Abstract
Background:
Acute alcohol consumption is known to be a risk factor for fall injuries.
Objective:
The study sought to determine whether usual alcohol consumption increases the risk for nonfatal fall injuries.
Method:
Data from 289,187 sample adults in the 2004–2013 U.S. National Health Interview Surveys were analyzed. Of these, 3,368 (~1 percent) reported a total of 3,579 fall-injury episodes requiring medical consultation in the past 3 months. Latent class analysis based on four contextual indicators identified four ecological subtypes of fall injury within two age groups (18–49 and 50+). Five drinking patterns (i.e., lifetime abstainer, former drinker, low-risk drinker, increased-risk drinker, and highest-risk drinker) were categorized according to the National Institute on Alcohol Abuse and Alcoholism (NIAAA) low-risk drinking guidelines. Controlling for potential confounders, negative binomial regression estimated the adjusted rates of any type and subtypes of fall injury, by gender, for each drinking pattern relative to lifetime abstainer.
Results:
Compared with lifetime abstainers, the adjusted rate of any fall injury for adults ages 18–49 was significantly higher among highest-risk drinkers (men: incidence rate ratio [IRR]=2.59, 95% confidence interval [CI] [1.60, 4.20]; women: IRR=1.90, 95% CI [1.24, 2.91]) and increased-risk drinkers (men: IRR=1.94, 95% CI [1.25, 3.00]; women: IRR=1.51, 95% CI [1.11, 2.07]). Furthermore, highest-risk drinkers had higher adjusted rates of either leisure- or sports-related fall injuries than lifetime abstainers.
Conclusions:
Alcohol consumption exceeding NIAAA’s low-risk drinking guidelines is associated with elevated rates of nonfatal fall injuries. Findings underscore the importance of adhering to these recommendations.
Keywords: Usual Alcohol Consumption, Fall Injury, National Health Interview Survey, Latent Class Analysis
INTRODUCTION
Fall injuries are an enormous burden to society. In the United States, 9.2 million emergency department (ED) visits, 1.1 million hospitalizations, and 33,018 deaths were attributed to fall injuries in 2014. Furthermore, in 2010 (the most recent data available), the combined costs incurred by fall injuries for medical care and work loss from ED visits, hospitalizations, and fatalities were as high as $50.9 billion, $95.5 billion, and $8.3 billion, respectively (Centers for Disease Control and Prevention [CDC], 2016a).
Fatal falls are a well-established geriatric problem. In 2014, 82 percent of the fall deaths occurred in the age group 65 and older and 93 percent occurred in age group 50 and older (CDC, 2016b). Nonfatal fall injuries, however, affect Americans of all ages. Notably, unintentional falls were the leading cause of nonfatal injuries for all age groups except those ages 10–24, for whom unintentional falls ranked as the second-highest cause of nonfatal injuries (CDC, 2016a).
There is a consensus in the literature that acute alcohol consumption is a contributing factor to fall injuries. Studies show that increased blood alcohol concentrations diminish motor coordination, impair judgment, and lengthen reaction time (Grant, Millar, & Kenny, 2000; Modig, Fransson, Magnusson, & Patel, 2012). In a meta-analysis of five studies, Taylor and colleagues (2010) concluded that unintentional-fall-injury risk increased linearly with acute alcohol consumption. Cherpitel, Ye, Bond, Borges, and Monteiro (2015) further confirmed the monotonic increase of fall injuries with acute alcohol consumption, using data obtained from 37 EDs in 18 countries. In contrast, studies examining the role of usual alcohol consumption in increasing the risk for fall injuries have yielded inconsistent findings (Chang & Do, 2015; Kool, Ameratunga, & Jackson, 2008; Mukamal et al., 2004; Stenbacka, Jansson, Leifman, & Romelsjo, 2002).
Most studies on fall injuries have focused on injuries that occurred at home, presumably because they accounted for more than half of fatal and nonfatal falls (Chen, Warner, Fingerhut, & Makuc, 2009; Smith & Kraus, 1988). In contrast, there is limited information on the role of usual alcohol consumption in other settings, such as sports, leisure, or occupation-related activities (Alliston, 2012; Ramchand, Pomeroy, & Arkes, 2009). However, in the interests of public health, it is imperative to better understand the relationship between alcohol use and all subtypes of fall injury.
In this study, we sought to identify ecological types of fall injury using latent class analysis (LCA) based on four contextual indicators (i.e., cause and mechanism of injury, location and activity at the time of injury) and to relate the frequency of these episodes to usual drinking patterns as opposed to acute alcohol consumption. Our aim was to quantify the relative risk of overall and subtypes of nonfatal fall injuries associated with usual drinking patterns for both men and women in the United States based on data from a large, nationally representative survey. Previous studies had indicated that the risk of fall injuries increases steeply with age (Schiller, Kramarow, & Dey, 2007), even though binge-drinking prevalence and intensity tend to decrease with age (CDC, 2012). These observations suggested that the risk for fall injuries associated with usual drinking patterns may differ between younger and older populations. Based on our preliminary data analysis, this study examined the risk profiles with respect to nonfatal fall injuries separately for two age groups: those ages 18–49 and those ages 50 and older. While this dichotomization was data-driven, it is meaningful from a public health perspective (World Health Organization, 2006). On the one hand, people ages 50 and older have reduced odds for alcohol consumption compared with their younger counterparts (Lotfipour et al., 2015). On the other hand, physical performance may decrease as early as age 50 (Hall et al., 2016), and older individuals are at increased risk for osteoporosis or low bone mass, which in turn increases the likelihood of falls and fractures (Office of the Surgeon General, 2004).
METHODS
Data Source
Data were drawn from the National Health Interview Survey (NHIS), an annual multipurpose health survey conducted by the National Center for Health Statistics that collects information on the health of the U.S. civilian noninstitutionalized household population via face-to-face interviews using computer-assisted personal interviewing. The NHIS uses a multistage, stratified-sample design of primary sampling units (e.g., counties, small groups of contiguous counties, or metropolitan statistical areas) covering the 50 States and the District of Columbia. Blacks, Hispanics, and Asians are oversampled to allow more precise estimation for these populations. The NHIS samples exclude patients in long-term care facilities, people on active duty with the U.S. Armed Forces, people incarcerated in the prison system, and U.S. nationals living in foreign countries. The NHIS has been collecting data on both injuries (including poisoning) and alcohol consumption annually since 1997. However, this study pooled data only from 2004 to 2013 because of revisions to the injury section of the questionnaire implemented in 2000 and 2004 and a change in the heavy episodic drinking (HED) question for women starting in 2014 (Chen, Warner, Fingerhut, & Makuc, 2009). Overall, the total household response rate was close to 90 percent and the final response rate for the adult sample was about 75 percent. Further details about the NHIS sample designs have been described elsewhere (Parsons et al., 2014).
The total study sample included 289,187 adults ages 18 and older. Among them, 8,696 (~3 percent) reported one or more injury episodes (totaling 9,333 injury episodes) that required medical consultation in the past 3 months, of which 3,368 (~1 percent) reported one or more fall-injury episodes (totaling 3,579 fall-injury episodes).
Nonfatal Fall-Injury Measures
The NHIS asked all members of the family the questions regarding medically consulted nonfatal injuries within a 3-month (91-day) reference period preceding the interview. A medically consulted injury episode is defined as a traumatic event that causes an acute condition or physical harm resulting in a visit to an emergency room, doctor’s office, or other health clinic or a phone call to a doctor or other health care professional. The open-ended responses were coded by the NHIS according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) external-cause-of-injury codes. Cases of nonfatal fall injuries were ascertained by the first-listed external cause of injury with the following ICD-9-CM codes: E880.0 to E886.9, E888, E957.0 to E957.9, E968.1, and E987.0 to E987.9. Only 2 of the 3,579 fall injury episodes in our sample were coded as intentional injuries based on these ICD codes; therefore, presumably the vast majority of these nonfatal injuries were unintentional.
Additional information on fall-injury episodes pertained to what caused the person to fall (cause), how the person fell (mechanism), where the person was when the fall injury occurred (location), and what the person was doing at the time of injury (activity). Detailed categories are shown in Tables 3 and 4.
Table 3.
Probability distribution for cause and mechanism of injury, place of occurrence, and activity at time of injury conditional on four classes of fall injury episodes, among adults ages 18–49, United States, National Health Interview Survey, 2004–2013
| Class 1 Residential |
Class 2 Occupational |
Class 3 Leisure |
Class 4 Sports |
|
|---|---|---|---|---|
| Class Size (n = 1,325) | 0.411 | 0.195 | 0.223 | 0.170 |
| Cause | ||||
| Slipping or tripping | 0.605 | 0.642 | 0.588 | 0.554 |
| Jumping or diving | 0.019 | 0.004 | 0.035 | 0.167 |
| Bumping into an object or another person | 0.018 | 0.016 | 0.018 | 0.040 |
| Being shoved or pushed by another person | 0.002 | 0.004 | 0.008 | 0.097 |
| Losing balance or having dizziness (fainting or a seizure) | 0.195 | 0.053 | 0.139 | 0.053 |
| Other | 0.162 | 0.281 | 0.212 | 0.090 |
| Mechanism | ||||
| Stairs, steps, or escalator | 0.390 | 0.095 | 0.139 | 0.018 |
| Floor or level ground | 0.308 | 0.308 | 0.243 | 0.032 |
| Curb (including sidewalk) | 0.002 | 0.025 | 0.276 | 0.002 |
| Ladder or scaffolding | 0.036 | 0.127 | 0.000 | 0.000 |
| Sports field, court, or rink | 0.000 | 0.003 | 0.000 | 0.594 |
| Building or other structure | 0.022 | 0.076 | 0.003 | 0.012 |
| Chair, bed, sofa, or other furniture | 0.048 | 0.013 | 0.028 | 0.018 |
| Bathtub, shower, toilet, or commode | 0.056 | 0.007 | 0.000 | 0.000 |
| Hole or other opening | 0.018 | 0.037 | 0.039 | 0.000 |
| Other | 0.120 | 0.309 | 0.272 | 0.324 |
| Place of occurrence | ||||
| Home (inside) | 0.638 | 0.000 | 0.001 | 0.023 |
| Home (outside) | 0.329 | 0.039 | 0.334 | 0.045 |
| School, child care center, or preschool | 0.000 | 0.059 | 0.022 | 0.031 |
| Hospital or residential institution | 0.005 | 0.135 | 0.000 | 0.000 |
| Street including highway, sidewalk, or parking lot | 0.000 | 0.087 | 0.346 | 0.004 |
| Recreation—sport facility, recreation area, lake, river, or pool | 0.000 | 0.016 | 0.068 | 0.852 |
| Commercial—trade or service area | 0.000 | 0.143 | 0.093 | 0.000 |
| Commercial area—industrial, construction area, or farm | 0.001 | 0.192 | 0.000 | 0.000 |
| Other public building | 0.006 | 0.155 | 0.029 | 0.000 |
| Other places, not specified | 0.022 | 0.173 | 0.108 | 0.045 |
| Activity at time of injury | ||||
| Driving or riding in a motor vehicle | 0.004 | 0.008 | 0.013 | 0.000 |
| Working at a paid job | 0.014 | 0.825 | 0.005 | 0.000 |
| Working around the house or yard | 0.392 | 0.000 | 0.035 | 0.000 |
| Attending school | 0.002 | 0.009 | 0.024 | 0.000 |
| Sports and exercise | 0.000 | 0.000 | 0.091 | 0.759 |
| Leisure activity (excluding sports) | 0.238 | 0.017 | 0.522 | 0.241 |
| Sleeping, resting, eating, or drinking | 0.051 | 0.009 | 0.000 | 0.000 |
| Cooking | 0.011 | 0.000 | 0.010 | 0.000 |
| Other | 0.287 | 0.132 | 0.301 | 0.000 |
Table 4.
Probability distribution for cause and mechanism of injury, place of occurrence, and activity at time of injury conditional on four classes of fall injury episodes, among adults ages 50 and older, United States, National Health Interview Survey, 2004–2013
| Class 1 Residential |
Class 2 Occupational |
Class 3 Leisure |
Class 4 Homebound Residential |
|
|---|---|---|---|---|
| Class Size (n = 2,254a) | 0.403 | 0.152 | 0.127 | 0.318 |
| Cause | ||||
| Slipping or tripping | 0.608 | 0.701 | 0.693 | 0.322 |
| Jumping or diving | 0.002 | 0.003 | 0.000 | 0.000 |
| Bumping into an object or another person | 0.023 | 0.035 | 0.024 | 0.010 |
| Being shoved or pushed by another person | 0.003 | 0.008 | 0.010 | 0.000 |
| Losing balance or having dizziness (fainting or a seizure) | 0.182 | 0.070 | 0.126 | 0.481 |
| Other | 0.182 | 0.184 | 0.147 | 0.188 |
| Mechanism | ||||
| Stairs, steps, or escalator | 0.306 | 0.121 | 0.073 | 0.000 |
| Floor or level ground | 0.364 | 0.486 | 0.207 | 0.599 |
| Curb (including sidewalk) | 0.033 | 0.042 | 0.348 | 0.000 |
| Ladder or scaffolding | 0.065 | 0.036 | 0.000 | 0.000 |
| Sports field, court, or rink | 0.000 | 0.000 | 0.080 | 0.000 |
| Building or other structure | 0.007 | 0.035 | 0.000 | 0.005 |
| Chair, bed, sofa, or other furniture | 0.000 | 0.015 | 0.005 | 0.144 |
| Bathtub, shower, toilet, or commode | 0.000 | 0.000 | 0.001 | 0.120 |
| Hole or other opening | 0.026 | 0.019 | 0.026 | 0.000 |
| Other | 0.198 | 0.245 | 0.260 | 0.132 |
| Place of occurrence | ||||
| Home (inside) | 0.407 | 0.024 | 0.000 | 0.943 |
| Home (outside) | 0.561 | 0.011 | 0.238 | 0.012 |
| School, child care center, or preschool | 0.000 | 0.038 | 0.011 | 0.000 |
| Hospital or residential institution | 0.002 | 0.135 | 0.030 | 0.031 |
| Street including highway, sidewalk, or parking lot | 0.010 | 0.092 | 0.394 | 0.000 |
| Recreation—sport facility, recreation area, lake, river, or pool | 0.000 | 0.000 | 0.283 | 0.000 |
| Commercial—trade or service area | 0.000 | 0.265 | 0.000 | 0.000 |
| Commercial area—industrial, construction area, or farm | 0.002 | 0.083 | 0.003 | 0.000 |
| Other public building | 0.000 | 0.112 | 0.012 | 0.002 |
| Other places, not specified | 0.017 | 0.241 | 0.028 | 0.012 |
| Activity at time of injury | ||||
| Driving or riding in a motor vehicle | 0.011 | 0.011 | 0.012 | 0.000 |
| Working at a paid job | 0.000 | 0.399 | 0.015 | 0.000 |
| Working around the house or yard | 0.514 | 0.000 | 0.005 | 0.130 |
| Attending school | 0.000 | 0.008 | 0.000 | 0.000 |
| Sports and exercise | 0.000 | 0.000 | 0.225 | 0.007 |
| Leisure activity (excluding sports) | 0.205 | 0.296 | 0.498 | 0.197 |
| Sleeping, resting, eating, or drinking | 0.003 | 0.005 | 0.000 | 0.189 |
| Cooking | 0.005 | 0.000 | 0.000 | 0.023 |
| Other | 0.261 | 0.282 | 0.245 | 0.454 |
Two fall-injury episodes could not be classified due to missing values on all indicators.
Usual Alcohol Consumption Measures
NHIS’s alcohol consumption questionnaire asked sample adults whether they had at least 12 drinks of any type of alcoholic beverage in their entire life or in any one year. The survey further asked about the usual frequency (number of drinking days) and quantity (average number of drinks on the drinking days) of any type of alcohol consumption as well as the frequency of HED (i.e., number of days on which they had 5 or more drinks of any alcoholic beverage) in the past year.
The drinking frequency, quantity, and HED measures as well as the derived drinking volume were used to determine whether a respondent exceeded the NIAAA’s low-risk drinking guidelines with weekly drinking limits of no more than 14 drinks for men and no more than 7 drinks for women, and single-day drinking limits of no more than 4 drinks for men and 3 drinks for women (NIAAA, 2010). Owing to the limitation of the NHIS data, commensurate daily drinking limits had to be modified as no more than 4 drinks on a single day for both men and women. Based on the guidelines, five drinking patterns were constructed: lifetime abstainer (less than 12 drinks in the lifetime), former drinker (12+ drinks in the lifetime but none in the past year), and three types of current drinker (12+ drinks in the lifetime and at least 1 drink in the past year). These included low-risk drinker (exceeding neither single-day nor weekly drinking limits), increased-risk drinker (exceeding either single-day or weekly drinking limits), and highest-risk drinker (exceeding both single-day and weekly drinking limits). Of the 289,187 sample adults included in the study, 6,399 (2.21 percent) could not be classified into any drinking pattern because of missing data.
Covariates
Selected covariates that potentially predisposed respondents to certain drinking behaviors were examined. These covariates included survey year, age, race/ethnicity (Hispanic, White, Black, others), education (less than high school, high school, some college, college and above), employment/occupation (never worked, no job in the past 12 months, white collar job, service job, blue collar/other job), marital status (married, never married, divorced/separated, widowed, living with partner), smoking status (current, former, never), body mass index, functional limitation (limited, not limited), use of special equipment (uses equipment, doesn’t use equipment), physical health status (excellent, very good, good, fair, poor), frequency of doing physical activities to strengthen muscles, frequency of doing light/moderate physical activities, frequency of doing vigorous physical activities, and frequency of going to a hospital emergency room about own health in the past year. Gender was treated as a moderator interacting with drinking patterns in the regression analysis, which was further stratified by age group (ages 18–49 and ages 50 and older). Of the 289,187 sample adults in our study, 21,482 (7.43 percent) had at least one covariate with a missing value.
Statistical analysis
We first conducted a preliminary analysis based on cubic regression splines (Royston & Sauerbrei, 2007) to empirically determine the age cutoff for the subsequent analyses of differential risk for nonfatal fall injuries associated with usual alcohol consumption in younger and older populations. The smoothed relationship between age and 3-month incidence rates of nonfatal fall injuries, by drinking pattern, is illustrated in Figure 1, which revealed a good age cutoff around age 50. Compared with lifetime abstainers, low-risk and increased-risk drinkers had higher incidence rates in the younger age group (18–49) but lower incidence rates in the older age group (50 and older), although highest-risk drinkers had higher incidence rates before age 59. Accordingly, subsequent analyses were conducted separately for these two age groups (ages 18–49 and 50 and older).
Figure 1.
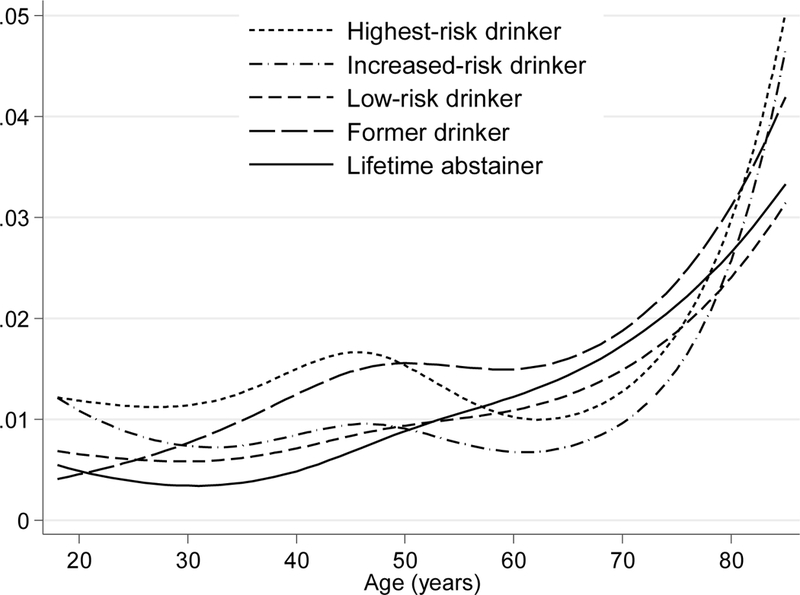
Three-month incidence rate of fall injuries, by drinking pattern, United States, National Health Interview Survey, 2004–2013 [Curves are based on cubic regression splines.]
We used the four injury measures mentioned previously (cause, mechanism, location, and activity) as indicators for LCA to identify subtypes of nonfatal fall injuries. The LCA was conducted in Mplus (Muthén & Muthén, 1998–2012), a statistical program specializing in latent variable modeling and taking into account complex designs and sampling weight for the analysis of survey data. LCA is a data-reduction technique that identifies a smaller number of latent classes from large combinations of responses to the indicators. This model-based clustering method produces posterior membership probabilities (i.e., probabilities of each case belonging to the classes). For practical purposes, the highest posterior probability was used to assign class membership to each injury episode. The number of latent classes was determined by Bayesian Information Criteria (BIC) in conjunction with entropy (a measure of classification certainty).
Once the number of classes had been determined and class membership had been assigned, we used negative binomial regression to model the relationship between the numbers of any type or specific types of nonfatal fall injuries in the past 3 months and drinking patterns by age group. The negative binomial regression, which allowed overdispersion for count data, was carried out with and without covariates in Stata (StataCorp, 2015), incorporating sampling weights and the NHIS’s complex survey design. Continuous covariates were included in the model in terms of cubic regression splines (Royston & Sauerbrei, 2007). Missing values (about 9 percent) in both drinking patterns and covariates were multiply imputed with five sets of plausible values using the random hot deck method (Andridge & Little, 2010). The imputed data sets were analyzed separately and then the results were combined; therefore, the standard errors combined variability within and between data sets to reflect estimation uncertainty due to missing values. For all statistical tests, two-tailed p-value < 0.05 was considered statistically significant.
RESULTS
The annualized rate of nonfatal fall injury episodes in 2004–2013 was 43 episodes per 1,000 population. The most common causes and mechanisms of these injuries were slipping or tripping (55 percent) and losing balance (20 percent) on the floor or level ground (36 percent) and from stairs, steps, or an escalator (17 percent). Furthermore, most injuries occurred at home (inside and outside) (63 percent), while working around the house or yard or at a paid job (32 percent) or while doing sports or leisure activities (33 percent). Those who sustained nonfatal fall injuries tended to be older (average age 54); were disproportionally female (63 percent), widowed or divorced (29 percent), or unemployed (45 percent); and had functional limitations (67 percent), fair/poor health (33 percent), or health problems that required special equipment (28 percent) [data not shown].
Percentage distributions of key demographics and other characteristics by drinking pattern are presented for respondents ages 18–49 and ages 50 and older in Tables 1 and 2, respectively. According to the chi-square and adjusted Wald F tests, significant differences existed across the drinking patterns with respect to all of these variables. Therefore, they were considered as confounders in the subsequent regression analyses. For both age groups, compared with lifetime abstainers, increased-risk drinkers and highest-risk drinkers were disproportionately male, non-Hispanic, White, college-educated, currently employed, and blue-collar workers; they tended to be current smokers and to engage more frequently in light/moderate and vigorous physical activities or muscle-strengthening activities. Moreover, they were less likely to have health problems that required special equipment. In the age group 50 and older, increased-risk drinkers and highest-risk drinkers additionally tended to be younger, currently married, not widowed, and healthier compared with lifetime abstainers and were less likely to have functional limitations or visit the emergency room because of health problems. This pattern was not observed in the younger age group (ages 18–49) and may even appear opposite.
Table 1.
Percentage distributions of key demographics and other characteristics, by drinking pattern, among adults ages 18–49, United States, National Health Interview Survey, 2004–2013
| Lifetime Abstainers (n = 34,768) |
Former Drinkers (n = 15,360) |
Low-Risk Drinkers (n = 60,612) |
Increased-Risk Drinkers (n = 37,365) |
Highest-Risk Drinkers (n = 8,591) |
|
|---|---|---|---|---|---|
| Age | 31.1 (0.1) | 37.0 (0.1) | 35.3 (0.1) | 32.3 (0.1) | 33.2 (0.2) |
| Male gender (%) | 39.3 (0.4) | 45.7 (0.5) | 43.8 (0.3) | 66.3 (0.3) | 60.4 (0.7) |
| Hispanic ethnicity (%) | 25.6 (0.5) | 17.6 (0.4) | 15.1 (0.2) | 15.5 (0.3) | 10.3 (0.4) |
| Race (%) | |||||
| White | 68.3 (0.5) | 80.4 (0.5) | 79.4 (0.3) | 88.0 (0.3) | 87.3 (0.5) |
| Black | 19.9 (0.4) | 13.9 (0.4) | 14.1 (0.3) | 7.7 (0.2) | 8.8 (0.4) |
| Other | 11.8 (0.3) | 5.7 (0.3) | 6.5 (0.1) | 4.3 (0.2) | 3.9 (0.3) |
| Education (%) | |||||
| Less than high school | 22.7 (0.4) | 18.3 (0.5) | 9.8 (0.2) | 11.2 (0.3) | 11.7 (0.5) |
| High school | 29.0 (0.4) | 30.6 (0.5) | 23.4 (0.3) | 24.9 (0.3) | 28.0 (0.7) |
| Some college | 28.7 (0.4) | 31.3 (0.5) | 33.0 (0.3) | 34.3 (0.4) | 34.7 (0.8) |
| College and above | 18.5 (0.4) | 19.3 (0.5) | 33.3 (0.3) | 29.2 (0.4) | 25.3 (0.6) |
| Employment/Occupation (%) | |||||
| Never worked | 18.4 (0.3) | 4.7 (0.2) | 2.9 (0.1) | 1.9 (0.1) | 1.7 (0.2) |
| No job in past 12 months | 12.7 (0.3) | 19.3 (0.4) | 10.8 (0.2) | 7.2 (0.2) | 8.8 (0.4) |
| White-collar job | 19.5 (0.3) | 24.3 (0.5) | 35.4 (0.3) | 31.4 (0.4) | 26.9 (0.6) |
| Service job | 31.6 (0.3) | 29.4 (0.4) | 32.6 (0.3) | 34.0 (0.3) | 34.9 (0.7) |
| Blue-collar/other job | 17.4 (0.3) | 22.2 (0.5) | 18.3 (0.2) | 25.4 (0.4) | 27.7 (0.6) |
| Marital status (%) | |||||
| Married | 45.1 (0.4) | 59.3 (0.5) | 56.3 (0.3) | 43.7 (0.4) | 35.1 (0.8) |
| Widowed | 0.5 (0.0) | 0.6 (0.1) | 0.5 (0.0) | 0.3 (0.0) | 0.3 (0.1) |
| Divorced | 4.2 (0.1) | 8.6 (0.2) | 7.1 (0.1) | 6.5 (0.1) | 8.6 (0.4) |
| Separated | 2.1 (0.1) | 2.8 (0.1) | 2.3 (0.1) | 1.9 (0.1) | 2.6 (0.2) |
| Never married | 42.8 (0.4) | 19.7 (0.4) | 24.9 (0.3) | 34.9 (0.4) | 38.6 (0.8) |
| Living with partner | 5.0 (0.1) | 8.8 (0.3) | 8.9 (0.2) | 12.5 (0.2) | 14.8 (0.5) |
| Functional limitation (%) | 17.2 (0.3) | 31.8 (0.5) | 20.3 (0.2) | 20.4 (0.3) | 23.0 (0.6) |
| Health problem that requires special equipment (%) | 2.3 (0.1) | 4.8 (0.2) | 2.0 (0.1) | 1.6 (0.1) | 1.5 (0.2) |
| Self-reported health status (%) | |||||
| Excellent | 37.0 (0.4) | 26.4 (0.5) | 36.5 (0.3) | 37.5 (0.3) | 33.5 (0.6) |
| Very good | 30.9 (0.3) | 30.6 (0.5) | 34.8 (0.3) | 35.5 (0.3) | 34.9 (0.6) |
| Good | 23.7 (0.3) | 27.4 (0.4) | 22.2 (0.2) | 21.9 (0.3) | 24.6 (0.6) |
| Fair | 6.5 (0.2) | 11.5 (0.3) | 5.4 (0.1) | 4.3 (0.1) | 5.7 (0.3) |
| Poor | 1.8 (0.1) | 4.0 (0.2) | 1.1 (0.0) | 0.8 (0.1) | 1.3 (0.1) |
| Smoking status (%) | |||||
| Current every-day smoker | 6.6 (0.2) | 22.3 (0.5) | 16.0 (0.2) | 22.7 (0.3) | 37.2 (0.7) |
| Current some-day smoker | 1.7 (0.1) | 3.5 (0.2) | 4.6 (0.1) | 8.6 (0.2) | 11.7 (0.4) |
| Former smoker | 2.9 (0.1) | 20.9 (0.4) | 14.7 (0.2) | 17.8 (0.3) | 17.4 (0.5) |
| Never smoker | 88.6 (0.3) | 53.2 (0.5) | 64.6 (0.2) | 50.8 (0.3) | 33.7 (0.8) |
| Body mass index (kg/m2) | 26.8 (0.0) | 28.6 (0.1) | 27.1 (0.0) | 27.2 (0.0) | 26.5 (0.1) |
| Frequency of doing physical activities to strengthen muscles (times per week) |
0.81 (0.02) | 0.84 (0.03) | 1.16 (0.01) | 1.52 (0.02) | 1.37 (0.04) |
| Frequency of doing light/moderate physical activities (times per week) |
2.08 (0.03) | 2.43 (0.04) | 2.73 (0.02) | 3.02 (0.03) | 3.07 (0.06) |
| Frequency of doing vigorous physical activities (times per week) |
1.51 (0.03) | 1.49 (0.03) | 1.99 (0.02) | 2.41 (0.02) | 2.30 (0.05) |
| # times in hospital emergency room, past 12 month | 0.29 (0.01) | 0.47 (0.01) | 0.30 (0.00) | 0.31 (0.01) | 0.38 (0.01) |
Standard errors are in parentheses.
Numbers may not add to full sample due to missing data.
Differences among drinking patterns are significant for all covariates at the 0.01 level based on adjusted Wald F tests.
Table 2.
Percentage distributions of key demographics and other characteristics, by drinking pattern, among adults ages 50 and older, United States, National Health Interview Survey, 2004–2013
| Lifetime Abstainers (n = 31,142) |
Former Drinkers (n = 28,546) |
Low-Risk Drinkers (n = 51,504) |
Increased-Risk Drinkers (n = 10,515) |
Highest-Risk Drinkers (n = 4,385) |
|
|---|---|---|---|---|---|
| Age | 66.5 (0.1) | 65.6 (0.1) | 62.7 (0.1) | 58.8 (0.1) | 59.5 (0.1) |
| Male gender (%) | 27.4 (0.3) | 50.2 (0.4) | 47.5 (0.3) | 67.4 (0.6) | 70.2 (0.9) |
| Hispanic ethnicity (%) | 12.5 (0.3) | 7.9 (0.2) | 6.6 (0.2) | 9.3 (0.4) | 5.5 (0.4) |
| Race (%) | |||||
| White | 76.6 (0.4) | 83.7 (0.3) | 88.7 (0.2) | 89.6 (0.4) | 90.2 (0.5) |
| Black | 14.1 (0.4) | 12.5 (0.3) | 7.7 (0.2) | 7.6 (0.3) | 7.5 (0.5) |
| Other | 9.2 (0.3) | 3.8 (0.2) | 3.5 (0.1) | 2.8 (0.2) | 2.4 (0.3) |
| Education (%) | |||||
| Less than high school | 26.5 (0.4) | 23.9 (0.3) | 9.5 (0.2) | 12.0 (0.4) | 13.5 (0.6) |
| High school | 32.8 (0.3) | 33.8 (0.4) | 26.5 (0.3) | 27.9 (0.5) | 28.6 (0.8) |
| Some college | 21.1 (0.3) | 25.0 (0.3) | 28.5 (0.2) | 29.4 (0.6) | 29.8 (0.9) |
| College and above | 18.0 (0.3) | 16.6 (0.3) | 35.1 (0.4) | 30.4 (0.7) | 27.8 (0.9) |
| Employment/Occupation (%) | |||||
| Never worked | 13.5 (0.3) | 4.2 (0.2) | 2.3 (0.1) | 1.3 (0.1) | 1.3 (0.2) |
| No job past 12 months | 49.5 (0.4) | 57.0 (0.4) | 39.3 (0.3) | 28.4 (0.6) | 35.6 (0.9) |
| White-collar job | 12.7 (0.3) | 12.6 (0.3) | 27.1 (0.3) | 26.8 (0.6) | 22.0 (0.8) |
| Service job | 15.2 (0.3) | 14.6 (0.3) | 20.0 (0.2) | 21.5 (0.5) | 19.6 (0.8) |
| Blue-collar/other job | 8.6 (0.2) | 11.4 (0.2) | 11.2 (0.2) | 22.0 (0.5) | 21.5 (0.8) |
| Marital status (%) | |||||
| Married | 57.0 (0.4) | 57.7 (0.4) | 66.6 (0.3) | 65.8 (0.6) | 62.1 (0.9) |
| Widowed | 22.9 (0.3) | 17.0 (0.3) | 10.5 (0.2) | 6.2 (0.2) | 6.1 (0.4) |
| Divorced | 9.6 (0.2) | 14.0 (0.2) | 12.6 (0.2) | 15.0 (0.4) | 16.5 (0.6) |
| Separated | 2.0 (0.1) | 2.1 (0.1) | 1.6 (0.1) | 2.1 (0.1) | 2.2 (0.2) |
| Never married | 6.6 (0.2) | 6.1 (0.2) | 5.4 (0.1) | 6.0 (0.2) | 5.8 (0.4) |
| Living with partner | 1.6 (0.1) | 2.9 (0.1) | 3.1 (0.1) | 4.9 (0.3) | 7.1 (0.5) |
| Functional limitation (%) | 55.1 (0.4) | 64.1 (0.4) | 46.9 (0.3) | 42.2 (0.6) | 46.0 (1.0) |
| Health problem that requires special equipment (%) | 16.9 (0.3) | 20.3 (0.3) | 8.7 (0.2) | 5.9 (0.3) | 7.5 (0.5) |
| Self-reported health status (%) | |||||
| Excellent | 14.7 (0.3) | 11.1 (0.2) | 23.4 (0.3) | 24.4 (0.5) | 22.4 (0.9) |
| Very good | 24.6 (0.3) | 23.2 (0.3) | 34.4 (0.3) | 34.1 (0.6) | 31.3 (0.9) |
| Good | 33.2 (0.3) | 33.6 (0.3) | 29.0 (0.2) | 28.8 (0.5) | 30.7 (0.9) |
| Fair | 19.3 (0.3) | 22.0 (0.3) | 10.3 (0.2) | 10.2 (0.4) | 11.7 (0.6) |
| Poor | 8.1 (0.2) | 10.1 (0.2) | 2.9 (0.1) | 2.5 (0.2) | 3.9 (0.4) |
| Smoking status (%) | |||||
| Current every-day smoker | 6.6 (0.2) | 15.6 (0.3) | 11.5 (0.2) | 21.1 (0.5) | 33.1 (0.9) |
| Current some-day smoker | 1.3 (0.1) | 2.2 (0.1) | 2.7 (0.1) | 5.2 (0.2) | 4.5 (0.4) |
| Former smoker | 14.4 (0.3) | 42.4 (0.4) | 36.7 (0.3) | 39.4 (0.6) | 38.5 (0.9) |
| Never smoker | 77.5 (0.3) | 39.6 (0.4) | 48.9 (0.3) | 34.3 (0.6) | 23.8 (0.8) |
| Body mass index (kg/m2) | 27.8 (0.1) | 28.5 (0.1) | 27.7 (0.0) | 28.0 (0.1) | 26.9 (0.1) |
| Frequency of doing physical activities to strengthen muscles (times per week) | 0.47 (0.01) | 0.63 (0.02) | 1.02 (0.02) | 1.07 (0.03) | 1.10 (0.06) |
| Frequency of doing light/moderate physical activities (times per week) | 1.84 (0.03) | 2.19 (0.03) | 2.87 (0.04) | 2.95 (0.05) | 3.03 (0.10) |
| Frequency of doing vigorous physical activities (times per week) | 0.76 (0.02) | 0.90 (0.02) | 1.49 (0.02) | 1.73 (0.04) | 1.65 (0.06) |
| # times in hospital emergency room, past 12 month | 0.36 (0.01) | 0.44 (0.01) | 0.25 (0.00) | 0.24 (0.01) | 0.25 (0.01) |
Standard errors are in parentheses.
Numbers may not add to full sample due to missing data.
Differences among drinking patterns are significant for all covariates at the 0.01 level based on adjusted Wald F tests.
Using BIC, we identified four subtypes of nonfatal fall injury for both age groups with good classification quality (entropy = 0.852 for ages 18–49 and 0.774 ages 50 and older). For both age groups, Classes 1 to 3 were categorized as residential, occupational, and leisure injuries, respectively. However, Class 4 differed for the two age groups and was categorized as sports injuries for the age group 18–49 and as homebound residential injuries for the age group 50 and older. Tables 3 and 4 present the response profiles of the four injury classes for ages 18–49 and 50 and older, respectively. Class 1 (residential) was the largest subtype of nonfatal fall injuries in both age groups, accounting for approximately 40 percent of injuries. These injuries occurred mainly inside or outside the home (approximately 95 percent) while working around the house or yard or engaging in nonsports-related leisure or other activities (more than 90 percent). Class 2 (occupational) injuries occurred primarily while working at a paid job, particularly in the age group 18–49 (82.5 percent), but to a lesser extent in the age group 50 and older (39.9 percent). Class 3 (leisure) injuries most commonly occurred while engaging in nonsports-related leisure activities (approximately 50 percent); in the age group 50 and older, sports and exercise (22.5 percent) also were common activities at the time of injury. In the age group 18–49, Class 4 (sports) injuries mainly occurred in a sports facility, recreation area, lake, river, or pool (85.2 percent) from an incident on a sports field, court, or rink (59.4 percent) while engaging in sports and exercise (75.9 percent) or a leisure activity (24.1 percent). By contrast, in the age group 50 and older, Class 4 (homebound residential) was the second most-common subtype of nonfatal fall injury and occurred predominantly inside the home (94.3 percent) and when working around the house or yard (13 percent); sleeping, resting, eating, or drinking (18.9 percent); or engaging in nonsports-related leisure (19.7 percent) or other activities (45.4 percent). This type of fall injuries was mainly caused by slipping or tripping (32.2 percent) and losing balance or feeling dizzy (48.1 percent) on the floor or level ground (59.9 percent) or from chair, bed, sofa, or other furniture (14.4 percent) or bathtub, shower, toilet, or commode (12 percent).
Tables 5 and 6 present adjusted and unadjusted incidence rate ratios (IRRs) relative to lifetime abstainers for having any or subtypes of nonfatal fall injury episodes, by usual drinking pattern and gender, for people ages 18–49 and ages 50 and older, respectively. The unadjusted IRRs only provide crude measures of the association between usual drinking patterns and nonfatal fall injuries. The magnitude of the associations generally decreased for adults ages 18–49 and increased for adults ages 50 and older after regression adjustments for confounders and did not reach statistical significance for most cases. For adults ages 18–49 (Table 5), the adjusted IRRs for having any nonfatal fall injuries among highest-risk drinkers were 2.59 (95% CI [1.60, 4.20]) in men and 1.90 (95% CI [1.24, 2.91]) in women. For subtypes of nonfatal fall injury, the IRRs remained significantly higher for Class 3 (leisure) fall injuries in women (IRR = 2.26, 95% CI [1.11, 4.58]) and for Class 4 (sports) fall injuries in men (IRR = 3.16, 95% CI [1.43, 6.97]). Similarly, increased-risk drinkers in this age group had significantly higher adjusted rates for any nonfatal fall injuries (IRR = 1.94, 95% CI [1.25, 3.00] in men and 1.51, 95% CI [1.11, 2.07] in women). Among the adults ages 50 and older, in contrast, neither the increased-risk drinkers nor the highest-risk drinkers differed significantly from the lifetime abstainers in their adjusted rates of any nonfatal fall injuries (Table 6). However, male highest-risk drinkers had a higher rate (IRR = 5.39, 95% CI [1.31, 22.1]) of Class 3 (leisure) fall injuries.
Table 5.
Adjusteda and unadjusted incidence rate ratios for having any type or subtypes of fall injury episodes, by drinking pattern, compared with lifetime abstainers, among adults ages 18–49, United States, National Health Interview Survey, 2004–2013
| Any fall injury | Class 1 Residential |
Class 2 Occupational |
Class 3 Leisure |
Class 4 Sports |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Male (n = 72,782) | ||||||||||
| Lifetime abstainer | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Former drinker | 2.72** (0.70) | 1.75* (0.45) | 4.51** (1.94) | 2.11 (0.94) | 2.78 (1.51) | 1.80 (0.99) | 1.78 (1.09) | 1.16 (0.69) | 0.98 (0.58) | 1.21 (0.68) |
| Low-risk drinker | 1.87** (0.43) | 1.66* (0.38) | 2.48* (0.93) | 2.07 (0.82) | 2.14 (0.99) | 1.74 (0.84) | 1.18 (0.67) | 1.05 (0.57) | 1.07 (0.40) | 1.12 (0.41) |
| Increased-risk drinker | 2.32** (0.51) | 1.94** (0.43) | 2.24* (0.80) | 1.92 (0.72) | 2.14 (0.94) | 1.50 (0.68) | 1.77 (0.89) | 1.51 (0.72) | 2.13* (0.73) | 1.87 (0.65) |
| Highest-risk drinker | 3.64** (0.91) | 2.59** (0.64) | 3.04* (1.52) | 2.10 (1.07) | 2.66 (1.46) | 1.54 (0.79) | 3.80* (2.15) | 2.84 (1.61) | 3.35** (1.35) | 3.16** (1.27) |
| Female (n = 87,404) | ||||||||||
| Lifetime abstainer | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Former drinker | 2.11** (0.40) | 1.30 (0.26) | 2.07** (0.48) | 1.04 (0.24) | 1.99 (0.87) | 1.36 (0.62) | 2.12* (0.67) | 1.21 (0.40) | 1.20 (0.99) | 1.20 (1.00) |
| Low-risk drinker | 1.28 (0.18) | 1.10 (0.16) | 1.38 (0.28) | 1.21 (0.23) | 1.62 (0.71) | 1.30 (0.60) | 1.12 (0.30) | 0.93 (0.26) | 0.73 (0.30) | 0.63 (0.26) |
| Increased-risk drinker | 1.92** (0.30) | 1.51** (0.24) | 1.54 (0.34) | 1.29 (0.29) | 1.72 (0.96) | 1.22 (0.71) | 2.22** (0.64) | 1.68 (0.51) | 2.36* (0.96) | 1.64 (0.67) |
| Highest-risk drinker | 2.73** (0.59) | 1.90** (0.41) | 2.45* (0.86) | 1.60 (0.48) | 2.15 (1.05) | 1.43 (0.71) | 3.26** (1.11) | 2.26* (0.81) | 1.63 (0.84) | 1.12 (0.57) |
Standard errors are in parentheses.
p < .05
p < .01
Adjusted for survey year, age, Hispanic ethnicity, race, education, employment/occupation, marital status, functional limitation, health problem that requires special equipment, self-reported health status, smoking status, body mass index, frequency of doing physical activities to strengthen muscles, frequency of doing light/moderate physical activities, frequency of doing vigorous physical activities, frequency of going to a hospital emergency room about own health in the past year.
Table 6.
Adjusteda and unadjusted incidence rate ratios for having any type or subtypes of fall injury episodes, by drinking pattern, compared with lifetime abstainers, among adults ages 50 and older, United States, National Health Interview Survey, 2004–2013
| Any fall injury | Class 1 Residential |
Class 2 Occupational |
Class 3 Leisure |
Class 4 Homebound Residential |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Male (n = 55,258) | ||||||||||
| Lifetime abstainer | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Former drinker | 1.48* (0.26) | 1.23 (0.23) | 1.93* (0.55) | 1.54 (0.45) | 0.77 (0.29) | 0.66 (0.25) | 1.80 (1.15) | 1.85 (1.20) | 1.43 (0.40) | 1.00 (0.29) |
| Low-risk drinker | 1.04 (0.18) | 1.24 (0.22) | 1.54 (0.44) | 1.79* (0.53) | 0.77 (0.27) | 0.75 (0.26) | 2.96 (1.79) | 3.22 (1.99) | 0.56* (0.15) | 0.79 (0.23) |
| Increased-risk drinker | 0.73 (0.18) | 1.04 (0.25) | 1.33 (0.48) | 1.78 (0.65) | 0.61 (0.27) | 0.59 (0.28) | 2.24 (1.52) | 3.07 (2.19) | 0.29** (0.13) | 0.64 (0.30) |
| Highest-risk drinker | 1.12 (0.29) | 1.42 (0.37) | 1.23 (0.57) | 1.45 (0.67) | 1.00 (0.53) | 0.94 (0.50) | 3.88 (2.74) | 5.39* (3.86) | 0.69 (0.30) | 1.00 (0.44) |
| Female (n = 73,743) | ||||||||||
| Lifetime abstainer | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Former drinker | 1.25* (0.12) | 1.14 (0.12) | 1.39* (0.20) | 1.17 (0.17) | 1.34 (0.41) | 1.18 (0.35) | 1.60 (0.40) | 1.66 (0.44) | 1.06 (0.16) | 0.95 (0.14) |
| Low-risk drinker | 0.79* (0.07) | 1.09 (0.11) | 0.95 (0.13) | 1.21 (0.18) | 1.18 (0.27) | 1.24 (0.28) | 1.36 (0.33) | 1.55 (0.42) | 0.49** (0.08) | 0.93 (0.15) |
| Increased-risk drinker | 0.65** (0.11) | 1.05 (0.19) | 0.77 (0.20) | 1.11 (0.30) | 0.93 (0.52) | 1.06 (0.60) | 0.98 (0.42) | 1.30 (0.59) | 0.46* (0.14) | 1.20 (0.37) |
| Highest-risk drinker | 0.77 (0.19) | 1.22 (0.34) | 0.86 (0.32) | 1.20 (0.46) | 1.92 (0.90) | 2.22 (1.06) | 1.80 (1.00) | 2.54 (1.48) | 0.14** (0.09) | 0.34 (0.22) |
Standard errors are in parentheses.
p < .05
p < .01
Adjusted for survey year, age, Hispanic ethnicity, race, education, employment/occupation, marital status, functional limitation, health problem that requires special equipment, self-reported health status, smoking status, body mass index, frequency of doing physical activities to strengthen muscles, frequency of doing light/moderate physical activities, frequency of doing vigorous physical activities, frequency of going to a hospital emergency room about own health in the past year.
DISCUSSION
Complementing the extant literature on acute alcohol consumption and fall injuries, the current study used population-based data to establish usual alcohol consumption as a risk factor for overall and some subtypes of nonfatal fall injuries among U.S. adults ages 18–49. Based on a large multi-year national survey, our findings suggest that irrespective of gender, people in this age group who exceed NIAAA-recommended daily and/or weekly drinking limits (i.e., increased-risk drinkers and highest-risk drinkers) are more susceptible to nonfatal fall injuries than lifetime abstainers. Conversely, no such association could be detected for adults ages 50 and older. Across subtypes of fall injuries, the associations with usual drinking patterns vary by age and gender. Although large and positive associations were identified, they generally were not statistically significant because of the limited number of cases in each subtype. For instance, for occupational fall injuries, none of the positive associations with usual drinking patterns were found to be significant. Significant risk increases were identified only among younger female and older male highest-risk drinkers for leisure-related fall injuries, among younger male highest-risk drinkers for sports-related fall injuries, and among older male low-risk drinkers for residential fall injuries.
The lack of significant associations between fall injuries and usual alcohol use in older adults is rather counter-intuitive, but is consistent with earlier studies that only found nonsignificant associations with alcohol use (Grundstrom, Guse, & Layde, 2012; Mukamal et al., 2004). While not focusing specifically on fall injuries, a Canadian study similarly detected no significant relationship between alcohol consumption patterns and car, work, sports, and home accidents in the older age groups, and only noted such a relationship in the age group of 15–34 (Wells & Macdonald, 1999). These findings may be explained by the fact that falls occur through the interplay of demographic, behavioral, biological/medical, and environmental risk factors (World Health Organization, 2007). The aging process itself with its associated frailty, medical conditions, and use of multiple medications to treat these conditions is a major risk for falls and fall injuries (Helgadóttir, Laflamme, Monarrez-Espino, & Moller, 2014; Milos et al., 2014; Rubenstein, 2006). Thus, in a recent Swedish study of people ages 65 and older from the Stockholm public health cohort (Helgadóttir, Moller, & Laflamme, 2015), those who were very old and did not report HED or smoking and those who were very old and were sedentary and less physically active had a higher risk for fall injuries than younger individuals with a tendency towards HED and smoking. In our study, older adults also had more health problems related to aging (e.g., functional limitations, health problems requiring special equipment, poorer subjective health status, or less physical activity) compared with younger adults. Thus, even without alcohol use, older adults are subject to a myriad of risk factors for fall injuries. At the same time, older adults are less likely than younger adults to be current drinkers and to exceed drinking limits. The effects from their alcohol use therefore may be overwhelmed or dwarfed by other more important risk factors that were not controlled for.
The discrepancy between younger and older adults in the association between exceeding low-risk drinking and nonfatal fall injuries can partly be attributed to selection bias, which often occurs in cross-sectional survey data. Older adults who consume alcohol, especially in large amounts, have distinctive characteristics. In our study, current drinkers tended to be healthier and have less functional limitations than lifetime abstainers, making them less likely to fall. These healthier older adults may have self-selected into drinking. The phenomenon of “healthy drinkers” may explain why the unadjusted IRRs spuriously indicate that exceeding the low-risk drinking guidelines may reduce the risk of any fall injuries.
The variation we observed in this study in the associations between usual alcohol consumption and subtypes of nonfatal fall injuries may be attributable to insufficient statistical power, which may render the deleterious effects of alcohol nonsignificant. Even with the pooled multi-year NHIS data, the combined sample size is not large enough to detect significant effects for all subtypes of fall injuries, especially among the older population, in whom excessive drinking is rare. It is also possible that alcohol’s deleterious effects became nonsignificant in our study because of overadjustment (i.e., control for an intermediate variable on a causal path from alcohol exposure to fall injury outcome in regression). For example, no significant effect of usual alcohol consumption on residential fall injuries was found in younger adults after statistical adjustment, although the unadjusted data showed a deleterious alcohol effect in line with that observed after acute alcohol consumption among working-age adults in two New Zealand studies (Kool, Ameratunga, Robinson, Crengle, & Jackson, 2008; Thornley, Kool, Marshall, & Ameratunga, 2014).
In other cases, the lack of a significant association between usual alcohol consumption and specific subtypes of nonfatal fall injuries may be genuine. For example, the nonsignificant finding on occupational fall injuries is consistent with previous studies (Stallones & Kraus, 1993; Webb et al., 1994). Although the report by Frone (2006) that about 8 percent of U.S. workers drink or get impaired before work or during the work day heightens the concern for alcohol-hangover effects on job performance, reports of hangover effects on fall injuries in the work environment are scarce, as alcohol often is prohibited at workplaces requiring vigorous or demanding manual activities or subject to work hazards (e.g., construction, fishery, repair services, and other low-skilled service jobs) (Macdonald et al., 2006).
Our findings that highest-risk drinkers may be significantly more likely than lifetime abstainers to sustain leisure-related and/or sport-related fall injuries also are plausible, given that many athletes are prone to HED (Martens, Dams-O’Connor, & Beck, 2006; O’Brien, & Lyons, 2000). HED increases injury risk because alcohol can impair a variety of psychomotor skills, such as reaction time, hand-eye coordination, accuracy, balance, and complex coordination (American College of Sports Medicine, 1982). Leisure-time physical activities, health status, and alcohol consumption collectively embody a lifestyle (Smothers & Bertolucci, 2001) susceptible to fall injuries. Although drinkers are healthier and more frequently engaged in muscle strengthening exercises (see Table 1), these supposedly protective characteristics may well be offset by the deleterious effect of excessive drinking on psychomotor performance.
As with any cross-sectional studies, our analysis has limitations in drawing causal inferences from the observed associations between usual alcohol consumption and fall injuries. To avoid recall bias (Warner, Schenker, Heinen, & Fingerhut, 2005), the NHIS limited the reference period for reporting injury episodes to the past 3 months, compared with the past 12 months for alcohol consumption, alleviating some concerns over the temporal sequence of drinking and injuries. However, as a result, fewer injury incidents are available for analysis, making the findings less powerful. Another limitation is the lack of information on acute alcohol consumption in the NHIS, precluding the removal of the partial effect of usual alcohol consumption confounded by acute alcohol consumption. However, post-hoc examinations of the verbatim responses on how the injury happened revealed few mentions of alcohol consumption at or before the injury; therefore, the confounding is likely to be minor, unless acute alcohol consumption was grossly underreported.
Despite our best efforts to control for confounding factors, residual confounding remains. The intrinsic and extrinsic risk factors for fall injuries are diverse, including demographic characteristics, illness, medication use, balance measurement, footwear, nutrition, cognitive function, social support, environment, and fear of falling (Huang, Lin, & Lin, 2008). These potential confounders vary for different subtypes of fall injuries. Work hazards, sleep problems, and fatigue may be more relevant to occupational fall injuries, whereas personality traits such as risk taking, impulsivity, or sensation seeking would be more relevant to sports- or leisure-related fall injuries (Cherpitel, Meyers, & Perrine, 1998; O’Brien & Lyons, 2000). Whether the relationship between drinking and risk of injuries may reflect risk-taking behavior or the underlying liability of externalizing behaviors warrants future studies. Further, alcohol users tend to co-use drugs and other substances such as tobacco or psychotropic drugs, which may have similar effects as alcohol (Gauchard et al., 2003) or have synergistic effects with alcohol on fall injury risk (Kurzthaler et al., 2005). The lack of personality-trait and drug-use information in the NHIS precludes our study from examining these effects. Classification error resulting from the modal assignment of injury episodes into subtypes of injuries also may introduce bias into the results.
Finally, our approach to dichotomizing age into a younger and an older age group at age 50 may have affected the results. The age cutoff was driven by data, but was consistent with the cutoff used in other studies (Clausen et al., 2015; Stewart Williams et al., 2015). Different age cutoffs may result in different categorizations of subtypes of fall injuries and alter the observed association with alcohol consumption. A sensitivity analysis using an age cutoff of 65 (the traditional retirement age in the United States) consistently confirmed the deleterious effect of exceeding low-risk drinking on any fall injury and on leisure- or sports-related injuries in the younger age group of 18–64 (supplementary tables). Insufficient sample size prohibited an analysis of the five drinking patterns in the older age group 65 and older. When comparing current drinkers and former drinkers with lifetime abstainers, no associations with fall injuries were observed except for a significantly higher adjusted rate of any fall injury for male current drinkers (supplementary tables). Future studies are needed to validate the age cutoff in association with alcohol consumption and nonfatal fall injury based on more stringent clinical criteria.
In conclusion, our findings complement other national studies of fall injuries based on the CDC’s Behavioral Risk Factor Surveillance System (BRFSS) (Grundstrom, Guse, & Layde, 2012; Stevens, Mack, Paulozzi, & Ballesteros, 2008). The use of LCA and multi-year NHIS data enables our study to identify subtypes of fall injuries and establish the adverse consequences of risky drinking on younger adults, particularly for leisure or sports-related fall injuries. Because usual alcohol consumption is more useful than acute alcohol consumption for identifying associations between general consumption habits and injury risk (Nordqvist, Holmqvist, Nilsen, Bendtsen, & Lindqvist, 2006), the findings have important implications for prevention and intervention. However, further research is needed to elucidate the pathways by which usual alcohol consumption relates to fall injuries and to reconcile the dose-response relationship with the threshold effect for the level of usual alcohol consumption. Unlike acute alcohol consumption at the time of injury, measures of usual alcohol consumption may not be directly linked to fall injuries. Nonetheless, it is reasonable to assume that high-risk drinkers are more likely to be intoxicated and, therefore, have greater risks for injuries (Cherpitel, 1992). Alternatively, the harmful and cumulative effects of usual alcohol consumption may contribute to peripheral neuropathy resulting in disturbed gait and balance, as well as to skeletal muscle myopathy and poor bone health (de la Monte, & Kril, 2014; Fein, & Greenstein, 2013; López-Larramona, Lucendo, & González-Delgado, 2013).
By quantifying the risks for nonfatal fall injuries associated with exceeding NIAAA-recommended low-risk drinking guidelines relative to lifetime abstinence, our findings underscore the importance of adhering to these recommendations. The suggestion that even healthy young adults can increase the risk of sustaining fall injuries by exceeding drinking guidelines should alert physicians to target falls risk, given some evidence that falls from height may also increase fracture risk (Parreira et al., 2014). Even though multifactorial assessment and intervention programs and some other effective interventions (e.g., the CDC’s fall-prevention program, Stopping Elderly Accidents, Deaths and Injuries [STEADI]) have been identified for preventing falls in older people living in the community and in nursing-care facilities and hospitals (Gillespie et al., 2015), intervention efforts should also target older people who are mobile and drink excessively. Additionally, assessment and intervention programs should be expanded or developed to prevent and reduce these types of fall injuries among younger adults who engage in excessive drinking, as falls are the leading cause of traumatic brain injury (CDC, 2016c) and may entail significant economic costs to the nation (Boake et al., 2005).
Footnotes
CONFLICT OF INTEREST: The authors declare that they have no conflict of interest.
Contributor Information
Mr Chiung M Chen, CSR, Incorporated, 4250 Fairfax Drive, Suite 500, Arlington, 22203 United States.
Dr Young-Hee Yoon, CSR, Incorporated, 4250 Fairfax Drive, Suite 500, Arlington, 22203 United States.
REFERENCES
- Alliston L (2012). Alcohol-related injury: An evidence-based literature review. Wellington, New Zealand: Research New Zealand. [Google Scholar]
- American College of Sports Medicine. (1982). Position statement on the use of alcohol in sports. Medicine & Science in Sports & Exercise, 14, ix–xi.7162384 [Google Scholar]
- Andridge RR, & Little RJ (2010). A review of hot deck imputation for survey non-response. International Statistical Review, 78, 40–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boake C, McCauley SR, Pedroza C, Levin HS, Brown SA, & Brundage SI (2005). Lost productive work time after mild to moderate traumatic brain injury with and without hospitalization. Neurosurgery, 56, 994–1003; discussion 994–1003. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2012). Vital signs: Binge drinking prevalence, frequency, and intensity among adults—United States, 2010. MMWR. Morbidity and Mortality Weekly Report, 61, 14–19. [PubMed] [Google Scholar]
- CDC. (2016a). WISQARS (Web-based Injury Statistics Query and Reporting System). Atlanta, GA: National Center for Injury Prevention and Control; Retrieved 1 June 2016, from http://www.cdc.gov/injury/wisqars/index.html. [Google Scholar]
- CDC. (2016b). CDC Wide-ranging ONline Data for Epidemiologic Research (CDC WONDER). Atlanta, GA: National Center for Injury Prevention and Control; Retrieved 5 December 2016, from https://wonder.cdc.gov/. [Google Scholar]
- CDC. (2016c). Traumatic brain injury in the United States: Fact sheet. Atlanta, GA: National Center for Injury Prevention and Control; Retrieved 10 January 2016, from http://www.cdc.gov/traumaticbraininjury/get_the_facts.html. [Google Scholar]
- Chang VC, & Do MT (2015). Risk factors for falls among seniors: Implications of gender. American Journal of Epidemiology, 181, 521–531. [DOI] [PubMed] [Google Scholar]
- Chen LH, Warner M, Fingerhut L, & Makuc D (2009). Injury episodes and circumstances: National Health Interview Survey, 1997–2007. Vital and Health Statistics. Series 10, Data from the National Health Survey, (241), 1–55. [PubMed] [Google Scholar]
- Cherpitel CJ (1992). Drinking patterns and problems: A comparison of ER patients in an HMO and in the general population. Alcoholism, Clinical and Experimental Research, 16, 1104–1109. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Meyers AR, & Perrine MW (1998). Alcohol consumption, sensation seeking and ski injury: A case-control study. Journal of Studies on Alcohol, 59, 216–221. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Borges G, & Monteiro M (2015). Relative risk of injury from acute alcohol consumption: Modeling the dose–response relationship in emergency department data from 18 countries. Addiction, 110, 279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clausen T, Martinez P, Towers A, Greenfield T, & Kowal P (2015). Alcohol Consumption at Any Level Increases Risk of Injury Caused by Others: Data from the Study on Global AGEing and Adult Health. Substance Abuse: Research and Treatment, 9(Suppl 2), 125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Monte SM, & Kril JJ (2014). Human alcohol-related neuropathology. Acta Neuropathologica, 127, 71–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards MH, Jameson K, Denison H, Harvey NC, Sayer AA, Dennison EM, & Cooper C (2013). Clinical risk factors, bone density and fall history in the prediction of incident fracture among men and women. Bone, 52, 541–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein G, & Greenstein D (2013). Gait and balance deficits in chronic alcoholics: No improvement from 10 weeks through one year abstinence. Alcoholism, Clinical and Experimental Research, 37, 86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frone MR (2006). Prevalence and distribution of alcohol use and impairment in the workplace: A U.S. national survey. Journal of Studies on Alcohol, 67, 147–156. [DOI] [PubMed] [Google Scholar]
- Gauchard GC, Chau N, Touron C, Benamghar L, Dehaene D, Perrin P, & Mur J-M (2003). Individual characteristics in occupational accidents due to imbalance: A case-control study of the employees of a railway company. Occupational and Environmental Medicine, 60, 330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, & Lamb SE (2012). Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews, 9, CD007146.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant SA, Millar K, & Kenny GN (2000). Blood alcohol concentration and psychomotor effects. British Journal of Anaesthesia, 85, 401–406. [DOI] [PubMed] [Google Scholar]
- Grundstrom AC, Guse CE, & Layde PM (2012). Risk factors for falls and fall-related injuries in adults 85 years of age and older. Archives of Gerontology and Geriatrics, 54, 421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Cohen HJ, Pieper CF, Fillenbaum GG, Kraus WE, Huffman KM, … Morey MC (2016). Physical Performance Across the Adult Life Span: Correlates With Age and Physical Activity. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, glw120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgadóttir B, Laflamme L, Monarrez-Espino J, & Moller J (2014). Medication and fall injury in the elderly population; do individual demographics, health status and lifestyle matter? BMC Geriatrics, 14, 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgadóttir B, Moller J, & Laflamme L (2015). Patterns in health-related behaviours and fall injuries among older people: A population-based study in Stockholm County, Sweden. Age and Ageing, 44, 604–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang HC, Lin WC, & Lin JD (2008). Development of a fall-risk checklist using the Delphi technique. Journal of Clinical Nursing, 17, 2275–2283. [DOI] [PubMed] [Google Scholar]
- Kool B, Ameratunga S, & Jackson R (2009). The role of alcohol in unintentional falls among young and middle-aged adults: A systematic review of epidemiological studies. Injury Prevention, 15, 341–347. [DOI] [PubMed] [Google Scholar]
- Kool B, Ameratunga S, Robinson E, Crengle S, & Jackson R (2008). The contribution of alcohol to falls at home among working-aged adults. Alcohol, 42, 383–388. [DOI] [PubMed] [Google Scholar]
- Kurzthaler I, Wambacher M, Golser K, Sperner G, Sperner-Unterweger B, Haidekker A, … Fleischhacker WW (2005). Alcohol and/or benzodiazepine use: Different accidents—different impacts? Human Psychopharmacology, 20, 583–589. [DOI] [PubMed] [Google Scholar]
- López-Larramona G, Lucendo AJ, & González-Delgado L (2013). Alcoholic liver disease and changes in bone mineral density. Revista Española De Enfermedades Digestivas: Organo Oficial De La Sociedad Española De Patología Digestiva, 105, 609–621. [DOI] [PubMed] [Google Scholar]
- Lotfipour S, Cisneros V, Ogbu UC, McCoy CE, Barrios C, Anderson CL, … Chakravarthy B (2015). A retrospective analysis of ethnic and gender differences in alcohol consumption among emergency department patients: A cross-sectional study. BMC Emergency Medicine, 15, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald S, Cherpitel CJ, DeSouza A, Stockwell T, Borges G, & Giesbrecht N (2006). Variations of alcohol impairment in different types, causes and contexts of injuries: Results of emergency room studies from 16 countries. Accident Analysis and Prevention, 38, 1107–1112. [DOI] [PubMed] [Google Scholar]
- Martens MP, Dams-O’Connor K, & Beck NC (2006). A systematic review of college student-athlete drinking: Prevalence rates, sport-related factors, and interventions. Journal of Substance Abuse Treatment, 31, 305–316. [DOI] [PubMed] [Google Scholar]
- Milos V, Bondesson A, Magnusson M, Jakobsson U, Westerlund T, & Midlov P (2014). Fall risk-increasing drugs and falls: A cross-sectional study among elderly patients in primary care. BMC Geriatrics, 14, 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modig F, Fransson PA, Magnusson M, & Patel M (2012). Blood alcohol concentration at 0.06 and 0.10% causes a complex multifaceted deterioration of body movement control. Alcohol, 46, 75–88. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Mittleman MA, Longstreth WT Jr., Newman AB, Fried LP, & Siscovick DS (2004). Self-reported alcohol consumption and falls in older adults: Cross-sectional and longitudinal analyses of the cardiovascular health study. Journal of the American Geriatrics Society, 52, 1174–1179. [DOI] [PubMed] [Google Scholar]
- Muthén LK & Muthén BO (1998. –2012). Mplus user’s guide. Seventh edition. Los Angeles, CA: Muthén and Muthén. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2010). Rethinking drinking: Alcohol and your health. NIH Pub. No. 10–3770. Washington, DC: U.S. Department of Health and Human Services; Retrieved from http://pubs.niaaa.nih.gov/publications/RethinkingDrinking/Rethinking_Drinking.pdf. [Google Scholar]
- Nordqvist C, Holmqvist M, Nilsen P, Bendtsen P, & Lindqvist K (2006). Usual drinking patterns and non-fatal injury among patients seeking emergency care. Public Health, 120, 1064–1073. [DOI] [PubMed] [Google Scholar]
- Office of the Surgeon General (US). (2004). Bone health and osteoporosis: A report of the surgeon general. Rockville (MD: ): Office of the Surgeon General (US) Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK45513/ [PubMed] [Google Scholar]
- O’Brien CP, & Lyons F (2000). Alcohol and the athlete. Sports Medicine, 29, 295–300. [DOI] [PubMed] [Google Scholar]
- Parreira JG, Matar MR, Tôrres ALB, Perlingeiro JAG, Solda SC, & Assef JC (2014). Comparative analysis between identified injuries of victims of fall from height and other mechanisms of closed trauma. Revista Do Colégio Brasileiro De Cirurgiões, 41, 272–277. [DOI] [PubMed] [Google Scholar]
- Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, & Tompkins L (2014). Design and estimation for the national health interview survey, 2006–2015. Vital and Health Statistics. Series 2: Data Evaluation and Methods Research, (165), 1–53. [PubMed] [Google Scholar]
- Ramchand R, Pomeroy A, & Arkes J (2009). The effects of substance use on workplace injuries. Santa Monica, CA: The RAND Corporation. [Google Scholar]
- Royston P, & Sauerbrei W (2007). Multivariable modeling with cubic regression splines: A principled approach. Stata Journal, 7(1), 45–70. [Google Scholar]
- Rubenstein LZ (2006). Falls in older people: Epidemiology, risk factors and strategies for prevention. Age and Ageing, 35 Suppl 2, ii37–ii41. [DOI] [PubMed] [Google Scholar]
- Schiller JS, Kramarow EA, & Dey AN (2007). Fall injury episodes among noninstitutionalized older adults: United States, 2001–2003. Advance Data, (392), 1–16. [PubMed] [Google Scholar]
- Smith GS, & Kraus JF (1988). Alcohol and residential, recreational, and occupational injuries: A review of the epidemiologic evidence. Annual Review of Public Health, 9, 99–121. [DOI] [PubMed] [Google Scholar]
- Smothers B, & Bertolucci D (2001). Alcohol consumption and health-promoting behavior in a U.S. household sample: Leisure-time physical activity. Journal of Studies on Alcohol, 62, 467–476. [DOI] [PubMed] [Google Scholar]
- Stallones L, & Kraus JF (1993). The occurrence and epidemiologic features of alcohol-related occupational injuries. Addiction, 88, 945–951. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata statistical software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- Stenbacka M, Jansson B, Leifman A, & Romelsjo A (2002). Association between use of sedatives or hypnotics, alcohol consumption, or other risk factors and a single injurious fall or multiple injurious falls: A longitudinal general population study. Alcohol, 28, 9–16. [DOI] [PubMed] [Google Scholar]
- Stevens JA, Mack KA, Paulozzi LJ, & Ballesteros MF (2008). Self-reported falls and fall-related injuries among persons aged ≥ 65 years—United States, 2006. Journal of Safety Research, 39, 345–349. [DOI] [PubMed] [Google Scholar]
- Stewart Williams J, Kowal P, Hestekin H, O’Driscoll T, Peltzer K, Yawson A, … SAGE collaborators. (2015). Prevalence, risk factors and disability associated with fall-related injury in older adults in low- and middle-income countries: Results from the WHO Study on global AGEing and adult health (SAGE). BMC Medicine, 13, 147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, … Rehm J (2010). The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug and Alcohol Dependence, 110, 108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornley S, Kool B, Marshall RJ, & Ameratunga S (2014). Alcohol intake, marijuana use, and sleep deprivation on the risk of falls occurring at home among young and middle-aged adults: A case-crossover study. New Zealand Medical Journal, 127(1406), 32–38. [PubMed] [Google Scholar]
- Warner M, Schenker N, Heinen MA, & Fingerhut LA (2005). The effects of recall on reporting injury and poisoning episodes in the National Health Interview Survey. Injury Prevention, 11, 282–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb GR, Redman S, Hennrikus DJ, Kelman GR, Gibberd RW, & Sanson-Fisher RW (1994). The relationships between high-risk and problem drinking and the occurrence of work injuries and related absences. Journal of Studies on Alcohol, 55, 434–446. [DOI] [PubMed] [Google Scholar]
- Wells S, & Macdonald S (1999). The relationship between alcohol consumption patterns and car, work, sports and home accidents for different age groups. Accident Analysis and Prevention, 31, 663–665. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2006). WHO SAGE Survey Manual: The WHO Study on Global AGEing and Adult Health (SAGE). Geneva, Switzerland: Author. [Google Scholar]
- World Health Organization. (2007). WHO global report on falls prevention in older age. Geneva, Switzerland: Author. [Google Scholar]


