Abstract
Air pollution is a very critical issue worldwide, particularly in developing countries. Particulate matter (PM) is a type of air pollution that comprises a heterogeneous mixture of different particle sizes and chemical compositions. There are various sources of fine PM (PM2.5), and the components may also have different effects on people. The pathogenesis of PM2.5 in several diseases remains to be clarified. There is a long history of epidemiological research on PM2.5 in several diseases. Numerous studies show that PM2.5 can induce a variety of chronic diseases, such as respiratory system damage, cardiovascular dysfunction, and diabetes mellitus. However, the epidemiological evidence associated with potential mechanisms in the progression of diseases need to be proved precisely through in vitro and in vivo investigations. Suggested mechanisms of PM2.5 that lead to adverse effects and chronic diseases include increasing oxidative stress, inflammatory responses, and genotoxicity. The aim of this review is to provide a brief overview of in vitro and in vivo experimental studies of PM2.5 in the progression of various diseases from the last decade. The summarized research results could provide clear information about the mechanisms and progression of PM2.5-induced disease.
Keywords: particulate matter (PM), PM2.5, animal model, in vitro study, disease progression
1. Introduction
Particulate matter (PM) is a complex mixture of solid and liquid elements that are distributed in the air. Most fine PM (PM2.5) is from anthropogenic emissions and a few are from natural emissions, with the major sources of anthropogenic emissions being industry, coal combustion, and traffic pollution. The components of PM2.5 also exhibit variety in different seasons and cities. Accordingly, the composition, size, biological properties, and physical properties of particles are related to the region, season, and change over time [1,2]. Differences in pollution levels are generated from various pollution sources. The main components of PM are heavy metals, carbon sources, sulfate, ammonium, nitrate, and various ions. In ambient air, several gas pollutants are generated from the same sources as PM pollution, such as carbon monoxide, ozone, nitrogen oxides, and sulfur dioxide. Gas pollutants combined with PM might have adverse effects on human health. The adverse health effects of PM on the progression of diseases mainly depend on gender due to exposure differences, hormonal status, life stages, and other factors [3].
Fine PM, with a size of less than 2.5 μm, is known as PM2.5, which is mostly derived from combustion sources. The carbon core of PM2.5 is coated with hydrocarbons, metals ions, and secondary particles derived from nitrogen oxides and sulfur oxides. The large surface area of PM2.5 contributes to the combination of toxic compounds, including polycyclic aromatic hydrocarbons (PAHs), volatile organic compounds (VOCs), and transition metals [4,5]. PM2.5 can be inhaled into the gas exchange area of human lungs [6,7] where the ultrafine component is released to the systemic circulatory system, causing damage to cells and tissues [8,9,10].
2. Potential Mechanisms of PM2.5 in Disease Progression
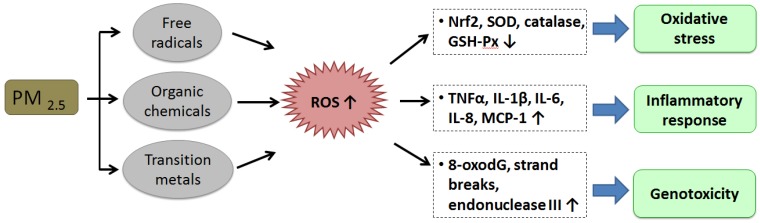
PM2.5 is closely related to adverse health outcomes. The potential mechanisms of the impact of PM2.5 on the pathogenesis of diseases include oxidative stress, inflammatory responses, and genotoxicity (Figure 1). PM2.5-induced reactive oxygen species (ROS) have been regarded as a crucial mediator of PM2.5 toxicity [11,12,13]. Organic compounds and free radicals generated from combustion sources could be connected with PM2.5. Reactive electrophilic metabolites are the electrophilic messengers for ROS that activates ROS through redox cycling and metabolic activation. [14,15,16,17,18,19,20]. Transition metals, such as Mn, Vn, Cu, and Fe, coated to PM2.5 and the resulting Fenton reaction produces intracellular ROS. Oxidative stress can be induced by increasing ROS, which impairs the antioxidant system by decreasing the nuclear factor, erythroid-2-related factor 2 (Nrf2) [11], and reducing the antioxidant ability of the cells by reducing antioxidant enzymes, such as superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), and catalase [21,22,23]. PM2.5 induces the activation of inflammatory cells, which can produce ROS due to the generation of oxidative stress in cells [24,25].
Figure 1.
The potential mechanisms of PM2.5 on disease progression. The cellular toxicity components, mainly including free radicals, organic chemicals, and transition metals, of PM2.5 may induce or produce reactive oxygen species (ROS) that impair the cellular physiological/biochemical processes by the mechanisms of inducing oxidative stress, inflammation, genotoxicity, and others, altering the normal physiological functions and/or fates of target cells, resulting in damage of the tissues and organs.
PM2.5-induced ROS enhances the gene and protein expression of pro-inflammatory factors, including tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), interleukin-6 (IL-6), interleukin-8 (IL-8), and monocyte chemoattractant protein-1 (MCP-1). ROS also enhances inflammation in the pathogenesis of various diseases [26,27,28,29,30]. Inflammation has been shown to be involved in most, if not all, of the adverse health effects of PM2.5, and has demonstrated a central role in the impacts of PM2.5. In genotoxicity, augmented levels of 7-hydro-8-oxo-2′-deoxyguanosine (8-oxodG) are critical predictors of oxidative DNA damage. PM2.5-induced ROS is associated with several types of DNA damage through enhanced levels of strand breaks, 8-oxodG, and endonuclease III in animal and human cells [17,29,31,32].
In recent years, PM2.5 pollution has gradually drawn more attention, and several countries are investigating the relationships between PM2.5 and human health. A number of epidemiological review articles have shown that PM2.5 is associated with the pathogenesis of several chronic diseases, including respiratory system injuries [33,34], cardiovascular diseases [35,36], and diabetes mellitus [37]. Some review articles also summarize the potential mechanisms of PM2.5 in ambient air on adverse health outcomes [38,39,40,41]. However, the mechanisms underlying these effects have not been fully understood. Therefore, this review discusses experimental cell and animal studies that may help in understanding the suggested links between increased PM2.5 levels and the progression of disease in humans.
3. In Vitro Experimental Studies of PM2.5-Induced Cell Damage
In vitro cell investigations can be used as representatives of various cell types. Cells can readily be obtained from detailed mechanism research for embryos, tissues, and animal organs [42]. Previous research indicates that the effects of PM2.5 on human health are related to the size and components of the particles, which have a fundamental relationship with the progression of multiple diseases [43,44]. Cell experiments are a useful tool and rapidly provide information on each component of PM2.5 and its specific health effects. The main limitation of in vitro investigations is that cells have been removed from biological conditions. Most in vitro investigations are performed using a monolayer of one cell type that excludes interacting neighboring cells, despite intercellular signaling being essential for tissue and organ homeostasis [45]. It is especially important for freshly isolated cells to preserve the multidimensional structures and interactions with different cell types that normally form tissues [45,46,47]. In the complex environment of human organisms, using only one cell type is too different from the normal biological state. Therefore, the development of in vitro cell co-culture systems are a useful tool to examine true exposure to airborne PM.
Consequently, submerged cell culture is a common method to explore the adverse effects of PM2.5 in cell experiments. Air liquid interface (ALI) cell culture is another critical method and displays similar differentiation and growth states to those observed in vivo. ALI cell culture can restore the pseudostratified striation of the respiratory airway in vitro, so it is a useful culture method for investigating the harmful effects of PM2.5 on the respiratory epithelium [48]. We review the recent in vitro research that indicates the cellular effects of the major components of PM2.5. The findings demonstrate the relationships between specific cell damage and different PM2.5 components, as well as clarify the potential mechanisms (Table 1). The results could provide a foundation for future research on disease progression caused by PM2.5.
Table 1.
Summary of in vitro studies for the effects of PM2.5 treatment on cell responses and damages.
| Diseases | Cell Line | Dosage | Cell Cultured Method | Study Findings and/or Conclusion | Reference |
|---|---|---|---|---|---|
| BEAS-2B | 50 mg/mL | submerged | Organic fraction of PM2.5 causes micronucleus formation and DNA breakage leads to inhibition of antioxidant enzymes, which increases the oxidative stress. | [49] | |
| 25, 50, and 100 µg/mL | submerged | PM2.5 enhances autophagy via PI3K/Akt/mTOR pathway inhibition. | [50] | ||
| 1.5, 3, and 6 μg/cm2 | submerged | PM2.5 inhibits the P53 levels through ROS-Akt-DNMT3B pathway-related p53 promoter hypermethylation. | [51] | ||
| 2.5, 5, and 10 μg/cm2 | submerged | PM2.5 induces expression of the IL-8 gene by endocytosis and oxidative stress induction. | [52] | ||
| 0.1 mg/mL | air-liquid interface | Secondary organic aerosol-PM2.5 downregulates the expression and activation of Nrf2-related transcription factor system. | [53] | ||
| 289.4 μg/m3 | air-liquid interface | Motorcycle exhaust-PM exposure reduces cell relative viabilities and induces ROS generation | [54] | ||
| 16HBE cells | 50 and 100 μg/mL | submerged | PM2.5 can regulate JAK/STAT signaling pathway leading to oxidative damage of cells | [55] | |
| 50 µM/cm2 | submerged | PM2.5 induces the Der p1 antigen-related innate immune response via the increasing of IL-25, IL-33, and TSLP levels. | [56] | ||
| 16, 32, 64, and 128 mg/mL | submerged | PM2.5 induces oxidative damage, DNA strand breaks, and apoptosis occurs by the p53-dependent pathway. | [57] | ||
| 100 mg/mL | submerged | PM2.5 elevates ROS generation, and inhibits mitochondrial genes expressions, resulting in mitochondrial damage and apoptosis. | [58] | ||
| Human AM/L132 | 18.84, 37.68, 56.52, 75.36, and 150.72 μg/mL | submerged | PM2.5-0.3 induces genetic instability and alterations of cell cycle via TP53-RB gene signaling pathway activation in the human alveolar macrophage and L132 co-culture model | [59] | |
| BEAS-2/THP-1 | 10 and 100 μg/mL | submerged | Industrial PM2.5 extracts enhance inflammation and pulmonary epithelial cells injuries via the RhoA/ROCK-dependent NF-кB signaling pathway. | [60] | |
| HBEC | 100 μg/mL | air-liquid interface | PM2.5 enhances arginase II levels via the EGF-related signaling pathway of oxidative stress and expression in human bronchial epithelial cells. | [61] | |
| 1, 10, and 100 μg/cm2 | air-liquid interface | PM2.5 elevates the tetra-OH-B[a]P and 8-OHdG levels in the DNA of primary human bronchial epithelial (HBE) cells from COPD patients compared to those in HBE from normal subjects. | [62] | ||
| PBEC | 1.1, 2.2, 5.6, and 11.1 μg/cm2 | air-liquid interface | Transition metals of PM increase the levels of IL-8 and HO-1, leading to ROS production in mucus-secreting ALI-cultured primary bronchial epithelial cells. | [63] | |
| A549 | _ | submerged | 10 transition metals and 16 critical PAHs were analyzed in PM2.5 samples, and their biological effects included the induction of cell death and the reduction of cell viability | [64] | |
| 50, 100, and 200 μg/mL | submerged | Organic and aqueous fraction of PM extracts inhibit cell proliferation by PM2.5 and induces LDH release by PM10. | [65] | ||
| 25, 50, 100, 200, 300, and 600 μg/mL | submerged | PM2.5 upregulates the metal-redox-sensitive transcription factors, NF-κβ and AP-1 in apoptosis. | [66] | ||
| 100 μg/mL | submerged | PM2.5-induces autophagy via the AMP-activated protein kinase signaling pathway. | [67] | ||
| 50 and 100 μg/mL | submerged | PM2.5-induces ROS increases ICAM-1 levels through the IL-6/Akt/STAT3/NF-κB axis. | [68] | ||
| 75 μg/mL | submerged | Cooking oil fumes-PM2.5 can lead A549 cells to apoptosis and inflammation that might be through the activation of the MAPK/NF-кB/STAT1 signaling pathway. | [69] | ||
| 12.5, 25, 50, 100, and 200 μg/mL | submerged | PM2.5 enhances oxidative stress and cell cycle alteration in theG2/M phase that is associated with increased p53 and p21 levels and decreased CDK1 mRNA expression in A549 cells. | [70] | ||
| A549/THP-1 | 10 μg/cm2 | submerged | PM0.4 and PM1 induce ROS generation and double strand DNA breaks in A549 and THP-1 cells co-culture model that may correlate with the exacerbation of respiratory diseases. | [71] | |
| Cardiovascular dysfunctions | EA.HY926 | 0.01, 0.1 and 1 mg/cm2 | submerged | Metal ions of PM2.5 cause oxidative stress, resulting in PM2.5-mediated mitochondrial apoptosis via the NF-κB pathway. | [72] |
| 0,20, 200, 400 mg/L | submerged | PM2.5 stimulates oxidative stress and inflammation in endothelial cells; ERK1/2 is involved in the signaling pathway. | [73] | ||
| 10, 25, and 50 μg/mL | submerged | Coal-fired PM2.5 has the potency to reduce cell viability, induce oxidative DNA damage, and global DNA methylation. | [74] | ||
| 25, 50, 100, and 200 μg/mL | submerged | PM2.5-induced ROS enhances VCAM-1 and ICAM-1 levels via the ERK/Akt/NF-κB axis that leads to monocyte adhesion to endothelial cells. | [75] | ||
| HUVEC/U937 | 5, 10, 20, and 40 μg/cm2 | submerged | PM2.5 and PM10 enhance monocytic adhesion via the expression of adhesion molecules, such as E-selectin, P-selectin, and ICAM-1, in the development of inflammatory responses, which may evaluate the progression of atherosclerosis | [76] | |
| H9c2 cells | 100, 200, 400 and 800 μg/mL | submerged | PM2.5 induces cell death and reduces cell viability via triggering of the MAPK signaling pathway and increasing intracellular ROS generation. | [77] | |
| Immune inflammatory responses | RAW 264.7 | _ | submerged | PM2.5 collected from six European cities increases the levels of chemokine (macrophage inflammatory protein 2), proinflammatory factors (TNF-α and IL-6), and NO production, and caused cytotoxicity. | [78] |
| _ | submerged | Transition metals (Co, Cu, V and Ni) of PM2.5 significantly induces ROS levels. | [79] | ||
| _ | submerged | Organic fractions of PM2.5 display Cyp1A1 activation and higher mutagenicity and led to greater activation of TNF-α release. | [80] | ||
| 25, 50, and 100 μg /mL | submerged | PM2.5 induces autophagy of pulmonary macrophages via the oxidative stress-mediated PI3K/AKT/mTOR pathway. | [81] | ||
| 30 μg /mL | submerged | PM2.5 induces NF-κB and p38 levels, leading to enhanced proinflammatory factors, and MCP-1 and TNF-αexpression, which triggers inflammatory responses. | [82] | ||
| 50, 100, and 200 mg/mL | submerged | PM2.5 induces NO release and increases levels of LDH and intracellular ROS. | [83] | ||
| 100 μg/mL | submerged | Aqueous and organic fractions of PM2.5 induce expression of IL-1β through the TLR4/NF-κB axis, conducive to nucleotide-binding domain and leucine-rich repeat protein 3 inflammasome formation. | [84] | ||
| CD4+ T/ DC | 50 µg/mL | submerged | PM2.5 enhances the activation of dendritic cells and Th17-immune responses through the aryl hydrocarbon receptor-dependent pathway. | [85] |
3.1. Pulmonary Diseases
The bronchial epithelium plays a role as a barrier and keeps the structure stable to protect the lungs in the respiratory system. The excretion of biological cytokines and other peripheral stimuli can lead to chronic and acute responses in this process. Human bronchial epithelial cells play an important role in biological effects under stress responses. Organic fractions (i.e., mainly PAHs) of PM2.5 induce gene and protein expression of pro-inflammatory cytokines in a time- and concentration-dependent manner. PAHs also cause micronucleus formation and DNA breakage, leading to the inhibition of antioxidant enzymes, including SOD, sodium selenite, mannitol, and catalase, in human bronchial epithelial cells (BEAS-2B) [49].
PM2.5 enhances autophagy mediated by the PI3K/Akt/mTOR pathway inhibition [50], inhibits P53 expression, and induces the hypermethylation of the P53 promoter through the ROS-Akt-DNMT3B pathway in BEAS-2B cells [51]. PM2.5 also induces the expression of the IL-8 gene by endocytosis and inducing oxidative stress in these cells [52]. Secondary organic aerosol-PM2.5 downregulates the expression and activation of the Nrf2-related transcription factor system in BEAS-2B cells [53]. Exposure of the ALI system to motorcycle exhaust increases oxidative stress and cytotoxicity. The use of a 0.20-μm PM filter dramatically reduces the particulate composition in PM and the concentration of total hydrocarbons. The filter displays protective effects by relieving the survival of exposed pulmonary epithelial cells and decreasing the ROS levels. Therefore, emission factors, such as different sizes of PM and total hydrocarbons from motorcycles, may play a role in motorcycle exhaust -related toxicity [54]. PM2.5-induced ROS also stimulates oxidative stress [55,56], apoptosis [57], and mitochondrial damage in 16-HBE cells [58].
PM2.5 could regulate the JAK/STAT signaling pathway and lead to oxidative damage in bronchial epithelial cells [55]. It also significantly induced oxidative damage, DNA strand breaks, and apoptosis by the p53-dependent pathway [57]. PM2.5–0.3 induces genetic instability and alterations of the cell cycle via TP53-RB gene signaling pathway activation in human alveolar macrophages and an L132 co-culture model [59]. Industrial PM2.5 extracts enhance inflammation and pulmonary epithelial cell injuries via the RhoA/ROCK-dependent NF-кB signaling pathway in a co-culture system of BEAS-2 and THP-1 cells [60].
PM2.5 enhances levels of arginase II via an EGF-related signaling pathway of oxidative stress and expression in human bronchial epithelial cells, which may be involved in the mechanism of adverse effects induced by PM exposure in asthma patients [61]. Tetra-OH-B[a]P and 8-OHdG levels are elevated in the DNA of primary human bronchial epithelial (HBE) cells from COPD patients compared to those in HBE from normal subjects. This indicates that COPD-DHBE cells were more sensitive to PM2.5 derived from air pollution [62]. Transition metals in PM increase the levels of IL-8 and HO-1, leading to ROS production in mucus-secreting ALI-cultured primary bronchial epithelial cells (PBECs) [63].
According to these studies, PM2.5 extracts impact various epithelial cells of the airway. Organic matter can affect the expression of crucial enzymes, and it influences the repair and synthesis of DNA. Organic extracts also play a key role in oxidative damage, the inflammatory response, and signaling pathways. Hydro-soluble fractions generate ROS, induce the secretion of inflammatory factors, and are related to genetic toxicity and the apoptotic response. Transition metals are related to genetic toxicity and inflammatory responses.
A549 cells are lung cancer cells derived from human alveolar basal epithelial cells, with properties of both malignant tumor cells and alveolar type II cells. Therefore, A549 cells are commonly used in investigations of the development and treatment of lung cancer. Pavagadhi et al. (2013) studied the effects of PM2.5 samples from Singapore on A549 cells. 10 transition metals and 16 critical PAHs were analyzed in PM2.5 samples, and their biological effects included the induction of cell death and the reduction of cell viability [64].
Studies on organic and aqueous fractions of PM extracts showed that PM2.5 inhibited cell proliferation and that PM10 induced the release of lactate dehydrogenase (LDH) in A549 cells [65]. In the inflammatory response, extracts of PM2.5 upregulated biological factors that are associated with down-stream stimulation of kinase pathways and the caspase cascade. Upregulation of metal-redox-sensitive transcription factors, activator protein-1 (AP-1), and the transcription factor, κB (NF-κB), is correlated with a mechanism of cell death triggered via Fenton-active transition metal redox catalysis [66]. The autophagy might occur through the AMP-activated protein kinase signaling pathway [67].
PM2.5-induced ROS increases levels of intercellular adhesion molecule 1 (ICAM-1) through the IL-6/Akt/STAT3/NF-κB axis, which promotes monocyte adhesion to endothelial cells [68]. Recent studies suggest that PM2.5 from cooking oil fumes could lead to apoptosis in A549 cells and inflammation, which might occur through the activation of the MAPK/NF-кB/STAT1 signaling pathway [69]. PM2.5 enhances oxidative stress and cell cycle alteration in the G2/M phase, which is associated with increased p53 and p21 levels and decreased CDK1 mRNA expression in A549 cells [70]. PM0.4 and PM1 induce ROS generation and double-strand DNA breaks in a co-culture model of A549 and THP-1 cells, which may correlate with the exacerbation of respiratory diseases [71]. In conclusion, PM2.5 extracts–induced ROS play a crucial role in cellular autophagy and the apoptosis pathway.
3.2. Cardiovascular Dysfunctions
Endothelial cells of vascular tissue form a tightly arranged layer on the surface of blood vessel linings. These cells regulate metabolism and the secretion functions of various physiological phenomena, including thrombosis prevention, blood volume, and blood pressure [72]. Metal ions of PM2.5 cause oxidative stress, resulting in PM2.5-mediated mitochondrial apoptosis via the NF-κB pathway in human umbilical vein endothelial cells (EA.hy926), which may enhance metal ions coated with endothelial cells [72]. PM2.5 stimulates oxidative stress and inflammation in endothelial cells; ERK1/2 is involved in the signaling pathway and leads to PM2.5-induced EA.hy926 endothelial cell injury [73].
Coal-fired PM2.5 from coal combustion has the potential to reduce cell viability, induce oxidative DNA damage, and induce global DNA methylation, and metal ions may be crucial factors that impact cellular toxicity in EA.hy926 cells [74]. PM2.5-induced ROS enhanced the levels of VCAM-1 and ICAM-1 via the ERK/Akt/NF-κB axis, which leads to monocyte adhesion to endothelial cells [75]. In a co-culture system of human umbilical vein endothelial cells and monocytic U937 cells, PM2.5 and PM10 enhanced monocytic adhesion via the expression of adhesion molecules, such as E-selectin, P-selectin, and ICAM-1, in the development of inflammatory responses, which may be used to evaluate the progression of atherosclerosis [76].
PM2.5 induced cell death and reduced cell viability via triggering of the MAPK signaling pathway and increasing intracellular ROS generation in rat H9c2 cells [77]. According to these results, metal ions of PM2.5 may be related to the induction of oxidative stress in endothelial cells. Organic soluble fractions of PM2.5 enhance the gene expression of antioxidant enzymes and oxidative stress. The dysfunction also affects the pathogenesis of various cardiovascular diseases, including hypertension, atherosclerosis, and diabetes.
3.3. Immune Inflammatory Responses
Macrophages are a major target for the immune inflammatory responses caused by PM2.5. They play a central role in releasing cytokines after the inhalation of particles, and they participate in almost every immune inflammatory response. PM2.5 collected from six European cities increased the levels of chemokine (macrophage inflammatory protein 2), proinflammatory factors (TNF-α and IL-6), and NO production, and caused cytotoxicity in RAW264.7 [78]. PM2.5 can contain soil-derived Co, Cu from vehicular abrasives, and combustion-derived elements from fuel oil, such as V and Ni. These components significantly induced ROS levels in rat alveolar macrophage cells. The results suggest a dominant role of transition metals in generating ROS compared to organic carbon [79].
PM2.5 was collected and compared from two cities of New Zealand: Auckland and Christchurch. Their components were explored and correlated with the oxidative response in RAW264.7 macrophage cells. The concentrations of PAHs and hydro-soluble metal were higher in Christchurch PM2.5 than Auckland PM2.5. The organic fractions of Christchurch PM2.5 displayed Cyp1A1 activation and higher mutagenicity compared with Auckland OE-PM2.5. Hydro-soluble extracts of Auckland PM2.5 were more cytotoxic and led to greater activation of TNF-α release than those from Christchurch PM2.5 [80].
Studies report that PM2.5 induces autophagy of pulmonary macrophages by the ROS-related PI3K/Akt/mTOR pathway [81]. PM2.5 also could increase p38 and NF-κB levels in RAW 264.7 cells, leading to enhanced proinflammatory factors MCP-1 and TNF-α expression [82]. It also induces NO release and increases levels of LDH and intracellular ROS [83], which triggers the inflammatory response. Aqueous and organic fractions of PM2.5 induced the expression of the IL-1β through the TLR4/NF-κB axis, as well as the formation of the nucleotide-binding domain and leucine-rich repeat protein 3 inflammasome [84]. In a co-culture model of CD4+ T cell and dendritic cells, PM2.5 enhances the activation of dendritic cells and Th17-immune responses through the aryl hydrocarbon receptor-dependent pathway [85].
The above results show that the carbon core, hydro-soluble, hydro-insoluble, and lipid-soluble constituents of PM2.5 can result in injury to macrophages. Particularly, hydro-insoluble fractions, such as PAHs and VOCs, have a high correlation with mutation, cell toxicity, and the release of inflammatory cytokines. The metal elements of hydro-soluble constituents can lead to oxidative stress, and, transition metals particularly, show close correlations with the inflammatory response. Metal ions can also affect the antibacterial ability of macrophages. The interaction influences between each element may induce cell damage.
4. In Vivo Studies of PM2.5-Induced Damage by Animal Models
Animal experimental models are usually used to explore the possible health effects on humans due to environmental and occupational exposure to PM2.5. The high profile of the potential effects of occupational or environmental exposure to PM2.5 has led to numerous relevant studies on animals [86,87,88]. We attempted to summarize the in vivo experimental studies of PM2.5 on animal models regarding health effects, such as respiratory diseases, cardiovascular dysfunctions, diabetes mellitus, and allergic sensitization (Table 2).
Table 2.
Summary of in vivo studies on health effects of PM2.5.
| Health Effects | Animal Models | PM2.5 Dosage | Methods of PM2.5 Treatment | Study Findings and/or Conclusion | Reference |
|---|---|---|---|---|---|
| Respiratory diseases | C57BL/6 mice | 5 and 15 μg/mouse | Instillation | Low doses of PM2.5 may simulate histological and functional changes in lung tissue, but do not impact oxidative stress and inflammations. Acute PM2.5 exposure enhances pulmonary oxidative stress, inflammatory responses, and deteriorated pulmonary impedance. | [106] |
| 6 h/day, 5 days/week for 5, 14, and 21 days | Inhalation | PM2.5 induces MCP-1 and neutrophils levels in pulmonary inflammation. | [107] | ||
| 6.25 mg/kg/day, once a day for 3 days | Instillation | ACE2 deficiency enhances inflammatory responses and tissue remodeling through p-STAT3 and p-ERK1/2 signaling pathways in PM2.5-induced acute lung injury. | [108] | ||
| 2.5, 5, and 10 mg/kg/mouse | Instillation | Acute PM2.5 exposure triggered the Th2-mediated immune response and leads to locally and systemically acute inflammations in mice. | [109] | ||
| Wistar rats | 0.3, 1.0, and 3.0 μg /mL | Instillation | PM2.5 upregulates endothelin A receptors and endothelin B receptors, and are associated with JNK and p38 pathways and MEK1/2 and p38 pathways in rat bronchi. | [110] | |
| 0.4 mg/mL/rat | Inhalation | PM2.5 can significantly enhance changes of Cyclin-dependent kinase 2 and p53 in the early phase, cyclin B and Cell Cycle Controller 2 in mid-term, and p21 in long-term exposure. | [111] | ||
| 8 mg/rat | Instillation | PM2.5 exposure significantly induces the expression level of SOD, IL-6 and IL-8, and neutrophil under cold stress. | [112] | ||
| 0.3, 0.75, 2, and 5 mg/rat | Instillation | PM2.5 can induce the inflammation response and reduce the phagocytic activity of alveolar macrophages, resulting in lung injuries in female rats. | [113] | ||
| 0.375, 1.5, 6.0, and 24.0 mg/kg (body weight) | Inhalation | PM2.5-induced pathological injury is related to ROS production, mitochondrial fusion–fission dysfunction, mitochondrial lipid peroxidation, and abnormal cellular homeostasis | [114] | ||
| 0.1, 0.5, 2.5, and 7.5 mg/kg | Intraperitoneal instillation | Maternal PM2.5 may upregulate the epithelial-mesenchymal transition ion through the TGF-β/Smad3 signaling pathway in postnatal pulmonary dysfunction. | [115] | ||
| Cardiovascular dysfunction | Balb/c mice | 10 mg/kg | Instillation | PM2.5 increases T helper 17-mediated viral replication, perforin response, and imbalance of MMP-2/TIMP-1 in virus-induced myocarditis. | [123] |
| 10 mg/kg | Instillation | PM2.5 induces T regulatory cells (Treg) responses in virus-induced myocarditis. | [124] | ||
| 0.3 mg/mouse | Instillation | PM2.5 exposure induces HO-1, ET-1, Cyp1A1, Cyp1B1 myeloperoxidase, and Hsp70 levels of lung and heart. | [125] | ||
| Apoe(-/-) mice | 6 h/day, 5 days/week for 6 months | Inhalation | Ni and P of PM2.5 may correlate with heart rate and heart rate variability. Long-range transported PM2.5 may positively associate with heart rate and negatively with heart rate variability. | [126] | |
| 3, 10, and 30 mg/kg | Instillation | PM2.5 can significantly enhance malondialdehyde and reduce heart rate variability in atherosclerosis. | [127] | ||
| 24 h/day, 7 days/week, for 2 months | Inhalation | PM2.5 can upregulate the visfatin to activate the inflammation, oxidative stress and accelerate the atherosclerosis. | [128] | ||
| 6 h/day, 5 days/week for 3 months | Inhalation | PM2.5 induces CD36-dependent 7-ketocholesterol accumulation in macrophages on the progression of atherosclerosis. | [129] | ||
| Kkay mice | 6 h/day, 5 day/week for 8 weeks | Inhalation | IKK/NFκB pathway also plays a critical role in mediating PM2.5-related cardiovascular impairment in a type 2 diabetes mellitus mice model. | [130] | |
| Wistar rats | 0.2, 0.8, and 3.2 mg/rat | Instillation | PM2.5 alone exposure induces inflammation, endothelial function, and ANS injuries, and ozone potentiated these effects induced by PM2.5. | [131] | |
| SD rats | 10 h/day for 4 or 5 consecutive days | Inhalation | PM2.5 exposure depresses cardiovascular system with diet-induced metabolic syndrome. | [132] | |
| 0.375, 1.5, 6, and 24 mg/kg | Instillation | PM2.5 induces oxidative stress, inflammation, and calcium homeostasis disorder, resulting in mitochondrial damage. | [133] | ||
| 0, 0.3, 1, and 3 mg/mL for 24 h | Instillation | PM2.5 induces the endothelin B and endothelin A receptor upregulation via the MEK/ERK1/2 pathway in rat coronary arteries. | [134] | ||
| 10 mg/mL/day for 7 days | Nasal Inoculation | PM2.5 might exaggerate neurobehavioral alterations that are associated with astrocytes activation and inflammatory reactions in ischemic stroke of SD male rats. | [135] | ||
| Diabetes mellitus | C57BL/6 mice | 6 h/day, 5 days/week for 10 months | Inhalation | Chronic PM2.5 exposure enhances gene expression, mitochondrial alterations, and oxidative stress in brown and white adipose tissues. | [141] |
| 6 h/day, for 9 or 30 consecutive days | Inhalation | PM2.5 induces NF-κB-related inflammasome activation and vascular insulin resistance leads to peripheral blood and bone marrow endothelial progenitor cells level recovery. | [142] | ||
| 6 h/day, 5 days/week for 10 months | Inhalation | Chronic PM2.5 exposure induces macrophage infiltration and Unfolded Protein Response in white adipose tissue. | [143] | ||
| 6 h/day, 5 days/week for 17 weeks | Inhalation | PM2.5 enhances insulin resistance through regulation of hepatic lipid metabolism, visceral adipose tissue inflammatory responses, and glucose utilization in skeletal muscle through both CCR2-dependent and -independent pathways in HFD-fed mice. | [144] | ||
| B6.129SF2/J mice | 5 μg/day/mouse for 12 weeks | Instillation | PM2.5 promotes [eHsp72]/[iHsp70] and the cell stress response, leading to an increased risk of metabolic dysfunction and type 2 diabetes mellitus in HFD-fed mice | [145] | |
| SD rats | 24 h/day, 7 days/week, for 16 weeks. | Inhalation | PM2.5 exposure significantly elevates the levels of glycated hemoglobin A1c, IL-6, and fibrinogen, which lead to the deterioration of tubular injury, glomerulosclerosis, aortic medial thickness, and focal myocarditis in the kidney and heart. | [146] | |
| 5 h/day for 3 days | Inhalation | PM2.5 exposure increases the angiotensin/bradykinin systems, immune, and antioxidant imbalance in early kidney damage. | [147] | ||
| 3 and 30 μg/mouse | Instillation | Long-Term PM2.5 increases blood pressure by inhibition of the D1 receptor through regulation of the G protein-coupled receptor, kinase 4 | [148] | ||
| 15 mg/kg, cumulative dose is 30 mg/kg | Instillation | PM2.5 reduces levels of GSH-Px and induced malondialdehyde, resulting in an oxidative response and inflammation in the pancreas, and pancreatic GLUT2 levels declined. | [149] | ||
| Allergic sensitization | NC/Nga mice | Supernatant fraction: 50 μg; precipitate fraction: 200 μg | Nasal Inoculation | PM2.5 can enhance airway hyperresponsivness in mice through an inflammasome activation and synergistic action of insoluble and soluble fractions of PM2.5. | [155] |
| Balb/c mice | 1, 10, and 100 μg/mouse | Instillation | PM2.5 can synergize with allergens to exacerbate the progression of asthma via activation of the Th2-related immune response. | [156] | |
| 100 μg/mouse | Intraperitoneal injection | PM2.5 and formaldehyde co-exposure can induce oxidative stress to significantly exacerbate allergic asthma via the transient receptor potential vanilloid 1 pathway. | [157] | ||
| 10, 31.6, or 100 µg/mouse | Instillation | PM2.5 exacerbates allergic airway inflammation via thymic stromal lymphopoietin activation. | [158] | ||
| 33.3 µg/mouse | Instillation | PM2.5 and allergens from dust mites enhance the hyper-responsiveness of the airway through the activation of T-helper cell type 17 activation. | [159] | ||
| Guinea pig | 1.1 ± 0.2 kg/chamber | Inhalation | Acute PM2.5 exposure with aluminum hydroxide in sensitized animals enhances the specific-hyperresponsiveness and eosinophilic and neutrophilic airway inflammation in allergic asthma. | [160] |
The most common experimental species include mice, rats, and hamsters in exploring the effects of PM2.5. Due to the physical characteristics of their respiratory tracts, PM2.5 enters the alveolar cells. The major methods of PM2.5 exposure in animal models are intratracheal inhalation and intratracheal instillation. Both methods are in vivo methods that have strengths and weaknesses (Table 3). Inhalation exposure is a physiological method of exposure to PM2.5, and it requires an expensive exposure chamber, as well as technical experience. Intratracheal instillation involves applying the material directly to the trachea [89].
Table 3.
Strengths and weaknesses of intratracheal inhalation and intratracheal instillation on PM2.5 exposure to experimental rodents.
| Methods | Intratracheal Instillation | Intratracheal Inhalation |
|---|---|---|
| Operative difficulty | High | Low |
| Equipment cost | Low | High |
| Dosage | Instillated dosage (mg/kg of body weight or mg/animal). | Real deposition in the respiratory system of animal model. Defined by the PM2.5 concentration (mg/m3) |
| Deposition | Uneven distribution in the lung lobes | Evenly distributed in the lung lobes |
| Effects for animal | More severe Only affects lower respiratory tract |
Less severe Affects whole respiratory tract |
Intratracheal instillation is frequently used in mice, rats, and hamsters by inserting a needle into the mouth and throat. Compared to inhalation, intratracheal instillation is a more difficult operation that needs experienced animal trainers to inject the amount of liquid into the trachea and not the esophagus. It allows greater control over the concentrations and location of the material, and it is cheaper. The drawbacks of intratracheal instillation include its invasive and non-physiological nature, the fact that it bypasses the upper respiratory tract, and the confounding effects of the anesthesia and delivery vehicle [90].
4.1. Respiratory Diseases
The pulmonary system is a major target of PM2.5 effects. Many investigations demonstrate that PM2.5 can lead to an inflammatory response in the respiratory system [91,92], weakening of the pulmonary function [93,94], the incidence and deterioration of chronic obstructive pulmonary disease (COPD) and asthma [95,96,97], and making the lungs susceptible to infection [98,99]. Gender is also a vital factor in the relationship between PM2.5 and the pathogenesis of pulmonary disease. In a large lung health study, a higher prevalence of airway hyperresponsiveness was observed in female subjects among middle-aged smokers with mild COPD, which is due to the airway caliber in females being smaller than that in males [100]. Increased prenatal PM2.5 exposure at the mid-gestation stage was related to the progression of childhood asthma in boys [101]. Long-term SO2 exposure increases the risk of tuberculosis in men [102].
In human air-particulate exposure experiments, wood smoke can enhance the systemic inflammatory response and increase oxidative stress in the respiratory tract, especially in the lower airways of healthy people [103]. PAH-rich wood smoke particles induce DNA damage and cellular dysfunction, which deteriorate the airway’s inflammatory responses in humans [104]. Mouse-model studies show that desert-dust PM2.5 enhanced M2 macrophages and activated the Th2-mediated immune inflammatory response due to aggravation of pulmonary eosinophilia. In alveolar macrophages from mice, wood smoke PM2.5 induced v-rel reticuloendotheliosis viral oncogene homolog B activation and macrophage suppression, according to nuclear translocation [105]. These results indicate that low doses of PM2.5 may stimulate histological and functional changes in lung tissue, but do not impact oxidative stress and inflammation.
Acute PM2.5 exposure enhances pulmonary oxidative stress and inflammatory responses and deteriorates pulmonary impedance in mice [106]. C57BL/6 mice that were exposed to PM2.5 demonstrated a significant inflammatory response via the elevation of MCP-1 and neutrophils in the lung tissue [107]. ACE2 knockdown will enhance inflammatory response, tissue remodeling and attenuate injury repair in PM2.5-induced acute lung injury via p-STAT3 and p-ERK1/2 signaling pathways [108]. Acute PM2.5 exposure triggered the Th2-mediated immune response, which leads to locally and systemically acute inflammations in mice, and TLR2 and TLR4 are associated with the progression, PM2.5 exposure reduced SOD and GSH-Px activities [109]. Endothelin (ET)-1 is the most potent endogenous bronchoconstrictor that plays a key role in vascular homeostasis. PM2.5 exposure upregulates endothelin A receptor and endothelin B receptor, which are associated with the JNK/p38 and MEK1/2/p38 pathways in rat bronchus cells [110]. PM2.5 can significantly enhance the changes of cyclin-dependent kinase 2 and p53 in the early phase, as well as cyclin B and cell cycle controller 2 in mid-term, and p21 in long-term exposure. Time is also a factor in the levels of PM2.5-related injury to lung tissue and the trachea [111].
In experimental models using rats, PM2.5 exposure significantly induced the expression of SOD, IL-6, IL-8, and neutrophil under cold stress. The results showed that oxidative stress and inflammatory responses were associated with the additive effect of cold stress and PM2.5 exposure on pulmonary injury [112]. PM2.5 can induce the inflammation response and reduce the phagocytic activity of alveolar macrophages, resulting in lung injuries in female Wistar rats [113].
PM2.5-induced pathological injury is related to ROS production, mitochondrial fusion–fission dysfunction, mitochondrial lipid peroxidation, and abnormal cellular homeostasis [114]. Moreover, maternal PM2.5 exposure may also upregulate the epithelial-mesenchymal transition ion through the TGF-β/Smad3 signaling pathway in postnatal pulmonary dysfunction [115].
4.2. Cardiovascular Dysfunctions
Several investigations have shown that PM2.5 exposure is not only related to cardiovascular function, but also the morbidity and mortality in cardiovascular disease [116,117,118]. Age, gender, and hormonal status are impact mediators in the modification of vascular toxicity by phenanthraquinone extracted diesel exhaust [119]. A meta-analysis in China reported that elevated air pollution is correlated with increased cardiovascular mortality, and lower temperature, age > 65 years, and being female were related to higher risks of cardiovascular mortality [120].
In human exposure studies, wood-smoke PM2.5 particles in smoky indoor environments seem to affect coagulation, inflammation, thrombosis, and lipid peroxidation. These factors may be associated with the mechanisms of PM in morbidity and mortality in cardiovascular disease [121,122]. In mouse studies, PM2.5 induced inflammatory responses in the myocardium by increasing the T helper 17-based perforin response, viral replication, and the ratio of abnormal matrix metalloproteinases 2 (MMP-2) to tissue inhibitor of metalloproteinases-1 (TIMP-1). PM2.5 also aggravated virus-related myocarditis, possibly via immune response depression [123] and T regulatory cell responses [124]. In a European study, PM2.5 exposure increased HO-1, endothelin-1 (ET-1), Cyp1A1, Cyp1B1 myeloperoxidase, and Hsp70 levels of the lung and heart in BALB/c mice [125].
ApoE-/- mice are a useful model to investigate atherosclerotic disease. PM2.5 from motor vehicle traffic contains numerous components, such as residual oil, secondary sulfate, and resuspended soil, which depend on the time of day. The PM2.5 composition and different time periods are related to the alteration of heart rate and HR variability in ApoE-/- mice. [126]. PM2.5 exposure could significantly increase malondialdehyde, reduce heart rate variability [127], and upregulate visfatin [128], which are conducive to oxidative stress of the heart and atherosclerosis. PM2.5 also induced CD36-dependent 7-ketocholesterol accumulation in macrophages in the progression of atherosclerosis [129]. The IκB kinase (IKK)/NFκB pathway also played a critical role in mediating the PM2.5-related cardiovascular impairment in a mouse model of type 2 diabetes mellitus [130].
PM2.5 induced systemic inflammation in Wistar rats [131]. PM2.5 exposure also depressed the cardiovascular system with diet-induced metabolic syndrome [132] and induced oxidative stress, inflammation, and calcium homeostasis disorder, resulting in mitochondrial damage in Sprague-Dawley rats [133]. In rat coronary arteries, PM2.5 induces the upregulation of endothelin B and endothelin A receptors via the MEK/ERK1/2 pathway [134]. In SD male rats, PM2.5 might exaggerate the neurobehavioral alterations associated with astrocyte activation and inflammatory reactions in ischemic stroke [135].
4.3. Diabetes Mellitus
Early evidence shows that PM2.5 exposure exacerbates the decline of renal function, which is related to time. Recently, chronic PM2.5 exposure has also been found to promote the progression of diabetes mellitus, including visceral adipose inflammatory responses, hepatic endoplasmic reticulum stress, brown adipose mitochondrial variations, and insulin resistance [136,137]. Furthermore, even low levels of PM2.5 exposure could increase the risk of mortality in diabetes mellitus [137]. PM2.5 is associated with a higher susceptibility to diabetes mellitus in women (adjusted HR, 1.17; 95%CI, 1.03–1.32), but not in men (adjusted HR, 1.03; 95%CI, 0.91–1.16) [138]. Furthermore, the prevalence of diabetes mellitus increases with an increasing of PM2.5 concentrations, with a rise of 4.0% (1.5–6.4%) for women and 3.5% (1.3–5.6%) for men per unit of elevated PM2.5 [139].
Epidemiological and experimental investigations reveal a relationship between insulin resistance and PM2.5 exposure, and the activation of innate immune responses may play a crucial role in the pathological progression of these effects. In type 2 diabetes patients, exposure to ultrafine elemental carbon particles enhances vascular endothelium and blood platelet activation, which shows that airborne particles could increase the risk for adverse cardiovascular effects in diabetes patients [140]. In C57BL/6 mice, long-term PM2.5 exposure induced impairment of glucose tolerance, insulin resistance, inflammation, and mitochondrial changes in the progression of type 2 diabetes. Chronic PM2.5 exposure also enhanced gene expression, mitochondrial alterations, and oxidative stress in brown and white adipose tissues [141]. PM2.5 induces NF-κB-related inflammasome activation and vascular insulin resistance leads to peripheral blood and bone marrow endothelial progenitor cells level recovery [142]. Chronic PM2.5 exposure induced macrophage infiltration, unfolded protein response activation, and enhanced gene expression of adipocyte differentiation, lipogenesis, and lipid droplet generation in the white adipose tissue of C57BL/6 mice. [143]. CC-chemokine receptor 2 (CCR2) induced systemic cellular inflammatory responses play a critical role in diet-induced insulin resistance. In HFD-fed CCR2-/- male mice, PM2.5 enhanced insulin resistance through the regulation of hepatic lipid metabolism, inflammatory responses in visceral adipose tissue, and glucose utilization in skeletal muscle through both CCR2-dependent and independent pathways [144]. Exposure to PM2.5 markedly promoted [eHsp72]/[iHsp70] and the cell stress response, leading to increased metabolic dysfunction and risk for type 2 diabetes mellitus in HFD-fed mice [145].
In Sprague-Dawley rats, PM2.5 exposure significantly elevated the levels of glycated hemoglobin A1c, IL-6, and fibrinogen, which led to the deterioration of tubular injury, glomerulosclerosis, aortic medial thickness, and focal myocarditis in the kidney and heart [146]. PM2.5 exposure affected the angiotensin/bradykinin systems, immune system, and antioxidant imbalance in early kidney damage [147]. In PM2.5-induced hypertension, long-term PM2.5 exposure increases blood pressure by inhibiting D1 receptor-related sodium secretion through the regulation of G protein-coupled receptor kinase 4 in Sprague-Dawley Rats. [148]. In a rat model of gestational diabetes mellitus, PM2.5 exposure significantly reduced the levels of GSH-Px and induced malondialdehyde, resulting in an oxidative response and inflammation in the pancreas. Furthermore, pancreatic GLUT2 levels declined after PM2.5 exposure [149].
4.4. Allergic Sensitization
In mice and humans, studies demonstrate that numerous types of particles induce allergic inflammation [150]. Both the organic and inorganic constituents that coat particles and the particle cores have been shown to enhance allergic sensitization [151,152,153]. The components and solubility of particles have also been shown to play an important role in allergic sensitization [154]. In NC/Nga mice, which have a high susceptibility to mite allergens, PM2.5 can enhance allergic airway inflammation through inflammasome activation and the synergistic action of insoluble and soluble fractions of PM2.5 [155].
Acute exposure to PM2.5 could synergize with allergens to exacerbate the progression of asthma via activation of the Th2-related immune response in ovalbumin-sensitized mice [156]. Combined exposure to PM2.5 and formaldehyde could significantly exacerbate allergic asthma, which is associated with induced oxidative stress via the transient receptor potential vanilloid 1 signaling pathway [157], and also through thymic stromal lymphopoietin activation in mice [158]. In a recent report, PM2.5 and allergens from dust mites enhanced the hyper-responsiveness of the airway through the activation of T-helper cell type 17 (TH17) activation [159]. In a guinea pig model, acute PM2.5 exposure with aluminum hydroxide in sensitized animals enhanced the specific-hyperresponsiveness and eosinophilic and neutrophilic airway inflammation in allergic asthma [160].
5. Conclusions
PM2.5 air pollution is a major cause of morbidity and mortality around the world. Air pollution control and pathogenesis exploration of PM2.5 are extremely important issues. Oxidative stress, inflammation, and genotoxicity are the main potential mechanisms in PM2.5-induced disease progression. The research findings of in vitro cell and in vivo animal investigations have provided vital insights into the mechanisms of PM2.5 exposure in disease progression. Better understandings of the disease mechanisms associated with PM2.5 will allow the development of new strategies to help people who are at risk and to decrease the harmful effects of PM2.5 on the pathogenesis of various diseases. To better address the knowledge gaps; the focus of exploration should be on the molecular mechanisms by which PM2.5 and its components affect public health.
Acknowledgments
This work was supported by the grants of MOST 104-2313-B-009-001-MY3 from the Ministry of Science and Technology, and the grant of MMH-HB-10606, MMH-HB-10620 and MMH-CT-10702 from the Hsinchu Mackay Memorial Hospital, Taiwan. This work was also financially supported by the “Center For Intelligent Drug Systems and Smart Bio-devices (IDS2B)” from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan.
Abbreviations
| 8-oxod | G 7-hydro-8-oxo-2′-deoxyguanosine |
| COPD | chronic obstructive pulmonary disease |
| Cyp | cytochrome P450 |
| GSH-Px | glutathione peroxidase |
| Hsp72 | heat shock protein 72 |
| HO-1 | heme oxygenase-1 |
| ICAM-1 | intercellular Adhesion Molecule 1 |
| IL-1β | interleukin-1β |
| IL-6 | interleukin-6 |
| IL-8 | interleukin-8 |
| LDH | lactate dehydrogenase |
| MCP-1 | monocyte chemoattractant protein-1 |
| MMP-2 | matrix metalloproteinases 2 |
| NF-κB | transcription factor kappab |
| NO | nitric oxide |
| Nrf2 | nuclear factor erythroid-2-related factor 2 |
| OE-DEP | organic extract of diesel exhaust particles |
| PM | particulates matter |
| PAHs | polycyclic aromatic hydrocarbons |
| ROS | reactive oxygen species |
| SOD | superoxide dismutase |
| TIMP-1 | tissue inhibitors of metalloproteinases-1 |
| TNF-α | tumor necrosis factor-α |
| VOCs | volatile organic compounds |
Author Contributions
C.-S.L. conceived and designed the article; C.-C.C., W.-Y.H., C.-H.T., C.-Y.C., H.-F.C., wrote the paper.
Funding
This research received no external funding.
Conflicts of Interest
All authors declare no conflict of interest.
References
- 1.Wang W., Jariyasopit N., Schrlau J., Jia Y., Tao S., Yu T.W., Dashwood R.H., Zhang W., Wang X., Simonich S.L. Concentration and photochemistry of PAHs, NPAHs, and OPAHs and toxicity of PM2.5 during the Beijing Olympic Games. Environ. Sci. Technol. 2011;45:6887–6895. doi: 10.1021/es201443z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maksimov A.L., Sukhanova I.V., Vdovenko S.I. Seasonal dynamics of external respiration and gas exchange in the population of northeast Russia. Aviakosm. Ekolog. Med. 2013;47:28–33. doi: 10.1134/S0362119715070117. [DOI] [PubMed] [Google Scholar]
- 3.Clougherty J.E. A growing role for gender analysis in air pollution epidemiology. Environ. Health Perspect. 2010;118:167–176. doi: 10.1289/ehp.0900994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandey P., Patel D.K., Khan A.H., Barman S.C., Murthy R.C., Kisku G.C. Temporal distribution of fine particulates (PM2.5, PM10), potentially toxic metals, PAHs and Metal-bound carcinogenic risk in the population of Lucknow city, India. J. Environ. Sci. Health A Toxic Hazard. Subst. Environ. Eng. 2013;48:730–745. doi: 10.1080/10934529.2013.744613. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein J.R., Asteria-Peñaloza R., Diaz-Artiga A., Davila G., Hammond S.K., Ryde I.T. Exposure to polycyclic aromatic hydrocarbons and volatile organic compounds among recently pregnant rural Guatemalan women cooking and heating with solid fuels. Int. J. Hyg. Environ. Health. 2017;220:726–735. doi: 10.1016/j.ijheh.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulze F., Gao X., Virzonis D., Damiati S., Schneider M.R., Kodzius R. Air Quality Effects on Human Health and Approaches for Its Assessment through Microfluidic Chips. Genes. 2017;8:244. doi: 10.3390/genes8100244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xing Y.F., Xu Y.H., Shi M.H., Lian Y.X. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 2016;8:E69–E74. doi: 10.3978/j.issn.2072-1439.2016.01.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gualtieri M., Ovrevik J., Mollerup S., Asare N., Longhin E., Dahlman H.J., Camatini M., Holme J.A. Airborne urban particles (Milan winter-PM2.5) cause mitotic arrest and cell death: Effects on DNA, mitochondria, AhR binding and spindle organization. Mutat. Res. 2011;713:18–31. doi: 10.1016/j.mrfmmm.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Xu X., Deng F., Guo X., Lv P., Zhong M., Liu C., Wang A., Tzan K., Jiang S.Y., Lippmann M., et al. Association of systemic inflammation with marked changes in particulate air pollution in Beijing in 2008. Toxicol. Lett. 2012;212:147–156. doi: 10.1016/j.toxlet.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang G., Zhen L., Lü P., Jiang R., Song W. Effects of ozone and fine particulate matter (PM2.5) on rat cardiac autonomic nervous system and systemic inflammation. Wei Sheng Yan Jiu. 2013;42:554–560. [PubMed] [Google Scholar]
- 11.Deng X., Rui W., Zhang F., Ding W. PM2.5 induces Nrf2-mediated defense mechanisms against oxidative stress by activating PIK3/AKT signaling pathway in human lung alveolar epithelial A549 cells. Cell Biol. Toxicol. 2013;29:143–157. doi: 10.1007/s10565-013-9242-5. [DOI] [PubMed] [Google Scholar]
- 12.Weichenthal S.A., Godri-Pollitt K., Villeneuve P.J. PM2.5, oxidant defence and cardiorespiratory health: A review. Environ. Health. 2013;12:40. doi: 10.1186/1476-069X-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jin X., Xue B., Zhou Q., Su R., Li Z. Mitochondrial damage mediated by ROS incurs bronchial epithelial cell apoptosis upon ambient PM2.5 exposure. J. Toxicol. Sci. 2018;43:101–111. doi: 10.2131/jts.43.101. [DOI] [PubMed] [Google Scholar]
- 14.Kouassi K.S., Billet S., Garçon G., Verdin A., Diouf A., Cazier F., Djaman J., Courcot D., Shirali P. Oxidative damage induced in A549 cells by physically and chemically characterized air particulate matter (PM2.5) collected in Abidjan, Cote d’Ivoire. J. Appl. Toxicol. 2010;30:310–320. doi: 10.1002/jat.1496. [DOI] [PubMed] [Google Scholar]
- 15.Torres-Ramos Y.D., Montoya-Estrada A., Guzman-Grenfell A.M., Mancilla-Ramirez J., Cardenas-Gonzalez B., Blanco-Jimenez S., Sepulveda-Sanchez J.D., Ramirez-Venegas A., Hicks J.J. Urban PM2.5 induces ROS generation and RBC damage in COPD patients. Front. Biosci. 2011;3:808–817. doi: 10.2741/288. [DOI] [PubMed] [Google Scholar]
- 16.Gualtieri M., Longhin E., Mattioli M., Mantecca P., Tinaglia V., Mangano E., Proverbio M.C., Bestetti G., Camatini M., Battaglia C. Gene expression profiling of A549 cells exposed to Milan PM2.5. Toxicol. Lett. 2012;209:136–145. doi: 10.1016/j.toxlet.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 17.Longhin E., Holme J.A., Gutzkow K.B., Arlt V.M., Kucab J.E., Camatini M., Gualtieri M. Cell cycle alterations induced by urban PM2.5 in bronchial epithelial cells: Characterization of the process and possible mechanisms involved. Part. Fibre Toxicol. 2013;10:63. doi: 10.1186/1743-8977-10-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gehling W., Khachatryan L., Dellinger B. Hydroxyl radical generation from environmentally persistent free radicals (EPFRs) in PM2.5. Environ. Sci. Technol. 2014;48:4266–4272. doi: 10.1021/es401770y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Øvrevik J., Refsnes M., Låg M., Holme J.A., Schwarze P.E. Activation of Proinflammatory Responses in Cells of the Airway Mucosa by Particulate Matter: Oxidant- and Non-Oxidant-Mediated Triggering Mechanisms. Biomolecules. 2015;5:1399–1440. doi: 10.3390/biom5031399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li N., Xia T., Nel A.E. The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radic. Biol. Med. 2008;44:1689–1699. doi: 10.1016/j.freeradbiomed.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davel A.P., Lemos M., Pastro L.M., Pedro S.C., de André P.A., Hebeda C., Farsky S.H., Saldiva P.H., Rossoni L.V. Endothelial dysfunction in the pulmonary artery induced by concentrated fine particulate matter exposure is associated with local but not systemic inflammation. Toxicology. 2012;295:39–46. doi: 10.1016/j.tox.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Deng X., Zhang F., Rui W., Long F., Wang L., Feng Z., Chen D., Ding W. PM2.5-induced oxidative stress triggers autophagy in human lung epithelial A549 cells. Toxicol. Vitro. 2013;27:1762–1770. doi: 10.1016/j.tiv.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 23.Wang G., Zhao J., Jiang R., Song W. Rat lung response to ozone and fine particulate matter (PM2.5) exposures. Environ. Toxicol. 2015;30:343–356. doi: 10.1002/tox.21912. [DOI] [PubMed] [Google Scholar]
- 24.Hong Z., Guo Z., Zhang R., Xu J., Dong W., Zhuang G., Deng C. Airborne Fine Particulate Matter Induces Oxidative Stress and Inflammation in Human Nasal Epithelial Cells. Tohoku J. Exp. Med. 2016;239:117–125. doi: 10.1620/tjem.239.117. [DOI] [PubMed] [Google Scholar]
- 25.Valavanidis A., Vlachogianni T., Fiotakis K., Loridas S. Pulmonary oxidative stress, inflammation and cancer: Respirable particulate matter, fibrous dusts and ozone as major causes of lung carcinogenesis through reactive oxygen species mechanisms. Int. J. Environ. Res. Public Health. 2013;10:3886–3907. doi: 10.3390/ijerph10093886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gioda A., Fuentes-Mattei E., Jimenez-Velez B. Evaluation of cytokine expression in BEAS cells exposed to fine particulate matter (PM2.5) from specialized indoor environments. Int. J. Environ. Health Res. 2011;21:106–119. doi: 10.1080/09603123.2010.515668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dergham M., Lepers C., Verdin A., Billet S., Cazier F., Courcot D., Shirali P., Garçon G. Prooxidant and proinflammatory potency of air pollution particulate matter (PM2.5–3.0) produced in rural, urban, or industrial surroundings in human bronchial epithelial cells (BEAS-2B) Chem. Res. Toxicol. 2012;25:904–919. doi: 10.1021/tx200529v. [DOI] [PubMed] [Google Scholar]
- 28.Dieme D., Cabral-Ndior M., Garçon G., Verdin A., Billet S., Cazier F., Courcot D., Diouf A., Shirali P. Relationship between physicochemical characterization and toxicity of fine particulate matter (PM2.5) collected in Dakar city (Senegal) Environ. Res. 2012;113:1–13. doi: 10.1016/j.envres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 29.Corsini E., Budello S., Marabini L., Galbiati V., Piazzalunga A., Barbieri P., Cozzutto S., Marinovich M., Pitea D., Galli C.L. Comparison of wood smoke PM2.5 obtained from the combustion of FIR and beech pellets on inflammation and DNA damage in A549 and THP-1 human cell lines. Arch. Toxicol. 2013;87:2087–2199. doi: 10.1007/s00204-013-1071-z. [DOI] [PubMed] [Google Scholar]
- 30.Mitkus R.J., Powell J.L., Zeisler R., Squibb K.S. Comparative physicochemical and biological characterization of NIST interim reference material PM2.5 and SRM 1648 in human A549 and mouse RAW264.7 cells. Toxicol. Vitro. 2013;27:2289–2298. doi: 10.1016/j.tiv.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 31.Reche C., Moreno T., Amato F., Viana M., van Drooge B.L., Chuang H.C., Bérubé K., Jones T., Alastuey A., Querol X. A multidisciplinary approach to characterise exposure risk and toxicological effects of PM10 and PM2.5 samples in urban environments. Ecotoxicol. Environ. Saf. 2012;78:327–335. doi: 10.1016/j.ecoenv.2011.11.043. [DOI] [PubMed] [Google Scholar]
- 32.Vattanasit U., Navasumrit P., Khadka M.B., Kanitwithayanun J., Promvijit J., Autrup H., Ruchirawat M. Oxidative DNA damage and inflammatory responses in cultured human cells and in humans exposed to traffic-related particles. Int. J. Hyg. Environ. Health. 2014;217:23–33. doi: 10.1016/j.ijheh.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Wang J., Shu J.Z., Chen X.Y. The effect of PM2.5 carrier components on respiratory health. Zhonghua Jie He He Hu Xi Za Zhi. 2013;36:970–972. [PubMed] [Google Scholar]
- 34.Falcon-Rodriguez C.I., Osornio-Vargas A.R., Sada-Ovalle I., Segura-Medina P. Aeroparticles, Composition, and Lung Diseases. Front. Immunol. 2016;7:3. doi: 10.3389/fimmu.2016.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lippmann M. Toxicological and epidemiological studies of cardiovascular effects of ambient air fine particulate matter (PM2.5) and its chemical components: Coherence and public health implications. Crit. Rev. Toxicol. 2014;44:299–347. doi: 10.3109/10408444.2013.861796. [DOI] [PubMed] [Google Scholar]
- 36.Wang C., Tu Y., Yu Z., Lu R. PM2.5 and Cardiovascular Diseases in the Elderly: An Overview. Int. J. Environ. Res. Public Health. 2015;12:8187–8197. doi: 10.3390/ijerph120708187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balti E.V., Echouffo-Tcheugui J.B., Yako Y.Y., Kengne A.P. Air pollution and risk of type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2014;106:161–172. doi: 10.1016/j.diabres.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 38.Atkinson R.W., Kang S., Anderson H.R., Mills I.C., Walton H.A. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: A systematic review and meta-analysis. Thorax. 2014;69:660–665. doi: 10.1136/thoraxjnl-2013-204492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen M., Liang S., Qin X., Zhang L., Qiu L., Chen S., Hu Z., Xu Y., Wang W., Zhang Y., et al. Prenatal Exposure to Diesel Exhaust PM2.5 Causes Offspring β Cell Dysfunction in Adulthood. Am. J. Physiol. Endocrinol. Metab. 2017 doi: 10.1152/ajpendo.00336.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feng S., Gao D., Liao F., Zhou F., Wang X. The health effects of ambient PM2.5 and potential mechanisms. Ecotoxicol. Environ. Saf. 2016;128:67–74. doi: 10.1016/j.ecoenv.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 41.Jiřík V., Machaczka O., Miturová H., Tomášek I., Šlachtová H., Janoutová J., Velická H., Janout V. Air Pollution and Potential Health Risk in Ostrava Region—A Review. Cent. Eur. J. Public Health. 2016;24:S4–S17. doi: 10.21101/cejph.a4533. [DOI] [PubMed] [Google Scholar]
- 42.Alfaro-Moreno E., Nawrot T.S., Vanaudenaerde B.M., Hoylaerts M.F., Vanoirbeek J.A., Nemery B., Hoet P.H. Co-cultures of multiple cell types mimic pulmonary cell communication in response to urban PM10. Eur. Respir. J. 2008;32:1184–1194. doi: 10.1183/09031936.00044008. [DOI] [PubMed] [Google Scholar]
- 43.Kloog I., Melly S.J., Ridgway W.L., Coull B.A., Schwartz J. Using new satellite based exposure methods to study the association between pregnancy PM2.5 exposure, premature birth and birth weight in Massachusetts. Environ. Health. 2012;11:40. doi: 10.1186/1476-069X-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zanobetti A., Dominici F., Wang Y., Schwartz J.D. A national case-crossover analysis of the short-term effect of PM2.5 on hospitalizations and mortality in subjects with diabetes and neurological disorders. Environ. Health. 2014;13:38. doi: 10.1186/1476-069X-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carere A., Stammati A., Zucco F. In vitro toxicology methods: Impact on regulation from technical and scientific advancements. Toxicol. Lett. 2002;127:153–160. doi: 10.1016/S0378-4274(01)00495-7. [DOI] [PubMed] [Google Scholar]
- 46.Herseth J.I., Refsnes M., Låg M., Schwarze P.E. Role of IL-1 beta and COX2 in silica-induced IL-6. J. R. Soc. Interface. 2010;7(Suppl. 1):S27–S40. doi: 10.1016/j.tiv.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 47.Müller L., Riediker M., Wick P., Mohr M., Gehr P., Rothen-Rutishauser B. Release and loss of pneumocytes in co-cultures. Oxidative stress and inflammation response after nanoparticle exposure: Differences between human lung cell monocultures and an advanced three-dimensional model of the human epithelial airways. Toxicol. Vitro. 2009;23:1342–1353. doi: 10.1098/rsif.2009.0161.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karp P.H., Moninger T.O., Weber S.P., Nesselhauf T.S., Launspach J.L., Zabner J., Welsh M.J. An in vitro model of differentiated human airway epithelia. Methods for establishing primary cultures. Methods Mol. Biol. 2002;188:115–137. doi: 10.1385/1-59259-185-X:115. [DOI] [PubMed] [Google Scholar]
- 49.Oh S.M., Kim H.R., Park Y.J., Lee S.Y., Chung K.H. Organic extracts of urban air pollution particulate matter (PM2.5)-induced genotoxicity and oxidative stress in human lung bronchial epithelial cells (BEAS-2B cells) Mutat. Res. 2011;723:142–151. doi: 10.1016/j.mrgentox.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 50.Liu T., Wu B., Wang Y., He H., Lin Z., Tan J., Yang L., Kamp D.W., Zhou X., Tang J., et al. Particulate matter 2.5 induces autophagy via inhibition of the phosphatidylinositol 3-kinase/Akt/mammalian target of rapamycin kinase signaling pathway in human bronchial epithelial cells. Mol. Med. Rep. 2015;12:1914–1922. doi: 10.3892/mmr.2015.3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou W., Tian D., He J., Wang Y., Zhang L., Cui L., Jia L., Zhang L., Li L., Shu Y., et al. Repeated PM2.5 exposure inhibits BEAS-2B cell P53 expression through ROS-Akt-DNMT3B pathway-mediated promoter hypermethylation. Oncotarget. 2016;7:20691–20703. doi: 10.18632/oncotarget.7842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yan Z., Wang J., Li J., Jiang N., Zhang R., Yang W., Yao W., Wu W. Oxidative stress and endocytosis are involved in upregulation of interleukin-8 expression in airway cells exposed to PM2.5. Environ. Toxicol. 2016;31:1869–1878. doi: 10.1002/tox.22188. [DOI] [PubMed] [Google Scholar]
- 53.Lin Y.H., Arashiro M., Clapp P.W., Cui T., Sexton K.G., Vizuete W., Gold A., Jaspers I., Fry R.C., Surratt J.D. Gene Expression Profiling in Human Lung Cells Exposed to Isoprene-Derived Secondary Organic Aerosol. Environ. Sci. Technol. 2017;51:8166–8175. doi: 10.1021/acs.est.7b01967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu T., Zhang X., Zhong L., Cui Q., Hu X., Li B., Wang Z., Dai Y., Zheng Y., Bin P. The use of a 0.20 μm particulate matter filter decreases cytotoxicity in lung epithelial cells following air-liquid interface exposure to motorcycle exhaust. Environ. Pollut. 2017;227:287–295. doi: 10.1016/j.envpol.2017.04.080. [DOI] [PubMed] [Google Scholar]
- 55.Xu Z., Zhang Z., Ma X., Ping F., Zheng X. Effect of PM2.5 on oxidative stress-JAK/STAT signaling pathway of human bronchial epithelial cells. Wei Sheng Yan Jiu. 2015;44:451–455. [PubMed] [Google Scholar]
- 56.Bao Z.J., Fan Y.M., Cui Y.F., Sheng Y.F., Zhu M. Effect of PM2.5 mediated oxidative stress on the innate immune cellular response of Der p1 treated human bronchial epithelial cells. Eur. Rev. Med. Pharmacol. Sci. 2017;21:2907–2912. [PubMed] [Google Scholar]
- 57.Zhou B., Liang G., Qin H., Peng X., Huang J., Li Q., Qing L., Zhang L., Chen L., Ye L., et al. p53-Dependent apoptosis induced in human bronchial epithelial (16-HBE) cells by PM(2.5) sampled from air in Guangzhou, China. Toxicol. Mech. Methods. 2014;24:552–559. doi: 10.3109/15376516.2014.951814. [DOI] [PubMed] [Google Scholar]
- 58.Jin X., Su R., Li R., Song L., Chen M., Cheng L., Li Z. Amelioration of particulate matter-induced oxidative damage by vitamin c and quercetin in human bronchial epithelial cells. Chemosphere. 2016;144:459–466. doi: 10.1016/j.chemosphere.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 59.Abbas I., Verdin A., Escande F., Saint-Georges F., Cazier F., Mulliez P., Courcot D., Shirali P., Gosset P., Garçon G. In vitro short-term exposure to air pollution PM2.5–0.3 induced cell cycle alterations and genetic instability in a human lung cell coculture model. Environ. Res. 2016;147:146–158. doi: 10.1016/j.envres.2016.01.041. [DOI] [PubMed] [Google Scholar]
- 60.Yan J., Lai C.H., Lung S.C., Chen C., Wang W.C., Huang P.I., Lin C.H. Industrial PM2.5 cause pulmonary adverse effect through RhoA/ROCK pathway. Sci. Total Environ. 2017;599–600:1658–1666. doi: 10.1016/j.scitotenv.2017.05.107. [DOI] [PubMed] [Google Scholar]
- 61.Hyseni X., Soukup J.M., Huang Y.C. Pollutant particles induce arginase II in human bronchial epithelial cells. J. Toxicol. Environ. Health A. 2012;75:624–636. doi: 10.1080/15287394.2012.688479. [DOI] [PubMed] [Google Scholar]
- 62.Leclercq B., Platel A., Antherieu S., Alleman L.Y., Hardy E.M., Perdrix E., Grova N., Riffault V., Appenzeller B.M., Happillon M., et al. Genetic and epigenetic alterations in normal and sensitive COPD-diseased human bronchial epithelial cells repeatedly exposed to air pollution-derived PM2.5. Environ. Pollut. 2017;230:163–177. doi: 10.1016/j.envpol.2017.06.028. [DOI] [PubMed] [Google Scholar]
- 63.Loxham M., Morgan-Walsh R.J., Cooper M.J., Blume C., Swindle E.J., Dennison P.W., Howarth P.H., Cassee F.R., Teagle D.A., Palmer M.R., et al. The effects on bronchial epithelial mucociliary cultures of coarse, fine, and ultrafine particulate matter from an underground railway station. Toxicol. Sci. 2015;145:98–107. doi: 10.1093/toxsci/kfv034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pavagadhi S., Betha R., Venkatesan S., Balasubramanian R., Hande M.P. Physicochemical and toxicological characteristics of urban aerosols during a recent Indonesian biomass burning episode. Environ. Sci. Pollut. Res. Int. 2013;20:2569–2578. doi: 10.1007/s11356-012-1157-9. [DOI] [PubMed] [Google Scholar]
- 65.Alessandria L., Schilirò T., Degan R., Traversi D., Gilli G. Cytotoxic response in human lung epithelial cells and ion characteristics of urban-air particles from Torino, a northern Italian city. Environ. Sci. Pollut. Res. Int. 2014;21:5554–5564. doi: 10.1007/s11356-013-2468-1. [DOI] [PubMed] [Google Scholar]
- 66.Bourgeois B., Owens J.W. The influence of Hurricanes Katrina and Rita on the inflammatory cytokine response and protein expression in A549 cells exposed to PM2.5 collected in the Baton Rouge-Port Allen industrial corridor of Southeastern Louisiana in 2005. Toxicol. Mech. Methods. 2014;24:220–242. doi: 10.3109/15376516.2014.881945. [DOI] [PubMed] [Google Scholar]
- 67.Wang Y., Lin Z., Huang H., He H., Yang L., Chen T., Yang T., Ren N., Jiang Y., Xu N., et al. AMPK is required for PM2.5-induced autophagy in human lung epithelial A549 cells. Int. J. Clin. Exp. Med. 2015;8:58–72. [PMC free article] [PubMed] [Google Scholar]
- 68.Liu C.W., Lee T.L., Chen Y.C., Liang C.J., Wang S.H., Lue J.H., Tsai J.S., Lee S.W., Chen S.H., Yang Y.F., et al. PM2.5-induced oxidative stress increases intercellular adhesion molecule-1 expression in lung epithelial cells through the IL-6/AKT/STAT3/NF-κB-dependent pathway. Part. Fibre Toxicol. 2018;15:4. doi: 10.1186/s12989-018-0240-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dou C., Zhang J., Qi C. Cooking oil fume-derived PM2.5 induces apoptosis in A549 cells and MAPK/NF-кB/STAT1 pathway activation. Environ. Sci. Pollut. Res. Int. 2018;25:9940–9948. doi: 10.1007/s11356-018-1262-5. [DOI] [PubMed] [Google Scholar]
- 70.Yang J., Huo T., Zhang X., Ma J., Wang Y., Dong F., Deng J. Oxidative stress and cell cycle arrest induced by short-term exposure to dustfall PM2.5 in A549 cells. Environ. Sci. Pollut. Res. Int. 2017 doi: 10.1007/s11356-017-0430-3. [DOI] [PubMed] [Google Scholar]
- 71.Longhin E., Pezzolato E., Mantecca P., Holme J.A., Franzetti A., Camatini M., Gualtieri M. Season linked responses to fine and quasi-ultrafine Milan PM in cultured cells. Toxicol. Vitro. 2013;27:551–559. doi: 10.1016/j.tiv.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 72.Wei H., Wei D., Yi S., Zhang F., Ding W.J. Oxidative stress induced by urban fine particles in cultured EA.hy926 cells. Hum. Exp. Toxicol. 2011;30:579–590. doi: 10.1177/0960327110374207. [DOI] [PubMed] [Google Scholar]
- 73.Wan Q., Yang Y.P., Liu Z.Y. Puerarin attenuates PM2.5-induced vascular endothelial cells injury via ERK1/2 signaling pathway. Zhongguo Zhong Yao Za Zhi. 2016;41:2309–2314. doi: 10.4268/cjcmm20161223. [DOI] [PubMed] [Google Scholar]
- 74.Wang F.F., Geng C.M., Hao W.D., Zhao Y.D., Li Q., Wang H.M., Qian Y. The Cellular Toxicity of PM2.5 Emitted from Coal Combustion in Human Umbilical Vein Endothelial Cells. Biomed. Environ. Sci. 2016;29:107–116. doi: 10.3967/bes2016.012. [DOI] [PubMed] [Google Scholar]
- 75.Rui W., Guan L., Zhang F., Zhang W., Ding W. PM2.5-induced oxidative stress increases adhesion molecules expression in human endothelial cells through the ERK/AKT/NF-κB-dependent pathway. J. Appl. Toxicol. 2016;36:48–59. doi: 10.1002/jat.3143. [DOI] [PubMed] [Google Scholar]
- 76.Montiel-Dávalos A., Alfaro-Moreno E., López-Marure R. PM2.5 and PM10 induce the expression of adhesion molecules and the adhesion of monocytic cells to human umbilical vein endothelial cells. Inhal. Toxicol. 2007;19(Suppl. 1):91–98. doi: 10.1080/08958370701495212. [DOI] [PubMed] [Google Scholar]
- 77.Cao J., Qin G., Shi R., Bai F., Yang G., Zhang M., Lv J. Overproduction of reactive oxygen species and activation of MAPKs are involved in apoptosis induced by PM2.5 in rat cardiac H9c2 cells. J. Appl. Toxicol. 2016;36:609–617. doi: 10.1002/jat.3249. [DOI] [PubMed] [Google Scholar]
- 78.Jalava P.I., Hirvonen M.R., Sillanpää M., Pennanen A.S., Happo M.S., Hillamo R., Cassee F.R., Gerlofs-Nijland M., Borm P.J., Schins R.P., et al. Associations of urban air particulate composition with inflammatory and cytotoxic responses in RAW 246.7 cell line. Inhal. Toxicol. 2009;21:994–1006. doi: 10.1080/08958370802695710. [DOI] [PubMed] [Google Scholar]
- 79.Daher N., Saliba N.A., Shihadeh A.L., Jaafar M., Baalbaki R., Shafer M.M., Schauer J.J., Sioutas C. Oxidative potential and chemical speciation of size-resolved particulate matter (PM) at near-freeway and urban background sites in the greater Beirut area. Sci. Total Environ. 2014;470–471:417–426. doi: 10.1016/j.scitotenv.2013.09.104. [DOI] [PubMed] [Google Scholar]
- 80.Cavanagh J.A., Trought K., Brown L., Duggan S. Exploratory investigation of the chemical characteristics and relative toxicity of ambient air particulates from two New Zealand cities. Sci. Total Environ. 2009;407:5007–5518. doi: 10.1016/j.scitotenv.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 81.He M., Ichinose T., Kobayashi M., Arashidani K., Yoshida S., Nishikawa M., Takano H., Sun G., Shibamoto T. Differences in allergic inflammatory responses between urban PM2.5 and fine particle derived from desert-dust in murine lungs. Toxicol. Appl. Pharmacol. 2016;297:41–55. doi: 10.1016/j.taap.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 82.He M., Ichinose T., Yoshida S., Ito T., He C., Yoshida Y., Arashidani K., Takano H., Sun G., Shibamoto T. PM2.5-induced lung inflammation in mice: Differences of inflammatory response in macrophages and type II alveolar cells. J. Appl. Toxicol. 2017;37:1203–1218. doi: 10.1002/jat.3482. [DOI] [PubMed] [Google Scholar]
- 83.Liu X.C., Li Y.J., Wang Y.J., Li Q., Yang Q., Weng X.G., Chen Y., Cai W.Y., Guo Y., Kan X.X., et al. Protection of Shenlian extracts to PM2.5 infected RAW 264.7 cell damage. Zhongguo Zhong Yao Za Zhi. 2015;40:1977–1983. [PubMed] [Google Scholar]
- 84.Xu F., Qiu X., Hu X., Shang Y., Pardo M., Fang Y., Wang J., Rudich Y., Zhu T. Effects on IL-1β signaling activation induced by water and organic extracts of fine particulate matter (PM2.5) in vitro. Environ. Pollut. 2018;237:592–600. doi: 10.1016/j.envpol.2018.02.086. [DOI] [PubMed] [Google Scholar]
- 85.Castañeda A.R., Pinkerton K.E., Bein K.J., Magaña-Méndez A., Yang H.T., Ashwood P., Vogel C.F.A. Ambient particulate matter activates the aryl hydrocarbon receptor in dendritic cells and enhances Th17 polarization. Toxicol. Lett. 2018;292:85–96. doi: 10.1016/j.toxlet.2018.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sun Q., Wang A., Jin X., Natanzon A., Duquaine D., Brook R.D., Aguinaldo J.G., Fayad Z.A., Fuster V., Lippmann M., et al. Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. J. Am. Med. Assoc. 2005;294:3003–3010. doi: 10.1001/jama.294.23.3003. [DOI] [PubMed] [Google Scholar]
- 87.Gavett S.H., Haykal-Coates N., Copeland L.B., Heinrich J., Gilmour M.I. Metal composition of ambient PM2.5 influences severity of allergic airways disease in mice. Environ. Health. Perspect. 2003;111:1471–1477. doi: 10.1289/ehp.6300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Reymão M.S., Cury P.M., Lichtenfels A.J., Lemos M., Battlehner C.N., Conceição G.M., Capelozzi V.L., Montes G.S., Júnior M.F., Martins M.A., et al. Urban air pollution enhances the formation of urethane-induced lung tumors in mice. Environ. Res. 1997;74:150–158. doi: 10.1006/enrs.1997.3740. [DOI] [PubMed] [Google Scholar]
- 89.Driscoll K.E., Costa D.L., Hatch G., Henderson R., Oberdorster G., Salem H., Schlesinger R.B. Intratracheal instillation as an exposure technique for the evaluation of respiratory tract toxicity: Uses and limitations. Toxicol. Sci. 2000;55:24–35. doi: 10.1093/toxsci/55.1.24. [DOI] [PubMed] [Google Scholar]
- 90.Morimoto Y., Izumi H., Yoshiura Y., Fujishima K., Yatera K., Yamamoto K. Usefulness of Intratracheal Instillation Studies for Estimating Nanoparticle-Induced Pulmonary Toxicity. Int. J. Mol. Sci. 2016;17:165. doi: 10.3390/ijms17020165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Habre R., Moshier E., Castro W., Nath A., Grunin A., Rohr A., Godbold J., Schachter N., Kattan M., Coull B., et al. The effects of PM2.5 and its components from indoor and outdoor sources on cough and wheeze symptoms in asthmatic children. J. Expo. Sci. Environ. Epidemiol. 2014;24:380–387. doi: 10.1038/jes.2014.21. [DOI] [PubMed] [Google Scholar]
- 92.Duan Z., Du F.Y., Yuan Y.D., Zhang Y.P., Yang H.S., Pan W.S. Effects of PM2.5 exposure on Klebsiella pneumoniae clearance in the lungs of rats. Zhonghua Jie He He Hu Xi Za Zhi. 2013;36:836–840. [PubMed] [Google Scholar]
- 93.Jacobson Lda S., Hacon Sde S., Castro H.A., Ignotti E., Artaxo P., Ponce de Leon A.C. Association between fine particulate matter and the peak expiratory flow of schoolchildren in the Brazilian subequatorial Amazon: A panel study. Environ. Res. 2012;117:27–35. doi: 10.1016/j.envres.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 94.Wu S., Deng F., Hao Y., Shima M., Wang X., Zheng C., Wei H., Lv H., Lu X., Huang J., et al. Chemical constituents of fine particulate air pollution and pulmonary function in healthy adults: The healthy volunteer natural relocation study. J. Hazard. Mater. 2013;260:183–191. doi: 10.1016/j.jhazmat.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 95.Nachman K.E., Parker J.D. Exposures to fine particulate air pollution and respiratory outcomes in adults using two national datasets: A cross-sectional study. Environ. Health. 2012;11:25. doi: 10.1186/1476-069X-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tsai S.S., Chang C.C., Yang C.Y. Fine particulate air pollution and hospital admissions for chronic obstructive pulmonary disease: A case-crossover study in Taipei. Int. J. Environ. Res. Public Health. 2013;10:6015–6026. doi: 10.3390/ijerph10116015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jung K.H., Hsu S.I., Yan B., Moors K., Chillrud S.N., Ross J., Wang S., Perzanowski M.S., Kinney P.L., Whyatt R.M., et al. Childhood exposure to fine particulate matter and black carbon and the development of new wheeze between ages 5 and 7 in an urban prospective cohort. Environ. Int. 2012;45:44–50. doi: 10.1016/j.envint.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vempilly J., Abejie B., Diep V., Gushiken M., Rawat M., Tyner T.R. The synergetic effect of ambient PM2.5 exposure and rhinovirus infection in airway dysfunction in asthma: A pilot observational study from the Central Valley of California. Exp. Lung Res. 2013;39:434–440. doi: 10.3109/01902148.2013.840693. [DOI] [PubMed] [Google Scholar]
- 99.Gurley E.S., Homaira N., Salje H., Ram P.K., Haque R., Petri W., Bresee J., Moss W.J., Breysse P., Luby S.P., et al. Indoor exposure to particulate matter and the incidence of acute lower respiratory infections among children: A birth cohort study in urban Bangladesh. Indoor Air. 2013;23:379–386. doi: 10.1111/ina.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kanner R.E., Connett J.E., Altose M.D., Buist A.S., Lee W.W., Tashkin D.P., Wise R.A. Gender difference in airway hyperresponsiveness in smokers with mild COPD. The Lung Health Study. Am. J. Respir. Crit. Care Med. 1994;150:956–961. doi: 10.1164/ajrccm.150.4.7921469. [DOI] [PubMed] [Google Scholar]
- 101.Hsu H.H., Chiu Y.H., Coull B.A., Kloog I., Schwartz J., Lee A., Wright R.O., Wright R.J. Prenatal Particulate Air Pollution and Asthma Onset in Urban Children. Identifying Sensitive Windows and Sex Differences. Am. J. Respir. Crit. Care Med. 2015;192:1052–1059. doi: 10.1164/rccm.201504-0658OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hwang S.S., Kang S., Lee J.Y., Lee J.S., Kim H.J., Han S.K., Yim J.J. Impact of outdoor air pollution on the incidence of tuberculosis in the Seoul metropolitan area, South Korea. Korean J. Intern. Med. 2014;29:183–190. doi: 10.3904/kjim.2014.29.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Barregard L., Sällsten G., Andersson L., Almstrand A.C., Gustafson P., Andersson M., Olin A.C. Experimental exposure to wood smoke: Effects on airway inflammation and oxidative stress. Occup. Environ. Med. 2008;65:319–324. doi: 10.1136/oem.2006.032458. [DOI] [PubMed] [Google Scholar]
- 104.Muala A., Rankin G., Sehlstedt M., Unosson J., Bosson J.A., Behndig A., Pourazar J., Nyström R., Pettersson E., Bergvall C., et al. Acute exposure to wood smoke from incomplete combustion—Indications of cytotoxicity. Part. Fibre Toxicol. 2015;12:33. doi: 10.1186/s12989-015-0111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Migliaccio C.T., Kobos E., King Q.O., Porter V., Jessop F., Ward T. Adverse effects of wood smoke PM2.5 exposure on macrophage functions. Inhal. Toxicol. 2013;25:67–76. doi: 10.3109/08958378.2012.756086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Riva D.R., Magalhães C.B., Lopes A.A., Lanças T., Mauad T., Malm O., Valença S.S., Saldiva P.H., Faffe D.S., Zin W.A., et al. Low dose of fine particulate matter (PM2.5) can induce acute oxidative stress, inflammation and pulmonary impairment in healthy mice. Inhal. Toxicol. 2011;23:257–267. doi: 10.3109/08958378.2011.566290. [DOI] [PubMed] [Google Scholar]
- 107.Lin C.I., Tsai C.H., Sun Y.L., Hsieh W.Y., Lin Y.C., Chen C.Y., Lin C.S. Instillation of particulate matter 2.5 induced acute lung injury and attenuated the injury recovery in ACE2 knockout mice. Int. J. Biol. Sci. 2018;14:253–265. doi: 10.7150/ijbs.23489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Haberzettl P., O’Toole T.E., Bhatnagar A., Conklin D.J. Exposure to Fine Particulate Air Pollution Causes Vascular Insulin Resistance by Inducing Pulmonary Oxidative Stress. Environ. Health Perspect. 2016;124:1830–1839. doi: 10.1289/EHP212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang R., Xiao X., Cao L., Shen Z.X., Lei Y., Cao Y.X. Airborne fine particulate matter induces an upregulation of endothelin receptors on rat bronchi. Environ. Pollut. 2016;209:11–20. doi: 10.1016/j.envpol.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 110.Zhao H., Yang B., Xu J., Chen D.M., Xiao C.L. PM2.5-induced alterations of cell cycle associated gene expression in lung cancer cells and rat lung tissues. Environ. Toxicol. Pharmacol. 2017;52:77–82. doi: 10.1016/j.etap.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 111.Luo B., Shi H., Wang L., Shi Y., Wang C., Yang J., Wan Y., Niu J. Rat lung response to PM2.5 exposure under different cold stresses. Int. J. Environ. Res. Public Health. 2014;11:12915–12926. doi: 10.3390/ijerph111212915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Huang N.H., Wang Q., Xu D.Q. Immunological effect of PM2.5 on cytokine production in female Wistar rats. Biomed. Environ. Sci. 2008;2:63–68. doi: 10.1016/S0895-3988(08)60008-2. [DOI] [PubMed] [Google Scholar]
- 113.Zhao C., Liao J., Chu W., Wang S., Yang T., Tao Y. Involvement of TLR2 and TLR4 and Th1/Th2 shift in inflammatory responses induced by fine ambient particulate matter in mice. Inhal. Toxicol. 2012;24:918–927. doi: 10.3109/08958378.2012.731093. [DOI] [PubMed] [Google Scholar]
- 114.Li R., Kou X., Geng H., Xie J., Yang Z., Zhang Y., Cai Z., Dong C. Effect of ambient PM(2.5) on lung mitochondrial damage and fusion/fission gene expression in rats. Chem. Res. Toxicol. 2015;28:408–418. doi: 10.1021/tx5003723. [DOI] [PubMed] [Google Scholar]
- 115.Tang W., Du L., Sun W., Yu Z., He F., Chen J., Li X., Yu L., Chen D. Maternal exposure to fine particulate air pollution induces epithelial-to-mesenchymal transition resulting in postnatal pulmonary dysfunction mediated by transforming growth factor-β/Smad3 signaling. Toxicol. Lett. 2017;267:11–20. doi: 10.1016/j.toxlet.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 116.Hsieh Y.L., Tsai S.S., Yang C.Y. Fine particulate air pollution and hospital admissions for congestive heart failure: A case-crossover study in Taipei. Inhal. Toxicol. 2013;25:455–460. doi: 10.3109/08958378.2013.804609. [DOI] [PubMed] [Google Scholar]
- 117.Madrigano J., Kloog I., Goldberg R., Coull B.A., Mittleman M.A., Schwartz J. Long-term exposure to PM2.5 and incidence of acute myocardial infarction. Environ. Health Perspect. 2013;121:192–196. doi: 10.1289/ehp.1205284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bell M.L., Ebisu K., Leaderer B.P., Gent J.F., Lee H.J., Koutrakis P., Wang Y., Dominici F., Peng R.D. Associations of PM2.5 constituents and sources with hospital admissions: Analysis of four counties in Connecticut and Massachusetts (USA) for persons ≥ 65 years of age. Environ. Health Perspect. 2014;122:138–144. doi: 10.1289/ehp.1306656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Prisby R.D., Muller-Delp J., Delp M.D., Nurkiewicz T.R. Age, gender, and hormonal status modulate the vascular toxicity of the diesel exhaust extract phenanthraquinone. J. Toxicol. Environ. Health A. 2008;71:464–470. doi: 10.1080/15287390701839349. [DOI] [PubMed] [Google Scholar]
- 120.Zhao L., Liang H.R., Chen F.Y., Chen Z., Guan W.J., Li J.H. Association between air pollution and cardiovascular mortality in China: A systematic review and meta-analysis. Oncotarget. 2017;8:66438–66448. doi: 10.18632/oncotarget.20090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Barregard L., Sällsten G., Gustafson P., Andersson L., Johansson L., Basu S., Stigendal L. Experimental exposure to wood-smoke particles in healthy humans: Effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 2006;18:845–853. doi: 10.1080/08958370600685798. [DOI] [PubMed] [Google Scholar]
- 122.Croft D.P., Cameron S.J., Morrell C.N., Lowenstein C.J., Ling F., Zareba W., Hopke P.K., Utell M.J., Thurston S.W., Thevenet-Morrison K., et al. Associations between ambient wood smoke and other particulate pollutants and biomarkers of systemic inflammation, coagulation and thrombosis in cardiac patients. Environ. Res. 2017;154:352–361. doi: 10.1016/j.envres.2017.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Xie Y., Zhang X., Tian Z., Jiang R., Chen R., Song W., Zhao J. Preexposure to PM2.5 exacerbates acute viral myocarditis associated with Th17 cell. Int. J. Cardiol. 2013;168:3837–3845. doi: 10.1016/j.ijcard.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 124.Xie Y., Gong C., Bo L., Jiang S., Kan H., Song W., Zhao J., Li Y. Treg responses are associated with PM2.5-induced exacerbation of viral myocarditis. Inhal. Toxicol. 2015;27:281–286. doi: 10.3109/08958378.2015.1040139. [DOI] [PubMed] [Google Scholar]
- 125.Zhao J., Liu C., Bai Y., Wang T.Y., Kan H., Sun Q. IKK inhibition prevents PM2.5-exacerbated cardiac injury in mice with type 2 diabetes. J. Environ. Sci. (China) 2015;31:98–103. doi: 10.1016/j.jes.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 126.Chen L.C., Hwang J.S., Lall R., Thurston G., Lippmann M. Alteration of cardiac function in ApoE−/− mice by subchronic urban and regional inhalation exposure to concentrated ambient PM2.5. Inhal. Toxicol. 2010;22:580–592. doi: 10.3109/08958371003596579. [DOI] [PubMed] [Google Scholar]
- 127.Pei Y., Jiang R., Zou Y., Wang Y., Zhang S., Wang G., Zhao J., Song W. Effects of Fine Particulate Matter (PM2.5) on Systemic Oxidative Stress and Cardiac Function in ApoE(−/−) Mice. Int. J. Environ. Res. Public Health. 2016;13:484. doi: 10.3390/ijerph13050484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wan Q., Cui X., Shao J., Zhou F., Jia Y., Sun X., Zhao X., Chen Y., Diao J., Zhang L. Beijing ambient particle exposure accelerates atherosclerosis in ApoE knockout mice by upregulating visfatin expression. Cell Stress Chaperones. 2014;19:715–724. doi: 10.1007/s12192-014-0499-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rao X., Zhong J., Maiseyeu A., Gopalakrishnan B., Villamena F.A., Chen L.C., Harkema J.R., Sun Q., Rajagopalan S. CD36-dependent 7-ketocholesterol accumulation in macrophages mediates progression of atherosclerosis in response to chronic air pollution exposure. Circ. Res. 2014;115:770–780. doi: 10.1161/CIRCRESAHA.115.304666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sancini G., Farina F., Battaglia C., Cifola I., Mangano E., Mantecca P., Camatini M., Palestini P. Health risk assessment for air pollutants: Alterations in lung and cardiac gene expression in mice exposed to Milano winter fine particulate matter (PM2.5) PLoS ONE. 2014;9:e109685. doi: 10.1371/journal.pone.0109685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wang G., Jiang R., Zhao Z., Song W. Effects of ozone and fine particulate matter (PM(2.5)) on rat system inflammation and cardiac function. Toxicol. Lett. 2013;217:23–33. doi: 10.1016/j.toxlet.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 132.Wagner J.G., Allen K., Yang H.Y., Nan B., Morishita M., Mukherjee B., Dvonch J.T., Spino C., Fink G.D., Rajagopalan S., et al. Cardiovascular depression in rats exposed to inhaled particulate matter and ozone: Effects of diet-induced metabolic syndrome. Environ. Health Perspect. 2014;122:27–33. doi: 10.1289/ehp.1307085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Li R., Kou X., Geng H., Xie J., Tian J., Cai Z., Dong C. Mitochondrial damage: An important mechanism of ambient PM2.5 exposure-induced acute heart injury in rats. J. Hazard. Mater. 2015;287:392–401. doi: 10.1016/j.jhazmat.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 134.Xiao X., Cao L., Wang R., Shen Z.X., Cao Y.X. Airborne fine particulate matter alters the expression of endothelin receptors in rat coronary arteries. Environ. Pollut. 2016;218:487–496. doi: 10.1016/j.envpol.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 135.Zhang C., Meng Q., Zhang X., Wu S., Wang S., Chen R., Li X. Role of astrocyte activation in fine particulate matter-enhancement of existing ischemic stroke in Sprague-Dawley male rats. J. Toxicol. Environ. Health A. 2016;79:393–401. doi: 10.1080/15287394.2016.1176615. [DOI] [PubMed] [Google Scholar]
- 136.Reis M.A., Carvalho A., Taborda A., Quaresma A., Dias G., Alves L.C., Mota M., Chaves P.C., Teixeira R., Rodrigues P.O. High airborne PM2.5 chlorine concentrations link to diabetes surge in Portugal. Sci. Total Environ. 2009;407:5726–5734. doi: 10.1016/j.scitotenv.2009.07.029. [DOI] [PubMed] [Google Scholar]
- 137.Brook R.D., Xu X., Bard R.L., Dvonch J.T., Morishita M., Kaciroti N., Sun Q., Harkema J., Rajagopalan S. Reduced Metabolic Insulin Sensitivity Following Sub-acute Exposures to Low Levels of Ambient Fine Particulate Matter Air Pollution. Sci. Total Environ. 2013;448:66–71. doi: 10.1016/j.scitotenv.2012.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Chen H., Burnett R.T., Kwong J.C., Villeneuve P.J., Goldberg M.S., Brook R.D., van Donkelaar A., Jerrett M., Martin R.V., Brook J.R., et al. Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario, Canada. Environ. Health Perspect. 2013;121:804–810. doi: 10.1289/ehp.1205958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Solimini A.G., D’Addario M., Villari P. Ecological correlation between diabetes hospitalizations and fine particulate matter in Italian provinces. BMC Public Health. 2015;15:708. doi: 10.1186/s12889-015-2018-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Stewart J.C., Chalupa D.C., Devlin R.B., Frasier L.M., Huang L.S., Little E.L., Lee S.M., Phipps R.P., Pietropaoli A.P., Taubman M.B., et al. Vascular effects of ultrafine particles in persons with type 2 diabetes. Environ. Health Perspect. 2010;118:1692–1698. doi: 10.1289/ehp.1002237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xu X., Liu C., Xu Z., Tzan K., Zhong M., Wang A., Lippmann M., Chen L.C., Rajagopalan S., Sun Q. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol. Sci. 2011;124:88–98. doi: 10.1093/toxsci/kfr211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Haberzettl P., McCracken J.P., Bhatnagar A., Conklin D.J. Insulin sensitizers prevent fine particulate matter-induced vascular insulin resistance and changes in endothelial progenitor cell homeostasis. Am. J. Physiol. Heart Circ. Physiol. 2016;310:1423–1438. doi: 10.1152/ajpheart.00369.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Mendez R., Zheng Z., Fan Z., Rajagopalan S., Sun Q., Zhang K. Exposure to fine airborne particulate matter induces macrophage infiltration, unfolded protein response, and lipid deposition in white adipose tissue. Am. J. Transl. Res. 2013;5:224–234. [PMC free article] [PubMed] [Google Scholar]
- 144.Liu C., Xu X., Bai Y., Wang T.Y., Rao X., Wang A., Sun L., Ying Z., Gushchina L., Maiseyeu A., et al. Air pollution-mediated susceptibility to inflammation and insulin resistance: Influence of CCR2 pathways in mice. Environ. Health Perspect. 2014;122:17–26. doi: 10.1289/ehp.1306841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Goettems-Fiorin P.B., Grochanke B.S., Baldissera F.G., Dos Santos A.B., Homem de Bittencourt P.I., Jr., Ludwig M.S. Fine particulate matter potentiates type 2 diabetes development in high-fat diet-treated mice: Stress response and extracellular to intracellular HSP70 ratio analysis. J. Physiol. Biochem. 2016;72:643–656. doi: 10.1007/s13105-016-0503-7. [DOI] [PubMed] [Google Scholar]
- 146.Yan Y.H., C-K Chou C., Wang J.S., Tung C.L., Li Y.R., Lo K., Cheng T.J. Subchronic effects of inhaled ambient particulate matter on glucose homeostasis and target organ damage in a type 1 diabetic rat model. Toxicol. Appl. Pharmacol. 2014;281:211–220. doi: 10.1016/j.taap.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 147.Aztatzi-Aguilar O.G., Uribe-Ramírez M., Narváez-Morales J., De Vizcaya-Ruiz A., Barbier O. Early kidney damage induced by subchronic exposure to PM2.5 in rats. Part. Fibre Toxicol. 2016;13:68. doi: 10.1186/s12989-016-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lu X., Ye Z., Zheng S., Ren H., Zeng J., Wang X., Jose P.A., Chen K., Zeng C. Long-Term Exposure of Fine Particulate Matter Causes Hypertension by Impaired Renal D1 Receptor-Mediated Sodium Excretion via Upregulation of G-Protein-Coupled Receptor Kinase Type 4 Expression in Sprague-Dawley Rats. J. Am. Heart Assoc. 2018;7:e007185. doi: 10.1161/JAHA.117.007185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yi L., Wei C., Fan W. Fine-particulate matter (PM2.5), a risk factor for rat gestational diabetes with altered blood glucose and pancreatic GLUT2 expression. Gynecol. Endocrinol. 2017;33:611–616. doi: 10.1080/09513590.2017.1301923. [DOI] [PubMed] [Google Scholar]
- 150.Granum B., Lovik M. The effect of particles on allergic immune responses. Toxicol. Sci. 2002;65:7–17. doi: 10.1093/toxsci/65.1.7. [DOI] [PubMed] [Google Scholar]
- 151.Heo Y., Saxon A., Hankinson O. Effect of diesel exhaust particles and their components on the allergen-specific IgE and IgG1 response in mice. Toxicology. 2001;159:143–158. doi: 10.1016/S0300-483X(00)00418-2. [DOI] [PubMed] [Google Scholar]
- 152.Siegel P., Saxena R., Saxena Q.B., Ma J., Ma J., Yin X.J., Castranova V., Al Humadi N., Lewis D. Effect of diesel exhaust particulate (DEP) on immune responses: Contributions of particulate versus organic soluble components. J. Toxicol. Environ. Health A. 2004;67:221–231. doi: 10.1080/15287390490266891. [DOI] [PubMed] [Google Scholar]
- 153.Van Zijverden M., van der Pijl A., Bol M., van Pinxteren F.A., de Haar C., Penninks A.H., van Loveren H., Pieters R. Diesel exhaust, carbon black, and silica particles display distinct Th1/Th2 modulating activity. Toxicol. Appl. Pharmacol. 2000;168:131–139. doi: 10.1006/taap.2000.9013. [DOI] [PubMed] [Google Scholar]
- 154.Lambert A.L., Dong W., Selgrade M.K., Gilmour M.I. Enhanced allergic sensitization by residual oil fly ash particles is mediated by soluble metal constituents. Toxicol. Appl. Pharmacol. 2000;165:84–93. doi: 10.1006/taap.2000.8932. [DOI] [PubMed] [Google Scholar]
- 155.Ogino K., Zhang R., Takahashi H., Takemoto K., Kubo M., Murakami I., Wang D.H., Fujikura Y. Allergic airway inflammation by nasal inoculation of particulate matter (PM2.5) in NC/Nga mice. PLoS ONE. 2014;9:e92710. doi: 10.1371/journal.pone.0092710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhang X., Zhong W., Meng Q., Lin Q., Fang C., Huang X., Li C., Huang Y., Tan J. Ambient PM2.5 exposure exacerbates severity of allergic asthma in previously sensitized mice. J. Asthma. 2015;52:785–794. doi: 10.3109/02770903.2015.1036437. [DOI] [PubMed] [Google Scholar]
- 157.Song J., Kang J., Lin B., Li J., Zhu Y., Du J., Yang X., Xi Z., Li R. Mediating Role of TRPV1 Ion Channels in the Co-exposure to PM2.5 and Formaldehyde of Balb/c Mice Asthma Model. Sci. Rep. 2017;7:11926. doi: 10.1038/s41598-017-11833-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Liu Y., Feng G.Z., Du Q., Jin X.X., Du X.R. Fine particulate matter aggravates allergic airway inflammation through thymic stromal lymphopoietin activation in mice. Mol. Med. Rep. 2017;16:4201–4207. doi: 10.3892/mmr.2017.7089. [DOI] [PubMed] [Google Scholar]
- 159.Zhang J., Fulgar C.C., Mar T., Young D.E., Zhang Q., Bein K.J., Cui L., Castañeda A., Vogel C.F.A., Sun X., et al. TH17-induced neutrophils enhance the pulmonary allergic response following BALB/c exposure to house dust mite allergen and fine particulate matter from California and China. Toxicol. Sci. 2018 doi: 10.1093/toxsci/kfy127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Falcon-Rodriguez C.I., De Vizcaya-Ruiz A., Rosas-Pérez I.A., Osornio-Vargas Á.R., Segura-Medina P. Inhalation of concentrated PM2.5 from Mexico City acts as an adjuvant in a guinea pig model of allergic asthma. Environ. Pollut. 2017;228:474–483. doi: 10.1016/j.envpol.2017.05.050. [DOI] [PubMed] [Google Scholar]