Abstract
Rationale:
Intragastric bezoar is a stony mass found trapped in the stomach, though it can occur in other locations of the gastro-intestinal tract. The etiology of intragastric bezoar is multifactorial, includes certain risk factors and predisposing factors such as coexisting medical disorders, anatomic abnormalities, and gastric motility disorders, which contribute to the development of intragastric bezoar.
Patient concerns:
In this report, we present a rare case of intragastric bezoar with epigastric pain after prolonged consumption of jujubes. To our knowledge, this is the first case of intragastric bezoar to be reported after jujubes ingestion.
Diagnoses:
An upper gastrointestinal (GI) endoscopy performed which revealed an 8 × 5-cm intragastric diospyrobezoar with an adjacent necrotic pressure ulcer of size 0.8 × 0.5-cm without signs of bleeding.
Interventions:
For therapeutic intervention, Coca-Cola ingestion and lithotripsy were applied.
Outcomes:
The therapeutic course was uneventful. There was no recurrence during 1-year follow-up.
Lessons:
In our literature, jujube emerged as a new player. A bezoar composed of unripened fruit content in the stomach, could be the cause of chronic abdominal pain, dyspepsia, gastric reflux or heartburn. Moreover, this study provides a detailed overview of recently published literature regarding intragastric manifestations of bezoar, etiological factors, diagnostic and therapeutic approaches.
Keywords: case presentation, intragastric bezoar, jujube, risk factors
1. Introduction
Bezoars are collections or concretions of undigested material anywhere in the gastro-intestinal tract (GIT), and most commonly found in the stomach due to altered or normal gastric physiology, abnormal GI motility, weakened gastric emptying, and other coexisting illness.[1,2] Bezoars occur frequently in people with certain risk factors, or comorbid conditions. Bezoars are classified according to the material that forms them, such as, phytobezoars or diospyrobezoars; indigestible fruit or vegetable content, trichobezoars; hair, lactobezoars; milk products and pharmacobezoars; tablets and medications.[3] In theory, all undigested and partly-digested foodstuffs together with gastric mucus can be a source of gastric bezoar. For decades, the jujubes fruit and its seeds have been commonly used among Chinese population as food and herbal medication for numerous health purposes.[4] Most intragastric bezoars occur in teenagers and young women with pica history, mainly with psychiatric disorders. By contrast, in adults, most intragastric bezoars are related to gastroparesis, anatomical abnormalities, and former gastric surgeries that decrease gastric motility.[5] The aim of this study was to raise alertness among clinicians that patients with certain etiological factors are at high risk of intragastric bezoar formation.
2. Case presentation
A 49-year-old male visited the digestive department of Tianjin Medical University General Hospital for evaluation of his symptoms. The patient presented with epigastric pain, nausea and vomiting dyspepsia, and gastric reflux for 4 months. Neither particular comorbidities—nor a specific diet was described in his personal history, except for habitual jujubes ingestion.
2.1. Physical checkup and investigation
On admission, he appeared anemic, but no change in weight loss was observed; moreover, an abdominal examination revealed abdominal tenderness. All other physical examinations were essentially normal. His medical history included controlled hypertension (3 years) but did not include drug treatments, medication, alcohol, or family risk factors for any illness. Initial laboratory investigations were insignificant except a hemoglobin level of 11.5 g/dL. An upper GI X-ray with air contrast was performed, which showed a distended stomach that appeared to be partially filled with debris, along with a normally filled duodenum.
An upper GI endoscopy performed at our institution, which demonstrated an 8 × 5-cm-diameter diospyrobezoar in the gastric body (Fig. 1) with an adjacent necrotic pressure ulcer of size 0.8 × 0.5 cm, located in the posterior wall of gastric pylorus without signs of bleeding (Fig. 2).
Figure 1.
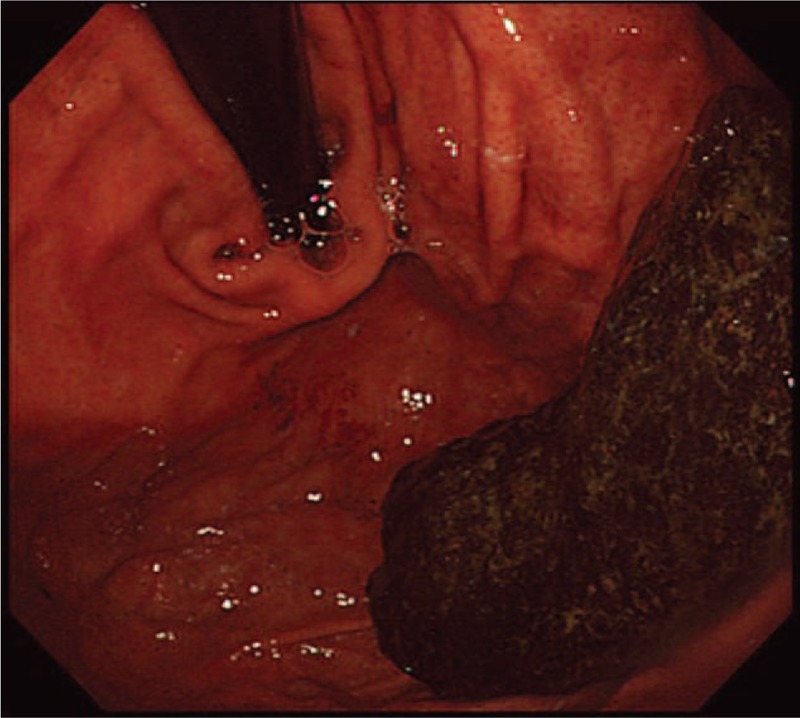
Upper GI endoscopy showing a giant 8 × 5-cm-diameter gastric diospyrobezoar.
Figure 2.

Upper GI endoscopy showing a necrotic pressure ulcer of size 0.8 × 0.5 cm (white coated).
2.2. Therapeutic intervention
For dissolution of the intragastric bezoar, the patient underwent Coca-Cola diet for 1 week. After a week of Coca-Cola ingestion, reexamination of the stomach showed partly dissolution of the bezoar. The residual intragastric bezoar was endoscopically fragmented by lithotripter and excellently retrieved with biopsy forceps and snares on multiple attempts. The patient discharged home on the same day with antacids regimen, and he recovered without complications. There was no recurrence during 1-year follow-up.
3. Discussion
An intragastric bezoar is a firmly packed collection of partly digested or undigested food content that is incapable to exit the stomach. This case is suggestive because, for decades, the jujube fruit and its seeds have been commonly used among Chinese population as food and herbal medication for multiple health purposes.[6] Recently, in China, the gastroenterologist frequently encounters intragastric bezoars in patients with a history of jujubes ingestion. This is the first intragastric bezoar after jujube ingestion to be reported (Fig. 3).
Figure 3.

Jujube fruit (Ziziphus jujuba).
The etiology of intragastric bezoar is multifactorial. Bezoars occur most often but not always associated with certain risk factors. However, people are definitely at risk when high-fibers diet in the areas or cultures/beliefs with a high ingestion of vegetables and fruits rich in fibers content. High-fiber diets are being recommended by the health institutes and producers of high-fiber foods. Though, this recommendation is applicable to the majority of customers and especially old-age population. But some people who underwent surgical procedures for abdomen such as gastric surgeries are prone to form phytobezoars and should avoid certain kinds of fiber to the diet. Diospyrobezoar is a kind of phytobezoar made from unripened-persimmons, coconuts, and jujubes. Moreover, undigested milk products which are frequently found in premature kids receiving formula foods, medications that do not properly dissolve in the GIT, pica ingestion that are characterized by a desire for substances that are mainly nonnutritious, such as ice; pagophagia, paper; papyrophagia, drywall or paint, metal; metallophagia, stones; lithophagia or soil; geophagia, glass; hyalophagia or feces; coprophagia and chalk, impaired mastication; dentate subjects and denture wearers are known to present with vastly different mastication efficacy inspissation, and honeycomb ingestion, etc (Table 1).[7–9] Other comorbid conditions such as first, coexisting medical disorders which includes psychiatric disorders, gastrointestinal amyloidosis, and certain systemic illnesses such as diabetes mellitus, cystic fibrosis, Guillain–Barre syndrome, bouveret's syndrome, hypothyroidism, renal failure, scleroderma, myotonic dystrophy, Ménétrier's disease, and hypochlorhydria or achlorhydria etc, have been associated with a higher risk of bezoar formation. Second, anatomic abnormalities include gastric diverticula's, gastric outlet obstruction, and cholecystogastric fistula. Third, gastric motility disorders, which includes gastroparesis and previous gastric surgeries (Table 2).[8–15]
Table 1.
Risk factors associated intragastric bezoar.

Table 2.
Coexisting medical disorders associated intragastric bezoar.

Intragastric bezoars can be asymptomatic or exist with a variety of GI symptoms such as nausea, vomiting, delayed gastric emptying, and weight loss.[16] Intragastric bezoars can also cause gastric ulcers, gastric outlet obstruction, peritonitis, and rarely gastric perforation.[10,16] Thus, early diagnosis and treatment of intragastric bezoars are vigorous to avoid bezoar-induced complications. Symptoms related to GI bleeding such as hematemesis, bloodstained stool, anemia, and fainting are the result of the gastric ulceration due to pressure necrosis caused by the bezoar.[5]
The standard diagnostic approach for intragastric bezoar includes upper GI endoscopy, abdominal ultrasound, computed tomography, or barium meal.[9] However, in our case, an upper GI X-ray with air contrast also showed promising results. According to Iwamuro et al[17] second-look upper GI endoscopy is paramount to detect intragastric bezoars in patients with gastric ulcers or gastric debris. Physical checkup has limited efficacy in diagnosing intragastric mass. Rarely, an abdominal examination may reveal a palpable mass[1] or halitosis[5] from the putrefying stuff inside the stomach. Yet, these outcomes are not definite and often hard to differentiate.
Management and dissolution of an intragastric bezoar may consist of either a medical, endoscopic or surgical method. As a medical approach toward the treatment of intragastric bezoar, there are 3 treatment modalities. First, conservative treatment for softening the intragastric bezoar includes (prokinetics, enzymes cellulose/papain, and Coca-Cola irrigations).[7,18] Second, most small size intragastric bezoars may pass through the digestive tract themselves or can be removed by upper GI endoscopic approach via (biopsy forceps, alligator forceps, polypectomy snares, needle-knife, lithotripters, argon plasma coagulation, and endoscopic lithotripsy with Nd:YAG laser-ignited mini-explosive technique).[7,19] Third, however, the best technique for the larger ones is surgical removal. A laparoscopic technique with Alexis wound retractor has been used successfully in the treatment of bezoars.[7] Ulukent et al[20] reported a new modified laparoscopic method wherein an endobag is located in the stomach instead of the peritoneal cavity in order to prevent spillage of the bezoar through laparoscopic removal. Recently, holmium:YAG laser lithotripsy has shown a promising result in the management of massive gastric phytobezoar.[19] Moreover, psychiatric therapy and dietary education are recommended.[2] Endoscopic examination for surveillance should be carried out if the disease recurs frequently.
3.1. Conclusion and future perspectives
Gastric diospyrobezoar, a bezoar composed of unripened fruit content in the stomach, could be the cause of chronic abdominal pain, dyspepsia, gastric reflux, or heartburn. In our literature, jujube emerged as a new player, and we believe there might be other uncountable risk factors which contribute to the development of intragastric bezoar but have not yet known to the clinicians. Thus, the clinicians especially gastroenterologist should be more focus on patient history in order to disclose the unrevealed information and risk factors. The best treatment for a diospyrobezoar is prevention based on good eating habits and oral hygiene, particularly in subjects with a history of existing illness, anatomical abnormalities, gastric motility disorders, and gastric or abdominal surgery.
More research is needed, in order to fully understand the gastric pathogenic environment and the association of intragastric bezoar with other comorbid conditions.
Author contributions
All the persons who have made substantial contributions to the work reported in the manuscript, e.g., technical help, writing and editing assistance and general supports. Their names declared in the author list. The authors SK & IAK contributed to the paper in writing, data collection and editing the manuscript. KU, SK, and XW contributed to data research, MUR & LPZ contributed in endoscopic data retrieval, BMW & XC contributed to conception. All authors read and approved the final manuscript.
Conceptualization: Xin CHEN, Bang-mao WANG.
Data curation: Ifthikhan-ahmad Khan, Kifayat Ullah, Saima Khan, Mujeeb ur Rehman.
Formal analysis: Ifthikhan-ahmad Khan, Xuan Wang.
Investigation: Samiullah Khan, Ifthikhan-ahmad Khan, Lan-ping ZHU.
Methodology: Samiullah Khan, Ifthikhan-ahmad Khan.
Software: Samiullah Khan, Lan-ping ZHU.
Supervision: Samiullah Khan, Ifthikhan-ahmad Khan, Xuan Wang.
Validation: Mujeeb ur Rehman.
Visualization: Samiullah Khan, Kifayat Ullah, Saima Khan, Xuan Wang, Lan-ping ZHU, Bang-mao WANG.
Writing – original draft: Samiullah Khan.
Writing – review & editing: Samiullah Khan, Bang-mao WANG.
Footnotes
Abbreviation: GIT = gastro-intestinal tract.
B-mW & XC equally contributed to the study conception.
Funding/support: None declared.
This study was approved by the Human Ethics Review Committee of Tianjin Medical University General Hospital, Tianjin, (PR China).
Consent for publication and Ethics approval: Written informed consent was obtained from the patient for publication of this case report.
The authors have no conflicts of interest to disclose.
References
- [1].Eng K, Kay M. Gastrointestinal bezoars: history and current treatment paradigms. Gastroenterol Hepatol 2012;8:776–8. [PMC free article] [PubMed] [Google Scholar]
- [2].Amjad W, Upadhya G, Hurairah A, et al. Endoscopic shaving of hair in a gastric bypass patient with a large bezoar. BMJ Case Rep 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Nour I, Abd Alatef M, Megahed A, et al. Rapunzel syndrome (gastric trichobezoar), a rare presentation with generalised oedema: case report and review of the literature. Paediatr Int Child Health 2017;1–3. [DOI] [PubMed] [Google Scholar]
- [4].Chen J, Liu X, Li Z, et al. A review of dietary Ziziphus jujuba Fruit (Jujube): developing health food supplements for brain protection. Evid Based Complement Alternat Med 2017;2017:3019568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chacko A, Masters BI, Isles A. Giant gastric bezoar complicating congenital esophageal atresia repaired by gastric interposition—a case report. Front Pediatr 2017;5:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chen J, Liu X, Li Z, et al. A review of dietary Ziziphus jujuba Fruit (Jujube): developing health food supplements for brain protection. Evid Based Complement Alternat Med 2017;2017:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ugenti I, Travaglio E, Lagouvardou E, et al. Successful endoscopic treatment of gastric phytobezoar: a case report. Int J Surg Case Rep 2017;37:45–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sarikaya M, Koçak E, Köklü S, et al. Acute gastric obstruction resulting from gallstone-induced bezoar. Am Surg 2012;78:E529. [PubMed] [Google Scholar]
- [9].Katsinelos P, Pilpilidis I, Chatzimavroudis G, et al. Huge gastric bezoar caused by honeycomb, an unusual complication of health faddism: a case report. Cases J 2009;2:7077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Parakh JS, McAvoy A, Corless DJ. Rapunzel syndrome resulting in gastric perforation. Ann R Coll Surg Engl 2016;98:e6–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Soga K, Kassai K, Itani K, et al. Gastric outlet obstruction induced by a gastric wall abscess after cholecystitis. Intern Med 2014;53:2675–8. [DOI] [PubMed] [Google Scholar]
- [12].Pan W, Wang Z, Tian F, et al. Electroacupuncture combined with mosapride alleviates symptoms in diabetic patients with gastroparesis. Exp Ther Med 2017;13:1637–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mohammad MK, Pepper DJ, Kedar A, et al. Measures of autonomic dysfunction in diabetic and idiopathic gastroparesis. Gastroenterol Res 2016;9:65–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Liu N, Abell T. Gastroparesis updates on pathogenesis and management. Gut Liver 2017;11:579–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Cortes C, Silva C. Gastric bezoar as complication of gastric banding. Report of one case. Rev Med Chil 2008;136:1457–9. [DOI] [PubMed] [Google Scholar]
- [16].Gachabayov M, Abdullaev A, Mityushin P, et al. Each worm to his taste: some prefer to eat nettles—a giant gastric phytobezoar. Clin Case Rep 2016;4:710–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Iwamuro M, Tanaka S, Moritou Y, et al. Importance of second-look endoscopy on an empty stomach for finding gastric bezoars in patients with gastric ulcers. Acta Med Okayama 2017;71:241–7. [DOI] [PubMed] [Google Scholar]
- [18].Ladas SD, Kamberoglou D, Karamanolis G, et al. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther 2013;37:169–73. [DOI] [PubMed] [Google Scholar]
- [19].Grande G, Manno M, Zulli C, et al. An alternative endoscopic treatment for massive gastric bezoars: Ho:YAG laser fragmentation. Endoscopy 2016;48(Suppl 1):E217. [DOI] [PubMed] [Google Scholar]
- [20].Ulukent SC, Ozgun YM, Sahbaz NA. A modified technique for the laparoscopic management of large gastric bezoars. Saudi Med J 2016;37:1022–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


