Abstract
Objectives
Falls occur frequently in patients with impaired ambulation and may dramatically affect the elderly population. Aim was to document the incidence of falls in knee osteoarthritis (OA) patients undergoing total knee arthroplasty (TKA), and to identify factors and treatments that may influence the risk of falls.
Methods
A systematic literature search was conducted on three medical electronic databases, PubMed, PeDRO, and Cochrane Collaboration. The Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines were used. Risk of bias analysis and best evidence synthesis were performed. The main aspects related to falls were analyzed: prevalence, risk factors, correlation with clinical outcome, effect of treatments.
Results
The systematic review identified 11 papers on 1237 patients. Pre-operative fall prevalence ranged from 23% to 63%, while post-operative values ranged from 12% to 38%. Moderate evidence was found on no influence of clinical scales, no BMI differences between “faller” and “non-faller”, and on influence of limited pre-operative range of motion. Conflicting evidence was found for sex, history of previous falls, age, kyphosis, muscle weakness, fear of falling, depression, balance, gait impairment. No evidence was found for the effectiveness of surgical or rehabilitative strategies on falls reduction.
Conclusions
OA patients undergoing TKA are at high risk of falls, which is reduced but still present after surgery. Although some risk factors were identified, there are no studies demonstrating the possibility of reducing the incidence of this deleterious event, which warrants further research efforts to better manage this fragile population of elderly patients.
1. Introduction
Knee osteoarthritis (OA) is a common and debilitating chronic condition with a rapidly increasing prevalence, due to active lifestyle and the increasing life expectancy.1 Total knee arthroplasty (TKA) is a frequent and effective procedure usually performed in patients with end-stage knee OA.2 Significant advances in the type and quality of current implants allowed many patients to benefit from knee arthroplasty resurfacing, especially the aging population.3 It has been estimated that the demand for TKA will rise by 673%, reaching 3.48 million procedures by 2030 only in the United States. Analogously, revision TKA is estimated to increase by 601%.
Joint replacement generally provides pain relief, improves physical function and quality of life. Conversely, the effect on the risk of falls is not well established, especially in elderly patients with functional gait impairments.4 Falls may dramatically affect elderly patients, with a significant impact on life expectancy.5 TKA affects proprioceptors, neuromuscular control, and joint-related stability, which may influence dynamic stability and risk of falls.
A crucial factor in ambulation is balance, a complex function regulated different integrated systems, such as sensory inputs from somato-sensory (proprioception), visual, and vestibular systems6 as well as by muscles response capacity. Balance deficit has been identified as one of the key elements affecting activities in daily living.7 It has been also found to be responsible for poor mobility and increased risk of falls in knee OA patients, with more than 40% of all patients and 64% of female patients reporting falls within a year.8 In this patients balance is also influenced by knee instability, estimated in 60–80% of these patients.9 Moreover, OA patients undergoing TKA may present further loss of balance control due to surgical tissue replacement but this might be counteracted by an improvement in symptoms and joint function.10 In this light, TKA impact on OA falling patients remains to be determined. Since falls have the potential for serious morbidity and mortality in the elderly population, it is important to determine how TKA influences such deleterious events.11
Aim of this systematic review was to analyze the available literature on the prevalence of falls after prosthetic resurfacing, investigating evidence quality on risk factors and treatments that may influence falls in knee OA patients undergoing TKA.
2. Methods
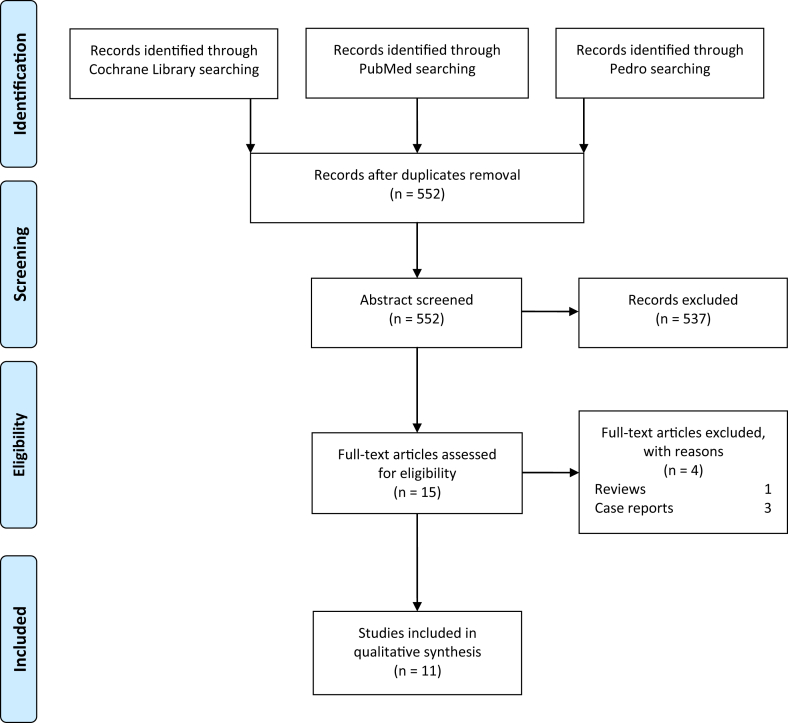
A systematic review of the literature was conducted using the following string on three medical electronic databases, PubMed, PeDRO, and Cochrane Collaboration: ((knee arthroplasty) OR (knee replacement)) AND ((proprioception) OR (sensorimotor) OR (postural control) OR (balance control) OR (falls) OR (risk of falls) OR (giving way)). The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines were used12 (Fig. 1).
Fig. 1.
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines. Flow diagram explaining the process of identification, screening, eligibility and inclusion of the studies.
First, articles were screened by title and abstract. The initial screening was conducted using the following inclusion criteria: clinical reports of any level of evidence, written in English language, with no time limitation, on the occurrence of falls in patients affected by knee OA undergoing TKA. In particular, falls were defined as unintentionally coming to rest on the ground, or at some other lower level, and not the result of a major intrinsic event such as a faint, stroke, or seizure, nor of an overwhelming external hazard such as a hit by a vehicle.13 Exclusion criteria were: reports written in languages other than English, non-clinical studies, reviews, case reports, studies focusing on anesthesiology related falls. In the second step, the full texts of the selected articles were screened to verify further exclusion criteria, according to those previously described. Reference lists from selected papers were also screened. Relevant data (type of study, n° of patients and demographics, pre-post incidence of falls, follow-up, fall influencing factors, correlation with clinical outcome, balance assessment, and influence of pre/post rehabilitation programs) were extracted and collected in a unique database to be analyzed according to the aim of the present study. Two independent authors performed the screening process, study analysis, and data tabulation separately, and a final summary was obtained by consensus, with discrepancies resolved by discussion with a third reviewer (GdLF, DG, AF). The main aspects related to falls in OA patients undergoing TKA were analyzed: prevalence, risk factors, correlation with functional level, and effect of treatments.
2.1. Risk of bias assessment and evidence
Risk of bias was studied according to Cochrane Collaboration's tool [REF] and Eijgenraam et al.14 two reviewers independently scored all the selected articles with a list including two questions concerning selection bias, four questions concerning information bias, and two questions concerning confounding bias; they discussed their findings and, if needed, asked a third reviewer for consensus. A low risk of bias was defined as ‘yes’ to at least six out of eight questions and at least one time ‘yes’ in each risk category (selection, information, and confounding bias). A moderate risk of bias was defined as ‘yes’ to at least five out of eight questions and at least one time ‘yes’ in two of the risk of bias categories. All other cases were considered as high risk of bias.
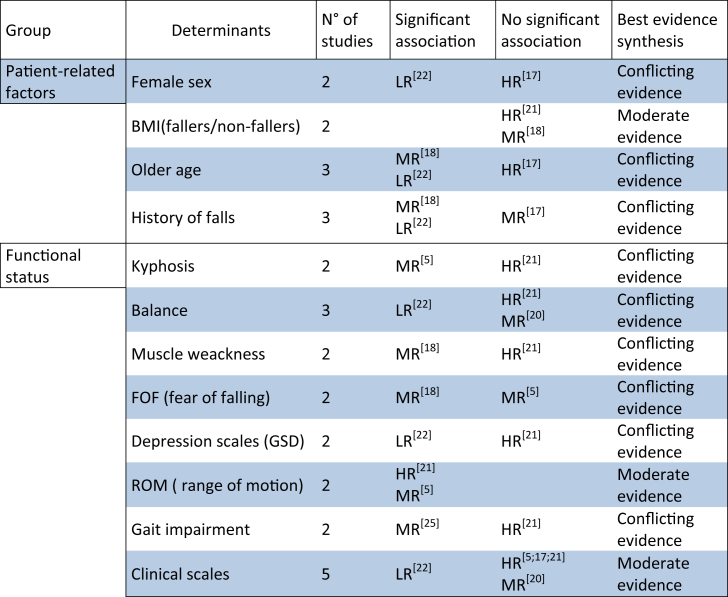
Finally a best evidence synthesis was performed using the algorithm developed by van Tulder et al.15 and Eijgenraam et al.14 in order to provide conclusions based on the best available evidence, since a meta-analysis could not be performed due to a lack of methodological homogeneity. The following ranking of evidence levels was used: strong evidence with two or more studies with low risk of bias and generally consistent findings in all studies (≥75% reporting consistent findings), moderate evidence with one low risk of bias study and two or more moderate/high risk of bias studies or with two or more moderate/high risk of bias and generally consistent findings in all studies (≥75%), limited evidence with one or more moderate/high risk of bias studies or one low risk of bias studies study and generally consistent findings (≥75%), conflicting evidence with conflicting findings (<75% of the studies reporting consistent findings) (Fig. 2).
Fig. 2.
Risk of bias and a best evidence synthesis based on the algorithm developed by van Tulder et al. and Eijgenraam et al.
3. Results
The systematic review of the literature revealed a low number of papers studying the correlation between OA patients undergoing TKA and falls, with a growing interest in the last 5 years, when more than two third of the articles were published.
The databases search identified 552 articles. After screening and selecting abstracts according to inclusion/exclusion criteria, a total of 15 full-text articles were assessed for eligibility: 4 articles did not match the inclusion criteria and were further excluded, resulting in a total of 11 papers used for the analysis. The selected articles analyzed a population of 1237 patients, including 345 females and 716 males (in 2 studies sex was not specified), with age ranging from 43 to 88 years. Study analysis showed heterogeneous evaluation approaches, with patient characteristics assessed with several clinical scales (WOMAC, GDS, MEFS, JKOM, PASE, CES-D, SF-36, HFRM II) and different clinical tests (TUG, ABC, ROM, gait analysis). Details of the included studies are summarized in Table 1, while the main aspects related to falls in OA patients undergoing TKA are reported and summarized in the following paragraphs.
Table 1.
Table summarising structural details of the included studies.
| Article | Type of study | No. pts Sex Age, mean (range) |
Follow-up (months) | Falls prevalence Pre-Post |
Risk factors | Correlation with functional level | |
|---|---|---|---|---|---|---|---|
| Webster K J Aging Phys Act 200623 |
N.S. | 36 20 M, 16 F 72 |
N.S. | 13% | N.S. | N.S. | N.S. |
| Swinkels A AgeAgeing 200922 |
Prospective | 118 46 M, 73 F 73 (69–78) |
12 | 24% | 12% | Gender (F > M) Age History of falls pre-op GDS (higher score) |
ABC (lower score) WOMAC (lower score) |
| Yakhdani HR Clin Biomech 201025 |
N.S. | 16 5 M, 11f 62 |
12 | N.S. | N.S | Gait impairment | N.S. |
| Matsumoto H AOTS 201221 |
Prospective | 74 8 M, 66 F 76 (60–88) |
12 | 33% | N.S. | Eyes problems, diabetes, cardiac disease, ROM deficit (knee and ankle) |
N.S. |
| Swinkels A Physio Theory Pract 201320 |
Observational | 22 6 M, 16 F 75 |
9 | 23% | 17% | N.S. | N.S. |
| Matsumoto H Yonago Acta Med 20145 |
Retrospective | 81 7 M, 74 F 79 |
N.S. | N.S. | 38% | Kiphosys ROM deficit (knee) |
N.S. |
| Smith TO AOTS 201619 | N.S. | 165 69 M, 96 F 68 |
12 | 26% | N.S. | N.S. | N.S. |
| Tsonga T Open Orthop J 201618 |
Prospective | 68 11 M, 57 F 73 |
12 | 63% | 22% | FOF (pre op), Age (>65 years) History of falls pre-op Muscle weakness |
N.S. |
| Tsonga T J Ortho Surg 201624 |
N.S. | 68 11 M, 57 F 73 |
N.S. | 63% | N.S. | N.S. | N.S. |
| Riddle DL Age Ageing 201617 |
Prospective | 413 162 M, 251 F 64 (45–79) |
108 | 32% | N.S. | N.S. | N.S. |
| Levinger P Arch Orth Trauma 201716 |
Prospective | 176 115 M, 128 F 68 |
12 | 34% | N.S. | N.S. | N.S. |
3.1. Falls prevalence in OA patients undergoing TKA
Falls rate was quantified in 10 out of 11 studies5,16, 17, 18, 19, 20, 21, 22, 23, 24; pre-operative prevalence ranged from 23% to 63% while post-operative values ranged from 12% to 38%. Furthermore, 3 out of these 9 studies18,20,22 investigated the effect of TKA on both pre and post-surgery rate of falls; only 1 study found a statistical correlation between surgery and changes in falls rate, with 41% of patients considered “fallers” who stopped falling after TKA. On the other hand, 10% of “non-faller” patients became “frequent-faller” after surgery.22 Falls rate was also evaluated over time post-operatively in 2 studies: the study of Swinkles et al. recorded a higher fall rate in the first quarter of the first year after surgery22; the study Riddle et al. reported a consistent fall rate up to 9 years post-surgery, with a prevalence ranging from 15% to 23% for females and from 8% to 13% for males.17
3.2. Risk factors of falls for TKA patients
Factors influencing patients' falls after TKA were explored in 7 out of 11 studies. These identified a statistical correlation with a higher risk of falls in 6 out of 7 papers.5,18,20,22,25 History of previous falls before surgical intervention and functional impairment were the most frequent elements influencing patients' falls post-surgery. In fact, in 2 studies authors noted a higher rate of falls after TKA significantly correlated to a higher pre-operative rate of falls,18,22 and to a limited pre-operative range of motion in other 2 studies.5,21 Other mentioned risk factors were: demographic characteristics (advanced age), personal factors (the fear of falling), and the presence of comorbidities (diabetes, heart disease, sight impairment, gait impairment and kyphosis).
3.3. Correlation with functional level
Functional assessment was used in 4 articles to identify further risk factors. Among these, only 1 study found a statistical correlation, showing that patients with a lower pre-operative WOMAC score fell more frequently than those with better pre-operative scores. Patient balance was investigated in 3 out of 11 studies with different assessment methods like ABC, TUG, MFES, BBS, and single leg standing test. Among these, only 1 study showed a correlation between lower pre-operative ABC score and a higher rate of falls after surgery.
No articles were found investigating treatments to address the number of falls in knee OA patients undergoing TKA.
3.4. Risk of bias and best evidence assessment
The 7 papers studying falls correlated factors in patients undergoing TKA were also qualitatively evaluated. More in detail, 57% of the studies showed a medium risk of bias related to selection, information and confounding bias, while 29% showed a high risk of bias mostly related to selection and information, and 14% a low risk of bias related to selection bias.
Evident heterogeneity of the studied population and of the outcome measures was not appropriate to conduct a meta-analysis. Thus, qualitative analysis was performed, according to the best evidence synthesis principle. No strong evidence was found. Moderate evidence was found for the influence of limited pre-operative ROM on falls, on no BMI differences between “faller” and “non-faller” patients and for no influence of worse clinical scales on falls. Conflicting evidence was found for sex, history of previous falls, age, kyphosis, muscle weakness, fear of falling, depression, balance and gait impairment. No evidence was found for the effectiveness of surgical or rehabilitative strategies in terms of reduction in the number of falls, with an agreement of 100% between the two reviewers.
4. Discussion
The main finding of this systematic review is that OA patients undergoing TKA are at high risk of falls, which decreases but is still persistent after surgery. Moderate evidence was found on no influence of clinical scales, on no BMI differences between “faller” and “non-faller” patients, and on the influence of limited pre-operative range of motion on falls after TKA. Although some factors influencing the risk of falls were identified, there are no studies demonstrating the possibility to reduce the incidence of this important event after TKA.
TKA is a valid end stage OA treatment aiming at avoiding pain and restoring function. However, while symptoms are improved, little is known about the recovery of proprioception, neuromuscular control, and joint-related stability. Patients frequently present a loss of balance control and proprioceptive ability that can be followed by a lack of confidence after surgical intervention.10 Moreover, asymmetric gait patterns, postural sway, and augmented forward trunk movement can be associated with increased balance difficulties and risk of falls, especially in the early post-operative period.26 During TKA, the replaced knee is deprived of a variety of proprioceptors, which are resected (ligaments, menisci, etc.). Therefore, in the replaced knee postural control regulated by oscillation of the joint cannot be able to reach a threshold detectable by sensory receptors.27 Residual functional deficit has been observed up to 7 years after TKA, with remarkable impairments (i.e. postural stability, walking speed, stair ascent/descent).28 Moreover, decreased muscle strength and compensatory movement strategies after surgery can negatively influence sensory and mechanical function of the joint. These factors contribute to cause a high risk of falls, with a significant impact on society, especially in the ageing population. On the other hand, TKA reduces symptomatology and increases the overall function, which could counteract the increased risk of falls. In this light, balance control and patient stability should be considered as key aspects of OA patients undergoing TKA.
To this regard, this systematic review underlined interesting findings. While the overall failure rate was reported to decrease after surgery, falls remain a frequent and dramatic event. The early recovery of mobility and the compensation of the extra-capsular proprioceptors are inadequate to abolish the risk of falls,29 as shown by the results of this systematic review. Moreover, new falls were observed in people previously considered as non-faller.22 This makes the identification of specific populations and factors, which may expose TKA patients to the risk of falls, of paramount importance.
The analysis of the available literature highlighted different aspects influencing patients' falls. Some of the reasons believed to be responsible were: demographic aspects (i.e. age), clinical impairment (i.e. eyes problem, cardiac disease, or diabetes), and functional impairment (i.e. muscle weakness, reduced ROM, gait impairment, and balance control). On the other hand, the best evidence synthesis analysis could identify mainly conflicting or limited evidence findings and could just preliminary highlight specific populations that may be exposed to a higher risk of falls. Moderate evidence was found on no influence of clinical scales and on the influence of limited pre-operative range of motion, on no BMI differences between “faller” and “non-faller” patients. Despite functional improvement and pain relief provided by TKA, especially in patients with the aforementioned risk factors, falls and the risk of tremendous consequences like periprosthetic fractures and death remain a major problem. To this regard, many aspects remain unsolved and controversial, such as the lack of proper scores or scales with predictive values for identifying subjects at risk of falling.30
Falls are the consequence of many different factors and the proper strategy to avoid them is still missing. Several authors addressed the influence of the surgical technique without focusing directly on the correlation with the number of falls, but rather on proprioception impairment. Some authors stated that reloading of lax collateral tissues at the time of surgery can adequately restore joint alignment and ‘joint space height’, improving the sense of position.31 Moreover, soft tissue balance has been shown to be a crucial factor, in fact, differences in the tension of the medial and lateral collateral structures could be perceived as varus or valgus movement of the leg that could lead to an antagonistic and corrective action from hamstring and quadriceps muscles, hence affecting knee post-operative proprioception.32 Different types of surgical approaches (posterior stabilization versus posterior cruciate ligament retained), nor the addition of a patellar (prosthetic) component showed contradictory findings on their influence on balance, proprioception, and risk of falls.10,33 Other authors have investigated the influence of rehabilitation that could play a key role for lowering the risk of falls by implementing balance control. Training programs usually contemplate both static and dynamic tasks addressed at muscular strengthening, improvement of proprioception and balance34 for the achievement of movement and weight distribution symmetry, also via the use of biofeedback.35 While these elements are common in many rehabilitative treatments, no standard protocol or evidence are currently available on falls prevention exercises after TKA.
Literature presents important limitations that need to be addressed, including the low number of studies, the low quality of their design, and the small number of patients. Moreover, it is not possible to draw a clear conclusion due to the heterogeneity of the methods for patient's evaluation and many different aspects about patients' balance control and risk of falls have yet to be understood. Despite the aforementioned limitations, hampering the feasibility of a meta-analysis, important indications are still offered. By acquiring reliable and comparable results with clearly stated eligibility criteria and by summarising findings in a standardized way, conclusions based on the best available evidence could still be drawn. Different factors have been suggested to affect patients' falls, highlighting that knee OA in patients undergoing TKA has to be considered not merely as a joint related disease but as a whole in its functional and clinical impairment and its interplay with visual and vestibular components. On the other hand, by taking risk of bias into account, a best evidence synthesis underlined mainly conflicting evidence for prognostic factors, showing that different scales are needed, since the existing ones are not specific to predict or prevent falls. Further research is needed to identify specific risk factors and treatments for patients' management before and after surgery in order to minimize the risk of falls and deleterious consequences, in this fragile population of elderly OA patients undergoing TKA.
5. Conclusions
The systematic review of the literature documented that OA patients undergoing TKA are at high risk of falls, which is reduced but still present after surgery. Although some risk factors were identified, taking risk of bias into account a best evidence synthesis underlined mainly conflicting evidence for prognostic factors, and there are no studies demonstrating the possibility of reducing the incidence of this deleterious event. This warrants further research efforts to better manage this fragile population of elderly patients.
References
- 1.Heiden T.L., Lloyd D.G., Ackland T.R. Knee extension and flexion weakness in people with knee osteoarthritis: is antagonist cocontraction a factor? J Orthop Sports Phys Ther. 2009;39(11):807–815. doi: 10.2519/jospt.2009.3079. [DOI] [PubMed] [Google Scholar]
- 2.Losina E. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113–1121. doi: 10.1001/archinternmed.2009.136. discussion 1121-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deirmengian C.A., Lonner J.H. What's new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2013;95(2):184–190. doi: 10.2106/JBJS.L.01050. [DOI] [PubMed] [Google Scholar]
- 4.Bruyere O. Health-related quality of life after total knee or hip replacement for osteoarthritis: a 7-year prospective study. Arch Orthop Trauma Surg. 2012;132(11):1583–1587. doi: 10.1007/s00402-012-1583-7. [DOI] [PubMed] [Google Scholar]
- 5.Matsumoto H. Incidence and risk factors for falling in patients after total knee arthroplasty compared to healthy elderly individuals. Yonago Acta Med. 2014;57(4):137–145. [PMC free article] [PubMed] [Google Scholar]
- 6.Bascuas I. Balance 1 year after TKA: correlation with clinical variables. Orthopedics. 2013;36(1):e6–12. doi: 10.3928/01477447-20121217-11. [DOI] [PubMed] [Google Scholar]
- 7.Williams S.B. Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study. Arch Phys Med Rehabil. 2010;91(1):106–114. doi: 10.1016/j.apmr.2009.08.150. [DOI] [PubMed] [Google Scholar]
- 8.Gillespie L.D. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fitzgerald G.K., Piva S.R., Irrgang J.J. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51(6):941–946. doi: 10.1002/art.20825. [DOI] [PubMed] [Google Scholar]
- 10.Moutzouri M. The effect of total knee arthroplasty on patients' balance and incidence of falls: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3439–3451. doi: 10.1007/s00167-016-4355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliver D. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334(7584):82. doi: 10.1136/bmj.39049.706493.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The prevention of falls in later life. A report of the Kellogg International work group on the prevention of falls by the elderly. Dan Med Bull. 1987;34(Suppl 4):1–24. [PubMed] [Google Scholar]
- 14.Eijgenraam S.M. Can we predict the clinical outcome of arthroscopic partial meniscectomy? A systematic review. Br J Sports Med. 2018 Apr;52(8):514–521. doi: 10.1136/bjsports-2017-097836. Epub 2017 Nov 28. [DOI] [PubMed] [Google Scholar]
- 15.van Tulder M. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003;28(12):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 16.Levinger P. Pre-operative predictors of post-operative falls in people undergoing total hip and knee replacement surgery: a prospective study. Arch Orthop Trauma Surg. 2017;137(8):1025–1033. doi: 10.1007/s00402-017-2727-6. [DOI] [PubMed] [Google Scholar]
- 17.Riddle D.L., Golladay G.J. A longitudinal comparative study of falls in persons with knee arthroplasty and persons with or at high risk for knee osteoarthritis. Age Ageing. 2016;45(6):794–800. doi: 10.1093/ageing/afw126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsonga T. Reduction of falls and factors affecting falls a year after total knee arthroplasty in elderly patients with severe knee osteoarthritis. Open Orthop J. 2016;10:522–531. doi: 10.2174/1874325001610010522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith T.O., Pearson M., Latham S.K. Are people following hip and knee arthroplasty at greater risk of experiencing a fall and fracture? Data from the Osteoarthritis Initiative. Arch Orthop Trauma Surg. 2016;136(6):865–872. doi: 10.1007/s00402-016-2445-5. [DOI] [PubMed] [Google Scholar]
- 20.Swinkels A., Allain T.J. Physical performance tests, self-reported outcomes, and accidental falls before and after total knee arthroplasty: an exploratory study. Physiother Theory Pract. 2013;29(6):432–442. doi: 10.3109/09593985.2012.755590. [DOI] [PubMed] [Google Scholar]
- 21.Matsumoto H. Fall incidence and risk factors in patients after total knee arthroplasty. Arch Orthop Trauma Surg. 2012;132(4):555–563. doi: 10.1007/s00402-011-1418-y. [DOI] [PubMed] [Google Scholar]
- 22.Swinkels A., Newman J.H., Allain T.J. A prospective observational study of falling before and after knee replacement surgery. Age Ageing. 2009;38(2):175–181. doi: 10.1093/ageing/afn229. [DOI] [PubMed] [Google Scholar]
- 23.Webster K.E., Feller J.A., Wittwer J.E. Balance confidence and function after knee-replacement surgery. J Aging Phys Activ. 2006;14(2):181–191. doi: 10.1123/japa.14.2.181. [DOI] [PubMed] [Google Scholar]
- 24.Tsonga T. Risk factors for fear of falling in elderly patients with severe knee osteoarthritis before and one year after total knee arthroplasty. J Orthop Surg. 2016;24(3):302–306. doi: 10.1177/1602400306. [DOI] [PubMed] [Google Scholar]
- 25.Yakhdani H.R. Stability and variability of knee kinematics during gait in knee osteoarthritis before and after replacement surgery. Clin Biomech. 2010;25(3):230–236. doi: 10.1016/j.clinbiomech.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Chang Q.Z. Alternation of trunk movement after arthroplasty in patients with osteoarthritis of the knee. J Orthop Sci. 2011;16(4):382–388. doi: 10.1007/s00776-011-0066-y. [DOI] [PubMed] [Google Scholar]
- 27.Cash R.M. Proprioception after arthroplasty: role of the posterior cruciate ligament. Clin Orthop Relat Res. 1996;(331):172–178. [PubMed] [Google Scholar]
- 28.van der Linden M.L. Knee kinematics in functional activities seven years after total knee arthroplasty. Clin Biomech. 2007;22(5):537–542. doi: 10.1016/j.clinbiomech.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 29.Warren P.J. Proprioception after knee arthroplasty. The influence of prosthetic design. Clin Orthop Relat Res. 1993;(297):182–187. [PubMed] [Google Scholar]
- 30.Oliver D. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122–130. doi: 10.1093/ageing/afh017. [DOI] [PubMed] [Google Scholar]
- 31.Attfield S.F. Soft-tissue balance and recovery of proprioception after total knee replacement. J Bone Joint Surg Br. 1996;78(4):540–545. [PubMed] [Google Scholar]
- 32.Barrett D.S., Cobb A.G., Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. 1991;73(1):53–56. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- 33.Swanik C.B., Lephart S.M., Rubash H.E. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004;86-A(2):328–334. doi: 10.2106/00004623-200402000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Moutzouri M. What is the effect of sensori-motor training on functional outcome and balance performance of patients' undergoing TKR? A systematic review. Physiotherapy. 2016;102(2):136–144. doi: 10.1016/j.physio.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Zeni J., Jr. Biofeedback to promote movement symmetry after total knee arthroplasty: a feasibility study. J Orthop Sports Phys Ther. 2013;43(10):715–726. doi: 10.2519/jospt.2013.4657. [DOI] [PMC free article] [PubMed] [Google Scholar]