Abstract
We report the case of a 44-year-old school teacher who experienced long-term relief from tension-type headache (TTH) and major depression following chiropractic treatment. It is well recognized that psychiatric comorbidity and suicide risk are commonly found in patients with painful physical symptoms such as chronic headache, backache, or joint pain. Recent studies indicated that autonomic dysfunction plays a role in the pathogenesis of TTHs and depressive disorders. The autonomic nervous system is mainly controlled by reflex centers located in the spinal cord, brain stem, and hypothalamus. This report highlights the rewarding outcomes from spinal adjustment in certain neuropsychiatric disorders. Long-term results of chiropractic adjustment in this particular case were very favorable. Further studies with larger groups are warranted to better clarify the role of chiropractic.
Keywords: Autonomic nerve system, chiropractic, depression, headache, spinal adjustment
Introduction
At one time, sustained muscular spasm of pain-sensitive structures of the cranium was assumed to be the primary cause of tension-type headache (TTH). More recent research suggests that the core cause of TTH resides in the autonomic nervous system.[1] Autonomic dysregulation has also been considered to play a role in the pathogenesis of depressive disorders.[2] Sympathetic reflex centers are located in the T1 to L2 segments of the spinal cord. Parasympathetic reflex centers are associated with the nuclei of cranial nerves (III, VII, IX, and X) and with sacral spinal cord. Recent studies provide preliminary evidence that cervical adjustments may result dominantly in parasympathetic responses, whereas thoracic adjustments result dominantly in sympathetic responses.[3,4] In association to the particular segment(s) adjusted it appears that these responses may lead to some therapeutic outcomes in certain neuropsychiatric disorders.[3]
Case Report
A 44-year-old, single, woman presented to the chiropractic office with ongoing headaches of 2-year duration. Her headaches were on a daily basis and varied in intensity. The pain was described as disabling, going across the forehead, to her nuchal area and right shoulder. She could not maintain daily activities without acetaminophen and aspirin. The patient initially consulted her family physician to rule out possible pathological causes. Her blood tests, brain magnetic resonance imaging, and cervical radiographs all came back unremarkable. She was diagnosed with TTH and then sent for physiotherapy a couple of times, but it did not help. She had also tried acupuncture, traditional Chinese therapy, and alternative medications for quite some time; but nothing had changed her headache pattern. She worked as a primary school teacher and lived alone. She denied substance abuse or any systemic disorder. There was no family history of mental illness.
Sometime later, she started experiencing episodes of extreme low moods, characterized by feelings of overwhelming sadness and seeking an immediate sense of relief. She was referred to the psychiatry services and was diagnosed with a major depressive disorder without psychotic features. Over the past 6 months, a combination of Deanxit (Flupentixol + Melitracen) for treating depression, alprazolam for anxiety, and acetaminophen for pain had been used at different doses at different times. Both disabling headache and severe depression led to impair her job and regular activities. Under stress of health and financial impacts, she had recurrent thoughts of death. She reported that she had once been getting ready for charcoal-burning to end her life at home. A primary concern for her was ending of troubles at all.
For evaluation and treatment of neck pain and headache, the patient presented to our clinic with a guarded neck posture. She rated her peak headache intensity to be 6–8/10 on the numeric pain rating scale. Spinal ranges of motion indicated restricted in the lower cervical and upper thoracic segments. Palpation revealed spasm of the sternocleidomastoid, suboccipital and cervical paraspinal muscles. Neurological findings of both upper extremities were unremarkable. Radiographs demonstrated mild osteophytes at lower cervical vertebrae and straightened cervical spine of 24° (normal range: 31°–40°) [Figure 1a]. She was diagnosed with cervical spondylosis and TTH. The strategy of chiropractic approach was to stretch and relax the spastic muscles, restore the motion in the respective segments, and rehabilitate sensorimotor integration through neuromuscular facilitations, including diversified spinal manipulation, ultrasound vibration therapy, and home heat pack.
Figure 1.
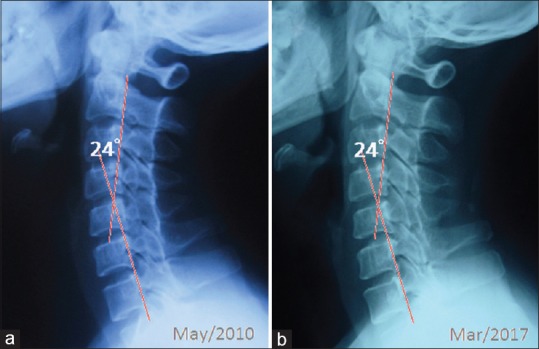
(a) Cervical radiographs showed a slightly straightened cervical spine of 24° (normal range: 31°–40°) and mild osteophytes at lower cervical vertebrae. (b) Cervical radiographs taken at 7-year follow-up revealed integrity of the joint and disk, and ruled out any pathology
The treatment was commenced 5 times for the 1st week and then shifted to 3 times weekly for the next 3 months. After 3 months, the patient regained confidence in her health and started reducing the dose of medications. She rated her headache as 3–5/10 on the pain scale. The second phase of chiropractic treatment was performed twice a week for another 3 months to restore functions of the spine. All of her symptoms disappeared, and she was able to discontinue all medications after 6 months of adjustment. Sometimes, the patient experienced sharp head pain around the menstrual periods which would eventually be relieved by rest. Having enjoyed headache free and mood stability over the past 6 years, the patient continued maintenance care on a monthly basis. Cervical radiographs taken at 7-year follow-up revealed integrity of the joint and disk and ruled out any pathology [Figure 1b].
Discussion
Chronic pain and depression can influence one another through complex webs of connections. The autonomic nervous system is one of the major neural pathways activated by chronic stress.[2,5] Under the influence of chronic stress, such as backache or headache, the sympathetic nervous system is continuously provoked without parasympathetic counteraction appropriately. As a result, increased epinephrine and norepinephrine levels can incite an increase of proinflammatory cytokines, which can cause the downstream kynurenine metabolites to rise. This neuroinflammation can exert neurotoxic changes in the brain with the pathophysiology of depression.[2] The link between pain and depression also appears to be a shared neurologic pathway.
The biochemical theory of depression assumes that depression is caused by an imbalance or a functional deficiency of key neurotransmitters (serotonin, norepinephrine, and dopamine).[6] Dysregulation of these transmitters is linked to both depression and pain.[7] Drugs that specifically inhibit the reuptake of both serotonin and norepinephrine are widely prescribed as a first-line treatment for depression and painful physical symptoms.[7] Elevated levels of serotonin often result in the relief of depression and anxiety, as well as substantial reduction in pain sensitivity. Antidepressant drugs, such as Melitracen (a tricyclic antidepressant component of Deanxit), as prescribed for this patient, may increase levels of neurotransmitters within the brain and correct the imbalance of neurotransmitters. The Flupentixol (an antipsychotic component of Deanxit) inhibits dopamine-mediated effects by blocking postsynaptic dopamine receptors in the central nervous system.
Recent studies are finding that chiropractic care is a way to reduce the frequency of pain, and the duration and intensity of headaches. A study of 62 women with tension headaches, the authors found that, when compared to the control, the individuals who engaged in spinal adjustment showed improvements in their physical role, bodily pain, and social functioning 1 month after treatment.[8] In a trial comparing spinal adjustments with the use of amitriptyline (Elavil®) in the treatment of TTHs, study participants in both groups showed improvement, but those who received spinal adjustments had longer lasting benefits.[9] A mechanical slack of the pericranial tissues and a consistent reflex both in local and distant muscles inducing by spinal adjustment were assumed to be the therapeutic mechanism.[8] According to the acknowledgment that autonomic dysfunction correlates with TTH[1] and depression,[5] the biological mechanism of spinal adjustment, as seen in our case, should have related to parasympathetic response. Nevertheless, better pain control from chiropractic care might be further beneficial for reducing depressive mood.
The main limitation of this case report is that the causes of TTH and depression are still uncertain, and our speculation for chiropractic effect is based on the inclusion of clinical possibilities. A single case report is not proof of concept, but the patient's experience is supportive. Second, the patient did not want further monitoring her mental condition, and subsequent measures for depressive symptoms are lacking. Eventually, long-term outcomes of chiropractic adjustment in this particular case were very favorable. The application of chiropractic services appeared helpful for some neuropsychiatric disorders.
Conclusion
This case report describes a long-term relief from chronic headache and improvement in depression with chiropractic in a school teacher. The application of chiropractic services appeared helpful to the outcome of some neuropsychiatric disorders. Further researches to better clarify the role of chiropractic are warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yerdelen D, Acil T, Goksel B, Karataş M. Autonomic function in tension-type headache. Acta Neurol Belg. 2007;107:108–11. [PubMed] [Google Scholar]
- 2.Kim YK, Won E. The influence of stress on neuroinflammation and alterations in brain structure and function in major depressive disorder. Behav Brain Res. 2017;329:6–11. doi: 10.1016/j.bbr.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 3.Welch A, Boone R. Sympathetic and parasympathetic responses to specific diversified adjustments to chiropractic vertebral subluxations of the cervical and thoracic spine. J Chiropr Med. 2008;7:86–93. doi: 10.1016/j.jcm.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Win NN, Jorgensen AM, Chen YS, Haneline MT. Effects of upper and lower cervical spinal manipulative therapy on blood pressure and heart rate variability in volunteers and patients with neck pain: A Randomized controlled, cross-over, preliminary study. J Chiropr Med. 2015;14:1–9. doi: 10.1016/j.jcm.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Won E, Kim YK. Stress, the autonomic nervous system, and the immune-kynurenine pathway in the etiology of depression. Curr Neuropharmacol. 2016;14:665–73. doi: 10.2174/1570159X14666151208113006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med. 2003;163:2433–45. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 7.Trivedi MH. The link between depression and physical symptoms. Prim Care Companion J Clin Psychiatry. 2004;6:12–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Espí-López GV, Rodríguez-Blanco C, Oliva-Pascual-Vaca A, Molina-Martínez F, Falla D. Do manual therapy techniques have a positive effect on quality of life in people with tension-type headache? A randomized controlled trial. Eur J Phys Rehabil Med. 2016;52:447–56. [PubMed] [Google Scholar]
- 9.Boline PD, Kassak K, Bronfort G, Nelson C, Anderson AV. Spinal manipulation vs.amitriptyline for the treatment of chronic tension-type headaches: A randomized clinical trial. J Manipulative Physiol Ther. 1995;18:148–54. [PubMed] [Google Scholar]


