Abstract
In this paper, we examine patterns of self-reported diagnosis of noncommunicable diseases (NCDs) and prevalences of algorithm/measured test-based, undiagnosed, and untreated NCDs in China, Ghana, India, Mexico, Russia, and South Africa. Nationally representative samples of older adults aged ≥50 years were analyzed from wave 1 of the World Health Organization's Study on Global Ageing and Adult Health (2007–2010; n = 34,149). Analyses focused on 6 conditions: angina, arthritis, asthma, chronic lung disease, depression, and hypertension. Outcomes for these NCDs were: 1) self-reported disease, 2) algorithm/measured test-based disease, 3) undiagnosed disease, and 4) untreated disease. Algorithm/measured test-based prevalence of NCDs was much higher than self-reported prevalence in all 6 countries, indicating underestimation of NCD prevalence in low- and middle-income countries. Undiagnosed prevalence of NCDs was highest for hypertension, ranging from 19.7% (95% confidence interval (CI): 18.1, 21.3) in India to 49.6% (95% CI: 46.2, 53.0) in South Africa. The proportion untreated among all diseases was highest for depression, ranging from 69.5% (95% CI: 57.1, 81.9) in South Africa to 93.2% (95% CI: 90.1, 95.7) in India. Higher levels of education and wealth significantly reduced the odds of an undiagnosed condition and untreated morbidity. A high prevalence of undiagnosed NCDs and an even higher proportion of untreated NCDs highlights the inadequacies in diagnosis and management of NCDs in local health-care systems.
Keywords: chronic disease, diagnosis, low- and middle-income countries, noncommunicable diseases, untreated diseases
Chronic noncommunicable diseases (NCDs) and mental health conditions, including cardiovascular conditions, chronic respiratory conditions, and depression, are currently the main cause of both mortality and morbidity worldwide (1). Moreover, although the burden of NCDs is escalating across all regions of the world, previous research indicates that NCDs have a disproportionately high impact on low- and middle-income countries (LMICs) (2). Of the estimated 38 million deaths attributed to NCDs in 2012, 28 million (74% of all cases) occurred in LMICs (2). Numbers of deaths from NCDs are expected to increase rapidly over the next 25 years, such that the total number of NCD-related deaths is projected to increase globally to 52 million by 2030 (3). Of these projected 52 million deaths, 42 million (81%) are projected to occur in LMICs (3).
Despite the rising burden of NCDs in these settings, health-care systems in many LMICs continue to remain focused on the treatment and management of acute infectious illnesses (including malaria, diarrheal disease, and respiratory infections) and on the provision of maternal and child health services (4–6). Consequently, many countries are not adequately equipped to effectively manage NCDs, either in the primary health-care sector (4, 7), which deals with the bulk of disease management, or in terms of access to specialty/tertiary care when required. Such specialty care in LMICs tends to get lost in the aggregation of health-care services into large urban centers, nonengagement with primary health-care providers, and the high cost of treatment (8, 9).
Inadequate health-care systems are likely to have lower rates of diagnosis and treatment of chronic diseases and a continually rising disease burden from these conditions (5). The influence of socioeconomic inequalities on NCD prevalence, magnitude of undiagnosed disease, and access to treatment shows unequal distributions across socioeconomic groups based on wealth and education, but their impacts on these groups remain inadequately explored (10, 11). This raises additional concerns regarding the future implications of NCDs in developing countries and highlights the urgent need for prevention and control strategies.
Currently, there is a lack of population-based estimates of NCDs for many LMICs. Second, there is much less knowledge about appropriate strategies for improving the prevention and treatment of NCDs. Consequently, policy-makers often rely on information from high-income countries when designing prevention and treatment programs (8). Implementing prevention and management strategies based on results from high-income countries in LMICs may not yield similar outcomes (12). Therefore, research on disease burden and on prevention and management strategies for NCDs in local LMIC settings is needed. The findings from the current study have the potential to generate substantial attention for improving the treatment and prevention of NCDs in LMICs (8, 13).
We addressed this need by utilizing data from wave 1 of the World Health Organization's Study on Global Ageing and Adult Health (SAGE), carried out between 2007 and 2010. The objectives of this study were to: estimate the prevalence of 6 major NCDs (angina, asthma, arthritis, chronic lung disease, depression, and hypertension) using both self-reported diagnoses and an algorithm or measured test (based on a pattern of symptoms or on measured blood pressure); determine the prevalence of undiagnosed disease and the proportion of untreated conditions for each condition; and examine the sociodemographic correlates of each outcome.
METHODS
Sample
This study used data from SAGE wave 1 (2007–2010). SAGE is a longitudinal study of aging and health with nationally representative samples of adults from 6 LMICs: China, Ghana, India, Mexico, the Russian Federation, and South Africa. SAGE was designed as a multiwave panel study representative of the population aged 50 years or older in each participating country. Sample sizes for each country were as follows: China, n = 13,177; Ghana, n = 4,307; India, n = 6,560; Mexico, n = 2,327; Russia, n = 3,938; and South Africa, n = 3,840.
SAGE employed a multistage cluster design with samples drawn from an updated national sampling frame. Face-to-face interviews were used to capture respondent information. A detailed description of the study, the sample design, and weighting is provided elsewhere (14, 15).
Measurement
SAGE included self-reported diagnoses of 8 chronic conditions: angina, arthritis, asthma, chronic lung disease, diabetes, depression, hypertension, and stroke. These 8 conditions are thought to contribute a large portion of the overall burden of disease in older adults—covering both prevalent physical and mental health conditions. However, information from algorithm/measured test-based assessment was available for only 6 conditions—namely angina, arthritis, asthma, chronic lung diseases, depression, and hypertension. Since the analysis in this study was based on comparative assessment of self-reported diagnoses and algorithm/measured test-based appraisals of chronic diseases, only the 6 diseases for which both measures were available were included.
Noncommunicable diseases
Disease prevalence was estimated on the basis of the following 2 types of measures.
Self-reported diagnoses. Self-reported diagnosis of angina, arthritis, asthma, chronic lung disease, depression, or hypertension was assessed by means of the question, “Has a health-care professional ever told you that you have (disease name)?”
Algorithm-based diagnosis/measured test. SAGE additionally included a set symptomatic questions for assessment of angina pectoris, arthritis, asthma, chronic lung disease, and depression and measurement of blood pressure for assessment of hypertension. The symptomatic questions and algorithm used for each disease are listed in Table 1. The World Health Organization's Rose angina questionnaire was used for symptom-based assessment of angina pectoris (16, 17). The symptom questions for arthritis, asthma, and chronic lung disease were validated in a multicountry study, the Diagnostic Item Probability Study (18). The questionnaire for depression was based on the World Mental Health Survey version of the Composite International Diagnostic Interview (19). Hypertension was determined on the basis of 3 sitting blood pressure readings taken at 1-minute intervals. The average value of these 3 readings was used for all countries except Mexico, where the average of 2 available readings was used. An individual was considered hypertensive if average systolic or diastolic blood pressure exceeded 140 mmHg or 90 mmHg, respectively (20).
Table 1.
Symptoms and Algorithms Used to Derive the Prevalences of 5 Chronic Diseases in Wave 1 of the Study on Global Ageing and Adult Health (SAGE), 2007–2010
| Question No. | Question and Corresponding Algorithm Used to Ascertain Disease |
|---|---|
| Arthritis | |
| Question 1 | During the last 12 months, have you experienced, pain, aching, stiffness, or swelling in or around the joints (like arms, hands, legs, or feet) which was not related to an injury and lasted for more than a month? |
| Question 2 | During the last 12 months, have you experienced stiffness in the joint in the morning after getting up from bed, or after a long rest of the joint without movement? |
| If “yes” to question 2: | |
| Question 3 | How long did this stiffness last?—1) less than 30 minutes; 2) more than 30 minutes |
| Question 4 | Did this stiffness go away after exercise or movement in the joint?—1) yes; 2) no |
| Algorithm | If the response to questions 1 and 2 was “yes” and the response to questions 3 and 4 was the first option, the respondent was said to have arthritis. |
| Angina | |
| Question 1 | During the last 12 months, have you experienced any pain or discomfort in your chest when you walk uphill or hurry? |
| Question 2 | During the last 12 months, have you experienced any pain or discomfort in your chest when you walk at an ordinary pace on level ground? |
| If “yes” to question 2: | |
| Question 3 | What do you do if you get the pain or discomfort when you are walking?—1) stop or slow down; 2) carry on after taking a pain-relieving medicine that dissolves in your mouth; 3) carry on walking |
| Question 4 | If you stand still, what happens to the pain or discomfort?—1) relieved; 2) not relieved |
| Question 5 | Apart from these questions, respondents were asked to identify the points of pain in the upper part of the body (excluding the head) with the help of a picture depicting the upper parts of the body. |
| Algorithm | If the response to questions 1 and 2 was “yes” and the response to questions 3 and 4 was the first option, and in question 5 the respondent indicated that the pain was in the upper left part of the body, the person was said to have angina. |
| Chronic Lung Disease | |
| Question 1 | During the last 12 months, have you experienced any shortness of breath at rest (while awake)? |
| Question 2 | During the last 12 months, have you experienced any coughing or wheezing for 10 minutes or more at a time? |
| Question 3 | During the last 12 months, have you experienced any coughing up of sputum or phlegm on most days of the month for at least 3 months? |
| Algorithm | A respondent was ascertained to have chronic lung disease if his/her response was “yes” to question 1 or “yes” to both question 2 and question 3. |
| Asthma | |
| Question 1 | During the last 12 months, have you experienced attacks of wheezing or whistling breathing? |
| Question 2 | During the last 12 months, have you experienced an attack of wheezing that came on after you stopped exercising or some other physical activity? |
| Question 3 | During the last 12 months, have you had a feeling of tightness in your chest? |
| Question 4 | During the last 12 months, have you woken up with a feeling of tightness in your chest in the morning or any other time? |
| Question 5 | During the last 12 months, have you had an attack of shortness of breath that came on without an obvious cause when you were not exercising or doing some physical activity? |
| Algorithm | A respondent was said to suffer from asthma if s/he responded “yes” to question 1 and “yes” to any of the subsequent questions (2–5). |
| Depression | |
| Question 1 | During the last 12 months, have you had a period lasting several days when you felt sad, empty, or depressed? |
| Question 2 | During the last 12 months, have you had a period lasting several days when you lost interest in most things you usually enjoy, such as personal relationships, work, or hobbies/recreation? |
| Question 3 | During the last 12 months, have you had a period lasting several days when you have been feeling your energy decreased or that you are tired all the time? |
| If the response to any of the above 3 questions was “yes,” then the following set of questions was asked: | |
| Question 4 | Did this period (of sadness/loss of interest/low energy) last for more than 2 weeks? |
| Question 5 | Was this period (of sadness/loss of interest/low energy) most of the day, nearly every day? |
| Question 6 | During this period, did you lose your appetite? |
| Question 7 | Did you notice any slowing down in your thinking? |
| Question 8 | Did you notice any problems falling asleep? |
| Question 9 | Did you notice any problems waking up too early? |
| Question 10 | During this period, did you have any difficulties concentrating—for example, listening to others, working, watching television, listening to the radio? |
| Question 11 | Did you notice any slowing down in your moving around? |
| Question 12 | During this period, did you feel anxious and worried most days? |
| Question 13 | During this period, were you so restless or jittery nearly every day that you paced up and down and couldn't sit still? |
| Question 14 | During this period, did you feel negative about yourself or like you had lost confidence? |
| Question 15 | Did you frequently feel hopeless—that there was no way to improve things? |
| Question 16 | During this period, did your interest in sex decrease? |
| Question 17 | Did you think of death, or wish you were dead? |
| Question 18 | During this period, did you ever try to end your life? |
| Algorithm | To ascertain depression from this set of questions, 2 set of variables were computed. |
| The first set of variables was based on questions 1–5 and question 16. From this set, 3 variables were computed taking the values 0 and 1, as follows: 1) The first variable takes the value 1 if the response to any of questions 1, 4, and 5 is “yes.” 2) The second variable takes the value 1 if the response to question 2 or 16 is “yes.” 3) The third variable takes the value 1 if the response to question 3 is “yes.” | |
| The second set of variables was based on questions 6–15, 17, and 18. From these questions, 7 variables were computed. 1) The first variable takes the value 1 if the response to question 14 or 15 is “yes.” 2) The second variable takes the value 1 if the response to question 12 or 13 is “yes.” 3) The third variable takes the value 1 if the response to question 17 or 18 is “yes.” 4) The fourth variable takes the value 1 if the response to question 7 or 10 is “yes.” 5) The fifth variable takes the value 1 if the response to question 11 is “yes.” 6) The sixth variable takes the value 1 if the response to question 8 or 9 is “yes.” 7) The seventh variable takes the value 1 if the response to question 6 is “yes.” | |
| These newly created variables from the respective sets were added to obtain 2 new variables, the first consisting of the sum of the first set of variables (maximum value 3) and the second consisting of the sum of the second set of variables (maximum value 7). On the basis of these 2 variables, a respondent was said to suffer from depression if s/he had a value for the first variable of 2 or more and a value for the second variable of 4 or more. | |
Additionally, for each of the 6 NCDs, persons who reported having been diagnosed and having received treatment in the last 12 months but did not have the condition based on an algorithm-based diagnosis/measured test were considered to have the condition.
Undiagnosed chronic conditions
A respondent was considered to have undiagnosed chronic disease(s) if he/she did not report having received that diagnosis but was positive for that particular condition on the basis of the algorithm-based diagnosis/measured test.
Untreated chronic conditions
A respondent was considered to have an untreated chronic condition if s/he was found positive in algorithm/measured test-based assessment but had not received treatment in the last 12 months. The proportion of respondents untreated was calculated by taking the number of respondents who did not receive treatment (in the numerator) and dividing by those who were found to be positive in the algorithm/measured test-based assessment (in the denominator).
Thus, 4 binary outcome variables for each of the 6 selected NCDs were generated: 1) self-reported disease; 2) algorithm/measured test-based disease; 3) undiagnosed disease; and 4) untreated disease.
Analytical methods
The analysis for these outcomes was carried out in 3 stages. First, national-level prevalences of self-reported diagnosis, algorithm/measured test-based and undiagnosed disease, and proportion untreated were calculated for each of the 6 NCDs. Secondly, the prevalence of each of the diseases was calculated according to sociodemographic covariates. Finally, a multivariable regression analysis was conducted to examine the socioeconomic and demographic correlates of the aforementioned indicators.
The multivariable analysis was conducted on the pooled sample of all 6 countries, accounting for the complex survey design. Multivariable logistic models were fitted for the aforementioned binary outcome variables for each of the diseases. The missing values were excluded from the analysis under the assumption that the characteristics of persons with missing and nonmissing observations were similar (analysis not shown).
The following predictors were used in the multivariate logistic regression models: age, sex, place of residence, education, wealth quintile, and country of residence. The regression models for self-reported diagnosis and algorithm/measured test-based measures additionally included major health risk factors—namely current tobacco use, alcohol consumption, physical inactivity, and obesity. A detailed description of the categories of the predictors is given in the Web Appendix (available at http://aje.oxfordjournals.org/).
Furthermore, the probabilities of self-reported diagnosis, algorithm/measured test-based, and undiagnosed and untreated disease were predicted from the logit models for each country and each of the 6 NCDs to obtain national estimates of the outcomes after adjustment for the sociodemographic differences.
RESULTS
We analyzed data on a total of 34,149 older adults from the 6 LMICs. Table 2 shows the characteristics (weighted percentages using sample weights) of the sample. Ghana had the highest proportion (33%) of respondents aged ≥70 years, and South Africa had the lowest (20%). The proportion of the rural adult population ranged from 21% in Mexico to 71% in India. The percentage of the sample with no formal schooling was highest in Ghana (55%) and India (52%) and lowest in Russia (0.5%).
Table 2.
Distribution (Weighted Percentage) of Older Respondents (Aged ≥50 Years) According to Selected Socioeconomic and Demographic Characteristics in the Study on Global Ageing and Adult Health (Wave 1), 2007–2010
| Country | Pooled Data | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| India (n = 6,560) |
China (n = 13,177) |
Ghana (n = 4,307) |
Mexico (n = 2,327) |
Russia (n = 3,938) |
South Africa (n = 3,840) | All Countries (n = 34,149) | Men (n = 15,597) |
Women (n = 18,332) |
|
| Age group, years | |||||||||
| 50–59 | 48.6 | 44.9 | 39.7 | 48.1 | 44.1 | 49.9 | 49.6 | 51.3 | 48.0 |
| 60–69 | 30.9 | 31.9 | 27.5 | 25.6 | 26.7 | 30.6 | 28.6 | 28.9 | 28.4 |
| ≥70 | 20.5 | 23.2 | 32.8 | 26.4 | 29.1 | 19.5 | 21.7 | 19.8 | 23.6 |
| Sex | |||||||||
| Male | 51.0 | 49.8 | 52.4 | 46.8 | 40.3 | 44.1 | 48.8 | ||
| Female | 49.0 | 50.2 | 47.6 | 53.2 | 59.7 | 55.9 | 51.2 | ||
| Residence | |||||||||
| Urban | 28.9 | 47.3 | 41.1 | 78.9 | 70.1 | 64.9 | 44.1 | 42.8 | 45.2 |
| Rural | 71.1 | 52.7 | 58.9 | 21.1 | 29.9 | 35.1 | 56.0 | 57.2 | 54.8 |
| Marital status | |||||||||
| Never married | 0.7 | 1.1 | 1.3 | 7.4 | 2.6 | 14.3 | 1.4 | 1.6 | 1.3 |
| Currently married/cohabiting | 76.9 | 85.0 | 59.3 | 72.6 | 60.5 | 55.9 | 80.1 | 89.7 | 70.9 |
| Widowed/divorced/separated | 22.3 | 13.8 | 39.4 | 20.0 | 36.9 | 29.8 | 18.5 | 8.7 | 27.8 |
| Years of education completed | |||||||||
| No formal education | 51.6 | 23.5 | 54.8 | 17.4 | 0.5 | 24.5 | 29.4 | 17.6 | 40.5 |
| 1–5 | 19.1 | 25.2 | 8.4 | 38.1 | 5.4 | 21.5 | 22.2 | 23.0 | 21.4 |
| 6–9 | 13.1 | 34.8 | 8.3 | 34.2 | 18.6 | 30.9 | 27.9 | 33.9 | 22.1 |
| ≥10 | 16.2 | 16.5 | 28.5 | 10.3 | 75.5 | 23.1 | 20.6 | 25.4 | 16.0 |
| Income quintile | |||||||||
| Q1 (lowest) | 18.2 | 16.3 | 18.2 | 15.2 | 13.3 | 20.7 | 16.9 | 16.1 | 17.6 |
| Q2 | 19.5 | 18.1 | 19.1 | 24.8 | 17.1 | 19.9 | 18.8 | 18.6 | 19.0 |
| Q3 | 18.8 | 20.5 | 20.5 | 17.1 | 19.6 | 18.2 | 19.6 | 19.2 | 19.9 |
| Q4 | 19.6 | 23.4 | 20.7 | 16.5 | 22.1 | 19.8 | 21.9 | 22.3 | 21.4 |
| Q5 (highest) | 23.9 | 21.8 | 21.6 | 26.4 | 27.8 | 21.3 | 22.9 | 23.8 | 22.0 |
Abbreviation: Q, quintile.
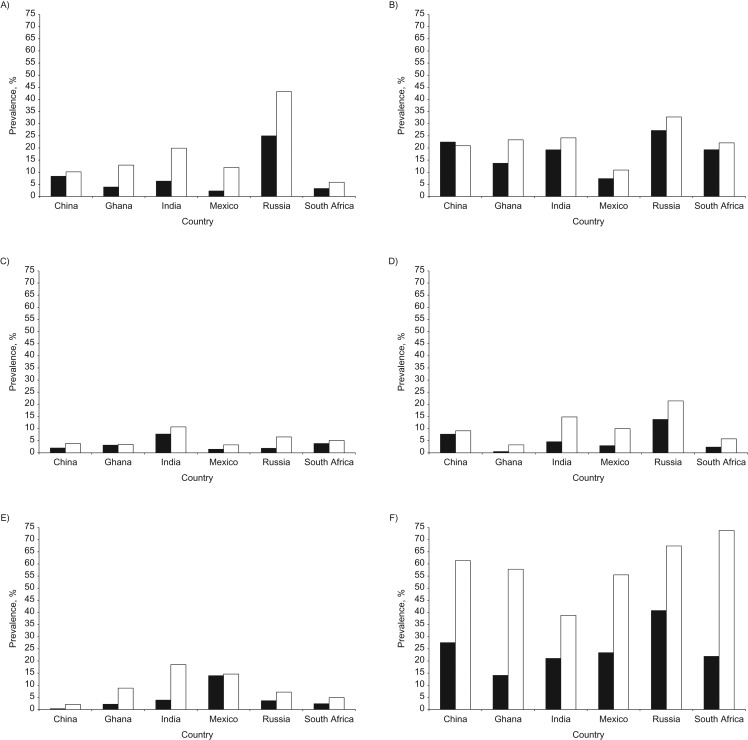
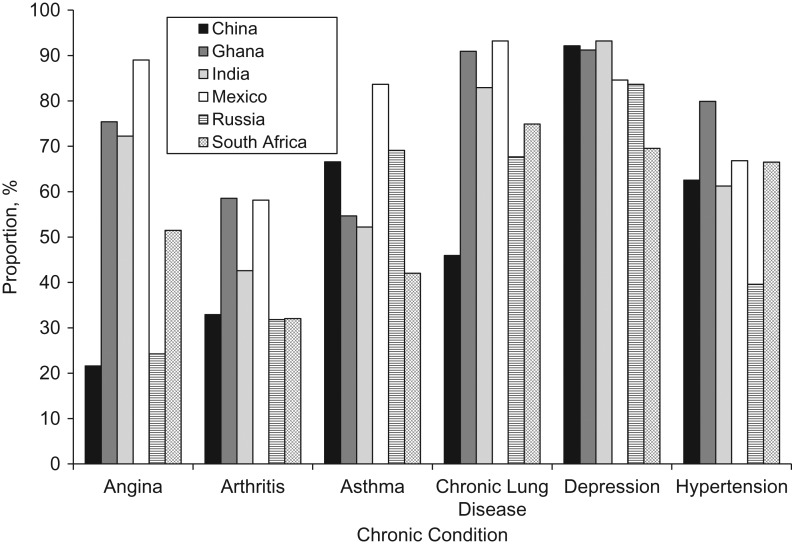
The adjusted (predicted probabilities from logit regression estimates) self-reported and algorithm/measured test-based prevalences of the 6 NCDs among older adults are shown in Figure 1. Results show that algorithm/measured test-based prevalence was higher than self-reported prevalence for all 6 chronic diseases in each country. Hypertension was the most prevalent condition in all countries, both in terms of self-report and in terms of measurement. The prevalence of self-reported hypertension ranged from 14.1% (95% confidence interval (CI): 12.6, 15.5) in Ghana to 40.8% (95% CI: 35.8, 45.7) in Russia, whereas prevalence of measured hypertension ranged from 38.8% (95% CI: 36.8, 40.8) in India to 73.8% (95% CI: 70.4, 77.2) in South Africa. The prevalence of self-reported arthritis was second-highest after hypertension in all countries, ranging from 27.2% (95% CI: 22.5, 31.9) in Russia to 7% (95% CI: 4.3, 10.4) in Mexico. In addition, Russia had the highest prevalence of both self-reported (25%, 95% CI: 21.1, 28.9) and algorithm-based (43%, 95% CI: 36.6, 49.8) angina. The prevalence of self-reported asthma was less than 5% in all countries except India (7.7%, 95% CI: 6.2, 9.3). The prevalences of both self-reported and algorithm-based chronic lung disease were lowest in Ghana (0.5% (95% CI: 0.3, 0.7) and 3% (95% CI: 2.5, 4.1), respectively) and highest in Russia (13.7% (95% CI: 10.4, 17.1) and 21.4% (95% CI: 17.0, 25.8), respectively). The adjusted prevalences of self-reported and algorithm-based depression were lowest in China (0.3% (95% CI: 0.2, 0.4) and 2.1% (95% CI: 1.6, 2.5), respectively), whereas Mexico had the highest prevalence of self-reported depression (13.9%, 95% CI: 6.5, 21.4) and India had the highest algorithm-based prevalence (18.5%, 95% CI: 15.8.6, 21.3).
Figure 1.
Adjusted (for sociodemographic characteristics) self-reported and algorithm/measured test-based prevalences of noncommunicable diseases in 6 low- and middle-income countries, Study on Global Ageing and Adult Health (wave 1), 2007–2010. Black bars, self-reported prevalence; white bars, algorithm/measured test-based prevalence. A) Angina; B) arthritis; C) asthma; D) chronic lung disease; E) depression; F) hypertension.
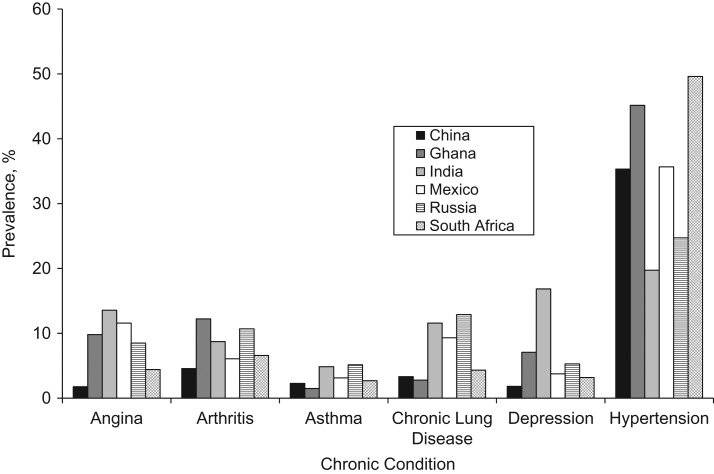
Figure 2 shows the adjusted prevalence of undiagnosed NCDs. Results showed that undiagnosed prevalence of hypertension was higher relative to other diseases for all countries, ranging from 19.7% (95% CI: 18.1, 21.3) in India to 49.6% (95% CI: 46.2, 53.0) in South Africa. The prevalence of undiagnosed angina was highest in India (13.6%, 95% CI: 10.1, 16.2), followed by Mexico (11.6%, 95% CI: 5.0, 18.1), and was lowest in China (1.8%, 95% CI: 1.5, 2.0). India had the highest prevalence of undiagnosed depression (16.8%, 95% CI: 14.0, 19.7), while China had the lowest (1.8%, 95% CI: 1.4, 2.2). China had the lowest undiagnosed prevalence for most chronic diseases (Figure 2).
Figure 2.
Adjusted (for sociodemographic characteristics) prevalences of undiagnosed chronic diseases in 6 low- and middle-income countries, Study on Global Ageing and Adult Health (wave 1), 2007–2010.
Figure 3 shows the adjusted (for sociodemographic characteristics) prevalence of untreated chronic diseases in the previous 12 months. In all 6 countries, a very high percentage of older adults with an algorithm-based chronic disease did not report taking medication in the past 12 months. The proportion untreated was highest for depression; specifically, among persons with algorithm-based depression, 93.2% (95% CI: 90.1, 95.7) did not receive treatment in India, 92.1% (95% CI: 87.8, 96.5) did not receive treatment in China, 91.2% (95% CI: 86.8, 95.7) did not get treatment in Ghana, and 69.5% (95% CI: 57.1, 81.9) did not get treatment in South Africa. The other 5 chronic conditions exhibited similarly high rates of untreated disease in all countries. Cross-country differences in the prevalence of untreated conditions were pronounced. Compared with other countries, the prevalence of untreated morbidity (for all 5 conditions) was consistently higher among older adults living in Ghana, India, and Mexico and lower in China, Russia, and South Africa.
Figure 3.
Adjusted (for sociodemographic characteristics) proportions of untreated chronic diseases in 6 low- and middle-income countries, Study on Global Ageing and Adult Health (wave 1), 2007–2010.
Sociodemographic patterns
Given the importance of within-country sociodemographic variations, the self-reported and algorithm/measured test-based prevalences of chronic diseases are presented according to sociodemographic strata in Web Tables 1 and 2. Both self-reported and algorithm/measured test-based prevalence increased with age for all 6 NCDs across the SAGE countries. Women exhibited a higher prevalence of both self-reported and algorithm/measured test-based angina, arthritis, depression, and hypertension in all countries except India, where the prevalence of self-reported angina was lower among women. Prevalences of both self-reported and algorithm-based asthma were lower among women in China, Ghana, India, and South Africa. Educational level did not uniformly influence self-reported disease prevalence, although algorithm/measured test-based prevalence generally declined as educational levels increased for each disease across all countries.
Web Table 3 shows the undiagnosed prevalence of each disease according to background characteristics for each country. Prevalence of undiagnosed diseases typically increased with age; further, women displayed a higher prevalence of undiagnosed conditions for all 6 NCDs, except hypertension. Older adults with higher educational levels and from higher wealth quintiles had a lower prevalence of undiagnosed disease.
Age did not appear to be uniformly associated with the prevalence of untreated conditions; a higher percentage of women had untreated chronic conditions. Persons with higher levels of education and wealth were characterized by a lower prevalence of untreated chronic conditions (Web Table 4).
Multivariable analyses
Table 3 presents results from a logit model estimating the association between socioeconomic/health risk factors and self-reported conditions. Participants aged 70 years or older had a higher likelihood of self-reported chronic disease. Women were significantly more likely than men to report arthritis (odds ratio (OR) = 1.35, 95% CI: 1.11, 1.63), depression (OR = 1.38, 95% CI: 0.93, 2.05), or hypertension (OR = 1.41, 95% CI: 1.22, 1.63) and less likely to report asthma (OR = 0.62, 95% CI: 0.45, 0.84) or chronic lung disease (OR = 0.67, 95% CI: 0.56, 0.79). Neither educational level nor wealth quintile appeared to consistently influence the likelihood of self-reported chronic conditions; in fact, the odds ratios were statistically insignificant for most of the 6 NCDs. Physical inactivity and obesity were associated with a higher likelihood of self-reported chronic diseases. Compared with Russia (the reference group), respondents in the other 5 countries had significantly lower odds of reported angina, arthritis, chronic lung disease, and hypertension. Compared with Russia, the odds of reporting asthma were 4 times higher in India, while the odds of reporting depression were 4 times higher in Mexico.
Table 3.
Odds Ratios (Logit Model Estimates) for Factors Associated With the Prevalence of Reported Chronic Diseases in the Study on Global Ageing and Adult Health (Wave 1), 2007–2010
| Covariate | Angina | Arthritis | Asthma | Chronic Lung Disease | Depression | Hypertension | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Socioeconomic status | ||||||||||||
| Years of schooling | ||||||||||||
| No schooling | 0.61 | 0.44, 0.85 | 1.15 | 0.93, 1.42 | 0.89 | 0.61, 1.30 | 1.02 | 0.75, 1.38 | 0.89 | 0.52, 1.54 | 0.75 | 0.63, 0.90 |
| 1–5 | 0.95 | 0.70, 1.29 | 1.32 | 1.07, 1.63 | 0.84 | 0.52, 1.37 | 0.96 | 0.72, 1.30 | 1.01 | 0.61, 1.67 | 0.83 | 0.69, 1.00 |
| 6–9 | 0.99 | 0.67, 1.49 | 1.08 | 0.84, 1.38 | 0.87 | 0.58, 1.29 | 1.04 | 0.85, 1.26 | 0.94 | 0.56, 1.58 | 0.99 | 0.84, 1.17 |
| ≥10 (referent) | ||||||||||||
| Wealth quintile | ||||||||||||
| Q1 (lowest) | 0.80 | 0.56, 1.14 | 0.90 | 0.71, 1.13 | 1.96 | 1.21, 3.16 | 1.20 | 0.90, 1.60 | 1.27 | 0.76, 2.14 | 0.53 | 0.42, 0.66 |
| Q2 | 0.97 | 0.70, 1.35 | 1.07 | 0.85, 1.33 | 1.58 | 0.95, 2.60 | 1.15 | 0.87, 1.52 | 1.13 | 0.72, 1.78 | 0.72 | 0.58, 0.89 |
| Q3 | 1.08 | 0.74, 1.56 | 1.06 | 0.84, 1.35 | 1.55 | 1.14, 2.10 | 1.05 | 0.82, 1.34 | 1.01 | 0.70, 1.47 | 0.83 | 0.66, 1.05 |
| Q4 | 0.92 | 0.65, 1.30 | 0.96 | 0.78, 1.18 | 1.26 | 0.88, 1.79 | 1.11 | 0.86, 1.43 | 1.56 | 0.94, 2.58 | 0.89 | 0.74, 1.08 |
| Q5 (highest; referent) | ||||||||||||
| Country | ||||||||||||
| India | 0.19 | 0.13, 0.27 | 0.63 | 0.47, 0.85 | 4.44 | 2.52, 7.83 | 0.30 | 0.19, 0.45 | 1.07 | 0.63, 1.85 | 0.35 | 0.27, 0.46 |
| China | 0.26 | 0.20, 0.33 | 0.77 | 0.59, 0.99 | 1.05 | 0.64, 1.72 | 0.52 | 0.38, 0.70 | 0.08 | 0.05, 0.15 | 0.52 | 0.41, 0.66 |
| Ghana | 0.11 | 0.08, 0.16 | 0.42 | 0.31, 0.56 | 1.70 | 1.02, 2.83 | 0.03 | 0.02, 0.05 | 0.59 | 0.34, 1.05 | 0.21 | 0.16, 0.27 |
| Mexico | 0.06 | 0.03, 0.13 | 0.21 | 0.12, 0.34 | 0.78 | 0.43, 1.42 | 0.18 | 0.11, 0.30 | 4.35 | 2.08, 9.10 | 0.41 | 0.28, 0.60 |
| South Africa | 0.09 | 0.07, 0.14 | 0.63 | 0.46, 0.87 | 2.09 | 1.21, 3.61 | 0.15 | 0.09, 0.24 | 0.65 | 0.37, 1.13 | 0.37 | 0.28, 0.50 |
| Russia (referent) | ||||||||||||
| Age group, years | ||||||||||||
| 50–59 (referent) | ||||||||||||
| 60–69 | 1.49 | 1.14, 1.95 | 1.37 | 1.17, 1.60 | 1.68 | 1.33, 2.12 | 1.65 | 1.37, 1.99 | 1.17 | 0.85, 1.60 | 1.54 | 1.33, 1.77 |
| ≥70 | 2.54 | 1.86, 3.48 | 1.51 | 1.25, 1.84 | 1.76 | 1.34, 2.31 | 2.11 | 1.63, 2.74 | 0.86 | 0.57, 1.29 | 2.30 | 1.99, 2.65 |
| Residence | ||||||||||||
| Urban (referent) | ||||||||||||
| Rural | 0.89 | 0.70, 1.13 | 0.88 | 0.73, 1.06 | 0.81 | 0.57, 1.14 | 0.87 | 0.68, 1.12 | 0.97 | 0.54, 1.73 | 0.73 | 0.63, 0.84 |
| Sex | ||||||||||||
| Male (referent) | ||||||||||||
| Female | 0.92 | 0.69, 1.22 | 1.35 | 1.11, 1.63 | 0.62 | 0.45, 0.84 | 0.67 | 0.56, 0.79 | 1.38 | 0.93, 2.05 | 1.41 | 1.22, 1.63 |
| Marital status | ||||||||||||
| Never married (referent) | ||||||||||||
| Currently married/cohabiting | 1.47 | 0.82, 2.62 | 1.41 | 0.95, 2.09 | 1.43 | 0.84, 2.43 | 0.97 | 0.62, 1.54 | 1.32 | 0.59, 2.98 | 1.15 | 0.81, 1.62 |
| Widow/divorced/separated | 1.81 | 0.99, 3.34 | 1.56 | 1.02, 2.40 | 1.73 | 1.01, 2.97 | 0.87 | 0.53, 1.44 | 1.35 | 0.59, 3.08 | 1.21 | 0.84, 1.74 |
| Current tobacco consumption | ||||||||||||
| No (referent) | ||||||||||||
| Yes | 1.04 | 0.76, 1.41 | 0.95 | 0.78, 1.15 | 0.97 | 0.70, 1.34 | 1.13 | 0.91, 1.42 | 1.32 | 1.01, 1.72 | 0.91 | 0.76, 1.07 |
| Alcohol consumption | ||||||||||||
| No (referent) | ||||||||||||
| Yes | 0.64 | 0.46, 0.90 | 0.94 | 0.75, 1.18 | 0.83 | 0.61, 1.15 | 1.15 | 0.89, 1.47 | 0.76 | 0.48, 1.19 | 0.79 | 0.67, 0.95 |
| Physical activity | ||||||||||||
| Yes (referent) | ||||||||||||
| No | 1.22 | 1.04, 1.44 | 1.15 | 1.00, 1.32 | 1.56 | 1.24, 1.96 | 1.31 | 1.10, 1.55 | 1.33 | 0.88, 2.00 | 1.09 | 0.96, 1.23 |
| Obesity | ||||||||||||
| No (referent) | ||||||||||||
| Yes | 1.87 | 1.36, 2.58 | 1.64 | 1.26, 2.13 | 1.53 | 1.05, 2.21 | 1.46 | 1.09, 1.96 | 1.10 | 0.71, 1.70 | 2.96 | 2.29, 3.83 |
Abbreviations: CI, confidence interval; OR, odds ratio; Q, quintile.
Table 4 presents logit model estimates (odds ratios) showing correlates of algorithm/measured test-based chronic disease prevalence. In contrast to the pattern for self-reported disease prevalence, both years of education and age showed a consistent and negative association with each of the chronic diseases. Compared with the reference group (≥10 years of schooling), older adults with fewer years of schooling displayed higher odds of algorithm/measured test-based chronic disease. Age was positively associated with algorithm/measured test-based chronic disease. Sex differences were also observed, such that older women were more likely than men to have symptom/measured angina, arthritis, depression, and hypertension but less likely to have asthma and chronic lung diseases. Physical inactivity and obesity were positively associated with symptom-based diseases. Compared with Russia, older adults in the other 5 countries were less likely to have angina, arthritis, and chronic lung disease.
Table 4.
Odds Ratios (Logit Model Estimates) for Factors Associated With the Prevalence of Algorithm/Measured Test-Based Chronic Diseases in the Study on Global Ageing and Adult Health (Wave 1), 2007–2010
| Covariate | Angina | Arthritis | Asthma | Chronic Lung Disease | Depression | Hypertension | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Socioeconomic status | ||||||||||||
| Years of schooling | ||||||||||||
| No schooling | 1.50 | 1.12, 2.01 | 1.35 | 1.09, 1.66 | 1.56 | 1.13, 2.15 | 1.65 | 1.23, 2.20 | 1.29 | 0.98, 1.69 | 1.04 | 0.91, 1.20 |
| 1–5 | 1.54 | 1.16, 2.04 | 1.33 | 1.09, 1.64 | 1.45 | 1.09, 1.93 | 1.53 | 1.25, 1.88 | 1.05 | 0.78, 1.40 | 1.17 | 0.99, 1.36 |
| 6–9s | 1.46 | 1.04, 2.04 | 1.24 | 0.94, 1.64 | 1.29 | 0.98, 1.70 | 1.29 | 0.99, 1.68 | 1.11 | 0.77, 1.61 | 1.17 | 1.00, 1.37 |
| ≥10 (referent) | ||||||||||||
| Wealth quintile | ||||||||||||
| Q1 (lowest) | 1.29 | 0.86, 1.94 | 1.04 | 0.84, 1.30 | 1.63 | 1.22, 2.17 | 1.63 | 1.27, 2.09 | 1.78 | 1.40, 2.27 | 0.84 | 0.72, 0.99 |
| Q2 | 1.27 | 0.90, 1.78 | 1.21 | 0.98, 1.50 | 1.51 | 1.14, 1.98 | 1.40 | 1.08, 1.83 | 1.85 | 1.45, 2.38 | 0.91 | 0.76, 1.08 |
| Q3 | 1.36 | 0.94, 1.98 | 1.12 | 0.89, 1.42 | 1.53 | 1.12, 2.09 | 1.49 | 1.14, 1.96 | 1.75 | 1.24, 2.49 | 0.95 | 0.77, 1.16 |
| Q4 | 1.11 | 0.76, 1.62 | 1.10 | 0.88, 1.37 | 1.18 | 0.88, 1.59 | 1.20 | 0.93, 1.56 | 1.40 | 1.11, 1.76 | 1.08 | 0.93, 1.25 |
| Q5 (highest; referent) | ||||||||||||
| Country | ||||||||||||
| India | 0.30 | 0.20, 0.46 | 0.65 | 0.48, 0.88 | 1.73 | 1.10, 2.72 | 0.63 | 0.44, 0.89 | 2.98 | 1.74, 5.10 | 0.29 | 0.22, 0.38 |
| China | 0.13 | 0.10, 0.18 | 0.54 | 0.40, 0.72 | 0.57 | 0.38, 0.85 | 0.36 | 0.27, 0.47 | 0.28 | 0.16, 0.47 | 0.76 | 0.58, 0.99 |
| Ghana | 0.18 | 0.13, 0.25 | 0.62 | 0.47, 0.82 | 0.51 | 0.32, 0.79 | 0.12 | 0.08, 0.17 | 1.25 | 0.75, 2.09 | 0.65 | 0.50, 0.86 |
| Mexico | 0.16 | 0.08, 0.32 | 0.24 | 0.16, 0.38 | 0.48 | 0.27, 0.85 | 0.40 | 0.26, 0.60 | 2.23 | 1.11, 4.50 | 0.59 | 0.40, 0.87 |
| South Africa | 0.07 | 0.05, 0.11 | 0.58 | 0.43, 0.77 | 0.76 | 0.48, 1.21 | 0.22 | 0.15, 0.32 | 0.67 | 0.40, 1.10 | 1.38 | 1.01, 1.88 |
| Russia (referent) | ||||||||||||
| Age group, years | ||||||||||||
| 50–59 (referent) | ||||||||||||
| 60–69 | 1.55 | 1.27, 1.88 | 1.22 | 1.04, 1.42 | 1.56 | 1.28, 1.91 | 1.63 | 1.41, 1.89 | 1.25 | 0.98, 1.59 | 1.45 | 1.27, 1.66 |
| ≥70 | 2.27 | 1.83, 2.81 | 1.35 | 1.12, 1.63 | 1.79 | 1.45, 2.21 | 1.90 | 1.57, 2.31 | 1.35 | 1.06, 1.71 | 2.01 | 1.77, 2.28 |
| Residence | ||||||||||||
| Urban (referent) | ||||||||||||
| Rural | 0.94 | 0.67, 1.31 | 0.99 | 0.83, 1.19 | 1.04 | 0.78, 1.38 | 1.03 | 0.83, 1.28 | 0.87 | 0.60, 1.26 | 1.07 | 0.94, 1.20 |
| Sex | ||||||||||||
| Male (referent) | ||||||||||||
| Female | 1.29 | 1.01, 1.63 | 1.39 | 1.15, 1.68 | 0.66 | 0.54, 0.83 | 0.81 | 0.68, 0.96 | 1.29 | 1.06, 1.56 | 1.14 | 1.03, 1.26 |
| Marital status | ||||||||||||
| Never married (referent) | ||||||||||||
| Currently married/cohabiting | 2.30 | 1.32, 4.00 | 1.65 | 1.06, 2.56 | 0.81 | 0.44, 1.50 | 0.79 | 0.50, 1.24 | 1.33 | 0.77, 2.31 | 0.90 | 0.66, 1.23 |
| Widow/divorced/separated | 2.38 | 1.30, 4.37 | 1.69 | 1.09, 2.63 | 0.86 | 0.46, 1.58 | 0.81 | 0.50, 1.30 | 1.42 | 0.81, 2.49 | 0.99 | 0.72, 1.40 |
| Current tobacco consumption | ||||||||||||
| No (referent) | ||||||||||||
| Yes | 1.04 | 0.82, 1.33 | 1.02 | 0.85, 1.22 | 1.04 | 0.85, 1.22 | 1.18 | 1.00, 1.40 | 1.11 | 0.91, 1.34 | 0.90 | 0.80, 1.01 |
| Alcohol consumption | ||||||||||||
| No (referent) | ||||||||||||
| Yes | 0.70 | 0.52, 0.94 | 0.93 | 0.76, 1.14 | 0.93 | 0.72, 1.19 | 0.85 | 0.70, 1.04 | 0.80 | 0.62, 1.03 | 1.23 | 1.07, 1.40 |
| Physical activity | ||||||||||||
| Yes (referent) | ||||||||||||
| No | 1.25 | 1.05, 1.48 | 1.04 | 0.93, 1.16 | 1.38 | 1.15, 1.64 | 1.29 | 1.14, 1.47 | 0.90 | 0.72, 1.13 | 1.07 | 0.96, 1.18 |
| Obesity | ||||||||||||
| No (referent) | ||||||||||||
| Yes | 2.00 | 1.38, 2.89 | 1.77 | 1.34, 2.32 | 1.69 | 1.27, 2.25 | 1.29 | 0.98, 1.72 | 1.06 | 0.73, 1.53 | 1.35 | 0.84, 2.17 |
Abbreviations: CI, confidence interval; OR, odds ratio; Q, quintile.
Multivariable analyses indicated that sociodemographic factors strongly influenced the likelihood of undiagnosed chronic disease (Table 5). Participants aged 70 years or older had 3 times’ higher odds of undiagnosed chronic disease as younger individuals. Further, for each chronic disease, women were significantly more likely than men to have an undiagnosed condition (Table 5). Both education and household wealth significantly influenced disease diagnosis; specifically, more years of schooling and higher levels of wealth significantly decreased the odds of having an undiagnosed condition.
Table 5.
Odds Ratios (Logit Model Estimates) for Factors Associated With the Prevalence of Undiagnosed Chronic Diseases in the Study on Global Ageing and Adult Health (Wave 1), 2007–2010
| Covariate | Angina | Arthritis | Asthma | Chronic Lung Disease | Depression | Hypertension | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Socioeconomic status | ||||||||||||
| Years of schooling | ||||||||||||
| No schooling | 1.85 | 1.27, 2.70 | 1.69 | 1.09, 2.62 | 1.77 | 1.20, 2.61 | 2.18 | 1.46, 3.23 | 1.44 | 1.05, 1.99 | 1.40 | 1.18, 1.66 |
| 1–5 | 1.79 | 1.20, 2.67 | 1.29 | 0.85, 1.96 | 1.59 | 1.08, 2.35 | 2.03 | 1.45, 2.84 | 1.11 | 0.79, 1.56 | 1.34 | 1.11, 1.61 |
| 6–9 | 1.41 | 0.91, 2.16 | 1.35 | 0.88, 2.06 | 1.40 | 0.99, 1.98 | 1.64 | 1.14, 2.36 | 1.24 | 0.80, 1.91 | 1.23 | 1.04, 1.45 |
| ≥10 (referent) | ||||||||||||
| Wealth quintile | ||||||||||||
| Q1 (lowest) | 2.13 | 1.46, 3.11 | 1.33 | 0.99, 1.78 | 1.36 | 0.95, 1.95 | 1.64 | 1.23, 2.19 | 1.74 | 1.31, 2.30 | 1.37 | 1.13, 1.65 |
| Q2 | 1.60 | 1.16, 2.22 | 1.38 | 1.07, 1.78 | 1.47 | 1.07, 2.02 | 1.33 | 0.94, 1.89 | 1.74 | 1.33, 2.29 | 1.20 | 1.00, 1.43 |
| Q3 | 1.78 | 1.22, 2.59 | 1.19 | 0.91, 1.55 | 1.40 | 0.95, 2.06 | 1.60 | 1.13, 2.28 | 1.70 | 1.19, 2.43 | 1.14 | 0.97, 1.34 |
| Q4 | 1.51 | 1.05, 2.15 | 1.36 | 0.86, 2.16 | 1.06 | 0.76, 1.47 | 1.25 | 0.91, 1.71 | 1.27 | 0.99, 1.63 | 1.26 | 1.05, 1.50 |
| Q5 (highest; referent) | ||||||||||||
| Country | ||||||||||||
| India | 1.72 | 1.07, 2.74 | 0.80 | 0.47, 1.34 | 0.94 | 0.56, 1.59 | 0.88 | 0.58, 1.34 | 3.70 | 2.19, 6.25 | 0.75 | 0.56, 0.99 |
| China | 0.19 | 0.13, 0.28 | 0.40 | 0.24, 0.66 | 0.43 | 0.27, 0.68 | 0.23 | 0.15, 0.34 | 0.33 | 0.20, 0.55 | 1.68 | 1.29, 2.19 |
| Ghana | 1.18 | 0.78, 1.78 | 1.17 | 0.72, 1.90 | 0.28 | 0.16, 0.48 | 0.19 | 0.12, 0.30 | 1.37 | 0.85, 2.21 | 2.56 | 1.92, 3.41 |
| Mexico | 1.42 | 0.68, 2.98 | 0.54 | 0.31, 0.92 | 0.59 | 0.32, 1.12 | 0.69 | 0.42, 1.13 | 0.70 | 0.41, 1.19 | 1.71 | 1.12, 2.61 |
| South Africa | 0.49 | 0.31, 0.79 | 0.59 | 0.36, 0.95 | 0.51 | 0.30, 0.85 | 0.30 | 0.19, 0.47 | 0.59 | 0.34, 1.01 | 3.07 | 2.32, 4.07 |
| Russia (referent) | ||||||||||||
| Age group, years | ||||||||||||
| 50–59 (referent) | ||||||||||||
| 60–69 | 1.39 | 1.17, 1.65 | 1.02 | 0.83, 1.25 | 1.36 | 1.10, 1.70 | 1.46 | 1.20, 1.78 | 1.27 | 0.96, 1.67 | 1.04 | 0.93, 1.17 |
| ≥70 | 1.31 | 0.99, 1.74 | 1.01 | 0.77, 1.32 | 1.54 | 1.19, 2.00 | 1.73 | 1.37, 2.20 | 1.31 | 1.00, 1.73 | 1.00 | 0.88, 1.15 |
| Residence | ||||||||||||
| Urban (referent) | ||||||||||||
| Rural | 0.95 | 0.61, 1.50 | 1.28 | 0.84, 1.93 | 1.16 | 0.73, 1.84 | 1.07 | 0.82, 1.39 | 0.94 | 0.64, 1.39 | 1.41 | 1.22, 1.63 |
| Sex | ||||||||||||
| Male (referent) | ||||||||||||
| Female | 1.78 | 1.38, 2.29 | 1.33 | 0.99, 1.78 | 0.78 | 0.63, 0.96 | 0.98 | 0.81, 1.19 | 1.20 | 1.00, 1.45 | 0.79 | 0.72, 0.87 |
| Marital status | ||||||||||||
| Never married (referent) | ||||||||||||
| Currently married/cohabiting | 2.07 | 1.15, 3.70 | 1.64 | 0.75, 3.61 | 0.67 | 0.31, 1.44 | 0.83 | 0.43, 1.62 | 1.03 | 0.60, 1.77 | 0.76 | 0.55, 1.03 |
| Widow/divorced/separated | 1.74 | 0.95, 3.18 | 1.33 | 0.62, 2.84 | 0.68 | 0.32, 1.48 | 0.87 | 0.44, 1.71 | 1.16 | 0.67, 2.00 | 0.81 | 0.58, 1.14 |
Abbreviations: CI, confidence interval; OR, odds ratio; Q, quintile.
Socioeconomic status (SES) measures—both educational level and wealth quintile—were negatively associated with untreated chronic diseases (Table 6). Older adults in the lower-SES groups (all countries pooled) were more likely to remain untreated than those with higher SES. The likelihood of not being treated for a chronic condition varied across countries. In general, compared with Russia, older adults of other countries were more likely to have untreated hypertension and angina. Compared with men, older women had a significantly higher likelihood of not being treated for angina and chronic lung diseases but a lower likelihood of not being treated for hypertension. Overall, SES and country of residence were the most significant variables determining the likelihood of untreated disease (Table 6).
Table 6.
Socioeconomic and Demographic Covariates of Untreated Morbidity in the Past 12 Months for Each of 6 Chronic Diseases in the Study on Global Ageing and Adult Health (Wave 1), 2007–2010
| Covariate | Angina | Arthritis | Asthma | Chronic Lung Disease | Depression | Hypertension | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Socioeconomic status | ||||||||||||
| Years of schooling | ||||||||||||
| No schooling | 1.93 | 1.20, 3.09 | 1.32 | 0.88, 1.98 | 1.28 | 0.72, 2.27 | 1.70 | 1.13, 2.54 | 2.92 | 1.44, 5.96 | 1.67 | 1.29, 2.15 |
| 1–5 | 1.19 | 0.77, 1.84 | 0.96 | 0.63, 1.47 | 1.31 | 0.77, 2.22 | 1.48 | 1.03, 2.12 | 1.35 | 0.74, 2.47 | 1.45 | 1.13, 1.87 |
| 6–9 | 0.91 | 0.60, 1.38 | 1.20 | 0.83, 1.72 | 1.24 | 0.77, 1.99 | 1.20 | 0.85, 1.68 | 1.18 | 0.60, 2.30 | 1.23 | 0.99, 1.52 |
| ≥10 (referent) | ||||||||||||
| Wealth quintile | ||||||||||||
| Q1 (lowest) | 2.25 | 1.43, 3.55 | 1.33 | 0.92, 1.93 | 0.94 | 0.58, 1.53 | 1.18 | 0.81, 1.71 | 1.27 | 0.64, 2.52 | 2.43 | 1.77, 3.35 |
| Q2 | 1.88 | 1.20, 2.95 | 1.15 | 0.81, 1.62 | 1.30 | 0.84, 2.01 | 1.30 | 0.84, 2.02 | 0.64 | 0.33, 1.27 | 1.74 | 1.31, 2.32 |
| Q3 | 1.24 | 0.74, 2.08 | 1.09 | 0.78, 1.53 | 0.98 | 0.59, 1.64 | 1.23 | 0.84, 1.80 | 0.91 | 0.43, 1.93 | 1.47 | 1.13, 1.91 |
| Q4 | 1.32 | 0.79, 2.22 | 1.19 | 0.76, 1.88 | 0.76 | 0.50, 1.17 | 1.53 | 1.07, 2.21 | 0.39 | 0.18, 0.82 | 1.35 | 1.03, 1.77 |
| Q5 (highest; referent) | ||||||||||||
| Country | ||||||||||||
| India | 9.83 | 6.11, 15.81 | 1.61 | 0.99, 2.62 | 0.48 | 0.24, 0.96 | 2.37 | 1.20, 4.71 | 2.81 | 1.25, 6.31 | 2.60 | 1.85, 3.66 |
| China | 0.85 | 0.55, 1.32 | 1.05 | 0.68, 1.63 | 0.89 | 0.48, 1.65 | 0.39 | 0.25, 0.61 | 2.39 | 1.04, 5.50 | 2.76 | 2.08, 3.67 |
| Ghana | 11.71 | 7.13, 19.22 | 3.10 | 1.91, 5.04 | 0.53 | 0.27, 1.06 | 4.95 | 2.50, 9.82 | 2.12 | 0.96, 4.68 | 6.99 | 4.99, 9.78 |
| Mexico | 32.66 | 10.32, 103.4 | 3.05 | 1.45, 6.40 | 2.32 | 0.90, 5.97 | 6.80 | 3.52, 13.12 | 1.08 | 0.37, 3.15 | 3.38 | 2.18, 5.25 |
| South Africa | 3.70 | 2.11, 6.48 | 1.01 | 0.64, 1.59 | 0.32 | 0.16, 0.63 | 1.44 | 0.78, 2.67 | 0.42 | 0.19, 0.90 | 3.32 | 2.44, 4.53 |
| Russia (referent) | ||||||||||||
| Age group, years | ||||||||||||
| 50–59 (referent) | ||||||||||||
| 60–69 | 0.96 | 0.68, 1.35 | 0.82 | 0.64, 1.05 | 0.78 | 0.53, 1.14 | 1.04 | 0.76, 1.43 | 1.59 | 0.85, 2.95 | 0.69 | 0.59, 0.81 |
| ≥70 | 0.48 | 0.32, 0.71 | 0.79 | 0.59, 1.06 | 0.75 | 0.54, 1.04 | 1.01 | 0.71, 1.42 | 0.88 | 0.46, 1.69 | 0.51 | 0.42, 0.60 |
| Residence | ||||||||||||
| Urban (referent) | ||||||||||||
| Rural | 1.01 | 0.69, 1.48 | 1.28 | 0.90, 1.83 | 1.30 | 0.75, 2.24 | 1.23 | 0.78, 1.95 | 0.89 | 0.49, 1.62 | 1.45 | 1.18, 1.79 |
| Sex | ||||||||||||
| Male (referent) | ||||||||||||
| Female | 1.75 | 1.20, 2.55 | 1.05 | 0.78, 1.41 | 1.12 | 0.80, 1.58 | 1.57 | 1.20, 2.04 | 0.66 | 0.37, 1.16 | 0.55 | 0.46, 0.65 |
| Marital status | ||||||||||||
| Never married (referent) | ||||||||||||
| Currently married/cohabiting | 1.79 | 0.82, 3.90 | 1.20 | 0.65, 2.22 | 0.64 | 0.27, 1.51 | 1.27 | 0.64, 2.53 | 0.36 | 0.10, 1.25 | 0.87 | 0.56, 1.34 |
| Widow/divorced/separated | 1.53 | 0.69, 3.39 | 0.91 | 0.48, 1.74 | 0.51 | 0.21, 1.24 | 1.27 | 0.61, 2.65 | 0.45 | 0.14, 1.51 | 0.88 | 0.55, 1.40 |
Abbreviations: CI, confidence interval; OR, odds ratio; Q, quintile.
DISCUSSION
In this study, we assessed sociodemographic patterns and correlates of self-reported, algorithm/measured test-based, undiagnosed, and untreated angina, arthritis, asthma, chronic lung disease, depression, and hypertension in 6 LMICs.
Results showed that algorithm/measured NCD prevalence was higher than self-reported prevalence for all 6 diseases in each of the 6 SAGE countries. These findings are consistent with the findings from previous studies in LMICs (18, 21–23). Prevalence of NCDs based on self-report of a physician's diagnosis typically underestimates the true extent of the chronic disease burden in these countries. Previous research suggests that the accuracy of self-reported prevalence estimates is influenced by health literacy, access to health care, and cultural factors (21, 24, 25). It is therefore critical to assess the reliability of self-reported disease estimates in LMICs against other measures, such as algorithm-based assessments or more objective measurements, to ascertain how well self-reported disease corresponds to a more objective assessment across multiple countries (26, 27).
Further, the estimates of chronic disease prevalence from algorithm/measured test-based assessment in this study were higher than the prevalence estimates for LMICs reported in other contemporary studies for angina (28–32), arthritis (30, 33), asthma (34, 35), and depression (36).
Rates of undiagnosed hypertension were also high in each SAGE country, with the highest undiagnosed prevalence of hypertension being observed in South Africa. China had the lowest prevalence of undiagnosed disease for all 6 chronic conditions, except hypertension. India had the highest prevalences of undiagnosed angina, asthma, and depression. Except for hypertension, South Africa and Mexico had more or less similar prevalences of undiagnosed NCDs. The rates of untreated morbidity were remarkably high for all 6 diseases in all SAGE countries.
Prevalences of self-reported, algorithm/measured test-based, and undiagnosed chronic disease were higher in older age groups. However, the age associations were less consistent for untreated chronic diseases. Overall, women had higher prevalences of self-reported, algorithm/measured test-based, undiagnosed, and untreated NCDs. Higher levels of education and wealth significantly reduced the odds of undiagnosed conditions and untreated morbidity. This was reported in earlier studies examining inequalities in health-care access and receipt of treatment for NCDs (37, 38).
Our finding of high prevalence of undiagnosed and untreated NCDs points to multiple gaps in NCD health-care provision in LMICs. Such gaps are known to exist in all the building blocks of the health system—namely governance, policies and plans, health-care delivery, health information systems, the health workforce, and access to essential technologies and medicines (1, 4, 39, 40). For example, a large proportion of people with high cardiovascular risk remain undiagnosed (41, 42), and even those diagnosed have insufficient access to treatment at the primary-care level (39). One of the major problems with NCD care in LMICs is the model of care, which is basically hospital-centered, where chronic conditions are treated as serial acute episodes with multiple visits to the hospital (4). Since chronic diseases need continuity of care, a hospital-centered approach may force patients to discontinue treatment or not seek treatment at all on account of financial constraints and limitations in access. Alongside systematic deficiencies in health-care delivery, persistent poverty and socioeconomic disparities in access to social and material resources in LMICs cause underutilization of health-care, which in turn leads to undiagnosed and untreated diseases (43).
These findings should be viewed in the light of following limitations. Undiagnosed disease prevalence was estimated as the proportion of older adults who failed to report having a disease yet exhibited a positive algorithm/measured test-based diagnosis. Given the limitations of algorithm-based measures (22), the symptom-based estimates used here may not have measured the prevalence of the undiagnosed chronic diseases with complete accuracy. However, more accurate clinical diagnostic procedures are often not feasible in large population-based surveys; thus, well-tested symptom-based assessments provide a pragmatic alternative (22). Importantly, these findings provide some insight into the undiagnosed prevalence of 6 chronic diseases. It is also noteworthy that cases of asthma and chronic obstructive pulmonary disease might overlap somewhat, as these 2 conditions share similar symptoms. Despite these limitations, this study provides new evidence of the high burden of undiagnosed and untreated diseases among older adults in a set of LMICs. It dispels the myth that these conditions impose a high health burden primarily in high-income countries and points to the marked treatment gap that exists in these countries as they move towards providing universal health coverage.
Alongside these limitations, this study had a number of strengths. First, the SAGE data set provided nationally representative estimates of the undiagnosed and untreated prevalence of 6 major chronic conditions in 6 LMICs. These 6 countries were home to 42% of the world's 1.4 billion people aged 50 years or older in 2010, 40% of the 771 million persons aged 60 years or older, and 38% of the 354 million people aged 70 years or older (44). Given that these are representative data, the findings presented here would be likely to represent around 50% of the world's older adult population. Additionally, the SAGE countries were strategically selected to capture populations from LMICs from all continents: According to the 2007 World Bank classification, Ghana and India were considered low-income countries and China, Mexico, Russia, and South Africa were considered middle-income countries (45). In addition, the prevalences of undiagnosed and untreated NCDs provided in this study were not available from previous studies; therefore, these findings have vital implications for health-care planning regarding NCDs in these countries.
In conclusion, LMICs face a substantial burden of chronic diseases, much of it undiagnosed and thus underestimated by self-reporting alone. This study revealed much higher algorithm/measured test-based prevalence rates of angina, chronic lung disease, depression, and hypertension than have been indicated by self-reports alone (21, 22). Furthermore, the high prevalence of undiagnosed NCDs and the even higher proportion of untreated NCDs demonstrate the inadequacy of current NCD diagnosis and management strategies in LMIC health-care systems. The results also show not only a higher burden of disease among women and low-SES individuals but also higher odds of undiagnosed and untreated disease among these groups, indicating inequities in health management as well as in disease risk. Future studies should incorporate more objective NCD measures to obtain an accurate measurement of chronic disease burden and to refine symptom-based algorithms based on robust validations; these efforts will also help ensure that all persons with a health condition receive proper diagnosis and treatment, ultimately alleviating the considerable burden of NCDs internationally.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: International Institute for Population Sciences, Mumbai, India (Perianayagam Arokiasamy, Uttamacharya); Study on Global Ageing and Adult Health (SAGE), Division of Information, Evidence and Research, World Health Organization, Geneva, Switzerland (Paul Kowal); Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota (Benjamin D. Capistrant); Department of Anthropology, College of Arts and Sciences, University of Oregon, Eugene, Oregon (Theresa E. Gildner, Melissa A. Liebert, Geeta Eick, Kirstin N. Sterner, J. Josh Snodgrass); Department of Biology, Vassar College, Poughkeepsie, New York (Elizabeth Thiele); Department of Community Health, College of Health Sciences, University of Ghana, Accra, Ghana (Richard B. Biritwum, Alfred E. Yawson, George Mensah); Russian Academy of Medical Sciences, Moscow, Russian Federation (Tamara Maximova); Shanghai Municipal Center for Disease Control and Prevention, Shanghai, China (Fan Wu, Yanfei Guo, Yang Zheng); Institute of Ageing in Africa, Department of Medicine, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa (Sebastiana Zimba Kalula); Center for Evaluation and Surveys Research, National Institute of Public Health, Cuernavaca, Morelos, Mexico (Aarón Salinas Rodríguez, Betty Manrique Espinoza); Department of Anthropology, Weinberg College of Arts and Sciences, Northwestern University, Evanston, Illinois (Tyler M. Barrett); School of Basic and Biomedical Sciences, University of Health and Allied Sciences, Ho, Ghana (Kwabena Duedu); School of Social Work, Boston University, Boston, Massachusetts (Ernest Gonzales); Epidemiology and Global Health Unit, Department of Public Health and Clinical Medicine, Faculty of Medicine, Umeå University, Umeå, Sweden (Nawi Ng); School of Public Health, University of Sydney, Sydney, New South Wales, Australia (Joel Negin); Beijing Tianton Hospital, Capital Medical University, Beijing, China (Yong Jiang); Research Centre for Generational Health and Ageing, University of Newcastle, Newcastle, New South Wales, Australia (Julie Byles); Global Clinical and Viral Laboratory, Durban, South Africa (Savathree Lorna Madurai); National Research Council, Neuroscience Institute, Padova, Veneto, Italy (Nadia Minicuci); and Department of Health Statistics and Information Systems, Division of Information, Evidence and Research, World Health Organization, Geneva, Switzerland (Nirmala Naidoo, Somnath Chatterji).
No specific funding was provided for this article. However, SAGE is supported by the World Health Organization and the US National Institute on Aging (interagency agreements OGHA 04034785, YA1323-08-CN-0020, and Y1-AG-1005-01 and grant R01-AG034479).
We acknowledge the expertise and contributions of the SAGE Principal Investigators and their respective survey teams in each country.
The donors played no role in study design, data collection, and analysis, the decision to publish, or the preparation of the manuscript.
Conflict of interest: none declared.
REFERENCES
- 1. World Health Organization Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 2. World Health Organization Global Health Estimates: Deaths by Cause, Age, Sex and Country, 2000–2012. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 3. World Health Organization Global Health Estimates Summary Tables: Projections of Deaths by Cause, Age and Sex by World Bank Income Category and WHO Region. Geneva, Switzerland: World Health Organization; 2013. http://www.who.int/healthinfo/global_burden_disease/GHE_DthWHOReg7_Proj_2015_2030.xls?ua=1. Accessed March 28, 2016. [Google Scholar]
- 4. Allotey P, Reidpath DD, Yasin S, et al. . Rethinking health-care systems: a focus on chronicity. Lancet. 2011;377(9764):450–451. [DOI] [PubMed] [Google Scholar]
- 5. Samb B, Desai N, Nishtar S, et al. . Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376(9754):1785–1797. [DOI] [PubMed] [Google Scholar]
- 6. Remais JV, Zeng G, Li G, et al. . Convergence of non-communicable and infectious diseases in low- and middle-income countries. Int J Epidemiol. 2013;42(1):221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Allotey P, Davey T, Reidpath DD. NCDs in low and middle-income countries—assessing the capacity of health systems to respond to population needs. BMC Public Health. 2014;14(suppl 2):S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ebrahim S, Pearce N, Smeeth L, et al. . Tackling non-communicable diseases in low- and middle-income countries: is the evidence from high-income countries all we need. PLoS Med. 2013;10(1):e1001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reddy KS. India's aspirations for universal health coverage. New Engl J Med. 2015;373(1):1–5. [DOI] [PubMed] [Google Scholar]
- 10. Galobardes B, Lynch J, Smith GD. Measuring socioeconomic position in health research. Br Med Bull. 2007;81–82:21–37. [DOI] [PubMed] [Google Scholar]
- 11. Hosseinpoor AR, Bergen N, Mendis S, et al. . Socioeconomic inequality in the prevalence of noncommunicable diseases in low- and middle-income countries: results from the World Health Survey. BMC Public Health. 2012;12:474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Joshi R, Chow CK, Raju PK, et al. . The Rural Andhra Pradesh Cardiovascular Prevention Study (RAPCAPS): a cluster randomized trial. J Am Coll Cardiol. 2012;59(13):1188–1196. [DOI] [PubMed] [Google Scholar]
- 13. Sankoh O, Byass P. The INDEPTH Network: filling vital gaps in global epidemiology. Int J Epidemiol. 2012;41(3):579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kowal P, Chatterji S, Naidoo N, et al. . Data resource profile: the World Health Organization Study on global AGEing and adult health (SAGE). Int J Epidemiol. 2012;41(6):1.6 39–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Naidoo N. WHO's Study on Global AGEing and Adult Health (SAGE) waves 0 and 1—sampling information for China, Ghana, India, Mexico, Russia and South Africa. (SAGE Working Paper no. 5). Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 16. Rose GA. The diagnosis of ischaemic heart pain and intermittent claudication in field surveys. Bull World Health Organ. 1962;27:645–658. [PMC free article] [PubMed] [Google Scholar]
- 17. Fischbacher CM, Bhopal R, Unwin N, et al. . The performance of the Rose angina questionnaire in South Asian and European origin populations: a comparative study in Newcastle, UK. Int J Epidemiol. 2001;30(5):1009–1016. [DOI] [PubMed] [Google Scholar]
- 18. Moussavi S, Chatterji S, Verdes E, et al. . Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. [DOI] [PubMed] [Google Scholar]
- 19. Kessler RC, Ustün TB. The World Mental Health (WMH) Survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Whitworth JA. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. World Health Organization, International Society of Hypertension Writing Group J Hypertens. 2003;21(11):1983–1992. [DOI] [PubMed] [Google Scholar]
- 21. Vellakkal S, Millett C, Basu S, et al. . Are estimates of socioeconomic inequalities in chronic disease artefactually narrowed by self-reported measures of prevalence in low-income and middle-income countries? Findings from the WHO-SAGE survey. J Epidemiol Community Health. 2015;69(3):218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Levesque JF, Mukherjee S, Grimard D, et al. . Measuring the prevalence of chronic diseases using population surveys by pooling self-reported symptoms, diagnosis and treatments: results from the World Health Survey of 2003 for South Asia. Int J Public Health. 2013;58(3):435–447. [DOI] [PubMed] [Google Scholar]
- 23. Wu F, Guo Y, Kowal P, et al. . Prevalence of major chronic conditions among older Chinese adults: the Study on Global AGEing and adult health (SAGE) wave 1. PLoS One. 2013;8(9):e74176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kriegsman DM, Penninx BW, van Eijk JT, et al. . Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996;49(12):1407–1417. [DOI] [PubMed] [Google Scholar]
- 25. Mackenbach JP, Looman CW, van der Meer JB. Differences in the misreporting of chronic conditions, by level of education: the effect on inequalities in prevalence rates. Am J Public Health. 1996;86(5):706–711.8629723 [Google Scholar]
- 26. Gross R, Bentur N, Elhayany A, et al. . The validity of self-reports on chronic disease: characteristics of underreporters and implications for the planning of services. Public Health Rev. 1996;24(2):167–182. [PubMed] [Google Scholar]
- 27. Capistrant BD, Glymour MM, Berkman LF. Assessing mobility difficulties for cross-national comparisons: results from the World Health Organization Study on Global AGEing and adult health. J Am Geriatr Soc. 2014;62(2):329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328(7443):807–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Srinath Reddy K, Shah B, Varghese C, et al. . Responding to the threat of chronic diseases in India. Lancet. 2005;366(9498):1744–1749. [DOI] [PubMed] [Google Scholar]
- 30. Van Minh H, Ng N, Juvekar S, et al. . Self-reported prevalence of chronic diseases and their relation to selected sociodemographic variables: a study in INDEPTH Asian sites, 2005. Prev Chronic Dis. 2008;5(3):A86. [PMC free article] [PubMed] [Google Scholar]
- 31. Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006;124(3):235–244. [PubMed] [Google Scholar]
- 32. Ramaraj R, Alpert JS. Indian poverty and cardiovascular disease. Am J Cardiol. 2008;102(1):102–106. [DOI] [PubMed] [Google Scholar]
- 33. Joshi VL, Chopra A. Is there an urban-rural divide? Population surveys of rheumatic musculoskeletal disorders in the Pune region of India using the COPCORD Bhigwan model. J Rheumatol. 2009;36(3):614–622. [DOI] [PubMed] [Google Scholar]
- 34. Aggarwal AN, Chaudhry K, Chhabra SK, et al. . Prevalence and risk factors for bronchial asthma in Indian adults: a multicentre study. Indian J Chest Dis Allied Sci. 2006;48(1):13–22. [PubMed] [Google Scholar]
- 35. Jindal SK. Bronchial asthma: the Indian scene. Curr Opin Pulm Med. 2007;13(1):8–12. [DOI] [PubMed] [Google Scholar]
- 36. Hosain GM, Chatterjee N, Ara N, et al. . Prevalence, pattern and determinants of mental disorders in rural Bangladesh. Public Health. 2007;121(1):18–24. [DOI] [PubMed] [Google Scholar]
- 37. Di Cesare M, Khang YH, Asaria P, et al. . Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381(9866):585–597. [DOI] [PubMed] [Google Scholar]
- 38. Yusuf S, Islam S, Chow CK, et al. . Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–1243. [DOI] [PubMed] [Google Scholar]
- 39. Mendis S, Al Bashir I, Dissanayake L, et al. . Gaps in capacity in primary care in low-resource settings for implementation of essential noncommunicable disease interventions. Int J Hypertens. 2012;2012:584041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mendis S, Fukino K, Cameron A, et al. . The availability and affordability of selected essential medicines for chronic diseases in six low- and middle-income countries. Bull World Health Organ. 2007;85(4):279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Health Organization Prevention of Recurrent Heart Attacks and Strokes in Low and Middle Income Populations: Evidence Based Recommendations for Policy-Makers and Health Professionals. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 42. Gakidou E, Mallinger L, Abbott-Klafter J, et al. . Management of diabetes and associated cardiovascular risk factors in seven countries: a comparison of data from national health examination surveys. Bull World Health Organ. 2011;89(3):172–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Peters DH, Garg A, Bloom G, et al. . Poverty and access to health care in developing countries. Ann NY Acad Sci. 2008;1136:161–171. [DOI] [PubMed] [Google Scholar]
- 44. US Census Bureau International Programs. International Data Base. 2012. www.census.gov/population/international/data/idb/informationGateway.php. Updated August 2016. Accessed February 27, 2012.
- 45. Swanson E. World Development Indicators '07. Washington, DC: World Bank; 2007; http://documents.worldbank.org/curated/en/336241468138277212/pdf/541660WDI0200710Box345641B01PUBLIC1.pdf. Accessed February 6, 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.