Abstract
BACKGROUND
There is limited evidence from nationally representative samples about changes in prescription drug use for financial reasons among cancer survivors in the United States.
METHODS
The 2011 to 2014 National Health Interview Survey was used to identify adults who reported ever having been told they had cancer (cancer survivors; n = 8931) and individuals without a cancer history (n = 126,287). Measures of changes in prescription drug use for financial reasons included: 1) skipping medication doses, 2) taking less medicine, 3) delaying filling a prescription, 4) asking a doctor for lower cost medication, 5) buying prescription drugs from another country, and 6) using alternative therapies. Multivariable logistic regression analyses were controlled for demographic characteristics, number of comorbid conditions, interactions between cancer history and number of comorbid conditions, and health insurance coverage. Main analyses were stratified by age (nonelderly, ages 18–64 years; elderly, ages ≥65 years) and time since diagnosis (recently diagnosed, <2 years; previously diagnosed, ≥2 years).
RESULTS
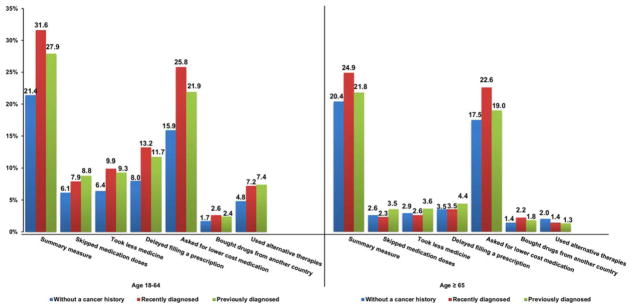
Among nonelderly individuals, both recently diagnosed (31.6%) and previously diagnosed (27.9%) cancer survivors were more likely to report any change in prescription drug use for financial reasons than those without a cancer history (21.4%), with the excess percentage changes for individual measures ranging from 3.5% to 9.9% among previously diagnosed survivors and from 2.6% to 2.7% among recently diagnosed survivors (P < .01). Elderly cancer survivors and those without a cancer history had comparable rates of changes in prescription drug use for financial reasons.
CONCLUSIONS
Nonelderly cancer survivors are particularly vulnerable to changes in prescription drug use for financial reasons, suggesting that targeted efforts are needed.
Keywords: cancer survivors, comorbid conditions, financial burden, high-deductible plan, prescription drugs
INTRODUCTION
The rising cost of cancer drugs imposes a significant financial burden on patients with cancer and their families.1,2 The direct medical cost of a new cancer medication per patient can routinely exceed $100,000 annually.2,3 Because of rising deductibles, copayments, coinsurance, and tiered drug formularies, an increasing portion of the cost of cancer drugs is shifted to the patient as out-of-pocket (OOP) costs.4,5 Previous studies demonstrated that cancer survivors faced significantly higher OOP costs than individuals without a cancer history.6–8 The financial burden caused by the high OOP costs for cancer drugs may further impair cancer survivors’ overall well being, adversely affect treatment choices and health outcomes, and result in higher medical expenditures in the long run.9–13 Moreover, the increasing number of expensive, patient-administrated, oral antineoplastic agents may increase the likelihood that patients with cancer may delay, skip, or even forgo their prescription medications for financial reasons.13–16
A cancer diagnosis is associated with reduced adherence to recommended prescription drugs for other comorbid conditions, such as diabetes and cardiovascular disease, although, in some studies, it was unknown whether this was for financial reasons.17–19 Previous studies demonstrating that patients with cancer make changes in prescription drug use to defray OOP costs are limited to small sample sizes, specific cancer sites, single-institutional experience, or trials without a noncancer control group.11,20–22 In the current study, we used nationally representative data to compare the changes in prescription drug use for financial reasons between cancer survivors and individuals without a cancer history. Because the intensity and aggressiveness of cancer-related treatments and associated costs are likely to be greater in nonelderly than in elderly patients and in those diagnosed in the most recent time period than in the past,23–25 we stratified the analyses by age group and time since diagnosis. Moreover, we examined whether high private health insurance deductibles were associated with changes in prescription drug use for financial reasons among nonelderly cancer survivors. We also examined whether the pattern of changes in prescription drug use varies according to the number of comorbid conditions among cancer survivors.
MATERIALS AND METHODS
Data Sources
The National Health Interview Survey (NHIS) from 2011 through 2014 was used to identify cancer survivors and individuals without a cancer history. The NHIS is a cross-sectional household interview survey conducted annually by the Centers for Disease Control and Prevention’s National Center for Health Statistics. It is a nationally representative survey of the civilian, noninstitutionalized population of the United States. The survey collects information on health status, access to and use of health care services, and comorbid conditions. The annual NHIS response rate ranged from 73.8% to 82% of eligible households during our study period.26
Individual-Level Characteristics and Analytic Sample
In the NHIS, cancer history is self-reported. We defined cancer survivors as those who reported ever having been told by a physician or other health professional that they had cancer or a malignancy of any kind. Cancer survivors who reported nonmelanoma skin cancer or skin cancer with unknown type were excluded.27,28 Individual-level demographic and clinical characteristics included, age at the time of the survey (nonelderly: ages 18–49 or 50–64 years; elderly: ages 65–74 or ≥75 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other), educational attainment (≤high school graduate or ≥some college), marital status (married or not married), geographic region (Northeast, Midwest, South, or West), health insurance coverage, and number of comorbid conditions (0, 1, 2, or ≥3). The health insurance coverage variable was defined differently for the 2 age groups (nonelderly: any private, other, or uninsured; elderly: Medicare with any private or other). Comorbid conditions included: arthritis, asthma, diabetes, emphysema, coronary heart disease, hypertension, stroke, angina pectoris, and heart attack.
Time since diagnosis was calculated using age at cancer diagnosis and age at the time of the survey. We used 2 years as the cutoff point for categorizing those who were recently diagnosed and previously diagnosed to be consistent with previous studies.7,29 In the NHIS, private health insurance with an annual deductible >$1200 per individual or $2400 per family was categorized as a high-deductible plan.26 An indicator for high insurance deductible status was created among nonelderly cancer survivors who had any private health insurance coverage during the survey year. The final sample was stratified by age group (nonelderly population, ages 18–64 years; elderly population, ages ≥65 years) and time since diagnosis (recently diagnosed, <2 years; previously diagnosed, ≥2 years), including recently diagnosed (nonelderly, n = 686; elderly, n = 720) and previously diagnosed (nonelderly, n = 3295; elderly, n = 4230) cancer survivors and individuals without a cancer history (nonelderly, n = 76,096; elderly, n =16,989).
Measures of Changes in Prescription Drug Use for Financial Reasons
The NHIS included 6 measures of changes in prescription drug use for financial reasons. These are general questions about all prescriptions drugs and thus are not cancer specific. Respondents were asked the following questions: “During the past 12 months, were any of the following true for you: 1) you skipped medication doses to save money, 2) you took less medicine to save money, 3) you delayed filling a prescription to save money, 4) you asked your doctor for a lower cost medication to save money, 5) you bought prescription drugs from another country to save money, 6) you used alternative therapies to save money.” A summary measure (yes/no) of any of the 6 measures and a categorical count of changes in prescription drug use for financial reasons (scored as 0, 1, or ≥2) also were also created.
Statistical Methods
We compared the distributions of individual-level characteristics between cancer survivors and those without a cancer history. We used multivariable logistic regression models for each of the 6 measures and the summary measure to estimate the changes in prescription drug use for financial reasons for both cancer survivors and individuals without a cancer history. Among nonelderly cancer survivors with private health insurance, we used multivariable logistic regressions to compare the patterns of changes in prescription drug use between high-deductible plans and low-deductible plans. We did not examine this association among the elderly cancer survivors because of their nearly universal eligibility for insurance through Medicare. Among all cancer survivors, multivariable ordered logistic regression was used to investigate associations between the number of comorbid conditions and changes in prescription drug use for financial reasons. Sensitivity analyses were conducted to examine the robustness of our findings by evaluating various summary measures based on a different reduced set of questions about changes in prescription drug use.
All multivariable regressions adjusted for survey year, age, race/ethnicity, sex, educational attainment, marital status, geographic region, health insurance coverage, the number of comorbid conditions, and interactions between cancer history and the number of comorbid conditions. The NHIS annual sampling weights were adjusted to reflect pooling data across multiple years and were used in all analyses to provide nationally representative estimates.30 All adjusted estimates of changes in prescription drug use for financial reasons are presented as predictive margins.31 All analytic files were created using SAS version 9.3. Multivariable logistic and ordered logistic regressions were performed using STATA 13.1. Statistical comparisons were 2-sided, and significance was defined as P < .05.
RESULTS
Distribution of Individual-Level Characteristics and Unadjusted Changes in Prescription Drug Use for Financial Reasons
Compared with individuals who had no history of cancer, cancer survivors were more likely to be older, non-Hispanic white, married (nonelderly population only), and privately insured and to have more comorbid conditions (Table 1). Nonelderly cancer survivors were more likely to be women, whereas elderly cancer survivors were more likely to be men compared with individuals who had no history of cancer. Among privately insured non-elderly cancer survivors, 41% of those who were recently diagnosed and 64% of those who were previously diagnosed enrolled in high-deductible plans. We also observed that both recently diagnosed and previously diagnosed nonelderly cancer survivors were more likely to report changes in prescription drug use for financial reasons than individuals without a history of cancer.
TABLE 1.
Distribution of Unadjusted Measures of Changes in Prescription Drug Use for Financial Reasons and Individual-Level Characteristics of Cancer Survivors and Individuals Without a Cancer History, Stratified by Age (18–64 and ≥65 Years) and Time Since Diagnosis (<2 and ≥2 Years): 2011–2014 National Health Interview Surveya
| Unadjusted Changes in Prescription Drug Use for Financial Reasons | Cancer Survivors, n = 8931 | Percentage | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Recently Diagnosed: <2 Years, n = 1496 | Previously Diagnosed: ≥2 Years, n = 8065 | |||||||||
|
|
|
|
|
|||||||
| Ages 18–64, n = 715 | Aged ≥65 Years, n = 781 | Ages 18–64 Years, n = 3519 | Aged ≥65 Years, n = 4546 | Individuals Without a Cancer History, n = 126,287 | ||||||
|
|
|
|
|
|
||||||
| Percentage | Pb | Percentage | Pc | Percentage | Pb | Percentage | Pc | Ages 18–64 Years, n = 102,630 | Aged ≥65 Years, n = 23,657 | |
| Summary measure | 35.1 | < .001 | 24.4 | .067 | 34.2 | < .001 | 22.1 | .056 | 21.1 | 20.3 |
| 1. Skipped medication doses | 9.6 | .008 | 2.4 | .634 | 11.7 | < .001 | 3.2 | .123 | 6 | 2.7 |
| 2. Took less medicine | 10.4 | .004 | 2.7 | .676 | 12.3 | < .001 | 3.3 | .242 | 6.3 | 2.9 |
| 3. Delayed filling a prescription | 13.8 | < .001 | 4.1 | .540 | 15.2 | < .001 | 4 | .234 | 7.9 | 3.5 |
| 4. Asked doctor for lower cost medication | 29.9 | < .001 | 21.9 | .040 | 28.1 | < .001 | 19.5 | .017 | 15.6 | 17.4 |
| 5. Bought prescription drugs from another country | 2.1 | .607 | 1.8 | .582 | 2 | .472 | 1.7 | .400 | 1.8 | 1.4 |
| 6. Used alternative therapies | 6.6 | .118 | 1.2 | .044 | 7.6 | < .001 | 1.2 | .005 | 4.8 | 2 |
|
| ||||||||||
| Individual-level characteristics | ||||||||||
|
| ||||||||||
| Survey year | ||||||||||
| 2011 | 25.2 | .934 | 24.6 | .551 | 23.7 | .591 | 23.7 | .582 | 24.8 | 23.1 |
| 2012 | 25.9 | 25.5 | 24.8 | 24.6 | 24.9 | 24.5 | ||||
| 2013 | 23.9 | 23 | 26.1 | 26.3 | 25.1 | 25.6 | ||||
| 2014 | 25 | 26.9 | 25.3 | 25.4 | 25.2 | 26.8 | ||||
| Age, y | ||||||||||
| 18–49 | 40 | <.001 | 35.1 | < .001 | 70.4 | |||||
| 50–64 | 60 | 64.9 | 29.6 | |||||||
| 65–74 | 47.3 | < .001 | 50.1 | <.001 | 59.3 | |||||
| ≥75 | 52.7 | 49.9 | 40.7 | |||||||
| Sex | ||||||||||
| Men | 44.5 | <.001 | 51.3 | < .001 | 33.1 | < .001 | 47.7 | <.001 | 49.7 | 42.5 |
| Women | 59.5 | 48.7 | 66.9 | 52.3 | 50.3 | 57.5 | ||||
| Race/ethnicity | ||||||||||
| Non-Hispanic white | 76.6 | <.001 | 83.8 | < .001 | 78.8 | < .001 | 84.9 | <.001 | 62.7 | 76.2 |
| Non-Hispanic black | 9.3 | 7.7 | 8.1 | 7.6 | 12.5 | 9.3 | ||||
| Hispanic | 8.9 | 5.8 | 8.1 | 4.2 | 17 | 8.7 | ||||
| Other | 5.2 | 2.7 | 5 | 3.3 | 7.8 | 5.9 | ||||
| Education | ||||||||||
| ≤High school | 37.8 | .775 | 53.6 | .409 | 37.1 | .193 | 47.9 | < .001 | 38.5 | 51.6 |
| ≥Some college | 62.2 | 46.4 | 62.9 | 52.1 | 61.5 | 48.4 | ||||
| Marital status | ||||||||||
| Not married | 38.6 | < .001 | 45.4 | .628 | 41.2 | < .001 | 43.6 | .484 | 48.3 | 44.4 |
| Married | 61.4 | 54.6 | 58.8 | 56.4 | 51.7 | 55.6 | ||||
| No. of chronic conditionsd | ||||||||||
| 0 | 30 | < .001 | 15.5 | .002 | 32.6 | < .001 | 11.6 | < .001 | 59.6 | 18.7 |
| 1 | 36.4 | 240 | 30.6 | 27.3 | 25.4 | 28.6 | ||||
| 2 | 16.8 | 26.6 | 19.1 | 29.3 | 9.7 | 26.5 | ||||
| ≥3 | 16.8 | 33.9 | 17.7 | 31.8 | 5.3 | 26.2 | ||||
| Health insurance | ||||||||||
| Aged ≤64 y | ||||||||||
| Any privatee | 65.3 | < .001 | 65.5 | < .001 | 64.8 | |||||
| Other coverage | 25 | 21.5 | 14.9 | |||||||
| Uninsured | 9.7 | 13 | 20.3 | |||||||
| Aged ≥65 y | ||||||||||
| Medicare with any private | 52.9 | .002 | 51.5 | < .001 | 45.9 | |||||
| Other coverage | 47.1 | 48.5 | 54.1 | |||||||
| Family income level | ||||||||||
| $0–$34,999 | 29.6 | .675 | 39.4 | .298 | 28.3 | .252 | 37.0 | .003 | 29.2 | 39.9 |
| $35,000–$74,999 | 28.8 | 26.6 | 28.9 | 30.6 | 29.4 | 29.1 | ||||
| ≥$75,000 | 36.8 | 22.3 | 37.2 | 21.4 | 35 | 18.9 | ||||
| Unknown | 4.8 | 11.8 | 5.7 | 11 | 6.4 | 12.1 | ||||
| Region | ||||||||||
| Northeast | 17.6 | .978 | 18.2 | .728 | 18.6 | .051 | 18.4 | .018 | 17.4 | 19.6 |
| Midwest | 23.2 | 21.6 | 24.1 | 24.4 | 22.9 | 22 | ||||
| South | 35.4 | 39.5 | 36.7 | 37.2 | 36.4 | 36.9 | ||||
| West | 23.8 | 20.6 | 26.6 | 20 | 23.3 | 21.5 | ||||
All statistical tests were 2-sided, and all P values were calculated using the Pearson chi-square test statistic, and all percentages were column percentages.
The comparison group consisted of nonelderly individuals without a cancer history.
The comparison group consisted of elderly individuals without a cancer history.
The number of chronic conditions was defined as the sum of the following conditions that a respondent was ever told by a physician or other health professional that s/he had: arthritis, asthma, diabetes, emphysema, coronary heart disease, hypertension, stroke, angina pectoris, and heart attack. High cholesterol was not included because of the inconsistency of the availability of this variable across years.
Among nonelderly cancer survivors who had any private health insurance during the survey year, 41% of those who were recently diagnosed and 64% of those who were previously diagnosed had high-deductible insurance plans.
Adjusted Changes in Prescription Drug Use Between Cancer Survivors and Individuals Without a Cancer History
In the adjusted analyses, we observed that nonelderly cancer survivors were more likely to report changes in prescription drug use for financial reasons than nonelderly individuals without a cancer history (see Fig. 1 for total percentage changes and Table 2 for excess percentage changes). For the summary measure, 31.6% of recently diagnosed and 27.9% of previously diagnosed cancer survivors reported any change in prescription drug use for financial reasons, compared with 21.4% of individuals without a cancer history. The excess changes in prescription drug use for financial reasons associated with cancer were 10.2% (95% confidence interval [CI], 5.6%–14.8%) and 6.6% (95% CI, 4.4%–8.7%; all P < .05) for recently and previously diagnosed cancer survivors, respectively.
Figure 1.
Individual measures and summary measures of changes in prescription drug use for financial reasons are illustrated among cancer survivors and individuals without a cancer history (National Health Interview Survey, 2011–2014). All analyses were stratified by age (nonelderly vs elderly) and time since diagnosis (recently diagnosed vs previously diagnosed). Multivariable logistic regressions controlled for survey year, age, race/ethnicity, sex, educational attainment, marital status, number of comorbid conditions, health insurance coverage, and geographic region. Blue bars represent individuals without a cancer history; red bars, recently diagnosed cancer survivors; green bars, previously diagnosed cancer survivors.
TABLE 2.
Excess Adjusted Changes in Prescription Drug Use for Financial Reasons Among Cancer Survivors Compared With Individuals Without a Cancer History: Results From Multivariable Logistic Regression and Stratified by Age (18–64 vs ≥65 Years), 2011–2014 National Health Interview Studya
| Changes in Prescription Drug Use Measures | Cancer Survivors | |||
|---|---|---|---|---|
|
| ||||
| Recently Diagnosed: <2 Years | Previously Diagnosed: ≥2 Years | |||
|
|
|
|||
| Excess Percentage (95% CI) | Pb | Excess Percentage (95% CI) | Pb | |
| Ages 18–64 y | n = 715 | n = 3,519 | ||
| Summary measurec | 10.2 (5.6, 14.8) | < .001 | 6.6 (4.4, 8.7) | < .001 |
| 1. Skipped medication dosesd | 1.8 (−0.5, 4.0) | .121 | 2.7 (1.4, 3.9) | < .001 |
| 2. Took less medicine | 3.5 (0.3, 6.6) | .032 | 2.8 (1.6, 4.1) | < .001 |
| 3. Delayed filling a prescription | 5.2 (1.4, 9.1) | .007 | 3.7 (2.3, 5.1) | < .001 |
| 4. Asked doctor for lower cost medication | 9.9 (5.6, 14.2) | < .001 | 6.0 (4.1, 7.9) | < .001 |
| 5. Bought prescription drugs from another country | 0.9 (−1.2, 3.0) | .411 | 0.7 (−0.3, 1.7) | .186 |
| 6. Used alternative therapies | 2.3 (−0.5, 5.2) | .113 | 2.6 (1.3, 3.8) | < .001 |
| Aged ≥65 y | n = 781 | n = 4,546 | ||
| Summary measurec | 4.5 (0.2, 8.8) | .041 | 1.5 (−0.3, 3.2) | .099 |
| 1. Skipped medication doses | −0.3 (−1.5, 0.9) | .629 | 0.9 (0.1, 1.6) | .017 |
| 2. Took less medicine | −0.3 (−1.5, 0.9) | .605 | 0.7 (0.1, 1.4) | .037 |
| 3. Delayed filling a prescription | 0.0 (−1.5, 1.5) | .999 | 0.9 (0.1, 1.7) | .035 |
| 4. Asked doctor for lower cost medication | 5.0 (1.0, 9.1) | .016 | 1.5 (−0.2, 3.1) | .079 |
| 5. Bought prescription drugs from another country | 0.8 (−0.5, 2.2) | .241 | 0.4 (−0.2, 1.0) | .214 |
| 6. Used alternative therapies | −0.6 (−1.5, 0.3) | .187 | 0.6 (−1.1, −0.1) | .012 |
Abbreviations: CI, confidence interval; OR, odds ratio.
All statistical tests were 2-sided, and all P values were derived from multivariable logistic regressions. All logistic regression analyses were controlled for survey year, age, sex, race/ethnicity, education, marital status, number of comorbid conditions, interactions between cancer history and number of comorbid conditions, health insurance status, and geographic region (Northeast, Midwest, South, and West).
P values reflect the statistical significance level of the changes in prescription drug use among cancer survivors versus individuals without a cancer history using multivariable logistic regression analysis.
All questions about changes in prescription drug use were asked for the last 12 months at the time of the survey. It was determined that the respondent was trying to save money if any of the items (skipped medication doses, took less medicine, delayed filing a prescription, asked doctor for lower cost medication, bought prescription drugs from another country, or used alternative therapies) were reported.
The survey question asks, “During the past 12 months, were any of the following true for you? . . .You skipped medication doses to save money.”
For individual measures among the nonelderly population, we observed that, compared with the control group: 1) 8.8% of previously diagnosed cancer survivors reported skipping medication doses (excess change, 2.7%; 95% CI, 1.4%–3.9%); 2) 9.9% of recently diagnosed and 9.3% of previously diagnosed cancer survivors reported taking less medicine (excess changes, 3.5% [95% CI, 0.3%–6.6%] and 2.8% [95% CI, 1.6%–4.1%], respectively); 3) 13.2% of recently diagnosed and 11.7% of previously diagnosed cancer survivors reported delaying filing a prescription (excess changes, 5.2% [95% CI, 1.4%–9.1%] and 3.7% [95% CI, 2.3%–5.1%], respectively); 4) 25.8% of recently diagnosed and 21.9% of previously diagnosed cancer survivors reported asking for lower cost medication (excess changes, 9.9% [95% CI, 5.6%–14.2%] and 6% [95% CI, 4.1%–7.9%], respectively); and 5) 7.4% of previously diagnosed cancer survivors reported using alternative therapies (excess change, 2.6%; 95% CI, 1.3%–3.8%; all P < .05).
Among the elderly population, we observed that, compared with the control group: 1) 22.6% of recently diagnosed cancer survivors reported asking for lower cost medication (excess change, 5% [95% CI, 1%–9.1%]; 2) on average, approximately 4% of previously diagnosed cancer survivors reported skipping medication doses, taking less medicine, and delaying filling a prescription (excess change, <1%) compared with individuals without a cancer history (all P < .05).
When the analyses were stratified by the number of comorbid conditions and compared with the control group (Supporting Table 1; see online supporting information), we observed that nonelderly cancer survivors were more likely to report changes in prescription drug use for financial reasons when the number of comorbid conditions was ≤1 for recently diagnosed patients and ≤2 for previously diagnosed patients (all P < .05). Elderly cancer survivors and those without a cancer history had comparable rates of changes in prescription drug use for financial reasons when stratified by the number of comorbid conditions.
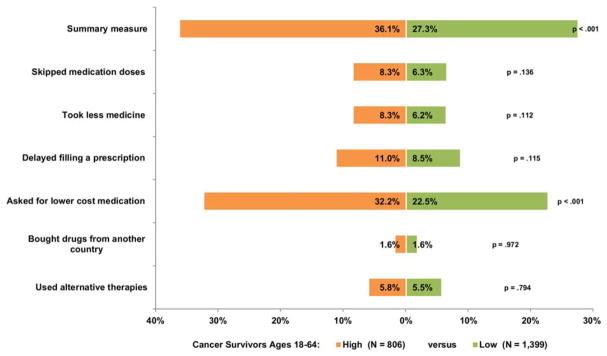
Insurance Deductible Status and Adjusted Changes in Prescription Drug Use for Financial Reasons Among Nonelderly Cancer Survivors
Among privately insured nonelderly cancer survivors, 806 were enrolled in high-deductible plans, and 1399 enrolled in low-deductible plans (Fig. 2). Compared with those enrolled in low-deductible plans (22.5%), nonelderly cancer survivors enrolled in high-deductible plans (32.2%) were more likely to ask their doctor for lower cost medication (odds ratio, 1.71; 95% CI, 1.32–2.22) (Supporting Table 2; see online supporting information).
Figure 2.
Patterns of changes in prescription drug use for financial reasons are illustrated among nonelderly cancer survivors who were enrolled in high-deductible plans versus low-deductible plans (multivariable adjusted; National Health Interview Survey, 2011–2014).
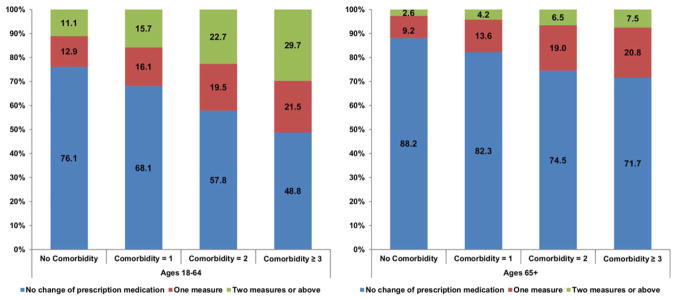
Adjusted Changes in Prescription Drug Use by Number of Comorbid Conditions Among Cancer Survivors
We observed that, as the number of comorbid conditions increased from 0 to ≥ 3 (Fig. 3): 1) the adjusted percentages of nonelderly cancer survivors increased from 24% to 51.2% for reporting any change and from 11.1% to 29.7% for reporting 2 or more changes in prescription drug use (all P < .001), respectively; 2) the adjusted percentages of elderly cancer survivors increased from 11.8% to 28.3% for reporting any change and from 2.6% to 7.5% for reporting 2 or more changes in prescription drug use (all P < .001), respectively. Time since diagnosis was not associated with the number of changes in prescription drug use that cancer survivors reported for financial reasons (Supporting Table 3; see online supporting information).
Figure 3.
Patterns of changes in prescription drug use for financial reasons are illustrated by the number of comorbid conditions among cancer survivors only (multivariable, ordered logistic regression stratified by age [18–64 vs ≥ 65 years]; National Health Interview Survey, 2011–2014). Blue areas represent the percentages of cancer survivors that had no change in prescription drug use; red areas, the percentages that had exactly 1 change in prescription drug use; green areas, the percentages that had at least 2 changes in prescription drug use.
Sensitivity Analysis
Our findings of the summary measure were robust to various definitions that included different measures between cancer survivors and those without a cancer history (Supporting Table 4; see online supporting information).
DISCUSSION
Our study used a nationally representative sample to estimate patterns of changes in prescription drug use for financial reasons in both the nonelderly and elderly population of cancer survivors in the United States. We observed that both recently and previously diagnosed cancer survivors in the United States are more likely to alter their prescription drug use for financial reasons compared with individuals who do not have a history of cancer. This is particularly true in the nonelderly population. Moreover, nonelderly cancer survivors with high-deductible plans are more likely to ask for lower cost medication than those with low-deductible plans.
Nonelderly cancer survivors are particularly vulnerable to the risk of changing their prescription drug use for financial reasons, which may be explained in part by the complex relationship between employment and insurance coverage. A cancer diagnosis can result in barriers to working, productivity loss at work, reduced income, and employment disability.7,8,32–34 The loss of employment-based insurance coverage increases the likelihood of delaying and missing care because of cost.35 Cancer survivors have been reported to have difficulties living within their household income, accrued debt, sold or refinanced their home, borrowed money from friends or family, or experienced a decline ≥20% in annual income because of treatment-related expenses.9,36 Our findings are consistent with the literature indicating that younger age is associated with increased risks of cancer-related financial problems and higher rates of personal bankruptcy because of medical bills.9,29,32
Although elderly cancer survivors are likely to take more prescription drugs than elderly individuals without a history of cancer and may forgo expensive cancer drugs for financial reasons, we did not observe systematic differences in the probabilities of reporting changes in prescription drug use for financial reasons between them. This is likely because of the near universal enrollment in Medicare, including prescription drug coverage for many, which may reduce the impact of medication cost on drug use.23 Moreover, the measures of changes in prescription drug use include both cancer drugs and prescription drugs for other comorbid conditions. More than one-half of elderly individuals without a history of cancer had 2 or more comorbid conditions, which may also require prescription drugs. Although nonelderly and elderly populations are quite different in health status and financial situation, our results suggest that establishing programs that expand equitable access to care and prescription coverage in the nonelderly population can attenuate the financial burden of prescription drugs.
In the current study, we observed that the number of comorbid conditions was associated with changes in prescription drug use for financial reasons among cancer survivors. Others have reported that a new cancer diagnosis was associated with nonadherence to prescription drugs for diabetes and cardiovascular disease,17–19 which can have adverse consequences for the treatment of these conditions and may increase the risk of competing illnesses. Cancer is a life-threatening disease and may shift the focus of patients and providers from other comorbid conditions to cancer-related treatments.37 In addition, the discontinuation of recommended prescription drugs for other co-morbid conditions may result from a poor cancer prognosis, in which the risk of dying from cancer exceeds the risk of dying from other comorbid conditions.19,38
Our finding of an association between health insurance deductible status and asking physicians for lower cost medication among privately insured nonelderly cancer survivors is consistent with the research literature indicating that high OOP costs are associated with medication nonadherence.13,21,39–42 Future studies should monitor the changes in prescription drug use among cancer survivors, because several provisions of the Affordable Care Act (ACA) may play an important role in providing insurance coverage and reducing OOP costs.43 Under the ACA, nonelderly cancer survivors will not be precluded from coverage because of preexisting conditions and will not lose coverage because of a cancer diagnosis. Elderly cancer survivors will benefit from the elimination of the coverage gap in Medicare Part D. Affordable health insurance plans through the Health Insurance Marketplace and tax credits toward reductions in OOP costs will also help cancer survivors reduce financial burden. Additional coverage through Medicaid expansion in certain states will also help low-income families lower the financial burden associated with cancer and its treatments. However, the extent to which the ACA can improve medication adherence among cancer survivors and whether total health care costs can be reduced because of improved treatment outcomes remain to be examined.44,45
Although we do not have information about whether these measures of changes in prescription drug use were specifically for cancer, our results from the summary measure were robust for the majority of cancer survivors in our sample when stratified according to the number of co-morbid conditions. Therefore, our findings have implications for both oncologists and primary care physicians. The American Society of Clinical Oncology has identified patient-oncologist communication about cost as an important component of high-quality cancer care.46 However, the majority of patients with cancer do not discuss costs with their providers despite their common concerns about the financial burden.47,48 Medical oncologists also need guidance about how to discuss costs with their patients, particularly when incremental costs are substantial but the marginal benefit is very small.46,49–51 Moreover, the increasing availability of expensive oral regimens may also require oncologists and patients to discuss the financial burden when making treatment decisions.3,52–56 Primary care physicians may want to consider the overall financial burden of prescription drugs among cancer survivors when coordinating care with oncologists, managing other comorbid conditions, and providing follow-up care to patients with cancer.57,58
Our study has several limitations. The cancer history was self-reported. However, previous studies indicated that medical records and self-reported cancer history are highly consistent.59,60 Time since diagnosis was measured by the difference between age at the time of the survey and age at cancer diagnosis,7,28,61 which may have been subject to measurement error. Moreover, we did not have information on health insurance premiums, copayments, or coinsurance. Despite these limitations, our study used a nationally representative sample of adult cancer survivors, a comparison group without a history of cancer in both nonelderly and elderly populations, and detailed measures of health insurance stratified by age group. Our study provides a comprehensive analysis on the patterns of changes in prescription drug use at the national level and can be used to improve the quality of care among cancer survivors.
Conclusions
Compared with individuals without a cancer history, US cancer survivors face greater risks of changing their prescription drug use for financial reasons, particularly those aged <65 years. The patterns of changes in prescription drug use among cancer survivors vary by the number of comorbid conditions. Health care policies that help cancer survivors address the financial burden of prescription drugs should target those who have multiple comorbid conditions and high-deductible health plans.
Supplementary Material
Acknowledgments
FUNDING SUPPORT
No specific funding was disclosed.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the US Department of Health and Human Services.
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
AUTHOR CONTRIBUTIONS
Zhiyuan Zheng: Contributed to study concept and design, acquisition of data, statistical analysis, interpretation of data, and writing of the initial draft. Xuesong Han: Critical revision of the article for intellectual content. Gery P. Guy, Jr: Critical revision of the article for intellectual content. Amy J. Davidoff: Critical revision of the article for intellectual content. Chunyu Li: Critical revision of the article for intellectual content. Matthew P. Banegas: Critical revision of the article for intellectual content. Donatus U. Ekwueme: Critical revision of the article for intellectual content. K. Robin Yabroff: Contributed to study concept and design, writing of the initial draft, analysis and interpretation of data, critical article revision, study supervision, and guarantor of the overall content. Ahmedin Jemal: Contributed to study concept and design, writing of the initial draft, analysis and interpretation of data, critical article revision, study supervision, and guarantor of the overall content.
Additional supporting information may be found in the online version of this article.
References
- 1.Goldman DP, Joyce GF, Lawless G, Crown WH, Willey V. Benefit design and specialty drug use. Health Aff (Millwood) 2006;25:1319–1331. doi: 10.1377/hlthaff.25.5.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kantarjian HM, Fojo T, Mathisen M, Zwelling LA. Cancer drugs in the United States: justum pretium—the just price. J Clin Oncol. 2013;31:3600–3604. doi: 10.1200/JCO.2013.49.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mailankody S, Prasad V. Comparative effectiveness questions in oncology. N Engl J Med. 2014;370:1478–1481. doi: 10.1056/NEJMp1400104. [DOI] [PubMed] [Google Scholar]
- 4.Davidoff AJ, Erten M, Shaffer T, et al. Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 2013;119:1257–1265. doi: 10.1002/cncr.27848. [DOI] [PubMed] [Google Scholar]
- 5.The Henry J. Kaiser Family Foundation. [Accessed September 2015];Distribution of Covered Workers Facing Different Cost-Sharing Formulas for Prescription Drug Benefits, 2000–2012. Available at: http://kff.org/health-costs/slide/distribution-of-covered-workers-facing-different-cost-sharing-formulas-for-prescription-drug-benefits-2000-2012/
- 6.Bernard DS, Farr SL, Fang Z. National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol. 2011;29:2821–2826. doi: 10.1200/JCO.2010.33.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guy GP, Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;20:3749–3757. doi: 10.1200/JCO.2013.49.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekwueme DU, Yabroff KR, Guy GP, Jr, et al. Medical costs and productivity losses of cancer survivors—United States, 2008–2011. MMWR Morb Mortal Wkly Rep. 2014;63:505–510. [PMC free article] [PubMed] [Google Scholar]
- 9.Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11:145–150. doi: 10.1200/JOP.2014.001542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ubel PA, Abernethy AP, Zafar SY. Full disclosure—out-of-pocket costs as side effects. N Engl J Med. 2013;369:1484–1486. doi: 10.1056/NEJMp1306826. [DOI] [PubMed] [Google Scholar]
- 11.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18:381–390. doi: 10.1634/theoncologist.2012-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guy GP, Jr, Yabroff KR, Ekwueme DU, et al. Healthcare expenditure burden among nonelderly cancer survivors, 2008–2012. Am J Prev Med. 2015;49(6 suppl 5):S489–S497. doi: 10.1016/j.amepre.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Darkow T, Henk HJ, Thomas SK, et al. Treatment interruptions and non-adherence with imatinib and associated healthcare costs: a retrospective analysis among managed care patients with chronic myelogenous leukaemia. Pharmacoeconomics. 2007;25:481–496. doi: 10.2165/00019053-200725060-00004. [DOI] [PubMed] [Google Scholar]
- 14.Streeter SB, Schwartzberg L, Husain N, Johnsrud M. Patient and plan characteristics affecting abandonment of oral oncolytic prescriptions. J Oncol Pract. 2011;7(3 suppl):46s–51s. doi: 10.1200/JOP.2011.000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruddy K, Mayer E, Partridge A. Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin. 2009;59:56–66. doi: 10.3322/caac.20004. [DOI] [PubMed] [Google Scholar]
- 16.Partridge AH, Avorn J, Wang PS, Winer EP. Adherence to therapy with oral antineoplastic agents. J Natl Cancer Inst. 2002;94:652–661. doi: 10.1093/jnci/94.9.652. [DOI] [PubMed] [Google Scholar]
- 17.Zanders MJ, Haak H, van Herk-Sukel MP, van de Poll-Franse L, Johnson J. Impact of cancer on adherence to glucose-lowering drug treatment in individuals with diabetes. Diabetologia. 2015;58:951–960. doi: 10.1007/s00125-015-3497-8. [DOI] [PubMed] [Google Scholar]
- 18.Stuart BC, Davidoff AJ, Erten MZ. Changes in medication management after a diagnosis of cancer among Medicare beneficiaries with diabetes. J Oncol Pract. 2015;11:429–434. doi: 10.1200/JOP.2014.003046. [DOI] [PubMed] [Google Scholar]
- 19.Stavrou EP, Buckley N, Olivier J, Pearson SA. Discontinuation of statin therapy in older people: does a cancer diagnosis make a difference? An observational cohort study using data linkage [serial online] BMJ Open. 2012;2:e000880. doi: 10.1136/bmjopen-2012-000880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zullig LL, Peppercorn JM, Schrag D, et al. Financial distress, use of cost-coping strategies, and adherence to prescription medication among patients with cancer. J Oncol Pract. 2013;9(6 suppl):60s–63s. doi: 10.1200/JOP.2013.000971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neugut AI, Subar M, Wilde ET, et al. Association between prescription co-payment amount and compliance with adjuvant hormonal therapy in women with early stage breast cancer. J Clin Oncol. 2011;29:2534–2542. doi: 10.1200/JCO.2010.33.3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee M, Khan MM. Gender differences in cost-related medication non-adherence among cancer survivors. J Cancer Surviv. 2015;10:384–393. doi: 10.1007/s11764-015-0484-5. [DOI] [PubMed] [Google Scholar]
- 23.Smith JC, Medalia C. US Census Bureau, Current Population Reports, P60–250, Health Insurance Coverage in the United States: 2013. Washington, DC: US Government Printing Office; 2014. [Google Scholar]
- 24.Bechis SK, Carroll PR, Cooperberg MR. Impact of age at diagnosis on prostate cancer treatment and survival. J Clin Oncol. 2011;29:235–241. doi: 10.1200/JCO.2010.30.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith TJ, Penberthy L, Desch CE, et al. Differences in initial treatment patterns and outcomes of lung cancer in the elderly. Lung Cancer. 1995;13:235–252. doi: 10.1016/0169-5002(95)00496-3. [DOI] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics. Survey Description, National Health Interview Survey, 2013. Hyattsville, MD: Division of Health Interview Statistics, National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services; 2014. [Google Scholar]
- 27.Dowling EC, Chawla N, Forsythe LP, et al. Lost productivity and burden of illness in cancer survivors with and without other chronic conditions. Cancer. 2013;119:3393–3401. doi: 10.1002/cncr.28214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–1330. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 29.Kent EE, Forsythe LP, Yabroff KR, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119:3710–3717. doi: 10.1002/cncr.28262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the National Health Interview Survey, 2006–2015. Vital Health Stat 2. 2014;165:1–53. [PubMed] [Google Scholar]
- 31.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 32.Ramsey S, Blough D, Kirchhoff A, et al. Washington state cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 2013;32:1143–1152. doi: 10.1377/hlthaff.2012.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chirikos TN, Russell-Jacobs A, Cantor AB. Indirect economic effects of long-term breast cancer survival. Cancer Pract. 2002;10:248–255. doi: 10.1046/j.1523-5394.2002.105004.x. [DOI] [PubMed] [Google Scholar]
- 34.de Boer AM, Taskila T, Ojajarvi A, van Dijk FH, Verbeek JM. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009;301:753–762. doi: 10.1001/jama.2009.187. [DOI] [PubMed] [Google Scholar]
- 35.Sabatino SA, Coates RJ, Uhler RJ, Alley LG, Pollack LA. Health insurance coverage and cost barriers to needed medical care among U.S. adult cancer survivors age <65 years. Cancer. 2006;106:2466–2475. doi: 10.1002/cncr.21879. [DOI] [PubMed] [Google Scholar]
- 36.Shankaran V, Jolly S, Blough D, Ramsey SD. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. J Clin Oncol. 2012;30:1608–1614. doi: 10.1200/JCO.2011.37.9511. [DOI] [PubMed] [Google Scholar]
- 37.Anvik T, Holtedahl KA, Mikalsen H. “When patients have cancer, they stop seeing me”—the role of the general practitioner in early follow-up of patients with cancer—a qualitative study [serial online] BMC Family Pract. 2006;7:19. doi: 10.1186/1471-2296-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bayliss EA, Bronsert MR, Reifler LM, et al. Statin prescribing patterns in a cohort of cancer patients with poor prognosis. J Palliat Med. 2013;16:412–418. doi: 10.1089/jpm.2012.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCowan C, Wang S, Thompson AM, Makubate B, Petrie DJ. The value of high adherence to tamoxifen in women with breast cancer: a community-based cohort study. Br J Cancer. 2013;109:1172–1180. doi: 10.1038/bjc.2013.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu EQ, Johnson S, Beaulieu N, et al. Healthcare resource utilization and costs associated with non-adherence to imatinib treatment in chronic myeloid leukemia patients. Curr Med Res Opin. 2010;26:61–69. doi: 10.1185/03007990903396469. [DOI] [PubMed] [Google Scholar]
- 41.Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol. 2014;32:306–311. doi: 10.1200/JCO.2013.52.9123. [DOI] [PubMed] [Google Scholar]
- 42.Experts in Chronic Myeloid Leukemia. The price of drugs for chronic myeloid leukemia (CML) is a reflection of the unsustainable prices of cancer drugs: from the perspective of a large group of CML experts. Blood. 2013;121:4439–4442. doi: 10.1182/blood-2013-03-490003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Virgo KS, Bromberek JL, Glaser A, Horgan D, Maher J, Brawley OW. Health care policy and cancer survivorship. Cancer. 2013;119:2187–2199. doi: 10.1002/cncr.28066. [DOI] [PubMed] [Google Scholar]
- 44.Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood) 2011;30:91–99. doi: 10.1377/hlthaff.2009.1087. [DOI] [PubMed] [Google Scholar]
- 45.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 46.Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009;27:3868–3874. doi: 10.1200/JCO.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 47.Irwin B, Kimmick G, Altomare I, et al. Patient experience and attitudes toward addressing the cost of breast cancer care. Oncologist. 2014;19:1135–1140. doi: 10.1634/theoncologist.2014-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bestvina CM, Zullig LL, Rushing C, et al. Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract. 2014;10:162–167. doi: 10.1200/JOP.2014.001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schrag D, Hanger M. Medical oncologists’ views on communicating with patients about chemotherapy costs: a pilot survey. J Clin Oncol. 2007;25:233–237. doi: 10.1200/JCO.2006.09.2437. [DOI] [PubMed] [Google Scholar]
- 50.de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: the COST measure. Cancer. 2014;120:3245–3253. doi: 10.1002/cncr.28814. [DOI] [PubMed] [Google Scholar]
- 51.Schnipper LE, Davidson NE, Wollins DS, et al. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33:2563–2577. doi: 10.1200/JCO.2015.61.6706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu G, Franssen E, Fitch MI, Warner E. Patient preferences for oral versus intravenous palliative chemotherapy. J Clin Oncol. 1997;15:110–115. doi: 10.1200/JCO.1997.15.1.110. [DOI] [PubMed] [Google Scholar]
- 53.Peeters L, Sibille A, Anrys B, et al. Maintenance therapy for advanced non-small-cell lung cancer: a pilot study on patients’ perceptions. J Thorac Oncol. 2012;7:1291–1295. doi: 10.1097/JTO.0b013e31825879ea. [DOI] [PubMed] [Google Scholar]
- 54.Mailankody S, Prasad V. Five years of cancer drug approvals: innovation, efficacy, and costs. JAMA Oncol. 2015;1:539–540. doi: 10.1001/jamaoncol.2015.0373. [DOI] [PubMed] [Google Scholar]
- 55.Brooks GA, Li L, Sharma DB, et al. Regional variation in spending and survival for older adults with advanced cancer. J Natl Cancer Inst. 2013;105:634–642. doi: 10.1093/jnci/djt025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hershman DL, Tsui J, Wright JD, Coromilas EJ, Tsai WY, Neugut AI. Household net worth, racial disparities, and hormonal therapy adherence among women with early stage breast cancer. J Clin Oncol. 2015;33:1053–1059. doi: 10.1200/JCO.2014.58.3062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Klabunde CN, Ambs A, Keating NL, et al. The role of primary care physicians in cancer care. J Gen Intern Med. 2009;24:1029–1036. doi: 10.1007/s11606-009-1058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26:1073–1079. doi: 10.1200/JCO.2007.11.9859. [DOI] [PubMed] [Google Scholar]
- 59.Bush TL, Miller SR, Golden AL, Hale WE. Self-report and medical record report agreement of selected medical conditions in the elderly. Am J Public Health. 1989;79:1554–1556. doi: 10.2105/ajph.79.11.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harlow S, Linet M. Agreement between questionnaire data and medical records: the evidence for accuracy of recall. Am J Epidemiol. 1989;129:233–248. doi: 10.1093/oxfordjournals.aje.a115129. [DOI] [PubMed] [Google Scholar]
- 61.Short PF, Moran JR, Punekar R. Medical expenditures of adult cancer survivors aged <65 years in the United States. Cancer. 2011;117:2791–2800. doi: 10.1002/cncr.25835. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.