factors. Though this communication, we share a pragmatic approach to the identification and management of DFS. We highlight clinically relevant issues which will help improve the quality of care provided to persons with diabetes.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Medical Writing and Editorial Assistance
No medical or editorial assistance was sought or received for the writing of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Sanjay Kalra and Rakesh Sahay have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced digital features
To view enhanced digital features for this article go to 10.6084/m9.figshare.6304445.
References
- 1.Fritschi C, Quinn L. Fatigue in patients with diabetes: a review. J Psychosom Res. 2010;69(1):33–41. doi: 10.1016/j.jpsychores.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weijman I, Ros WJ, Rutten GE, Schaufeli WB, Schabracq MJ, Winnubst JA. Fatigue in employees with diabetes: its relation with work characteristics and diabetes related burden. Occup Environ Med. 2003;60(suppl 1):i93–i98. doi: 10.1136/oem.60.suppl_1.i93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jain A, Sharma R, Choudhary PK, Yadav N, Jain G, Maanju M. Study of fatigue, depression, and associated factors in type 2 diabetes mellitus in industrial workers. Ind Psychiatry J. 2015;24(2):179. doi: 10.4103/0972-6748.181731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fatigue. http://www.dictionary.com/browse/fatigue?s=t. Accessed 10 May 2018.
- 5.Fritschi C, Quinn L, Hacker ED. Fatigue in women with type 2 diabetes. Diabetes Educator. 2012;38(5):662–672. doi: 10.1177/0145721712450925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh R, Teel C, Sabus C, McGinnis P, Kluding P. Fatigue in type 2 diabetes: impact on quality of life and predictors. PLoS One. 2016;11(11):e0165652. doi: 10.1371/journal.pone.0165652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lasselin J, Layé S, Dexpert S. Fatigue symptoms relate to systemic inflammation in patients with type 2 diabetes. Brain Behav Immun. 2012;26(8):1211–1219. doi: 10.1016/j.bbi.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Lasselin J, Layé S, Barreau JB. Fatigue and cognitive symptoms in patients with diabetes: relationship with disease phenotype and insulin treatment. Psychoneuroendocrinology. 2012;37(9):1468–1478. doi: 10.1016/j.psyneuen.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 9.Singh R, Kluding PM. Fatigue and related factors in people with type 2 diabetes. The Diabetes educator. 2013;39(3):320–326. doi: 10.1177/0145721713479144. [DOI] [PubMed] [Google Scholar]
- 10.Goedendorp MM, Tack CJ, Steggink E, Bloot L, Bazelmans E, Knoop H. Chronic fatigue in type 1 diabetes: highly prevalent but not explained by hyperglycemia or glucose variability. Diabetes Care. 2014;37(1):73–80. doi: 10.2337/dc13-0515. [DOI] [PubMed] [Google Scholar]
- 11.Varni JW, Limbers CA, Bryant WP, Wilson DP. The PedsQL™ Multidimensional Fatigue Scale in type 1 diabetes: feasibility, reliability, and validity. Pediatric diabetes. 2009;10(5):321–328. doi: 10.1111/j.1399-5448.2008.00482.x. [DOI] [PubMed] [Google Scholar]
- 12.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann Intern Med. 1994;121(12):953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 13.Michielsen HJ, De Vries J, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: the Fatigue Assessment Scale. J Psychosom Res. 2003;54(4):345–352. doi: 10.1016/S0022-3999(02)00392-6. [DOI] [PubMed] [Google Scholar]
- 14.Vøllestad NK, Sejersted OM. Biochemical correlates of fatigue. Eur J Appl Physiol. 1988;57(3):336–347. doi: 10.1007/BF00635993. [DOI] [PubMed] [Google Scholar]
- 15.Mastin DF, Bryson J, Corwyn R. Assessment of sleep hygiene using the Sleep Hygiene Index. J Behav Med. 2006;29(3):223–227. doi: 10.1007/s10865-006-9047-6. [DOI] [PubMed] [Google Scholar]
- 16.Bryer JB, Martines KA, Dignan MA. Millon Clinical Multiaxial Inventory Alcohol Abuse and Drug Abuse scales and the identification of substance-abuse patients. Psychol Assess J Consult Clin Psychol. 1990;2(4):438. [Google Scholar]
- 17.Targum SD, Fava M. Fatigue as a residual symptom of depression. Innov Clin Neurosci. 2011;8(10):40–43. [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. International statistical classification of diseases and related helath conditions. Geneva: World Health Organization;1992.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.