Abstract
Objective
To evaluate the safety and acceptability of a novel 8-week intervention integrating exercise, exposure therapy, cognitive restructuring, and a home safety evaluation, conducted by a physical therapist, in reducing fear of falling and activity avoidance. To collect preliminary evidence of efficacy.
Design
Randomized pilot study comparing the intervention to time- and attention-equivalent fall prevention education.
Setting
Participants’ homes.
Participants
42 older adults with disproportionate fear of falling (high fear, low to moderate objective fall risk).
Measurements
Falls Efficacy Scale-International, modified Activity Card Sort, satisfaction, falls.
Results
Relative to education, the intervention reduced fear of falling (d = 1.23) and activity avoidance (d = 1.02) at 8 weeks, but effects eroded over a six-month follow-up period. The intervention did not increase falls, and participants rated the exercise, exposure therapy, and non-specific elements as most helpful.
Conclusion
An integration of exercise and exposure therapy may help older adults with disproportionate fear of falling, but modifications to the intervention or its duration may be needed to maintain participants’ gains.
Keywords: Anxiety, fear of falling, exercise, activity avoidance, exposure therapy, physical therapy
Objective
Falls are a major cause of morbidity and mortality among older adults (1). Fear of falling is increasingly recognized as a related but distinct disabling condition (2). Fear of falling often leads to decreased physical and social activity which can result in deconditioning, depression, and need for assistance in basic and instrumental activities of daily living (e.g., bathing, grocery shopping) (3). Individuals who fear falling may also modify their gait in ways that can, particularly in the context of deconditioning, increase risk of falls (4).
Many older individuals develop fear of falling after a fall or in the context of a health condition that affects lower extremity strength or balance (5). Some older people, however, particularly those with a history of anxiety, may develop fear of falling despite having no history of falls, intact balance, and relatively good health (6). For these individuals, the level of fear and avoidance may exceed the actual level of fall risk. Older adults with disproportionate fear of falling may require a different treatment approach from older adults at high fall risk.
A number of interventions have addressed fear of falling. Most of these have primarily targeted fall prevention, with fear reduction as a secondary outcome (7–9). Exercise is particularly effective at reducing fear as well as fall risk in older adults (7). Interventions are usually conducted in person in the community, although home-based, technology-assisted, and virtual reality interventions have also demonstrated efficacy in reducing both falls and fear (10–12). Although “dismantling” studies are scarce in this area, one investigation suggested that cognitive restructuring plus exercise may reduce fear of falling relative to exercise alone (13).
At least three interventions have been developed to target fear of falling specifically, rather than ancillary to reducing fall risk. The oldest, A Matter of Balance, attempts to increase fall-related self-efficacy with cognitive restructuring techniques taught in a group format by peers or health care professionals (14). Extensive research in the U.S. and Netherlands has established the efficacy, disseminability, and cost-effectiveness of this program, relative to usual care (15–17). Dutch investigators have also adapted A Matter of Balance to create a seven-session (three in-home and four by telephone) nurse-conducted program (18). Results from a randomized trial suggested that this intervention reduced fear of falling, avoidance, and disability relative to usual care.
The Strategies for Increasing Independence, Confidence and Energy (STRIDE) program, in which paraprofessional health care assistants conducted individual CBT with participants, reduced fear of falling relative to usual care in a large U.K. study (19).
Most recently, in the Back on Your Feet program, mental health providers provided in-home psychotherapy using cognitive restructuring and imaginal and in vivo exposure techniques to reduce PTSD symptoms and fear of falling among 14 older adults who had experienced an injurious fall (20).
Although the literature generally supports the use of interventions that integrate CBT components for fear of falling, it is limited in several ways. First, most intervention programs require participants to attend classes in the community. Individuals with the highest levels of fear, who may avoid leaving their homes or yards, are the most likely to drop out or never attend such programs (14). Second, it may be challenging under current reimbursement constraints for U.S. mental health providers to conduct interventions in the home. Third, interventions for fear of falling do not always measure activity participation as an outcome. Fourth, previous studies have included individuals at high fall risk, rather than targeting those with disproportionate fear. Finally, even some of the larger trials have used a no-treatment or usual care control condition, which limits the scientific validity of the results (e.g., 17, 18, 19).
In an effort to test an intervention for fear of falling that addresses these limitations, our team developed Activity, Balance, Learning, and Exposure (ABLE; 21). In ABLE, physical therapists (PTs) recruited from home health care agencies conducted an 8-session, in-home intervention that combined an empirically supported fall prevention exercise program, a home safety evaluation, cognitive restructuring, and exposure to feared situations (e.g., walking across the street, getting into a van, using the bathtub) among older adults with disproportionate levels of fear of falling. In the present study, we tested ABLE against an active control condition, in-home fall prevention education (FPE), in a randomized pilot study in order to determine feasibility and safety and develop a preliminary estimate of efficacy. We examined whether ABLE would reduce fear of falling and avoidance more than FPE, and whether gains would be maintained six months following the end of the intervention. In order to evaluate safety of the intervention, we investigated whether ABLE would increase falls. Finally, we sought feedback in both structured and open-ended formats to improve the intervention for future research.
Methods
Participants
All procedures were approved by the local Institutional Review Board and the trial was registered with the National Institutes of Health clinical trials registry (NCT01609322). Participants were 42 community-dwelling older adults (31 female, 11 male) aged 65 to 91 (M = 77.9, SD = 7.3) with high levels of fear of falling as measured by a Falls Efficacy Scale-International (FES-I) score greater than 27 (22) recruited from senior health fairs, community presentations, and referrals from geriatric care providers. Because this was a pilot study, the sample size was determined based on feasibility of recruitment and ability to carry out the interventions and assessments rather than a power analysis. Exclusion criteria included high objective risk of falls, using an algorithm derived from (23) (either one fall in the past year plus walking speed ≤ 0.58 meters/second or two falls in the past year plus Body Mass Index ≤ 29.2), or risk of injury: > 2 falls in the past year, requiring the assistance of another person to walk or transfer, orthostasis (>20 point decrease in systolic or diastolic blood pressure from sitting to standing), history of osteoporotic fracture, Body Mass Index ≤ 17, cognitive impairment as measured by 10 or more errors on the Blessed Orientation Memory and Concentration Test (24), or legally blind (visual acuity <20/60 in both eyes). Individuals who were ineligible due to high fall risk were referred back to their primary care physician for appropriate services. We also excluded those with a history of schizophrenia or bipolar disorder, alcohol or drug abuse in the past 6 months, active suicidal ideation, or currently receiving physical therapy or psychotherapy. Figure 1 displays the flow chart of participants through the study. Two participants dropped out of ABLE (9.5%) after 4 weeks. A total of 40 participants completed treatment and follow-up.
Figure 1.
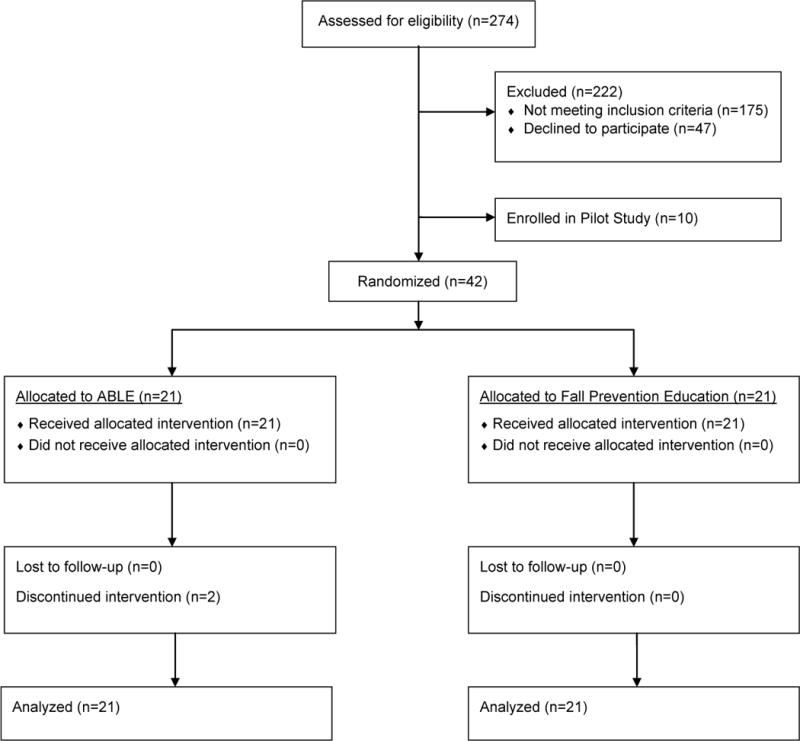
CONSORT diagram.
Design
Participants who met initial eligibility requirements after a phone screen were invited to an in-person screening with a psychologist (JW), physical therapist (KJ), and an orthopedist (DC) to evaluate subjective and objective fall risk based on the Lamb et al., 2008 algorithm and review medical history and medications. Eligible and consenting participants completed an in-home baseline assessment prior to randomization. Randomization was determined using a computer-generated sequence created and held by a colleague with no other connection to the study; the project coordinator obtained the assignment after each participant completed the baseline assessment. Both conditions consisted of 8 weekly in-home sessions lasting approximately 1 hour each. All assessments were completed by research associates blind to the participants’ treatment condition. Telephone assessments were completed at weeks 2 and 6, whereas in-home assessments were conducted at weeks 4 and 8. Post-treatment assessments were conducted in the participants’ homes at 3- and 6-months post-treatment. Additionally, all participants logged any falls on a calendar that was collected weekly during the active phase and mailed monthly during the follow-up phase.
Interventions
Activity, Balance, Learning, and Exposure
The ABLE intervention has been described in detail elsewhere (see 21). Briefly, ABLE is a weekly, 8-session, multi-component in-home therapy that combines an empirically supported fall prevention exercise program, a home safety evaluation, and exposure-based CBT (manual available upon request from the first author). The ABLE intervention was delivered by two home health care agency PTs who received weekly supervision from a PT (KJ) and clinical psychologist (JW). The exercise component is based on the Otago Exercise Programme to Prevent Falls in Older Adults, which combines flexibility, strengthening, and balance exercises delivered by a PT at sessions 1, 2, 4, and 8 (25–28). Participants were additionally instructed to practice the exercises three times a week and walk for up to 30 minutes twice a week. Additionally, participants were taught how to get up off the floor after a fall. The home safety assessment was conducted by a therapist in session 3 based on recommendations for eliminating hazards in the home (29). During this session, the therapist helped participants identify and develop an action plan for addressing hazards in the home (e.g., removing throw rugs, installing grab bars, replacing dim light bulbs with brighter ones). The exposure-based CBT component included psychoeducation about anxiety and the role of avoidance, creation of a fear hierarchy based on identified triggers and avoidance behaviors, exposure practice, cognitive restructuring, and problem-solving. The CBT component was primarily delivered in weeks 5-7, with some elements (e.g., psychoeducation about fear and avoidance, development of a fear hierarchy, relapse prevention) integrated into sessions 2, 4, and 8, respectively. Participants were offered the opportunity to invite caregivers or other support people to attend the sessions. In order to ensure fidelity to the intervention, videotapes of a sample of sessions (at least two per participant) were watched by a PT (KJ) and a psychologist (JW). Feedback was relayed directly to the therapists in weekly supervision calls.
Fall Prevention Education
Fall prevention education (FPE) was based on a guide developed by the Australian Government Department of Health and Ageing, Don’t Fall For It -A Guide to Preventing Falls for Older People (30). The intervention was delivered by one doctoral-level psychologist and three graduate students in clinical psychology who received weekly supervision. Sessions included education about reducing personal and environmental risk factors and reducing injury from falls.
Measures
The primary outcome measures were fear of falling and activity avoidance due to fear. Fear of falling was measured with Falls Efficacy Scale – International (FES-I; 31). The English language version of this 16-item scale asks participants how “concerned” they are, on a 4-point Likert scale, about falling while carrying out various activities (e.g., cleaning the house, taking a bath or shower, walking on an uneven surface). Although the FES-I is conceptualized as a measure of fall-related self-efficacy, the English version uses the word “concern,” which is a term often used by older adults to indicate anxiety (32). Because anxiety and fear are related constructs, and because the FES-I is well validated and frequently used, we chose it as our measure of fear of falling. One participant completed the brief 7-item version of the FES-I (39) at baseline and week 2 so the item mean was imputed for the missing items to estimate the full FES-I score.
Avoidance was conceptualized as the inverse of activity engagement, which was measured with an adaptation of the Activity Card Sort (33). The Activity Card Sort, commonly used by occupational therapists in assessment and development of rehabilitation plans, consists of a set of pictures of older adults engaging in various instrumental, leisure, physical, and social activities (e.g., shopping, gardening). For purposes of this study, we modified the original measure to include additional cards representing common activities that are often avoided due to fear of falling (e.g., taking a bath) and exclude cards representing activities that are not avoided due to fear of falling (e.g., playing cards) or that are less frequently performed regardless of fear of falling (e.g., travel). From these pictures, participants selected five activities that they would most like to do/do more if they were not afraid of falling. We then asked how many times they had engaged in each activity in the past month. We used the sum of the number of times engaged in each of the five activities as a patient-centered measure of activity engagement.
The study physician used patients’ medical history and records to complete the Cumulative Illness Rating Scale for Geriatrics (CIRS-G; 34), which gives a score based on number of organ systems affected by medical conditions. We also administered the Structured Clinical Interview for DSM-IV-TR Patient Edition (35) to diagnose rule-outs (substance abuse, psychosis) and to characterize the sample in terms of anxiety and depressive disorders. Finally, we used the Borkovec and Nau (36) scale to measure credibility and expectations for improvement after the first session and the Patient Satisfaction Questionnaire (37) to assess satisfaction following treatment.
We evaluated the safety of the intervention using a fall log. A fall was defined, per Prevention of Falls Network Europe (ProFaNE) guidelines, as a slip or trip in which a person loses balance and lands on the floor, ground, or lower level (38). Participants were given paper calendars and asked to mark days on which they experienced a fall according to those criteria. During the active intervention period, interventionists collected these data on a weekly basis. Following the intervention, participants used stamped, addressed envelopes to mail the calendars monthly to the research team. A research assistant called participants to follow up on reported falls, and the PI and orthopedist (DC) were informed and made additional contact with the participant or the participant’s primary care provider if clinically indicated.
After ABLE participants finished the study, we provided them with an anonymous survey and a stamped, addressed envelope in order to obtain feedback. We asked them to rate each component of ABLE (e.g., Otago exercises, home safety evaluation) on a 4-point scale from “less helpful” to “most helpful.” We asked about the duration of the program, whether they had made changes to their homes following the home safety evaluation, whether they found it helpful to have a caregiver participate, and whether holding the sessions in a group, or in a community location rather than the home, would have influenced their willingness to participate. We gave them the opportunity to provide open-ended comments and suggestions as well.
Statistics
We compared baseline characteristics of the two groups using chi-square and t-tests. Intention-to-treat analyses were conducted using repeated measures mixed effects models to examine differences between treatment groups on the outcomes of interest over time. All models included the fixed effects of time and treatment group, as well as the treatment group by time interaction. Subject variability was modeled as a random effect. Alpha was set at .05. Significant time by treatment group interactions were further examined using simple effects tests at weeks 2, 4, 6, and 8. Analyses were first conducted for the acute phase (pretreatment, week 2, week 4, week 6, and week 8). To evaluate differences between treatment groups during follow-up, a second set of analyses were conducted that included follow-up at months 3 and 6 (pretreatment, week 8, month 3, month 6). All models included credibility scores and presence or absence of a psychiatric disorder as covariates to control for group differences on these variables. The effect size was calculated using Cohen’s d (40). All analyses were conducted using SAS 9.3. Models were assessed using the MIXED procedure which does not use listwise deletion and thus preserves degrees of freedom in the presence of missing data.
Results
Participant Characteristics
Of the 42 participants, 21 were randomized to receive ABLE and 21 were randomized to receive FPE. Demographic characteristics were not significantly different across the two groups (Table 1). For most participants, fall risk derived from self-reports was higher than fall risk derived from objective measures such as gait speed and lower extremity strength (23), suggesting that these participants were overestimating their risk of falls, as would be expected in a group selected based on disproportionate fear. Mean FES-I scores did not differ significantly between those with objectively low vs. objectively moderate fall risk, 38.9 (6.9) vs. 42.2 (7.2), t(40) = −1.34, p = .19. There were no significant differences between groups at baseline on severity of fear of falling or avoidance; participants assigned to ABLE were more likely to meet criteria for a psychiatric disorder overall or a past or current history of major depression, and participants assigned to FPE were more likely to meet criteria for specific phobia (not related to falling; Table 2). On average, participants reported relatively low levels of medical comorbidity, with mean CIRS-G scores falling approximately 1 standard deviation below norms for community-dwelling older adults.
Table 1.
Participant Characteristics
| FPE (n = 21) |
ABLE (n = 21) |
t | df | p | |
|---|---|---|---|---|---|
| Age in years, M (SD) | 78.5 (7.8) | 77.3 (7.0) | 0.52 | 40 | 0.61 |
| Years of Education, M (SD)a | 15.0 (2.2) | 15.3 (3.4) | −0.28 | 39 | 0.78 |
| Blessed score, M (SD) | 3.0 (3.4) | 2.5 (2.8) | 0.59 | 40 | 0.56 |
| CIRS-G, M (SD) | 10.7 (3.7) | 13.5 (5.5) | −1.95 | 40 | 0.06 |
| χ2 | df | p | |||
| Female, % (n) | 81.0 (17) | 66.7 (14) | 1.11 | 1 | 0.29 |
| Race/Ethnicity, % (n) | 2.23 | 3 | 0.52 | ||
| Asian | 9.5 (2) | 14.3 (3) | |||
| Black/African American | 14.3 (3) | 4.8 (1) | |||
| Hispanic | 4.8 (1) | 14.3 (3) | |||
| NonHispanic White | 71.4 (15) | 66.7 (14) | |||
| Marital Status | 1.69 | 3 | 0.64 | ||
| Married | 33.3 (7) | 23.8 (5) | |||
| Widowed | 38.1 (8) | 33.3 (7) | |||
| Divorced/Separated | 28.6 (6) | 38.1 (8) | |||
| Never Married | 0 (0) | 4.8 (1) | |||
| Work Status | 3.23 | 3 | 0.36 | ||
| Full-time | 4.8 (1) | 0 (0) | |||
| Part-time | 4.8 (1) | 0 (0) | |||
| Retired | 85.7 (18) | 100 (21) | |||
| Leave of absence | 4.8 (1) | 0 (0) | |||
| Living Arrangements | 5.24 | 3 | 0.15 | ||
| Lives with spouse | 33.3 (7) | 28.6 (6) | |||
| Lives with roommate | 14.3 (3) | 9.5 (2) | |||
| Lives alone | 52.4 (11) | 61.9 (13) |
Note. CIRS-G = Cumulative Illness Rating Scale for Geriatrics.
n=20 for ABLE.
Table 2.
Clinical Characteristics
| FPE (n = 21) |
ABLE (n = 21) |
t or χ2 | df | p | |
|---|---|---|---|---|---|
| Falls Efficacy Scale – International, M (SD; range) | 39.0 (6.8; 27-51) | 40.7 (7.3; 29-56) | 0.79 | 40 | 0.44 |
| Activity Card Sort, M (SD; range) | 14.1 (13.2; 0-43) | 14.0 (10.9; 0-36) | −0.03 | 40 | 0.98 |
| Self-rated fall risk, % (n): | 4.03 | 2 | 0.13 | ||
| Low | 14.3 (3) | 4.8 (1) | |||
| Moderate | 85.7 (18) | 81.0 (17) | |||
| High | 0.0 (0) | 14.3 (3) | |||
| Objective fall risk, % (n): | 1.11 | 1 | 0.29 | ||
| Low | 81.0 (17) | 66.7 (14) | |||
| Moderate | 19.1 (4) | 33.3 (7) | |||
| Any psychiatric disorder, % (n) | 52.4 (11) | 85.7 (18) | 5.46 | 1 | 0.02 |
| Current major depression, % (n) | 0.0 (0) | 19.1 (4) | 4.42 | 1 | 0.04 |
| Past major depression, % (n)a | 4.8 (1) | 38.1 (8) | 655 | 1 | 0.01 |
| Specific phobia (not related to falls), % (n) | 42.9 (9) | 14.3 (3) | 430 | 1 | 0.04 |
| Agoraphobia, % (n) | 14.3 (3) | 4.8 (1) | 1.11 | 1 | 0.29 |
| PTSD (not due to fall), % (n) | 0.0 (0) | 9.5 (2) | 2.10 | 1 | 0.15 |
| OCD, % (n) | 4.8 (1) | 0.0 (0) | 1.02 | 1 | 0.31 |
| Social phobia, % (n) | 9.5 (2) | 19.1 (4) | 0.78 | 1 | 0.38 |
| Panic disorder, % (n) | 0.0 (0) | 4.8 (1) | 1.02 | 1 | 0.31 |
| GAD, % (n) | 4.8 (1) | 0.0 (0) | 1.02 | 1 | 0.31 |
| Anxiety disorder NOS, % (n) | 0.0 (0) | 9.5 (2) | 2.10 | 1 | 0.15 |
Note. Bolded values are statistically significant at p < .05. ABLE = Activity, Balance, Learning, and Exposure; FPE = Fall Prevention Education; GAD = Generalized Anxiety Disorder; OCD = Obsessive Compulsive Disorder; PTSD = Posttraumatic Stress Disorder.
n=20 for FPE.
Acceptability, Credibility, Compliance, and Satisfaction
Completion rates were over 90% (19 of 21) for ABLE and 100% for FPE, suggesting that both interventions were acceptable. One ABLE participant dropped out because of increased anxiety and one did not provide a reason. Credibility and satisfaction data were not available from one ABLE participant. ABLE participants found their intervention slightly more credible than did FPE participants, 9.3 (SD=0.9) vs. 8.6 (SD=1.2), t(39) = 1.99, p = 0.05. Satisfaction ratings, however, did not differ significantly between groups (29.9 vs. 27.6, t(37) = −1.83, p = 0.08). On average, ABLE participants completed some at-home assignments on 6.0 weeks and all assignments on 3.7 weeks (out of 7 weeks in which homework was assigned). FPE participants completed some at-home assignments on 6.3 weeks and all assignments on 5.2 weeks.
Outcomes
Fear of Falling
There was a significant group by time interaction for the FES-I, F(4, 37) = 4.28, p = 0.006 (Figure 2). Participants in the ABLE group demonstrated a significant reduction in fear of falling compared to the FPE group. Significant differences between groups arose at week 6, F(1, 37) = 4.84, p = 0.03 (Cohen’s d = −1.20), and week 8, F(1, 37) = 5.57, p = 0.02 (Cohen’s d = −1.23).
Figure 2.
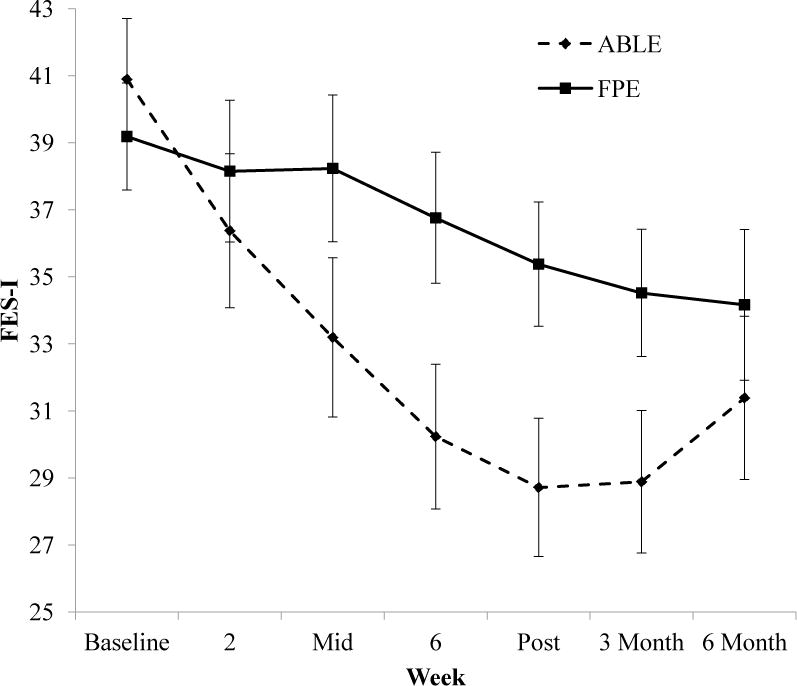
Comparison of an 8-week in-home, physical therapist-delivered exposure therapy based intervention (ABLE) and in-home fall prevention education (FPE) in reducing fear of falling in 42 older adults with disproportionate levels of fear. FES-I = Falls Efficacy Scale-International, scores range from 16 to 64 with higher scores indicating greater fear of falling. Bars represent standard errors.
Evaluation of follow-up effects also revealed a significant group by time interaction, F(3,37) = 4.24, p = 0.01. Simple effects tests at each time point were significant for week 8, F(1, 37) = 5.33, p = 0.03. Differences between groups were not significant at month 3, F(1, 37) = 3.72, p = 0.06, or month 6 follow-up, F(1, 37) = 0.56, p = 0.46.
Activity Avoidance
We found a significant group by time interaction from pre to post on the ACS, F(2, 37) = 4.33, p = 0.02 (Figure 3), demonstrating a significant reduction in avoidance of activities (i.e., increase in ACS score) in the ABLE group compared to the FPE group. Simple effects tests at each time point revealed that significant differences between groups arose at week 4, F(1, 37) = 6.43, p = 0.02 (Cohen’s d = 1.19), and week 8, F(1, 37) = 4.75, p = 0.04 (Cohen’s d = 1.02).
Figure 3.
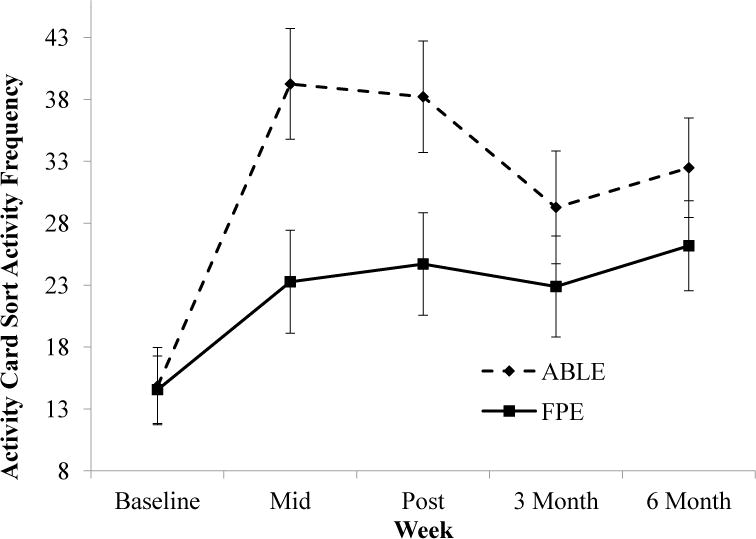
Comparison of an 8-week in-home, physical therapist-delivered exposure therapy based intervention (ABLE) and in-home fall prevention education (FPE) in reducing avoidance in 42 older adults with disproportionate levels of fear. Higher scores on the Activity Card Sort indicate greater frequency of engaging in the activity during the past month. Bars represent standard errors.
Evaluation of follow-up effects revealed only a significant effect of time, F(3, 37) = 12.33, p < 0.001. The group by time interaction did not remain significant through the follow-up phase, F(3, 37) = 1.59, p = 0.21.
Falls
In the year prior to enrollment, there were no differences between the groups in proportion of participants reporting none, one, or two falls (Table 3). Similarly, no differences in fall rates between ABLE and FPE were observed during the intervention or in the six months following the intervention. None of the falls resulted in serious injury.
Table 3.
Falls
| FPE (n=21) |
ABLE (n=21) |
χ2 | df | p | |
|---|---|---|---|---|---|
| Prior year: | 3.31 | 2 | 0.19 | ||
| Zero | 42.9% (9) | 28.6% (6) | |||
| One | 52.4% (11) | 57.6% (10) | |||
| Two | 4.8% (1) | 23.8% (5) | |||
| During intervention: | 0.36 | 2 | 0.83 | ||
| Zero | 85.7% (18) | 81.0% (17) | |||
| One | 4.8% (1) | 9.5% (2) | |||
| Two | 9.5% (2) | 9.5% (2) | |||
| 6 month follow-up:a | 5.01 | 4 | 0.29 | ||
| Zero | 81.0% (17) | 52.6% (10) | |||
| One | 9.5% (2) | 26.3% (5) | |||
| Two | 9.5% (2) | 10.5% (2) | |||
| Three or Four | 0.0% (0) | 10.5% (2) |
Note. ABLE = Activities, Balance, Learning, and Exposure; FPE = Fall Prevention Education.
n=19 for ABLE.
ABLE Evaluations
Seventeen of the 19 participants who completed the ABLE intervention returned an anonymous evaluation of the program. Participants rated the Otago exercises and exposure practice, as well as a supportive relationship with the interventionist (“talking to someone”), as the most helpful components of the program (Table 4). The physician office visit (during which medications were reviewed), home safety evaluation, and cognitive restructuring were less often identified as the most helpful components. The majority of participants felt that the number of sessions and exercises were about right (76.5% and 94.1%, respectively). Twelve participants (70.6%) made at least one change to their homes after the home evaluation (typically removing a floor rug or installing a grab bar). Of those who had a friend, family, or caregiver attend sessions (n = 7), 85.7% found it very helpful. The majority of participants reported that they would have been less likely to participate if sessions were held in a gym or a group rather than in home, one-on-one (Table 4).
Table 4.
Evaluations of ABLE (n = 17)
| How helpful were the different parts of the program?, % (n) | Less Helpful | Helpful | Very Helpful | Most Helpful |
|---|---|---|---|---|
| 1. Doctor office visit | 0 (0) | 41.1 (7) | 47.1 (8) | 11.8 (2) |
| 2. Exercises | 0 (0) | 17.6 (3) | 29.4 (5) | 52.9 (9) |
| 3. Walking | 0 (0) | 5.9 (1) | 64.7 (11) | 29.4 (5) |
| 4. Home safety evaluation | 5.9 (1) | 35.3 (6) | 29.4 (5) | 29.4 (5) |
| 5. Learning about concerns and avoidance | 0 (0) | 23.5 (4) | 52.9 (9) | 23.5 (4) |
| 6. Exposure practice | 0 (0) | 5.9 (1) | 47.1 (8) | 47.1 (8) |
| 7. Learning about unhelpful/helpful thoughts | 0 (0) | 29.4 (5) | 52.9 (9) | 17.6 (3) |
| 8. Talking to someone | 0 (0) | 17.6 (3) | 41.1 (7) | 41.1 (7) |
| How willing to participate would you have been if …, % (n) | Much less | A little less | No difference | |
| Half of the sessions were held in a physical therapy gym? | 70.6 (12) | 23.5 (4) | 5.9 (1) | |
| Exercise sessions were held in a group? | 47.1 (8) | 47.1 (8) | 5.9 (1) |
Conclusions
Relative to an in-home fall prevention education program, the ABLE intervention integrating cognitive-behavioral therapy and exercise reduced fear of falling and avoidance in older adults with disproportionate fear of falling over the 8-week intervention period. There were no differences between the groups in fall rates during or in the six months after the intervention, suggesting that despite increasing activity, ABLE did not increase fall risk. ABLE’s effects on fear and avoidance tended to erode over a six-month follow-up period.
Results from this study compare favorably to four other CBT-based interventions for fear of falling (14, 17–19), all of which used the FES-I. Participants in these investigations had mean baseline FES-I scores ranging from approximately 29 to 42, and effect sizes (d) ranged from 0.16 to 0.43. The mean baseline FES-I in the present study was comparable at 39.9, but the effect size at 8 weeks was substantially larger at 1.23. The effect size of exercise on fear of falling as measured by the FES-I was estimated in a meta-analysis at 0.56 (7).
Sixty-nine percent of participants met criteria for a psychiatric disorder unrelated to falling; of these, most had a pre-existing anxiety disorder. This suggests that disproportionate fear of falling may, in some older adults, be more a manifestation of high pre-existing anxiety levels than a rational response to changes in fall risk due to aging. This further implies that treatment strategies such as exposure therapy may be more effective than other strategies that reduce fall risk without addressing underlying anxiety.
Participants assigned to ABLE were more likely to have a mental health condition, particularly past or current depression, whereas FPE participants had higher rates of current phobia. Although we attempted to control for these differences statistically, it is possible that behavioral interventions may be more potent among psychiatrically ill individuals, and that an intervention that does not include anxiety reduction techniques is particularly ineffective in a group with high levels of anxiety disorders. Both of these factors may have biased our findings in favor of the ABLE intervention.
It is also possible that our frequent assessment of fear of falling may have biased the results, as individuals receiving FPE may have become aware that their intervention was not targeting fear directly. It is not uncommon for intervention studies to include frequent assessments of a primary outcome variable, both to increase sensitivity to change and to minimize analytic problems associated with attrition. These advantages, however, may be outweighed by other factors in studies comparing two very different interventions.
It should be noted that despite the efficacy of the intervention in reducing fear of falling relative to FPE, participants on average still reported high levels of fear following ABLE, and gains associated with ABLE tended to erode over time. This suggests that more work is needed to amplify and extend the effects of the intervention in order to further reduce fear and prevent relapse. For example, it may be that in a relatively healthy older population at low fall risk, less emphasis should be devoted to fall prevention elements such as exercise and home safety and more to the fear reduction elements of exposure and cognitive restructuring. It should further be noted that the group receiving fall prevention education also tended to improve; it is likely that participants in both groups did better than they would have in usual care.
For this investigation, we deliberately recruited people whose fear exceeded their functional disability, as befits a model of disproportionate fear of falling as an anxiety disorder. Many older adults with high levels of fear are more disabled than those enrolled in this study, so the ABLE intervention may not benefit them to the same degree. However, intervening with individuals who have not yet reached a severe level of disability may serve an important preventive function, as well as improve activity levels in older adults with disproportionate fear of falling.
Strengths of this study include the employment of a novel mental health delivery model, using home care physical therapists to integrate elements of behavioral and cognitive therapy into their work. To our knowledge, this is the first study to involve PTs in this manner, despite the fact that they are accustomed to motivating patients to make difficult behavioral changes. One limitation is the relatively brief follow-up period. Furthermore, although we made an effort to develop an intervention that could be implemented with home care PTs as part of their routine practice, it is a relatively intensive treatment. Finally, the sample was predominantly female, although this is consistent with samples of anxious older adults, and Caucasian. Additional research should recruit a larger and more representative sample, in order to ensure generalizability to the population of older adults with disproportionate fear of falling.
Highlights.
An 8-week intervention integrating cognitive-behavioral therapy and exercise reduced fear of falling and avoidance in older adults with disproportionate fear of falling relative to in-home fall prevention education.
The intervention did not increase fall risk.
Effects on fear and avoidance tended to erode over a six-month follow-up period.
Acknowledgments
The authors thank Caroline Merz, Khanh Ly, Judith Condie, Leigh Malone White, Kimberly Bell, Jason Doctor, Joshua Klapow, M. Claire Robertson, and A. John Campbell for their helpful contributions.
Source of Funding: The project was supported by NIMH R34 MH086668.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: No disclosures to report.
Clinicaltrials.gov identifier: NCT01609322
References
- 1.Finlayson ML, Peterson EW. Falls, aging, and disability. Phys Med Rehabil Clin N Am. 2010;21:357–73. doi: 10.1016/j.pmr.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Gazibara T, Kurtagic I, Kisic-Tepavcevic D, et al. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics. 2017;17:215–23. doi: 10.1111/psyg.12217. [DOI] [PubMed] [Google Scholar]
- 3.Auais M, Alvarado BE, Curcio CL, et al. Fear of falling as a risk factor of mobility disability in older people at five diverse sites of the IMIAS study. Arch Gerontol Geriatr. 2016;66:147–53. doi: 10.1016/j.archger.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Ayoubi F, Launay CP, Annweiler C, et al. Fear of falling and gait variability in older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16:14–9. doi: 10.1016/j.jamda.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 5.Denkinger MD, Lukas A, Nikolaus T, et al. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 2015;23:72–86. doi: 10.1016/j.jagp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Painter JA, Allison L, Dhingra P, et al. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. Am J Occup Ther. 2012;66:169–76. doi: 10.5014/ajot.2012.002535. [DOI] [PubMed] [Google Scholar]
- 7.Kumar A, Delbaere K, Zijlstra GA, et al. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing. 2016;45:345–52. doi: 10.1093/ageing/afw036. [DOI] [PubMed] [Google Scholar]
- 8.Logghe IH, Verhagen AP, Rademaker AC, et al. The effects of Tai Chi on fall prevention, fear of falling and balance in older people: a meta-analysis. Prev Med. 2010;51:222–7. doi: 10.1016/j.ypmed.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kapan A, Luger E, Haider S, et al. Fear of falling reduced by a lay led home-based program in frail community-dwelling older adults: A randomised controlled trial. Arch Gerontol Geriatr. 2017;68:25–32. doi: 10.1016/j.archger.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Kwok BC, Pua YH. Effects of WiiActive exercises on fear of falling and functional outcomes in community-dwelling older adults: a randomised control trial. Age Ageing. 2016;45:621–7. doi: 10.1093/ageing/afw108. [DOI] [PubMed] [Google Scholar]
- 12.Levy F, Leboucher P, Rautureau G, et al. Fear of falling: efficacy of virtual reality associated with serious games in elderly people. Neuropsychiatr Dis Treat. 2016;12:877–81. doi: 10.2147/NDT.S97809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang TT, Chung ML, Chen FR, et al. Evaluation of a combined cognitive-behavioural and exercise intervention to manage fear of falling among elderly residents in nursing homes. Aging Ment Health. 2016;20:2–12. doi: 10.1080/13607863.2015.1020411. [DOI] [PubMed] [Google Scholar]
- 14.Tennstedt S, Howland J, Lachman M, et al. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci. 1998;53:P384–92. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]
- 15.Ullmann G, Williams HG, Plass CF. Dissemination of an evidence-based program to reduce fear of falling, South Carolina, 2006-2009. Prev Chronic Dis. 2012;9:E103. doi: 10.5888/pcd9.110093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Haastregt JC, Zijlstra GA, Hendriks MR, et al. Cost-effectiveness of an intervention to reduce fear of falling. Int J Technol Assess Health Care. 2013;29:219–26. doi: 10.1017/S0266462313000275. [DOI] [PubMed] [Google Scholar]
- 17.Zijlstra GA, van Haastregt JC, Ambergen T, et al. Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57:2020–8. doi: 10.1111/j.1532-5415.2009.02489.x. [DOI] [PubMed] [Google Scholar]
- 18.Dorresteijn TA, Zijlstra GA, Ambergen AW, et al. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: results of a randomized controlled trial. BMC Geriatr. 2016;16:2. doi: 10.1186/s12877-015-0177-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parry SW, Bamford C, Deary V, et al. Cognitive-behavioural therapy-based intervention to reduce fear of falling in older people: therapy development and randomised controlled trial - the Strategies for Increasing Independence, Confidence and Energy (STRIDE) study. Health Technol Assess. 2016;20:1–206. doi: 10.3310/hta20560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jayasinghe N, Sparks MA, Kato K, et al. Exposure-Based CBT for Older Adults After Fall Injury: Description of a Manualized, Time-Limited Intervention for Anxiety. Cogn Behav Pract. 2014;21:432–45. doi: 10.1016/j.cbpra.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wetherell JL, Johnson K, Chang D, et al. Activity, balance, learning, and exposure (ABLE): a new intervention for fear of falling. Int J Geriatr Psychiatry. 2016;31:791–8. doi: 10.1002/gps.4393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delbaere K, Close JC, Mikolaizak AS, et al. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing. 2010;39:210–6. doi: 10.1093/ageing/afp225. [DOI] [PubMed] [Google Scholar]
- 23.Lamb SE, McCabe C, Becker C, et al. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: The Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 2008;63A:1082–8. doi: 10.1093/gerona/63.10.1082. [DOI] [PubMed] [Google Scholar]
- 24.Katzman R, Brown T, Fuld P, et al. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry. 1983;140:734–9. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 25.Robertson MC, Devlin N, Gardner MM, et al. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ. 2001;322:697–701. doi: 10.1136/bmj.322.7288.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robertson MC, Gardner MM, Devlin N, et al. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ. 2001;322:701–4. doi: 10.1136/bmj.322.7288.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–9. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campbell AJ, Robertson MC, Gardner MM, et al. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28:513–8. doi: 10.1093/ageing/28.6.513. [DOI] [PubMed] [Google Scholar]
- 29.NSW Department of Health. Stay on your feet: Your home safety checklist. New South Whales Department of Health Web site. 2004 Available at: http://www.drsref.com.au/epc/ha/030295_stay_on_feet.pdf.
- 30.National Ageing Research Institute (Australia), Australia Department of Health and Ageing. Stay on Your Feet – Aelaide West: Don’t fall for it: A guide to preventing falls for older people. Canberra: Department of Health and Ageing; 2004. [Google Scholar]
- 31.Yardley L, Beyer N, Hauer K, et al. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age Ageing. 2005;34:614–9. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 32.Wuthrich VM, Johnco CJ, Wetherell JL. Differences in anxiety and depression symptoms: comparison between older and younger clinical samples. Int Psychogeriatr. 2015;27:1523–32. doi: 10.1017/S1041610215000526. [DOI] [PubMed] [Google Scholar]
- 33.Baum CM. The contribution of occupation to function in persons with Alzheimer’s disease. J Occup Sci. 1995;2:59–67. [Google Scholar]
- 34.Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–48. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- 35.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York State Psychiatric Institute; New York: 2007. (Biometrics Research). [Google Scholar]
- 36.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3:257–60. [Google Scholar]
- 37.Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann. 1982;5:233–7. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- 38.Hauer K, Lamb SE, Jorstad EC, et al. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35:5–10. doi: 10.1093/ageing/afi218. [DOI] [PubMed] [Google Scholar]
- 39.Kempen GIJM, Yardley L, Van Haastregt JCM, et al. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008;37:45–50. doi: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- 40.Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]


