Abstract
Background
Increased left ventricular (LV) myocardial stiffness may be associated with impaired LV hemodynamics and incident heart failure (HF). However, an indicator that estimates LV myocardial stiffness easily and non-invasively is lacking. The purpose of this study was to determine whether diastolic wall strain (DWS), an echocardiographic estimator of LV myocardial stiffness, is associated with incident HF in a middle-aged community-based cohort of African Americans.
Methods and results
We investigated associations between DWS and incident HF among 1528 African Americans (mean age 58.5 years, 66% women) with preserved LV ejection fraction (EF ≥50%) and without a history of cardiovascular disease in the Atherosclerosis Risk in Communities Study. Participants with the smallest DWS quintile (more LV myocardial stiffness) had a higher LV mass index, higher relative wall thickness, and lower arterial compliance than those in the larger four DWS quintiles (p < 0.01 for all). Over a mean follow-up of 15.6 years, there were 251 incident HF events (incidence rate: 10.9 per 1000 person-years). After adjustment for traditional risk factors and incident coronary artery disease, both continuous and categorical DWS were independently associated with incident HF (HR 1.21, 95%CI 1.04–1.41 for 0.1 decrease in continuous DWS, p = 0.014, HR 1.40, 95%CI 1.05–1.87 for the smallest DWS quintile vs other combined quintiles, p = 0.022).
Conclusions
DWS was independently associated with an increased risk of incident HF in a community-based cohort of African Americans. DWS could be used as a qualitative estimator of LV myocardial stiffness.
Keywords: Myocardial stiffness, Incident heart failure, Echocardiography
Introduction
Heart failure (HF) is a global public health problem affecting about 26 million people worldwide [1]. Overall, the prognosis for HF has improved over decades due to advances in medical therapies, but 50% of people diagnosed with HF will die within 5 Years [2]. Left ventricular (LV) diastolic function is an important determinant of LV end-diastolic pressure. Previous studies showed that indices of LV diastolic function are associated with incident HF [3,4]. LV myocardial stiffness is one of the components of diastolic function and has been associated with both HF with reduced ejection fraction (HFrEF) and HF with preserved EF (HFpEF) in cross-sectional studies [5,6]. However, there have been no studies to date examining the relationship between LV myocardial stiffness and incident HF mostly due to difficulty evaluating LV myocardial stiffness: evaluating LV myocardial stiffness requires invasive procedures and complicated computations [7].
Diastolic wall strain (DWS) is an indicator that estimates LV myocardial stiffness non-invasively using simple echocardiographic measurements [8]. DWS was developed based on the linear elastic theory, and predicts the impairment of diastolic LV wall thinning reflecting resistance to deformation in the diastolic period [9]. In animal models, DWS was correlated with the LV myocardial stiffness constant which is the gold standard measurement of the LV myocardial stiffness [8]. DWS was lower in HFpEF patients than asymptomatic patients with LV hypertrophy [8]. Furthermore, increase in LV myocardial stiffness assessed by DWS was associated with severe LV concentric remodeling and poor prognosis in HFpEF patients [9].
Racial disparities in the incidence of HF exist: African Americans have a higher incidence of HF than whites, Hispanics, and Asians [10]. Aortic stiffness is one potential mechanism that has been implicated in this racial disparity [11]. The aims of this study were two-fold: (1) to investigate the relationships among DWS, LV structure and function, and arterial stiffness, and (2) to determine whether DWS is associated with incident HF in an African American cohort of the Atherosclerosis Risk in Communities (ARIC) Study.
Methods
Study population
The ARIC Study is a prospective cohort study conducted to investigate the risks of cardiovascular disease (CVD) and atherosclerosis. The ARIC study’s design and methods have been described in detail elsewhere [12]. We used data from the African American cohort from Jackson (“the Jackson cohort”) at visit 3 as baseline because echocardiograms at visit 3 (1993–1995) were available only in the Jackson cohort (n = 2623). We excluded those with past history of CVD including coronary heart disease (CHD), stroke, and heart failure (n = 228), missing information of past history of CVD (n = 43), absence of echo M-mode image (n = 684), insufficient quality of M-mode image (n = 7), reduced LVEF or presence of wall motion abnormality (n = 108), and missing information of covariates (n = 25) (Fig. 1). Thus, a total of 1528 participants were included in the final analyses. Excluded participants were more likely to be older, male sex, had a higher body mass index (BMI), higher prevalence of hypertension, diabetes, and current smoking than those included in the study (Supplementary Table 1). Total cholesterol/high-density lipoprotein (HDL) cholesterol ratio, systolic blood pressure, and heart rate were also higher in excluded participants than included participants. These differences could be attributed to the difference of the prevalence of a history of CVD between included and excluded participants. The ARIC Study protocols were approved by the institutional review boards of each participating center, and informed consent was obtained from each study participant.
Fig.1.
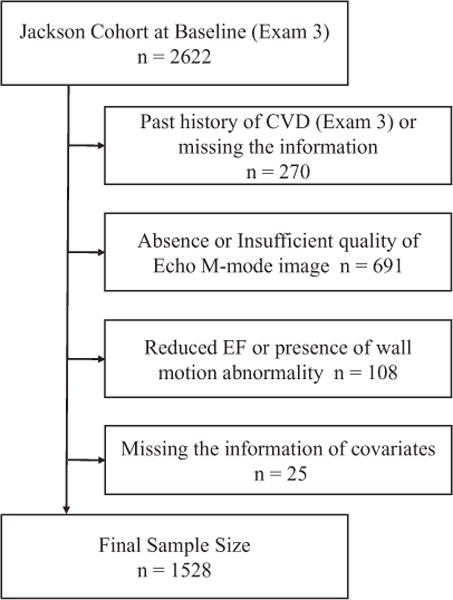
Inclusion and exclusion criteria for this study. CVD, cardiovascular disease; EF, ejection fraction.
Definition of co-morbidities
After a 5-minute rest, three sitting blood pressure measurements were taken with an oscillometric automated sphygmomanometer (Omron HEM-907 XL, Schaumburg, IL, USA); we averaged the last 2 measurements. Pulse pressure was calculated as systolic (SBP) – diastolic blood pressure (DBP). The information of antihypertensive medication use was obtained at visit 3. A diagnosis of hypertension was defined as prescription of antihypertensive medication use, systolic blood pressure ≥140 mmHg, or diastolic blood pressure ≥90 mmHg. BMI was calculated as weight in kilograms divided by the square of height in meters. Blood was drawn after an 8-hour fasting period, and glucose, plasma total cholesterol, and plasma HDL cholesterol levels were measured centrally by standard enzymatic methods. Diabetes was defined as fasting glucose concentration ≥126 mg/dL, non-fasting glucose concentration ≥200 mg/dL, a self-report of a physician’s diagnosis of diabetes or use of oral diabetes medication or insulin. Total cholesterol/HDL ratio was also used as a covariate in this study.
Diastolic wall strain and echocardiography
The quality control measures for echocardiography have been described previously [13]. LV internal dimension and interventricular septal and posterior wall thicknesses were measured at end-diastole and end-systole in 3 cardiac cycles according to the recommendations of the American Society of Echocardiography [14]. We used these variables measured on M-mode image. Calculations of LV mass were made using the following equation as recommended by the American Society of Echocardiography: LV mass index (g/m2) = (0.8*{1.04*[(LVDd + IVSd + PWd)3 − (LVDd)3]} + 0.6)/body surface area [14], where LVDd is left ventricular diastolic dimension, IVSd is interventricular septum thickness at end-diastole, PWd is posterior wall thickness at end-diastole. Relative wall thickness (RWT) was calculated as 2*(PWd)/LVDd. DWS was calculated as (PWs − PWd)/PWs, where PWs is posterior wall thickness at end-systole, and PWd is posterior wall thickness at end-diastole [15]. LVEF was calculated by the Teichholz method. Systemic arterial compliance (SAC) was calculated as stroke volume/pulse pressure. Effective arterial elastance was calculated as 0.9*systolic blood pressure/stroke volume.
Outcomes
To obtain information regarding hospitalizations and other health issues, participants were called annually. Incident HF was the primary outcome of this study. Incident HF was defined by HF hospitalization or HF death, according to the International Classification of Diseases-Ninth Revision (ICD-9) code 410 in any position for HF, obtained by ARIC Study retrospective surveillance of hospital discharges. HF events after 2004 were additionally adjudicated by an expert panel. Our secondary outcome was CHD. Incident CHD was obtained and adjudicated by an endpoints committee and defined as definite or probable myocardial infarction, death from CHD. The follow-up period was the time from the date of echocardiography to the date of the events, or December 31, 2012.
Statistical analysis
Data are presented as mean with standard deviations for normally distributed continuous variables, median with inter-quartile ranges for non-normally distributed continuous variables and frequencies and proportions for categorical variables. DWS was evaluated as a continuous variable as well as a categorical variable. Because of absence of any established ranges or cut points for DWS, clinical and demographic characteristics were examined by quintile of DWS. Thereafter the larger four DWS quintiles (0.282–0.563) were grouped into one category and compared to the smallest DWS quintile (0.055–0.282). Student t-test, Mann–Whitney U test, and chi-squared testing were used for comparison of variables between DWS category groups if applicable. To evaluate the determinant of DWS, correlations between DWS and other echocardiographic parameters were evaluated using Pear-son’s correlation coefficients. For illustrating the effect of DWS on outcomes, Kaplan–Meier curves for cumulative survival free from incident HF were constructed for each DWS group and DWS quintiles, and compared using log-rank tests. Cox proportional hazards models, were used to estimate the hazard ratios (HR) of incident HF or CHD using DWS groups and continuous DWS. The assumption of proportionality was tested using Schoenfeld residuals. No significant deviations from proportionality were observed. Several models were constructed to evaluate associations of DWS with outcomes. Model 1 included adjustment for age and sex, while model 2 additionally included BMI, SBP, use of anti-hypertension medications, ratio of total cholesterol/HDL cholesterol, history of diabetes mellitus, and current smoking status. Model 1 and Model 2 were used for both incident HF and incident CHD. Model 3 included Model 2 plus incident CHD as a time-dependent variable for the purpose to evaluate the influence of incident CHD on incident HF. We additionally included LV mass index (Model 4), LVEF (Model 5), SAC (Model 6), and Ea (Model 7) to Model 3 to evaluate the influence of each variable to the relationship between DWS and incident HF. A relationship between DWS and incident HF was visualized using restricted cubic spline analysis. The analysis was adjusted using multiple covariates (Model 2) and we used 5 knots. Knots were located at the 5%, 25%, 50%, 75%, and 95% percentiles corresponding to values of DWS of 0.202, 0.294, 0.350, 0.402, and 0.474, respectively.
Stratified analyses were then performed to estimate HRs based on age < 60 or ≥60 years, sex, systolic blood pressure < 140 or ≥140 mmHg, hypertension medication use, BMI < 30 or ≥30 kg/m2, ratio of total cholesterol/HDL cholesterol < 3.5 or ≥3.5, diabetes, and current smoking status. In the stratified analyses, we used DWS as a continuous variable. Interaction between these variables and DWS were examined by adding interaction terms in model 2. All statistical analyses were performed with STATA version 14 (STATA Corp, College Station, TX, USA). A 2-sided p-value < 0.05 was considered significant.
Results
Baseline characteristics
Table 1 shows clinical and demographic characteristics of the study cohort based on DWS category groups. The study population was composed of 1528 participants: 66% female, 58% hypertensive, 21% diabetic, 18% current smokers, and a mean age of 59 years. Participants with smallest DWS quintile were older, having higher prevalence of current smokers, and higher systolic blood pressure than larger four DWS quintiles. The prevalence of DM tended to be higher in participants with smallest DWS quintile than in those with larger four DWS quintiles. There were no statistically significant differences in other variables between the DWS category groups. The difference in clinical and demographic characteristics between those with and without incident HF is shown in the supplementary Table 2. Those who developed HF were older, more obese, had a higher prevalence of hypertension and diabetes, had higher total cholesterol/HDL cholesterol ratio, higher prevalence of current smoking, higher systolic and pulse pressure, and higher heart rate than those who did not develop HF.
Table 1.
Baseline characteristics.
| Variables | All participants (n = 1528) |
Larger four DWS quintiles (0.282–0.563) (n = 1223) |
Smallest DWS quintile (0.055–0.282) (n = 305) |
p-Value |
|---|---|---|---|---|
| Age, years | 57 (54, 62) | 57 (53, 62) | 58 (54, 64) | 0.002 |
| Female, n (%) | 1010 (66) | 810 (66) | 200 (66) | 0.828 |
| BM1, kg/m2 | 30.2 ± 6.0 | 30.1 ± 6.0 | 30.2 ± 6.2 | 0.950 |
| Hypertension, n (%) | 890 (58) | 699 (57) | 191 (63) | 0.083 |
| Diabetes, n (%) | 321 (21) | 247 (20) | 74 (24) | 0.119 |
| Tc HDL ratio | 3.8 (3.0, 4.8) | 3.8 (3.0, 4.8) | 3.8 (3.0, 4.7) | 0.836 |
| Current smoker, n (%) | 269 (18) | 201 (16) | 68 (22) | 0.016 |
| Systolic BP, mmHg | 130 ± 20 | 130 ± 20 | 133 ± 22 | 0.039 |
| Diastolic BP, mmHg | 77 ± 11 | 76 ± 10 | 77± 11 | 0.139 |
| Pulse pressure, mmHg | 54 ± 16 | 53 ± 15 | 55 ± 16 | 0.090 |
| Heart rate, bpm | 69 ± 10 | 69 ± 9 | 69 ± 10 | 0.529 |
BMI, body mass index; BP, blood pressure; DWS, diastolic wall strain; HDL, high-density lipoprotein cholesterol; Tc, total cholesterol.
Table 2.
Echocardiographic measurements.
| Variables | All participants (n = 1528) |
Larger four DWS quintiles (0.282–0.563) (n = 1223) |
Smallest DWS quintile (0.055–0.282) (n = 305) |
p-Value |
|---|---|---|---|---|
| LVDd, mm | 46.0 ± 5.5 | 46.3 ± 5.4 | 44.9 ± 5.7 | <0.001 |
| LVDs, mm | 27.8 ± 5.1 | 27.6 ± 5.1 | 28.8 ± 5.1 | <0.001 |
| IVSd, mm | 11.5 ± 2.3 | 11.3 ± 2.1 | 12.6 ± 2.7 | <0.001 |
| IVSs, mm | 15.8 ± 2.8 | 15.7 ± 2.7 | 16.3 ± 3.1 | <0.001 |
| LVPWd, mm | 11.5 ± 2.1 | 11.1 ± 1.8 | 13.1 ± 2.5 | <0.001 |
| LVPWs, mm | 17.7 ± 2.8 | 17.9 ± 2.7 | 16.9 ± 3.1 | <0.001 |
| Relative wall thickness | 0.51 ± 0.12 | 0.49 ± 0.10 | 0.59 ± 0.15 | <0.001 |
| LV mass, g | 248 ± 78 | 240 ± 70 | 281 ± 97 | <0.001 |
| LV mass index, g/m2 | 128 ± 36 | 124 ± 32 | 145 ± 45 | <0.001 |
| LVEF, % | 69.7 ± 8.5 | 70.7 ± 8.2 | 65.4 ± 8.0 | <0.001 |
| Stroke volume, ml | 68.8 ±19.1 | 70.7 ± 19.1 | 61.0 ± 17.1 | <0.001 |
| E wave velocity, cm/s | 77.7 ± 15.8 | 77.5 ±15.7 | 78.7 ± 16.0 | 0233 |
| A wave velocity, cm/s | 76.2 ±18.1 | 76.0 ± 17.8 | 77.3 ± 18.6 | 0271 |
| E/A ratio | 1.06 ± 0.29 | 1.06 ± 0.28 | 1.07 ± 0.29 | 0.834 |
| DWS | 0.347 ± 0.082 | 0.377 ± 0.058 | 0.228 ± 0.046 | N.A. |
| SAC, ml/mmHg | 1.37 ± 0.49 | 1.41 ± 0.50 | 1.18 ± 0.42 | <0.001 |
| Ea, mmHg/ml | 1.84 ± 0.60 | 1.76 ± 0.52 | 2.12 ± 0.77 | <0.001 |
DWS, diastolic wall strain; Ea, effective arterial elastance; IVSd, interventricular septum thickness at end-diastole; IVSs, interventricular septum thickness at end-systole; LVDd, left ventricular diastolic dimension; LVDs, left ventricular systolic dimension; LVEF, left ventricular ejection fraction; LVPWd, left ventricular posterior wall thickness at end-diastole; LVPWs, left ventricular posterior wall thickness at end-systole; SAC, systemic arterial compliance.
Diastolic wall strain and findings of baseline echocardiography
Table 2 shows baseline echocardiographic measurements. Participants with smallest DWS quintile (more LV stiffness) had a more concentric LV hypertrophy than those with the higher four DWS quintiles (LV mass index: smallest DWS quintile 145 ± 45 g/m2 vs larger four DWS quintiles 124 ± 32 g/m2, p < 0.001, RWT: smallest DWS quintile 0.59 ± 0.15 vs larger four DWS quintiles 0.49 ± 0.10, p < 0.001). Participants within the smallest DWS quintile had lower arterial compliance evaluated by SAC (smallest DWS quintile 1.18 ± 0.42 ml/mmHg vs larger four DWS quintiles 1.41 ± 0.50 ml/mmHg, p < 0.001), and a higher arterial load evaluated by Ea (smallest DWS quintile 2.12 ± 0.77 mmHg/ml vs larger four DWS quintiles 1.76 ± 0.52 mmHg/ml, p < 0.001). The correlations between DWS and the other echocardiographic parameters are shown in supplementary Table 3. DWS was significantly correlated with almost all the echocardiographic parameters other than E wave velocity, A wave velocity, and E/A ratio. DWS was moderately correlated with LVPWd and RWT, and mildly correlated with LVEF, stroke volume, and Ea.
Table 3.
Cox proportional hazards models for incident heart failure.
| Model 1
|
Model 2
|
Model 3
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| HRa | 95%CI | p-Value | HR* | 95%CI | p-Value | HR* | 95%CI | p-Value | |
| Continuous DWS | 1.27 | 1.09-1.47 | 0.002 | 1.19 | 1.02-1.38 | 0.024 | 1.21 | 1.04-1.41 | 0.014 |
|
| |||||||||
| Smallest DWS quintile | 1.44 | 1.08-1.92 | 0.013 | 1.35 | 1.01-1.79 | 0.043 | 1.40 | 1.05-1.87 | 0.022 |
Represents HR of 0.1 decrease in continuous DWS and HR of smallest DWS quintile against combined the other quintiles as a reference for incident heart failure. Model 1: adjusted for age and gender, Model 2: Model 1 + body mass index, systolic blood pressure, anti-hypertensive medication use, diabetes, total cholesterol/high-density lipoprotein cholesterol ratio and current smoking status, Model 3: Model 2 + incident coronary heart disease as a time-dependent variable.
CI, confidence interval; DWS, diastolic wall strain; HR, hazard ratio.
The difference in baseline echocardiographic findings between those with and without incident HF is shown in supplementary Table 4. Those who developed HF had larger LV internal dimension, increased LV wall thickness, higher relative wall thickness, larger LV mass and LV mass index, lower E/A ratio, lower DWS, lower SAC, and higher Ea than those who did not develop HF. LVEF was not different between those with and without incident HF.
Table 4.
Cox proportional hazards models for incident coronary heart disease.
| Model 1
|
Model 2
|
|||||
|---|---|---|---|---|---|---|
| HRa | 95%CI | p-Value | HR* | 95%CI | p-Value | |
| Continuous DWS | 1.53 | 1.11-1.65 | 0.002 | 1.28 | 1.05-1.55 | 0.014 |
|
| ||||||
| Smallest DWS quintile | 1.53 | 1.05-2.23 | 0.026 | 1.36 | 0.93-1.99 | 0.110 |
Represents HR of 0.1 decrease in continuous DWS and HR of smallest DWS quintile against combined the other quintiles as a reference for incident heart failure. Model 1: adjusted for age and gender; Model 2: Model 1 + body mass index, systolic blood pressure, anti-hypertensive medication use, diabetes, total cholesterol/high-density lipoprotein cholesterol ratio and current smoking status.
CI, confidence interval; DWS, diastolic wall strain; HR, hazard ratio.
Diastolic wall strain and incident heart failure
Over a mean follow-up of 15.6 years, there were 251 HF events (incidence rate: 10.9 per 1000 person-years). Table 3 shows HRs and 95% confidence intervals (CI) of incident HF based on both continuous as well as categorical DWS. DWS was associated with incident HF independent of several CVD risk factors and incident CHD as a time-dependent variable (continuous DWS: HR 1.21, 95% CI 1.04–1.41 for 0.1 decrease of DWS, p = 0.024; categorical DWS: HR 1.40, 95%CI 1.05–1.87 in smallest DWS quintile vs larger four DWS quintiles, p = 0.022). Fig. 2 shows Kaplan–Meier survival curves for incident HF for each DWS category. The smallest DWS quintile (more LV diastolic stiffness) had a higher incidence of HF than larger four DWS quintiles (log-rank p < 0.01). We also provided the Kaplan–Meier survival curves for incident HF for DWS quintiles (supplementary Fig. 1). The smaller DWS quintiles had a higher incidence of HF than larger DWS quintiles (log-rank p = 0.013). Multivariable adjusted restricted cubic spline analysis provides the visualized relationship between continuous DWS and incident HF (supplementary Fig. 2). Fig. 3 shows the results of stratified analyses for incidence of HF. The associations of DWS with incident HF were qualitatively consistent across all subgroups except in those with a history of diabetes. Supplementary Table 5 showed the results of Models 4–7. After adding LV mass index or LVEF to Model 3, the relationship between DWS and incident HF was not significant. After additionally including SAC or Ea to Model 3, the relationship between DWS and incident HF was still significant.
Fig. 2.
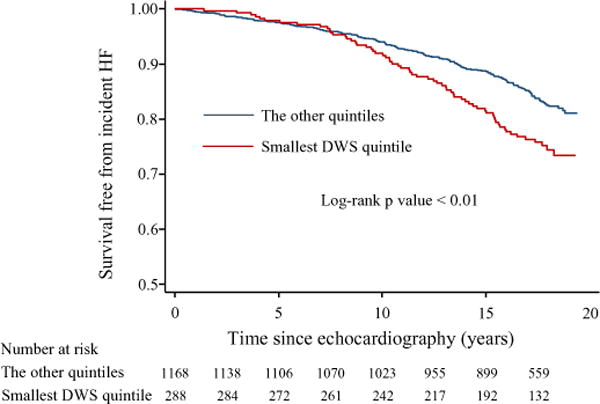
Kaplan–Meier survival curves for the length of time to the incident heart failure based on DWS category. DWS, diastolic wall strain; HF, heart failure.
Fig. 3.
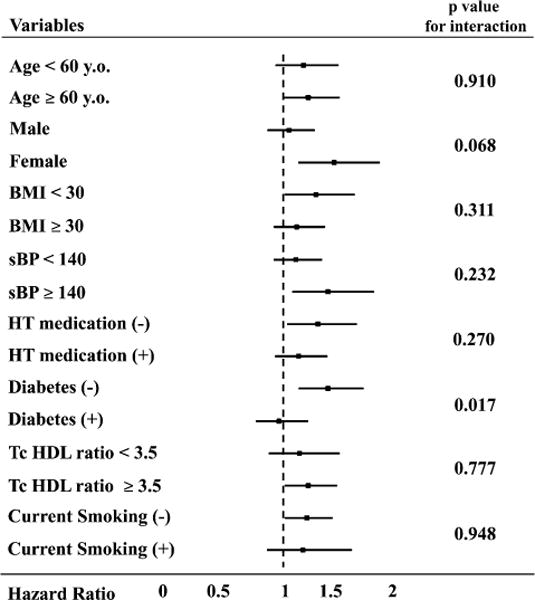
Stratified analysis with regard to incident heart failure. Hazard ratio represents 0.1 decrease of continuous DWS. BMI, body mass index; HT, hypertension; sBP, systolic blood pressure; Tc HDL ratio, total cholesterol/high-density lipoprotein cholesterol ratio. (+): present, (−): absent.
Diastolic wall strain and incident coronary heart disease
Over a mean follow-up of 16.1 years, there were 142 incident CHD (incident rate: 5.8 per 1000 person-years). Table 4 shows HRs and 95% CI of incident CHD based on categorical and continuous DWS. Smaller DWS was associated with a higher risk of incident CHD in both continuous and categorical variables in Model 1. However, after further adjustment for traditional CVD risk factors, only continuous DWS remained significant (HR 1.28, 95%CI 1.05–1.55 for 0.1 decrease of DWS, p = 0.014), but categorical DWS became insignificant.
Discussion
In this large, prospectively enrolled, middle-aged community-based African American cohort with preserved LVEF, participants with lower DWS (more LV myocardial stiffness) had a more severe LV concentric hypertrophy geometry and higher arterial stiffness at baseline. Furthermore, participants with lower DWS (increased myocardial stiffness) had a higher risk of incident HF compared to those with higher DWS after adjustment for conventional cardiovascular risk factors. But after additionally adjusting for LVEF or LV mass index, the relationships became insignificant. These findings suggest that DWS, which can be easily calculated from standard echocardiographic indices, may be used as a quick and qualitative estimator of LV myocardial stiffness and predictor of future HF risk, albeit not beyond classic measures such as LVEF or LV mass index.
Previous studies have suggested that LV myocardial stiffness plays an important role in the pathophysiology of both HFrEF and HFpEF. In HFrEF patients, it has been reported that LV passive myocardial stiffness is higher than in those without HF, and LV myocardial stiffness is the most important determinant of plasma brain natriuretic peptide (BNP) production [5,16]. On the other hand, in HFpEF patients, LV myocardial stiffness is higher compared to patients with hypertension without HF despite having similar LV mass index [6]. Increased LV myocardial stiffness due to increases in myocyte stiffness and collagen accumulation is thought to play a significant role in the pathophysiology of this type of HF [6,17]. However, because measuring LV myocardial stiffness generally requires an invasive procedure and complicated computations, it has been difficult to examine the relationship between LV myocardial stiffness and incident HF in large cohorts. DWS, an indicator that may be able to estimate LV myocardial stiffness, can be easily calculated from indices that are measured routinely in standard echocardiographic examinations, and previous studies have shown its usefulness in the clinical setting [8,9]. In this study, participants with lower DWS had a higher risk of incident HF even if they did not have any history of CVD at baseline and after adjustment for possible confounding factors, suggesting increases in LV myocardial stiffness play a pivotal role in the development of HF.
Ohtani and colleagues have reported that patients with HFpEF had a lower DWS than healthy controls, and in HFpEF patients, those with lower DWS had more severe LV concentric remodeling, higher BNP levels, and poorer prognosis than those with higher DWS [9]. In our study, among those without a history of CVD, participants with lower DWS had more severe LV concentric hypertrophy and a higher risk of incident HF. Thus, our study findings were in line with the previous study in HFpEF patients and suggest the importance of assessing LV myocardial stiffness in those with American College of Cardiology/American Heart Association HF classification stage A: those at risk for HF, but who have not yet developed structural heart changes, and furthermore, to those without any risks [18].
Liu and colleagues reported that patients with lower DWS had a higher carboxy-terminal propeptide of procollagen type 1 which is a surrogate marker of cardiac fibrosis [19]. Increased LV fibrosis is a main contributor to increased LV myocardial stiffness and is also associated with higher incidences of both HFpEF and HFrEF [20,21]. Takagi and colleagues reported that in patients without obvious myocardial ischemia, low DWS was associated with increased LV filling pressure assessed by E/e′ on echocardiography after exercise [22]. Therefore, these previous studies corroborate our findings.
In the present study, lower DWS was associated with higher SAC and Ea. In other words, lower DWS (more LV myocardial stiffness) was closely associated with higher systemic arterial stiffness or arterial load. This finding is reasonable because LV myocardial stiffness is closely associated with arterial stiffness through ventricular arterial coupling and it is consistent with several previous studies [23–25].
Based on the values of DWS in previous studies, one-fifth of the subjects of this study had a low value of DWS which indicates impaired diastolic function [8,9]. This proportion may be relatively high compared with the general population. However, African Americans have a high prevalence of hypertension, obesity, and HF [10,26,27]. Also, the prevalence of HFpEF in which increases in LV myocardial stiffness plays a critical role in the development of HF, is high among African Americans [28]. Thus, our findings suggestive of a high proportion of participants with diastolic stiffness is not completely unexpected.
LV hypertrophy is an important risk factor for incident HF, therefore, we additionally adjusted for LV mass index [29]. After adjustment for LV mass index, the association between DWS and incident HF became insignificant. Increased LV myocardial stiffness has been reported to occur immediately before the development of HF that is after the development of compensatory LV concentric hypertrophy in an experimental hypertensive HF model [30]. Thus, those with increased LV myocardial stiffness and hypertensive heart disease might already have LV hypertrophy at the onset of HF. On the other hand, LV hypertrophy itself is a component of LV chamber stiffness as well as LV myocardial stiffness [31]. Therefore, it might be difficult to completely exclude the influence of LV hypertrophy on the relationship between LV myocardial stiffness assessed by DWS and incident HF in this study. Also, after additionally adjusting for LVEF, the relationship between DWS and incident HF became insignificant. Further investigation is warranted to clarify whether LVEF is better to predict incident HF than LV myocardial stiffness.
In this study, continuous DWS was associated with incident CHD as well as incident HF. It is well known that arterial stiffening is associated with LV stiffening through ventricular-arterial coupling [23]. It is also known that arterial stiffening is associated with CHD [32,33]. Therefore, the relationship between DWS and incident CHD observed in this study might indirectly show the relationship between arterial stiffening and CHD. On the other hand, symptomatic CHD may be associated with increased myocardial stiffness [34]. There may be other possible causal factors in this relationship warranting further investigation.
Our study has some limitations. First, the DWS indicator was aimed to non-invasively estimate LV myocardial stiffness using echocardiography. However, the relationship between DWS and LV myocardial stiffness constant which is the gold standard to evaluate LV myocardial stiffness, was proved only in a basic experimental study [8]. The equation of DWS is PWs − PWd/PWs = 1 − PWd/PWS. Thus, it may be argued that the equation includes the inverse of wall thickening and it may just reflect the LV contractility rather than wall distensibility. LV wall thickening is used as an indicator of regional systolic function because there is a significant correlation between fractional shortening and wall thickening in the heart without regional wall motion abnormalities [35,36]. LV fractional shortening is an indicator of LV systolic function which is calculated using LV endocardial movement, and it is not necessarily the same as LV wall thickening. In the previous study DWS was not associated with LV fractional shortening, and it may suggest that DWS does not simply reflect LV systolic function [8]. Second, we could not compare DWS with other LV diastolic function indicators. There were limited markers of diastolic function (trans-mitral inflow indices) evaluated in the studied cohort that we could compare our findings to, and it is well known that the trans-mitral inflow indices cannot estimate LV end-diastolic pressure in those with preserved LVEF [37]. Thus, DWS needs to be compared with other LV diastolic function parameters in the future studies. Third, our study was performed only in African Americans, so these findings may not necessarily be generalized to other racial groups. However, this study adds important information regarding myocardial stiffness to African Americans who are disproportionately affected by CVD including HF [10,26]. Fourth, we could not examine the relationship between DWS and the incidence of both HFrEF and HFpEF, because the ARIC Study started to evaluate the incidence of the separate phenotypes of HF in 2005 while the echocardiograms for the current study were performed from 1993 to 1995. Increased LV myocardial stiffness might have different impacts on both HF phenotypes. However, it has been suggested that diastolic function plays an important role even in those with HFrEF [38,39]. Our study has several strengths. To our knowledge, this is the first study that investigated the role of LV myocardial stiffness in the development of HF in a well characterized, large prospectively enrolled cohort study. We also have a long follow-up period. The median follow-up was >15 years and adequate to evaluate for HF incidence in a middle-aged cohort.
Conclusions
In summary, increased LV myocardial stiffness assessed by DWS was associated with increased LV concentric hypertrophy and aortic stiffness indicators at baseline. After adjustment for conventional risk factors, DWS was associated with an increased risk of HF incidence in a community-based cohort of African Americans. However, after additionally adjusting for LV mass index or LVEF, the relationship became insignificant. These results suggest that DWS, easily calculated from routine echocardiographic measurements, could be used as a quick and qualitative estimator of LV myocardial stiffness and predictor of incident HF among those without previous CVD similar to classic measures such as LVEF or LV mass index.
Supplementary Material
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions. The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). We also acknowledge support from NIH/NIDDK 1K08DK099415 and NIH P20GM104357 (MEH).
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.jjcc.2017.11.004.
Footnotes
Author contributions
Daisuke Kamimura: Concept/design, Data analysis/interpretation, Drafting article.
Takeki Suzuki: Concept/design, Critical revision.
Michael E. Hall: Concept/design, Critical revision.
Wanmei Wang: Data analysis, Statistics.
Michael D. Winniford: Critical revision.
Amil M. Shah: Critical revision.
Carlos J. Rodriguez: Critical revision.
Kenneth R. Butler: Data collection, Critical revision.
Thomas H. Mosley: Concept/design, Funding, Data collection, Critical revision.
Conflict of interest
None.
References
- 1.Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. doi: 10.1038/nrcardio.2010.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Kane GC, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC, Jr, et al. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306:856–63. doi: 10.1001/jama.2011.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gharacholou SM, Scott CG, Takahashi PY, Nkomo VT, McCully RB, Fine NM, et al. Left ventricular diastolic function and long-term outcomes in patients with normal exercise echocardiographic findings. Am J Cardiol. 2013;112:200–7. doi: 10.1016/j.amjcard.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watanabe S, Shite J, Takaoka H, Shinke T, Imuro Y, Ozawa T, et al. Myocardial stiffness is an important determinant of the plasma brain natriuretic peptide concentration in patients with both diastolic and systolic heart failure. Eur Heart J. 2006;27:832–8. doi: 10.1093/eurheartj/ehi772. [DOI] [PubMed] [Google Scholar]
- 6.Zile MR, Baicu CF, Ikonomidis JS, Stroud RE, Nietert PJ, Bradshaw AD, et al. Myocardial stiffness in patients with heart failure and a preserved ejection fraction: contributions of collagen and titin. Circulation. 2015;131:1247–59. doi: 10.1161/CIRCULATIONAHA.114.013215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakano K, Sugawara M, Ishihara K, Kanazawa S, Corin WJ, Denslow S, et al. Myocardial stiffness derived from end-systolic wall stress and logarithm of reciprocal of wall thickness. Contractility index independent of ventricular size. Circulation. 1990;82:1352–61. doi: 10.1161/01.cir.82.4.1352. [DOI] [PubMed] [Google Scholar]
- 8.Takeda Y, Sakata Y, Higashimori M, Mano T, Nishio M, Ohtani T, et al. Noninvasive assessment of wall distensibility with the evaluation of diastolic epicardial movement. J Card Fail. 2009;15:68–77. doi: 10.1016/j.cardfail.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Ohtani T, Mohammed SF, Yamamoto K, Dunlay SM, Weston SA, Sakata Y, et al. Diastolic stiffness as assessed by diastolic wall strain is associated with adverse remodelling and poor outcomes in heart failure with preserved ejection fraction. Eur Heart J. 2012;33:1742–9. doi: 10.1093/eurheartj/ehs135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:2138–45. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall JL, Duprez DA, Barac A, Rich SS. A review of genetics, arterial stiffness, and blood pressure in African Americans. J Cardiovasc Transl Res. 2012;5:302–8. doi: 10.1007/s12265-012-9362-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goncalves A, Claggett B, Jhund PS, Rosamond W, Deswal A, Aguilar D, et al. Alcohol consumption and risk of heart failure: the Atherosclerosis Risk in Communities Study. Eur Heart J. 2015;36:939–45. doi: 10.1093/eurheartj/ehu514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skelton TN, Andrew ME, Arnett DK, Burchfiel CM, Garrison RJ, Samdarshi TE, et al. Echocardiographic left ventricular mass in African-Americans: the Jackson cohort of the Atherosclerosis Risk in Communities Study. Echocardiography. 2003;20:111–20. doi: 10.1046/j.1540-8175.2003.03000.x. [DOI] [PubMed] [Google Scholar]
- 14.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Takeda Y, Sakata Y, Mano T, Nishio M, Ohtani T, Hori M, et al. Noninvasive assessment of diastolic function in subjects with preserved left ventricular ejection fraction: usefulness of color kinetic imaging. J Card Fail. 2008;14:569–76. doi: 10.1016/j.cardfail.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 16.Borbely A, Falcao-Pires I, van Heerebeek L, Hamdani N, Edes I, Gavina C, et al. Hypophosphorylation of the Stiff N2B titin isoform raises cardiomyocyte resting tension in failing human myocardium. Circ Res. 2009;104:780–6. doi: 10.1161/CIRCRESAHA.108.193326. [DOI] [PubMed] [Google Scholar]
- 17.Hamdani N, Paulus WJ. Myocardial titin and collagen in cardiac diastolic dysfunction: partners in crime. Circulation. 2013;128:5–8. doi: 10.1161/CIRCULATIONAHA.113.003437. [DOI] [PubMed] [Google Scholar]
- 18.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 19.Liu YW, Lee WH, Lin CC, Huang YY, Lee WT, Lee CH, et al. Left ventricular diastolic wall strain and myocardial fibrosis in treated hypertension. Int J Cardiol. 2014;172:e304–6. doi: 10.1016/j.ijcard.2013.12.187. [DOI] [PubMed] [Google Scholar]
- 20.Schelbert EB, Piehler KM, Zareba KM, Moon JC, Ugander M, Messroghli DR, et al. Myocardial fibrosis quantified by extracellular volume is associated with subsequent hospitalization for heart failure, death, or both across the spectrum of ejection fraction and heart failure stage. J Am Heart Assoc. 2015:4. doi: 10.1161/JAHA.115.002613. pii: e002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamamoto K, Masuyama T, Sakata Y, Nishikawa N, Mano T, Yoshida J, et al. Myocardial stiffness is determined by ventricular fibrosis, but not by compensatory or excessive hypertrophy in hypertensive heart. Cardiovasc Res. 2002;55:76–82. doi: 10.1016/s0008-6363(02)00341-3. [DOI] [PubMed] [Google Scholar]
- 22.Takagi T, Takagi A, Yoshikawa J. Low diastolic wall strain is associated with raised post-exercise E/E′ ratio in elderly patients without obvious myocardial ischemia. J Echocardiogr. 2014;12:106–11. doi: 10.1007/s12574-014-0225-1. [DOI] [PubMed] [Google Scholar]
- 23.Borlaug BA, Kass DA. Ventricular-vascular interaction in heart failure. Heart Fail Clin. 2008;4:23–36. doi: 10.1016/j.hfc.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Little WC, Cheng CP. Left ventricular-arterial coupling in conscious dogs. Am J Physiol. 1991;261:H70–6. doi: 10.1152/ajpheart.1991.261.1.H70. [DOI] [PubMed] [Google Scholar]
- 25.Lam CS, Roger VL, Rodeheffer RJ, Bursi F, Borlaug BA, Ommen SR, et al. Cardiac structure and ventricular-vascular function in persons with heart failure and preserved ejection fraction from Olmsted County, Minnesota. Circulation. 2007;115:1982–90. doi: 10.1161/CIRCULATIONAHA.106.659763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wali RK, Weir MR. Hypertensive cardiovascular disease in African Americans. Curr Hypertens Rep. 1999;1:521–8. doi: 10.1007/s11906-996-0025-8. [DOI] [PubMed] [Google Scholar]
- 27.Jones DW. What is the role of obesity in hypertension and target organ injury in African Americans? Am J Med Sci. 1999;317:147–51. doi: 10.1097/00000441-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Gupta DK, Shah AM, Castagno D, Takeuchi M, Loehr LR, Fox ER, et al. Heart failure with preserved ejection fraction in African Americans: The ARIC (Atherosclerosis Risk In Communities) study. JACC Heart Fail. 2013;1:156–63. doi: 10.1016/j.jchf.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bluemke DA, Kronmal RA, Lima JA, Liu K, Olson J, Burke GL, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;52:2148–55. doi: 10.1016/j.jacc.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sakata Y, Masuyama T, Yamamoto K, Doi R, Mano T, Kuzuya T, et al. Renin angiotensin system-dependent hypertrophy as a contributor to heart failure in hypertensive rats: different characteristics from renin angiotensin system-independent hypertrophy. J Am Coll Cardiol. 2001;37:293–9. doi: 10.1016/s0735-1097(00)01064-0. [DOI] [PubMed] [Google Scholar]
- 31.Sakata Y, Masuyama T, Yamamoto K, Nishikawa N, Yamamoto H, Kondo H, et al. Calcineurin inhibitor attenuates left ventricular hypertrophy, leading to prevention of heart failure in hypertensive rats. Circulation. 2000;102:2269–75. doi: 10.1161/01.cir.102.18.2269. [DOI] [PubMed] [Google Scholar]
- 32.Mulders TA, van den Bogaard B, Bakker A, Trip MD, Stroes ES, van den Born BJ, et al. Arterial stiffness is increased in families with premature coronary artery disease. Heart. 2012;98:490–4. doi: 10.1136/heartjnl-2011-300999. [DOI] [PubMed] [Google Scholar]
- 33.Duprez DA, Cohn JN. Arterial stiffness as a risk factor for coronary atherosclerosis. Curr Atheroscler Rep. 2007;9:139–44. doi: 10.1007/s11883-007-0010-y. [DOI] [PubMed] [Google Scholar]
- 34.Visner MS, Arentzen CE, Parrish DG, Larson EV, O’Connor MJ, Crumbley AJ, 3rd, et al. Effects of global ischemia on the diastolic properties of the left ventricle in the conscious dog. Circulation. 1985;71:610–9. doi: 10.1161/01.cir.71.3.610. [DOI] [PubMed] [Google Scholar]
- 35.Sasayama S, Franklin D, Ross J, Jr, Kemper WS, McKown D. Dynamic changes in left ventricular wall thickness and their use in analyzing cardiac function in the conscious dog. Am J Cardiol. 1976;38:870–9. doi: 10.1016/0002-9149(76)90800-6. [DOI] [PubMed] [Google Scholar]
- 36.Lieberman AN, Weiss JL, Jugdutt BI, Becker LC, Bulkley BH, Garrison JG, et al. Two-dimensional echocardiography and infarct size: relationship of regional wall motion and thickening to the extent of myocardial infarction in the dog. Circulation. 1981;63:739–46. doi: 10.1161/01.cir.63.4.739. [DOI] [PubMed] [Google Scholar]
- 37.Yamamoto K, Nishimura RA, Chaliki HP, Appleton CP, Holmes DR, Jr, Redfield MM. Determination of left ventricular filling pressure by Doppler echocardiography in patients with coronary artery disease: critical role of left ventricular systolic function. J Am Coll Cardiol. 1997;30:1819–26. doi: 10.1016/s0735-1097(97)00390-2. [DOI] [PubMed] [Google Scholar]
- 38.Nikitin NP, Loh PH, Silva R, Ghosh J, Khaleva OY, Goode K, et al. Prognostic value of systolic mitral annular velocity measured with Doppler tissue imaging in patients with chronic heart failure caused by left ventricular systolic dysfunction. Heart. 2006;92:775–9. doi: 10.1136/hrt.2005.067140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Giannuzzi P, Temporelli PL, Bosimini E, Silva P, Imparato A, Corra U, et al. Independent and incremental prognostic value of Doppler-derived mitral deceleration time of early filling in both symptomatic and asymptomatic patients with left ventricular dysfunction. J Am Coll Cardiol. 1996;28:383–90. doi: 10.1016/0735-1097(96)00163-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


