Abstract
Objectives:
Cardiovascular risk factors are prevalent in the population undergoing non-cardiac surgery. Changes in perioperative cardiovascular risk factor profiles over time are unknown.
The objective of this study was to evaluate national trends in cardiovascular risk factors and atherosclerotic cardiovascular disease (ASCVD) among patients undergoing non-cardiac surgery.
Methods:
Adults ≥45 years old who underwent non-cardiac surgery were identified using the United States National Inpatient Sample from 2004 to 2013. The prevalence of traditional cardiovascular risk factors [hypertension, dyslipidemia, diabetes mellitus, obesity, and chronic kidney disease] and ASCVD [coronary artery disease, peripheral artery disease, and prior stroke] were evaluated over time.
Results:
A total of 10,581,621 hospitalizations for major non-cardiac surgery were identified. Between 2008–2013, ≥2 cardiovascular risk factors and ASCVD were present in 44.5% and 24.3% of cases, respectively. Over time, the prevalence of multiple (≥2) cardiovascular risk factors increased from 40.5% in 2008–09 to 48.2% in 2012–13, p<0.001. The proportion of patients with coronary artery disease (17.2% in 2004–05 vs. 18.2% in 2012–13, p<0.001), peripheral artery disease (6.3% in 2004–05 vs. 7.4% in 2012–13, p<0.001), and prior stroke (3.5% in 2008–09 vs. 4.7% 2012–13, p<0.001) also increased over time. The proportion of patients with a modified RCRI score ≥3 increased from 6.6% in 2008–09 to 7.7% in 2012–13 (p<0.001).
Conclusions:
Among patients undergoing major non-cardiac surgery, the burden of cardiovascular risk factors and the prevalence of ASCVD increased over time. Adverse trends in risk profiles require continued attention to improve perioperative cardiovascular outcomes.
Keywords: Cardiovascular Disease, Cardiovascular Risk Factors, Coronary Artery Disease, Operative Risk, Noncardiac Surgery, Peripheral Artery Disease, Perioperative, Surgery
Introduction:
Perioperative cardiovascular complications are a significant source of morbidity and mortality for 300 million patients worldwide undergoing non-cardiac surgery each year.(1) Major cardiovascular and cerebrovascular complications, including death, myocardial infarction, or stroke, occur in approximately 1 of every 33 hospitalizations for non-cardiac surgery.(2) Patients with the greatest perioperative cardiovascular risk are routinely identified using clinical risk prediction models, such as the popular Revised Cardiac Risk Index (RCRI).(3–5) The RCRI and other models incorporate cardiovascular risk factors, the presence of atherosclerotic cardiovascular disease (ASCVD), and procedure-specific risks to identify individuals who may derive the greatest benefit from careful medical optimization prior to surgery. Despite the significance of these clinical factors to predict perioperative risk, the prevalence of ASCVD and its risk factors in patients undergoing non-cardiac surgery has not been reported. We evaluated national trends in cardiovascular risk factors, ASCVD, and a simple perioperative cardiovascular risk index among adults age ≥45 years undergoing major non-cardiac surgery.
Methods
Study Population
Adults ≥45 years of age undergoing non-cardiac surgery were identified from the Healthcare Cost and Utilization Project’s (HCUP) National Inpatient Sample (NIS).(2) The NIS is a nationwide administrative database reporting discharge-level data collected from a 20% stratified sample of hospitals in the United States.(6) Patients undergoing non-cardiac surgery were included if the principal International Classification of Diseases, Ninth Revision (ICD-9) procedure codes represented major therapeutic operating room procedures (HCUP Procedure Class 4). Clinical Classifications Software (CCS) principal procedure codes, aggregates of related primary ICD-9 procedure codes, were clustered by major surgical subtypes: endocrine, general, genitourinary, gynecologic, neurosurgery, obstetrics, orthopedic, otolaryngology, skin and breast, thoracic, non-cardiac transplant, and vascular surgery. Subjects who underwent major cardiac procedures (n=1,465,792), cardiac surgery (including cardiac transplantation) (n=522,635), bone marrow transplantation (n=16,934), ophthalmologic surgery (n=11,458), radiation therapy (n=8,216), dental surgery (n=1,570), and non-operating room procedures (n=311) were excluded from the analysis.
Risk Factor and Disease Prevalence
Major cardiovascular risk factors were defined by the presence of ICD-9 diagnosis codes for hypertension, dyslipidemia, diabetes mellitus, obesity, and chronic kidney disease. ASCVD was defined by ICD-9 diagnosis codes for coronary artery disease, peripheral artery disease, or prior stroke or transient ischemic attack. Modified Revised Cardiac Risk Index (RCRI) scores were generated using ICD-9 diagnosis codes for ischemic heart disease, heart failure, prior transient ischemic attack or stroke, chronic kidney disease, diabetes mellitus, and high-risk surgery. ICD-9 diagnosis codes for cardiovascular risk factors and comorbidities are presented in Supplementary Table 1.
Data on cardiovascular risk factor and disease prevalence were reported for patients hospitalized for surgery between January 1st 2004 and December 31st 2013. Due to the introduction of an ICD-9 diagnosis code for prior stroke or transient ischemic attack in mid-2007, stroke prevalence, the composite of ASCVD, and modified RCRI scores were only reported for years 2008 to 2013. Similarly, changes in ICD-9 diagnosis coding for chronic kidney disease during the analysis time period rendered CKD diagnoses unreliable prior to 2007. As a consequence, chronic kidney disease prevalence and the composite of ≥1 cardiovascular risk factors were only reported for years 2007 to 2013.
Statistical Analysis
All continuous variables were presented as mean ± standard deviation (SD) and compared using the Student’s t test. Categorical variables were presented as percentages and compared by Chi-square tests. Analyses of proportions over time were performed using the Cochran-Armitage test for trend. To facilitate data presentation, patient demographics, cardiovascular risk factors, and cardiovascular disease prevalence rates were reported in 2-year intervals: 2004 to 2005, 2006 to 2007, 2008 to 2009, 2010 to 2011, and 2012 to 2013. Survey weights were applied to calculate rates for trend analyses and to determine national population estimates as per HCUP guidance. Statistical analyses were performed using SPSS 20 (IBM SPSS Statistics, Armonk, NY) and STATA 15 (StataCorp, College Station, TX). Statistical tests were two-sided and all P-values <0.05 were considered to be statistically significant. The NIS is a publicly available, de-identified dataset and the study was exempt from institutional board review.
Patient Involvement
Patients were not involved in developing the research question, study outcome measures, study design, or conduct of the study. No patients provided input into the data analysis or interpretation of the results. There are no plans to disseminate the results of the research to study participants. No patients served as authors or contributors to this work.
Results
Study Population
Between January 2004 and December 2013, we identified 12,863,389 surgical hospitalizations among adults 45 years and older in the United States. After the exclusion of hospitalizations for cardiac surgery, low-risk, and non-operative procedures, the final sample consisted of 10,581,621 major non-cardiac surgical hospitalizations. This corresponds to an estimated 50,558,529 hospitalizations for non-cardiac surgery after applying sampling weights to generate nationwide estimates for the United States population. Characteristics of the surgical population over time are shown in Table 1.
Table 1.
Characteristics of patients undergoing major non-cardiac surgery in the United States over time.
| 2004–2005 (n=9,693,521) |
2006–2007 (n=9,996,788) |
2008–2009 (n=10,550,525) |
2010–2011 (n=10,591,720) |
2012–2013 (n=9,725,977) |
|
|---|---|---|---|---|---|
| Age, mean ± SD | 65.84 ± 12.62 | 65.79 ± 12.53 | 65.68 ± 12.38 | 65.63 ± 12.20 | 65.75 ± 11.82 |
| Female Sex | 5589394 (57.9%) | 5689768 (57.1%) | 5949514 (56.5%) | 5916307 (55.9%) | 5395649 (55.5%) |
| Race/Ethnicity | |||||
| White Non-Hispanic | 5754014 (59.4%) | 5674232 (56.8%) | 6890699 (65.3%) | 7410284 (70%) | 7164308 (73.7%) |
| Black Non-Hispanic | 621994 (6.4%) | 667387 (6.7%) | 762159 (7.2%) | 980609 (9.3%) | 920045 (9.5%) |
| Hispanic | 461121 (4.8%) | 521991 (5.2%) | 578980 (5.5%) | 680828 (6.4%) | 611450 (6.3%) |
| Other | 286897 (3%) | 328680 (3.3%) | 451586 (4.3%) | 413358 (3.9%) | 448515 (4.6%) |
| Unknown | 2569495 (26.5%) | 2804498 (28.1%) | 1867101 (17.7%) | 1106641 (10.4%) | 581659 (6%) |
| Cardiovascular Risk Factors | |||||
| Hypertension | 5037464 (52%) | 5539559 (55.4%) | 6158092 (58.4%) | 6458906 (61%) | 6109494 (62.8%) |
| Dyslipidemia | 1824214 (18.8%) | 2402166 (24%) | 3068510 (29.1%) | 3546994 (33.5%) | 3564159 (36.6%) |
| Diabetes Mellitus | 1998912 (20.6%) | 2256253 (22.6%) | 2568785 (24.3%) | 2789983 (26.3%) | 2666755 (27.4%) |
| Obesity | 693180 (7.2%) | 849103 (8.5%) | 1138106 (10.8%) | 1378557 (13%) | 1481470 (15.2%) |
| Chronic Kidney Disease* | - | - | 867785 (8.2%) | 1036492 (9.8%) | 1010385 (10.4%) |
| Atherosclerotic Cardiovascular Disease | |||||
| Coronary Artery Disease | 1663065 (17.2%) | 1769400 (17.7%) | 1904903 (18.1%) | 1909707 (18%) | 1768060 (18.2%) |
| Prior PCI | 259489 (2.7%) | 316478 (3.2%) | 395303 (3.7%) | 446224 (4.2%) | 443915 (4.6%) |
| Prior CABG | 451158 (4.7%) | 465580 (4.7%) | 497467 (4.7%) | 504427 (4.8%) | 448550 (4.6%) |
| Peripheral Artery Disease | 611540 (6.3%) | 689773 (6.9%) | 743397 (7%) | 765677 (7.2%) | 723645 (7.4%) |
| Prior Stroke / TIA* | - | - | 370442 (3.5%) | 455399 (4.3%) | 455780 (4.7%) |
| High Risk RCRI (≥3)* | - | - | 695962 (6.6%) | 793764 (7.5%) | 747340 (7.7%) |
| Elective Surgery | 5786955 (59.9%) | 6039704 (60.6%) | 6358297 (60.4%) | 6422392 (60.8%) | 5893653 (60.8%) |
| Surgery Type | |||||
| General | 2109829 (21.8%) | 2124750 (21.3%) | 2274616 (21.6%) | 2244348 (21.2%) | 2069899 (21.3%) |
| Endocrine | 120446 (1.2%) | 121490 (1.2%) | 126854 (1.2%) | 127751 (1.2%) | 89645 (0.9%) |
| Genitourinary | 755181 (7.8%) | 765407 (7.7%) | 782145 (7.4%) | 771275 (7.3%) | 613875 (6.3%) |
| Gynecologic | 725420 (7.5%) | 694472 (6.9%) | 648903 (6.2%) | 513542 (4.8%) | 368140 (3.8%) |
| Skin / Breast | 528414 (5.5%) | 493552 (4.9%) | 422569 (4%) | 393954 (3.7%) | 345340 (3.6%) |
| Neurosurgery | 572821 (5.9%) | 579856 (5.8%) | 576642 (5.5%) | 610353 (5.8%) | 548425 (5.6%) |
| Obstetric | 7920 (0.1%) | 8718 (0.1%) | 8641 (0.1%) | 8334 (0.1%) | 7345 (0.1%) |
| Orthopedic | 3489279 (36%) | 3731127 (37.3%) | 4211433 (39.9%) | 4485811 (42.4%) | 4425009 (45.5%) |
| Otolaryngology | 79950 (0.8%) | 75890 (0.8%) | 73094 (0.7%) | 74163 (0.7%) | 71900 (0.7%) |
| Thoracic | 203556 (2.1%) | 216880 (2.2%) | 242978 (2.3%) | 241240 (2.3%) | 212515 (2.2%) |
| Transplant | 27218 (0.3%) | 25816 (0.3%) | 37842 (0.4%) | 33457 (0.3%) | 30635 (0.3%) |
| Vascular | 1073485 (11.1%) | 1158829 (11.6%) | 1144807 (10.9%) | 1087491 (10.3%) | 943250 (9.7%) |
Denotes risk factors and clinical ASCVD only available for analysis from 2008–2013.
Risk Factors for Atherosclerotic Cardiovascular Disease
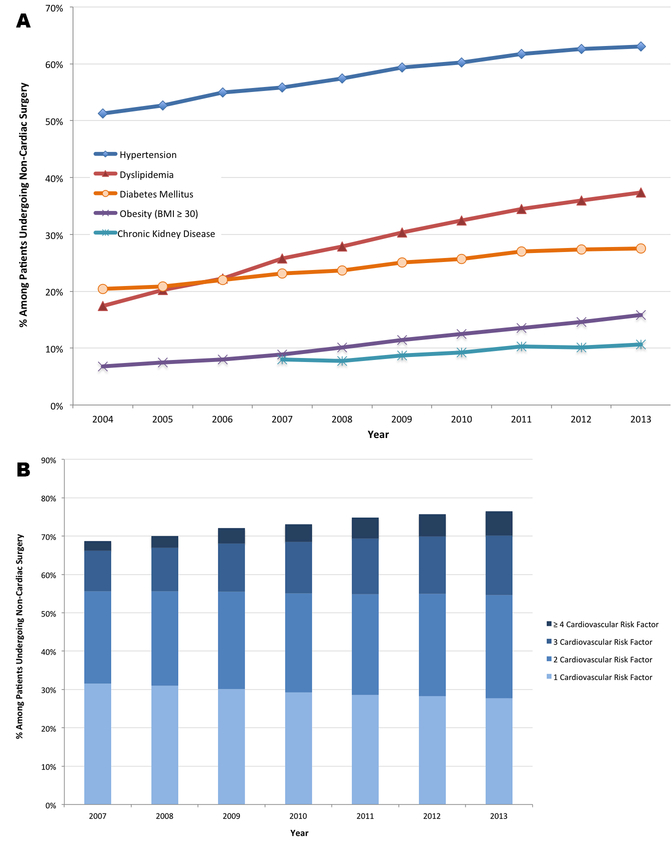
Between 2008–2013, ≥1 cardiovascular risk factor was present in 73.7% of cases, and multiple (≥2) cardiovascular risk factors were present in 44.5% of cases. As expected, the frequency of ≥1 cardiovascular risk factor increased with advancing age (Supplementary Figure 1). Over time, the proportion of patients with ≥1 cardiovascular risk factor increased by 5.1% [1.0% annually], from 71.1% in 2008–2009 to 76.1% in 2012–2013 (p<0.001; RR 1.07, 95% CI 1.07–1.07) and multiple cardiovascular risk factors increased from 40.5% in 2008–09 to 48.2% in 2012–13 (p<0.001; RR 1.19, 95% CI 1.19 – 1.19). Prevalence of individual risk factors, including hypertension (52.0% in 2004–2005 vs. 62.8% in 2012–2013, p<0.001; RR 1.21, 95% CI 1.21–1.21), dyslipidemia (18.8% in 2004–2005 vs. 36.6% in 2012–2013, p<0.001; RR 1.95, 95% CI 1.95–1.96), diabetes mellitus (20.6% in 2004–2005 vs. 27.4% in 2012–2013, p<0.001; RR 1.33, 95% CI 1.33–1.33), obesity (7.2% in 2004–2005 vs. 15.2% in 2012–2013, p<0.001; RR 2.13, 95% CI 2.12–2.14), and chronic kidney disease (8.2% in 2008–2009 vs. 10.4% in 2012–2013, p<0.001; RR 1.26, 95% CI 1.26–1.27) all increased during the study period (Figure 1A). The burden of cardiovascular risk based on the number of cardiovascular risk factors present for years 2007 through 2013 is shown in Figure 1B. Trends in cardiovascular risk factors adjusted for age, sex, and race are shown in Supplementary Figure 2. The prevalence of major cardiovascular risk factors in the general adult US population is shown in Supplementary Figure 3 for comparison.
Figure 1.
Panel A: Trends in individual cardiovascular risk factors over time among all patients hospitalized for major non-cardiac surgery (p for trend <0.001 for all cardiovascular risk factors). Panel B: Burden of cardiovascular risk factors over time among patients hospitalized for major non-cardiac surgery. Cardiovascular risk factors were defined as ≥1 of the following: hypertension, dyslipidemia, diabetes mellitus, chronic kidney disease, and obesity.
Diagnoses of Atherosclerotic Cardiovascular Disease
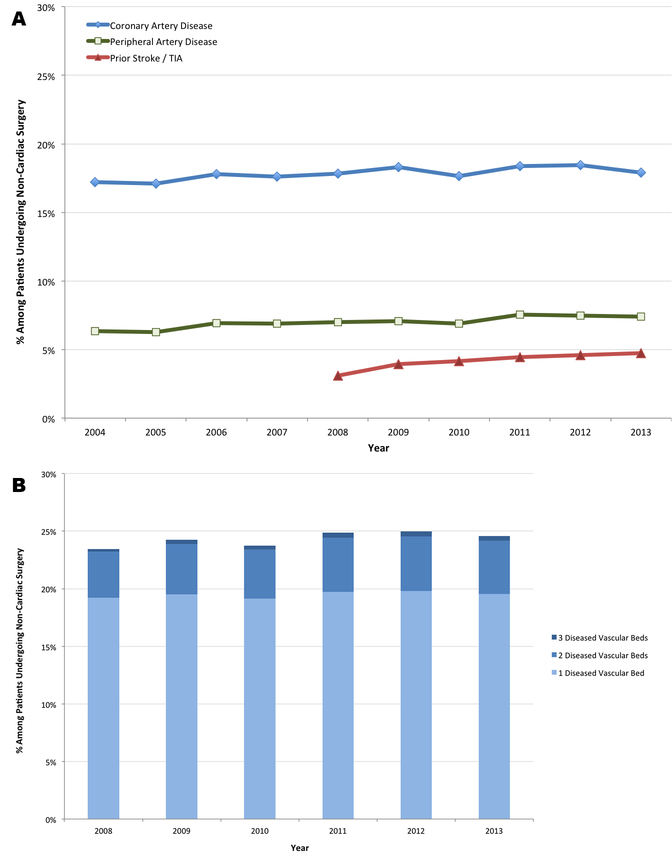
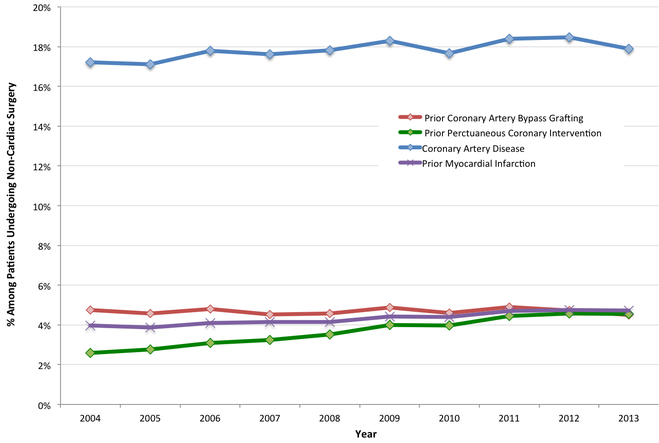
Any diagnosis of ASCVD was present in 24.3% of cases between 2008–2013. The proportion of patients with ASCVD undergoing surgery increased by 0.94% [0.19% annually] during the analysis period, from 23.8% in 2008–2009 to 24.8% in 2012–2013 (p<0.001; RR 1.04, 95% CI 1.04–1.04). The prevalence of coronary artery disease increased by 1.0% [0.11% annually] (17.2% in 2004–2005 vs. 18.2% in 2012–2013, p<0.001; RR 1.06, 95% CI 1.06–1.06), peripheral artery disease increased by 1.1% [0.13% annually] (6.3% in 2004–2005 vs. 7.4% in 2012–2013, p<0.001; RR 1.18, 95% CI 1.18–1.18) and prior stroke or transient ischemic attack increased by 1.2% [0.24% annually] (3.5% in 2008–2009 vs. 4.7% in 2012–2013, p<0.001; RR 1.33, 95% CI 1.33–1.34) over time (Figure 2A). The burden of vascular disease by the number of vascular beds affected is shown in Figure 2B. Trends in cardiovascular disease adjusted for age, sex, and race are shown in Supplementary Figure 4. Among patients undergoing non-cardiac surgery, the proportion of patients with prior MI increased by 0.81% during the analysis period [0.09% annually] (3.9% in 2004–2005 vs. 4.7% in 2012–2013, p<0.001; RR 1.21, 95% CI 1.20–1.21). Although the prevalence of prior revascularization with coronary artery bypass grafting was stable between 2004 and 2013 (4.7% in 2004–2005 vs. 4.6% in 2012–2013, p=0.21; RR 0.99, 95% CI 0.99–1.00), the proportion of patients with prior percutaneous coronary intervention increased by 1.9% [0.21% annually] during this time (2.7% in 2004–2005 vs. 4.6% in 2012–2013, p<0.001; RR 1.71, 95% CI 1.70–1.71) (Figure 3, Supplementary Figures 5 & 6).
Figure 2.
Panel A: Trends in the prevalence of cardiovascular disease (history of CAD, PAD, TIA/CVA) over time among patients hospitalized for major non-cardiac surgery (p for trend <0.001 for CAD, PAD, and prior stroke). Panel B: The burden of cardiovascular disease by number of vascular beds affected (CAD, PAD, Stroke) over time among patients hospitalized for major non-cardiac surgery.
Figure 3.
Trends in CAD, prior myocardial infarction, and coronary revascularization over time among patients hospitalized for major non-cardiac surgery.
P-value for trend <0.001 for prior MI, PCI and CAD and p-value for trend = 0.11 for CABG.
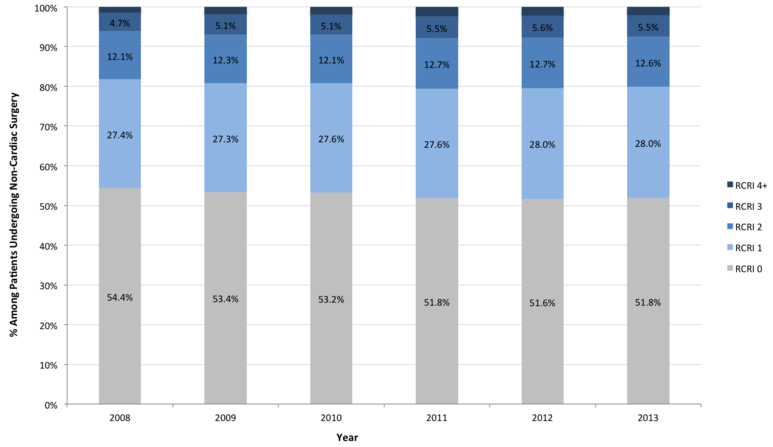
Trends in Estimated Perioperative Risk
Current perioperative care guidelines recommend cardiovascular risk assessment using the Revised Cardiac Risk Index (RCRI) and other clinical risk prediction models.(3–5) The RCRI incorporates ASCVD diagnoses and select cardiovascular risk factors to score surgical candidates on a scale from 0 to 6, with a higher RCRI associated with greater perioperative risk. Between 2008 and 2013, 16,271,712 (52.7%) of subjects undergoing non-cardiac surgery nationwide had a modified RCRI of zero, 8,532,467 (27.6%) had an RCRI of 3,826,977 (12.4%) had an RCRI of 2, and 2,237,066 (7.3%) had an RCRI of ≥3. The proportion of subjects with a modified RCRI score ≥3 increased by 1.1% [0.22% annually] (from 6.6% in 2008–2009 to 7.7% in 2012–2013, p<0.001; RR 1.16, 95% CI 1.16–1.17), as shown in Figure 4.
Figure 4.
Modified Revised Cardiac Risk Index over time among patients hospitalized for major non-cardiac surgery from 2008–2013.
Modified Revised Cardiac Risk Index (RCRI) score using ICD-9 codes for ischemic heart disease, heart failure, prior TIA or stroke, chronic kidney disease, diabetes mellitus, and high-risk surgery. Due to the introduction of an ICD9 diagnosis code for prior stroke or TIA in mid-2007, modified RCRI scores were calculated from 2008–2013 data.
Discussion
In a large national cohort of adults ≥45 years of age undergoing major non-cardiac surgery in the United States, the prevalence of cardiovascular risk factors increased over time. Diagnoses of hypertension, dyslipidemia, diabetes mellitus, and obesity were more common in 2013 in comparison to 2004. The prevalence of ASCVD at the time of non-cardiac surgery increased during the study period. Between 2008 and 2013, the years when modified RCRI scores could be determined, we observed an increase in the proportion of patients at high perioperative cardiovascular risk.
This is the first study to report changes in ASCVD and perioperative cardiovascular risk over time in the overall population of patients undergoing major non-cardiac surgery.
The increasing prevalence of risk factors and cardiovascular disease in the present analysis may be partially explained by recent trends towards outpatient ambulatory surgical procedures for the healthiest surgical candidates, thereby increasing cardiovascular risk profiles of hospitalized surgical patients over time.(7,8) Still, the trends observed in the present analysis appear to be consistent with those described among the adult population at large. In this analysis, for example, the prevalence of hypertension was similar to the corresponding prevalence reported for similar subgroups based on data from the 2011 National Health and Nutrition Examination Survey (NHANES) survey,(9) and trends in the diagnosis of hypertension also grossly mirrored those reported in the general population.(10) Similarly, diabetes mellitus diagnoses increased in the both perioperative and general populations during the study timeframe.(10–12) However, not all trends observed in this surgical cohort correlate with those of the general population. Dyslipidemia, as identified by ICD-9 diagnoses codes, increased markedly between 2004 and 2013 in the present analysis, while significant increases in the age-adjusted prevalence of serum cholesterol ≥200 mg/dL over time were not identified from NHANES data.(10)
In light of data demonstrating steady increases in cardiovascular risk over time, it is surprising that perioperative major adverse cardiovascular events declined from 3.1% to 2.6% between 2004 and 2013, driven by reductions in perioperative death and MI, in a recent report using the same national cohort.(2) The mechanisms of these observed declines in perioperative MACCE are uncertain. Despite increasing cardiovascular risk profiles, improved perioperative outcomes may be attributed to improved medical management of cardiovascular risk factors and atherosclerotic disease (i.e. antiplatelet therapy and/or statins), minimally invasive or less morbid surgical approaches and techniques, improved anesthesia care and hemodynamic management, and advances in post-operative care to promote early mobilization and reduce iatrogenic complications. Additionally, among patients with coronary artery disease, improved guidance regarding perioperative risk prediction, optimal timing of surgery after coronary revascularization, and the appropriate use of antiplatelet therapies in the perioperative period may have contributed to these favorable trends.(13)
Study Limitations
There are a number of limitations to this study. First, the present analysis was performed in a subgroup of adults age ≥45, a population enriched for cardiovascular disease and consistent with clinical trials of patients undergoing non-cardiac surgery.(14) Second, the data are derived from ICD-9 diagnosis codes recorded in a large national administrative database and are subject to reporting bias, errors, and changes in coding practices over time. Increases in the prevalence of cardiovascular risk factors and cardiovascular disease during the study period, for example, may have been affected by local hospital efforts to improve electronic documentation of administrative data and ensure accurate coding of all clinical diagnoses.(15) Even so, ICD-9 diagnosis codes for cardiovascular risk factors may be underreported. As discussed previously, data on stroke or TIA and chronic kidney disease were unavailable for analysis in the earlier years of the study. The prevalence of obesity in this cohort was lower than that reported based on national surveys of the general population, suggesting the potential for under-coding of this risk factor. However, the prevalence of most other cardiovascular risk factors in this cohort are similar to those reported in other large observational studies of patients undergoing major non-cardiac surgery, supporting the validity of these administrative data (Supplementary Table 2).(16,17) Furthermore, the NIS data provides a more complete sample of non-cardiac surgical procedures performed in the United States, with a higher proportion of patients undergoing urgent or emergent surgery, in comparison to prior large prospective cohort studies.(16) Third, increased utilization of diagnostic screening during the study timeframe, including more frequent use of troponin measurement, computed tomography coronary calcium scoring and angiography, stress testing, magnetic resonance angiography, and other imaging modalities to identify vascular disease, may have also affected the reported prevalence of ASCVD. Changes in cardiovascular risk profiles of patients hospitalized for surgery may also be due to the increasing use of ambulatory surgery facilities during this time period.(8) Fourth, the results of clinical laboratory data, including measurements of glucose, lipids, creatinine, or cardiac biomarkers, were not available from this administrative dataset to corroborate trends observed from administrative data. Similarly, in-hospital medical therapy was also not available to confirm coded diagnoses of hypertension, dyslipidemia, diabetes, or ASCVD.
Conclusions:
Atherosclerotic cardiovascular disease was present in nearly 1 of every 4 patients undergoing non-cardiac surgery and cardiovascular risk factors were reported in nearly 3 of every 4 surgical patients. Cardiovascular risk factor burden and the prevalence of ASCVD increased among surgical patients over time. Unfavorable changes in perioperative risk profiles and cardiovascular disease prevalence will likely require renewed attention to ensure continued improvements in perioperative outcomes. Cardiovascular disease specialists may play an expanding role in perioperative care in the years to come.
Supplementary Material
Key Messages:
What is already known about this subject?
Cardiovascular risk factors are prevalent in the population undergoing non-cardiac surgery. Patients undergoing surgery are at risk for cardiovascular events in the post-operative period.
What does this study add?
Among patients undergoing major non-cardiac surgery, the burden of cardiovascular risk factors and the prevalence of ASCVD increased significantly over time.
How might this impact on clinical practice?
Adverse trends in risk profiles require continued attention to improve post-operative cardiovascular outcomes.
Acknowledgments
Sponsor / Funding: NRS was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award 5T32Hl098129–09.
Abbreviations List:
- ASCVD
Atherosclerotic Cardiovascular Disease
- CCS
Clinical Classifications Software
- CABG
Coronary Artery Bypass Grafting
- HCUP
Healthcare Cost and Utilization Project’s
- NIS
National Inpatient Sample
- PCI
Percutaneous Coronary Intervention
- RCRI
Revised Cardiac Risk Index
Footnotes
Disclosures: Dr. Beckman reports serving on advisory boards for AstraZeneca, Sanofi, Aralez, and Abbott Vascular, and has received research grants from Merck. The remainder of the authors report no relationships that could be construed as a conflict of interest.
References:
- 1.Weiser TG, Haynes AB, Molina G et al. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet 2015;385 Suppl 2:S11. [DOI] [PubMed] [Google Scholar]
- 2.Smilowitz NR, Gupta N, Ramakrishna H, Guo Y, Berger JS, Bangalore S. Perioperative Major Adverse Cardiovascular and Cerebrovascular Events Associated With Noncardiac Surgery. JAMA Cardiol 2017;2:181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldman L, Caldera DL, Nussbaum SR et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845–50. [DOI] [PubMed] [Google Scholar]
- 4.Lee TH, Marcantonio ER, Mangione CM et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043–9. [DOI] [PubMed] [Google Scholar]
- 5.Gupta PK, Gupta H, Sundaram A et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation 2011;124:381–7. [DOI] [PubMed] [Google Scholar]
- 6.Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract 2002;5:143–51. [PubMed] [Google Scholar]
- 7.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report 2009:1–25. [PubMed] [Google Scholar]
- 8.Hollenbeck BK, Dunn RL, Suskind AM, Zhang Y, Hollingsworth JM, Birkmeyer JD. Ambulatory surgery centers and outpatient procedure use among Medicare beneficiaries. Med Care 2014;52:926–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief 2013:1–8. [PubMed] [Google Scholar]
- 10.Mozaffarian D, Benjamin EJ, Go AS et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 11.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med 2014;160:517–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng YJ, Imperatore G, Geiss LS et al. Secular changes in the age-specific prevalence of diabetes among U.S. adults: 1988–2010. Diabetes Care 2013;36:2690–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smilowitz NR, Berger JS. Perioperative Management to Reduce Cardiovascular Events. Circulation 2016;133:1125–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Group PS, Devereaux PJ, Yang H et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet 2008;371:1839–47. [DOI] [PubMed] [Google Scholar]
- 15.Abelson R, Creswell J, Palmer G. Medicare Bills Rise as Records Turn Electronic. New York, NY: The New York Times, 2012. [Google Scholar]
- 16.Vascular Events In Noncardiac Surgery Patients Cohort Evaluation Study I, Devereaux PJ, Chan MT et al. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA 2012;307:2295–304. [DOI] [PubMed] [Google Scholar]
- 17.Writing Committee for the VSI, Devereaux PJ, Biccard BM et al. Association of Postoperative High-Sensitivity Troponin Levels With Myocardial Injury and 30-Day Mortality Among Patients Undergoing Noncardiac Surgery. JAMA 2017;317:1642–1651. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.