Abstract
Individuals with schizophrenia or substance use disorder have a substantially increased mortality compared to the general population. Despite a high and probably increasing prevalence of comorbid substance use disorder in people with schizophrenia, the mortality in the comorbid group has been less studied and with contrasting results. We performed a nationwide open cohort study from 2009 to 2015, including all Norwegians aged 20–79 with schizophrenia and/or substance use disorder registered in any specialized health care setting in Norway, a total of 125,744 individuals. There were 12,318 deaths in the cohort, and total, sex-, age- and cause-specific standardized mortality ratios (SMRs) were calculated, comparing the number of deaths in patients with schizophrenia, schizophrenia only, substance use disorder only or a co-occurring diagnosis of schizophrenia and substance use disorder to the number expected if the patients had the age-, sex- and calendar-year specific death rates of the general population. The SMRs were 4.9 (95% CI 4.7–5.1) for all schizophrenia patients, 4.4 (95% CI 4.2–4.6) in patients with schizophrenia without substance use disorder, 6.6 (95% CI 6.5–6.8) in patients with substance use disorder only, and 7.4 (95% CI 7.0–8.2) in patients with both schizophrenia and substance use disorder. The SMRs were elevated in both genders, in all age groups and for all considered causes of death, and most so in the youngest. Approximately 27% of the excess mortality in all patients with schizophrenia was due to the raised mortality in the subgroup with comorbid SUD. The increased mortality in patients with schizophrenia and/or substance use disorder corresponded to more than 10,000 premature deaths, which constituted 84% of all deaths in the cohort. The persistent mortality gap highlights the importance of securing systematic screening and proper access to somatic health care, and a more effective prevention of premature death from external causes in this group.
Introduction
Individuals with schizophrenia have a two- to three-fold increased mortality compared to the general population [1–3] and a 10-20-year reduction in average life span [2, 4–6]. Individuals with substance use disorder (SUD) have an even higher risk of premature death, ranging from a four-fold increased mortality among persons with alcohol use disorder (AUD) [7–10] to a four to-15-fold increased mortality among opioid users [11–13]. A concurrent diagnosis of schizophrenia spectrum disorder (SCZ) and SUD (henceforth referred to as SCZ+SUD) is associated with a variety of detrimental outcomes, among these increased somatic morbidity [14–19], increased risk of fatal overdoses, violent behavior [20–23] and victimization [24, 25]. Despite these vulnerabilities and a high [26, 27], and probably increasing [28], prevalence of comorbid SUD in SCZ patients, the mortality in the comorbid group has been less studied and with contrasting results. Studies of SCZ individuals with co-morbid SUD have found both increased [29–34] and decreased [35] all-cause mortality, increased suicide mortality [36, 37], but no difference in cardiovascular mortality [38] compared to SCZ individuals without SUD. Studies of SUD individuals report both higher [39, 40], similar [12, 13, 40–43], and lower [44] mortality in individuals also diagnosed with a psychotic disorder, compared to individuals with SUD-only, depending on type of SUD and gender [40]. Only a few studies with complete national coverage have investigated all cause [30, 33, 34, 40] or cause-specific mortality [33, 34] in patients with SCZ-only, SUD-only or co-morbid SCZ and SUD, and neither of these reported results for different age groups or mortality from unnatural causes of death.
The aims of the present study were to (i) investigate standardized mortality ratios for all cause mortality (SMRs) in patients with SCZ, SCZ-only, SUD-only and SCZ+SUD, diagnosed in Norwegian psychiatric or somatic specialist health care, (ii) describe how much of the excess mortality that could be attributed to a concurrent diagnosis of SCZ and SUD, and (iii) investigate age-, sex-, and cause-specific SMRs in patients with SCZ-only, SUD-only or SCZ+SUD. We hypothesized that mortality in patients with SCZ and/or SUD would be increased compared to the general population for all main causes of death, and that patients with a concurrent diagnosis of SCZ and SUD would have particularly high SMRs.
Materials and methods
Study population
The study population included all in- and outpatients diagnosed with SCZ and/or SUD in the Norwegian specialized health care system during 2009–2015, who were 20–79 years old when they had their first consultation in the time bracket. Patients with SCZ and/or SUD were identified through the Norwegian Patient Registry (NPR), which is a mandatory national registry covering all patients receiving specialist health care (i.e. government-owned hospitals and outpatient clinics, publicly financed substance use treatment facilities and private health clinics with governmental reimbursement). Since 2009 the coverage in the NPR is almost 100% [45, 46]. The exception is private mental health clinics with governmental reimbursement, where the proportion of the episodes that were reported to the NPR increased from 76% in 2009 [47] to 97% in 2015 [48], but only 0.2% of patients in the present study were treated solely in these clinics. Patients were excluded if an invalid ID number (n = 6,178), a diagnosis of intellectual disability (ICD-10 codes F70-F79) (n = 1,632), or inconsistent data regarding age, gender or emigration date (n = 666) were recorded.
Diagnostic categories
Diagnostic codes in the NPR follow the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) [49]. Patients were included in the SCZ group if a diagnosis of schizophrenia-related disorders (F20-F29) was recorded in the NPR during 2009–2015. The SUD group included patients with a diagnosis of mental and behavioral disorders due to use of psychoactive substances (F10-F19, excluding tobacco (F17)), and patients with at least one somatic diagnosis strongly indicating alcohol abuse (see list of ICD-10 codes in S1 Table). Patients identified by somatic diagnoses only constituted 4.1% of the SUD group. A total of 275 patients treated in substance use treatment facilities, with a diagnosis of SCZ, but no registered diagnosis of SUD (excluding pathological gambling (F63.0)), were included in the SCZ+SUD group. In subgroup analyses, we differentiated between patients with a non-alcohol SUD (F11-F16, F18-F19, Z50.3, Z71.5 and Z72.2), and patients with AUD only. Hard drug use disorder was deemed present if the patient was diagnosed with disorders due to use of opioids (F11), cocaine (F14), other stimulants (mostly amphetamines, F15), hallucinogens (F16), volatile solvents (F18), and multiple drug use and use of other psychoactive substances (F19).
Information on deaths
The Cause of Death Registry (CDR), which includes 98% of all deaths in Norway [50], provided data on the underlying cause of death, based on death certificates issued by physicians. The National Population Registry provided information about year of birth and date of death or emigration. Accurate linkage regarding mortality of the patients was obtained using the unique 11 digit personal ID number included in all the registries. Causes of death were coded according to ICD-10 [49] and divided into natural causes (A00-R99), unnatural causes (V01-Y98) and missing cause of death. Natural causes of death were further divided into cardiovascular (I00-I99), respiratory (J00-J99), cancer (C00-C97) and other natural causes. Unnatural causes of death were divided into poisoning (X40-X49), suicide (X60-X84 and Y87.0) and other unnatural causes.
The reference population included all residents in Norway aged 20–79 during 2009–2015. Annual number of deaths in gender-stratified five-year age groups for the reference population were obtained from the Norwegian Institute of Public Health [51], and annual population figures in the age groups 20–79 in the years 2009–2015 were obtained from Statistics Norway [52].
Follow-up
The study cohort was followed from the admission date of the index episode (their first consultation during 2009–2015). Patients already hospitalized before January 1, 2009, were followed from this date (n = 2,633). To account for diagnostic instability in SCZ patients, we defined an extended diagnostic spectrum covering schizophrenia (F20-F29), affective disorders (F30-F39), and personality disorder (F60). If a diagnosis of SCZ was ever recorded, the index episode was defined as the first episode with a diagnosis within the extended diagnostic spectrum. Follow-up ended on December 31, 2015, on the date of emigration from Norway, on December 31 in the year of the 79th birthday, or on the date of death, whichever came first.
Statistical analysis
For comparison with the mortality of the general population of Norway, SMRs with corresponding 95% confidence intervals were calculated for patients with SCZ, SCZ-only, SUD-only, and SCZ+SUD. SMR reflects the relative mortality of the patient group compared to that of the general population and is computed as the observed number of deaths divided by the expected number of deaths. The expected number of deaths was calculated as the total number of person-years at risk in each sex-, age group- and calendar year band, multiplied by the corresponding age- (5-year age groups), sex- and calendar-year specific (2009–2015) death rate in the general population. Age was defined as attained age at the end of each calendar year, as we did not have access to exact birth dates. Person-years at risk contributed by persons who moved from one age band to the next during follow-up was assigned to the respective sex-, age group- and calendar year bands, using the “lexis” method [53]. The number of excess deaths was calculated as the difference between observed and expected deaths.
Biased SMRs may be a major problem when the prevalence of exposure in the general population is high [54]. In contrast to SCZ, unnatural deaths in the SUD subgroup constitute a large proportion of unnatural deaths in the general population, implicating risk of biased SMRs for unnatural causes of death in this subgroup. We consequently investigated the impact on SMRs for poisoning, suicide and all-cause mortality in patients with SUD (SUD-only and SCZ+SUD combined), using an unexposed comparison group, rather than the general population, for calculation of the expected number of deaths. This unexposed comparison group constituted the Norwegian population excluding subjects with recorded SUD in specialized health care and corresponding deaths from the relevant age-/gender group in the reference population. The mortality rates in this unexposed population was calculated and applied when computing the expected number of deaths.
We also investigated the impact on SMRs of the temporal ordering of SCZ and SUD diagnoses in comorbid patients, and of varying inclusion criteria in a series of pre-specified sensitivity analyses (i) excluding patients treated solely in somatic hospitals during follow-up (e.g. older individuals with presumably stable mental illness suffering from somatic health problems), (ii) excluding patients diagnosed with SCZ as a secondary diagnosis only, and (iii) including only patients diagnosed with narrow schizophrenia (F20) in the SCZ group.
The analyses were conducted using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, N.C.)
Ethics
All patient data were fully de-identified when accessed by the investigators. In Norway, studies with de-identified information from medical health registries do not require participant consent. Legal basis and exemption from professional secrecy requirements for the use of personal health data in research was granted by the regional committee for medical and health research ethics (2014/72/REK nord).
Results
Characteristics of the study population
A total of 125,744 individuals were included in the study during 2009–2015. They were aged 20–79 at start of follow-up. Of these, 27,859 (22.2%) were registered with a diagnosis of SCZ, 20,537 (16.3%) with SCZ-only, 97,885 (77.8%) with SUD-only, and 7,322 (5.8%) with SCZ+SUD (Table 1). Men were overrepresented in the SUD groups (66.6% in SUD-only and 70.1% in SCZ+SUD). In patients with SUD, AUD was most common in patients with SUD-only (66.4%), whereas non-alcohol SUD was most common in comorbid patients (76.5%).
Table 1. Characteristics of the study population.
Patients aged 20–79 with schizophrenia spectrum disorder (SCZ) and/or substance use disorder (SUD).
| SCZ-only | SUD-only | SCZ+SUD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Men | |||||||||
| Patients, n (%) | 10,509 | 65,175 | 5,126 | ||||||
| Personyears, sum | 48,776 | 250,350 | 26,873 | ||||||
| Personyears, mean (SD) | 4.6 | (2.3) | 3.8 | (2.2) | 5.2 | (2.0) | |||
| Age at start of follow-up, mean (SD) | 43.4 | (15.2) | 43.5 | (15.7) | 35.2 | (12.0) | |||
| No. of patients with substance use disorder, n (%) | |||||||||
| Alcohol use disorder | - | 44,198 | (67.8) | 2,230 | (43.5) | ||||
| Alcohol use disorder only | - | 33,917 | (52.0) | 980 | (19.1) | ||||
| Non-alcohol substance use disorder | - | 31,258 | (48.0) | 3,984 | (77.7) | ||||
| Cannabis use disorder | - | 13,688 | (21.0) | 1,805 | (35.2) | ||||
| Hard drug use disorders | - | 23,073 | (35.4) | 3,202 | (62.5) | ||||
| Non-alcohol substance use disorder only | - | 20,977 | (32.2) | 2,734 | (53.3) | ||||
| Unknown substance use disorder | - | 0 | (0.0) | 162 | (3.2) | ||||
| No. of health care episodes per person-year, median (IQR) | |||||||||
| No. of admissions, mental care | 0.2 | (0.0–0.4) | 0.0 | (0.0–0.0) | 0.3 | (0.2–0.6) | |||
| No. of outpatient visits, mental care | 5.6 | (1.1–16.5) | 0.0 | (0.0–2.0) | 7.3 | (1.9–19.0) | |||
| No. of admissions, medical care | 0.0 | (0.0–0.2) | 0.2 | (0.0–0.4) | 0.1 | (0.0–0.3) | |||
| No. of outpatient visits, medical care | 0.6 | (0.0–1.9) | 1.5 | (0.5–4.2) | 0.9 | (0.3–2.0) | |||
| No. of admissions, SUD treatment | - | 0.0 | (0.0–0.2) | 0.0 | (0.0–0.1) | ||||
| No. of outpatient visits, SUD treatment | - | 0.2 | (0.0–3.9) | 0.0 | (0.0–1.8) | ||||
| Women | |||||||||
| Patients, n (%) | 10,028 | 32,710 | 2,196 | ||||||
| Personyears, sum | 45,970 | 126,174 | 11,946 | ||||||
| Personyears, mean (SD) | 4.6 | (2.3) | 3.9 | (2.2) | 5.4 | (1.9) | |||
| Age at start of follow-up, mean (SD) | 47.9 | (16.1) | 42.5 | (16.2) | 39.1 | (14.0) | |||
| No. of patients with substance use disorder, n (%) | |||||||||
| Alcohol use disorder | - | 20,800 | (63.6) | 965 | (43.9) | ||||
| Alcohol use disorder only | - | 15,471 | (47.3) | 442 | (20.1) | ||||
| Non-alcohol substance use disorder | - | 17,239 | (52.7) | 1,641 | (74.7) | ||||
| Cannabis use disorder | - | 4,573 | (14.0) | 433 | (19.7) | ||||
| Hard drug use disorders | - | 11,834 | (36.2) | 1,247 | (56.8) | ||||
| Non-alcohol substance use disorder only | - | 11,910 | (36.4) | 1,118 | (50.9) | ||||
| Unknown substance use disorder | - | 0 | (0.0) | 113 | (5.1) | ||||
| No. of health care episodes per person-year, median (IQR) | |||||||||
| No. of admissions, mental care | 0.2 | (0.0–0.4) | 0.0 | (0.0–0.2) | 0.4 | (0.2–0.7) | |||
| No. of outpatient visits, mental care | 5.8 | (1.2–17.0) | 0.8 | (0.0–6.1) | 8.4 | (2.5–21.6) | |||
| No. of admissions, medical care | 0.1 | (0.0–0.3) | 0.2 | (0.0–0.5) | 0.2 | (0.0–0.5) | |||
| No. of outpatient visits, medical care | 1.0 | (0.2–3.1) | 2.4 | (0.9–6.0) | 1.5 | (0.6–3.3) | |||
| No. of admissions, SUD treatment | - | 0.0 | (0.0–0.0) | 0.0 | (0.0–0.0) | ||||
| No. of outpatient visits, SUD treatment | - | 0.0 | (0.0–3.7) | 0.0 | (0.0–1.6) | ||||
Abbreviations: SCZ, schizophrenia spectrum disorder; SUD, substance use disorder; SCZ+SUD, concurrent diagnoses of schizophrenia and substance use disorder; SD, standard deviation; IQR, interquartile range.
All-cause mortality
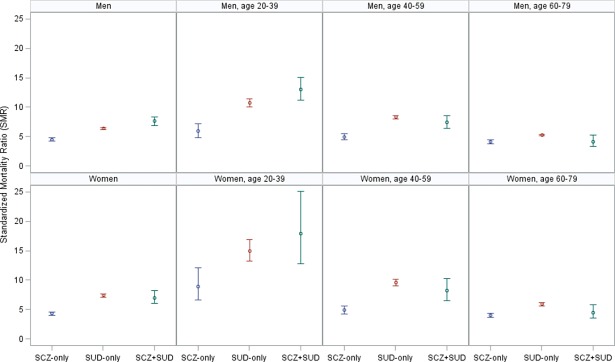
Of the 125,744 individuals included, 12,318 (9.8%) died during follow-up (Table 2). Mean age at death was highest in patients with SCZ-only (62.0 years) and lowest in patients with SCZ+SUD (47.3 years), and particularly low in comorbid men (45.3 years). Comparing with the expected number of deaths based on the mortality of the general population, we found a SMR of 4.9 (95% CI 4.7–5.1) in SCZ patients (with or without SUD), and SMRs of 4.4 (95% CI 4.2–4.6), 6.6 (95% CI 6.5–6.7) and 7.4 (95% CI 6.9–8.1) in patients with SCZ-only, SUD-only, and SCZ+SUD, respectively, corresponding to 10,328 excess deaths (of which 18% were in SCZ patients). In men, the SMRs for patients with SCZ (with or without SUD), SCZ-only, SUD-only, and SCZ+SUD were 5.1 (95% CI 4.8–5.4), 4.5 (95% CI 4.2–4.8), 6.4 (95% CI 6.2–6.5) and 7.6 (95% CI 6.9–8.4), respectively. In women, the corresponding figures were 4.6 (95% CI 4.3–4.9), 4.3 (95% CI 4.0–4.6), 7.4 (95% CI 7.1–7.6) and 7.0 (95% CI 6.0–8.2). All-cause mortality was elevated for both genders and in all age groups (Fig 1), but the SMRs were consistently higher in the youngest age groups. Women aged 20–39 years with SUD had particularly high SMRs; 15 in the SUD-only group and 18 in the SCZ+SUD group.
Table 2. Number of deaths (overall and in different age groups) and mean age of death, according to sex.
Patients aged 20–79 with schizophrenia spectrum disorder (SCZ) and/or substance use disorder (SUD).
| SCZ-only | SUD-only | SCZ+SUD | ||||||
|---|---|---|---|---|---|---|---|---|
| Men | ||||||||
| Deaths, n | 972 | 7,334 | 423 | |||||
| Age at death 20–39, n (%) | 90 | (9.3) | 847 | (11.5) | 170 | (40.2) | ||
| Age at death 40–59, n (%) | 295 | (30.3) | 2,445 | (33.3) | 171 | (40.4) | ||
| Age at death 60–79, n (%) | 587 | (60.4) | 4,042 | (55.1) | 82 | (19.4) | ||
| Age at death, mean (SD) | 60.3 | (13.6) | 58.6 | (13.7) | 45.3 | (14.2) | ||
| Women | ||||||||
| Deaths, n | 832 | 2,592 | 165 | |||||
| Age at death 20–39, n (%) | 42 | (5.0) | 256 | (9.9) | 34 | (20.6) | ||
| Age at death 40–59, n (%) | 198 | (23.8) | 928 | (35.8) | 75 | (45.5) | ||
| Age at death 60–79, n (%) | 592 | (71.2) | 1,408 | (54.3) | 56 | (33.9) | ||
| Age at death, mean (SD) | 64.0 | (12.3) | 59.0 | (13.6) | 52.5 | (14.2) | ||
Abbreviations: SCZ, schizophrenia spectrum disorder; SUD, substance use disorder; SCZ+SUD, concurrent diagnoses of schizophrenia and substance use disorder; SD, standard deviation.
Fig 1. All-cause age, gender, and calendar-year standardized mortality ratios according to gender and age among patients with schizophrenia and/or substance use disorders.
Sensitivity analyses (i) excluding patients treated solely in somatic hospitals during follow-up, or (ii) patients with a secondary diagnosis of SCZ only indicated decreased SMRs for SCZ-only (both models) and SUD-only (model ii), whereas application of a narrow definition of SCZ (F20) (model iii) resulted in moderately increased SMRs for SCZ-only (S2 Table).
Impact of a concurrent diagnosis of SCZ and SUD
Overall, comorbid patients had higher all-cause SMRs than patients with SCZ-only or SUD-only. However, when stratified according to sex and type of SUD (Table 3), SMRs were similar in SUD patients with or without comorbid SCZ, except in comorbid men with a non-alcohol SUD who had higher SMR than men with non-alcohol SUD-only. Comorbid patients aged 20–39, 40–59 and 60–69 had 107%, 57% and 6% higher numbers of deaths compared to what could be expected if the same age-specific SMRs as patients with SCZ-only had applied, whereas application of age-specific SMRs for SUD-only in the comorbid had smaller impact on hypothetical numbers of death. Thus, the major reason for the high SMRs in comorbid patients was the SUD component. In this total Norwegian patient population, approximately 27% of the excess number of deaths in all patients with SCZ was due to the raised mortality in the subgroup with comorbid SUD. This effect was strongest in men and in the youngest.
Table 3. All-cause age, gender, and calendar-year standardized mortality ratios among patients aged 20–79 with substance use disorders only (SUD-only) or concurrent SUD and schizophrenia related disorders (SCZ+SUD), according to type of SUD.
| SUD-only | SCZ+SUD | ||||||
|---|---|---|---|---|---|---|---|
| Obs | SMRa | (95% CI) | Obs | SMRa | (95% CI) | ||
| Men | 7,334 | 6.4 | (6.2–6.5) | 423 | 7.6 | (6.9–8.3) | |
| AUD-only | 5,109 | 5.9 | (5.7–6.0) | 120 | 5.4 | (4.5–6.4) | |
| Non-alcohol SUD | 2,225 | 8.0 | (7.7–8.3) | 295 | 9.4 | (8.4–10.5) | |
| Unknown SUD | 0 | 8 | 4.0 | (2.0–8.0) | |||
| Women | 2,592 | 7.4 | (7.1–7.7) | 165 | 7.0 | (6.0–8.2) | |
| AUD-only | 1,520 | 7.0 | (6.6–7.3) | 47 | 6.4 | (4.8–8.5) | |
| Non-alcohol SUD | 1,072 | 8.0 | (7.5–8.5) | 111 | 7.4 | (6.1–8.9) | |
| Unknown SUD | 0 | 7 | 6.9 | (3.3–14.4) | |||
Abbreviations: SUD, substance use disorder; SCZ+SUD, concurrent diagnoses of schizophrenia and substance use disorder; Obs, observed deaths; SMR, standardized mortality ratio; 95% CI, 95% confidence interval; AUD, Alcohol Use Disorder.
a The standard population used for the sex- and calendar year specific age standardization was the annual population of Norway aged 20–79 in the years 2009–2015.
Supplementary analyses examining the temporal ordering of SCZ and SUD diagnoses in comorbid patients showed that SCZ and SUD were mostly co-occurring: 39% had both diagnoses within three months, 55% within one year and 70% within two years. One in four comorbid patients had a SUD diagnosis more than three months prior to the SCZ diagnosis, whereas 36% had a SCZ diagnosis more than three months prior to the SUD diagnosis. The SMRs tended to be higher when the SUD diagnosis preceded the SCZ diagnosis, and were highest when the first diagnosis of SCZ and SUD during follow-up were recorded within a short time interval (S3 Table).
Cause specific mortality
We found elevated mortality from all considered causes of death in all subgroups (Table 4). In both men and women, the highest SMRs were observed for poisoning, suicides and respiratory diseases. Women had higher SMRs for unnatural death than men in all age groups, and higher SMRs for suicides. SMRs for natural causes of death did not differ much with age neither for men nor for women. For unnatural causes of death, SMRs in people with SCZ-only were stable across age groups, except in women aged 20–39, who had elevated SMRs compared to other age groups. In patients with SUD, SMRs in the age group 20–59 were elevated compared to age 60–79, except in comorbid women who had a 30-fold increased SMR across all age groups. Overall, 73% of excess number of deaths were from natural causes. In SCZ-only and SUD-only, natural causes accounted for 82% and 73% of all deaths, respectively, with cancer and cardiovascular disease being the most common causes. In the SCZ+SUD group, unnatural causes accounted for 54% of all deaths. Women with SUD-only had higher SMRs than men with SUD-only for nearly all considered causes of death. Women with SUD (with or without SCZ) had particularly high SMRs (approximately 45) for poisoning.
Table 4. Cause-specific age, gender, and calendar-year standardized mortality ratios among men and women aged 20–79 with schizophrenia-related disorders (SCZ) and/or substance use disorders (SUD).
| SCZ-only | SUD-only | SCZ+SUD | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs | SMRa | 95% CI | Obs | SMRa | 95% CI | Obs | SMRa | 95% CI | |||||
| Men | |||||||||||||
| Natural causes | 775 | 4.2 | (3.9–4.5) | 5,293 | 5.4 | (5.3–5.6) | 182 | 4.6 | (4.0–5.3) | ||||
| Age 20–39 | 17 | 3.3 | (2.1–5.3) | 141 | 5.5 | (4.6–6.4) | 24 | 5.7 | (3.8–8.5) | ||||
| Age 40–59 | 211 | 4.7 | (4.1–5.3) | 1,555 | 6.9 | (6.6–7.2) | 86 | 5.1 | (4.1–6.3) | ||||
| Age 60–79 | 547 | 4.1 | (3.8–4.5) | 3,597 | 5.0 | (4.8–5.2) | 72 | 3.9 | (3.1–5.0) | ||||
| Subtype | |||||||||||||
| Cardiovascular | 200 | 3.9 | (3.4–4.5) | 1,252 | 4.7 | (4.4–4.9) | 35 | 3.3 | (2.4–4.6) | ||||
| Respiratory | 123 | 8.5 | (7.1–10.1) | 617 | 8.0 | (7.4–8.7) | 30 | 13.1 | (9.1–18.7) | ||||
| Cancer | 197 | 2.6 | (2.3–3.0) | 1,180 | 2.9 | (2.7–3.1) | 30 | 1.9 | (1.3–2.7) | ||||
| Other | 255 | 6.1 | (5.4–6.9) | 2,244 | 10.2 | (9.8–10.7) | 87 | 8.3 | (6.7–10.3) | ||||
| Unnatural causes | 186 | 6.9 | (5.9–7.9) | 1,837 | 13.3 | (12.7–13.9) | 228 | 16.3 | (14.3–18.5) | ||||
| Age 20–39 | 72 | 7.8 | (6.2–9.8) | 684 | 14.1 | (13.1–15.2) | 140 | 17.4 | (14.8–20.6) | ||||
| Age 40–59 | 76 | 6.4 | (5.1–8.0) | 807 | 14.2 | (13.3–15.3) | 81 | 16.0 | (12.9–19.9) | ||||
| Age 60–79 | 38 | 6.4 | (4.6–8.7) | 346 | 10.4 | (9.4–11.6) | 7 | 7.6 | (3.6–16.0) | ||||
| Subtype | |||||||||||||
| Poisoning | 30 | 4.6 | (3.2–6.5) | 903 | 27.5 | (25.8–29.3) | 115 | 29.0 | (24.2–34.9) | ||||
| Suicide | 115 | 11.6 | (9.7–13.9) | 499 | 9.9 | (9.0–10.8) | 87 | 16.0 | (13.0–19.8) | ||||
| Other | 41 | 3.8 | (2.8–5.2) | 435 | 7.9 | (7.2–8.7) | 26 | 5.6 | (3.8–8.3) | ||||
| Missing | 11 | 1.6 | (0.9–2.8) | 204 | 5.4 | (4.7–6.2) | 13 | 5.5 | (3.2–9.5) | ||||
| Women | |||||||||||||
| Natural causes | 703 | 3.9 | (3.6–4.2) | 1,921 | 6.0 | (5.8–6.3) | 90 | 4.4 | (3.6–5.4) | ||||
| Age 20–39 | 8 | 3.0 | (1.5–6.0) | 46 | 5.2 | (3.9–7.0) | 8 | 7.9 | (4.0–15.8) | ||||
| Age 40–59 | 146 | 4.2 | (3.6–4.9) | 608 | 7.4 | (6.8–8.0) | 40 | 5.2 | (3.8–7.0) | ||||
| Age 60–79 | 549 | 3.9 | (3.6–4.2) | 1,267 | 5.6 | (5.3–5.9) | 42 | 3.6 | (2.6–4.8) | ||||
| Subtype | |||||||||||||
| Cardiovascular | 150 | 4.3 | (3.7–5.1) | 306 | 5.4 | (4.8–6.1) | 17 | 5.1 | (3.2–8.2) | ||||
| Respiratory | 126 | 7.1 | (6.0–8.4) | 292 | 10.0 | (8.9–11.2) | 22 | 13.4 | (8.9–20.4) | ||||
| Cancer | 239 | 2.7 | (2.4–3.1) | 451 | 2.8 | (2.5–3.0) | 19 | 1.7 | (1.1–2.7) | ||||
| Other | 188 | 4.7 | (4.1–5.5) | 872 | 12.6 | (11.8–13.4) | 32 | 7.2 | (5.1–10.1) | ||||
| Unnatural causes | 113 | 9.9 | (8.2–11.9) | 629 | 23.2 | (21.4–25.0) | 74 | 30.9 | (24.6–38.9) | ||||
| Age 20–39 | 29 | 15.7 | (10.9–22.6) | 201 | 26.7 | (23.2–30.6) | 26 | 32.4 | (22.1–47.7) | ||||
| Age 40–59 | 47 | 9.7 | (7.3–12.9) | 305 | 25.8 | (23.1–28.9) | 35 | 29.9 | (21.5–41.7) | ||||
| Age 60–79 | 37 | 7.8 | (5.7–10.8) | 123 | 15.8 | (13.2–18.8) | 13 | 30.9 | (18.0–53.3) | ||||
| Subtype | |||||||||||||
| Poisoning | 11 | 5.1 | (2.8–9.2) | 263 | 44.7 | (39.6–50.4) | 25 | 43.5 | (29.4–64.4) | ||||
| Suicide | 77 | 19.0 | (15.2–23.8) | 248 | 22.7 | (20.0–25.7) | 38 | 36.7 | (26.7–50.4) | ||||
| Other | 25 | 4.8 | (3.2–7.1) | 118 | 11.4 | (9.5–13.7) | 11 | 14.1 | (7.8–25.4) | ||||
| Missing | 16 | 5.0 | (3.1–8.2) | 42 | 6.7 | (5.0–9.1) | 1 | nr | nr | ||||
Abbreviations: Obs, observed deaths; SMR, standardized mortality ratio; 95% CI, 95% confidence interval; nr, Not reportable because of small samples (no. of deaths < 5) within the data category.
a The standard population used for the sex- and calendar year specific age standardization was the annual population of Norway aged 20–79 in the years 2009–2015.
Deaths due to poisoning and suicide in SUD patients in our sample constituted a large proportion of all deaths from these causes in Norway in the years 2009–2015 (52% and 22%, respectively). In a supplementary analysis we assessed the bias in SMRs for poisoning and suicide for patients with SUD (SUD-only and SCZ+SUD combined) using an unexposed comparison group (e.g. no diagnosis of SUD in specialized health care), rather than the general population, to calculate expected deaths. This resulted in a three-fold increase in SMR for poisoning in men and a doubled SMR for poisoning in women (from 27.7 to 82.9 in men, and from 44.6 to 98.5 in women), whereas SMRs for suicides increased from 10.5 to 13.7 in men and from 23.9 to 33.8 in women. The SMRs for all-cause mortality were also affected (increased from 6.4 to 7.3 in men, and from 7.3 to 7.9 in women).
Discussion
Our study shows that patients in specialized health care with SCZ, SCZ-only or SUD (with or without SCZ) had a five-, four- and seven-fold increased total mortality, respectively, compared to the general population. Mortality was elevated for both genders, in all age groups and for all considered causes of death, with the highest SMRs observed for poisoning, suicides and respiratory diseases. Very high SMRs for poisoning were noted in women with SUD (with or without SCZ). The highest SMRs were found in the age group 20–39, mainly due to unnatural causes of death.
The excess mortality corresponded to more than 10 000 premature deaths (84% of all deaths in the cohort). About 27% of the excess deaths in SCZ patients could be attributed to SUD (or factors associated with SUD). The nearly five-fold increased mortality in SCZ (with and without SUD) was substantially higher than reported in meta-analyses [1, 55], and also higher than reported in a recent Nordic study [56]. The omission of patients in primary care, and the relatively short follow-up, may have led to a selection of more severe cases, oversampling patients with many health care episodes and patients with increased suicide risk. Inclusion of older individuals suffering from somatic health problems, such as cardiovascular and respiratory diseases, is another explanation of the elevated SMR in SCZ patients, as shown in the sensitivity analysis. Differences in case finding criteria might also have contributed, also shown in the sensitivity analyses, whereas survivor bias resulting from inclusion of prevalent cases would have the opposite effect. Also, catchment of SCZ might be higher in Norway compared to countries without universal health care. Another contributing explanation might be the rising mortality gap in schizophrenia patients compared to the general population reported in recent studies [1, 57, 58], partly explained by decreased mortality from cardiovascular disease in the general population [59, 60].
The increased all cause and suicide mortality, as well as the similar cardiovascular mortality in comorbid patients, is in accordance with some previous studies [29–34, 38], but not in line with a study reporting decreased mortality in persons with co-occurring psychosis and cannabis use/abuse, compared to psychosis only [35]. In the present study, mortality from cannabis use disorder was not studied separately, due to few deaths and suspicion of selective recording of less severe cases in comorbid patients.
Overall, a co-occurring diagnosis of SCZ also conferred increased SMRs in SUD patients. However, when stratified according to type of SUD, we found similar SMRs for non-alcohol SUD patients with and without SCZ, in accordance with other studies [12, 13, 41, 42], and similar SMRs in AUD patients with and without SCZ, in contrast to a 50-year follow-up study of AUD persons [39]. Differences in length of follow-up may be one explanation for the latter finding. Furthermore, when stratified according to gender, we found increased SMR in comorbid men, but not in comorbid women, in accordance with a study conducted in inpatients [40]. Thus, in our study, the increased SMRs in comorbid patients, both genders combined, was explained by the high proportion of young comorbid men with a non-alcohol SUD. The eight-to-nine-fold increased SMR in patients with non-alcohol SUD with and without SCZ, is similar to [61] or higher than [12, 31] reported elsewhere. Norway has one of the highest rates of injecting drug users among hard drug users [62], which may have contributed to this finding.
The very high all cause SMRs found among young patients were similar to [63] or higher than [31, 64] reported earlier. Previous studies have found excess mortality to be highest the year following a first diagnosis of severe mental illness, due to increased mortality from unnatural causes of death [2, 65]. Besides low expected death rates in the youngest in the general population, the inverse relationship between the SMR and age may thus partly be explained by the inclusion of presumably more incident cases in the youngest and more prevalent cases among the oldest in our study, and may have been amplified by survivor bias, treatment-compliant patients in our sample and lower suicide rates with increasing age in SCZ patients [66]. Comorbid women did not, however, experience a decrease in SMR with increasing age, but had very high mortality across all age groups. We found very high SMRs for poisoning and suicide in women with SUD, which confirms earlier findings [60, 67], and high SMRs for respiratory diseases, probably associated with increased smoking prevalence in individuals with severe mental disorders [68]. The increased mortality due to suicide in patients with SCZ was more pronounced than reported in a systematic review [1], but of similar magnitude as reported in a sample with comparable age span [37].
The excess mortality in patients with severe mental illness has been ascribed to a wide range of factors, both at the individual level, health system level and at the societal level [69]. Explanations include lifestyle factors [38, 70] (such as smoking, substance use, physical inactivity and unhealthy diet), poorer socioeconomic conditions [71], suboptimal use of or access to medical care [72], and metabolic side effects of high dosages of antipsychotic medication [73], as well as higher levels of suicides, poisoning, violent behavior [20–23] and victimization [24, 25]. It is thus a huge challenge to address the complex needs of patients with severe mental illness in combination with SUD, both with regard to general improvement of outcome as well as prevention of premature mortality. Despite the well known high association between SUD and SCZ there is no evidence supporting one specific treatment strategy for patients with dual diagnoses [69, 74, 75]. Likewise, there is little evidence for successful interventions addressing somatic risk factors in patients with severe mental disorders [70, 76], although evidence-based interventions for smoking cessation and weight reduction in persons with severe mental illness exist [69]. The universal health care system in Norway, designed to prevent socioeconomic differences in health care, has unfortunately not been able to address these issues. Generally, a population approach for prevention is considered the key avenue for non-communicable diseases, e.g. cardiovascular diseases and cancer [77]. The patients here studied clearly constitute a high-risk group, but there is limited knowledge of effective intervention and treatment strategies to use with these vulnerable patients [4]. An approach that includes both individual focused and system focused interventions is probably needed, involving both primary and integrated specialist health care. Further research is needed to pinpoint effective system focused interventions specifically aiming at reaching the high-risk subgroup with mental illness. The extremely high mortality risk in young patients highlights the need for such efforts to be implemented in the younger age groups.
Strengths and limitations
The major strength of this study is the use of unselected and complete nationwide registry data of recent date, covering all specialist health care settings, and with no bias associated with selective self-reporting. The inclusion of outpatients and patients treated solely in somatic hospitals also enabled more generalizable risk estimates. The CDR is found to provide high quality data on the underlying cause of death [78]. Also, the validity of a schizophrenia diagnosis in hospital case registries is good when compared to diagnoses based on structured research interviews [79, 80]. Furthermore, in Norway, treatment of psychosis is mainly a specialist task, with free admission to hospital treatment and a maximum annual cost of 2205 NOK (approximately 235 €) for outpatient treatment, implying high coverage for SCZ in the NPR.
The relatively short follow-up is a limitation, which also precluded analysis of secular trends in SMRs. Another important limitation is the lack of control for unmeasured individual risk factors associated with mortality. However, studies adjusting for such factors [30, 38, 81] still revealed an increased mortality after adjustment. The SMRs in the current study may be prone both to under- and overestimation. We found underestimated SMRs for unnatural causes of death in SUD patients when the general population, rather than an unexposed population, was used as reference. Survivor bias in comorbid patients may also have resulted in underestimation, as patients would have to live long enough to receive both diagnoses. On the other hand, underreporting of less severe SUD in specialized care may have led to overestimated SMRs in all groups, although a higher detection rate of less severe SUD in comorbid patients (Berkson’s bias) may be suspected. SCZ and SUD were identified independently of time, ignoring the possibility that the two diagnoses were not co-occurring. However, supplementary analyses showed that a majority of comorbid patients had both diagnosed within a year. We were not able to differentiate between patients with a primary psychotic disorder that co-occurs with SUD and patients with substance-induced psychosis, although we found indications that patients with a SUD diagnosis preceding SCZ had worse outcomes. We found a 26% prevalence of SUD in SCZ patients during a mean follow-up of four years, which is similar to a previous Norwegian study [27] SUD diagnoses in the NPR have not been subject to formal validity checks [80], but a Norwegian validation study found hospital diagnosis of SUD to be fairly valid, although only 31% classified with SUD by expert opinion was identified in administrative data [79] Another Nordic study found nearly 50% underreporting of SUD in individuals with schizophrenia in the Danish Psychiatric Register [82]. However, a sensitivity analysis identifying SUD patients from hospital data only did not change results appreciably in the study by Hjorthøj et al [30]. We had no information concerning frequency and level of past and current substance abuse, nor information concerning prescriptions for treatment of SUD. Finally, this study included only patients in specialized health care, possibly implying higher mortality than would be found among patients with SCZ and/or SUD in the general population. The generalizability of these findings is therefore to specialized care settings with similar health care systems and socioeconomic features.
Conclusion
Our study demonstrates that patients with SCZ and/or SUD who receives specialized health care have a substantially elevated risk of premature mortality compared to the general population for both natural and unnatural causes of death. The high mortality in these vulnerable patients, and the differences in causes of death between the subgroups in our study, call for complex intervention strategies addressing several aspects of prevention, follow-up and treatment at all levels of primary and specialist health care. Young patients and women with SUD (with or without SCZ) have for unnatural causes particularly high mortality compared to the general population. The high proportion of deaths directly linked to poisoning in SUD patients urgently calls for a more effective societal prevention of SUD-related unnatural deaths.
Disclaimer
Data from the Norwegian Patient Registry have been used in this publication. The interpretation and reporting of these data are the sole responsibility of the authors, and no endorsement by the Norwegian Patient Registry is intended nor should be inferred.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Data Availability
Confidentiality requirements according to Norwegian law prevents sharing of individual patient level data in public repositories. Application of legal basis and exemption from professional secrecy requirements for the use of personal health data in research may be sent to a regional committee for medical and health research ethics (https://helseforskning.etikkom.no/), and requests for the data to The Norwegian Patient Registry (https://helsedirektoratet.no/English) and the Cause of Death Registry (https://www.fhi.no/en/). Information on annual number of deaths by sex, age and cause of death are freely available at http://statistikkbank.fhi.no/webview, and annual population numbers freely available at http://statistikkbank.fhi.no.
Funding Statement
The study is funded by a research grant offered by the Regional Health Authorities in Northern Norway. Grant number: PFP1236-15. URL: https://helse-nord.no/. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123–31. Epub 2007/10/03. 10.1001/archpsyc.64.10.1123 . [DOI] [PubMed] [Google Scholar]
- 2.Nordentoft M, Wahlbeck K, Hällgren J, Westman J, Ösby U, Alinaghizadeh H, et al. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. 2013;8(1):e55176 Epub 2013/02/02. 10.1371/journal.pone.0055176 ; PubMed Central PMCID: PMCPmc3555866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature Mortality Among Adults With Schizophrenia in the United States. JAMA Psychiatry. 2015:1–10. Epub 2015/10/29. 10.1001/jamapsychiatry.2015.1737 . [DOI] [PubMed] [Google Scholar]
- 4.Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. The lancet Psychiatry. 2017. Epub 2017/02/27. 10.1016/s2215-0366(17)30078-0 . [DOI] [PubMed] [Google Scholar]
- 5.Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One. 2011;6(5):e19590 Epub 2011/05/26. 10.1371/journal.pone.0019590 ; PubMed Central PMCID: PMCPmc3097201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. Bmj. 2013;346:f2539 Epub 2013/05/23. 10.1136/bmj.f2539 ; PubMed Central PMCID: PMCPmc3660620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–60. Epub 2014/06/04. 10.1002/wps.20128 ; PubMed Central PMCID: PMCPmc4102288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roerecke M, Rehm J. Alcohol use disorders and mortality: a systematic review and meta-analysis. Addiction (Abingdon, England). 2013;108(9):1562–78. Epub 2013/05/01. 10.1111/add.12231 . [DOI] [PubMed] [Google Scholar]
- 9.Wahlbeck K, Westman J, Nordentoft M, Gissler M, Laursen TM. Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. The British journal of psychiatry: the journal of mental science. 2011;199(6):453–8. Epub 2011/05/20. 10.1192/bjp.bp.110.085100 . [DOI] [PubMed] [Google Scholar]
- 10.Westman J, Wahlbeck K, Laursen TM, Gissler M, Nordentoft M, Hällgren J, et al. Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland and Sweden. Acta Psychiatr Scand. 2015;131(4):297–306. Epub 2014/09/23. 10.1111/acps.12330 ; PubMed Central PMCID: PMCPmc4402015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Degenhardt L, Bucello C, Mathers B, Briegleb C, Ali H, Hickman M, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction (Abingdon, England). 2010;106(1):32–51. Epub 2010/11/09. 10.1111/j.1360-0443.2010.03140.x . [DOI] [PubMed] [Google Scholar]
- 12.Arendt M, Munk-Jørgensen P, Sher L, Jensen SO. Mortality among individuals with cannabis, cocaine, amphetamine, MDMA, and opioid use disorders: a nationwide follow-up study of Danish substance users in treatment. Drug and alcohol dependence. 2011;114(2–3):134–9. Epub 2010/10/26. 10.1016/j.drugalcdep.2010.09.013 . [DOI] [PubMed] [Google Scholar]
- 13.Bogdanowicz KM, Stewart R, Broadbent M, Hatch SL, Hotopf M, Strang J, et al. Double trouble: Psychiatric comorbidity and opioid addiction-all-cause and cause-specific mortality. Drug and alcohol dependence. 2015;148:85–92. Epub 2015/01/13. 10.1016/j.drugalcdep.2014.12.025 . [DOI] [PubMed] [Google Scholar]
- 14.Esse K, Fossati-Bellani M, Traylor A, Martin-Schild S. Epidemic of illicit drug use, mechanisms of action/addiction and stroke as a health hazard. Brain and behavior. 2011;1(1):44–54. Epub 2012/03/09. 10.1002/brb3.7 ; PubMed Central PMCID: PMCPMC3217673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Batki SL, Meszaros ZS, Strutynski K, Dimmock JA, Leontieva L, Ploutz-Snyder R, et al. Medical comorbidity in patients with schizophrenia and alcohol dependence. Schizophr Res. 2009;107(2–3):139–46. Epub 2008/11/22. 10.1016/j.schres.2008.10.016 ; PubMed Central PMCID: PMCPmc2649875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dickey B, Normand SL, Weiss RD, Drake RE, Azeni H. Medical morbidity, mental illness, and substance use disorders. Psychiatric services (Washington, DC). 2002;53(7):861–7. Epub 2002/07/04. 10.1176/appi.ps.53.7.861 . [DOI] [PubMed] [Google Scholar]
- 17.Adrian M, Barry SJ. Physical and mental health problems associated with the use of alcohol and drugs. Substance use & misuse. 2003;38(11–13):1575–614. Epub 2003/10/30. . [DOI] [PubMed] [Google Scholar]
- 18.Maraj S, Figueredo VM, Lynn Morris D. Cocaine and the heart. Clinical cardiology. 2010;33(5):264–9. Epub 2010/06/01. 10.1002/clc.20746 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frasch K, Larsen JI, Cordes J, Jacobsen B, Wallenstein Jensen SO, Lauber C, et al. Physical illness in psychiatric inpatients: comparison of patients with and without substance use disorders. The International journal of social psychiatry. 2013;59(8):757–64. Epub 2012/10/05. 10.1177/0020764012456803 . [DOI] [PubMed] [Google Scholar]
- 20.Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS medicine. 2009;6(8):e1000120 Epub 2009/08/12. 10.1371/journal.pmed.1000120 ; PubMed Central PMCID: PMCPmc2718581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Volavka J. Violence in schizophrenia and bipolar disorder. Psychiatria Danubina. 2013;25(1):24–33. Epub 2013/03/09. . [PubMed] [Google Scholar]
- 22.Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PLoS One. 2013;8(2):e55942 Epub 2013/02/19. 10.1371/journal.pone.0055942 ; PubMed Central PMCID: PMCPmc3572179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Large M, Mullin K, Gupta P, Harris A, Nielssen O. Systematic meta-analysis of outcomes associated with psychosis and co-morbid substance use. The Australian and New Zealand journal of psychiatry. 2014;48(5):418–32. Epub 2014/03/05. 10.1177/0004867414525838 . [DOI] [PubMed] [Google Scholar]
- 24.Latalova K, Kamaradova D, Prasko J. Violent victimization of adult patients with severe mental illness: a systematic review. Neuropsychiatric disease and treatment. 2014;10:1925–39. Epub 2014/10/23. 10.2147/NDT.S68321 ; PubMed Central PMCID: PMCPmc4200170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maniglio R. Severe mental illness and criminal victimization: a systematic review. Acta Psychiatr Scand. 2009;119(3):180–91. Epub 2008/11/20. 10.1111/j.1600-0447.2008.01300.x . [DOI] [PubMed] [Google Scholar]
- 26.Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiatry. 2014;71(3):248–54. Epub 2014/01/03. 10.1001/jamapsychiatry.2013.3726 ; PubMed Central PMCID: PMCPmc4060740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nesvåg R, Knudsen GP, Bakken IJ, Høye A, Ystrom E, Surén P, et al. Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: a registry-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(8):1267–76. Epub 2015/02/15. 10.1007/s00127-015-1025-2 . [DOI] [PubMed] [Google Scholar]
- 28.Westermeyer J. Comorbid schizophrenia and substance abuse: a review of epidemiology and course. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2006;15(5):345–55. Epub 2006/09/13. 10.1080/10550490600860114 . [DOI] [PubMed] [Google Scholar]
- 29.Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia—a 15-year follow-up study: dual diagnosis over 15 years. Schizophr Res. 2011;130(1–3):228–33. Epub 2011/05/20. 10.1016/j.schres.2011.04.011 . [DOI] [PubMed] [Google Scholar]
- 30.Hjorthøj C, Østergaard ML, Benros ME, Toftdahl NG, Erlangsen A, Andersen JT, et al. Association between alcohol and substance use disorders and all-cause and cause-specific mortality in schizophrenia, bipolar disorder, and unipolar depression: a nationwide, prospective, register-based study. The lancet Psychiatry. 2015;2(9):801–8. Epub 2015/08/19. 10.1016/S2215-0366(15)00207-2 . [DOI] [PubMed] [Google Scholar]
- 31.Reininghaus U, Dutta R, Dazzan P, Doody GA, Fearon P, Lappin J, et al. Mortality in schizophrenia and other psychoses: a 10-year follow-up of the ÆSOP first-episode cohort. Schizophr Bull. 2015;41(3):664–73. Epub 2014/09/30. 10.1093/schbul/sbu138 ; PubMed Central PMCID: PMCPmc4393685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Allgulander C. Psychoactive drug use in a general population sample, Sweden: correlates with perceived health, psychiatric diagnoses, and mortality in an automated record-linkage study. Am J Public Health. 1989;79(8):1006–10. Epub 1989/08/01. ; PubMed Central PMCID: PMCPmc1349896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Björkenstam E, Ljung R, Burström B, Mittendorfer-Rutz E, Hallqvist J, Weitoft GR. Quality of medical care and excess mortality in psychiatric patients—a nationwide register-based study in Sweden. BMJ Open. 2012;2:e000778 Epub 2012/03/01. 10.1136/bmjopen-2011-000778 ; PubMed Central PMCID: PMCPmc3289986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lumme S, Pirkola S, Manderbacka K, Keskimaki I. Excess Mortality in Patients with Severe Mental Disorders in 1996–2010 in Finland. PLoS One. 2016;11(3):e0152223 Epub 2016/03/25. 10.1371/journal.pone.0152223 ; PubMed Central PMCID: PMCPmc4807083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Koola MM, McMahon RP, Wehring HJ, Liu F, Mackowick KM, Warren KR, et al. Alcohol and cannabis use and mortality in people with schizophrenia and related psychotic disorders. J Psychiatr Res. 2012;46(8):987–93. Epub 2012/05/19. 10.1016/j.jpsychires.2012.04.019 ; PubMed Central PMCID: PMCPmc3392453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Björkenstam C, Björkenstam E, Hjern A, Bodén R, Reutfors J. Suicide in first episode psychosis: a nationwide cohort study. Schizophr Res. 2014;157(1–3):1–7. Epub 2014/06/05. 10.1016/j.schres.2014.05.010 . [DOI] [PubMed] [Google Scholar]
- 37.Limosin F, Loze JY, Philippe A, Casadebaig F, Rouillon F. Ten-year prospective follow-up study of the mortality by suicide in schizophrenic patients. Schizophr Res. 2007;94(1–3):23–8. Epub 2007/06/19. 10.1016/j.schres.2007.04.031 . [DOI] [PubMed] [Google Scholar]
- 38.Kilbourne AM, Morden NE, Austin K, Ilgen M, McCarthy JF, Dalack G, et al. Excess heart-disease-related mortality in a national study of patients with mental disorders: identifying modifiable risk factors. General hospital psychiatry. 2009;31(6):555–63. Epub 2009/11/07. 10.1016/j.genhosppsych.2009.07.008 ; PubMed Central PMCID: PMCPmc4033835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mattisson C, Bogren M, Öjehagen A, Nordström G, Horstmann V. Mortality in alcohol use disorder in the Lundby Community Cohort—a 50 year follow-up. Drug and alcohol dependence. 2011;118(2–3):141–7. Epub 2011/04/09. 10.1016/j.drugalcdep.2011.03.008 . [DOI] [PubMed] [Google Scholar]
- 40.Steingrímsson S, Sigurdsson MI, Aspelund T, Sigfússon S, Magnusson A. Total population-based study of the impact of substance use disorders on the overall survival of psychiatric inpatients. Nord J Psychiatry. 2016;70(3):161–6. Epub 2015/09/01. 10.3109/08039488.2015.1062143 . [DOI] [PubMed] [Google Scholar]
- 41.Sørensen HJ, Jepsen PW, Haastrup S, Juel K. Drug-use pattern, comorbid psychosis and mortality in people with a history of opioid addiction. Acta Psychiatr Scand. 2005;111(3):244–9. Epub 2005/02/11. 10.1111/j.1600-0447.2004.00445.x . [DOI] [PubMed] [Google Scholar]
- 42.Nyhlén A, Fridell M, Hesse M, Krantz P. Causes of premature mortality in Swedish drug abusers: a prospective longitudinal study 1970–2006. Journal of forensic and legal medicine. 2011;18(2):66–72. Epub 2011/02/15. 10.1016/j.jflm.2011.01.003 . [DOI] [PubMed] [Google Scholar]
- 43.Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Andreasson S, Allebeck P. Cannabis, schizophrenia and other non-affective psychoses: 35 years of follow-up of a population-based cohort. Psychol Med. 2012;42(6):1321–8. Epub 2011/10/18. 10.1017/S0033291711002078 . [DOI] [PubMed] [Google Scholar]
- 44.Nyhlén A, Fridell M, Bäckström M, Hesse M, Krantz P. Substance abuse and psychiatric co-morbidity as predictors of premature mortality in Swedish drug abusers: a prospective longitudinal study 1970–2006. BMC Psychiatry. 2011;11:122 Epub 2011/08/02. 10.1186/1471-244X-11-122 ; PubMed Central PMCID: PMCPmc3163521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Helsedirektoratet [The Norwegian Directorate of Health]. Aktivitetsdata for somatisk spesialisthelsetjeneste 2009 [Data on activities in specialized somatic health services 2009] Oslo2010. Available from: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/525/Aktivitetsdata-for-somatisk-spesialisthelsetjeneste-2009-IS-1800.pdf.
- 46.Helsedirektoratet [The Norwegian Directorate of Health]. Aktivitetsdata for psykisk helsevern for voksne og tverrfaglig spesialisert behandling av rusmiddelmisbruk 2010 [Activity data for mental health care for adults and children interdisciplinary specialized drug abuse treatment 2010] Oslo2011. Available from: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/518/Aktivitetsdata-for-psykisk-helsevern-for-voksne-og-tverrfaglig-spesialisert-behandling-av-rusmiddelmisbruk-2010-IS-1911.pdf.
- 47.Helsedirektoratet [The Norwegian Directorate of Health]. Aktivitetsdata for avtalespesialister 2009 [Data on activities by specialists in private practice 2009] Oslo2010. Available from: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/504/Aktivitetsdata-for-avtalespesialister-2009-IS-1818.pdf.
- 48.Helsedirektoratet [The Norwegian Directorate of Health]. Aktivitetsdata for avtalespesialister 2015 [Data on activities by specialists in private practice 2015] Oslo2016. Available from: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/1180/Aktivitetsdata%20for%20avtalespesialister%202015.pdf.
- 49.World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision: World Health Organization; 2004.
- 50.Pedersen AG, Ellingsen CL. Data quality in the Causes of Death Registry. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2015;135(8):768–70. Epub 2015/05/08. 10.4045/tidsskr.14.1065 . [DOI] [PubMed] [Google Scholar]
- 51.Norwegian Institute of Public Health. Dødsfall etter kjønn, alder og detaljert dødsårsak [Deaths by sex, age and cause of death] 2015 [December 1, 2015]. Available from: http://statistikkbank.fhi.no/webview/.
- 52.Statistics Norway. Folkemengde og befolkningsendringar [Population and population changes] 2016 [November 21, 2016]. Available from: http://statistikkbank.fhi.no/.
- 53.Carstensen B, Dickman P. SAS-macro for splitting of follow-up data [Web page]. 2007 [updated December 200723rd November 2016]. Available from: http://bendixcarstensen.com/Lexis/Lexis.sas.
- 54.Jones ME, Swerdlow AJ. Bias in the standardized mortality ratio when using general population rates to estimate expected number of deaths. American journal of epidemiology. 1998;148(10):1012–7. Epub 1998/11/26. . [DOI] [PubMed] [Google Scholar]
- 55.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41. Epub 2015/02/12. 10.1001/jamapsychiatry.2014.2502 ; PubMed Central PMCID: PMCPmc4461039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Laursen TM, Wahlbeck K, Hällgren J, Westman J, Ösby U, Alinaghizadeh H, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS One. 2013;8(6):e67133 Epub 2013/07/05. 10.1371/journal.pone.0067133 ; PubMed Central PMCID: PMCPmc3691116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Høye A, Jacobsen BK, Hansen V. Increasing mortality in schizophrenia: are women at particular risk? A follow-up of 1111 patients admitted during 1980–2006 in Northern Norway. Schizophr Res. 2011;132(2–3):228–32. Epub 2011/08/27. 10.1016/j.schres.2011.07.021 . [DOI] [PubMed] [Google Scholar]
- 58.Nielsen RE, Uggerby AS, Jensen SO, McGrath JJ. Increasing mortality gap for patients diagnosed with schizophrenia over the last three decades—a Danish nationwide study from 1980 to 2010. Schizophr Res. 2013;146(1–3):22–7. Epub 2013/03/26. 10.1016/j.schres.2013.02.025 . [DOI] [PubMed] [Google Scholar]
- 59.Laursen TM, Nordentoft M. Heart disease treatment and mortality in schizophrenia and bipolar disorder—changes in the Danish population between 1994 and 2006. J Psychiatr Res. 2011;45(1):29–35. Epub 2010/06/16. 10.1016/j.jpsychires.2010.04.027 . [DOI] [PubMed] [Google Scholar]
- 60.Ösby U, Westman J, Hällgren J, Gissler M. Mortality trends in cardiovascular causes in schizophrenia, bipolar and unipolar mood disorder in Sweden 1987–2010. European journal of public health. 2016;26(5):867–71. Epub 2016/01/10. 10.1093/eurpub/ckv245 ; PubMed Central PMCID: PMCPmc5054269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Onyeka IN, Beynon CM, Hannila ML, Tiihonen J, Föhr J, Tuomola P, et al. Patterns and 14-year trends in mortality among illicit drug users in Finland: the HUUTI study. The International journal on drug policy. 2014;25(6):1047–53. Epub 2014/08/26. 10.1016/j.drugpo.2014.07.008 . [DOI] [PubMed] [Google Scholar]
- 62.Bretteville-Jensen AL, Lillehagen M, Gjersing L, Andreas JB. Illicit use of opioid substitution drugs: prevalence, user characteristics, and the association with non-fatal overdoses. Drug and alcohol dependence. 2015;147:89–96. Epub 2014/12/30. 10.1016/j.drugalcdep.2014.12.002 . [DOI] [PubMed] [Google Scholar]
- 63.Kiviniemi M, Suvisaari J, Pirkola S, Häkkinen U, Isohanni M, Hakko H. Regional differences in five-year mortality after a first episode of schizophrenia in Finland. Psychiatric services (Washington, DC). 2010;61(3):272–9. Epub 2010/03/03. 10.1176/appi.ps.61.3.272 . [DOI] [PubMed] [Google Scholar]
- 64.Chang CK, Hayes RD, Broadbent M, Fernandes AC, Lee W, Hotopf M, et al. All-cause mortality among people with serious mental illness (SMI), substance use disorders, and depressive disorders in southeast London: a cohort study. BMC Psychiatry. 2010;10:77 Epub 2010/10/06. 10.1186/1471-244X-10-77 ; PubMed Central PMCID: PMCPmc2958993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Walter F, Carr MJ, Mok PLH, Astrup A, Antonsen S, Pedersen CB, et al. Premature Mortality Among Patients Recently Discharged From Their First Inpatient Psychiatric Treatment. JAMA Psychiatry. 2017;74(5):485–92. Epub 2017/03/16. 10.1001/jamapsychiatry.2017.0071 ; PubMed Central PMCID: PMCPmc5417353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sørensen HJ, Larsen JT, Mors O, Nordentoft M, Mortensen PB, Petersen L. Analysis of risk factors for schizophrenia with two different case definitions: a nationwide register-based external validation study. Schizophr Res. 2015;162(1–3):74–8. Epub 2015/01/27. 10.1016/j.schres.2015.01.018 . [DOI] [PubMed] [Google Scholar]
- 67.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug and alcohol dependence. 2004;76 Suppl:S11–9. Epub 2004/11/24. 10.1016/j.drugalcdep.2004.08.003 . [DOI] [PubMed] [Google Scholar]
- 68.Lawrence D, Mitrou F, Zubrick SR. Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health. 2009;9:285 Epub 2009/08/12. 10.1186/1471-2458-9-285 ; PubMed Central PMCID: PMCPmc2734850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu NH, Daumit GL, Dua T, Aquila R, Charlson F, Cuijpers P, et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. 2017;16(1):30–40. Epub 2017/01/28. 10.1002/wps.20384 ; PubMed Central PMCID: PMCPmc5269481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Beary M, Hodgson R, Wildgust HJ. A critical review of major mortality risk factors for all-cause mortality in first-episode schizophrenia: clinical and research implications. Journal of psychopharmacology (Oxford, England). 2012;26(5 Suppl):52–61. Epub 2012/04/03. 10.1177/0269881112440512 . [DOI] [PubMed] [Google Scholar]
- 71.Gale CR, Batty GD, Osborn DP, Tynelius P, Whitley E, Rasmussen F. Association of mental disorders in early adulthood and later psychiatric hospital admissions and mortality in a cohort study of more than 1 million men. Arch Gen Psychiatry. 2012;69(8):823–31. Epub 2012/08/08. 10.1001/archgenpsychiatry.2011.2000 ; PubMed Central PMCID: PMCPmc4170756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mitchell AJ, Lord O. Do deficits in cardiac care influence high mortality rates in schizophrenia? A systematic review and pooled analysis. Journal of psychopharmacology (Oxford, England). 2010;24(4 Suppl):69–80. Epub 2010/10/15. 10.1177/1359786810382056 ; PubMed Central PMCID: PMCPmc2951596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Correll CU, Detraux J, De Lepeleire J, De Hert M. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. 2015;14(2):119–36. Epub 2015/06/05. 10.1002/wps.20204 ; PubMed Central PMCID: PMCPmc4471960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hunt GE, Siegfried N, Morley K, Sitharthan T, Cleary M. Psychosocial interventions for people with both severe mental illness and substance misuse. The Cochrane database of systematic reviews. 2013;(10):Cd001088 Epub 2013/10/05. 10.1002/14651858.CD001088.pub3 . [DOI] [PubMed] [Google Scholar]
- 75.Murthy P, Chand P. Treatment of dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):194–200. Epub 2012/03/08. 10.1097/YCO.0b013e328351a3e0 . [DOI] [PubMed] [Google Scholar]
- 76.Speyer H, Christian Brix Norgaard H, Birk M, Karlsen M, Storch Jakobsen A, Pedersen K, et al. The CHANGE trial: no superiority of lifestyle coaching plus care coordination plus treatment as usual compared to treatment as usual alone in reducing risk of cardiovascular disease in adults with schizophrenia spectrum disorders and abdominal obesity. World Psychiatry. 2016;15(2):155–65. Epub 2016/06/07. 10.1002/wps.20318 ; PubMed Central PMCID: PMCPmc4911772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30(3):427–32; discussion 33–4. Epub 2001/06/21. . [DOI] [PubMed] [Google Scholar]
- 78.Phillips DE, Lozano R, Naghavi M, Atkinson C, Gonzalez-Medina D, Mikkelsen L, et al. A composite metric for assessing data on mortality and causes of death: the vital statistics performance index. Population health metrics. 2014;12:14 Epub 2014/07/02. 10.1186/1478-7954-12-14 ; PubMed Central PMCID: PMCPmc4060759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Øiesvold T, Nivison M, Hansen V, Skre I, Østensen L, Sørgaard KW. Diagnosing comorbidity in psychiatric hospital: challenging the validity of administrative registers. BMC Psychiatry. 2013;13:13 Epub 2013/01/10. 10.1186/1471-244X-13-13 ; PubMed Central PMCID: PMCPmc3544620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nesvåg R, Jönsson EG, Bakken IJ, Knudsen GP, Bjella TD, Reichborn-Kjennerud T, et al. The quality of severe mental disorder diagnoses in a national health registry as compared to research diagnoses based on structured interview. BMC Psychiatry. 2017;17(1):93 Epub 2017/03/16. 10.1186/s12888-017-1256-8 ; PubMed Central PMCID: PMCPmc5351165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom's General Practice Research Database. Arch Gen Psychiatry. 2007;64(2):242–9. Epub 2007/02/07. 10.1001/archpsyc.64.2.242 . [DOI] [PubMed] [Google Scholar]
- 82.Hansen SS, Munk-Jørgensen P, Guldbæk B, Solgård T, Lauszus KS, Albrechtsen N, et al. Psychoactive substance use diagnoses among psychiatric in-patients. Acta Psychiatr Scand. 2000;102(6):432–8. Epub 2001/01/06. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
Confidentiality requirements according to Norwegian law prevents sharing of individual patient level data in public repositories. Application of legal basis and exemption from professional secrecy requirements for the use of personal health data in research may be sent to a regional committee for medical and health research ethics (https://helseforskning.etikkom.no/), and requests for the data to The Norwegian Patient Registry (https://helsedirektoratet.no/English) and the Cause of Death Registry (https://www.fhi.no/en/). Information on annual number of deaths by sex, age and cause of death are freely available at http://statistikkbank.fhi.no/webview, and annual population numbers freely available at http://statistikkbank.fhi.no.