Abstract
Introduction:
Wildland fires degrade air quality and adversely affect human health. A growing body of epidemiology literature reports increased rates of emergency departments, hospital admissions and premature deaths from wildfire smoke exposure.
Objective:
Our research aimed to characterize excess mortality and morbidity events, and the economic value of these impacts, from wildland fire smoke exposure in the U.S over a multi-year period; to date no other burden assessment has done this.
Methods:
We first completed a systematic review of the epidemiologic literature and then performed photochemical air quality modeling for the years 2008 to 2012 in the Continental U.S. Finally, we estimated the morbidity, mortality, and economic burden of wildland fires.
Results:
Our models suggest that areas including northern California, Oregon and Idaho in the West, and Florida, Louisiana and Georgia in the East were most affected by wildland fire events in the form of additional premature deaths and respiratory hospital admissions. We estimated the economic value of these cases due to short term exposures as being between $11 and $20B (2010$) per year, with a net present value of $63B (95% confidence intervals $6-$170); we estimate the value of long- term exposures as being between $76 and $130B (2010$) per year, with a net present value of $450B (95% confidence intervals $42-$1,200).
Conclusion:
The public health burden of wildland fires—in terms of the number and economic value of deaths and illnesses—is considerable.
Keywords: Health impact assessment, source apportionment, PM2.5, ozone, CMAQ, wildland fires, wildfires
1. Introduction
The increasing frequency and intensity of large wildfires deteriorates air quality and adversely affects human health (Crimmins et al. 2016; Henderson et al. 2009; Liu et al. 2015, 2016; Westerling et al. 2006). These events in turn both promote, and are exacerbated by, long-term changes to the climate; current trends in these events are expected to continue (Crimmins et al. 2016; Stavros et al. 2014). While the level and type of pollutants emitted during wildfires vary according to region and fuel type, all fires release directly emitted particulate matter (PM) as well as precursors to fine particles (PM2.5) and can contribute to downwind formation of ozone (Knorr et al. 2012).
While risks to human health from exposure to PM are especially well characterized in the epidemiological, toxicological and controlled human exposure literature (US EPA 2009), health impacts from PM stemming from wildland fires have been less extensively studied, though epidemiological literature has consistently observed adverse human health impacts attributable to wildfire-related PM2.5 (Liu et al. 2015). For example, Rappold et al., (2012b, 2011) found that a peat fire episode in eastern North Carolina was associated with increasing numbers of Emergency Department visits for cardiopulmonary and respiratory outcomes. Similarly, Delfino et al., (2009) observed increasing rates of respiratory and cardiovascular hospital admissions resulting from a month-long wildland fire episode in southern California. Epidemiological studies conducted in other countries, including Australia, have observed similar affects (Johnston et al. 2007a; Morgan et al. 2010b). A systematic review of literature from the U.S., Australia and elsewhere by Liu et al., (2014) found that wildland fire-related coarse particles (PM10) was most consistently associated with respiratory outcomes.
Despite the growing body of epidemiological studies, there are a relatively small number of air pollution risk assessments that attribute the number of premature deaths and illnesses and the economic value of health impacts to wildfire episodes. The risk assessments performed thus far have been limited in their temporal scope, using a single (2005) and projected (2016) year (Fann et al., 2013), or have been limited to examining one fire at a time (Jones et al. 2015; Kochi et al. 2012; Rappold et al. 2014; Rittmaster et al. 2006). This paper builds upon this literature to estimate the number and economic value of wildland fire PM2.5-related premature deaths and illnesses in the contiguous United States using chemical transport model predictions of PM2.5 from wildland fire episodes over a 5-year period beginning in 2008. Considering a national scope allows us to more fully capture the impact that wildland fires may have on human health.
2. Materials and Methods
In this study we characterized the overall magnitude and distribution of adverse health impacts by age and race that were associated with exposure to fire-PM2.5 during wildfire smoke episodes. We used health impact functions derived from epidemiological studies that assessed the relationship between fire-PM2.5 and expected incidence of health outcomes. We also performed a systematic literature review and meta-analysis; however, using results from the meta-analysis in a health impact function would have introduced considerable uncertainty into the estimates, and thus were not used.
2.1. Health Impact Function
The risk assessment employs a health impact function to quantify the number of wildland fire-attributable premature deaths and illnesses in each of the five years we modelled. We estimated the number of PM2.5-related deaths and hospital admissions (yij) during each year i (i=2008, 2009, 2010, 2011, 2012) among individuals in each county j (j=1,…,J where J is the total number of counties) as:
where, β is the risk coefficient, m0ija is the baseline death rate or hospital admission rate for the population in county j in year i among individuals for 5-year age strata a, Cij is annual mean wildfire-attributable PM2.5 concentration in county j in year i, and Pija is the number of residents in county j in year i for five-year age strata a.
To perform a health impact risk assessment we used baseline incidence rates, population counts, and health impact functions included in the environmental Benefits Mapping and Analysis Program—Community Edition (BenMAP-CE, v1.1) (U.S. Environmental Protection Agency 2014) to estimate counts of PM2.5 attributable deaths and respiratory hospital admissions in each of five years from 2008 to 2012. These inputs have previously been used to estimate health and economic impacts in the national ambient air quality standards reviews, and the methods have been validated in previous publications (Berman et al. 2012; Fann et al. 2011; Office of Air Quality Planning and Standards 2011). Below we describe how we specify inputs and use the BenMAP-CE tool with the appropriate input data.
2.2. Air quality modeling predictions
We simulated daily air quality from 2008 to 2012 using the Community Multiscale Air Quality version 5.1 (CMAQ v5.1) model with and without emissions from wildland fires in the contiguous United States. Wildland fires in our study included wildfires, prescribed fires, and other significant fires but it excluded agricultural fires. The difference between the two model runs represents the contribution of fire-PM2.5 and PM2.5 precursor emissions. Inputs to the model included gridded meteorological fields, emissions data, and boundary conditions. Gridded meteorological fields were provided by annual CONUS Weather Research and Forecasting (WRF) model simulation. Meteorological fields were defined on a 12 ×12 km horizontal grid with 35 vertical layers of variable thickness extending up to 50 hPa. The lowest model layer, which extended to approximately 20m above ground was used to calculate the annual mean concentration of PM2.5 (Δx) in the health impact function.
The CMAQ input emissions were based on a 12 km national U.S. domain with speciation for the Carbon-Bond 05 chemical mechanism (Yarwood et al. 2005). The emission inventory and ancillary files were based on the 2008 emissions modeling platform for 2008, 2009, and 2010 (EPA, 2012) and on the 2011 emission modeling platform for 2011 and 2012 (EPA, 2016). Since the focus of this study is wildland fires, any additional information about the non-fire emission sources is noted in the references. The fire emissions were based on year specific daily fire estimates using the Hazard Mapping System fire detections and Sonoma Technology SMARTFIRE system version 2 (Sonoma Technology 2007). Smartfire2 is a framework for producing fire activity data and allows for the merging of multiple data sources. Some of the fires included in the fire inventory come from satellite based remote sensing sources which cannot distinguish large prescribed or debris burning fires from wildfires with certainty. After multiple sources of fire information are reconciled to create fire activity estimates, the fire emissions are estimated using fuel moistures (via the USFS Wildland Fire Assessment System), consumption estimates from the Consume model (Ottmar, 2014; US Forest Service 2015), emission factors from the Fire Emission Production Simulator (Ottmar, 2014; US Forest Service 2015), and fuel loading from the United States Forest Service Fuel Characteristic Classification System (FCCS) database (McKenzie et al., 2012). Plume rise for all point sources including the wildland fires was calculated within the CMAQ model. Biogenic emissions were processed in CMAQ and are based on the Biogenic Emissions Inventory System v3.14 (Schwede et al, 2005; Carlton et al, 2011)
2.3. Effect coefficients
To identify PM2.5 effect coefficients suitable for the health burden impact assessment, we consulted two sources of evidence. The first is the U.S. EPA’s 2009 Integrated Science Assessment for Particulate Matter (PM ISA), which classified human health endpoints as having a “causal” or “likely to be causal” relationship with short-term and long-term exposure to PM2.5. The PM ISA synthesizes the epidemiological, toxicological and controlled human exposure studies published to that point, and was peer reviewed by the independent Clean Air Scientific Advisory Committee (U.S. EPA, 2009). The PM ISA indicated that mortality and cardiovascular outcomes were causally related, and respiratory outcomes were likely to be causally related, to short-term and long-term exposure to fine particle levels (U.S. EPA 2009). The ISA did not differentiate these effects by particle composition or source.
Next, we performed a systematic review and quantitative meta-analysis. We included epidemiological studies that looked at associations between PM2.5 during smoke events and various health endpoints. Studies identified were conducted in the U.S., Australia, South America, and Asia, and were limited to health endpoints identified by the PM ISA as being causally related to PM2.5 exposure. The systematic review employed a machine learning technique to identify relevant literature. We report detailed information regarding the search terms, our procedure for identifying and screening eligible literature, and a Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram in the Supplemental Materials. The machine learning literature review identified a total of 276 epidemiological studies, of which we judged 21 to be suitable to be included in the quantitative meta-analysis (Supplemental Figure 1). These 21 studies reported a total of 902 relative risks or odds ratios for respiratory (n=455) or cardiovascular (n=308) hospital or emergency department visits, or all-cause or non-accidental deaths (n=139).
A subset of 4 studies reported risk estimates for respiratory hospital admissions that reported effect coefficients for a common endpoint, PM indicator (in this case, PM10), lag structure and population age strata and so were suitable for pooling in a quantitative meta-analysis (Henderson et al. 2015; Johnston et al. 2007,b; Morgan et al. 2010a; Tham et al. 2009). Using the Metafor library in the R statistical package, we perform a random effects meta-analysis (R Core Team 2016; Viechtbauer 2010). A forest plot illustrating the studies included in the meta-analysis, a random-effects pooled estimate, and additional information regarding tests for funnel plot asymmetry can be found in the Supplemental Materials (Supplemental Figures 2 and 3).
Ultimately, for the health impact assessment, we did not use this pooled estimate because the exposure of interest for our nationwide risk assessment was PM2.5, not PM10. Additionally, the risk coefficients may not be generalizable because all 4 studies were based on wildland fire events outside of the U.S. (Henderson et al. 2015; Johnston et al. 2007b; Morgan et al. 2010a; Tham et al. 2009).Populations in other countries may respond differently to wildland fire episodes to those in the U.S., have access to a different healthcare system, may be more or less susceptible to wildland fire smoke, and may differ in other ways that we cannot observe using the available data. For these reasons, we used a risk coefficients drawn Delfino et al. (2009), which reported risk estimates for both respiratory and cardiovascular hospital admissions during the wildland fire episodes in Southern California.
We also selected PM2.5 epidemiological studies that reported short-term and long-term PM2.5 effect coefficients that did not specifically report effect estimates for exposures to wildland fire PM2.5. We used risk estimates U.S. EPA previously employed to evaluate the health benefits of alternative air quality standards (EPA 2011), recognizing that these studies do not consider PM2.5 particles originating from wildland fire events specifically and they generally consider PM2.5 concentrations at levels significantly below those observed during wildland fire episodes. The short-term studies include Zanobetti et al. (2009), a multi-city time-series study that reported hospital admissions for respiratory outcomes, and Zanobetti and Schwartz (2009), a multi-city time series study of PM2.5-related mortality. Because wildfire episodes can affect long-term levels of PM2.5, we also employ effect coefficients from long-term epidemiological studies; these include an extended analysis of the American Cancer Society (Krewski et al. 2009) and an extended analysis of the Harvard Six Cities cohort (Lepeule et al. 2012).
2.4. Baseline rates of death and hospital admissions
The epidemiological studies noted above report estimates of risk that are expressed as being relative to a baseline rate. In this analysis we used effect coefficients to quantify cases of hospital admissions and premature deaths, and thus we applied baseline rates of rates of all-cause mortality and hospital admissions. We selected county-level age-stratified all-cause death rates from the Centers for Disease Control (WONDER) database for the year 2010 (Centers for Disease Control and Prevention 2016). We selected hospital visit rates from the Healthcare Cost and Utilization Program (HCUP); these are a mixture of county, state and regional rates (See Supplemental Table 2).
2.5. Assigning PM2.5 concentrations to the population
We quantified changes in population-level exposure by assigning the predicted PM2.5 concentrations to the population in each 12km by 12km model grid cell. The BenMAP-CE tool contains 2010 U.S. Census reported population counts stratified by age, sex, race and ethnicity, assigned to each air quality grid. We used the census-reported population counts for the years 2010 and then projected these counts to the years 2011 and 2012 using the Woods and Poole forecast (Woods and Poole 2012). Population data in each year are stratified by age, sex, race, and ethnicity.
To calculate a national wildland fire PM2.5 concentrations for each of the five years that was weighted to the size of the population exposed to wildland fire PM2.5 concentrations for all counties combined (Ci) in year i as
where Cij is the wildfire-attributable annual mean PM2.5 concentration in county j in year i, Pij is the population in county j in year i, and Pi is the total population over all counties combined in year i.
2.6. Economic Values
We estimated the value of avoided premature deaths using a Value of Statistical Life (VSL) recommended by the U.S. EPA’s Guidelines for Preparing Economic Analyses (US EPA 2010). Following U.S. EPA guidelines, we indexed this value to the inflation and income year of the analysis. Using a 2010 inflation year and assuming 2016 income levels, we calculated a VSL of $10.1M. To value changes in respiratory hospital admissions, we used a cost of illness estimate U.S. EPA employed in its Regulatory Impact Analysis for the PM2.5 National Ambient Air Quality Standards (US EPA 2012). This value of $36,000 reflects the direct medical costs associated with the hospital visit as well as lost earnings.
3. Results
3.1. Air Quality
The median of the predicted annual mean wildland fire-attributable PM2.5 concentrations across all model grid cells ranges from between 0.3 μg/m3, in 2009 and 0.8 μg/m3 in 2012, while the population-weighted annual mean PM2.5 concentration ranges from between 0.6 μg/m3 in 2009 to 1.1 μg/m3 in 2008 (Table 1). In general, the distribution of wildfire attributable PM2.5 concentrations are greatest in the year 2008 and lowest in the years 2009 and 2010 of the years included in this analysis.
Table 1.
Summary statistics of annual mean PM2.5 (μg/m3) predictions across 12km grid cells attributable to wildfires (2008 to 2012)
| YearA | |||||
|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | |
| 10th %ile | 0.26 | 0.14 | 0.14 | 0.26 | 0.33 |
| 25th %ile | 0.37 | 0.18 | 0.23 | 0.40 | 0.52 |
| 50th %ile | 0.61 | 0.33 | 0.43 | 0.60 | 0.81 |
| Mean | 1.1 | 0.56 | 0.70 | 0.80 | 0.92 |
| 75th %ile | 1.4 | 0.79 | 0.96 | 1.1 | 1.2 |
| 90th %ile | 2.3 | 1.3 | 1.7 | 1.7 | 1.6 |
| Max | 42 | 6.5 | 6.5 | 23 | 17 |
| Population-weighted PM2.5 level | 1.1 | 0.61 | 0.68 | 0.73 | 0.75 |
Values rounded to two significant figures
A small number of states are most greatly affected by wildland fire events across the 5-year period (Figure 1). In the western U.S, states including California, Oregon, Idaho and Montana experience wildland fires in each year. Among the Southeastern states, North Carolina, South Carolina, Georgia, Louisiana, Arkansas, Florida and eastern Texas are most impacted.
Figure 1.
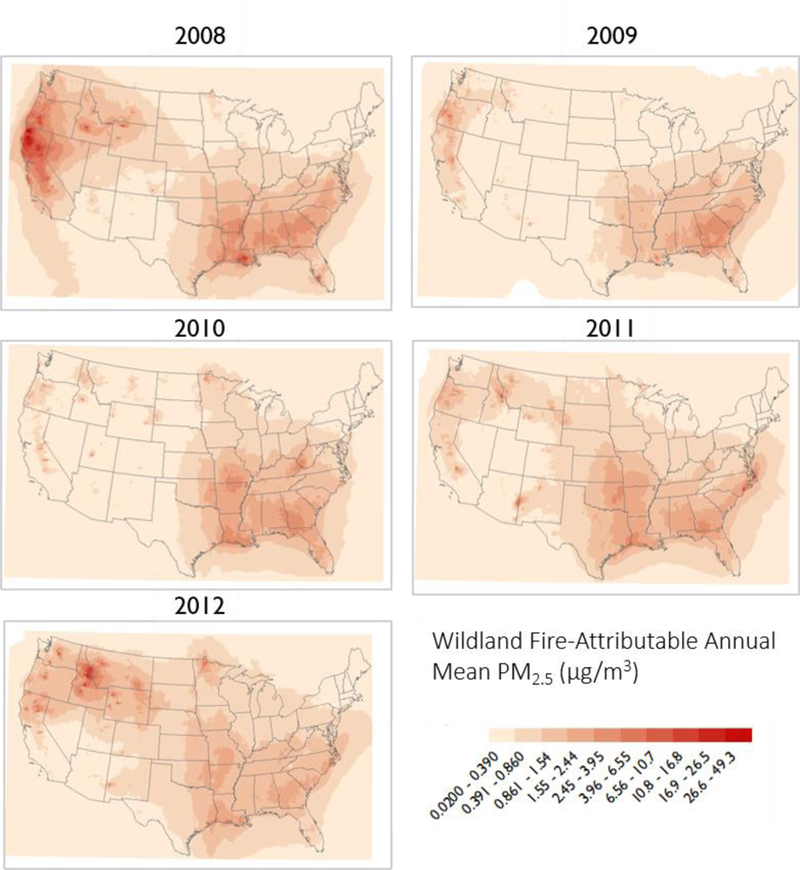
Annual mean wildland fire-attributable PM2.5 concentrations (2008– 2012)
3.2. Estimated health impacts and economic values of wildland fire events
We estimate between 5,200 to 8,500 respiratory hospital admissions per year (Table 2) (From 2008 to 2012) from wildland fires when using the concentration-response relationship from the Delfino et al. (2009) study. This range is within the same order of magnitude as the values estimated using a concentration-response relationship from the Zanobetti et al. (2009) multi-city study that did not explicitly account for wildland fire episodes (3,900 to 6,300). Using an effect coefficient from the Delfino et al. (2009) study, we also estimate between 1,500 and 2,500 cardiovascular hospital admissions. As noted above, we could not identify a suitable wildland fire study that reported a mortality effect coefficient and so used a risk coefficient from a multi-city time-series study (Zanobetti & Schwartz). We quantified between 1,500 and 2,500 wildland-attributable PM2.5-related deaths from short-term changes in PM2.5 concentrations over the five-year period (Table 2). We estimate the largest number of excess deaths and hospital admissions for the year 2008, when wildland fire attributable PM2.5 concentrations are the greatest out of the years included here.
Table 2.
Premature deaths and illnesses attributable to wildfire-related PM2.5 concentrations in each year calculated using alternative concentration-response functions (95% confidence intervals)
| Endpoint | Year |
|||||
|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | ||
| Respiratory Hospital Admissions | ||||||
| Delfino et al. (2009) | 8,500 | 5,200 | 6,200 | 6,300 | 6,400 | |
| (4,400—12,000) | (2,700—7,700) | (3,200—9,100) | (3,300—9,300) | (3,300—9,400) | ||
| Zanobetti et al. (2009) | 6,300 | 3,900 | 4,600 | 4,700 | 4,800 | |
| (3,600—9,000) | (2,300—5,500) | (2,600—6,500) | (2,700—6,700) | (2,800—6,800) | ||
| Cardiovascular Hospital Admissions | ||||||
| Delfino et al. (2009) | 2,800 | 1,700 | 2,100 | 2,100 | 2,100 | |
| (−500−−6,000) | (−320−−3,700) | (−380−−4,400) | (−380−−4,500) | (−390−−4,600) | ||
| Premature deaths from short-term exposure to PM2.5 | ||||||
| Zanobetti & Schwartz (2009) | 2,500 | 1,500 | 1,700 | 1,900 | 1,800 | |
| (1,900—3,000) | (1,100—1,800) | (1,300—2,100) | (1,400—2,200) | (1,400—2,200) | ||
| Premature deaths from long-term exposure to PM2.5 | ||||||
| Krewski et al. (2009) | 14,000 | 8,700 | 10,000 | 11,000 | 11,000 | |
| (9,700—19,000) | (5,800—11,000) | (6,900—14,000) | (7,300—14,000) | (7,600—15,000) | ||
| Lepeule et al. (2012) | 32,000 | 19,000 | 23,000 | 24,000 | 25,000 | |
| (16,000—48,000) | (9,800—29,000) | (12,000—35,000) | (12,000—36,000) | (13,000—38,000) | ||
Values rounded to two significant figures; all functions estimated for populations ages 0–99
To provide context for the estimates above, in the secondary analysis we also applied PM2.5 concentration-response relationships recently employed in U.S. EPA health impact assessments, estimating thousands of non-fatal heart attacks, thousands of respiratory and cardiovascular hospital admissions, hundreds of thousands of cases of upper and lower respiratory symptoms and millions of cases of acute respiratory symptoms (Supplemental Table 4).
Summing the economic value of the short-term premature deaths and hospital admissions we estimated a total dollar value of between $11B and $20B per year (2010$) (Table 3). The present value of these economic values across the 5-year time period is $63B (3% discount rate, 2016$). We estimated the value of the long-term PM2.5 related premature deaths and hospital admissions to fall between $76B and $130B per year (2010$). The present value of these economic values across the 5-year time period is $450B (3% discount rate, 2010$).
Table 3.
Estimated economic value of wildfire-attributable PM2.5-related premature deaths and respiratory hospital admissions (2008 to 2012) (Billions of 2010$, 95% confidence intervals)A.
| Health Endpoints | Year |
Present Value | ||||
|---|---|---|---|---|---|---|
| 2008 | 2009 | 2010 | 2011 | 2012 | ||
| Sum of mortality from short-term exposures and respiratory hospital admissions A | $20 | $12 | $14 | $11 | $12 | $63 |
| ($2—$53) | ($1—$31) | ($1—$37) | ($1—$30) | ($1—$31) | ($6—$170) | |
| Sum of mortality from long-term exposures and respiratory hospital admissions B | $130 | $76 | $90 | $96 | $100 | $450 |
| ($12—$340) | ($7—$210) | ($8—$250) | ($9—$260) | ($9—$270) | ($42—$1,000) | |
Sum of Delfino et al. (2009) respiratory hospital admission estimates and Zanobetti & Schwartz (2009) mortality.
Sum of Delfino et al. (2009) hospital admission estimates and Krewski (2009) mortality.
3.3. The distribution of wildland fire-attributable health impacts among population subgroups
We next sought to better understand how the 5-year wildland fire episodes that we modeled in CMAQ were affecting populations across the U.S. For the 2008 to 2012 time period in which we modeled wildland fire episodes we mapped the cumulative CMAQ predicted wildland fire PM2.5 concentrations as a distribution, and identified the upper 75th, 90th and 95th percentile. We then identified the portions of the CMAQ modeling domain at or above this level across the continental U.S. (Figure 2). We next characterized the populations exposed to these elevated concentrations according to their race (Table 4).
Figure 2.
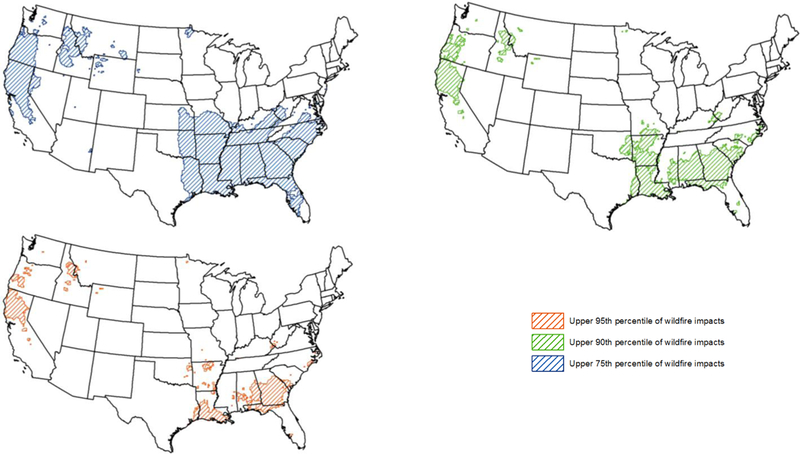
Locations of the U.S. Experiencing Elevated Wildfire-Related PM2.5 Concentrations Over a 5-year Period
Table 4.
The percentage of individuals living in locations highly affected, and less affected, by wildland fires (2008 to 2012)A
| Race | National Average | Location of the U.S.B |
Difference between highly and less affected | |
|---|---|---|---|---|
| Highly affected | Less affected | |||
| Asian | 5% | 4% | 5% | −1% |
| Black | 13% | 18% | 13% | 12% |
| Native American | 1% | 2% | 1% | 1% |
| White | 81% | 75% | 81% | −6% |
| Total | 100% | 100% | 100% | |
Highly affect subgroups are those individuals who have experienced cumulative levels of wildland fire attributable PM2.5 concentrations that are at or above the 75th percentile, identified in Figure 2 with blue hatched shading. Less affected subgroups are those not living in these areas.
Estimates rounded to two significant figures
When comparing the wildland fire-attributable PM2.5 concentrations occurring among the highly affected and less affected areas, we found that: (1) in locations of the U.S. that are most affected by wildland fires, black populations represent a larger share of the individuals exposed to wildland fire PM2.5 and a smaller share in those locations of the U.S. that are less affected by wildland fires; (2) by contrast, white populations experience a smaller share of the population in the highly affected areas and a larger share in the less affected areas.
3.4. Sensitivity Analysis
The estimated number of premature deaths and illnesses are sensitive to the predicted daily change in wildfire related PM2.5 concentrations. Smoke plume height has been repeatedly identified as one of the critical sources of uncertainty in air quality modeling (Baker et al 2016).
This parameter in turn affects the range in which particles disperse and therefore the predicted level of concentrations are most sensitive at both very short and far distances from fires. Examining model performance indicated that the model tends to over-predict at low concentrations, possibly over representing small fires, as well as at very high concentrations. Over-dispersion of particles in the model can yield an excess number of low impact days that can have a cumulative impact on the estimate of exposure.
To understand the sensitivity of our results to the high number of days with low concentrations we quantified the number of wildland fire-attributable deaths from daily changes in PM2.5 that were at least 1, 3 and 5 μg/m3 in size (Supplemental Table 3). We find that when quantifying PM2.5-related deaths on days in which wildland PM2.5 concentrations are at or above 1 μg/m3, the estimated number of premature deaths is on average 17% lower than when we do not apply this threshold; when estimating premature deaths occurring on days when PM2.5 levels at or above 5 μg/m3, there are about 44% fewer premature deaths. These results suggest that our results were sensitive to low levels of model-predicted wildland PM2.5 concentrations.
4. Discussion and Conclusions
To our knowledge, this is the first manuscript to characterize the PM2.5-related incidence and economic value of wildland fire impacts in the continental United States across an extended time period. The number of wildland fire-attributable PM2.5-related hospital admissions, emergency department visits and other outcomes we estimated in this analysis are comparable to those reported in Fann, Fulcher and Baker (2013) for the year 2016. That analysis, like this one, employed photochemical modeling surfaces and used a similar array of health impact functions. However, Fann, Fulcher and Baker (2013) calibrated the air quality modeling predictions to monitored air quality data, which would affect the level and distribution of the wildland fire-attributable PM2.5 concentrations. Here we do not calibrate model predictions with observed data because it has been noted that high concentrations of particles during wildfires restrict air flow to the pumps, shutting the monitors down and missing high concentration episodes, thus leading to potentially biased observed values. We also recognize the potential for CMAQ to overestimate wildland fire impacts (Baker et al. 2016). More complex calibration and data fusion models specific to the wildland fires are likely to become available with the increased usability of remote sensing in this area of research as well as improved parameterizations based on results from field campaigns such as the Fire and Smoke Model Evaluation Experiment (FASMEE) (http://www.fasmee.net).
The epidemiological literature reporting risks from wildland fire-related PM2.5 is sparse; this makes quantifying wildland-attributable risks challenging. The epidemiology studies that the U.S. EPA and others commonly use to quantify PM-related mortality and morbidity impacts, and reported in the Supplemental Materials to this article, were not explicitly designed to characterize risks from this emission source. However, it is reasonable to expect that many epidemiologic studies that did not explicitly address wildland fire impacts will have at least partially accounted for them, given that wildland fire particles tend to account for large portion of PM in the atmosphere (Verma et al. 2014). The National Emissions inventory of 2011 estimates that 41% of PM2.5 emissions originate with wildland burning (U.S. EPA, 2011).
In light of this limitation, when we designed the health impact assessment, we took two steps to ensure that we were using effect coefficients that were well matched to the unique characteristics of wildland fire smoke events. First, we performed a random effects quantitative meta-analysis of respiratory hospital admission epidemiological studies of smoke events in the U.S. and elsewhere in the world. Second, we selected concentration-response relationships from epidemiological studies that we believe would better account for the episodic nature of smoke events and the corresponding elevated levels of particles (Zanobetti et al. 2009; Zanobetti and Schwartz 2009).
The overall economic value of wildland fire-attributable premature deaths and respiratory hospital admissions is considerable. Depending on whether we quantify short-term PM2.5-related premature deaths or long-term PM2.5-realted deaths, the cumulative 5-year economic value is in the tens to hundreds of billions of dollars.
Nearly all states in the U.S. experienced elevated fine particle concentrations from wildland fire events over the 5-year period, according to our simulation of air quality. Certain states were affected by severe wildland fire events occurring across two or more years, including Louisiana (some of which may be due to debris burning after an active hurricane season because remote sensing of fires cannot distinguish between large debris burning from wildfires or prescribed fires), California, Idaho, and Georgia. Within these states, certain population subgroups were affected disproportionately. In particular, black populations, and to a lesser extent Asian populations, accounted for a greater share of wildland fire-attributable health impacts. State and local officials may wish to consider how best to communicate with subgroups that are most affected when deploying warning systems that alert the public to the health risks of wildland fire smoke. State and local officials deploying warning systems to alert the public to the health risks of wildland fire smoke may wish to consider how best to reach these subgroups.
This analysis is subject to certain limitations and uncertainties that shape the way in which the results may be interpreted. Considering first the air quality inputs, we assessed the performance of the chemical transport model by matching CMAQ grid locations to the locations of environmental monitors and comparing predicted and observed values. We found that the model is biased high when predicting low levels of PM2.5 concentrations. The model also over predicts PM2.5 (mainly Organic Carbon and Elemental Carbon) during all seasons for fire events. Baker et al (2016) found the Flint Hills fire overestimated OC and EC but the Wallow fire did not overestimate to the same degree suggesting there is a lot of complexity in terms of how different fires are characterized in CMAQ. Another limitation is that only fire events that are part of the emission inventory have been evaluated. Any misspecification of emissions in the inventory fires is not included in our analysis. Further scientific advances and research efforts aimed to improve characterization of fire, fuel and emissioninventories, and to improve measure characterization of differential toxicity of smoke emitted from different fuel types can potentially improve future health risk assessments.
The health impacts quantified using concentration-response relationships described in this paper are also subject to uncertainties. More specifically, questions remain regarding the extent to which certain species of fire-attributable PM may be more or less toxic than others (Sullivan et al. 2008). Thus, using effect coefficients from the epidemiological studies that did not specifically consider wildland fire episodes, may under- or over-estimate impacts. By contrast, the quantitative meta-analysis draws upon epidemiological studies of wildland fire events, but is limited to respiratory hospital admissions and PM10. Several of these studies were conducted outside of the U.S.; differences between the health care system, wildland fire particle composition, behavioral responses to smoke events and other factors may bias the meta-analysis pooled risk coefficient. We also apply the effect coefficients from the Delfino et al. (2009) study of wildfires in Southern California nationwide; this may bias our estimates of risk high or low depending on the area that it is applied to. Finally, the present value calculation assumes that the wildland fire-related premature deaths estimated for each year are independent of those estimated in all other years. For example, individuals modeled as dying prematurely from wildland fire smoke exposure in year 1 cannot also die in year 2, but the net present value calculation introduces the possibility that deaths may have been counted more than once across years. However, given that the fraction of total deaths accounted for by air pollution episodes is relatively small (approximately 6% on a national basis), the potential for this approach to bias-high the number of wildland-attributable deaths is likely small (Fann et al. 2011).
Despite these uncertainties, this manuscript also exhibits a number of strengths and unique features. First, this analysis is, to our knowledge, the first to characterize the incidence and economic value of human health impacts attributable to wildland fire-emitted fine particles in the continental U.S. over a 5-year period. Second, while previous studies have incorporated a systematic review of wildland fire studies, none to our knowledge have performed a quantitative meta-analysis. Third, we characterize both the size, and distribution, of wildland fire-related premature deaths and hospital admissions across population subgroups. Taken together, the results in this analysis suggest that the number and value of wildland fire events is considerable and that these impacts are not shared equally across the U.S. population.
Supplementary Material
Acknowledgements:
We gratefully acknowledge the comments received from Bryan Hubbell and Karen Wesson, who reviewed early versions of this manuscript.
Abbreviations
- BenMAP-CE
environmental Benefits Mapping and Analysis Program—Community Edition
- CMAQ
Community Multi-Scale Air Quality Model
- U.S. EPA
United States Environmental Protection Agency
- ICD
International Classification of Disease
- NH3
Ammonia
- NOx
Nitrogen Dioxide
- O3
Ground-level ozone
- PM2.5
Particulate matter, 2.5 microns or less in diameter
- SO2
Sulfur Dioxide
- WHO
World Health Organization
Footnotes
Disclaimer
The research described in this article has been reviewed by the National Health and Environmental Effects Research Laboratory, U.S. Environmental Protection Agency, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the Agency, nor does the mention of trade names of commercial products constitute endorsement or recommendation for use.
Competing financial interests: The authors declare no competing financial interests.
5. References
- Baker KR, Woody MC, Tonnesen GS, Hutzell W, Pye HOT, Beaver MR, et al. 2016. Contribution of regional-scale fire events to ozone and PM2.5 air quality estimated by photochemical modeling approaches. Atmos. Environ. 140:539–554; doi: 10.1016/j.atmosenv.2016.06.032. [DOI] [Google Scholar]
- Berman JD, Fann N, Hollingsworth JW, Pinkerton KE, Rom WN, Szema AM, et al. 2012. Health benefits from large-scale ozone reduction in the United States. Environ. Health Perspect. 120:1404–10; doi: 10.1289/ehp.1104851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins A, Balbus J, Gamble JL, Beard CB, Bell JE, Dodgen D, et al. 2016. HUMAN HEALTH THE IMPACTS OF CLIMATE CHANGE ON IN THE UNITED STATES THE IMPACTS OF CLIMATE CHANGE ON HUMAN HEALTH IN THE UNITED STATES. U.S. Glob. Chang. Res. Progr. [Google Scholar]
- Delfino RJ, Brummel S, Wu J, Stern H, Ostro B, Lipsett M, et al. 2009. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup. Environ. Med. 66:189–97; doi: 10.1136/oem.2008.041376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA. 2011. Regulatory Impact Assessment for Final Transport Rule.
- Fann N, Lamson AD, Anenberg SC, Wesson K, Risley D, Hubbell BJ. 2011. Estimating the National Public Health Burden Associated with Exposure to Ambient PM(2.5) and Ozone. Risk Anal. 32:81–95; doi: 10.1111/j.1539-6924.2011.01630.x. [DOI] [PubMed] [Google Scholar]
- Henderson SB, Brauer M, Kennedy S, MacNab Y. 2009. Three Measures of Forest Fire Smoke Exposure and Their Association with Respiratory and Cardiovascular Physician Visits and Hospital Admissions. Epidemiology 20:S82; doi: 10.1097/01.ede.0000362956.02139.fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson SB, Brauer M, MacNab YC, Kennedy SM. 2015. Three Measures of Forest Fire Smoke Exposure and Their Associations with Respiratory and Cardiovascular Health Outcomes in a Population-Based Cohort; doi: 10.14288/1.0074714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston FH, Bailie RS, Pilotto LS, Hanigan IC. 2007a. Ambient biomass smoke and cardio-respiratory hospital admissions in Darwin, Australia. BMC Public Health 7:240; doi: 10.1186/1471-2458-7-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston FH, Bailie RS, Pilotto LS, Hanigan IC, Samet J, Zeger S, et al. 2007b. Ambient biomass smoke and cardio-respiratory hospital admissions in Darwin, Australia. BMC Public Health 7:240; doi: 10.1186/1471-2458-7-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RR, Hogrefe C, Fitzgerald EF, Hwang SA, Özkaynak H, Garcia VC, et al. 2015. Respiratory hospitalizations in association with fine PM and its components in New York State. J. Air Waste Manag. Assoc. 65:559–569; doi: 10.1080/10962247.2014.1001500. [DOI] [PubMed] [Google Scholar]
- Knorr W, Lehsten V, Arneth A. 2012. Determinants and predictability of global wildfire emissions. Atmos. Chem. Phys. 12:6845–6861; doi: 10.5194/acp-12-6845-2012. [DOI] [Google Scholar]
- Kochi I, Champ PA, Loomis JB, Donovan GH. 2012. Valuing mortality impacts of smoke exposure from major southern California wildfires. J. For. Econ. 18:61–75; doi: 10.1016/j.jfe.2011.10.002. [DOI] [Google Scholar]
- Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, et al. 2009. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res. Rep. Health. Eff. Inst. 5-114–36. [PubMed] [Google Scholar]
- Lepeule J, Laden F, Dockery D, Schwartz J. 2012. Chronic exposure to fine particles and mortality: an extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environ. Health Perspect. 120:965–970; doi: 10.1289/ehp.1104660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Mickley LJ, Sulprizio MP, Dominici F, Yue X, Ebisu K, et al. 2016. Particulate air pollution from wildfires in the Western US under climate change. Clim. Change 1–12; doi: 10.1007/s10584-016-1762-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Pereira G, Uhl Sa, Bravo Ma, Bell ML. 2014. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res. 136:120–132; doi: 10.1016/j.envres.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu JC, Pereira G, Uhl SA, Bravo MA, Bell ML. 2015. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res. 136:120–132; doi: 10.1016/j.envres.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie D, French NH and Ottmar RD (2012). National database for calculating fuel available to wildfires. Eos, Transactions American Geophysical Union 93(6): 57–58. [Google Scholar]
- Morgan G, Sheppeard V, Khalaj B, Ayyar A, Lincoln D, Jalaludin B, et al. 2010a. Effects of Bushfire Smoke on Daily Mortality and Hospital Admissions in Sydney, Australia. Epidemiology 21:47–55; doi: 10.1097/EDE.0b013e3181c15d5a. [DOI] [PubMed] [Google Scholar]
- Morgan G, Sheppeard V, Khalaj B, Ayyar A, Lincoln D, Jalaludin B, et al. 2010b. Effects of bushfire smoke on daily mortality and hospital admissions in Sydney, Australia. Epidemiology 21:47–55; doi: 10.1097/EDE.0b013e3181c15d5a. [DOI] [PubMed] [Google Scholar]
- Office of Air Quality Planning and Standards. 2011. Regulatory Impact Assessment for the Mercury and Air Toxics Standards.
- Ottmar RD (2014). Wildland fire emissions, carbon, and climate: Modeling fuel consumption. Forest Ecology and Management 317: 41–50 DOI: 10.1016/j.foreco.2013.06.010. [DOI] [Google Scholar]
- R Core Team. 2016. R: A language and environment for statistical computing.
- Rappold AG, Fann NL, Crooks J, Huang J, Cascio WE, Devlin RB, et al. 2014. Forecast-Based Interventions Can Reduce the Health and Economic Burden of Wildfires. Environ. Sci. Technol. [DOI] [PubMed] [Google Scholar]
- Rittmaster R, Adamowicz WL, Amiro B, Pelletier RT. 2006. Economic analysis of health effects from forest fires. 877:868–877; doi: 10.1139/X05-293. [DOI] [Google Scholar]
- Sonoma Technology. 2007. SMARTFIRE system version 2.
- Stavros EN, McKenzie D, Larkin N. 2014. The climate-wildfire-air quality system: interactions and feedbacks across spatial and temporal scales. Wiley Interdiscip. Rev. Clim. Chang. 5:719–733; doi: 10.1002/wcc.303. [DOI] [Google Scholar]
- Sullivan AP, Holden AS, Patterson LA, McMeeking GR, Kreidenweis SM, Malm WC, et al. 2008. A method for smoke marker measurements and its potential application for determining the contribution of biomass burning from wildfires and prescribed fires to ambient PM 2.5 organic carbon. J. Geophys. Res. 113:D22302; doi: 10.1029/2008JD010216. [DOI] [Google Scholar]
- THAM R, ERBAS B, AKRAM M, DENNEKAMP M, ABRAMSON MJ. 2009. The impact of smoke on respiratory hospital outcomes during the 2002–2003 bushfire season, Victoria, Australia. Respirology 14:69–75; doi: 10.1111/j.1440-1843.2008.01416.x. [DOI] [PubMed] [Google Scholar]
- U.S. Environmental Protection Agency. 2014. Environmental Benefits Mapping and Analysis Program--Community Edition (BenMAP-CE).
- U.S. EPA LU-USEPA. 2009. Integrated science assessment for particulate matter. EPA/600/R-. [PubMed]
- US EPA. 2010. Guidelines for Preparing Economic Analyses.
- US EPA. 2009. Integrated Science Assessment for Particulate Matter (Final Report).
- U.S. EPA. 2011. National Emissions Inventory, 2011.
- US EPA. 2012. Regulatory Impact Assessment for the PM NAAQS RIA.
- US Forest Service. 2015. PNW - Fire and Environmental Research Applications Team (FERA) Research/Studies. Available: https://www.fs.fed.us/pnw/fera/fft/consumemodule.shtml [accessed 13 March 2017].
- Verma V, Fang T, Guo H, King L, Bates JT, Peltier RE, et al. 2014. Reactive oxygen species associated with water-soluble PM 2.5 in the southeastern United States: spatiotemporal trends and source apportionment. Atmos. Chem. Phys 14:12915–12930; doi: 10.5194/acp-14-12915-2014. [DOI] [Google Scholar]
- Viechtbauer W 2010. Conducting Meta-Analyses in R with the metafor Package. J. Stat. Softw. 36:1–48; doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- Westerling AL, Hidalgo HG, Cayan DR, Swetnam TW. 2006. Warming and earlier spring increase western U.S. forest wildfire activity. Science 313:940–3; doi: 10.1126/science.1128834. [DOI] [PubMed] [Google Scholar]
- Woods and Poole. 2012. Woods & Poole.
- Yarwood G, Rao S, Yocke M, Whitten G. 2005. Updates to the carbon bond mechanism: CB05; doi:RT-04006758. [Google Scholar]
- Zanobetti A, Franklin M, Koutrakis P, Schwartz J. 2009. Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environ. Health 8:58; doi: 10.1186/1476-069X-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanobetti A, Schwartz J. 2009. The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ. Health Perspect. 117:898–903; doi: 10.1289/ehp.0800108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


