INTRODUCTION
Sleep disturbances increase in prevalence during the menopausal transition, with the most common complaint being nighttime awakenings.1, 2 Sleep disturbances impact health-related quality of life, work productivity, and healthcare utilization,3 and can have long-term effects on health and wellbeing across several years of the menopausal transition. Here, we aim to provide an overview of sleep disturbances in the context of the menopausal transition, considering self-reported and objectively measured indicators of sleep. We also consider factors that could mediate sleep disturbance, including female sex steroids, vasomotor symptoms (e.g. hot flashes and sweating), aging, and stressful life events. Finally, we provide an overview of potential treatment options and their efficacy and highlight the need for further research. Understanding the causes, as well as effective preventative and treatment strategies for menopausal sleep disturbances, is essential for better health, quality of life, and work ability.
DEFINITION AND PHYSIOLOGY OF MENOPAUSE
Menopause (defined as the time of the final menstrual period) is a natural process in normal female aging, resulting from depletion of ovarian follicles, and occurs at a median age of 51 years,4 with the menopausal transition usually starting at about 47 years.5 The Stages of Reproductive Aging Workshop (STRAW +10) standardizes the division of a woman’s late reproductive life, broadly grouping women into three categories (reproductive, menopausal transition, and post-menopause) further subdivided, according to menstrual cycle length and regularity.6 Peri-menopause encompasses the menopausal transition and the first year after the final menstrual period. The term “climacteric” may also be used to describe peri-menopause and the part of the post-menopausal period in which climacteric symptoms occur.
Ovarian function begins to deteriorate, and function of the hypothalamic-pituitary-ovarian axis begins to change, several years before menopause. These endocrinological changes typically occur gradually and are not linear. Levels of follicle stimulating hormone (FSH) rise overall, and are typically ≥25IU/L in the late menopausal transition. In association with the fluctuation and gradual decline in estrogen (typically estradiol) across the menopausal transition, menopausal symptoms emerge and include vasomotor symptoms (hot flashes and sweating), sleep disturbances, and mood symptoms (Table 1).
Table 1.
Typical menopausal symptoms and their prevalence in midlife women
| Symptom | Prevalence (%) |
|---|---|
| Hot flashes and/or night sweats | 36 – 87 |
| Sleep problems | 40 – 60 |
| Mood symptoms | 15 – 78 |
| Weight gain | 60 – 70 |
| Muscle and/or joint pain | 48 – 72 |
| Palpitation | 44 – 50 |
| Headache | 32 – 71 |
| Memory impairment | 41 – 44 |
| Genitourinary symptoms | 25 – 30 |
| Sexual dysfunction | 20 – 30 |
SLEEP QUALITY DURING THE MENOPAUSAL TRANSITION
Self-reported sleep quality
Among menopausal symptoms, sleep disturbances are one of the most bothersome symptoms, and are reported by 40–60% of menopausal women.7 There is convincing evidence from several cross-sectional8-12 and longitudinal13-16 studies that the prevalence of perceived sleep disturbances increases in the menopausal transition, even after controlling for age. A recent meta-analysis of cross-sectional data from 24 studies reported higher odds of experiencing sleep disturbance in peri-menopause (1.60), post-menopause (1.67), and surgical menopause (2.17) relative to women who are pre-menopausal.17
The most common sleep-related complaint is nighttime awakenings.8, 11, 14, 16 In their seven-year follow-up of 3045 women, the Study of Women’s Health Across the Nation (SWAN) reported an increase in odds ratios (OR) for difficulty staying asleep across the menopausal transition after adjusting for demographics and health-related factors.14 ORs also increased for difficulty falling asleep across the transition, but decreased for early morning awakening from late peri-menopause to post-menopause. While the majority of studies examined associations between sleep and menopausal stages based on bleeding patterns, some studies have investigated the association between follicle stimulating hormone (FSH) concentrations and self-reported sleep.14, 16 Increasing FSH was associated with greater odds of waking up several times, whereas decreasing estrogen (E2) was associated with higher odds of difficulty falling and staying asleep in SWAN.14
Polysomnographic (PSG) studies
Even though the evidence for declining self-reported sleep quality across the menopausal transition is strong, polysomnographic (PSG) studies have generally not found a corresponding negative change in sleep architecture. PSG-derived measures of sleep do not necessarily reflect self-report sleep quality ratings18 and psychological state may influence sleep quality judgments by affecting the sleep appraisal process rather than sleep itself.19 Also, most PSG studies have been cross-sectional and included small samples, with few exceptions.12, 20 Further, studies have varied in methodology including definitions of menopausal stages, age ranges, assessment of the presence of sleep disorders like obstructive sleep apnea, and inclusion of an adaptation night, leading to contradictory results and challenges when trying to make study comparisons.
Some studies have found no differences in sleep architecture between pre- and post-menopausal women,21-23 while a few studies have reported more slow wave sleep (SWS) in peri- and post-menopausal women than pre-menopausal women.12, 20, 24 More SWS could be interpreted as reflecting a better sleep pattern, on the one hand, but alternatively could reflect a recovery response to sleep deprivation; further studies are needed to better understand potential changes in SWS post-menopause. Post-menopausal women had a higher apnea-hypopnea index (AHI) and lower arterial oxyhemoglobin saturation (SaO2).20 Finally, SWAN investigators found no differences in PSG measures according to menopausal status.21 However, late peri-menopausal and post-menopausal women had more high frequency beta EEG activity, suggesting greater cortical hyperarousal, during sleep than pre-menopausal and early peri-menopausal women, an effect partially explained by higher frequency of self-report hot flashes.21
A limited number of studies have investigated the association between FSH, as an endocrine marker of transitioning menopause, with PSG measures. SWAN investigators found that a more rapid rate of FSH change over the previous few years was associated with higher amount of SWS and longer total sleep time (TST) during a subsequent sleep study.25 Another cross-sectional study of women mostly in the early menopausal transition (aged 43–52 years) without sleep complaints found that higher FSH concentrations were associated with more wakefulness after sleep onset (WASO), awakenings, and arousals, after adjusting for age and BMI.26 However, in women with menopausal insomnia, PSG measures did not correlate with FSH and instead were associated with anxiety and depression symptoms.26 In a small study that evaluated associations of sleep and hypothalamic-pituitary-ovarian (HPO) axis hormones in a group of pre- and post-menopausal women with diagnoses of depression, FSH level was positively associated with WASO and negatively associated with SWS.27
In the only longitudinal study of changes in PSG measures across the menopausal transition, Lampio and colleagues24 studied 60 midlife women at a pre-menopausal baseline visit and again, six years later. At follow-up, women had less TST and more WASO after adjusting for vasomotor symptoms, BMI, and mood (See Figure 1 showing the PSG changes in a representative participant). These changes in sleep were linked with advancing age rather than increased FSH levels. Increasing FSH was associated with a greater proportion of SWS (although not with slow wave EEG activity), which the authors propose as reflecting an adaptive change to counteract the age-related sleep fragmentation.24
Figure 1:
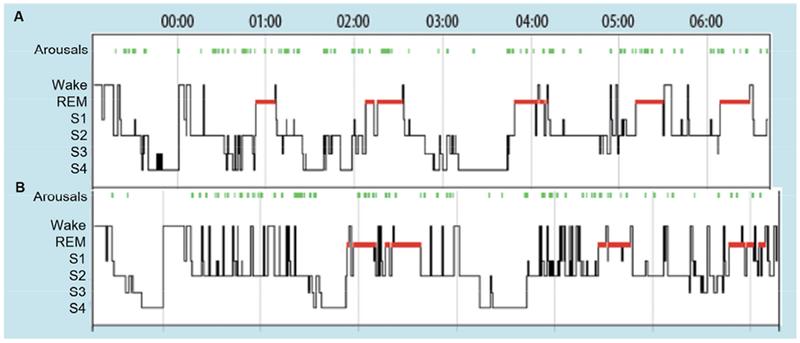
Hypnograms derived from the polysomnograms of one representative participant during her premenopausal baseline visit (A) and at a follow-up visit 6 years later (B), when she was peri-menopausal. Data from Lampio L, Polo-Kantola P, Himanen SL, et al. Sleep during menopausal transition: A six-year follow-up. Sleep. 2017.
In summary, PSG studies have shown few consistent effects of menopausal stage on sleep architecture independent of age. All but one study were cross-sectional and therefore unable to track changes in sleep across the transition, and few studies have used more complex indicators of sleep disruption, like quantitative EEG analysis. Given between-women variability in hormone trajectories, speed of transitioning menopause, and life experiences as they transition menopause, all of which can interact with sleep, further longitudinal studies are needed in midlife women to establish if PSG measures fluctuate in association with the changing hormone environment in the menopausal transition. Also, as discussed next, subgroups of women might be more susceptible to sleep disturbances, particularly women with severe vasomotor symptoms or insomnia disorder.
VASOMOTOR SYMPTOMS (HOT FLASHES AND SWEATING) AND SLEEP DISTURBANCE
Vasomotor symptoms, an umbrella term used to describe hot flashes and sweating, affect up to 80% of women during menopause transition.28 Data from SWAN show a median duration for vasomotor symptoms of 7.4 years29 but the temporal pattern based on symptom onset and persistence varies,30, 31 with symptoms persisting more than 10 years in some women.29, 32
The precise mechanism of vasomotor symptoms is poorly understood, but is hypothesized to result from disturbance of the temperature-regulating system in the hypothalamus, triggered by a decline in E2.28 Vasomotor symptoms may occur at any time, and usually begin with sensations of heat or warmth in the upper body, associated with peripheral vasodilation, sweating, and elevated skin blood flow.33 Vasomotor symptoms are proposed to be triggered by small elevations in core body temperature acting within a narrowed thermoneutral zone.33 The duration of a flash usually ranges from one to five minutes, but some flashes last up to 60 minutes.28, 33
Self-reported vasomotor symptoms are consistently associated with poorer self-reported sleep quality and chronic insomnia.10, 14, 34, 35 Longitudinal SWAN data show that women with moderate-severe hot flashes are almost three times more likely to report frequent nocturnal awakenings compared to women without hot flashes.36 Studies that investigated relationships between reported vasomotor symptoms and objectively measured sleep (with actigraphy or PSG) have produced conflicting results, with early studies showing no relationship12, 22 and more recent studies finding an association between hot flashes and disrupted sleep.37-39
Vasomotor symptoms can be measured objectively using sternal skin conductance.40 Objectively detected vasomotor symptoms have been linked to sleep disruption in some,37, 38, 41, 42 but not all studies. 22, 39, 43 Differences between studies might relate to the classification of hot flashes in association with awakenings,37 as well as between-women variability in the impact of hot flashes on sleep. In an experimental model of new-onset hot flashes in young pre-menopausal women treated with a gonadotropin-releasing hormone agonist that simulates menopause, hot flashes were linked with more PSG awakenings, more WASO, and more Stage 1 sleep.44 Thus, these data provide support for a link between hot flashes and disturbed sleep. In an analysis of the overall impact of hot flashes on sleep architecture, de Zambotti and colleagues reported that wake time attributed to hot flashes was responsible for, on average, 27% of objective WASO, although there was wide variability in hot flash impact between women.37 They also reported that an awakening occurred coincident with the majority (69%) of hot flashes.
In summary, while not all hot flashes are associated with disturbed sleep, they are a strong correlate of poor sleep, and many nocturnal hot flash events are closely linked with periods of PSG-wake. The strong overlap in timing between hot flash onset and awakenings suggests that these events may be driven by a common mechanism within the central nervous system in response to fluctuating estrogen levels, although sweating triggered by a hot flash may still contribute to, or extend, the interval of waking.37 Nocturnal hot flashes are an important component of sleep disturbance during midlife, particularly in women with severe sleep difficulties that qualifies them for insomnia disorder, as discussed later. However, not all women who have menopause-related sleep problems complain of hot flashes41 and it is important to consider other factors that could disturb sleep, including the presence of sleep-disordered breathing (SDB), mood disturbances, medical conditions, and socioeconomic factors (See Figure 2). Importantly, several of these factors may interact with each other, making it challenging to determine the primary cause of sleep disturbance.
Figure 2.
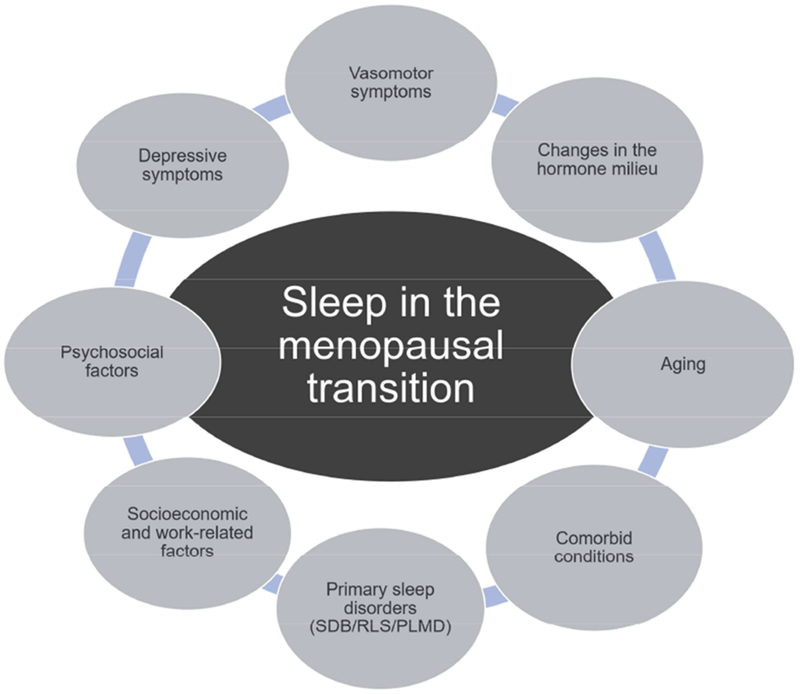
Many factors are associated with sleep disturbances in the context of the menopausal transition. Some factors may also interact to worsen sleep quality. SDB, sleep-disordered breathing; PLMD, periodic limb movement disorder; RLS, restless legs syndrome.
DEPRESSION AND SLEEP DISTURBANCE IN MENOPAUSAL TRANSITION
Risk for depression increases during the menopausal transition, independently of other factors.45-48 In SWAN, women were two to four times more likely to develop major depressive disorder in menopausal transition and early post-menopause compared to pre-menopause, after adjusting for confounding factors.46 It is hypothesized that fluctuation and an eventual drop in estrogen is responsible for impaired mood49, 50 and women vulnerable to developing mood symptoms during other reproductive transitions (e.g. pre-menstrual phase of the menstrual cycle or postpartum) are at greater risk for developing depressive symptoms in menopausal transition.51
There is a bi-directional relationship between mood and sleep disturbances.52, 53 The relationship between depressive symptoms and subjective sleep disturbances has also been documented in women in the menopausal transition.54-56 In a longitudinal analysis of 309 women transitioning menopause, Avis and colleagues reported that depressive symptoms were unrelated to menopausal status or annual change in E2, but were associated with hot flashes and sleep disturbance.57 Further, in a longitudinal analysis of SWAN data, Bromberger and colleagues found that the presence of subjective sleep problems at baseline was a significant predictor of persistent/recurrent major depressive disorder at follow-up.58
Researchers have also investigated the association of sleep architecture with depressive symptoms, although findings are conflicting. In one study, more depressive symptoms were associated with lower sleep efficiency and shorter TST in peri-menopausal women, and with a higher percentage of REM sleep in post-menopausal women.56 In contrast, a substudy of SWAN found that mood symptoms were not independently related to sleep architecture; anxiety symptoms were related to longer sleep onset latency and lower sleep efficiency; however, this was found only in women who also reported vasomotor symptoms.59
The “domino theory,” which predicts that vasomotor symptoms lead to insomnia, which then leads to the development of mood symptoms,60 currently has only partial support.1 Recent data showed that hot flashes and depressive symptoms were associated with different sleep disturbance patterns; hot flashes being uniquely associated with frequent awakenings and depression uniquely associated with difficulty falling asleep and waking up earlier than desired.61 Further, an intervention study of peri-menopausal women with depressive symptoms found that, in adjusted models, improvement in depression was predicted by improved sleep and increasing E2, but not by reduction of vasomotor symptoms.62 Therefore, the causal directionality between these factors in relation to the decline in ovarian function in the approach to menopause still needs to be clarified.
SLEEP DISORDERS IN THE MENOPAUSAL TRANSITION
Insomnia Disorder
While epidemiological studies show a clear increase in poor sleep quality as women enter menopause, the severity and persistence of poor sleep, as well as the extent of impairment in daytime function, varies between women. Insomnia disorder is the most severe clinical manifestation of recurrent and chronic perceived poor sleep (difficulty falling asleep and staying asleep despite adequate opportunity to sleep), occurring three or more times per week and causing significant distress and daytime consequences. In the context of menopause, classic clinical features of insomnia such as rumination, anxiety, and generalized hyperarousal63, 64 overlap with aspects of insomnia specific to menopause, such as vasomotor symptoms.
Based on a structured phone interview of almost 1000 women, Ohayon and colleagues reported that 26% of peri-menopausal women qualified for a DSM-IV diagnosis of insomnia, with difficulty maintaining sleep the most common symptom.35 The likelihood of having chronic insomnia symptoms increased with the severity of hot flashes.35 Other factors that are associated with increased risk for insomnia disorder in the context of the menopausal transition include personality factors such as neuroticism, past depression, a history of severe premenstrual symptoms, and chronic stress.65-67
There are limited data on PSG measures for insomnia disorder in the menopausal transition. One study found significant objective sleep disruption, with shorter TST, more WASO, and poorer sleep efficiency; the disruption matching subjective reports of poor sleep quality in this group relative to women without insomnia who were also in menopausal transition.68 In fact, almost 50% of the insomnia group had short sleep duration (<6 hours). These data matched sleep diary data collected over a 2-week period.68 Women with insomnia were more likely to have objectively measured hot flashes, and the presence of hot flashes predicted the number of PSG-awakenings per hour of sleep.68 While data were only available from one study, findings suggest that in cases of severe subjective sleep disturbance qualifying for insomnia disorder, there is PSG evidence of poor sleep that is partly attributed to the impact of hot flashes.
In another study Xu and colleagues69 compared subjective and PSG measures in pre-, peri/post-menopausal women with insomnia. While subjective measures of sleep disturbance and depression were similar between groups, peri/post-menopausal women had a longer PSG-defined total wake time and lower sleep efficiency, suggesting that PSG measures of sleep quality are impacted to a greater extent in peri/post-menopausal than in pre-menopausal women with insomnia. The presence of hot flashes was not evaluated in this study.
The links between insomnia disorder and adverse mental and physical conditions, including depression and cardiovascular disease, are well established,70 and insomnia combined with short sleep duration is proposed as the most biologically severe phenotype of the disorder.71 It is unclear if insomnia disorder that develops in the context of the menopausal transition has a similar impact on long-term health compared with insomnia that develops in other circumstances, and how comorbid features, such as hot flashes or depression, might interact with sleep difficulties to contribute to impairment. Emerging data show an association between menopausal insomnia and unfavorable nocturnal blood pressure72 and heart rate73 profiles, however, the causes and long-term consequences of this altered blood pressure profile remain to be determined.
Primary Sleep Disorders and Other Medical Disorders
Sleep disturbances may arise during the menopausal transition and post-menopause in association with primary sleep disorders, such as SDB, restless legs syndrome (RLS), and periodic limb movement disorder (PLMD).2, 74
Sleep disordered breathing
SDB is characterized by snoring, upper airway obstruction, inspiratory flow limitation, and excessive daytime sleepiness.75 An apnea hypopnea index (AHI) of five or more per hour of sleep is usually considered abnormal and indicates SDB.75 The prevalence of SDB is higher in men than in women before menopause,76 however, the prevalence increases in women following menopausal transition.77-81
In the Wisconsin Sleep Cohort, post-menopausal women were 2.6 times more likely to have an AHI ≥ 5 per hour and 3.5 times more likely to have an AHI ≥ 15 per hour, compared with pre-menopausal women, after adjusting for confounding factors (age, BMI, and smoking).80 In the recent longitudinal analyses of that dataset, AHI increased from pre-menopause to peri- and post-menopause, independent of age and changes in body habitus, although these factors were also associated with AHI.77 The greater prevalence of SDB after menopause might be due in part to loss of protective effects of female reproductive steroid hormones, especially progesterone,80, 81 as well as changes in fat distribution after menopause.78
The clinical picture of SDB in women usually differs from that of men. Women are more symptomatic with lower AHI compared to men, and they have more prolonged partial upper airway obstruction, and report insomnia as a symptom of SDB more frequently.82, 83 Of importance, patients with SDB and insomnia-like symptoms have higher burden of cardiovascular, pulmonary and psychiatric comorbidity compared to patients with traditional sleepy phenotype despite less severe SDB in terms of AHI.83 Further, patients with SDB and insomnia symptoms have lower adherence to continuous positive airway pressure treatment83, 84 and may benefit from concomitant cognitive behavioral therapy for insomnia (CBT-I).85 Perhaps as a consequence of these differences in clinical presentation, women with SDB are more often underdiagnosed, as well as undertreated compared to men.86
Restless legs syndrome (RLS) and periodic limb movement disorder (PLMD)
The prevalence of RLS and PLMD increases with age, and RLS is more common in women.87 Freedman and colleagues found periodic limb movements and apneas to be the best predictors for poorer sleep efficiency in peri- and post-menopausal women reporting sleep disturbances.43 However, in a group of asymptomatic post-menopausal women, the incidence of periodic limb movements was unrelated to E2 or FSH levels,88 suggesting that the increase in prevalence of RLS and PLMD after menopause may be related more to aging than to hormonal changes.
Other medical disorders and use of medications
In addition to primary sleep disorders, other medical disorders, as well as use of medications, become more common with advancing age and may affect sleep in midlife women.89-91 In one of the few prospective studies assessing predictors for menopausal sleep disturbances, medical diseases and use of prescribed medication predicted future sleep disturbances.92 In another prospective study depressive symptoms, personal crises, use of medications affecting the CNS and perceived impaired general health already five years before menopause predicted various sleep disturbances in menopausal transition.67
DEMOGRAPHIC AND PSYCHO-SOCIAL FACTORS AND SLEEP IN MENOPAUSAL TRANSITION
Women face multiple challenges and personal life stressors in midlife, including changing family roles, loss of significant others, changes and increasing demands at work, and health concerns and worries about retiring and getting old.93 Peri-menopausal women have higher levels of psychological distress compared to pre-menopausal women94 and employment, depressed mood, and poor perceived health are among the most significant factors causing stress in midlife women.95 Life stressors and experiencing stress could contribute to sleep disturbances.93, 96, 97 Indeed, perceived stress and poor perceived health have been associated with sleep disturbances in midlife women.16, 90 Further, Hall and colleagues66 found that midlife women with more chronic stress exposure over a 9-year period had greater PSG-assessed WASO and were more likely to have insomnia at follow-up than participants with moderate stress exposure.
A limited number of studies have investigated the relationship between work stresses specifically and menopausal symptoms including sleep disturbances. An Australian study of 476 peri- and post-menopausal women working in the higher education sector found that higher supervisor support, being employed on a full-time basis, and having control over workplace temperature were independently associated with lower menopausal symptom reporting.98 This study did not specifically assess sleep disturbances. However, there is good evidence that job strain and high work demands are associated with increased prevalence of sleep disturbances in the general population.99-101 A recent Finnish prospective study with over 24,000 participants (82% women, mean age 44 years) showed that the disappearance of job strain was associated with lower odds of insomnia symptoms.101 In addition, according to a sleep diary study, post-menopausal women had worse sleep than pre-menopausal women during working days, but few differences during leisure days, showing an existing coping mechanism of work stress after menopause and the necessity of enough rest.102
Some socioeconomic factors are protective against the development of sleep disturbances in the menopausal transition; higher educational level,34 lower financial strain,103 and satisfactory marriage104, 105 are all associated with less sleep disturbance. Further, the prevalence of menopausal sleep disturbance is influenced by race and ethnicity: Caucasian women have higher rates while Hispanic women have lower rates of sleep disturbance.14
There is a bi-directional relationship between psychosocial factors and menopausal symptoms, including sleep disturbance. Just as psychological distress, stressors, and poor health can lead to sleep disturbances, sleep disturbances can also lead to poorer health and quality of life, depressed mood, and reduced work productivity. For example, in a study of 131 Egyptian teachers in the menopausal transition (aged 46–59 years), the most important menopausal symptoms that affected their work capacity and performance were tiredness (83%) and sleep disturbances (64%).106 A larger study of 961 midlife women found that insomnia symptoms were the most problematic menopausal symptoms to affect daily life and working performance.107
Recent studies have demonstrated that the presence of menopausal symptoms increases health care utilization and costs, as well as sick leave days.3, 108-110 In one study that assessed the burden of menopausal sleep disturbances on societal costs, Bolge and colleagues concluded that menopausal chronic insomnia, characterized by nighttime awakenings, was linked with increased health care utilization and associated costs, decreased work productivity, and decreased health-related quality of life after adjustment for demographics and comorbidity.3
MANAGEMENT OF SLEEP DISTURBANCES IN THE CONTEXT OF MENOPAUSE
As discussed in the above sections, there are potentially multiple, and sometimes overlapping, causes of sleep disturbances in midlife women as they approach and pass menopause. For some women, the sleep disturbances may be transient and without associated distress and therefore not require active treatment. However, others may experience severe sleep disturbances with a significant impact on functioning and quality of life, necessitating treatment. In some cases, combined treatments may be required, such as for women who have depression in addition to severe vasomotor symptoms and sleep problems.
During evaluation of sleep problems with a sleep history assessment111 or sleep diary,112 women should be questioned about the timing of sleep difficulties in relation to menopausal symptoms, changes in bleeding patterns, and presence and severity of menopausal symptoms like hot flashes and night sweats, in addition to screening for sleep breathing and movement disorders. Treatment options include hormone therapy (HT), non-hormonal pharmacological medications, non-pharmacological and self-management strategies.
Cognitive-behavioral treatment of insomnia
Cognitive-behavioral treatment of insomnia (CBT-I) is considered the primary intervention for patients with chronic insomnia,113 and is superior to sleep medication alone in the long-term.114 CBT-I has recently been evaluated for insomnia during the menopausal transition in a randomized clinical trial of peri- and post-menopausal women with insomnia symptoms as well as daily hot flashes.115 Compared to a menopause education control condition, 8-weeks of CBT-I led to a greater reduction in insomnia symptoms, with improvements maintained at 6 months post-treatment.115 Preliminary data from an open trial of CBT-I in women with menopausal sleep problems also indicated a reduction in insomnia (and depression) symptoms post-treatment.116 While further trials are needed, initial findings provide support for effectiveness of CBT-I in women with insomnia during the menopausal transition.
Other non-pharmacological approaches for treating menopausal insomnia, including acupuncture, yoga, massage, exercise and nutritional supplements containing soy isoflavones have been tried, with mixed effects (reviewed in Attarian, 2015).
Hormone Therapy (HT) and Sleep
HT, comprised of estrogen combined with progestin, or estrogen alone for women with a history of hysterectomy, is the most effective treatment for menopausal symptoms.117 HT has other beneficial effects, including prevention of bone loss and osteoporosis-related fractures.118, 119 However, HT may also have negative effects. Oral (but not transdermal) administration of HT increases the risk for venous thromboembolism.118, 120 In addition, there is a slightly elevated risk for breast cancer that seems to be primarily, but not exclusively, related to the progestin used in combined therapy.118, 121, 122 According to current opinion, therefore, the indications and possible contraindications (e.g. history of breast or gynecological cancer, venous thromboembolism, or severe cardiovascular diseases) should be evaluated before initiating HT. HT should be considered when the balance of potential benefits and risks is favorable for a woman123 at the lowest effective dose, using transdermal administration when appropriate. The duration should be individualized based on duration of menopausal symptoms, age, and possible risk factors.118
Several studies have evaluated the effect of HT on sleep, however, findings are mixed and difficult to compare, given the heterogeneity in study populations, tools to evaluate sleep, and various HT preparations (formulation, dose and type of administration). According to a recent meta-analysis, HT modestly improves subjectively evaluated sleep disturbance.124 In most studies, improved sleep quality has co-occurred with improvement in vasomotor symptom.124-128 However, there are also data on enhanced sleep quality with HT without the report of vasomotor symptoms.126 PSG studies examining the effect of HT on sleep architecture in menopausal women share the same problems with study design as the studies evaluating subjective sleep quality and HT. Those studies are rare, and their results are conflicting. Some studies have observed positive changes in sleep architecture with HT,129-132 mainly decreasing WASO, although other studies found no improvement.133-135
In cases where HT is contra-indicated or not preferred, non-hormonal pharmacological options for treating hot flashes and associated insomnia symptoms are available.136 Low-dose selective serotonin/serotonin norepinephrine reuptake inhibitors reduce hot flashes to some extent and modestly reduce insomnia symptoms in women with hot flashes,137-139 although the adverse-effect profiles of these medications need to be carefully considered before use. Evidence from a single trial shows that gabapentin improves sleep quality in peri-menopausal women with hot flashes and insomnia.140
CONCLUSION
Sleep difficulties increase as women approach menopause. For some women, sleep problems are severe and thus impact daytime functioning and quality of life, having long-term consequences for mental and physical health. Menopausal vasomotor symptoms typically interfere with sleep, and are strongly associated with self-reports of sleep disturbances as well as PSG-measured wakefulness. However, when evaluating the causes of sleep disturbance during menopause other factors directly related to the menopausal transition (e.g., instability/changes in the hormone environment with progressive decreases in estradiol and increases in FSH) and factors coincident with the transition (e.g., SDB or movement disorders, mood disturbance, presence of medical conditions, or life stressors) also need to be considered. Given the presence of unique sleep-disruptive factors (e.g., hot flashes) and the multifactorial nature of sleep difficulties in women approaching menopause, often with many interacting factors, treatment options need to be tailored to the individual woman.
KEY POINTS.
There is an increase in self-reported sleep disturbance, particularly nocturnal awakenings, across the menopausal transition. Symptoms are bothersome and impact quality of life, health, and productivity.
Vasomotor symptoms, both self-reported and measured hot flashes and sweating, are critical symptoms associated with disrupted sleep in the menopausal transition.
Associations between menopausal stage and/or hormone levels and polysomnographic (PSG) measures are less consistent and further longitudinal studies are required.
Sleep disturbances may arise during the menopausal transition in association with primary sleep disorders (e.g. sleep-disordered breathing). Women with sleep complaints should be evaluated and appropriately treated.
Effective management strategies for menopausal sleep disturbances include hormone therapy, other pharmacological treatments (e.g. gabapentin), and cognitive behavioral therapy for insomnia.
SYNOPSIS.
The menopausal transition is associated with an increase in insomnia symptoms, especially difficulty staying asleep, which negatively impacts quality of life. Vasomotor symptoms are a key component of sleep disruption. Findings from polysomnographic studies are less consistent in showing disrupted sleep in the menopausal transition independent of aging; further prospective studies are needed. Hormone therapy alleviates subjective sleep disturbances, particularly if vasomotor symptoms are present. However, due to contraindications, other options, including cognitive behavioral therapy for insomnia, should be considered. Further work is needed to develop preventive and treatment strategies for alleviating sleep disturbances to ensure better health, quality of life, and productivity in midlife women.
Acknowledgments
This work is supported by National Institutes of Health, Grant HL103688 (FCB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. FCB has received funding unrelated to this work from Ebb Therapeutics Inc., Fitbit Inc., and International Flavors & Fragrances Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE STATEMENT
Other authors have nothing to disclose.
REFERENCES
- 1.Shaver JL, Woods NF. Sleep and menopause: a narrative review. Menopause. 2015;22(8):899–915. [DOI] [PubMed] [Google Scholar]
- 2.Polo-Kantola P. Sleep problems in midlife and beyond. Maturitas. 2011;68(3):224–232. [DOI] [PubMed] [Google Scholar]
- 3.Bolge SC, Balkrishnan R, Kannan H, Seal B, Drake CL. Burden associated with chronic sleep maintenance insomnia characterized by nighttime awakenings among women with menopausal symptoms. Menopause. 2010;17(1):80–86. [DOI] [PubMed] [Google Scholar]
- 4.Luoto R, Kaprio J, Uutela A. Age at natural menopause and sociodemographic status in Finland. Am J Epidemiol. 1994;139(1):64–76. [DOI] [PubMed] [Google Scholar]
- 5.Roberts H, Hickey M. Managing the menopause: An update. Maturitas. 2016;86:53–58. [DOI] [PubMed] [Google Scholar]
- 6.Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012;97(4):1159–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson HD. Menopause. Lancet. 2008;371(9614):760–770. [DOI] [PubMed] [Google Scholar]
- 8.Cheng MH, Hsu CY, Wang SJ, Lee SJ, Wang PH, Fuh JL. The relationship of self-reported sleep disturbance, mood, and menopause in a community study. Menopause. 2008;15(5):958–962. [DOI] [PubMed] [Google Scholar]
- 9.Hung HC, Lu FH, Ou HY, Wu JS, Yang YC, Chang CJ. Menopause is associated with self-reported poor sleep quality in women without vasomotor symptoms. Menopause. 2014;21(8):834–839. [DOI] [PubMed] [Google Scholar]
- 10.Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause. 2003;10(1):19–28. [DOI] [PubMed] [Google Scholar]
- 11.Shin C, Lee S, Lee T, et al. Prevalence of insomnia and its relationship to menopausal status in middle-aged Korean women. Psychiatry Clin Neurosci. 2005;59(4):395–402. [DOI] [PubMed] [Google Scholar]
- 12.Young T, Rabago D, Zgierska A, Austin D, Laurel F. Objective and subjective sleep quality in premenopausal, perimenopausal, and postmenopausal women in the Wisconsin Sleep Cohort Study. Sleep. 2003;26(6):667–672. [DOI] [PubMed] [Google Scholar]
- 13.Berecki-Gisolf J, Begum N, Dobson AJ. Symptoms reported by women in midlife: menopausal transition or aging?. Menopause. 2009;16(5):1021–1029. [DOI] [PubMed] [Google Scholar]
- 14.Kravitz HM, Zhao X, Bromberger JT, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31(7):979–990. [PMC free article] [PubMed] [Google Scholar]
- 15.Tom SE, Kuh D, Guralnik JM, Mishra GD. Self-reported sleep difficulty during the menopausal transition: results from a prospective cohort study. Menopause. 2010;17(6):1128–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woods NF, Mitchell ES. Sleep symptoms during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Sleep. 2010;33(4):539–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu Q, Lang CP. Examining the relationship between subjective sleep disturbance and menopause: a systematic review and meta-analysis. Menopause. 2014;21(12):1301–1318. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan KA, Hardas PP, Redline S, Zeitzer JM, Sleep Heart Health Study Research Group. Correlates of sleep quality in midlife and beyond: a machine learning analysis. Sleep Med. 2017;34:162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9 Suppl 1:S10–7. [DOI] [PubMed] [Google Scholar]
- 20.Hachul H, Frange C, Bezerra AG, et al. The effect of menopause on objective sleep parameters: data from an epidemiologic study in Sao Paulo, Brazil. Maturitas. 2015;80(2):170–178. [DOI] [PubMed] [Google Scholar]
- 21.Campbell IG, Bromberger JT, Buysse DJ, et al. Evaluation of the association of menopausal status with delta and beta EEG activity during sleep. Sleep. 2011;34(11):1561–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freedman RR, Roehrs TA. Lack of sleep disturbance from menopausal hot flashes. Fertil Steril. 2004;82(1):138–144. [DOI] [PubMed] [Google Scholar]
- 23.Kalleinen N, Polo-Kantola P, Himanen SL, et al. Sleep and the menopause - do postmenopausal women experience worse sleep than premenopausal women?. Menopause Int. 2008;14(3):97–104. [DOI] [PubMed] [Google Scholar]
- 24.Lampio L, Polo-Kantola P, Himanen SL, et al. Sleep during menopausal transition: A six-year follow-up. Sleep. 2017. [DOI] [PubMed] [Google Scholar]
- 25.Sowers MF, Zheng H, Kravitz HM, et al. Sex steroid hormone profiles are related to sleep measures from polysomnography and the Pittsburgh Sleep Quality Index. Sleep. 2008;31(10):1339–1349. [PMC free article] [PubMed] [Google Scholar]
- 26.de Zambotti M, Colrain IM, Baker FC. Interaction between reproductive hormones and physiological sleep in women. J Clin Endocrinol Metab. 2015;100(4):1426–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Antonijevic IA, Murck H, Frieboes RM, Uhr M, Steiger A. On the role of menopause for sleep-endocrine alterations associated with major depression. Psychoneuroendocrinology. 2003;28(3):401–418. [DOI] [PubMed] [Google Scholar]
- 28.Archer DF, Sturdee DW, Baber R, et al. Menopausal hot flushes and night sweats: where are we now?. Climacteric. 2011;14(5):515–528. [DOI] [PubMed] [Google Scholar]
- 29.Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mishra GD, Kuh D. Health symptoms during midlife in relation to menopausal transition: British prospective cohort study. BMJ. 2012;344:e402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tepper PG, Brooks MM, Randolph JF Jr, et al. Characterizing the trajectories of vasomotor symptoms across the menopausal transition. Menopause. 2016;23(10):1067–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freeman EW, Sammel MD, Lin H, Liu Z, Gracia CR. Duration of menopausal hot flushes and associated risk factors. Obstet Gynecol. 2011;117(5):1095–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freedman RR. Menopausal hot flashes: mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol. 2014;142:115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blümel JE, Cano A, Mezones-Holguin E, et al. A multinational study of sleep disorders during female mid-life. Maturitas. 2012;72(4):359–366. [DOI] [PubMed] [Google Scholar]
- 35.Ohayon MM. Severe hot flashes are associated with chronic insomnia. Arch Intern Med. 2006;166(12):1262–1268. [DOI] [PubMed] [Google Scholar]
- 36.Kravitz HM, Joffe H. Sleep during the perimenopause: a SWAN story. Obstet Gynecol Clin North Am. 2011;38(3):567–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Zambotti M, Colrain IM, Javitz HS, Baker FC. Magnitude of the impact of hot flashes on sleep in perimenopausal women. Fertil Steril. 2014;102(6):1708–15. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joffe H, White DP, Crawford SL, et al. Adverse effects of induced hot flashes on objectively recorded and subjectively reported sleep: results of a gonadotropin-releasing hormone agonist experimental protocol. Menopause. 2013;20(9):905–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thurston RC, Santoro N, Matthews KA. Are vasomotor symptoms associated with sleep characteristics among symptomatic midlife women? Comparisons of self-report and objective measures. Menopause. 2012;19(7):742–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mann E, Hunter MS. Concordance between self-reported and sternal skin conductance measures of hot flushes in symptomatic perimenopausal and postmenopausal women: a systematic review. Menopause. 2011;18(6):709–722. [DOI] [PubMed] [Google Scholar]
- 41.Joffe H, Massler A, Sharkey KM. Evaluation and management of sleep disturbance during the menopause transition. Semin Reprod Med. 2010;28(5):404–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savard MH, Savard J, Caplette-Gingras A, Ivers H, Bastien C. Relationship between objectively recorded hot flashes and sleep disturbances among breast cancer patients: investigating hot flash characteristics other than frequency. Menopause. 2013;20(10):997–1005. [DOI] [PubMed] [Google Scholar]
- 43.Freedman RR, Roehrs TA. Sleep disturbance in menopause. Menopause. 2007;14(5):826–829. [DOI] [PubMed] [Google Scholar]
- 44.Joffe H, Crawford S, Economou N, et al. A gonadotropin-releasing hormone agonist model demonstrates that nocturnal hot flashes interrupt objective sleep. Sleep. 2013;36(12):1977–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bromberger JT, Matthews KA, Schott LL, et al. Depressive symptoms during the menopausal transition: the Study of Women’s Health Across the Nation (SWAN). J Affect Disord. 2007;103(1-3):267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bromberger JT, Kravitz HM. Mood and menopause: findings from the Study of Women’s Health Across the Nation (SWAN) over 10 years. Obstet Gynecol Clin North Am. 2011;38(3):609–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385–390. [DOI] [PubMed] [Google Scholar]
- 48.Steinberg EM, Rubinow DR, Bartko JJ, et al. A cross-sectional evaluation of perimenopausal depression. J Clin Psychiatry. 2008;69(6):973–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Soares CN. Mood disorders in midlife women: understanding the critical window and its clinical implications. Menopause. 2014;21(2):198–206. [DOI] [PubMed] [Google Scholar]
- 50.Borrow AP, Cameron NM. Estrogenic mediation of serotonergic and neurotrophic systems: implications for female mood disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2014;54:13–25. [DOI] [PubMed] [Google Scholar]
- 51.Studd JW. A guide to the treatment of depression in women by estrogens. Climacteric. 2011;14(6):637–642. [DOI] [PubMed] [Google Scholar]
- 52.Kahn M, Sheppes G, Sadeh A. Sleep and emotions: bidirectional links and underlying mechanisms. Int J Psychophysiol. 2013;89(2):218–228. [DOI] [PubMed] [Google Scholar]
- 53.Sivertsen B, Salo P, Mykletun A, et al. The bidirectional association between depression and insomnia: the HUNT study. Psychosom Med. 2012;74(7):758–765. [DOI] [PubMed] [Google Scholar]
- 54.Burleson MH, Todd M, Trevathan WR. Daily vasomotor symptoms, sleep problems, and mood: using daily data to evaluate the domino hypothesis in middle-aged women. Menopause. 2010;17(1):87–95. [DOI] [PubMed] [Google Scholar]
- 55.Pien GW, Sammel MD, Freeman EW, Lin H, DeBlasis TL. Predictors of sleep quality in women in the menopausal transition. Sleep. 2008;31(7):991–999. [PMC free article] [PubMed] [Google Scholar]
- 56.Toffol E, Kalleinen N, Urrila AS, et al. The relationship between mood and sleep in different female reproductive states. BMC Psychiatry. 2014;14:177-244X-14-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Avis NE, Crawford S, Stellato R, Longcope C. Longitudinal study of hormone levels and depression among women transitioning through menopause. Climacteric. 2001;4(3):243–249. [PubMed] [Google Scholar]
- 58.Bromberger JT, Kravitz HM, Youk A, Schott LL, Joffe H. Patterns of depressive disorders across 13 years and their determinants among midlife women: SWAN mental health study. J Affect Disord. 2016;206:31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kravitz HM, Avery E, Sowers M, et al. Relationships between Menopausal and Mood Symptoms and EEG Sleep Measures in a Multi-ethnic Sample of Middle-Aged Women: The SWAN Sleep Study. Sleep. 2011;34(9):1221–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eichling PS, Sahni J. Menopause related sleep disorders. J Clin Sleep Med. 2005;1(3):291–300. [PubMed] [Google Scholar]
- 61.Vousoura E, Spyropoulou AC, Koundi KL, et al. Vasomotor and depression symptoms may be associated with different sleep disturbance patterns in postmenopausal women. Menopause. 2015. [DOI] [PubMed] [Google Scholar]
- 62.Joffe H, Petrillo LF, Koukopoulos A, et al. Increased estradiol and improved sleep, but not hot flashes, predict enhanced mood during the menopausal transition. J Clin Endocrinol Metab. 2011;96(7):E1044–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14(5):547–558. [DOI] [PubMed] [Google Scholar]
- 64.Shaver JL, Johnston SK, Lentz MJ, Landis CA. Stress exposure, psychological distress, and physiological stress activation in midlife women with insomnia. Psychosom Med. 2002;64(5):793–802. [DOI] [PubMed] [Google Scholar]
- 65.Sassoon SA, de Zambotti M, Colrain IM, Baker FC. Association between personality traits and DSM-IV diagnosis of insomnia in peri- and postmenopausal women. Menopause. 2014;21(6):602–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hall MH, Casement MD, Troxel WM, et al. Chronic Stress is Prospectively Associated with Sleep in Midlife Women: The SWAN Sleep Study. Sleep. 2015;38(10):1645–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lampio L, Saaresranta T, Engblom J, Polo O, Polo-Kantola P. Predictors of sleep disturbance in menopausal transition. Maturitas. 2016;94:137–142. [DOI] [PubMed] [Google Scholar]
- 68.Baker FC, Willoughby AR, Sassoon SA, Colrain IM, de Zambotti M. Insomnia in women approaching menopause: Beyond perception. Psychoneuroendocrinology. 2015;60:96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xu M, Belanger L, Ivers H, Guay B, Zhang J, Morin CM. Comparison of subjective and objective sleep quality in menopausal and non-menopausal women with insomnia. Sleep Med. 2011;12(1):65–69. [DOI] [PubMed] [Google Scholar]
- 70.Buysse DJ. Insomnia. JAMA. 2013;309(7):706–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17(4):241–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Zambotti M, Trinder J, Javitz H, Colrain IM, Baker FC. Altered nocturnal blood pressure profiles in women with insomnia disorder in the menopausal transition. Menopause. 2017;24(3):278–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.de Zambotti M, Trinder J, Colrain IM, Baker FC. Menstrual cycle-related variation in autonomic nervous system functioning in women in the early menopausal transition with and without insomnia disorder. Psychoneuroendocrinology. 2017;75:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guidozzi F. Sleep and sleep disorders in menopausal women. Climacteric. 2013;16(2):214–219. [DOI] [PubMed] [Google Scholar]
- 75.Shneerson JM. Obstructive sleep apnoeas and snoring In: Shneerson JM, ed. Handbook of sleep medicine. 1st ed. Oxford: Blackwell Science; 2000:194–218. [Google Scholar]
- 76.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mirer AG, Young T, Palta M, Benca RM, Rasmuson A, Peppard PE. Sleep-disordered breathing and the menopausal transition among participants in the Sleep in Midlife Women Study. Menopause. 2017;24(2):157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Polesel DN, Hirotsu C, Nozoe KT, et al. Waist circumference and postmenopause stages as the main associated factors for sleep apnea in women: a cross-sectional population-based study. Menopause. 2015;22(8):835–844. [DOI] [PubMed] [Google Scholar]
- 79.Anttalainen U, Saaresranta T, Aittokallio J, et al. Impact of menopause on the manifestation and severity of sleep-disordered breathing. Acta Obstet Gynecol Scand. 2006;85(11):1381–1388. [DOI] [PubMed] [Google Scholar]
- 80.Young T, Finn L, Austin D, Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2003;167(9):1181–1185. [DOI] [PubMed] [Google Scholar]
- 81.Bixler EO, Vgontzas AN, Lin HM, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163(3 Pt 1):608–613. [DOI] [PubMed] [Google Scholar]
- 82.Anttalainen U, Tenhunen M, Rimpilä V, et al. Prolonged partial upper airway obstruction during sleep - an underdiagnosed phenotype of sleep-disordered breathing. Eur Clin Respir J. 2016;3:31806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Saaresranta T, Hedner J, Bonsignore MR, et al. Clinical Phenotypes and Comorbidity in European Sleep Apnoea Patients. PLoS One. 2016;11(10):e0163439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pien GW, Ye L, Keenan BT, et al. Changing Faces of OSA: Treatment Effects by Cluster Designation in the Icelandic Sleep Apnea Cohort. Sleep. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lack L, Sweetman A. Diagnosis and Treatment of Insomnia Comorbid with Obstructive Sleep Apnea. Sleep Med Clin. 2016;11(3):379–388. [DOI] [PubMed] [Google Scholar]
- 86.Lindberg E, Benediktsdottir B, Franklin KA, et al. Women with symptoms of sleep-disordered breathing are less likely to be diagnosed and treated for sleep apnea than men. Sleep Med. 2017;35:17–22. [DOI] [PubMed] [Google Scholar]
- 87.Harmell A, Ancoli-Israel S. Diagnosis and treatment of sleep disorders in older adults In: Avidan AY, ed. Handbook of sleep medicine. 2nd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011:261–273. [Google Scholar]
- 88.Polo-Kantola P, Rauhala E, Erkkola R, Irjala K, Polo O. Estrogen replacement therapy and nocturnal periodic limb movements: a randomized controlled trial. Obstet Gynecol. 2001;97(4):548–554. [DOI] [PubMed] [Google Scholar]
- 89.Polo-Kantola P, Laine A, Aromaa M, et al. A population-based survey of sleep disturbances in middle-aged women--associations with health, health related quality of life and health behavior. Maturitas. 2014;77(3):255–262. [DOI] [PubMed] [Google Scholar]
- 90.Vaari T, Engblom J, Helenius H, Erkkola R, Polo-Kantola P. Survey of sleep problems in 3421 women aged 41-55 years. Menopause Int. 2008;14(2):78–82. [DOI] [PubMed] [Google Scholar]
- 91.Plotkin K. Insomnia caused by medical disorders In: Attarian HP, Schuman C, eds. Clinical handbook of insomnia. 2nd ed. Totowa, N.J.: Humana; 2010:195–208. [Google Scholar]
- 92.Tom SE, Kuh D, Guralnik JM, Mishra GD. Patterns in trouble sleeping among women at mid-life: results from a British prospective cohort study. J Epidemiol Community Health. 2009;63(12):974–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Darling CA, Coccia C, Senatore N. Women in midlife: stress, health and life satisfaction. Stress Health. 2012;28(1):31–40. [DOI] [PubMed] [Google Scholar]
- 94.Bromberger JT, Meyer PM, Kravitz HM, et al. Psychologic distress and natural menopause: a multiethnic community study. Am J Public Health. 2001;91(9):1435–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Woods NF, Mitchell ES, Percival DB, Smith-DiJulio K. Is the menopausal transition stressful? Observations of perceived stress from the Seattle Midlife Women’s Health Study. Menopause. 2009;16(1):90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Saaresranta T, Polo-Kantola P, Polo O. Practical approach to the diagnosis and management of menopausal insomnia In: Attarian HP, Viola-Saltzman, eds. Sleep disorders in women: A guide to practical management. 2nd ed. the Netherlands: Humana press/Springer; 2013:293–324. [Google Scholar]
- 97.Cuadros JL, Fernandez-Alonso AM, Cuadros-Celorrio AM, et al. Perceived stress, insomnia and related factors in women around the menopause. Maturitas. 2012;72(4):367–372. [DOI] [PubMed] [Google Scholar]
- 98.Bariola E, Jack G, Pitts M, Riach K, Sarrel P. Employment conditions and work-related stressors are associated with menopausal symptom reporting among perimenopausal and postmenopausal women. Menopause. 2017;24(3):247–251. [DOI] [PubMed] [Google Scholar]
- 99.Åkerstedt T, Garefelt J, Richter A, et al. Work and Sleep--A Prospective Study of Psychosocial Work Factors, Physical Work Factors, and Work Scheduling. Sleep. 2015;38(7):1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chazelle E, Chastang JF, Niedhammer I. Psychosocial work factors and sleep problems: findings from the French national SIP survey. Int Arch Occup Environ Health. 2016;89(3):485–495. [DOI] [PubMed] [Google Scholar]
- 101.Halonen JI, Lallukka T, Pentti J, et al. Change in Job Strain as a Predictor of Change in Insomnia Symptoms: Analyzing Observational Data as a Non-randomized Pseudo-Trial. Sleep. 2017;40(1): 10.1093/sleep/zsw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lampio L, Saaresranta T, Polo O, Polo-Kantola P. Subjective sleep in premenopausal and postmenopausal women during workdays and leisure days: a sleep diary study. Menopause. 2013;20(6):655–660. [DOI] [PubMed] [Google Scholar]
- 103.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32(1):73–82. [PMC free article] [PubMed] [Google Scholar]
- 104.Troxel WM, Buysse DJ, Matthews KA, et al. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010;33(7):973–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Troxel WM, Buysse DJ, Hall M, Matthews KA. Marital happiness and sleep disturbances in a multi-ethnic sample of middle-aged women. Behav Sleep Med. 2009;7(1):2–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hammam RA, Abbas RA, Hunter MS. Menopause and work--the experience of middle-aged female teaching staff in an Egyptian governmental faculty of medicine. Maturitas. 2012;71(3):294–300. [DOI] [PubMed] [Google Scholar]
- 107.Simon JA, Reape KZ. Understanding the menopausal experiences of professional women. Menopause. 2009;16(1):73–76. [DOI] [PubMed] [Google Scholar]
- 108.Kleinman NL, Rohrbacker NJ, Bushmakin AG, Whiteley J, Lynch WD, Shah SN. Direct and indirect costs of women diagnosed with menopause symptoms. J Occup Environ Med. 2013;55(4):465–470. [DOI] [PubMed] [Google Scholar]
- 109.Whiteley J, DiBonaventura M, Wagner JS, Alvir J, Shah S. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health (Larchmt). 2013;22(11):983–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Whiteley J, Wagner JS, Bushmakin A, Kopenhafer L, Dibonaventura M, Racketa J. Impact of the severity of vasomotor symptoms on health status, resource use, and productivity. Menopause. 2013;20(5):518–524. [DOI] [PubMed] [Google Scholar]
- 111.Morin CM, Espie CA. Insomnia: A clinical guide to assessment and treatment. New York: Kluwer Academic/Plenum Publishers; 2003. [Google Scholar]
- 112.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(2):307–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sivertsen B, Omvik S, Pallesen S, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. 2006;295(24):2851–2858. [DOI] [PubMed] [Google Scholar]
- 115.McCurry SM, Guthrie KA, Morin CM, et al. Telephone-Based Cognitive Behavioral Therapy for Insomnia in Perimenopausal and Postmenopausal Women With Vasomotor Symptoms: A MsFLASH Randomized Clinical Trial. JAMA Intern Med. 2016;176(7):913–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hall MH, Kline CE, Nowakowski S. Insomnia and sleep apnea in midlife women: prevalence and consequences to health and functioning. F1000Prime Rep. 2015;7:63–63. eCollection 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Maclennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database Syst Rev. 2004;(4)(4):CD002978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.de Villiers TJ, Hall JE, Pinkerton JV, et al. Revised global consensus statement on menopausal hormone therapy. Maturitas. 2016;91:153–155. [DOI] [PubMed] [Google Scholar]
- 119.Cauley JA, Robbins J, Chen Z, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA. 2003;290(13):1729–1738. [DOI] [PubMed] [Google Scholar]
- 120.Canonico M, Oger E, Plu-Bureau G, et al. Hormone therapy and venous thromboembolism among postmenopausal women: impact of the route of estrogen administration and progestogens: the ESTHER study. Circulation. 2007;115(7):840–845. [DOI] [PubMed] [Google Scholar]
- 121.Chlebowski RT, Anderson GL. Menopausal hormone therapy and cancer: changing clinical observations of target site specificity. Steroids. 2014;90:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Manson JE, Chlebowski RT, Stefanick ML, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013;310(13):1353–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753. [DOI] [PubMed] [Google Scholar]
- 124.Cintron D, Lipford M, Larrea-Mantilla L, et al. Efficacy of menopausal hormone therapy on sleep quality: systematic review and meta-analysis. Endocrine. 2017;55(3):702–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hays J, Ockene JK, Brunner RL, et al. Effects of estrogen plus progestin on health-related quality of life. N Engl J Med. 2003;348(19):1839–1854. [DOI] [PubMed] [Google Scholar]
- 126.Polo-Kantola P, Erkkola R, Helenius H, Irjala K, Polo O. When does estrogen replacement therapy improve sleep quality?. Am J Obstet Gynecol. 1998;178(5):1002–1009. [DOI] [PubMed] [Google Scholar]
- 127.Savolainen-Peltonen H, Hautamäki H, Tuomikoski P, Ylikorkala O, Mikkola TS. Health-related quality of life in women with or without hot flashes: a randomized placebo-controlled trial with hormone therapy. Menopause. 2014;21(7):732–739. [DOI] [PubMed] [Google Scholar]
- 128.Welton AJ, Vickers MR, Kim J, et al. Health related quality of life after combined hormone replacement therapy: randomised controlled trial. BMJ. 2008;337:a1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Parry BL, Meliska CJ, Martinez LF, et al. Menopause: neuroendocrine changes and hormone replacement therapy. J Am Med Womens Assoc (1972). 2004;59(2):135–145. [PubMed] [Google Scholar]
- 130.Montplaisir J, Lorrain J, Denesle R, Petit D. Sleep in menopause: differential effects of two forms of hormone replacement therapy. Menopause. 2001;8(1):10–16. [DOI] [PubMed] [Google Scholar]
- 131.Polo-Kantola P, Erkkola R, Irjala K, Pullinen S, Virtanen I, Polo O. Effect of short-term transdermal estrogen replacement therapy on sleep: a randomized, double-blind crossover trial in postmenopausal women. Fertil Steril. 1999;71(5):873–880. [DOI] [PubMed] [Google Scholar]
- 132.Scharf MB, McDannold MD, Stover R, Zaretsky N, Berkowitz DV. Effects of estrogen replacement therapy on rates of cyclic alternating patterns and hot-flush events during sleep in postmenopausal women: a pilot study. Clin Ther. 1997;19(2):304–311. [DOI] [PubMed] [Google Scholar]
- 133.Tansupswatdikul P, Chaikittisilpa S, Jaimchariyatam N, Panyakhamlerd K, Jaisamrarn U, Taechakraichana N. Effects of estrogen therapy on postmenopausal sleep quality regardless of vasomotor symptoms: a randomized trial. Climacteric. 2015;18(2):198–204. [DOI] [PubMed] [Google Scholar]
- 134.Kalleinen N, Polo O, Himanen SL, Joutsen A, Polo-Kantola P. The effect of estrogen plus progestin treatment on sleep: a randomized, placebo-controlled, double-blind trial in premenopausal and late postmenopausal women. Climacteric. 2008;11(3):233–243. [DOI] [PubMed] [Google Scholar]
- 135.Purdie DW, Empson JA, Crichton C, Macdonald L. Hormone replacement therapy, sleep quality and psychological wellbeing. Br J Obstet Gynaecol. 1995;102(9):735–739. [DOI] [PubMed] [Google Scholar]
- 136.Attarian H, Hachul H, Guttuso T, Phillips B. Treatment of chronic insomnia disorder in menopause: evaluation of literature. Menopause. 2015;22(6):674–684. [DOI] [PubMed] [Google Scholar]
- 137.Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: a randomized controlled trial. Menopause. 2012;19(8):848–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ensrud KE, Guthrie KA, Hohensee C, et al. Effects of estradiol and venlafaxine on insomnia symptoms and sleep quality in women with hot flashes. Sleep. 2015;38(1):97–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pinkerton JV, Joffe H, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Low-dose paroxetine (7.5 mg) improves sleep in women with vasomotor symptoms associated with menopause. Menopause. 2015;22(1):50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yurcheshen ME, Guttuso T Jr, McDermott M, Holloway RG, Perlis M. Effects of gabapentin on sleep in menopausal women with hot flashes as measured by a Pittsburgh Sleep Quality Index factor scoring model. J Womens Health (Larchmt). 2009;18(9):1355–1360. [DOI] [PubMed] [Google Scholar]
- 141.Brincat M, Studd JW. Menopause--a multi system disease. Baillieres Clin Obstet Gynaecol. 1988;2(2):289–316. [DOI] [PubMed] [Google Scholar]
- 142.Kronenberg F. Hot flashes: epidemiology and physiology. Ann N Y Acad Sci. 1990;592:52–86; discussion 123-33. [DOI] [PubMed] [Google Scholar]
- 143.Erkkola R, Holma P, Järvi T, et al. Transdermal oestrogen replacement therapy in a Finnish population. Maturitas. 1991;13(4):275–281. [DOI] [PubMed] [Google Scholar]
- 144.Gold EB, Sternfeld B, Kelsey JL, et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. Am J Epidemiol. 2000;152(5):463–473. [DOI] [PubMed] [Google Scholar]
- 145.Santoro N. Perimenopause: From Research to Practice. J Womens Health (Larchmt). 2016;25(4):332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]


