Abstract
Rationale:
Among the patients who complain of neuralgia in the upper extremities, it is very rare to be caused by the first thoracic (T1) spinal nerve dermatome.
Patient concerns:
A 65-year-old presented with neuropathic pain of the left medial antebrachial cutaneous nerve and the medial brachial cutaneous nerve for 2 months.
Diagnoses:
Electrodiagnostic study revealed left thoracic radiculopathy mainly involving the T1 nerve root. Cervical spine magnetic resonance imaging revealed a metastatic tumor of T1 vertebral body compressing the left spinal cord and nerve root. After a systemic diagnostic work-up, he was finally diagnosed with primary hepatocellular carcinoma.
Interventions:
He received transarterial chemoembolization in the liver and radiotherapy to the T1 spine.
Outcomes:
After radiotherapy, the neuropathic pain was slightly improved.
Lessons:
If the patient is suspected of having thoracic radiculopathy, the physician should consider not only a herniated disc disease but also systemic disease. Because the prevalence of thoracic radiculopathy is very low and there is a high incidence of cancer that can spread to the spine in the elderly.
Keywords: neoplasm metastasis, neuropathic pain, radiculopathy
1. Introduction
Neuralgia of the upper extremity is common problem in the clinical practice and caused by various conditions. Mononeuropathy like carpal tunnel syndrome is most common and cervical radiculopathy is also common. Most radiculopathies arise from nerve root compression. The 2 predominant mechanisms of compressive radiculopathy are spondylosis and disc herniation.[1] In approximately 20% of patients, spinal cord compression by metastatic tumors is an initial sign of malignancy[2] and between 5% and 10% of all cancer patients develop spinal metastases during the course of their disease.[3] Metastatic spinal tumors can cause pain and various neurologic symptoms. They usually affect the lower thoracic or lumbosacral spine and cause symptoms related to the spinal nerve roots or spinal cord. Involvement of the cervical and upper thoracic spine is rare and the incidence of thoracic radiculopathy is very low in practice (approximately 0.15%–4%).[4] In this case report, we describe a patient who initially presented with neuropathic pain in the first thoracic (T1) dermatome, which was caused by hepatocellular carcinoma (HCC) with T1 spinal metastasis.
2. Case presentation
A 65-year-old man presented with a 2-month history of neuropathic pain in the left upper extremity. He complained of a tingling sensation and hypoesthesia on the dermatome of the left medial antebrachial cutaneous nerve (MABC) and medial brachial cutaneous nerve (MBC). Additionally, the patient complained of mild weakness and atrophy of the left abductor pollicis brevis, adductor digiti minimi, and first dorsal interosseous muscles. Deep tendon reflexes of the biceps brachii and triceps brachii muscles were normal and upper motor neuron sign such as Hoffmann reflex were not observed. Clinically, cervicothoracic radiculopathy involving the C8-T1 nerve roots was suspected and electrodiagnostic study (EDx) was conducted. A sensory nerve conduction study (NCS) showed normal response. However, a motor NCS showed reduced amplitude of the median nerve recording from left abductor pollicis brevis muscle compared with the right (right: 12.0 mV, left: 7.8 mV) (Table 1). Needle electromyography detected abnormal spontaneous activity in the left abductor pollicis brevis (APB), first dorsal interosseus (FDI), and T1-T2 paraspinal muscles (Table 2). In summary, EDx study revealed left thoracic radiculopathy mainly involving the T1 nerve root. Because the incidence of thoracic radiculopathy is very low, we conducted laboratory blood test and magnetic resonance imaging (MRI) of the cervical spine to identify the anatomic lesion and other disease. In a blood test, there was no abnormality other than elevation of creatinine kinase to 426 IU/L. The spine MRI revealed a hypointense lesion of the T1 vertebral body compressing the left spinal cord and nerve root (Fig. 1). These findings are a typical feature of metastatic tumors. Further studies on tumor markers have resulted in elevated levels of prothrombin in vitamin K absence level (383mAU/mL, normal range < 40 mAU/mL). We consulted the oncology department for further evaluation. The patient was finally diagnosed with primary HCC (Fig. 2) with T1 radiculopathy due to a spinal metastatic lesion. He was transferred to the gastroenterology department and received transarterial chemoembolization in the liver. He is now undergoing radiotherapy to the T1 spine in the outpatient clinic, and his neuropathic pain is slightly improved. The patient signed informed consent. In our case, the patient accepted regular examinations and proved therapy, so the ethical approval was not necessary.
Table 1.
Nerve conduction study of the patient.

Table 2.
Results of needle electromyography.
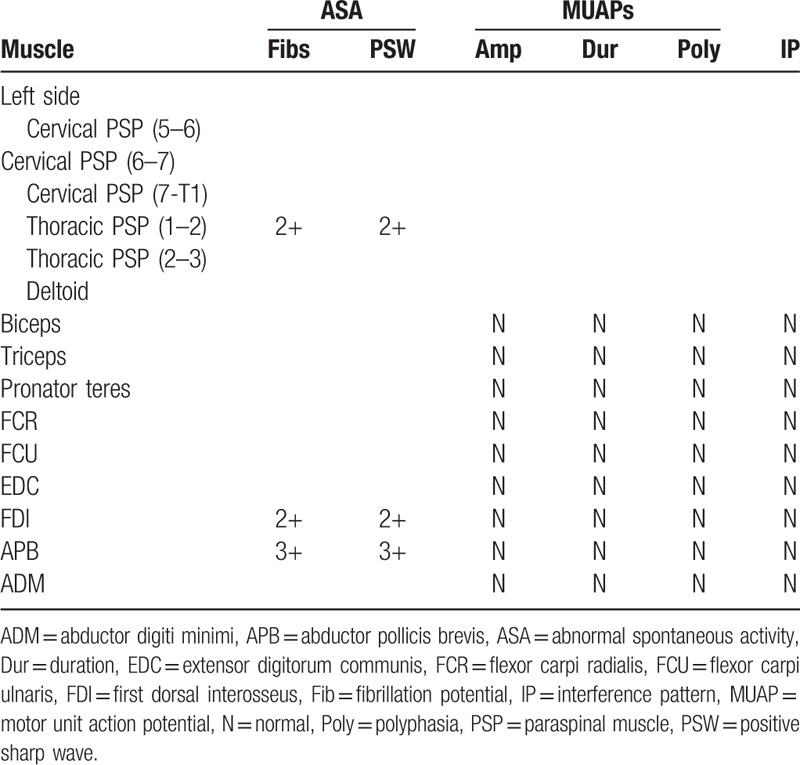
Figure 1.
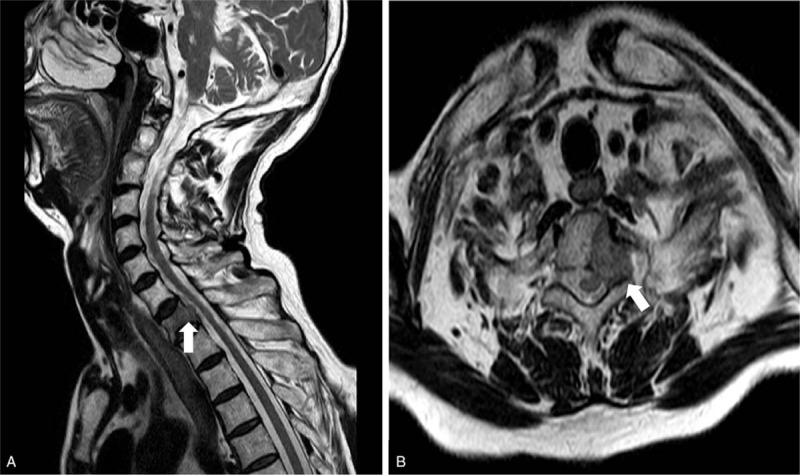
(A) Sagittal T2 weighted magnetic resonance imaging (MRI) of spine revealed metastatic lesion (white arrow) on T1 vertebral body. (B) Horizontal T2 weighted MRI of spine shows the mass (white arrow) compressing the left spinal cord and nerve root.
Figure 2.
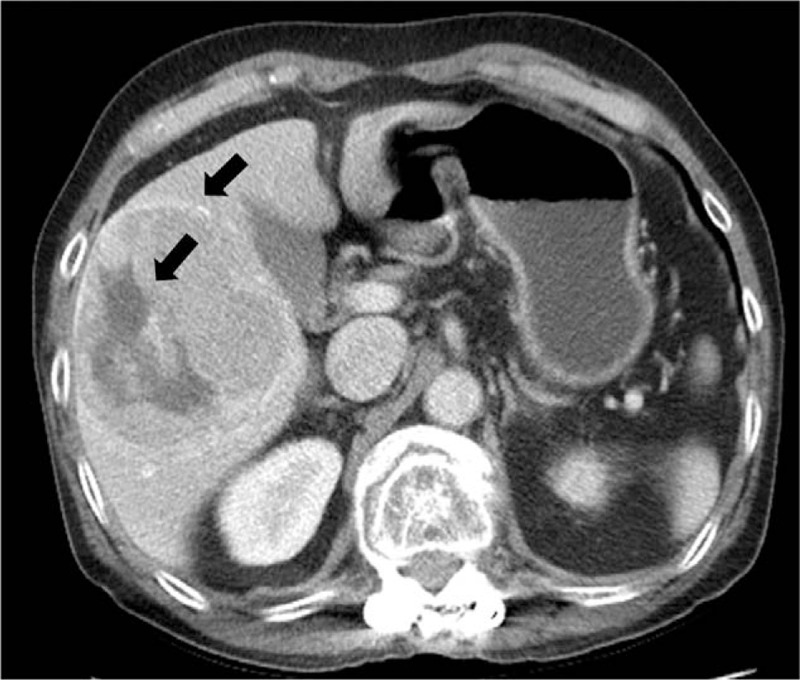
Enhanced abdomen-pelvic computed tomography revealed 9 cm sized encapsulated heterogeneous enhancing mass (black arrow) with central low-density portion in liver segment 5 and 6.
3. Discussion
HCC metastases are a significant cause of cancer-related morbidity and mortality and the incidence is expected to increase with the improvements in systemic therapies.[5] Especially, within the skeletal system, the spinal column is the most common site of metastasis.[6] Metastatic tumors of the spine are known to cause early aggravation or neurological symptoms. Edema and hemorrhage of the tumor and rapid tumor growth or secondary obstruction of spinal blood vessels may rapidly aggravate the symptoms.[7]
At first visit, malignant tumors were not suspected in this patient because he did not have systemic symptoms such as unintended weight loss, fever, excessive fatigue and HCC-related symptoms like jaundice, abdominal pain, and palpable mass. Early detection of metastatic spinal tumors is critical because the functional outcome rely on the neurological status of the patient at the time of presentation.[3]
In this case, the initial symptom was only neuropathic pain in the medial aspect of left upper arm and forearm innervated by MABC and MBC. The MABC originates from the medial cord of the brachial plexus and consists mainly of C8 and T1 spinal nerves. The MABC courses distally 10 cm above the medial epicondyle and divided branches providing the sensory supply of the medial aspect of forearm.[8] The MBC providing the sensory supply of the medial aspect of the upper arm arises from the medial cord of the brachial plexus and consists mainly of T1 spinal nerve.[9] The lesion of MABC and MBC produce only sensory discomfort and do not cause weakness of the hand muscles, and rarely occur without special injury.[10] Therefore, it is appropriate to consider the abnormalities of C8 and T1 spinal nerve root that constitutes the medial cord from which 2 nerves originate. The findings of abnormal spontaneous activities of the APB muscle in the needle electromyography and decreased amplitude of left median nerve compared with right one also support the T1 radiculopathy. Although the nerve distribution of the paraspinalis and the FDI muscle are overlapped and inaccurate, the APB muscle is predominantly innervated by T1 spinal nerve root.[11]
The 3 treatment modalities for metastatic spinal tumors are chemotherapy, radiation therapy, and surgery. However, chemotherapy is not preferred because it has limited efficacy except for chemosensitive tumors such as neuroblastoma, Ewing's sarcoma, osteogenic sarcoma, germ cell tumors, and lymphoma.[3] When determining radiation therapy or surgical treatment, various factors should be taken into consideration. Yasukai et al. systematically organized the scoring system. The total score of the evaluation system was 15 points, which was determining by systemic status, metastasis to external bones or internal organs, location of primary lesion, and degree of paralysis. According to this system, the patient in this case was in good general condition, no extraspinal lesion, and slight weakness, but the primary lesion was liver and poor prognosis was expected compared with other sites. This patient was expected to survive for more than 6 months with a total score of 11, and excisional surgery for spinal tumor was possible.
In conclusion, we report a rare case of thoracic radiculopathy as initial sign of hepatocellular carcinoma. If the patient is suspected of having thoracic radiculopathy, the physician should consider not only herniated disc diseases but also systemic diseases because the prevalence of thoracic radiculopathy is very low. Especially in the elderly, it is necessary to keep in mind the possibility of malignant disease and a systemic diagnostic work-up can be an effective approach.
Author contributions
Supervision: Sooa Kim, Kiyoung Oh.
Writing – original draft: Yongmin Kim.
Writing – review & editing: Yuntae Kim.
Footnotes
Abbreviations: EDx = electrodiagnostic study, HCC = hepatocellular carcinoma, MABC = medial antebrachial cutaneous nerve, MBC = medial brachial cutaneous nerve.
This research was supported by the Soonchunhyang University Research Fund.
The authors have no conflicts of interest to disclose.
References
- [1].Kim K-T, Kim Y-B. Cervical radiculopathy due to cervical degenerative diseases: anatomy, diagnosis and treatment. J Korean Neurosurg Soc 2010;48:473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Constans JP, de Divitiis E, Donzelli R, et al. Spinal metastases with neurological manifestations: review of 600 cases. J Neurosurg 1983;59:111–8. [DOI] [PubMed] [Google Scholar]
- [3].Bilsky MH, Eric L, Raizer J, et al. The diagnosis and treatment of metastatic spinal tumor. Oncologist 1999;4:459–69. [PubMed] [Google Scholar]
- [4].Arce CA, Dohrmann GJ. Thoracic disc herniation: improved diagnosis with computed tomographic scanning and a review of the literature. Surg Neurol 1985;23:356–61. [DOI] [PubMed] [Google Scholar]
- [5].Tokuhashi Y, Matsuzaki H, Oda H, et al. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine 2005;30:2186–91. [DOI] [PubMed] [Google Scholar]
- [6].Schmidt PKJaMH. Surgical management of spinal metastases. Oncologist 2004;9:188–96. [DOI] [PubMed] [Google Scholar]
- [7].Green JLBJ, Trump DL. Clinical features and natural history of intramedullary spinal cord metastasis. Cancer 1985;56:2305–14. [DOI] [PubMed] [Google Scholar]
- [8].Oh CH, Park NS, Kim JM, et al. Determination of an ideal stimulation site of the medial antebrachial cutaneous nerve using ultrasound and investigation of the efficiency. Ann Rehabil Med 2014;38:836–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Race CMSM. Anatomic course of the medial cutaneous nerves of the arm. J Hand Surg 1991;16A:48–52. [DOI] [PubMed] [Google Scholar]
- [10].Yildiz N, Ardic F. A rare cause of forearm pain: anterior branch of the medial antebrachial cutaneous nerve injury: a case report. J Brachial Plex Peripher Nerve Inj 2008;3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Radecki J, Feinberg JH, Zimmer ZR. T1 radiculopathy: electrodiagnostic evaluation. HSS J 2009;5:73–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


