Abstract
Objectives:
Insufficient sleep has become recognized as a pervasive problem in modern society. Sleep debt is a novel measure of sleep adequacy that may be useful in describing those at risk for inadequate sleep. Our objective was to investigate factors that may be associated with sleep debt at the population level, as well as build upon previous data that showed that minority groups may be more likely to have sleep debt.
Design:
A cross-sectional population phone survey included questions regarding amount of sleep required and amount of sleep achieved. Sleep debt was calculated by subtracting sleep achieved from sleep required.
Setting:
This study was designed by the Philadelphia Health Management Corporation and conducted over landlines and cell phones.
Participants:
8,752 adults over age 18 were randomly chosen from several counties in and around Philadelphia by the Random Digit Dialing methodology and answered questions about sleep.
Measurements:
Logistic regression was performed to test associations between sleep debt and various sociodemographic factors in different population subgroups to identify those at risk for sub-optimal sleep duration.
Results:
Sleep debt was seen to decrease with age, a novel finding that is in contrast with literature suggesting that older adults have poor sleep. Greater sleep debt was also associated with female gender, Hispanic/Latino ethnicity, <40 years of age, self-reported poor health, and increased stress.
Conclusions:
Although older adults may sleep less as they age, they may also require less sleep to feel rested, resulting in less sleep debt. This and other demographic factors, such as female gender and Hispanic/Latino ethnicity, can be used to identify those at higher risk of inadequate sleep and potentially manage their sleep debt.
Keywords: Sleep debt, sleep quality, sleep duration, insomnia, older adults
Introduction
Accumulating evidence has shown that chronic sleep deprivation and insufficient sleep have become pervasive in modern society.1–4 The National Sleep Foundation sleep duration recommendations were updated in 2015 to reflect current understanding of sleep requirements in different age brackets. Although they concede that some people may fall outside the guidelines, the majority of people should fall within the recommended 7-9 hours for healthy adults.5 This is further supported by a consensus statement from the American Academy of Sleep Medicine and Sleep Research Society, which states that healthy adults should sleep at least 7 hours per night to promote optimal health.6 The common occurrence of insufficient sleep and the risks associated with it makes it a major public health issue. For example, insufficient sleep has been linked to poor health, motor vehicle accidents, poor job performance, obesity, diabetes, cardiovascular disease, depression, and morbidity.3,4,7,8 Job, economic, and domestic pressures as well as unhealthy behaviors, artificial lighting, and the widespread use of electronic devices such as smartphones, computers, and televisions are all contributing factors to insufficient sleep. Other causes of sleep disturbances include medical and mental disorders.2,4
In addition to these factors, there is a strong relationship between sleep duration and socioeconomic position as well as sociodemographic status. Poor sleep is associated with low income and poverty.9–11 Jackson and colleagues found that socioeconomic factors appeared to partially explain the association for short sleep in African Americans.12 Ertel et al investigated the interaction between socioeconomic status, occupational factors and ethnicity on sleep duration using wrist actigraphy. They found that night work, total work hours, and male gender were salient predictors of shorter sleep duration in African and Caribbean immigrants.13
Sleep debt is a measure of sleep adequacy calculated by subtracting the average duration of sleep achieved from the duration of sleep needed to feel rested. Sleep debt is thought to accumulate over multiple nights of insufficient sleep and can have negative consequences over time.14 With polysomnography, duration of sleep achieved can be determined objectively, but for this study, both of these values were subjective. Duration of sleep needed to feel rested is a value that is likely different for everyone. We decided to investigate sleep debt at a population level to describe which portions of a community might be more affected by it. Our goal was to describe population variation in sleep debt using common, self-reported demographic variables. We hypothesized that certain minority groups would be more likely to have sleep debt, based on an earlier study by our group.10
The Philadelphia Health Management Corporation (PHMC) is a non-profit institute that focuses on community health. PHMC administers an uncompensated, cross-sectional community survey in southeast Pennsylvania, with the most recent survey available for analysis conducted in 2008. A survey that took place in 2006 found that poor sleep quality was strongly associated with poverty and race and that African-American and Latino groups had worse overall sleep quality than the Caucasian groups.10 The 2008 survey focused on sleep duration and awareness of sufficient sleep on an individual level. We examined this dataset to statistically test associations between sleep debt and various sociodemographic factors.
Methods
Subjects
The Philadelphia Health Management Corporation (PHMC) conducts a cross -sectional community health survey in southeastern Pennsylvania periodically. The survey data used here was conducted between June and October 2008 by a market research firm based in New York City. The methods for the PHMC have been previously described.10 Briefly, 10,000 households residing in the Bucks, Chester, Delaware, Montgomery, and Philadelphia counties were chosen by Random Digit Dialing to participate in telephone interviews given in either English or Spanish. Interviews averaged 24 minutes. Response rates were not provided in the PHMC dataset, but samples from each county were found to be representative of the population of the counties. One adult 18 years of age or above was selected from each household using the “last birthday” method, meaning if there was more than one adult in the house, the adult with the most recent birthday was chosen to survey. Permission from the PHMC was obtained before analysis of this dataset. This study received approved from the University of Pennsylvania Institutional Review Board.
Measurements
Three sleep questions were included in the 2008 PHMC survey: 1) Quality of sleep: “In general, how would you rate the quality of your sleep in the past week on a scale of 1 to 5, with 1 being restless and 5 being restful”; 2) Duration of sleep: “In general, how many hours of sleep do you get at night? This may be different than the number of hours you spend in bed”; and 3) Estimated sleep need: “How many hours of sleep do you feel you need at night? This may be different from how many hours of sleep you actually get at night”. Subjects who answered that they needed or obtained 0 hours of sleep as well as those who needed or obtained more than 12 hours of sleep were excluded since these are physiologically implausible.
Socioeconomic factors, sociodemographic factors and other covariates
Age, sex, race/ethnicity, and marital status were included in the statistical analysis. Income status (above or below 2× the federal poverty level), Medicaid insurance status, educational level and employment status were provided by participants as well. Self- reported health and lifestyle indicators including body mass index (BMI), smoking status, heavy alcohol use, diagnosis of mental illness, and stress levels were also included in the analysis. Stress level, sleep quality and number of children were grouped to simplify data analysis. Stress level was rated by participants on a scale of 1-10; data was grouped as 1-2 for low, 3-4 for mild, 5-6 for moderate, 7-8 for high, and 9-10 for very high. Sleep quality was rated on a scale of 1 to 5, with 1 being restless; data was grouped as 1 for restless, and 2-5 for restful (i.e. not restless). Number of children did not have predefined values; data was grouped as 0 (no children) or ≥1 (children). A detailed description of these factors has been published previously.10
Statistical Analysis
SAS 9.0 (SAS Institute, Inc. Cary, NC) was used for all statistical analyses. An alpha value of 0.05 was used for all tests unless specified otherwise. The two SAS procedures used were FREQ and SURVEYLOGISTIC. We first calculated odds ratios to determine which variables were likely to influence sleep debt. After odds ratios were calculated, logistic regression was performed with those variables that were significant from the odds ratios. A series of multivariate logistic regressions were undertaken to assess predictors of sleep debt. Using a backward-stepwise method (with p = 0.05 being the condition for removal of factors from the model) a series of variables was entered. The first model uses an interaction term of race × income, as this had previously been found to be significant.10 However, this was not significant in our model, so we dropped the interaction term to analyze the race variable alone. Model 3 reflects only the variables that remained as significant covariates as described above. Analyses were conducted using sample weights so that results would be applicable to the general population.10
Results
Sample Characteristics
In 2010, The Philadelphia Health Management Corporation contacted 10,007 potential participants for a phone survey. Of the participants, 8,752 chose to respond to the sleep questions. Comparison with the United States Census 2014 for age, gender, race, and ethnicity showed similar values.15 Of the participants, 32.4% were aged 18-39, 49.8% were aged 40-64, and 17.8% were aged greater than 65. 73.1% of the participants identified as white, 20.6% identified as African-American, and 6.2% identified as Latino/Hispanic. Table 1 shows the remaining demographic and social breakdown of the participants.
Table 1.
Demographic information of survey respondents
| Participant Characteristics (n = 8752) |
% Total | % Males | % Females |
|---|---|---|---|
| Age | |||
| 18-39 | 32.42 | 31.63 | 33.08 |
| 40-64 | 49.83 | 50.66 | 49.83 |
| >65 | 17.76 | 17.70 | 17.80 |
| Race | |||
| White | 73.14 | 75.44 | 71.20 |
| African American | 20.65 | 18.63 | 22.35 |
| Latino/Hispanic | 6.21 | 5.93 | 6.45 |
| Income Threshold | |||
| Above 2× | 76.23 | 80.95 | 72.24 |
| Below 2× | 23.77 | 19.05 | 27.76 |
| Race × Income Interaction | |||
| White, Not Poor | 62.21 | 66.16 | 58.88 |
| White, Poor | 10.93 | 9.28 | 12.32 |
| AA, Not Poor | 11.23 | 11.73 | 10.81 |
| AA, Poor | 9.42 | 6.90 | 11.54 |
| Latino, Not Poor | 2.79 | 3.07 | 2.55 |
| Latino, Poor | 3.43 | 2.86 | 3.90 |
| Education | |||
| < High school graduate | 7.01 | 7.31 | 6.76 |
| High school graduate | 30.63 | 28.56 | 32.36 |
| Some college | 20.37 | 19.91 | 20.76 |
| College graduate | 25.55 | 25.77 | 25.36 |
| Post college | 16.44 | 18.44 | 14.76 |
| Employment Status | |||
| Employed | 63.77 | 68.09 | 60.14 |
| Unemployed | 12.65 | 12.25 | 12.99 |
| Retired | 17.66 | 17.95 | 17.42 |
| Disabled | 5.91 | 1.71 | 9.45 |
| Marital Status | |||
| Married | 58.37 | 62.50 | 54.89 |
| Living with partner | 6.79 | 8.23 | 5.58 |
| Single | 19.97 | 19.12 | 20.69 |
| Widow | 6.70 | 3.88 | 9.08 |
| Other | 8.16 | 6.27 | 9.76 |
| Sleep Quality | |||
| 1 – Restless | 9.83 | 8.37 | 11.07 |
| 2 | 8.26 | 7.01 | 9.31 |
| 3 | 22.99 | 21.60 | 24.16 |
| 4 | 27.84 | 30.80 | 25.36 |
| 5 – Restful | 31.07 | 32.22 | 30.11 |
| General Health | |||
| Excellent | 33.98 | 33.93 | 34.02 |
| Good | 47.75 | 48.43 | 47.18 |
| Fair | 14.67 | 14.36 | 14.93 |
| Poor | 3.60 | 3.28 | 3.88 |
| Mental Illness | |||
| Absent | 82.12 | 87.18 | 77.86 |
| Present | 17.88 | 12.82 | 22.14 |
| Body Mass Index | |||
| ≤25 | 39.16 | 29.74 | 47.08 |
| 25-30 | 36.10 | 44.53 | 29.00 |
| >30 | 24.74 | 25.72 | 29.91 |
| Stress Level | |||
| Low (1-2) | 16.90 | 20.83 | 13.59 |
| Mild (3-4) | 20.33 | 21.80 | 19.09 |
| Moderate (5-6) | 28.57 | 27.93 | 29.11 |
| High (7-8) | 22.56 | 21.42 | 23.51 |
| Very high (9-10) | 11.64 | 8.02 | 14.70 |
| Smoking Status | |||
| No | 80.27 | 79.98 | 80.51 |
| Yes | 19.73 | 20.02 | 19.49 |
| Children | |||
| No children | 64.12 | 67.69 | 61.12 |
| ≥1 children | 35.88 | 32.31 | 38.88 |
| Sleep Debt | |||
| No sleep debt (0 or surplus) | 46.37 | 52.48 | 41.22 |
| Sleep debt(1-5 hours) | 53.63 | 47.52 | 58.78 |
Many respondents reported poor sleep, with 18.1% noting a sleep quality score of 1 or 2 (with 1 being restless sleep and 5 being restful sleep quality; Table 1). Only 31.1% of the sample reported receiving restful sleep (those who selected 5 for sleep quality). More than half of respondents (53.6%) reported having at least 1 hour of sleep debt normally. 11.4 % of females reported “restless” sleep quality compared to 8.4% of males (χ2 = 126.39, p<0.00001). 58.8% of female respondents carried a sleep debt of at least 1 hour compared with 47.5% for males (χ2 = 222.59, p<0.00001).
Unadjusted Odds Ratios
Table 2 shows the unadjusted odds ratios for sleep debt with and without sample weights. Age differences were observed, with middle aged participants (ages 40-64) and older adults (ages>64) having less sleep debt than the youngest age group (OR = 0.66, 95% CI = 0.58 – 0.75 and OR = 0.26, 95% CI = 0.22 – 0.31, respectively; p<0.0001). Females were found to have significantly more sleep debt than males (OR = 1.57, 95% CI 1.41 – 1.74; p<0.0001). Those below 2× the federal poverty line (poor) reported a higher sleep debt than those with an income above 2× the poverty line (not poor; OR = 1.26, 95% CI = 1.12 – 1.43). This association had a significant interaction with race; poor whites had a slightly increased sleep debt over not poor whites (OR = 1.19, 95% CI = 1.00 – 1.41). This association was amplified for not poor and poor African Americans (OR = 1.23, 95% CI = 1.05 – 1.44 and OR = 1.38, 95% CI = 1.15 – 1.65, respectively) and even further for Latinos (OR = 1.79, 95% CI = 1.28 – 2.51 and OR = 1.75, 95% CI = 1.23 – 2.49).
Table 2.
Weighted and unweighted odds ratios of sleep debt by demographic factors
| Participant Characteristics (n = 8752) |
Weighted | Unweighted | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age (ref = 18-39) |
||||||
| 40-64 | 0.66 | 0.58 – 0.75 | <0.0001 | 0.65 | 0.58 – 0.73 | <0.0001 |
| >64 | 0.26 | 0.22 – 0.31 | <0.0001 | 0.28 | 0.24 – 0.32 | <0.0001 |
| Sex (ref = Male) |
||||||
| Female | 1.57 | 1.41 – 1.74 | <0.0001 | 1.58 | 1.44 – 1.73 | <0.0001 |
| Income Threshold (ref = Above 2× Poverty) |
||||||
| Below 2× Poverty Line | 1.26 | 1.12 – 1.43 | <0.0001 | 1.21 | 1.09 – 1.34 | <0.0001 |
| Race × Income Categories (ref = White, Not Poor) |
||||||
| White, Poor | 1.19 | 1.00 – 1.41 | 0.0396 | 1.06 | 0.92 – 1.22 | 0.3775 |
| AA, Not Poor | 1.23 | 1.05 – 1.44 | 0.0076 | 1.25 | 1.10 – 1.42 | 0.0004 |
| AA, Poor | 1.38 | 1.15 – 1.65 | 0.0004 | 1.37 | 1.19 – 1.59 | <0.0001 |
| Latino, Not Poor | 1.79 | 1.28 – 2.51 | 0.0007 | 1.50 | 1.14 – 1.98 | 0.0038 |
| Latino, Poor | 1.75 | 1.23 – 2.49 | 0.0018 | 2.09 | 1.58 – 2.77 | <0.0001 |
| Race (ref = White, Not Latino) |
||||||
| Black, Not Latino | 1.26 | 1.11 – 1.43 | 0.0002 | 1.29 | 1.17 – 1.42 | <0.0001 |
| Latino | 1.72 | 1.34 – 2.21 | <0.0001 | 1.76 | 1.44 – 2.14 | <0.0001 |
| Education (ref = < HS grad) |
||||||
| HS graduate | 0.93 | 0.75 – 1.16 | 0.5675 | 0.85 | 0.71 – 1.01 | 0.0757 |
| Some college | 1.14 | 0.90 – 1.43 | 0.2661 | 1.09 | 0.90 – 1.31 | 0.3416 |
| College graduate | 1.08 | 0.86 – 1.35 | 0.5054 | 1.02 | 0.85 – 1.23 | 0.7738 |
| Post college | 0.94 | 0.74 – 1.19 | 0.6318 | 0.96 | 0.79 – 1.16 | 0.6758 |
| Employment (ref = Employed) |
||||||
| Unemployed | 1.24 | 1.05 – 1.47 | 0.0101 | 1.24 | 1.09 – 1.43 | 0.0014 |
| Retired | 0.36 | 0.31 – 0.41 | <0.0001 | 0.39 | 0.35 – 0.43 | <0.0001 |
| Disabled | 1.19 | 0.95 – 1.51 | 0.1274 | 1.02 | 0.84 – 1.23 | 0.8388 |
| Marital Status (ref = Married) |
||||||
| Living with partner | 1.42 | 1.13 – 1.79 | 0.0026 | 1.37 | 1.13 – 1.67 | 0.0012 |
| Single | 1.49 | 1.30 – 1.72 | <0.0001 | 1.45 | 1.30 – 1.62 | <0.0001 |
| Widow | 0.62 | 0.52 – 0.73 | <0.0001 | 0.65 | 0.56 – 0.75 | <0.0001 |
| Other | 1.25 | 1.05 – 1.47 | 0.0085 | 1.18 | 1.03 – 1.36 | 0.0135 |
| Sleep Quality (ref = 1 – Restless) |
||||||
| 2 | 0.77 | 0.56 – 1.06 | 0.1187 | 0.77 | 0.59 – 1.01 | 0.0605 |
| 3 | 0.42 | 0.33 – 0.54 | <0.0001 | 0.41 | 0.33 – 0.50 | <0.0001 |
| 4 | 0.16 | 0.12 – 0.20 | <0.0001 | 0.16 | 0.13 – 0.19 | <0.0001 |
| 5 - Restful | 0.07 | 0.05 – 0.09 | <0.0001 | 0.07 | 0.05 – 0.08 | <0.0001 |
| General Health (ref = excellent) |
||||||
| Good | 1.22 | 1.09 – 1.38 | 0.0005 | 1.19 | 1.08 – 1.31 | 0.0002 |
| Fair | 1.49 | 1.27 – 1.75 | <0.0001 | 1.46 | 1.29 – 1.67 | <0.0001 |
| Poor | 1.67 | 1.26 – 2.20 | <0.0001 | 1.87 | 1.49 – 2.34 | <0.0001 |
| Mental Illness (ref = Absent) |
||||||
| Present | 1.96 | 1.71 – 2.25 | <0.0001 | 1.94 | 1.73 – 2.17 | <0.0001 |
| BMI (ref = <25) |
||||||
| 25-30 | 0.85 | 0.76 – 0.96 | 0.012 | 0.89 | 0.80 – 0.98 | 0.0202 |
| >30 | 1.03 | 0.90 – 1.17 | 0.631 | 1.07 | 0.96 – 1.19 | 0.1697 |
| Stress Levels (ref = Low [1-2]) |
||||||
| Mild (3-4) | 1.62 | 1.36 – 1.92 | <0.0001 | 1.77 | 1.53 – 2.04 | <0.0001 |
| Moderate (5-6) | 2.36 | 2.01 – 2.78 | <0.0001 | 2.57 | 2.25 – 2.93 | <0.0001 |
| High (7-8) | 3.95 | 3.32 – 4.71 | <0.0001 | 4.33 | 3.76 – 5.00 | <0.0001 |
| Very high (9-10) | 5.30 | 4.30 – 6.52 | <0.0001 | 5.14 | 4.33 – 6.10 | <0.0001 |
| Smoking (ref = No) |
||||||
| Yes | 1.21 | 1.06 – 1.38 | 0.0032 | 1.11 | 1.00 – 1.23 | 0.0495 |
| Children (ref = No children) |
||||||
| ≥1 children | 1.61 | 1.44 – 1.80 | <0.0001 | 1.68 | 1.53 – 1.85 | <0.0001 |
Interestingly, education status was not associated with sleep debt while employment status was. Unemployed participants had a significantly higher sleep debt than those who reported employment (OR = 1.24, 95% CI = 1.05 – 1.47). Retired participants had a significantly lower sleep debt than employed participants as well (OR = 0.36, 95% CI = 0.31 – 0.41).
Marital status was also associated with sleep debt. Compared to being married, living with a partner or being single both were independently associated with sleep debt (OR = 1.42, 95% CI = 1.13 – 1.79 and OR = 1.49, 95% CI = 1.30 – 1.72). Widows and widowers had significantly less sleep debt than married participants (OR = 0.62, 95% CI = 0.52 – 0.73). Participants who reported having at least one child in the house were associated with significantly higher sleep debt than those with no children (OR = 1.61, 95% CI = 1.44 – 1.80).
Sleep quality scores correlated with sleep debt. Those who rated their sleep quality a 2 (1 = restless, 5 = restful) did not differ significantly from those who rated it a 1. Those who rated it a 3, 4 or 5 were associated with significantly less sleep debt than those who rated their normal sleep a 1 (OR = 0.42, 95% CI = 0.33 – 0.54; OR = 0.16, 95% CI = 0.12 – 0.20; OR = 0.07, 95% CI = 0.05 – 0.09, respectively).
We also found significant associations with sleep debt for several physical and mental health measures. Participants who self-reported their health to be good, fair or poor had significantly more sleep debt than those who reported excellent overall health (OR = 1.22, 95% CI = 1.09 – 1.38; OR = 1.49, 95% CI = 1.27 – 1.75; OR = 1.67, 95% CI = 1.26 – 2.20, respectively). Participants who reported mental illness had significantly more sleep debt (OR = 1.96, 95% CI = 1.71 – 2.25). Those with an overweight BMI (25-30) showed slightly decreased sleep debt than participants with normal BMI (<25) (OR = 0.85, 95% CI = 0.76 – 0.96). Obese persons showed no difference in sleep debt. Smokers reported having significantly more sleep debt than non-smokers (OR = 1.21, 95% CI = 1.06 – 1.38).
Mental health appeared to have the largest role of any question included in the PHMC study. Stress was rated on a 1-10 scale (1 = low, 10 = very high). As reported stress levels increased, so did sleep debt by several factors. Participants who reported their stress to be mild, moderate, high, or very high had significantly more sleep debt than those who reported low levels of stress (OR = 1.62, 95 %CI = 1.36 – 1.92; OR = 2.36, 95% CI = 2.01 – 2.78; OR = 3.95, 95% CI = 3.32 – 4.71; OR = 5.30, 95% CI = 4.30 – 6.52; respectively).
Logistic Regression and Adjusted Odds Ratios
Next, multivariable models were constructed to explore the associations of various factors taken together (Table 3). Model 1 included the following factors: age, sex, race × poverty (interaction term), employment, marital status, sleep quality, overall health, presence of psychiatric disease, BMI, stress, smoking status, and presence of children in the house. We included a race × poverty term because we had noted this to be significant in our prior analyses of sleep quality 10. We found several of these variables to be significant: age, sex, employment, sleep quality, overall health, psychiatric disorders, stress, smoking status, and children in the house (all p<0.05). Race × poverty was not significant in this analysis of sleep debt, unlike our prior work on sleep quality 10.
Table 3.
Weighted logistic regression for sleep debt by demographic factors
| Participant Characteristics (n = 8752) |
Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (ref = 18-39) |
||||||
| 40-64 | 0.76* | 0.65 – 0.88 | 0.76* | 0.65 – 0.88 | 0.71** | 0.62 – 0.82 |
| >64 | 0.50** | 0.40 – 0.63 | 0.50** | 0.40 – 0.63 | 0.45** | 0.36 – 0.56 |
| Sex (ref = Male) |
||||||
| Female | 1.41** | 1.25 – 1.59 | 1.41 ** | 1.25 – 1.58 | 1.43** | 1.27 – 1.60 |
| Race × Income † (ref = White, Not Poor)† |
||||||
| White, Poor | 1.11 | 0.90 – 1.37 | - | - | - | - |
| AA, Not Poor | 1.19 | 0.99 – 1.42 | - | - | - | - |
| AA, Poor | 1.14 | 0.90 – 1.45 | - | - | - | - |
| Latino, Not Poor | 1.55* | 1.10 – 2.19 | - | - | - | - |
| Latino, Poor | 1.32 | 0.88 – 1.98 | - | - | - | - |
| Race † (ref = White [Non-Latino])† |
||||||
| Black (Non-Latino) | - | - | 1.14 | 0.98 – 1.33 | - | - |
| Latino | - | - | 1.39* | 1.05 – 1.82 | - | - |
| Race † (ref = Non-Latino)† |
||||||
| Latino | - | - | - | - | 1.32* | 1.00 – 1.73 |
| Income † (ref = Above 2× Poverty) |
||||||
| Below 2× Poverty | - | - | 1.03 | 0.87 – 1.22 | - | - |
| Education (ref = < HS grad) |
||||||
| HS graduate | 1.03 | 0.79 – 1.34 | 1.04 | 0.80 – 1.36 | - | - |
| Some college | 1.17 | 0.88 – 1.54 | 1.19 | 0.89 – 1.57 | - | - |
| College graduate | 1.23 | 0.93 – 1.64 | 1.25 | 0.94 – 1.66 | - | - |
| Post college | 1.12 | 0.83 – 1.51 | 1.14 | 0.85 – 1.53 | - | - |
| Employment (ref = Employed) |
||||||
| Unemployed | 0.85 | 0.69 – 1.04 | 0.85 | 0.69 – 1.04 | 0.87 | 0.72 – 1.06 |
| Retired | 0.62** | 0.51 – 0.75 | 0.62** | 0.51 – 0.75 | 0.61** | 0.51 – 0.74 |
| Disabled | 0.92 | 0.71 – 1.18 | 0.92 | 0.71 – 1.18 | 0.90 | 0.70 – 1.15 |
| Marital Status (ref = Married) |
||||||
| Living with partner | 1.16 | 0.90 – 1.51 | 1.16 | 0.89 – 1.51 | - | - |
| Single | 1.14 | 0.97 – 1.35 | 1.15 | 0.97 – 1.35 | - | - |
| Widow | 0.94 | 0.76 – 1.16 | 0.94 | 0.77 – 1.16 | - | - |
| Other | 1.08 | 0.89 – 1.32 | 1.09 | 0.90 – 1.32 | - | - |
| Sleep Quality (ref = 1 – Restless) |
||||||
| Restful | 0.19** | 0.14 – 0.24 | 0.18** | 0.14 – 0.24 | 0.19** | 0.15 – 0.24 |
| General Health (ref = Excellent) |
||||||
| Good | 1.28* | 1.12 – 1.46 | 1.28* | 1.12 – 1.46 | 1.28* | 1.12 – 1.45 |
| Fair | 1.46* | 1.20 – 1.78 | 1.46* | 1.20 – 1.78 | 1.47** | 1.22 – 1.77 |
| Poor | 1.27 | 0.92 – 1.74 | 1.27 | 0.92 – 1.74 | 1.26 | 0.92 – 1.72 |
| Mental Illness (ref = Absent) |
||||||
| Present | 1.34* | 1.15 – 1.57 | 1.34* | 1.15 – 1.57 | 1.34* | 1.15 – 1.57 |
| BMI (ref = <25) |
||||||
| 25-30 | 0.94 | 0.82 – 1.08 | 0.94 | 0.83 – 1.08 | - | - |
| >30 | 0.96 | 0.83 – 1.11 | 0.96 | 0.83 – 1.08 | - | - |
| Stress Levels (ref = Low [1-2]) |
||||||
| Mild (3-4) | 1.41* | 1.18 – 1.70 | 1.42* | 1.18 – 1.70 | 1.40* | 1.17 – 1.68 |
| Moderate (5-6) | 1.79** | 1.50 – 2.13 | 1.79** | 1.50 – 2.13 | 1.76** | 1.48 – 2.10 |
| High (7-8) | 2.77** | 2.29 – 3.34 | 2.77** | 2.29 – 3.34 | 2.73** | 2.26 – 3.30 |
| Very high (9-10) | 2.86** | 2.28 – 3.59 | 2.88** | 2.29 – 3.61 | 2.86** | 2.28 – 3.58 |
| Smoking (ref = No) |
||||||
| Yes | 0.85* | 0.73 – 0.99 | 0.85* | 0.73 – 1.00 | 0.85* | 0.74 – 0.99 |
| Children (ref = No children) |
||||||
| ≥1 children | 1.22* | 1.06 – 1.39 | 1.21* | 1.06 – 1.39 | 1.19* | 1.05 – 1.36 |
= p < 0.05
= p < 0.0001
= Race × Income interaction variable used in Model 1; separate Race and Income variables used in Models 2 and 3
Model 2 included these same factors, substituting race and poverty for the race × poverty interaction term, and adding high school graduation status. For this model, we found several variables remained significant: age, sex, race, employment, sleep quality, overall health, psychiatric disorder, stress, smoking status, and children in the house (all p<0.05). We note that in Model 2, only race and not poverty showed a significant association with sleep debt.
Finally, Model 3 included only significant factors from the previous model: age, sex, employment, sleep quality, overall health, psychiatric disorder, stress, smoking status, children in the house, and Hispanic/Latino ethnicity status. All categories were significant (p<0.05); however, there were non-significant differences within some of the above variables. We found diminishing sleep debt associated with aging participants, with both 40-64 year-olds and 65+ year-olds having less sleep debt than <40 year-olds (OR = 0.71, 95% CI = 0.62 – 0.82 and OR = 0.45, 95% CI = 0.36 – 0.56, respectively). Sleep debt was more highly associated with females than males (OR = 1.43, 95% CI = 1.27 – 1.60). Retired persons were associated with lower likelihood of sleep debt than employed persons (OR = 0.61, 95% CI = 0.51 – 0.74), but being unemployed or disabled had no association with sleep debt. Unsurprisingly, ratings of sleep quality as restful were associated with less sleep debt than those who rated it restless (OR = 0.19, 95% CI = 0.15 – 0.24).
Self-reported health statuses also had significant correlations with sleep debt. Participants who rated their overall health as good or fair were associated with significantly higher sleep debt than those who rated their health excellent (OR = 1.28, 95% CI = 1.12 – 1.45 and OR = 1.47, 95% CI = 1.22 – 1.77, respectively). Interestingly, this association did not extend to those who rated their health poor. Participants with a psychiatric disorder were associated with increased sleep debt (OR = 1.34, 95% CI = 1.15 – 1.57).
As before, all levels of self-reported stress levels were associated with increased sleep debt in a stepwise fashion. Stress levels was noted as the variable with highest odds ratios in this study. Participants who reported their stress to be mild, moderate, high, or very high had significantly more sleep debt than those who reported low levels of stress (OR = 1.40, 95% CI = 1.17 – 1.68; OR = 1.76, 95% CI = 1.48 – 2.10; OR = 2.73, 95% CI = 2.26 – 3.30; OR = 2.86, 95% CI = 2.28 – 3.58, respectively).
Smoking was associated with less sleep debt than non-smokers, a reversal of our initial results outlined above (OR = 0.85, 95% CI = 0.74 – 0.99). The reasons for this remain unclear, but it appears that after correcting for other factors in the model, smoking showed a weaker associated with sleep debt. Participants with 1 or more children living with them were likely to have more sleep debt compared with those who had no children in the house (OR = 1.19, 95% CI = 1.05 – 1.36).
Finally, participants who identified as Hispanic/Latino ethnicity were more likely to have sleep debt (OR = 1.32, 95% CI = 1.00 – 1.73). It is interesting to note that after controlling for other variables, neither race nor poverty status were significantly associated with sleep debt, but ethnicity was.
We also found decreasing sleep debt associated with increasing age. In younger subjects (age 18-39), sleep debt was consistent at approximately negative 2 hours. This dropped to approximately 1 hour by middle age and continued dropping to close to zero sleep debt in older participants (age >65).
Discussion
Sleep quantity and quality are oft-overlooked measures of health and societal well-being. Lack of sleep is thought to be responsible for numerous avoidable deaths such as motor vehicle accidents.4 Poor sleep has also been linked to huge economic losses in the United States and worldwide.10
This study expands on a previous study by this group that explored effects of demographics and several other variables on sleep quality.10 However, this study utilized the 2010 Philadelphia Health Management Corporation survey, which included two additional questions regarding amount of sleep required and amount of sleep achieved. Namely, this allowed us to calculate sleep debt and run a similar analysis to determine how the above variables are correlated with both sleep quality and sleep debt.
Similar to our previous paper, we found that some minority groups had stronger associations with sleep debt than the reference groups. Longer sleep latency has been correlated in adults with lower levels of education, food insecurity, and identifying as African American.11 Others have found differences in pediatric populations as well. African American children were noted to sleep less during the night than white children.16 However, the decreased sleep of participants identifying as African-American was modulated by inclusion of other variables like age, employment status, and a myriad of self-reported health variables. This may indicate that groups such as Latinos are more susceptible to the effects of poor sleep and that as a group they are not as well equipped to deal with circumstances that lead to less or poor-quality sleep.
Females were more likely to report poor sleep quality than males (11.1% vs 8.4%, respectively). Female respondents were also more likely than males to carry a sleep debt of at least 1 hour (58.8% vs 47.5% for males). We are unsure why women appeared to report lower quality sleep and be more likely to carry sleep debt. This study was not powered to detect this difference and we invite future research to focus efforts on this disparity.
We noted that sleep debt was associated with increasing age, a finding that was not previously reported in the literature. That is, after approximately age 45, participants transitioned from significant sleep debt to sufficient sleep. This is intriguing as it runs counter to conventional wisdom regarding sleep debt as we age – namely, that the older segment of the population carries more sleep debt. Surprisingly, we found that the opposite was true. This may be attributable to several factors. Older participants are more likely to have fewer children in the house, work less, and carry less stress in general. Older adults may also have more control over their sleep schedule, allowing them to align their actual sleep with their perceived needs. All these factors may predispose them towards attaining more and higher quality sleep.
Previous results have shown that aging leads to worse sleep, as measured by increased sleep latency and decreased REM sleep.17 Although this is the opposite result from what we found in this study, the authors of the previously cited study noted that the associations were minimized when controlling for additional covariates. Older adults may have more opportunities to sleep. Further, even though adults may get less sleep as they age they may also require less sleep, and thus the sleep debt falls as subjects age. Some have observed that as we age, we get less sleep objectively. Our measure of sleep debt is subjective, and thus this difference in outcomes may also explain the different result. Finally, the decrease in sleep debt in older adults may be a result of increased acceptability of health problems in aged populations.18 Older adults are more likely to perceive their health problem as normal, and rate it as less of a problem for them as they age. In our case, they may be more reticent to rate their sleep poorly because they perceive it to be normal for their age group.
Other studies have found that reported sleep may differ significantly from expected or actual sleep. One study found that sleep disturbances and reported tiredness appeared to decrease as participants got older, but that these factors may have been influenced by declining health or presence of psychological disorders.19 In general, sleep actually appeared to increase in quality and duration in older participants, contrary to some previous studies.17,20 This may be due to discrepancies between reported and actual sleep in older adults.21 Subjects with reported insomnia symptoms tended to underestimate their sleep efficiency while normal controls over-estimated their sleep efficiency. It is clear that self-reported measures of sleep quality may be unreliable, and our measure of sleep debt may be a better indicator of sleep status.
Overall, self-reported stress level held the strongest correlation with sleep debt. This is unsurprising but warrants further analysis because of the high odds ratios. Those who reported high stress levels were more than twice as likely to carry sleep debt as those who reported low levels of stress. It is likely that stressed participants took longer to fall asleep, woke up in the middle of the night, or woke up early due to stress.
As noted above, we report that smokers were associated with less sleep debt than non-smokers when controlling for self-reported health variables. It is possible that smoking may reduce stress or causes short periods of relaxation in the evening that facilitate somnolence faster than in non-smokers. However, further work is needed to elucidate this relationship.
Limitations
The major limitation of this study is the subjectivity inherent in the survey questions. Although sleep duration can be accurately measured with polysomnography, this survey required participants to estimate their average amount of sleep. This may have been misinterpreted as time spent in bed, or time trying to fall asleep, etc. Additionally, participants were also asked to estimate the amount of sleep needed to feel rested. Although we removed outliers as described above, there is likely great variability among these estimates. Due to the large sample size, we acknowledge that certain biases (i.e. needing more or less sleep to feel rested) are likely present in the data, and we were unable to control for them.
The second limitation was that participants were drawn from a relatively small geographical area in the greater Philadelphia region, and thus their survey results may not be applicable to all populations. This may bias the study against those who did not want to participate in research, those who could not be on the phone for some time, or those with a disability that prevented them from talking on the phone. Although the surveyors made every effort to communicate with the participants, including conducting interviews in Spanish and using a proxy if the participant could not use a phone, it is likely that one or several portions of the general population was not included properly in the results. In addition, this survey was only conducted with those persons that owned a telephone. The majority of those surveyed were done so via their home phone, a technology that many people do not use anymore. The only cell phone respondents were located in Philadelphia County and these numbered 300. Thus, while efforts were made to use a study sample that represents the larger population, it is possible that the survey instrument did not capture some portions of the population.
Finally, there are a number of other variables that were not collected in the PHMC survey that may bias the results. For example, there is no way to parse out participants with sleep or circadian rhythm disorders. The survey did not include any questions about work schedule, meaning those that work the third shift are grouped in with the rest of the cohort. Finally, there are numerous other factors that affect nightly sleep quality and quantity, such as medication use, caffeine and other stimulant use, or illicit drug use. Therefore, the data presented may not be representative of these groups.
Conclusion
This study is the first to our knowledge to describe sleep debt in a large population. Other studies have used objective data, which may under- or over-report sleep based on a number of factors. Due to this, sleep debt may be a useful metric when assessing sleep on a population level, particularly since sleep debt may be additive over multiple nights of inadequate sleep and has increasingly deleterious effects. Furthermore, we were able to clarify that sleep debt is associated with younger, not older, participants, a finding that is contrary to some previous literature. Further research is required to confirm this finding to help us better understand sleeping habits of older adults.
Figure 1.
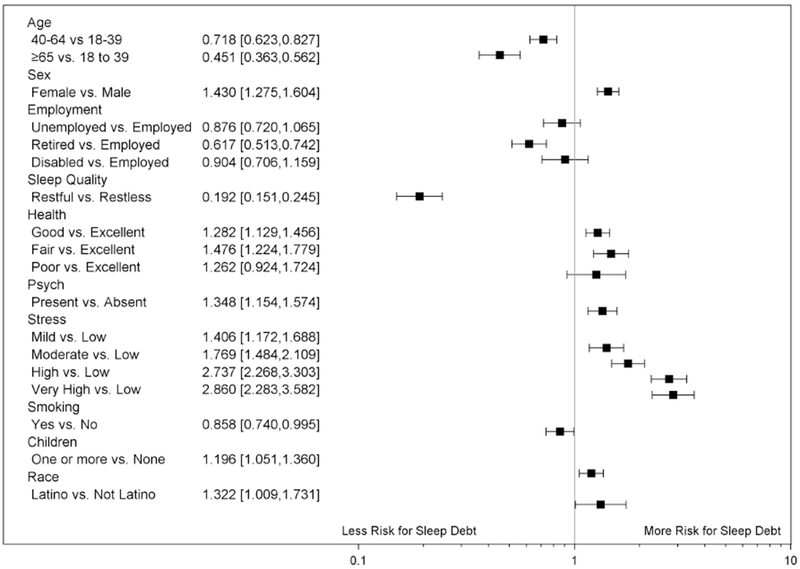
Odds ratios for sleep debt by demographic factors from Model 3 above
Figure 2.
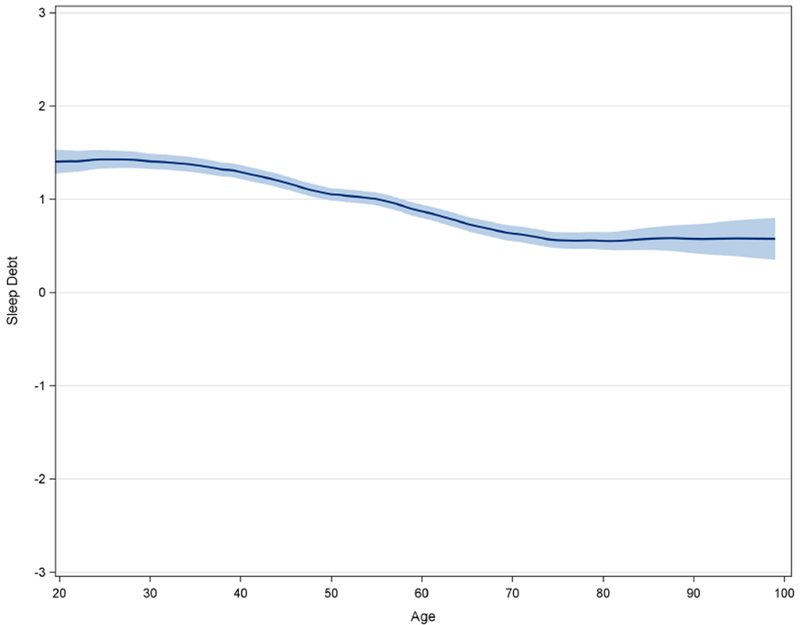
Sleep debt by age
Acknowledgements:
We would like to dedicate this manuscript to the memory of Dr. Nirav Patel.
Funding: Support for this project has been provided by the following: Pilot funds from the University of Pennsylvania Center for Sleep & Circadian Rhythm, as well as funds from NIH T32 Grant awarded to Nirav Patel and Michael Grandner.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rosekind MR. Awakening a nation: A call to action. Sleep Health. 2015;1(1):9–10. doi: 10.1016/j.sleh.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Broman JE, Lundh LG, Hetta J. Insufficient sleep in the general population. Neurophysiol Clin. 1996;26(1):30–39. doi: 10.1016/0987-7053(96)81532-2. [DOI] [PubMed] [Google Scholar]
- 3.Geiger SD, Sabanayagam C, Shankar A. The relationship between insufficient sleep and self-rated health in a nationally representative sample. J Environ Public Health. 2012;2012:518263. doi: 10.1155/2012/518263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wells ME, Vaughn BV. Poor sleep challenging the health of a Nation. Nenrodiagn J. 2012;52(3):233–249. http://www.ncbi.nlm.nih.gov/pubmed/23019761. [PubMed] [Google Scholar]
- 5.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015; 1 (1) :40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Consensus Conference Panel, Watson NF, Badr MS, et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. J Clin Sleep Med. 2015; 11(8):931–952. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buxton OM, Enrico M. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5): 1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 8.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep. 2007;30(12): 1667–1673. http://www.ncbi.nlm.nih.gov/pubmed/18246976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11(5):470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10:475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grandner MA, Ruiter Petrov ME, Pinyo R, Nicholas J, Alec P, Patel NP. Sleep Symptoms, Race/Ethnicity, and Socioeconomic Position. J Clin Sleep Med. 2013. doi: 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jackson CL, Redline S, Kawachi I, Hu FB. Association between sleep duration and diabetes in black and white adults. Diabetes Care. 2013;36(11):3557–3565. doi: 10.2337/dcl3-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US White health care workers. Sleep. 2011. ;34(4):509–518. http://www.ncbi.nlm.nih.gov/pubmed/21461330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitamura S, Katayose Y, Nakazaki K, et al. Estimating individual optimal sleep duration and potential sleep debt. Sci Rep. 2016;6:35812. doi: 10.1038/srep35812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Population estimates, July 1, 2015, (V2015). http://www.census.gov/quickfacts/table/PST045215/00 Accessed May 30, 2016.
- 16.Crosby B Racial Differences in Reported Napping and Nocturnal Sleep in 2- to 8-Year-Old Children. Pediatrics. 2005;115(1):225–232. doi: 10.1542/peds.2004-0815d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7): 1255–1273. http://www.ncbi.nlm.nih.gov/pubmed/15586779. [DOI] [PubMed] [Google Scholar]
- 18.Brouwer WBF, van Exel NJA, Stolk EA. Acceptability of less than perfect health states. Soc Sci Med. 2005;60(2):237–246. doi: 10.1016/j.socscimed.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 19.Martin JL, Fiorentino L, Jouldjian S, Josephson KR, Alessi CA. Sleep quality in residents of assisted living facilities: effect on quality of life, functional status, and depression. J Am Geriatr Soc. 2010;58(5):829–836. doi: 10.1111/j.1532-5415.2010.02815.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grandner MA, Jackson NJ, Izci-Balserak B, et al. Social and Behavioral Determinants of Perceived Insufficient Sleep. Front Neurol. 2015;6:112. doi: 10.3389/fneur.2015.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gooneratne NS, Bellamy SL, Pack F, et al. Case-control study of subjective and objective differences in sleep patterns in older adults with insomnia symptoms. J Sleep Res. 2011;20(3):434–444. doi: 10.1111/j.1365-2869.2010.00889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


