Abstract
Background
Data was limited on prevalence of overweight and obesity among primary school-aged children in Jiangsu Province. We aimed to present the current situation of obesity in Jiangsu Province and explore the relationship between obesity and other common diseases in children.
Methods
Physical examination among children aged 7 to 14 years in Jiangsu Province was conducted since 2014, and more than one third primary schools were covered annually. The physical measurements included body height, weight, blood pressure, vision, sex, age, and so on.
Results
The prevalence of overweight and obesity among primary school children was 15.2% (18.7% for male students and 11.0% for female students), and 11.7% (14.5% for male students and 8.2% for female students) respectively. Obesity/overweight prevalence varied by regions. Among them the lowest prevalence was found in the southern region of Jiangsu Province, where residents had the highest average income level. Obesity group had elevated blood pressure comparing with the normal group, and obesity group especially in the male children aged 7 to 12 years had a higher prevalence of uncorrected visual acuity (UCVA) than that of normal group.
Conclusion
This study found that obesity/overweight prevalence differed by sex, age, and regions in Jiangsu Province. In addition, obese children were closely associated with other common disease. Further studies are needed to explore the basis of biological and statistical theories.
Introduction
The prevalence of obesity among children and adolescents has increased dramatically during the past decades all over the world[1, 2]. Meanwhile, childhood obesity is a multisystem disease with potentially devastating results. It can develop serious medical and psychosocial complications and greatly increase the risk of morbidity and mortality in adults[3].
It has been reported that about 30% to 50% of childhood obesity will continue to become obese adults[4], and obesity may vary by regions, population, climate factors, economic levels, and so on[5, 6]. Marie Ng et found that the prevalence of obesity has increased substantially in children in both developed and developing countries[1]. In China, the prevalence of childhood obesity has gradually increased to the point where it is now similar to developed countries[7, 8]. Several studies were also conducted in China. Ji CY collected data from National Surveys on Chinese Students’ Constitution and Health which were carried in 1985, 1991, 1995 and 2000 suggesting that the prevalence of both obesity and overweight remained relatively low[8]. In adults, however, prevalence of obesity increased by 97.2% from 1992 to 2002[9]. Xi B et also reported that prevalence of obesity increased 1.68 times from 1993 to 2009 in Chinese adults[10].
In addition, childhood obesity significantly contributes to related adverse health problems, such as dyslipidemia, hypertension, cardiovascular disease, insulin resistance or diabetes, asthma, fatty liver disease, and psychosocial complications[11–13].
Located in the eastern China, Jiangsu Province is one of the developed regions in China. We conducted a successive surveillance among primary school children here since 2014, More than 100,000 students were included in the study annually which covers over 40% area of the province. The purpose of this study was to estimate the prevalence of childhood overweight and obesity among primary school children in Jiangsu Province, and observe the trend of body mass index (BMI) from 2014–2015 to 2016–2017 academic season. We also explored relationships between obesity and other common diseases in student to further understand the harmful effects that obesity may bring about.
Materials and methods
Study sites
This study was conducted in Jiangsu Province, which divided into 13 cities consisting of 97 districts or counties. We selected 40districts or counties which were taken up 41.2% regions of this province since 2014, and fifty-three primary schools were chosen into our study with average108, 331 students annually included. (S1 Fig)
Data collection
Students in all schools were included in cluster sampling and received physical examination from 2014 to 2017. Weight and height were measured after students had removed shoes and clothes. Height (measured to nearest 0.1 cm) and weight (measured to the nearest 0.1 kg) were measured using standardized equipment and procedures according to Health check list for primary and junior school students (GB 16134–2011). BMI was calculated as weight in kilograms divided by height in meters squared. Blood pressure and defects of vision were also measured in this study. Uncorrected visual acuity (UCVA) was measured for the right eye, followed by the left eye, with an E Standard Logarithm Vision Acuity Chart (GB11533-2011) in 5-grade notation, with illumination of the chart around 500 lx. The 5-grade notation was obtained using the formula: L = 5-LogMAR. The children were asked to indicate the direction of the E optotype within 5 seconds. They were asked to start with the fourth line, if optotypes of the line were correctly described, otherwise the previous line was continued. When the children falsely described at least 1 character in the 5.1–5.3 line, or at least 2 characters in the 4.6–5.0 line, or at least 3 characters in the 4.0–4.5line, visual acuity was recorded as the value of the previous line. Visual acuity less than 5.0 in 5 graded is defined as UCVA[14]. All students also filled in a simple questionnaire to provide basic demographic information such as name, sex, age and so on.
Definition for overweight and obesity
Obesity is defined by BMI in this study, and We used unified classification criteria for overweight, obesity and BMI screening among children and adolescents by Working Group on Obesity in China (WGOC)[15] (S1 Table).
Statistical analysis
Descriptive statistics were used to summarize variables concerning characteristics of primary school students, and the prevalence of overweight and obesity were presented as the prevalence and 95% confidence interval(CI) of the prevalence. Continuous variables like blood pressure were presented as the mean with standard deviation(SD) of the mean. Student t tests were used for comparisons of 2-group with continuous variables, and Chi-square tests were performed for comparing two proportions of UCVA. Poisson regression analysis was performed and adjusted risk ratio values were computed to assess the relationship between obesity and other common childhood disease[16–18]. Data was analyzed by SPSS 20.0 and SAS9.2 software, and figures were drawn by ArcGis10.0 and office software.
Ethics statement
The study protocol was approved by the Institutional Review Board of Ethics committee of Jiangsu Province. Ministry of education published an Official Notice of Implementation Plan of National Student Physical Health Monitoring Network Work since 2002, which was belonging as part of nine years of compulsory education welfare(Specific content could be acquired by landing on the URL: http://www.moe.gov.cn/jyb_xxgk/gk_gbgg/moe_0/moe_8/moe_25/tnull_285.html). According to this Official Notice, Education Department of Jiangsu Province conducted physical examination for students every year since 2005. During the period of student’s physical examination, the Centers for Disease Control and prevention would be invited to provide technical guidance. Therefore, acquisition of informed consent is mainly organized by the Education Department and the Health Department will require school to keep a written consent in the name of school as an indicator of annual performance check.
Detailed implementation process can be described as follows: At the beginning of each semester schools will hold parent-teacher conference, and every student’s guardian would be consulted by teachers. If parents do not intend to attend the examination, they will tell the teacher verbally, and the other students will be regarded as oral informed consent. Certainly, if it involves extraction of biological materials such as blood, pleural effusion, CSF sampling, there will be a written consent.
Results
In our study 108,331 observations were enrolled annually and a total of 324,993 observations were included since 2014, which were consisting of 177,103 male children and 147,980 female children and the male to female ratio was 1.2. Children aged 7 to 12 years accounted for 95% in primary school and more than half were from south of Jiangsu Province. (Table 1)
Table 1. Characteristics of primary school students in Jiangsu Province, 2014–2017.
| Characteristic | No. | Percentage (%) | |
|---|---|---|---|
| Sex | Male | 177,103 | 54.5 |
| Female | 147,980 | 45.5 | |
| Age | 7- | 57,631 | 17.7 |
| 8- | 55,800 | 17.2 | |
| 9- | 55,486 | 17.1 | |
| 10- | 55,527 | 17.1 | |
| 11- | 51,126 | 15.7 | |
| 12- | 33,170 | 10.2 | |
| 13- | 10,031 | 3.1 | |
| 14- | 6,222 | 1.9 | |
| Area | South | 171,327 | 52.7 |
| Middle | 67,700 | 20.8 | |
| North | 85,966 | 26.5 | |
| Year | 2014–2015 | 107,677 | 33.2 |
| 2015–2016 | 108,316 | 33.3 | |
| 2016–2017 | 109,000 | 33.5 | |
| Total | 324,993 | 100.0 | |
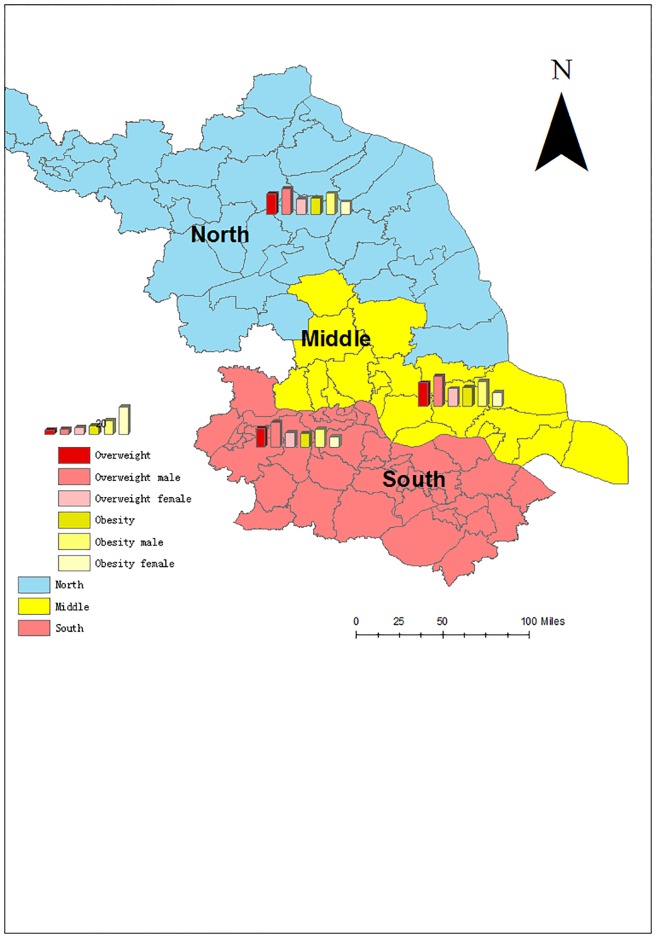
The prevalence of overweight and obesity in the middle of Jiangsu Province ranked at the first place:17.5% for overweight and 14.1% for obesity, and the northern region was at the second place: 15.0% for overweight and 12.3% for obesity. The southern region remained lowest the prevalence of overweight and obesity: 14.2% for overweight and 10.2% for obesity. However, the prevalence of overweight and obesity for male children were always higher than those of female children in the three regions. (P <0.01) (Fig 1).
Fig 1. Prevalence of overweight and obesity for students from different regions in Jiangsu Province 2014–2017.
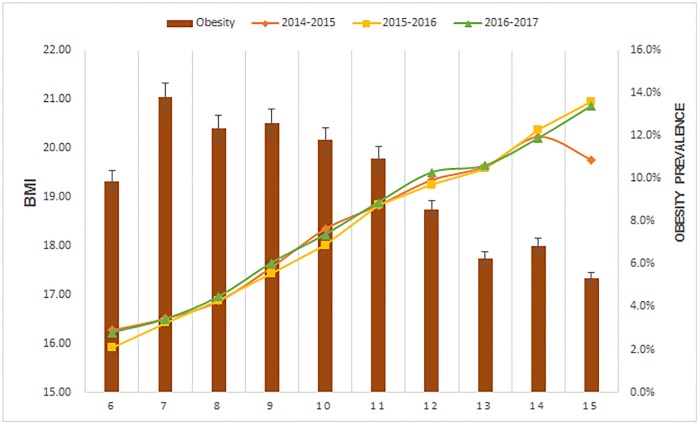
From 2014–2015 to 2016–2017 academic year the average value of BMI maintained stable ranging from 16.5 to 21.0, and the value of BMI increased by age. However, the prevalence of obesity decreased by age ranging from 13.8% to 6.3%. (Fig 2)
Fig 2. Trend for BMI changes for primary students in Jiangsu Province 2014–2017.
The prevalence of combined obesity and overweight among children in primary schools was 26.8%, 95%CI:26.7%-27.0%, which for male students was 33.2%, 95%CI: 33.0%-33.4% and for female students was 19.2%,95%CI:19.0%-19.2%. The prevalence of obesity was 11.7%, 95%CI:11.5%-11.8%, which for male students was 14.5%,95%CI:14.3%-14.7% and for female students was 8.2%, 95%CI:8.1%-8.4%. For children aged 7 years the prevalence of combined overweight and obesity was the highest and for children aged 13 years the prevalence was the lowest. (Table 2)
Table 2. Age-specific prevalence for children and adolescents with overweight and obesity for them in Jiangsu Province 2014–2017.
| Age | Combined obesity and overweight(95%CI) | Obesity(95%CI) | Overweight (95CI%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (%) | Male (%) | Female (%) | Total (%) | Male (%) | Female (%) | Total (%) | Male (%) | Female (%) | |
| 7- | 28.3(27.9–28.6) | 31.8(31.2–32.3) | 24.1(23.6–24.6) | 13.8(13.5–14.1) | 16.2(15.8–16.6) | 11.0(10.6–11.3) | 14.5(14.2–14.8) | 15.6(15.2–16.0) | 13.2(12.7–13.6) |
| 8- | 26.1(25.8–26.5) | 30.6(30.1–31.1) | 20.8(20.3–21.3) | 12.3(12.1–12.6) | 14.8(14.4–15.2) | 9.5(9.1–9.8) | 13.8(13.5–14.1) | 15.9(15.5–16.3) | 11.3(10.9–11.7) |
| 9- | 27.0(26.7–27.4) | 33.6(33.1–34.2) | 19.1(18.6–19.6) | 12.6(12.3–12.9) | 16.0(15.5–16.4) | 8.6(8.3–8.9) | 14.4(14.1–14.7) | 17.7(17.2–18.1) | 10.5(10.1–10.9) |
| 10- | 27.8(27.4–28.2) | 35.7(35.1–36.2) | 18.4(17.9–18.9) | 11.8(11.5–12.1) | 15.1(14.7–15.5) | 7.9(7.6–8.2) | 16.0(15.7–16.3) | 20.6(20.1–21.1) | 10.5(10.1–10.9) |
| 11- | 27.3(27.0–27.7) | 36.6(36.0–37.2) | 16.3(15.8–16.7) | 10.9(10.7–11.2) | 14.4(14.0–14.8) | 6.8(6.5–7.1) | 16.4(16.1–16.7) | 22.2(21.7–22.7) | 9.5(9.1–9.8) |
| 12- | 25.6(25.1–26.1) | 33.9(33.2–34.5) | 15.5(15.0–16.1) | 8.6(8.3–8.9) | 11.2(10.7–11.6) | 5.4(5.0–5.7) | 17.1(16.7–17.5) | 22.7(22.1–23.3) | 10.2(9.7–10.7) |
| 13- | 20.9(20.1–21.7) | 25.1(24.0–26.3) | 15.9(14.8–16.9) | 6.3(5.8–6.7) | 7.7(7.0–8.4) | 4.6(4.0–5.2) | 14.6(13.9–15.3) | 17.4(16.4–18.4) | 11.3(10.8–13.1) |
| 14- | 21.2(20.2–22.3) | 25.1(23.6–26.6) | 16.8(15.4–18.2) | 6.8(6.2–7.5) | 8.6(7.6–9.5) | 4.9(4.1–5.6) | 14.4(13.5–15.3) | 16.5(15.3–17.8) | 12.0(10.8–13.1) |
| Total | 26.8(26.7–27.0) | 33.2(33.0–33.4) | 19.2(19.0–19.2) | 11.7(11.5–11.8) | 14.5(14.3–14.7) | 8.2(8.1–8.4) | 15.2(15.1–15.3) | 18.7(18.5–18.9) | 11.0(10.8–11.1) |
Obesity-related blood pressure including diastolic pressure and systolic pressure in the obesity group were higher than children without obesity, while the blood pressure of both groups was all within reference range. (Table 3) Poisson regression analysis showed that male children and female children aged 10 to 12 years had the same phenomenon. (Table 4)
Table 3. Obesity related blood pressure among children and adolescents in Jiangsu Province 2014–2017.
| Sex | Age | Obesity | Normal | Obesity VS Normal (P value) | |||
|---|---|---|---|---|---|---|---|
| Diastolic pressure | Systolic pressure | Diastolic pressure | Systolic pressure | Diastolic pressure | Systolic pressure | ||
| Male | 7 | 103.7±12.4 | 66.7±9.4 | 101.0±12.6 | 65.2±9.7 | 0.000 | 0.000 |
| 8 | 106.0±11.8 | 67.6±8.8 | 102.5±12.1 | 66.0±9.5 | 0.000 | 0.000 | |
| 9 | 108.6±11.7 | 68.7±8.7 | 103.7±11.6 | 66.1±9.0 | 0.000 | 0.000 | |
| 10 | 110.7±11.7 | 69.9±8.7 | 105.5±11.6 | 67.1±9.1 | 0.000 | 0.000 | |
| 11 | 113.5±11.5 | 71.1±8.5 | 107.6±11.4 | 68.0±8.8 | 0.000 | 0.000 | |
| 12 | 116.3±11.8 | 71.7±8.5 | 110.2±11.5 | 68.7±8.8 | 0.000 | 0.000 | |
| 13 | 121.9±11.4 | 72.7±8.8 | 115.0±11.9 | 69.9±8.9 | 0.000 | 0.000 | |
| 14 | 122.3±11.6 | 73.7±7.9 | 118.4±11.5 | 71.5±8.8 | 0.000 | 0.000 | |
| Total | 109.4±12.6 | 69.1±9.0 | 105.4±12.4 | 67.0±9.3 | 0.000 | 0.000 | |
| Female | 7 | 102.1±12.6 | 66.2±9.3 | 99.8±12.7 | 64.8±9.6 | 0.000 | 0.000 |
| 8 | 105.1±12.0 | 67.4±8.5 | 101.1±12.0 | 65.5±9.2 | 0.000 | 0.000 | |
| 9 | 107.0±12.0 | 68.8±8.6 | 102.0±11.6 | 65.6±8.8 | 0.000 | 0.000 | |
| 10 | 110.0±12.1 | 69.8±9.2 | 104.4±11.7 | 66.7±8.8 | 0.000 | 0.000 | |
| 11 | 113.9±11.9 | 71.0±8.4 | 106.8±11.4 | 67.7±8.5 | 0.000 | 0.000 | |
| 12 | 116.1±11.2 | 72.1±8.5 | 109.0±11.2 | 68.9±8.7 | 0.000 | 0.000 | |
| 13 | 119.2±11.6 | 74.3±8.5 | 112.6±11.2 | 70.4±8.7 | 0.000 | 0.000 | |
| 14 | 120.0±11.1 | 76.1±8.3 | 113.3±10.8 | 71.1±8.5 | 0.000 | 0.000 | |
| Total | 107.8±13.0 | 68.8±9.1 | 104.0±12.3 | 66.6±9.1 | 0.000 | 0.000 | |
Table 4. Poisson regression analysis of relationship between other children common disease and obesity.
| Variable in All subjects | β | SE | P | RR (95%CI) |
|---|---|---|---|---|
| Age group one 7–9 | ||||
| Diastolic BP Male | 0.003 | 0.000 | 0.001 | 1.003(1.002–1.003) |
| Systolic BP Male | 0.001 | 0.000 | 0.000 | 1.001(1.000–1.002) |
| Diastolic BPFemale | 0.003 | 0.000 | 0.197 | 1.000(0.999–1.000) |
| Systolic BP Female | 0.000 | 0.000 | 0.000 | 1.003(1.002–1.003) |
| UCVA Male | 0.237 | 0.017 | 0.000 | 1.267(1.225–1.311) |
| UCVA Female | 0.199 | 0.024 | 0.000 | 1.221(1.166–1.279) |
| Age group two 10–12 | ||||
| Diastolic BP Male | 0.003 | 0.000 | 0.000 | 1.003(1.002–1.003) |
| Systolic BP Male | 0.002 | 0.000 | 0.000 | 1.002(1.001–1.003) |
| Diastolic BPFemale | 0.002 | 0.000 | 0.000 | 1.002(1.000–1.003) |
| Systolic BP Female | 0.003 | 0.000 | 0.000 | 1.003(1.003–1.004) |
| UCVA Male | 0.118 | 0.020 | 0.000 | 1.125(1.082–1.169) |
| UCVA Female | 0.054 | 0.031 | 0.082 | 1.056(0.993–1.123) |
| Age group three 13–14 | ||||
| Diastolic BP Male | 0.006 | 0.000 | 0.000 | 1.006(1.003–1.008) |
| Systolic BP Male | 0.003 | 0.003 | 0.000 | 1.034(1.002–1.005) |
| Diastolic BPFemale | -0.001 | 0.006 | 0.870 | 0.999(0.988–1.010) |
| Systolic BP Female | 0.004 | 0.004 | 0.309 | 1.004(0.996–1.012) |
| UCVA Male | 0.113 | 0.095 | 0.236 | 1.119(0.929–1.348) |
| UCVA Female | 0.163 | 0.164 | 0.320 | 1.177(0.854–1.621) |
β indicates parameter estimate;
SE, standard error of estimate.
We also found that obesity group especially for male children aged from 7 to 12 years had a higher UCVA prevalence than that of normal group. However, children aged 13 to 14 years had a similar UCVA prevalence for both groups. (Table 5) For children aged 7–9 years, multiple linear regression analysis suggested obesity was associated with UCVA. (Table 4)
Table 5. Relationship between obesity and UCVA among children and adolescents in Jiangsu Province from 2014–2015 to 2016–2017.
| Age | Obesity (95%CI) | Normal(95%) | χ2 | P | ||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||
| 7 | 32.4(31.1–33.7) | 35.3(33.5–37.0) | 26.7(26.2–27.3) | 30.9(30.3–31.5) | χ2male = 68.2 χ2female = 22.6 χ2m VS f = 6.9 |
0.000 0.000 0.009 |
| 8 | 37.9(36.5–39.3) | 41.7(39.7–43.7) | 30.4(29.9–31.0) | 33.8(33.2–34.4) | χ2male = 98.1 χ2female = 60.7 χ2m VS f = 9.5 |
0.000 0.000 0.002 |
| 9 | 46.3(44.9–47.7) | 49.3(47.2–51.4) | 39.7(39.1–40.3) | 43.7(43.1–44.4) | χ2male = 73.7 χ2female = 24.6 χ2m VS f = 5.3 |
0.000 0.000 0.021 |
| 10 | 52.7(51.2–54.1) | 54.8(52.6–57.0) | 48.5(47.9–49.1) | 53.6(53.0–54.2) | χ2male = 26.4 χ2female = 1.0 χ2m VS f = 2.5 |
0.000 0.305 0.114 |
| 11 | 60.5(59.0–62.0) | 66.9(64.5–69.2) | 57.0(56.4–57.6) | 63.6(62.9–64.2) | χ2male = 16.8 χ2female = 7.0 χ2m VS f = 19.7 |
0.000 0.008 0.000 |
| 12 | 67.6(65.5–69.6) | 73.7(70.6–76.7) | 63.5(62.7–64.2) | 71.1(70.3–71.8) | χ2male = 13.0 χ2female = 2.5 χ2m VS f = 10.0 |
0.000 0.114 0.002 |
| 13 | 77.8(73.8–81.8) | 83.6(78.5–88.6) | 73.5(72.2–74.7) | 81.8(80.6–82.9) | χ2male = 3.8 χ2female = 0.4 χ2m VS f = 2.9 |
0.052 0.513 0.091 |
| 14 | 83.6(79.3–87.9) | 93.6(89.5–97.6) | 85.8(84.6–87.0) | 91.1(90.0–92.1) | χ2male = 1.1 χ2female = 1.0 χ2m VS f = 8.2 |
0.304 0.309 0.004 |
| Total | 48.0(47.4–48.7) | 50.3(49.5–51.2) | 44.7(44.4–44.9) | 49.7(49.4–50.0) | χ2male = 100.0 χ2female = 1.8 χ2m VS f = 17.4 |
0.000 0.178 0.000 |
Discussion
This study showed the prevalence of overweight and obesity among children aged 7 to 14 years using aged- and sex-specific cut-off points for BMI recommended by WGOC[15]. Since2014, average 108,331 children were enrolled annually in Jiangsu Province, and the prevalence of combined overweight and obesity was26.8%(33.2% for male and 19.2% for female). The prevalence of both obesity and overweight indicated there were regional and age differences. BMI value maintained stable in our three surveys. The relationship between obesity and blood pressure as well as UCVA were also explored in this study.
The prevalence of overweight and obesity was similar to other studies in China. In 2010, Song et estimated the prevalence of obesity among Chinese children aged 7 to 9 years (15.8% for boys and 8.0% for girls), 10 to 12 years (12.5% for boys and 6.5% for girls)and 13 to 15 years (8.5% for boys and 4.0% for girls), which was similar to our results[19]. Ji et noted that the prevalence of overweight among children aged 7 to 12 years was 36.8% and 24.6% in the major cities of north coast and the upper cities of south coast, respectively[20]. However, these studies were of small sample sizes and didn’t display detailed age-specific information about obesity and overweight.
Income is another factor that plays an important role in obesity[21, 22]. The income level of the residents in Jiangsu Province residents was closely associated with geographical distribution: Southern>Middle>Northern (detailed information can be referred to S2 Table from Jiangsu Statistical Yearbook). In the United states, the prevalence of childhood obesity was low among youths living in households in the highest income families[23]. In our study, the lowest prevalence of overweight and obesity was found in the southern region of Jiangsu Province, where the residents had the highest average income levels. However, this pattern was not seen in all families and may be affected by other factors such as education level [24]. Similar to other studies, males tend to be overweight or obesity, and reason for this phenomenon can be explained by differences in lifestyle, gene and sex behaviors and so on[9, 25–28]. The value of BMI increased by age, but the prevalence of obesity decreased by age among primary school students aged 7 to 14 years.
Childhood obesity is associated with an increased prevalence of pediatric diseases, such as type 2 diabetes, dyslipidaemia, hypertension, asthmaand so on[12, 29]. In our study, we also explored the relationships between obesity and other health issues. In obese children, their blood pressure were higher than children without obesity, while both groups were within the reference range. Several systematic reviews have confirmed that higher BMI in childhood and adolescence increases the risk of cardiovascular disease in adulthood. This finding indicated that BMI levels were positively associated with SBP and DBP levels[30, 31]. In addition, we found that obese children aged 7 to 9 years seemed to have poorer visions comparing with children without obesity, and even variations can last to 12 years of age for boys. Qi et found that the prevalence of myopia was associated with the intake of proteins such as milk, egg, beans and meat[32], which was related to high prevalence of obesity. Lim et carried out an 851-Chinese-school-children experiment in Singapore, and found that the eye axial length, which was associated with refractive error or a diagnosis of myopia, was longest in the highest quartile group of total cholesterol intake compared with the lowest group[33].
This study has several limitations. First, we only enrolled children from 41.2% districts or counties of Jiangsu Province, so the results therefore may not totally represent the prevalence of the whole province. Moreover, the observations in the study, such as the relationship between obesity and other diseases, should need for further exploration.
Conclusion
We found that obesity/overweight prevalence differed by sex, age, and region in Jiangsu Province. In addition, obese children were closely associated with other common disease. Further studies are needed to explore the basis of biological and statistical theories.
Supporting information
(TIF)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by Demonstration project of comprehensive prevention and control of emerging infectious diseases (BE2015714); http://www.jshealth.com/xxgk/sewcjz/xmzl/sbjkt/201708/t20170830_59379.html. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. LANCET 2014;384(9945):766–81. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. LANCET 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. LANCET 2002;360(9331):473 10.1016/S0140-6736(02)09678-2 [DOI] [PubMed] [Google Scholar]
- 4.Rivera JÁ, de Cossío TG, Pedraza LS, Aburto TC, Sánchez TG, Martorell R. Childhood and adolescent overweight and obesity in Latin America: a systematic review. LANCET DIABETES ENDO 2014;2(4):321–32. [DOI] [PubMed] [Google Scholar]
- 5.Wang K, Wang D, Pan L, Yu Y, Dong F, Li L, et al. Prevalence of Obesity and Related Factors among Bouyei and Han Peoples in Guizhou Province, Southwest China. PLOS ONE 2015;10(6):e129230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes MetabSyndrObes 2010;2010(default):285–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ji CY, Chen TJ. Empirical Changes in the Prevalence of Overweight and Obesity among Chinese Students from 1985 to 2010 and Corresponding Preventive Strategies. BIOMED ENVIRON SCI 2013;26(1):1–12. 10.3967/0895-3988.2013.01.001 [DOI] [PubMed] [Google Scholar]
- 8.Ji CY. The prevalence of childhood overweight/obesity and the epidemic changes in 1985–2000 for Chinese school-age children and adolescents. OBES REV 2008;9(1):78–81. [DOI] [PubMed] [Google Scholar]
- 9.Wu YF, Ma GS, Hu YH, Li YP, Li X, Cui ZH, et al. [The current prevalence status of body overweight and obesity in China: data from the China National Nutrition and Health Survey]. Zhonghuayu fang yixue za zhi [Chinese journal of preventive medicine] 2005;39(5):316. [PubMed] [Google Scholar]
- 10.Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obesity Reviews An Official Journal of the International Association for the Study of Obesity 2012;13(3):287–96. 10.1111/j.1467-789X.2011.00944.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniels SR. Complications of obesity in children and adolescents. INT J OBESITY 2009;33 Suppl 1(33 Suppl 1):S60. [DOI] [PubMed] [Google Scholar]
- 12.Barros R, Moreira P, Padrão P, Teixeira VH, Carvalho P, Delgado L, et al. Obesity increases the prevalence and the incidence of asthma and worsens asthma severity. CLIN NUTR 2016. [DOI] [PubMed] [Google Scholar]
- 13.Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. Jama the Journal of the American Medical Association 2003;289(1):76–9. [DOI] [PubMed] [Google Scholar]
- 14.Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmology,15,1(2015-July-09) 2015;15(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chengye JI. Report on Childhood Obesity in China (1) Body Mass Index Reference for Screening Overweight and Obesity in Chinese School-age Children. BIOMED ENVIRON SCI 2005;18(6):390–400. [PubMed] [Google Scholar]
- 16.Petersen MR, Deddens JA. RE: “EASY SAS CALCULATIONS FOR RISK OR PREVALENCE RATIOS AND DIFFERENCES”. AM J EPIDEMIOL 2006;163(12):1159–61. [DOI] [PubMed] [Google Scholar]
- 17.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. AM J EPIDEMIOL 2005;162(3):199–200. 10.1093/aje/kwi188 [DOI] [PubMed] [Google Scholar]
- 18.Mcnutt LA, Wu C, Xue X, Hafner JP. Estimating the Relative Risk in Cohort Studies and Clinical Trials of Common Outcomes. AM J EPIDEMIOL 2003;157(10):940–3. [DOI] [PubMed] [Google Scholar]
- 19.Yi S, Wang HJ, Ma J, Wang Z. Secular Trends of Obesity Prevalence in Urban Chinese Children from 1985 to 2010: Gender Disparity. PLOS ONE 2013;8(1):e53069 10.1371/journal.pone.0053069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ji CY, Cheng TO. Prevalence and geographic distribution of childhood obesity in China in 2005. INT J CARDIOL 2008;131(1):1–8. 10.1016/j.ijcard.2008.05.078 [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. AM J CLIN NUTR 2006;84(4):707–16. 10.1093/ajcn/84.4.707 [DOI] [PubMed] [Google Scholar]
- 22.Ogden CL, Fakhouri TH, Carroll MD, Hales CM, Fryar CD, Li X, et al. Prevalence of Obesity Among Adults, by Household Income and Education—United States, 2011–2014. Mmwr Morbidity & Mortality Weekly Report 2017;66(50):1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. Nchs Data Brief 2010(51):1. [PubMed] [Google Scholar]
- 24.Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, Li X, et al. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household—United States 2011–2014. Morbidity and Mortality Weekly Report 2018 2018-February-16;67(6):186–9. 10.15585/mmwr.mm6706a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu L, Huang X, You C, Li J, Hong K, Li P, et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLOS ONE 2017;12(9):e183934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obesity Reviews An Official Journal of the International Association for the Study of Obesity 2012;13(3):287–96. 10.1111/j.1467-789X.2011.00944.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Z, Zhang L, Chen Z, Wang X, Shao L, Guo M, et al. Survey on prevalence of hypertension in China: background, aim, method and design. INT J CARDIOL 2014;174(3):721–3. 10.1016/j.ijcard.2014.03.117 [DOI] [PubMed] [Google Scholar]
- 28.Li C, Han X, Qi Z, Li Z, Zhang Y, Wang P, et al. Prevalence of Overweight and Obesity and Weight Loss Practice among Beijing Adults, 2011. PLOS ONE 2014;9(9):e98744 10.1371/journal.pone.0098744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. OBES REV 2004;5(s1):4. [DOI] [PubMed] [Google Scholar]
- 30.Freedman DS, Goodman A, Contreras OA, Dasmahapatra P, Srinivasan SR, Berenson GS. Secular trends in BMI and blood pressure among children and adolescents: the Bogalusa Heart Study. PEDIATRICS 2012;130(1):159–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obesity Reviews An Official Journal of the International Association for the Study of Obesity 2012;13(11):985 10.1111/j.1467-789X.2012.01015.x [DOI] [PubMed] [Google Scholar]
- 32.Qi SY, Li JW, Jia LD, Yan XL, Li JL, Xia L, et al. Factors Associated with Myopia in School Children in China: The Beijing Childhood Eye Study. PLOS ONE 2012;7(12):e52668 10.1371/journal.pone.0052668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim LS, Gazzard G, Yenling L, Choo R, Tan DTH, Tong L, et al. Dietary factors, myopia, and axial dimensions in children. OPHTHALMOLOGY 2010;117(5):993 10.1016/j.ophtha.2009.10.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.