Abstract
Certain cytokines modulate the expression of insulin-like growth factor- (IGF-) I. Since IL-4 and IGF-I promote growth of the protozoan Leishmania major, we here addressed their interaction in downregulating the expression of Igf-I mRNA using small interfering RNA (siRNA) in Leishmania major-infected macrophages. Parasitism was decreased in the siRNA-treated cells compared with the nontreated cells, reversed by the addition of recombinant IGF-I (rIGF-I). In IL-4-stimulated macrophages, parasitism and the Igf-I mRNA amount were increased, and the effects were nullified upon siRNA transfection. IGF-I downregulation inhibited both parasite and macrophage arginase activation even in IL-4-stimulated cells. Searching for intracellular signaling components shared by IL-4 and IGF-I, upon siRNA transfection, phosphorylated p44, p38, and Akt proteins were decreased, affecting the phosphatidylinositol-3-kinase (PI3K)/Akt pathway. In L. major-infected C57BL6-resistant mice, the preincubation of the parasite with rIGF-I changed the infection profile to be similar to that of susceptible mice. We conclude that IGF-I constitutes an effector element of IL-4 involving the PI3K/Akt pathway during L. major infection.
1. Introduction
Certain physiological processes are reciprocally controlled by the immune and endocrine systems, where the actions of cytokines and hormones efficiently regulate these processes [1–3]. In this context, the observation that certain cytokines modulate the expression of the hormone insulin-like growth factor- (IGF-) I [4–6] led us to explore this cross talk in the interaction of the Leishmania parasite with host cells since the essential roles of different cytokines and the effect of IGF-I on the development of Leishmania infection are known [7].
Leishmania is an obligatory intracellular protozoan that is transmitted vectorially and causes diseases called leishmaniases that affect two million people globally each year. These infections result in lesions on the skin, mucosa, or viscera, depending on the parasite species and the host response and features [8].
Leishmania infection leads to specific activation of the host cellular immune response, in which macrophages that harbor the parasite play a fundamental role in infection progression. Cytokines and growth factors, including IGF-I, act on macrophage leishmanicidal or parasite growth-promoting mechanisms. The metabolic products of L-arginine exert primary roles in these processes. Nitric oxide (NO), a main leishmanicidal element, is generated through the oxidation of L-arginine catalyzed by the inducible nitric oxide synthase (NOS2). In contrast, polyamines are essential nutrients for the growth of Leishmania, which are generated through the hydrolysis of L-arginine by arginase [9–11].
We began studying the role of IGF-I in Leishmania infection based on the observation that IGF-I is produced by different cell types, including macrophages, and is present in the skin, which is the tissue where the parasite initiates infection [12]. The addition of extrinsic recombinant IGF-I to cultures at a physiological concentration induces the proliferation of various species of Leishmania promastigotes and axenic amastigotes [13–15], promotes an increase in macrophage arginase-1 (ARG1) expression as well as in Leishmania arginase (Larg), in vitro [16, 17], and induces a significant increase in the lesion size and the number of viable parasites at the lesion site in experimental models [18]. Furthermore, macrophages contain endogenous IGF-I in the cytoplasm, which interacts with intracellular Leishmania parasites [19].
The initial data on the adaptive immune response in different mouse strains infected with L. major have shown that the susceptibility or resistance to this infection is related to the production of certain cytokines of the Th1 or Th2 profile, respectively, IFN-γ, or IL-4 and IL-13 [20–24]. Nevertheless, studies have indicated changes in the simplicity of this model with time. The production of IL-4 in resistant mice does not alter the evolution towards progressive disease, as expected. C3H mice that were treated with IL-4 or anti-IL-12 early in the infection developed a strong but transient increase in IL-4 level, with no change in their resistant phenotype [25–27]. Furthermore, the transfer of BALB/c cells with the high expression of IL-4 to genetically resistant chimeric mice on a C57BL/6 background did not result in susceptibility [28]. The findings from these studies thus suggest that the profiles of resistance and susceptibility are not exclusively due to Th1 and Th2 cytokines. Considering our previous results revealing an important role for IGF-I in the development of Leishmania infections and considering the differences in IGF-I expression in different strains of mice [29], IGF-I may emerge as a factor that could explain these differences. Furthermore, IFN-γ stimulation decreases IGF-I levels, whereas IL-4 and IL-13 stimulation increase IGF-I expression [4–6].
In the present work, we evaluated the role of intrinsic IGF-I in L. major-infected macrophages in vitro and its participation in modulating the effects of cytokines by silencing the expression of the Igf-I mRNA using a small interfering RNA. We studied the effects on parasitism and the L-arginine pathway upon cytokine stimulation. We next evaluated the effect on lesion development upon the injection of L. major promastigotes preincubated with recombinant IGF-I (rIGF-I) into the footpads of BALB/c and C57BL/6 mice, which differ in basal Igf-I mRNA amount.
Focusing on immune-endocrine cross talk, we are the first to observe a process in which a growth factor (i.e., IGF-I) acts as an effector element for the cytokine IL-4 in the induction of susceptibility to L. major infection since the expected parasite growth upon IL-4 stimulation was halted by silencing the IGF-I mRNA. The mechanism was directly related to the expression and activation of arginase and by the activation of the phosphatidylinositol-3-kinase (PI3K)/Akt pathway in macrophages. Furthermore, the injection of L. major promastigotes preincubated with rIGF-I into resistant C57BL/6 mice rendered the animals susceptible to the infection. The data thus suggest an essential role for IGF-I in the effect of IL-4 on the alternative macrophage activation pathway during L. major infection.
2. Materials and Methods
2.1. Mice
Six- to 8-week-old inbred BALB/c and C57BL/6 mice were obtained from the Animal Facility of the Faculdade de Medicina, Universidade de São Paulo (USP), and maintained in the animal facility of the Instituto de Medicina Tropical de São Paulo, USP.
2.2. Parasites
L. major LV39 (MRHO/Su/59/P) was maintained through regular passaging in BALB/c mice, and promastigotes were derived from amastigotes purified from the footpad lesions of BALB/c mice and expanded and maintained in 199 medium (Cultilab, Brazil) supplemented with 10% heat-inactivated fetal calf serum (FCS) (Cultilab, Brazil) at 26°C. The promastigotes used in the experiments were in the stationary phase of growth and had undergone no more than four passages in culture. All procedures were approved by the institutional guidelines for animal care and use and by the ethics committee of the institution.
2.3. Evaluation of the Effect of IGF-I on Promastigotes in Culture
L. major promastigote cultures (5 × 105/mL) were established in 24-well plates (Corning Costar, USA) in 199 medium (Cultilab, Brazil) supplemented with 2% heat-inactivated fetal calf serum (FCS) (Cultilab, Brazil) at 26°C, and parasites were stimulated with or without 50 ng/mL IGF-I (R&D Systems, USA). Parasites were counted daily under a light microscope (Carl Zeiss, Gottingen, Germany), and the result was expressed as the number of parasites × 107/mL followed for 10 days of culture.
2.4. Infection of Macrophages with L. major
The RAW 264.7 macrophage cell line (ATCC) and BALB/c and C57BL/6 peritoneal macrophages were grown in Dulbecco's modified Eagle's medium (DMEM) supplemented with 0.5% bovine serum albumin (BSA, insulin-free, Sigma, USA). Cells (5 × 105 or 2 × 106) were dispensed onto round 13 mm2 glass cover slips, which were placed in the wells of 24-well plates (Corning Costar, USA) and incubated for 30 minutes at 37°C in a humid atmosphere with 5% CO2 to allow adhesion. Thereafter, the wells were washed twice with culture medium to remove nonadherent cells. Then, the amastigote or promastigote suspensions (eight parasites per cell) were dispensed into the wells, and infection was allowed to occur for 4 hours at 33°C in a humid atmosphere with 5% CO2. After incubation, the noninternalized parasites were washed away. In one set of experiments, macrophages were treated with the Th1 cytokine IFN-γ (200 U/mL) or the Th2 cytokines IL-4 (2 ng/mL) and IL-13 (5 ng/mL), both separately and in combination. In other experiments, recombinant IGF-I (50 ng/mL; rIGF-I, R&D Systems, Minneapolis, MN, USA) was added. The culture was then maintained for 48 hours at 37°C in a humid atmosphere with 5% CO2.
2.5. Parasite Load in Macrophages
Cover slips were removed from the plates, and the slides were stained with Giemsa dyes, mounted, and processed to evaluate parasitism under a light microscope (Carl Zeiss, Germany). 600 cells per group were counted. The data are presented as the number of parasites per 100 cells [(number of parasites/number of infected cells) × (number of infected cells/total number of cells) × 100]. The analysis was performed by two independent observers who were blinded to the experimental conditions.
2.6. NO Production
Nitrite (NO2) accumulation in the cell culture supernatants was used as an indicator of NO production and was determined using the Griess reaction [30]. Fifty microliters of the culture supernatant was reacted with 50 μL of Griess reagent (1% sulfanilamide, 0.1% N-(1-naphthyl)ethylenediamine dihydrochloride, and 2.5% phosphoric acid in bidistilled water) for 10 min at room temperature. The absorbance was measured at 540 nm using a Multiskan MCC/340 P version 2.20 plate reader (Labsystems), and the nitrite concentration was calculated using a standard curve for sodium nitrite (NaNO2). The tests were run in triplicate.
2.7. Arginase Activity
Cells and infected cells were removed from the culture, lysed, and used to determine arginase activity [31]. Briefly, 50 μL of lysates was treated with the same volume of 10 mM MnCl2 and 50 mM Tris-HCl, pH of 7.4 at 56°C for 10 min to activate arginase. Then, 25 μL of 0.5 M L-arginine at a pH of 9.7 was added to 25 μL of the activated lysate and incubated at 37°C for 60 min. The reaction was stopped with 400 μL of H2SO4/H3PO4/H2O (1/3/7, v/v/v). The urea concentration was measured at 540 nm using a spectrophotometer Multiskan MCC/340 P version 2.20 plate reader (Labsystems, Vantaa, Finland) after the addition of 25 μL of 9% α-isonitrosopropiophenone in 100% methanol and incubation 100°C for 45 min. One unit of enzyme activity is defined as the amount of enzyme that catalyzes the formation of 1 μmol of urea per minute.
2.8. RNA Extraction and Reverse Transcription
Total RNA was extracted from 2 × 106 cells using TRIzol (Invitrogen, USA), according to the manufacturer's protocol. RNA integrity was verified by agarose gel electrophoresis/ethidium bromide staining and spectrophotometry (OD260/280 absorption ratio greater than 1.8). Total RNA (1 μg) was reverse transcribed using the High Capacity cDNA Reverse Transcription kit (Applied Biosystems, USA) following the manufacturer's protocol and then stored at −20°C.
2.9. Quantitative qPCR
For real-time quantitative qPCR, we used the corresponding primer pairs for mouse sequences (Igf-I: 5′ TAC TTC AAC AAG CCC ACA GG 3′ and 5′ AGT CTT GGG CAT GTC AGT GT 3′; Arg1: 5′ AGC ACT GAG GAA AGC TGG TC 3′ and 5′ CAG ACC GTG GGT TCT TCA CA 3′; Larg: 5′ CAA CAC CAT GTC TGG TAC GGT CTC 3′ and 5′ CAC AGC ACG TAG ACC AAT GTA GGC 3′; Nos2: 5′ AGA GCC ACA GTC CTC TTT GC 3′ and 5′ GCT CCT CTT CCA AGG TGC TT 3′; Cat-2b: 5′ TAT GTT GTC TCG GCA GGC TC 3′ and 5′GAA AAG CAA CCC ATC CTC CG 3′; β-actin: 5′ GCC TTC CTT CTT GGG TAT GGA ATC 3′ and 5′ ACG GAT GTC AAC GTC ACA CTT CAT 3′; and GAPDH: 5′ AAC GAG AAG TTC GGC ATA GTC GAG 3′ and 5′ ACT ATC CAC CGT CTT CTG CTT TGC 3′). Reactions including master mix (SYBR® Green; Applied Biosystems, USA), 0.3 μM of each primer, and 1 μg of cDNA templates were run in triplicate on a PCR system (StepOne; Applied Biosystems, USA). The PCR conditions were the same for all primer combinations: 95°C for 10 min and 40 cycles of 92°C for 2 min, 57.5°C for 30 s, and 70°C for 30 s. After amplification, a melting curve was used to confirm the specificity of the target product. The relative expression data were quantified using the 2−ΔΔCt method [32].
2.10. siRNA
Small interfering RNAs (siRNAs) targeting murine IGF-I were designed using GenBank (NM_010512) and IDT SciTools RNAi Design (Integrated DNA Technologies) (sense 5′ AAA GGA GAA GGA AAG GAA GUA CAT T 3′ and antisense 5′AAU GUA CUU CCU UUC CUU CUC CUU U 3′). Universal scrambled siRNAs were employed as controls (Invitrogen, USA). Macrophages were grown in DMEM supplemented with 0.5% bovine serum albumin (insulin-free BSA, Sigma, USA) in a 24-well plate and were transiently transfected with a 150 μM siRNA duplexes using Lipofectamine™ 2000, according to the manufacturer's instructions (Invitrogen, Carlsbad, CA, USA). Cells transfected with IGF-I siRNA were used after 48 h. The transfection efficiency was confirmed by real-time PCR and confocal microscopy. The inhibition percentage (% KD) for the IGF-I mRNA was calculated using the formula% KD = ([1 − 2−ΔΔCt] × 100) [32].
2.11. Confocal Microscopy
For immunofluorescence staining, cells infected with L. major promastigotes were grown on glass slides. Twenty-four hours after infection, cells were fixed with 4% paraformaldehyde, washed with 0.001 M phosphate-buffered saline (PBS; pH 7.2), blocked for one hour with 2% BSA/PBS, and then incubated overnight with a monoclonal goat anti-mouse IGF-I antibody (1 : 75, R&D Systems, USA) and a polyclonal mouse anti-Leishmania antibody (1 : 400) produced in our laboratory. Alex Fluor 546-conjugated donkey anti-goat IgG (1 : 200, Invitrogen, USA) and Alexa Fluor 488-conjugated donkey anti-mouse IgG (1 : 400, Invitrogen, USA) were used as secondary antibodies. Fluorescence imaging analyses were performed using a Zeiss LSM 510 Meta laser-scanning confocal microscope. As a negative control, the primary antibodies were omitted from the reaction.
2.12. SDS-PAGE and Western Blot
Cell lysates (20 μg of protein in 20 μL) were separated on a denaturing gradient 4–12% Bis-Tris NuPAGE gel (Invitrogen, USA) according to the manufacturer's instructions. Briefly, the separated proteins were blotted onto iBlot™ 2 Transfer Stack PVDF mini-membranes using an iBlot Dry Blotting System (Invitrogen, USA). Membranes were blocked with TBS-T buffer (150 mM NaCl, 20 mM Tris, 0.01% Tween 20, pH of 7.4) containing 5% fat-free milk for 1 h. Membranes were reacted with a 1 : 2000 dilution of a primary anti-phospho-Akt (Ser473) antibody, a 1 : 2000 dilution of a rabbit anti-p44/42 MAPK (137F5) mAb, and a 1 : 2000 dilution of a rabbit anti-p38 MAPK (D13E1) XP® mAb (Cell Signaling Technology, USA) overnight at 4°C and incubated with 1 : 1000 dilutions of a peroxidase-conjugated polyclonal anti-rabbit IgG and HRP-conjugated anti-biotin antibody (Cell Signaling Technology, USA) for 1 h at room temperature. Biotinylated protein molecular weight markers (Cell Signaling Technology, USA) were used. Bound antibodies were detected with an ECL chemiluminescence kit LumiGLO® Reagent (Cell Signaling Technology, USA) according to the manufacturer's instructions. An evaluation of the phosphorylation kinetics was conducted at different time points (0, 5, 10, 20, 30, and 60 minutes) after adding the stimulus (data not shown), and we chose the time of 30 minutes to present the results. Subsequently, protein bands were quantified by densitometry using AlphaEaseFC™ software 3.2 beta version (Alpha Innotech Corporation, San Leandro, CA, USA), and the results are expressed in arbitrary units, which were calculated by integrating the intensity of each pixel over the spot area and normalizing to the gel background.
2.13. Development of Footpad Lesions in Mice
Stationary-phase promastigotes (1 × 106) that had been preincubated with or without 50 ng/mL of recombinant human IGF-I (R&D Systems, USA) for 5 min and then washed were injected into the footpads of BALB/c and C57BL/6 mice. In the opposite footpad, we injected RPMI 1640 medium as a control. For six weeks, we measured the thickness of the foot to indicate the growth of the lesions using a micrometer (Mitsutoyo, Japan), and the difference between the infected and noninfected footpads in millimeters was considered the lesion size.
2.14. Statistical Analysis
Statistical analyses were performed with GraphPad Prism 5 software (GraphPad Software Inc., San Diego, CA, USA). Data were subjected to analysis of variance (ANOVA) and Tukey's posttest and were considered significant when P < 0.05.
3. Results
3.1. The Effect of IGF-I on L. major in Culture and within Macrophages
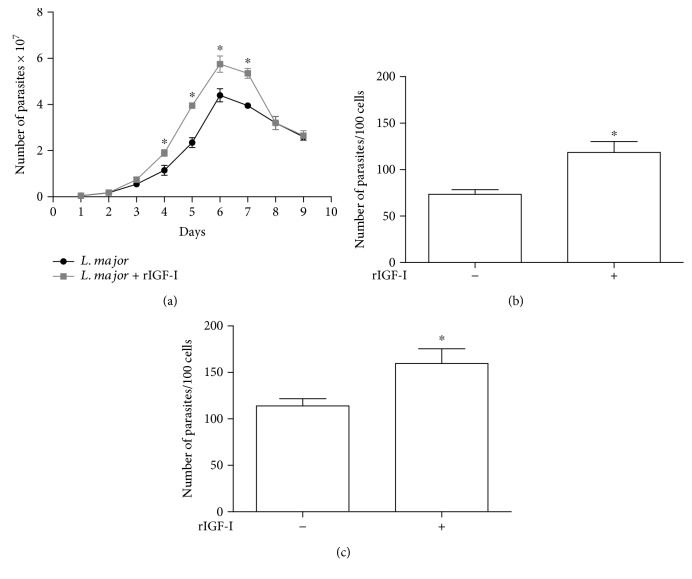
We first verified the effect of IGF-I on parasite growth in vitro. In the cultures stimulated with rIGF-I, we observed a larger number of parasites that reached the stationary phase earlier than nonstimulated cultures (Figure 1(a)).
Figure 1.
The effects of IGF-I on the growth of L. major in culture and within macrophages (mean ± standard deviation). (a) The effect of IGF-I on the growth of Leishmania promastigotes in culture maintained in 199 medium supplemented with 2% heat-inactivated FCS at 26°C is shown. Leishmania promastigotes were maintained with (gray line) or without (black line) 50 ng/mL rIGF-I. (b and c) The effect of IGF-I on the growth of Leishmania within macrophages is shown. RAW 264.7 cells were infected with L. major promastigotes (b) or amastigotes (c) treated with or without 50 ng/mL rIGF-I and incubated for 48 h. ∗P < 0.05 (one-way ANOVA and Student's t test) compared to the control without rIGF-I.
When we evaluated the effect of IGF-I on the parasite burden in L. major promastigote- or amastigote-infected macrophages, we observed a significant increase in the number of parasites in macrophages stimulated with rIGF-I compared with that in nonstimulated macrophages (Figure 1(b)). Similar results were observed when amastigotes were used (Figure 1(c)).
3.2. The Effects of Leishmania Infection and Th1 and Th2 Cytokines on IGF-I Expression
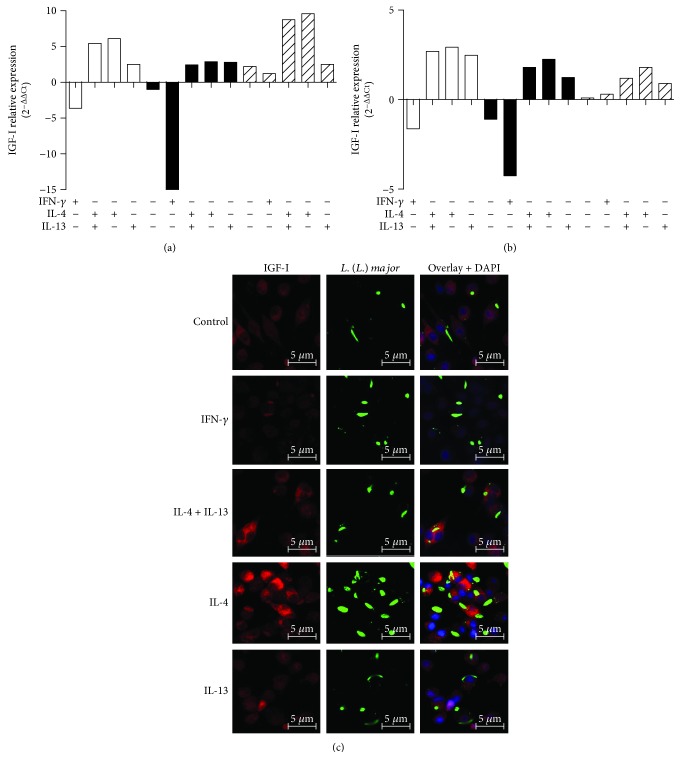
We analyzed the effects of Leishmania infection and Th1 and Th2 cytokines on the amount of the Igf-I mRNA. Infection of RAW 264.7 cells and BALB/c mouse peritoneal macrophages with promastigotes decreased the amount of Igf-I mRNA compared with that of the uninfected control cells. When promastigote-infected RAW 264.7 cells were stimulated with IFN-γ, we observed a 15-fold decrease in the amount of Igf-I mRNA. When cells were simultaneously stimulated with IL-4 and IL-13, we observed a 2.45-fold increase in the amount of Igf-I mRNA compared to that in the nonstimulated controls. When cells were stimulated with either IL-4 or IL-13, we observed a 2.9- or 4.8-fold increase in the amount of Igf-I mRNA, respectively (Figure 2(a)).
Figure 2.
IGF-I expression in response to cytokine treatment. (a and b) Quantification of Igf-I mRNA in L. major promastigote- (black bars) or amastigote-infected (striped bars) or noninfected (white bars) RAW 264.7 cells (a) and BALB/c peritoneal macrophages (b) is shown. Cells were stimulated with IFN-γ (200 U/mL), IL-4 (2 ng/mL), and IL-13 (5 ng/mL) for 48 hours. One representative experiment from three independent assays is shown. (c) Detection of IGF-I expression using confocal microscopy of cells labeled with a 1 : 75 dilution of an anti-IGF-I antibody (using an Alexa Fluor 546-conjugated secondary antibody; red) and a 1 : 200 dilution of an anti-Leishmania antibody (using an Alexa Fluor 488-conjugated secondary antibody; green) in L. major promastigote-infected macrophages is shown. Nuclei were stained with DAPI (blue). Images were captured using a confocal Leica LSM510 microscope with a 63x oil immersion objective. The expressions are relative to the expression in untreated cells (the baseline).
Upon amastigote infection of RAW 264.7 cells, we observed different amounts of Igf-I mRNA that increased in all infected cells compared with that in uninfected controls. A 2.2-fold increase in the amount of Igf-I mRNA was observed upon amastigote infection, a 1.2-fold increase was observed following stimulation with IFN-γ, and an 8.7-fold increase was observed when cells were simultaneously stimulated with IL-4 and IL-13. When cells were stimulated with either IL-4 or IL-13, we observed a 9.2- or 2.5-fold increase in the amount of Igf-I mRNA, respectively (Figure 2(a)). A similar profile was observed in BALB/c peritoneal macrophages (Figure 2(b)).
We confirmed these results using confocal microscopy. In Leishmania promastigote-infected macrophages, we observed a decrease in IGF-I immunostaining upon stimulation with IFN-γ compared with that in control cells. When cells were simultaneously stimulated with IL-4 and IL-13 or with IL-4 alone, we observed an increase in immunostaining, indicating increased IGF-I expression (Figure 2(c)).
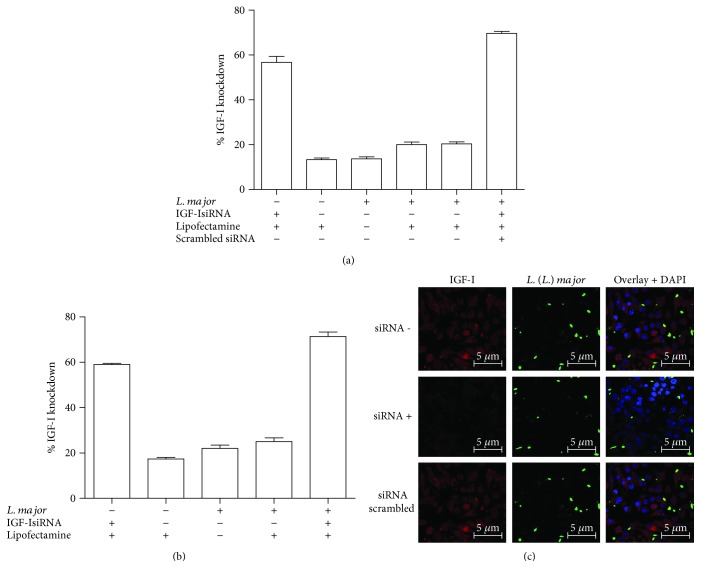
3.3. Inhibition of IGF-I Expression Using an IGF-I siRNA
Silencing IGF-I expression with siRNA resulted in an approximate 70% decrease in the mRNA amount in promastigote-infected RAW 264.7 cells (Figure 3(a)) and 78% in infected BALB/c peritoneal macrophages (Figure 3(b)). Using confocal microscopy, we observed a significant reduction in IGF-I immunostaining after siRNA transfection. Moreover, infection with L. major promastigotes alone inhibited IGF-I expression. A nonspecific double-stranded RNA (scrambled siRNA) was used as a negative control (Figure 3(c)). We observed similar results in cells infected with amastigotes (data not shown).
Figure 3.
Expression of Igf-I mRNA upon IGF-I silencing with an siRNA. The percentage decrease in the amount of Igf-I mRNA in RAW 264.7 cells (a) or BALB/c peritoneal macrophages (b) infected with L. major promastigotes that were transfected with 150 μM siRNA, scrambled siRNA, or Lipofectamine alone 6 h after infection is shown. One representative experiment from three independent assays is shown. (c) The detection of IGF-I expression in L. major promastigote-infected RAW 264.7 cells transfected with (siRNA+) or without the IGF-I siRNA (siRNA−) or with a scrambled siRNA using confocal microscopy of immunostaining with a 1 : 75 dilution of an anti-IGF-I antibody (using an Alexa Fluor 546-conjugated secondary antibody; red) and a 1 : 200 dilution of an anti-Leishmania antibody (using an Alexa Fluor 488-conjugated secondary antibody; green) is shown. Nuclei were stained with DAPI (blue). Images were captured using a confocal Leica LSM510 microscope with a 63x oil immersion objective.
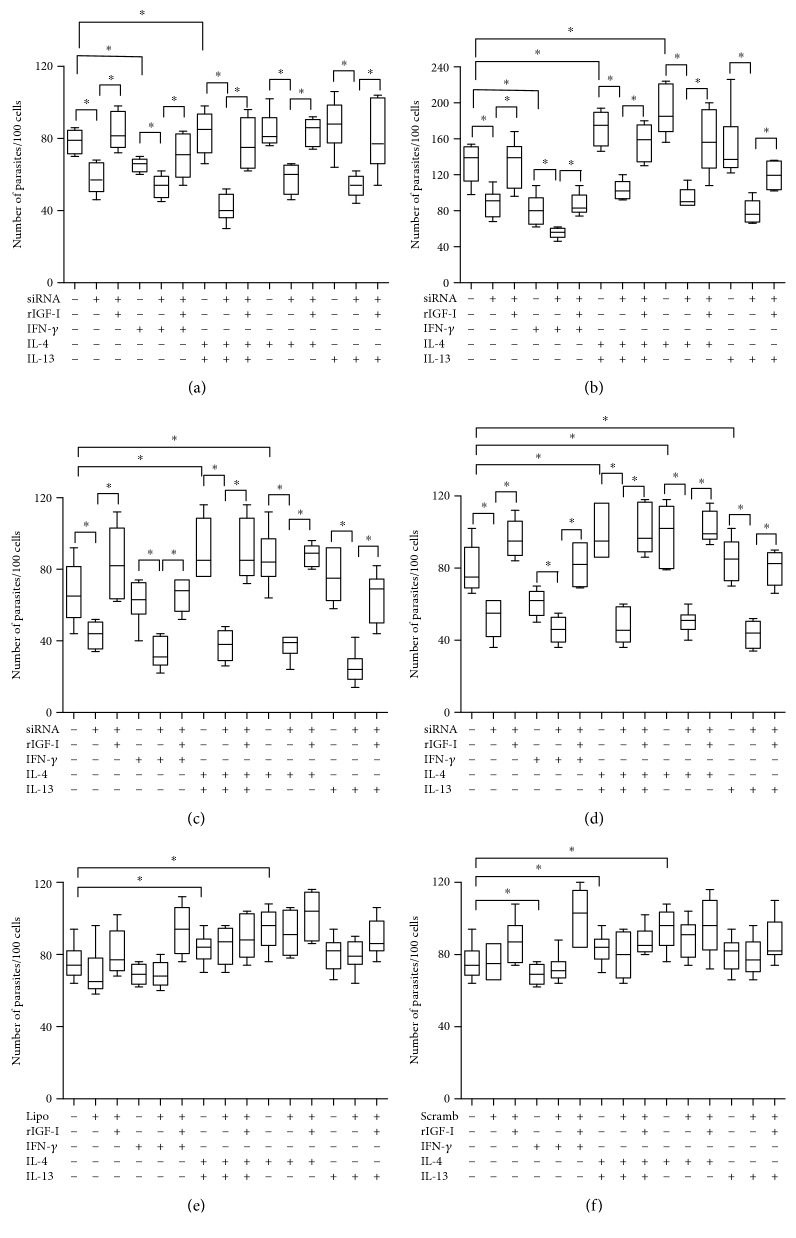
3.4. The Effect of IGF-I siRNA on Parasitism
Following infection with both promastigotes and amastigotes, we observed a significant increase in parasitism in cells exposed to Th2 cytokines (P < 0.05), as expected. In Th1 cytokine-stimulated cells, we noted a significant reduction in parasitism compared with that in the respective control (P < 0.05) (Figure 4).
Figure 4.
Parasitism in response to cytokine treatments and siRNA transfection. Parasitism (median number of parasites per 100 cells) in L. major-infected RAW 264.7 cells (a, b, e, and f) or BALB/c peritoneal macrophages (c and d) following transfection with IGF-I siRNA (a, b, c, and d), Lipofectamine alone (e), or scrambled siRNA (f) along with cytokine stimulation is shown. Promastigote- (a, c, e, and f) or amastigote-infected (b and d) cells transfected with or without siRNA or Lipofectamine were stimulated with IFN-γ (200 U/mL), IL-4 (2 ng/mL), IL-13 (5 ng/mL), and recombinant IGF-I (rIGF-I, 50 ng/mL) for 48 hours. One representative experiment from three independent assays is shown. ∗P < 0.05 (ANOVA and Tukey's tests).
Upon silencing IGF-I expression with an siRNA in L. major promastigote-infected RAW 264.7 cells, we observed a decrease in the parasite number from 79 parasites (median number in the control) to 57 parasites per 100 cells. In amastigote-infected cells, the parasite number was reduced from 139 to 91 parasites per 100 cells (P < 0.05). When we analyzed the involvement of Th1 and Th2 cytokines in parasitism following IGF-I silencing, all cells transfected with the siRNA showed a significant decrease in parasitism compared with that in the controls lacking siRNA following infection with both promastigotes and amastigotes (Figures 4(a) and 4(b)). The parasite load did not increase, even in Th2 cytokine-stimulated cells.
We observed similar results in L. major-infected BALB/c peritoneal macrophages to those obtained in L. major-infected RAW 264.7 cells, reinforcing the findings obtained from the RAW 264.7 cells (Figures 4(c) and 4(d)).
Experiments were performed to restore IGF-I activity after knockdown to ascertain the role of IGF-I. After transfection with siRNA, rIGF-I (50 ng/mL) was added to replace the loss of intracellular IGF-I, followed by an evaluation of parasitism. After the addition of rIGF-I to all cells transfected with siRNA, parasite numbers increased to the levels similar to the control cells lacking siRNA (Figure 4). We did not observe differences in parasitism in control cells treated with Lipofectamine or transfected with the scrambled siRNA compared with that in control cells. Infections with amastigotes or promastigotes produced similar results (Figures 4(e) and 4(f)).
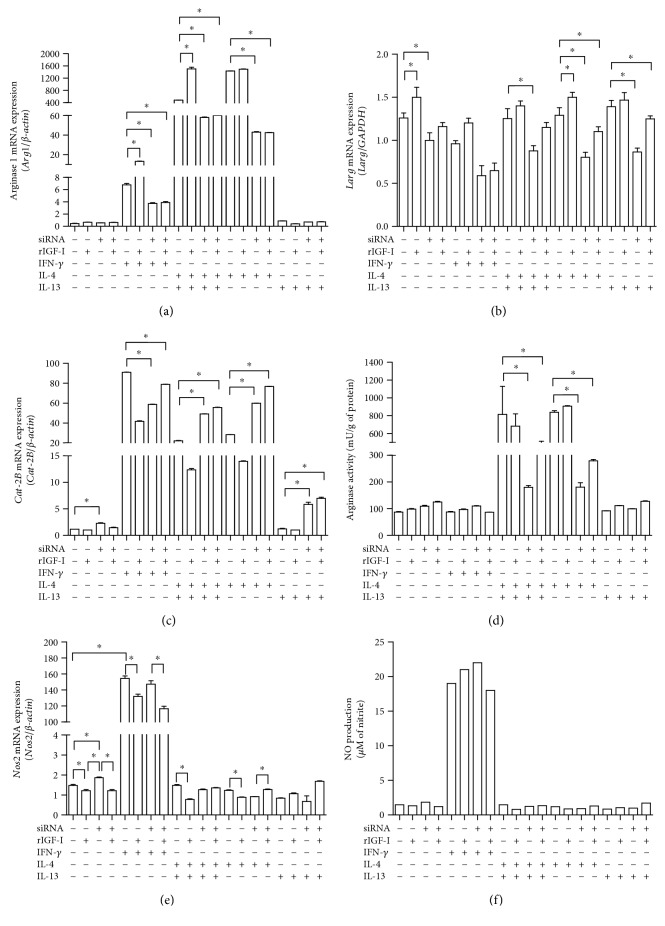
3.5. The Effects of IGF-I siRNA on the mRNA Amount of Nos2, Arginase (Arg1), and Cationic Amino Acid Transporter 2 (Cat-2B) in Macrophages and Leishmania Arginase (Larg) mRNA Expression and Enzyme Activity
We analyzed the effects of IFN-γ and IL-4 and/or IL-13 in combination with levels of IGF-I on L-arginine metabolism. IL-4 stimulation produced a significant increase in both Arg1 (Figure 5(a)) and Larg mRNAs (Figure 5(b)), as well as an increase in arginase activity (Figure 5(d)). However, IL-13 stimulation did not show an increase in Arg1 mRNA or arginase activity (Figures 5(a) and 5(d)) but showed an increase in Larg mRNA (Figure 5(b)). A significant increase in the amount of Cat-2B mRNA (Figure 5(c)) was observed after treatment with IL-4 (P < 0.05) compared to that in the control group.
Figure 5.
The effects of IGF-I siRNA transfection on the L-arginine metabolic pathway. The quantification of (a) Arg1 mRNA, (b) Larg mRNA, (c) Cat-2B mRNA, (d) arginase activity, (e) Nos2 mRNA, and (f) NO production in L. major-infected RAW 264.7 cells following transfection with IGF-I siRNA and cytokine stimulation is shown. Promastigote-infected cells transfected with or without IGF-I siRNA were stimulated with IFN-γ (200 U/mL), IL-4 (2 ng/mL), and IL-13 (5 ng/mL) for 48 hours. One representative experiment from three independent assays is shown. ∗P < 0.05 (ANOVA and Tukey's tests) compared to the respective control without siRNA.
When cells were treated with siRNA, all groups showed a significant decrease in both the Arg1 and Larg mRNA amounts and arginase activity and an increase in the Cat-2B mRNA amount (Figure 5(c)).
When IGF-I was restored by adding rIGF-I to cells transfected with siRNA, we observed increases in both the Larg mRNA amount and arginase activity. No differences in the Arg1 mRNA amount were observed in macrophages.
In another branch of the L-arginine metabolic pathway, we observed a decrease in the Nos2 mRNA amount in all groups treated with rIGF-I compared with the respective control group. In the group that was not stimulated with cytokines, we observed an increase in the Nos2 mRNA amount after siRNA transfection. Upon the addition of Th2 cytokines, an alteration in NO production was not observed (Figures 5(e) and 5(f)). Similar results were obtained using amastigotes and BALB/c peritoneal macrophages (data not shown).
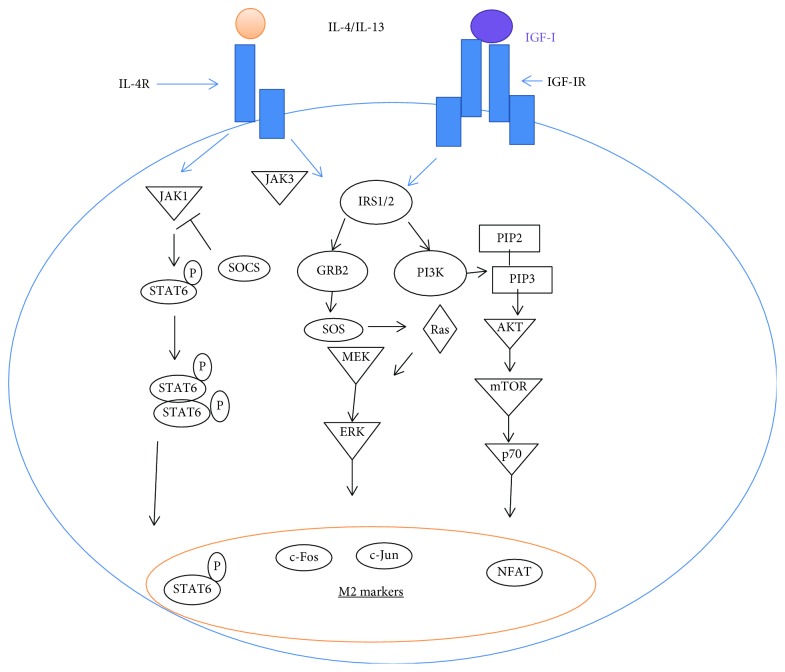
3.6. Evaluation of the Effects of siRNA and IL-4 on IGF-I Signaling Pathways
Because our results suggest that IGF-I is necessary for IL-4 to exert its effect on parasite growth in macrophages, we examined their intracellular signaling pathways. IGF-I and the cytokines IL-4 and IL-13 share common components in their signaling pathways. IGF-I triggers MAPK (ERK) and PI3K pathways [33, 34], and IL-4 sequentially activates IRS-2 and the PI3K/Akt and Ras-MAPK pathways [35, 36] (Figure 6). The Jak-Stat pathway is also known to be triggered by IL-4.
Figure 6.
Scheme of the common components of the IGF-I and IL-4 signaling pathways.
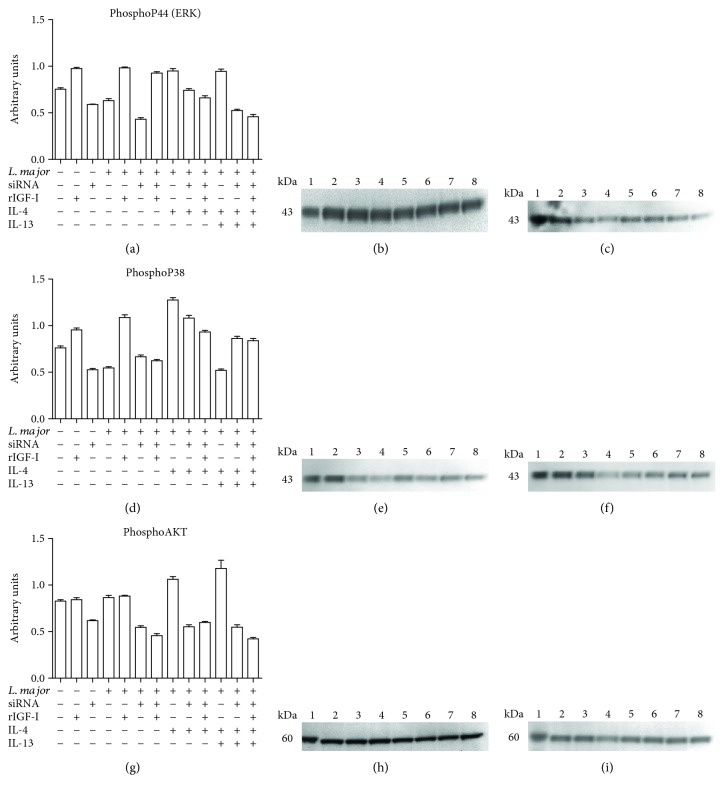
We analyzed the key components of the IGF-I signaling pathway, that is, p44 (ERK), p38 (MAPK), and total and phosphorylated AKT, upon stimulation with IL-4 and IL-4 plus IL-13 after IGF-I silencing. We did not observe any difference in the total protein levels across all groups (data not shown); however, differences in the levels of phosphorylated proteins were observed.
Cells infected with L. major displayed a decrease in the levels of phospho-p44 (Figure 7(a)) and phospho-p38 (Figure 7(d)), but a difference in the phospho-AKT level was not observed (Figure 7(g)) compared with that in the noninfected RAW cells. We observed an increase in the levels of these phosphorylated proteins in all groups treated with rIGF-I compared with noninfected RAW cells. A similar increase was also observed with IL-4.
Figure 7.
The effects of siRNA and IL-4 on components of the IGF-I signaling pathways: levels of phosphorylated p44 (ERK), p38 (MAPK), and AKT proteins. Promastigote-infected or noninfected cells transfected with or without IGF-I siRNA were stimulated for 30 minutes with IL-4 (2 ng/mL) and IL-13 (5 ng/mL). Cells were lysed, proteins were separated by 10% SDS-PAGE, and subsequently, Western blotting was performed using anti-phospho-p44 (a, b, and c), anti-phospho-p38 (d, e, and f), and anti-phospho-AKT (g, h, and i) antibodies. Protein bands corresponding to protein expression levels were subject to a densitometric analysis, and the data are expressed in arbitrary units (a, d, and g). A representative blot is shown. (b, e, h) The lanes represented the following: 1: control; 2: RAW; 3: RAW + rIGF; 4: RAW + siRNA; 5: RAW + Lm; 6: RAW + Lm + rIGF; 7: RAW + Lm + IL-4; and 8: RAW + Lm + IL-4 + IL-13. (c, f, i): 1: control; 2: RAW; 3: RAW + Lm + siRNA; 4: RAW + Lm + siRNA + rIGF; 5: RAW + Lm + siRNA + IL-4; 6: RAW + Lm + siRNA + IL-4 + rIGF; 7: RAW + Lm + siRNA + IL-4 + IL-13; and 8: RAW + Lm + siRNA + IL-4 + IL-13 + rIGF. See Materials and Methods for additional details.
Upon silencing IGF-I expression using siRNA, all groups showed a decrease in the expression of all phosphoproteins. In IGF-I-silenced cells, Th2 cytokine stimulation did not restore the decreased expression of phospho-p44, phospho-p38, and phospho-AKT.
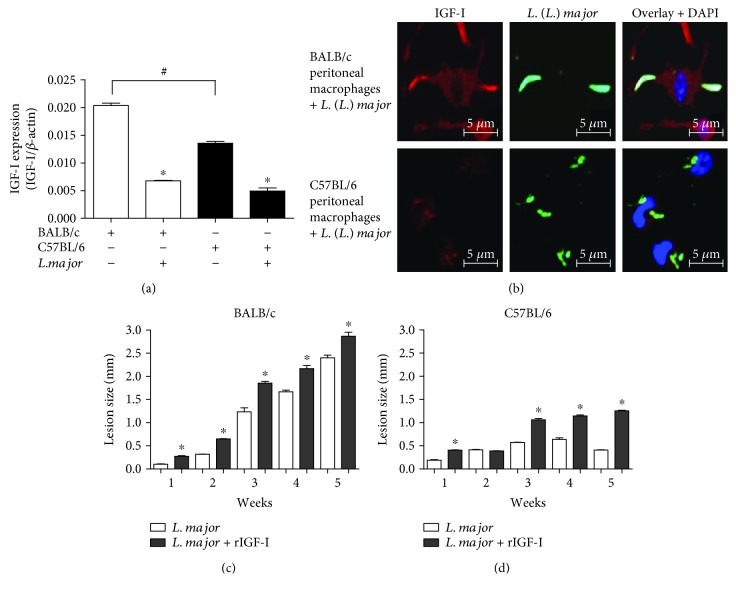
3.7. IGF-I Expression and the Effect of IGF-I on Lesion Development in L. major-Susceptible and -Resistant Mouse Strains
We initially evaluated the differences in the expression of IGF-I to determine whether the susceptibility of BALB/c mice and the resistance of C57BL/6 mice to L. major infection were related to IGF-I expression. The Igf-I mRNA was detected in higher levels in BALB/c cells than in C57BL/6 cells (P < 0.05) (Figure 8(a)). Confocal microscopy indicated a correlation between the amount of Igf-I mRNA and IGF-I expression, confirming that the C57BL/6 peritoneal macrophages showed less IGF-I immunostaining than BALB/c cells did (Figure 8(b)).
Figure 8.
IGF-I expression and the effect of IGF-I on lesion development in L. major-susceptible and -resistant mouse strains. (a) The ratio of the Igf-I mRNA amount to β-actin mRNA amount in L. major-infected BALB/c (white bars) and C57BL/6 peritoneal macrophages (black bars) is shown. (b) Confocal microscopy was used to detect IGF-I expression via immunostaining with a 1 : 75 dilution of an anti-IGF-I antibody (using an Alexa Fluor 546-conjugated secondary antibody; red) and a 1 : 200 dilution of an anti-Leishmania antibody (using an Alexa Fluor 488-conjugated secondary antibody; green). DAPI (blue) was used to stain the nuclei. Images were captured using a confocal Leica LSM510 microscope with a 63x oil immersion objective. (c and d) Stationary-phase promastigotes (106) that were preincubated with or without recombinant IGF-I (50 ng/mL) for 5 min were injected into the footpads of BALB/c and C57BL/6 mice, and lesion development was measured for six weeks. One representative experiment from three independent assays is shown. ∗P < 0.05 (ANOVA and Tukey's tests) compared to the respective controls. #P < 0.05 (ANOVA and Tukey's tests) between BALB/c and C57BL/6.
Then, we analyzed the effect of rIGF-I on lesion development in L. major-infected BALB/c and C57BL/6 mice. Parasites were preincubated with 50 ng/mL IGF-I for five minutes and then washed and injected into the footpads of the mice. In control BALB/c mice, the lesions progressed continuously, but when the parasites were preincubated with IGF-I, we observed a significantly greater lesion volume than that observed in the control mice (Figure 8(c)). In control C57BL/6 mice, the lesions progressed for three weeks and then stabilized and tended to diminish, but animals infected with parasites that were preincubated with IGF-I displayed significantly greater lesions, which, interestingly, progressed continuously, similar to that in the BALB/c mice (Figure 8(d)).
4. Discussion
Due to the known roles of Th1 and Th2 cytokines in the resistance and susceptibility of certain inbred mouse strains to L. major infection and their effects on the expression of the hormone IGF-I, which has an important impact on Leishmania growth within host macrophages, we examined the effect of interference in the hormone IGF-I expression on the adaptive immune response. We initially analyzed the effects of Th1 and Th2 cytokines on the amount of Igf-I mRNA and confirmed that IGF-I expression was decreased by IFN-γ and increased by IL-4 and IL-13, which was consistent with previous results [4, 6]. Furthermore, when we concomitantly analyzed IGF-I expression and the parasitism of L. major in RAW 264.7 cells or BALB/c peritoneal macrophages in vitro, we observed that the macrophages stimulated with IFN-γ exhibited a reduction in the parasite load, accompanied by a parallel reduction in IGF-I expression and ARG1 activity and an increase in NO production. Furthermore, IL-4 and IL-13 stimulation increased parasitism, accompanied by a parallel increase in IGF-I expression and arginase activity and a reduction in NO production.
These data showing the parallel effects of those cytokines and the expression of IGF-I on parasitism compelled us to explore the interference/participation of this hormone in the actions of cytokines and other factors during Leishmania infection.
The idea of immune-endocrine cross talk is not new and has been described in studies examining the roles of prolactin [37], growth hormone (GH) [38, 39], IGF-I, and thyroid-stimulating hormone in the development, maintenance, and function of the immune system, which in turn cause reciprocal changes in the endocrine system [5, 40].
IGF-I exhibits pleiotropic properties, including the ability to promote cellular proliferation, differentiation, nutrient transport, energy storage, gene transcription, protein synthesis, and activation of the immune response and inflammation [12, 41]. However, its specific role in the adaptive immune response is not known. Thus, we addressed this aspect in the present study using a knockdown strategy in RAW 264.7 and mouse peritoneal cells infected with L. major knowing that a significant amount of IGF-I colocalizes with L. major in the cytoplasm of Leishmania-infected RAW 264.7 cells.
Using an IGF-I siRNA, we silenced the Igf-I mRNA in macrophages and evaluated parasitism. We observed a significant decrease in parasitism in the siRNA-transfected group compared with that in the control group without siRNA transfection in response to both promastigote and amastigote infections. This effect was reversed by the addition of rIGF-I, which induced an increase in the number of parasites, even when siRNA-mediated knockdown was maintained. This restoration observed upon the addition of recombinant IGF-I was likely induced by an increase in the levels of Larg mRNA and Larg activity, accompanied by a slight decrease in the Nos-2 mRNA amount and NO production. Similar results were previously reported in which the addition of rIGF-I induced alternative activation of macrophages and arginase activation in L. amazonensis-infected macrophages [16, 17]. The present data definitively confirm the role of intrinsic IGF-I in intracellular parasite growth. Preliminary data further showed that the IGF-I siRNA decreased the parasite load in Leishmania major-infected BALB/c mouse footpad lesions (data not shown).
After observing such a clear-cut effect of IGF-I on parasite growth in macrophages, we proceeded to explore its role in infection development in L. major-infected macrophages stimulated with cytokines. After silencing Igf-I mRNA expression, the parasitism observed upon stimulation of the cells with cytokines did not follow the expected profile. IL-4 and IL-13 should have increased parasitism; however, they were completely ineffective when the Igf-I mRNA was silenced. Analyzing mRNA for components of L-arginine metabolism, we observed that the effect of IL-4 on infection progression was via the increase of Arg1 and Larg mRNAs, while the effect of IL-13 on infection progression was only via the increase in Larg mRNA.
The effects of IL-4 and IL-13 were restored by the administration of rIGF-I to IGF-I-silenced cells in a mechanism dependent on Leishmania arginase production, but not by ARG1. In another study using L. amazonensis-infected macrophages, a novel L-arginine usage pathway independent of macrophage NOS2 and ARG1 activation was involved in the response, suggesting that Leishmania may have the ability to obtain access to the intracellular L-arginine pool while residing within the host macrophage [42, 43]. This evidence was confirmed in the present study, as we observed an increase in parasitism upon the addition of rIGF-I in silenced cells without changes in the amount of Arg1 mRNA but an increase in the amount of Larg mRNA. Other studies have supported the importance of arginase production by the parasite since in vitro cultured L. donovani is capable of directly acquiring L-arginine from the medium and producing urea [44] or the deficiency in the infection and replication capabilities in L. amazonensis arginase knockout [45].
L-Arginine is supplied from the extracellular milieu by the cationic amino acid transporter 2 (CAT-2B), a member of the classical amino acid cationic transporter system y+ (SLC7) [42]. The observed increase in NOS2 expression may be related to an increase in CAT-2B expression since CAT-2B is required for the regulation of NOS2 activity that conversely may modulate CAT2-B expression through NO production [46–49].
The production of NO does not always follow the effect of the cytokines on parasitism, as the control of L. major parasitic infections does not appear to be related to NO production but rather to the presence or absence of IGF-I. Based on these results, cytokines alone are not sufficient to induce or control parasite growth, and IGF-I plays a crucial role in this process. We postulate that IGF-I may be an effector element of IL-4, which to the best of our knowledge constitutes the first evidence of cross talk between this hormone and the adaptive immune system in L. major infection.
Immune-endocrine cross talk involving IGF-I has been observed by others to mainly involve inflammatory cytokines IL-1 and TNF-α, which may inhibit both the expression of IGF-I or IGF-IR and the IGF-I-induced tyrosine phosphorylation of IRS-1 and IRS-2. This is an effect that is mediated by receptor cross talk and leads to intracellularly mediated IGF resistance [5]. Thus, these findings fundamentally differ from the findings of the present study showing that IGF-I plays a fundamental role as an effector element of Th2 cytokines.
The interaction of the endocrine and immune systems is somewhat expected, as they share several ligands and receptors in their signaling pathways. By analyzing the signaling pathways of IL-4/IL-13, which are related to the susceptibility to infection, we noticed shared components with the IGF-I pathway.
The biological effects of IGF-I occur through its binding to its receptor (IGF-IR), which is present in several cell types and tissues, mainly in macrophages. IGF-I signaling consists of two main pathways, the PI3K/Akt and mitogen-activated protein kinase (Ras/MAPK/ERK) pathways, when IRS-1 associates with the GRB2/SOS complex. IGF-I can also bind to insulin receptor (IR) when some excess of free IGF-I is present in the system that could have occurred in the present study but with lower affinity. IGF-IR and IR are highly homologous tyrosine kinase receptors sharing many common steps, inducing IRS1/2 phosphorylation and also AKT and MAPK [34, 50, 51]. Thus, if some IGF-I binds to IR, the resulted signaling will be nearly the same generating similar biological effects.
IL-4 mediates its effects through two receptors: the type I IL-4 receptor (IL-4Rα and IL-2Rγ) and the type II receptor (IL-4Rα and IL-13Rα1). Activation of these receptors results in STAT-6 phosphorylation that is necessary for the induction of the alternative macrophage pathway (M2). The ligation of the type I IL-4R activates JAK3 that participates in the activation of Akt, resulting in the induction of the M2 macrophage phenotype characterized by upregulation of molecules such as the mannose receptor, ARG1, and chitinase 3-like 3 [52]. IGF-I may also increase STAT-6 activity through IL-4, which is required to activate the expression of this cytokine [53].
In the present work, our analysis of the components of the IGF-I signaling pathway revealed increases in the amount of arginase mRNA, the phosphorylation of p44, p38, and Akt and parasitism in all groups treated either with rIGF-I or with IL-4. These results corroborated previous studies showing that IL-4 upregulates Akt activation and subsequently activates the alternative macrophage profile [54].
In the present study of L. major infection, we observed that all groups in which IGF-I expression was silenced using an siRNA, even IL-4-stimulated cells, showed decreases in both macrophage and parasite arginase mRNA amounts and decreases in the levels of all evaluated phosphorylated proteins. A decrease in parasitism accompanied these results, reinforcing the importance of IGF-I in the signaling induced by IL-4. In the literature, a similar study using an anti-IGF-I antibody or PI3K inhibitor in bone marrow-derived macrophages showed that IGF-I inhibition attenuated the IL-4-induced increases in the mRNA amount of M2 markers, such as mannose receptor, Arg1 mRNA and chitinase 3-like 3, as well as ARG1 protein expression, suggesting that IGF-I is required for IL-4-induced Akt phosphorylation and M2 activation [52]. Based on this evidence, we postulate that IGF-I is the element that actually activates the PI3K/Akt pathway, which IL-4 uses. In IFN-γ-treated cells, the application of the IGF-I siRNA strengthened the effect of decreasing the parasite load, and the addition of rIGF-I almost nullified this effect, returning it to levels similar to the control group. Reinforcing our finding, the inhibition of PI3K or treatment with an anti-IGF-I antibody exacerbates the effects of IFN-γ [52].
Our data are original in that they clearly show the interference of IGF-I on the IL-4 effect. In experimental visceral leishmaniasis, IGF-I increases the expression of arginase, while the deletion of IGF-IR leads to decreased arginase in a STAT-6-dependent mechanism and restriction of L. donovani growth [55]. These authors explored the role of extrinsic IGF-I but not of intrinsic IGF-I present within the cell, and they did not explore the interference of IGF-I on the IL-4 effect. Furthermore, it is known that the immune responses to Leishmania infection vary considerably according to the species of the parasite. In particular, the immune response to L. donovani and L. infantum, which are strains leading to visceral leishmaniasis, is quite different from the immune response established in the L. major model. In experimental visceral leishmaniasis, the role of IL-4 in the susceptibility to visceral disease is not clearly defined [55, 56]. Moreover, L-arginine metabolism of L. donovani is shown to be different from that of other species [57].
Regarding Leishmania infections in experimental models, we hypothesized that the profiles of mouse resistance and susceptibility to L. major infection are not only due to the effects of Th1 and Th2 cytokines, but that IGF-I may also play an important role in infection development due to constitutive differences in IGF-I expression. The BALB/c and C57BL/6 mouse strains did not exhibit similar expression profiles of IGF-I, with the latter displaying lower expression. Similarly, lower serum IGF-I levels have been detected in C57BL/6 mice compared to that in C3H/HeJ mice [29]. To address this issue, we analyzed the effect of IGF-I in vivo and found that lesion development in mice was increased when L. major promastigotes were preincubated with recombinant IGF-I and applied to susceptible and resistant mouse strains. The lesions in BALB/c mice increased in size and were progressive, but the profile of lesion development was more striking in C57BL/6 mice, as the lesions in mice injected with IGF-I-preincubated parasites not only increased in size but also became progressive, even in the late phase when the lesions in the control animals were diminishing. This resistant-to-susceptible profile reversion was not observed in certain previous studies [25, 28]. Although the lesions in C57BL/6 mice increased progressively following treatment with rIGF-I, the lesion size was smaller than lesions in BALB/c mice. This difference might be due to the IL-4 production pattern in these mouse strains. IL-4 production is similar in the initial phase of infection in both susceptible and resistant mice; however, the production of this cytokine in resistant mice is transient [26]. Another study also showed a nonsustained IL-4 level. In resistant mice, treatment with rIL-4 at the beginning of the infection did not induce the susceptible profile due to the noncontinuous production of IL-4 during the infection [25]. Thus, the main characteristics and differences in terms of susceptibility and resistance observed in certain L. major-infected mouse strains may be due to cytokines to some extent, but the susceptibility essentially depends on the presence of IGF-I.
5. Conclusions
The present study provides new insights into the immunology of leishmaniasis, reinforcing the importance of IGF-I in Leishmania infection by revealing a significant immune-endocrine interaction in this context. Our data strongly suggest that IGF-I is an effector element of IL-4 actions, leading to M2 macrophage differentiation, involving the PI3K/Akt pathway during L. major infection.
Our findings raise questions about pathogenic processes in other diseases in which Th2 cytokines play an important role. In relation to the pathogenesis of leishmaniasis, a polymorphism in the IGF-I gene has been detected in the human population [58, 59]; thus, we speculate that individuals in endemic areas will be susceptible or resistant or will exhibit exacerbation or modulation of the pathogenic process, depending on the expression of basal IGF-I.
Acknowledgments
This work was supported by grants from the Fundação de Amparo à Pesquisa do Estado de São Paulo (fellowships 2008/04106-0 to Luiza C. Reis and 2005/52271-1 to Fabricio Petitto-Assis), the Conselho Nacional de Desenvolvimento Científico e Tecnológico (Grant 484499/2006 and research fellowship to Hiro Goto), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior/SIU (Grant 001/2013 and fellowships 11613/13-0 to Luiza C. Reis and 11615/13-3 to Eduardo Milton Ramos-Sanchez), the Programa Nacional de Pós Doutorado (PNPD)/Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (fellowship 1476173 to Luiza C. Reis) and LIM 38 (Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo). The authors acknowledge Ana Lúcia Garippo for providing technical assistance with confocal microscopy, Celio Xavier da Costa dos Santos for providing initial assistance with the siRNA methodology, and Sandra Muxel for providing technical assistance with the arginase expression methodology.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Frystyk J. Free insulin-like growth factors -- measurements and relationships to growth hormone secretion and glucose homeostasis. Growth Hormone & IGF Research. 2004;14(5):337–375. doi: 10.1016/j.ghir.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Hehlgans T., Pfeffer K. The intriguing biology of the tumour necrosis factor/tumour necrosis factor receptor superfamily: players, rules and the games. Immunology. 2005;115(1):1–20. doi: 10.1111/j.1365-2567.2005.02143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valverde A. M., Benito M., Lorenzo M. The brown adipose cell: a model for understanding the molecular mechanisms of insulin resistance. Acta Physiologica Scandinavica. 2005;183(1):59–73. doi: 10.1111/j.1365-201X.2004.01384.x. [DOI] [PubMed] [Google Scholar]
- 4.Arkins S., Rebeiz N., Brunke-Reese D. L., Biragyn A., Kelley K. W. Interferon-gamma inhibits macrophage insulin-like growth factor-I synthesis at the transcriptional level. Molecular Endocrinology. 1995;9(3):350–360. doi: 10.1210/mend.9.3.7776981. [DOI] [PubMed] [Google Scholar]
- 5.O'Connor J. C., McCusker R. H., Strle K., Johnson R. W., Dantzer R., Kelley K. W. Regulation of IGF-I function by proinflammatory cytokines: at the interface of immunology and endocrinology. Cellular Immunology. 2008;252(1-2):91–110. doi: 10.1016/j.cellimm.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wynes M. W., Riches D. W. H. Induction of macrophage insulin-like growth factor-I expression by the Th2 cytokines IL-4 and IL-13. Journal of Immunology. 2003;171(7):3550–3559. doi: 10.4049/jimmunol.171.7.3550. [DOI] [PubMed] [Google Scholar]
- 7.Scott P., Novais F. O. Cutaneous leishmaniasis: immune responses in protection and pathogenesis. Nature Reviews Immunology. 2016;16(9):581–592. doi: 10.1038/nri.2016.72. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO) Control of leishmaniases. World Health Organ Technical Report Series. 2010;(949):xii–xiii. [PubMed] [Google Scholar]
- 9.Liew F. Y., Millott S., Parkinson C., Palmer R. M., Moncada S. Macrophage killing of Leishmania parasite in vivo is mediated by nitric oxide from L-arginine. The Journal of Immunology. 1990;144(12):4794–4797. [PubMed] [Google Scholar]
- 10.Roberts S. C., Tancer M. J., Polinsky M. R., Gibson K. M., Heby O., Ullman B. Arginase plays a pivotal role in polyamine precursor metabolism in Leishmania. Characterization of gene deletion mutants. The Journal of Biological Chemistry. 2004;279(22):23668–23678. doi: 10.1074/jbc.M402042200. [DOI] [PubMed] [Google Scholar]
- 11.da Silva M. F. L., Floeter-Winter L. M. Arginase in Leishmania. Sub-Cellular Biochemistry. 2014;74:103–117. doi: 10.1007/978-94-007-7305-9_4. [DOI] [PubMed] [Google Scholar]
- 12.Jones J. I., Clemmons D. R. Insulin-like growth factors and their binding proteins: biological actions. Endocrine Reviews. 1995;16(1):3–34. doi: 10.1210/edrv-16-1-3. [DOI] [PubMed] [Google Scholar]
- 13.Gomes C. M. C., Goto H., Corbett C. E. P., Gidlund M. Insulin-like growth factor-1 is a growth promoting factor for Leishmania promastigotes. Acta Tropica. 1997;64(3-4):225–228. doi: 10.1016/S0001-706X(96)00633-X. [DOI] [PubMed] [Google Scholar]
- 14.Gomes C. M. C., Monteiro H. P., Gidlund M., Corbett C. E. P., Goto H. Insulin-like growth factor-I induces phosphorylation in Leishmania (Leishmania) mexicana promastigotes and amastigotes. The Journal of Eukaryotic Microbiology. 1998;45(3):352–355. doi: 10.1111/j.1550-7408.1998.tb04548.x. [DOI] [PubMed] [Google Scholar]
- 15.Goto H., Gomes C. M. C., Corbett C. E. P., Monteiro H. P., Gidlund M. Insulin-like growth factor I is a growth-promoting factor for Leishmania promastigotes and amastigotes. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(22):13211–13216. doi: 10.1073/pnas.95.22.13211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vendrame C. M. V., Carvalho M. D. T., Rios F. J. O., Manuli E. R., Petitto-Assis F., Goto H. Effect of insulin-like growth factor-I on Leishmania amazonensis promastigote arginase activation and reciprocal inhibition of NOS2 pathway in macrophage in vitro. Scandinavian Journal of Immunology. 2007;66(2-3):287–296. doi: 10.1111/j.1365-3083.2007.01950.x. [DOI] [PubMed] [Google Scholar]
- 17.Vendrame C. M. V., Carvalho M. D. T., Tempone A. G., Goto H. Insulin-like growth factor-i induces arginase activity in leishmania amazonensis amastigote-infected macrophages through a cytokine-independent mechanism. Mediators of Inflammation. 2014;2014:13. doi: 10.1155/2014/475919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomes C. M., Goto H., Ribeiro da Matta V. L., Laurenti M. D., Gidlund M., Corbett C. E. Insulin-like growth factor (IGF)-I affects parasite growth and host cell migration in experimental cutaneous leishmaniasis. International Journal of Experimental Pathology. 2000;81(4):249–255. doi: 10.1046/j.1365-2613.2000.00157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reis L. C., Ramos-Sanchez E. M., Goto H. The interactions and essential effects of intrinsic insulin-like growth factor-I on Leishmania (Leishmania) major growth within macrophages. Parasite Immunology. 2013;35(7-8):239–244. doi: 10.1111/pim.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scott P., Farrell J. P. Experimental cutaneous leishmaniasis: induction and regulation of T cells following infection of mice with Leishmania major. Chemical Immunology. 1998;70:60–80. doi: 10.1159/000058698. [DOI] [PubMed] [Google Scholar]
- 21.Heinzel F. P., Sadick M. D., Holaday B. J., Coffman R. L., Locksley R. M. Reciprocal expression of interferon gamma or interleukin 4 during the resolution or progression of murine leishmaniasis. Evidence for expansion of distinct helper T cell subsets. Journal of Experimental Medicine. 1989;169(1):59–72. doi: 10.1084/jem.169.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Locksley R. M., Heinzel F. P., Sadick M. D., Holaday B. J., Gardner K. D., Jr Murine cutaneous leishmaniasis: susceptibility correlates with differential expansion of helper T-cell subsets. Annales de l'Institut Pasteur. Immunologie. 1987;138(5):744–749. doi: 10.1016/S0769-2625(87)80030-2. [DOI] [PubMed] [Google Scholar]
- 23.Matthews D. J., Emson C. L., McKenzie G. J., Jolin H. E., Blackwell J. M., McKenzie A. N. J. IL-13 is a susceptibility factor for Leishmania major infection. Journal of Immunology. 2000;164(3):1458–1462. doi: 10.4049/jimmunol.164.3.1458. [DOI] [PubMed] [Google Scholar]
- 24.Reiner S. L., Locksley R. M. The regulation of immunity to Leishmania major. Annual Review of Immunology. 1995;13(1):151–177. doi: 10.1146/annurev.iy.13.040195.001055. [DOI] [PubMed] [Google Scholar]
- 25.Hondowicz B. D., Scharton-Kersten T. M., Jones D. E., Scott P. Leishmania major-infected C3H mice treated with anti-IL-12 mAb develop but do not maintain a Th2 response. Journal of Immunology. 1997;159(10):5024–5031. [PubMed] [Google Scholar]
- 26.Stetson D. B., Mohrs M., Mallet-Designe V., Teyton L., Locksley R. M. Rapid expansion and IL-4 expression by Leishmania-specific naive helper T cells in vivo. Immunity. 2002;17(2):191–200. doi: 10.1016/S1074-7613(02)00363-1. [DOI] [PubMed] [Google Scholar]
- 27.Scott P., Eaton A., Gause W. C., di Zhou X., Hondowicz B. Early IL-4 production does not predict susceptibility to Leishmania major. Experimental Parasitology. 1996;84(2):178–187. doi: 10.1006/expr.1996.0103. [DOI] [PubMed] [Google Scholar]
- 28.Shankar A. H., Titus R. G. T cell and non-T cell compartments can independently determine resistance to Leishmania major. The Journal of Experimental Medicine. 1995;181(3):845–855. doi: 10.1084/jem.181.3.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iida K., Rosen C. J., Ackert-Bicknell C., Thorner M. O. Genetic differences in the IGF-I gene among inbred strains of mice with different serum IGF-I levels. The Journal of Endocrinology. 2005;186(3):481–489. doi: 10.1677/joe.1.06200. [DOI] [PubMed] [Google Scholar]
- 30.Green L. C., Wagner D. A., Glogowski J., Skipper P. L., Wishnok J. S., Tannenbaum S. R. Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Analytical Biochemistry. 1982;126(1):131–138. doi: 10.1016/0003-2697(82)90118-X. [DOI] [PubMed] [Google Scholar]
- 31.Corraliza I. M., Campo M. L., Soler G., Modolell M. Determination of arginase activity in macrophages: a micromethod. Journal of Immunological Methods. 1994;174(1-2):231–235. doi: 10.1016/0022-1759(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 32.Pfaffl M. W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Research. 2001;29(9, article e45) doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carvalheira J. B. C., Zecchin H. G., Saad M. J. A. Vias de sinalização da insulina. Arquivos Brasileiros de Endocrinologia e Metabologia. 2002;46(4):419–425. doi: 10.1590/S0004-27302002000400013. [DOI] [Google Scholar]
- 34.Laviola L., Natalicchio A., Perrini S., Giorgino F. Abnormalities of IGF-I signaling in the pathogenesis of diseases of the bone, brain, and fetoplacental unit in humans. American Journal of Physiology. Endocrinology and Metabolism. 2008;295(5):E991–E999. doi: 10.1152/ajpendo.90452.2008. [DOI] [PubMed] [Google Scholar]
- 35.Heller N. M., Matsukura S., Georas S. N., et al. Interferon-γ inhibits STAT6 signal transduction and gene expression in human airway epithelial cells. American Journal of Respiratory Cell and Molecular Biology. 2004;31(5):573–582. doi: 10.1165/rcmb.2004-0195OC. [DOI] [PubMed] [Google Scholar]
- 36.Gordon S., Martinez F. O. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32(5):593–604. doi: 10.1016/j.immuni.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 37.Gala R. R. Prolactin and growth hormone in the regulation of the immune system. Proceedings of the Society for Experimental Biology and Medicine. 1991;198(1):513–527. doi: 10.3181/00379727-198-43286B. [DOI] [PubMed] [Google Scholar]
- 38.Kooijman R., Hooghe-Peters E. L., Hooghe R. Prolactin, growth hormone, and insulin-like growth factor-I in the immune system. Advances in Immunology. 1996;63:377–454. doi: 10.1016/s0065-2776(08)60860-3. [DOI] [PubMed] [Google Scholar]
- 39.Weigent D. A. Immunoregulatory properties of growth hormone and prolactin. Pharmacology & Therapeutics. 1996;69(3):237–257. doi: 10.1016/0163-7258(96)00001-0. [DOI] [PubMed] [Google Scholar]
- 40.Kelley K. W., Weigent D. A., Kooijman R. Protein hormones and immunity. Brain, Behavior, and Immunity. 2007;21(4):384–392. doi: 10.1016/j.bbi.2006.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohick W. S., Clemmons D. R. The insulin-like growth factors. Annual Review of Physiology. 1993;55(1):131–153. doi: 10.1146/annurev.ph.55.030193.001023. [DOI] [PubMed] [Google Scholar]
- 42.Wanasen N., MacLeod C. L., Ellies L. G., Soong L. L-Arginine and cationic amino acid transporter 2B regulate growth and survival of Leishmania amazonensis amastigotes in macrophages. Infection and Immunity. 2007;75(6):2802–2810. doi: 10.1128/IAI.00026-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Castilho-Martins E. A., Laranjeira da Silva M. F., dos Santos M. G., Muxel S. M., Floeter-Winter L. M. Axenic Leishmania amazonensis promastigotes sense both the external and internal arginine pool distinctly regulating the two transporter-coding genes. PLoS One. 2011;6(11, article e27818) doi: 10.1371/journal.pone.0027818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kandpal M., Fouce R. B., Pal A., Guru P. Y., Tekwani B. L. Kinetics and molecular characteristics of arginine transport by Leishmania donovani promastigotes. Molecular and Biochemical Parasitology. 1995;71(2):193–201. doi: 10.1016/0166-6851(95)00042-Y. [DOI] [PubMed] [Google Scholar]
- 45.da Silva M. F. L., Zampieri R. A., Muxel S. M., Beverley S. M., Floeter-Winter L. M. Leishmania amazonensis arginase compartmentalization in the glycosome is important for parasite infectivity. PLoS One. 2012;7(3, article e34022) doi: 10.1371/journal.pone.0034022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nicholson B., Manner C. K., Kleeman J., MacLeod C. L. Sustained nitric oxide production in macrophages requires the arginine transporter CAT2. The Journal of Biological Chemistry. 2001;276(19):15881–15885. doi: 10.1074/jbc.M010030200. [DOI] [PubMed] [Google Scholar]
- 47.Huang C. J., Tsai P. S., Yang C. H., et al. Pulmonary transcription of CAT-2 and CAT-2B but not CAT-1 and CAT-2A were upregulated in hemorrhagic shock rats. Resuscitation. 2004;63(2):203–212. doi: 10.1016/j.resuscitation.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 48.Liu M. C., Tsai P. S., Yang C. H., Liu C. H., Chen C. C., Huang C. J. Propofol significantly attenuates iNOS, CAT-2, and CAT-2B transcription in lipopolysaccharide-stimulated murine macrophages. Acta Anaesthesiologica Taiwania. 2006;44(2):73–81. [PubMed] [Google Scholar]
- 49.Rath M., Muller I., Kropf P., Closs E. I., Munder M. Metabolism via arginase or nitric oxide synthase: two competing arginine pathways in macrophages. Frontiers in Immunology. 2014;5:p. 532. doi: 10.3389/fimmu.2014.00532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.White M. F. The IRS-signaling system: a network of docking proteins that mediate insulin and cytokine action. Recent Progress in Hormone Research. 1998;53:119–138. [PubMed] [Google Scholar]
- 51.Soon L., Flechner L., Gutkind J. S., et al. Insulin-like growth factor I synergizes with interleukin 4 for hematopoietic cell proliferation independent of insulin receptor substrate expression. Molecular and Cellular Biology. 1999;19(5):3816–3828. doi: 10.1128/MCB.19.5.3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barrett J. P., Minogue A. M., Falvey A., Lynch M. A. Involvement of IGF-1 and Akt in M1/M2 activation state in bone marrow-derived macrophages. Experimental Cell Research. 2015;335(2):258–268. doi: 10.1016/j.yexcr.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 53.Kim J. H., Park H. H., Lee C. E. IGF-1 potentiation of IL-4-induced CD23/FcεRII expression in human B cells. Molecules and Cells. 2003;15(3):307–312. [PubMed] [Google Scholar]
- 54.Ruckerl D., Jenkins S. J., Laqtom N. N., et al. Induction of IL-4Rα-dependent microRNAs identifies PI3K/Akt signaling as essential for IL-4-driven murine macrophage proliferation in vivo. Blood. 2012;120(11):2307–2316. doi: 10.1182/blood-2012-02-408252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Osorio E. Y., Travi B. L., da Cruz A. M., Saldarriaga O. A., Medina A. A., Melby P. C. Growth factor and Th2 cytokine signaling pathways converge at STAT6 to promote arginase expression in progressive experimental visceral leishmaniasis. PLoS Pathogens. 2014;10(6, article e1004165) doi: 10.1371/journal.ppat.1004165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kumar R., Nylén S. Immunobiology of visceral leishmaniasis. Frontiers in Immunology. 2012;3 doi: 10.3389/fimmu.2012.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Boitz J. M., Gilroy C. A., Olenyik T. D., et al. Arginase is essential for survival of Leishmania donovani promastigotes but not intracellular amastigotes. Infection and Immunity. 2016;85(1):e00554–e00516. doi: 10.1128/IAI.00554-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vaessen N., Heutink P., Janssen J. A., et al. A polymorphism in the gene for IGF-I: functional properties and risk for type 2 diabetes and myocardial infarction. Diabetes. 2001;50(3):637–642. doi: 10.2337/diabetes.50.3.637. [DOI] [PubMed] [Google Scholar]
- 59.Frayling T. M., Hattersley A. T., McCarthy A., et al. A putative functional polymorphism in the IGF-I gene: association studies with type 2 diabetes, adult height, glucose tolerance, and fetal growth in U.K. populations. Diabetes. 2002;51(7):2313–2316. doi: 10.2337/diabetes.51.7.2313. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.