Abstract
Objective:
Postoperative ileus (POI) is a common complication after surgery that requires a multifactorial therapeutic approach. This study aims to assess the effect of topical chamomile oil on postoperative bowel activity after cesarian section.
Methods:
This randomized controlled trial was carried out in 2015 at Chamran Hospital in Iran. A block randomization list was generated for 142 parturient divided into three groups. In the intervention group (arm A) (n = 47), chamomile oil was applied topically on abdominal region after the stability of the patient. Placebo group (arm B) (n = 47) received placebo oil and control group (arm C) (n = 48) had no intervention. A recovery program was used after surgery for all participants. The primary outcome was time to first flatus. Secondary outcomes were time to bowel sounds, defecation, return of appetite, hospital stay, and rate of nausea and vomiting, abdominal pain.
Findings:
Times to first flatus were significantly shorter in Group A (arm A vs. B, P < 0.001 and arm A vs. C, P < 0.001). In addition, time to first bowel sounds (arm A vs. B, P < 0.001 and arm A vs. C, P < 0.001) and return of appetite (arm A vs. B, P < 0.001 and arm A vs. C, P < 0.001) were significantly shorter in arm A. The times from surgery to first defecation were shorter in Group A versus B and C. However, there were no statistically significant differences between three groups.
Conclusion:
These results suggest that topical chamomile oil has a potential therapeutic effect on gastrointestinal motility and can reduce the duration of POI.
KEYWORDS: Cesarian section, complementary therapies, defecation, flatulence, ileus, Matricaria, surgery
INTRODUCTION
Postoperative ileus (POI) is a common complication following abdominal operations including cesarian section.[1] Ileus is a type of functional obstruction owing to the transient impairment of intestinal motility. This interference of the passing of gastrointestinal contents leads to delayed passage of flatus and feces, delayed oral feeding, nausea, vomiting, and postoperative pain.[2,3] The pathophysiology of POI is multifactorial and complex, including inflammatory and neurologic factors.[4] Parasympathetic dysfunction following intra-abdominal manipulation is an important etiologic factor.[5] Ileus can increase the health-care costs, prolong the hospital stay and reduce patient's satisfaction after surgery especially after cesarean section due to delay mother-baby bonding.[3] Fast recovery following cesarean section is important for both baby and mother. Therefore, finding a safe method to improve the management of POI is of great importance.
In clinical studies, several kinds of approaches have been experienced for the management of POI, such as using motility agents, early postoperative refeeding, and physical therapy but due to the limited clinical efficacy, these approaches have not been proposed to patients yet.[6,7] Therefore, looking for alternative treatment options to reduce the morbidity of the patient and the costs of hospitalization is necessary.
Matricaria chamomilla L.(Asteraceae), commonly known as chamomile, camomile, Italian camomilla, German chamomile, wild chamomile or Hungarian chamomile is one of the most common medicinal plants used for various medical conditions such as gastrointestinal disorders, colic, spasm, stomachache, irritable bowel syndrome, inflammatory diseases, and insomnia.[8] Different pieces of evidence have shown that chamomile has antispasmodic and anti-inflammatory properties and can improve gastrointestinal motility disorders.[9] It is an effective herbal remedy for dispelling gas and relaxation of the muscles of the intestinal wall due to its cholinergic effects.[10] In traditional Persian medicine, topical application of chamomile oil has been widely recommended for intestinal obstructive and motility disorders.[11] In in vitro studies, chamomile demonstrated bactericidal, acaricidal, antioxidant, antiplatelet, anticarcinoma, and anti-inflammatory activities.[12] Several animal studies suggested anxiolytic,[13] antimutagenic, cholesterol-lowering, wound healing,[14] and antidiabetic properties[15] for this plant. In clinical studies, chamomile was able to treat skin lesions and was beneficial to control mild-to-moderate inflammatory disorders.[16] Phytochemical investigation of chamomile showed the presence of quercetin, patuletin, apigenin, apigenin-7-O-glucoside, luteolin, luteolin-7-O-glucoside, caffeic acid, chlorogenic acid, bisabolol[17] farnesene, chamazulene, different coumarins, and a volatile oil composed of different kinds of monoterpenes and sesquiterpenes.[18]
Le Blanc-Louvry et al., have demonstrated that the massage of the abdominal wall after colectomy without the use of herbal oils can reduce the duration of POI.[19] Çetinkaya and Başbakkal demonstrated that the utilization of oil in massage aromatherapy is effective in reducing the symptoms of colic.[20] Moreover, in some scientific documents, it has been demonstrated that essential oils were used to massage patients during surgery.[21] Therefore, in this study, we aimed to assess the effect of topical application of chamomile oil on decreasing the duration of POI after cesarian section.
METHODS
This randomized controlled trial was carried out from April to December 2015 at Chamran Hospital of Tehran University of Medical Sciences in Iran. It is an educational and governmental center with more than 10,000 deliveries every year. The study protocol was approved by the ethics committee of Tehran University of Medical Sciences and registered with Iranian Registry of Clinical Trials (IRCT2014082818951N1). The inclusion criteria were consecutive pregnant women aged 18–35 years undergoing cesarean section, gestational age 38–42 weeks, starvation at least 8 h before surgery, clinical stability before and after surgery, agreeing to participate in the study and signing of the informed consent.
The exclusion criteria were epidural anesthesia/analgesia and other conditions that might influence gastrointestinal motility such as a history of abdominal surgery other than cesarian, chronic constipation or other gastrointestinal disorders, chronic use of opiates, chronic use of drugs with impact on intestinal peristalsis, cesarean hysterectomy, extensive adhesiolysis, peritoneal carcinomatosis, severe postpartum hemorrhage (exceeding 500 ml), the development of complications during or within 24 h after surgery, severe organ (kidney, liver, or heart) dysfunction and using other prokinetic drugs. Furthermore, the women with acute gestational complications such as preeclampsia and those who received magnesium sulfate were excluded, because this medication may affect intestinal peristalsis. Written informed consent was obtained from all participants before surgery. Two consultant surgeons performed all operations, and the technical aspects of the surgery were left to the individual surgeons' discretion. The duration of surgery was the time between incision of skin and dressing placement. The estimated intraoperative blood loss (in ml) was documented. A recovery program was employed after surgery in all participants for postoperative management. This program comprises early removal of urinary catheter, early mobilization, and drinking of liquids as soon as bowel movement occurs or passage of flatus and progress to a normal diet on the basis of tolerance after the operation. Postoperative pain was controlled using intravenous Pethidine (10 mg/kg) as a baseline analgesic treatment immediately after surgery for all patients. Thereafter, rescue pain relief was administered by the reception of Diclofenac suppository if necessary. Discharge of patients was based on off intravenous fluids, regular diet toleration and stool passing, full ambulant and without evidence of complications. A block randomization list was generated for 150 patients without stratification based on a computer-generated random allocation sequence with six sequences in each block. Randomization to three groups of study, intervention group (chamomile oil), placebo group (paraffin oil), and control group (no intervention), occurred preoperatively. The allocation was carried out by research assistant on the day of surgery after obtaining informed consent. Allocation assignments were deposited in consecutively, sealed, numbered, and opaque envelopes. The patient and the investigator were blinded to treatment assignment in the intervention group and placebo group. In the intervention group, chamomile oil (20 drops) was applied topically on the abdominal region after consciousness and stability of patient every 1 h in the first 4 h and then every 8 h until fecal defecation. Placebo group received placebo oil (paraffin oil) in the same manner. All group received postoperative routine care. The therapy was administered by the research assistant and was recorded in the patient's file on a separate masked record. The preparation of chamomile oil was done according to that proposed in traditional Persian medicine manuscripts. For this purpose, 200 g dried flowers of M. chamomilla var. chamomilla was soaked in 1 L of distilled water for 24 h. Thereafter, it was boiled by medium heat until one quadrant of the content was remaining. Then, it was filtered, and the same volume of mineral oil was added to the filtrate and placed over medium heat until the water was fully evaporated and only the oil remained.[22] The final product was packaged in airtight, light-resistant containers.
For standardization of chamomile oil, chemical composition of its essential oil was determined by gas chromatography–mass spectrometry (GC-MS). For this purpose, 100 ml of oil was mixed with 100 ml of distilled water and the essential oil was extracted by hydrodistillation using Clevenger apparatus for 5 h. The obtained essential oils were dried using anhydrous sodium sulfate and stored at low temperature (+4°C). The essential oil was analyzed using an Agilent 6890 GC with BPX5 column (30 m × 0.25 mm, ft 0.25 μm); carrier gas, He; split ratio, 1:25 and using Mass Detector. The column temperature was programmed at 50°C for 5 min and heated at the rate of 3°C/min until 240°C, then raised to 300°C at a rate of 15°C/min and then kept constant for 3 min. The MS was operated at 70 eV ionization energy. Retention indices were calculated using retention times of n-alkanes. The essential oil components were identified based on the National Institute of Standards and Technology and Wiley mass spectral library. The major endpoint of the study was to compare time to first passage of flatus in patients of three groups. Secondary outcomes were the time from surgery to first bowel sounds, defecation, return of appetite, start oral intake, and hospital stay. In addition, rate of nausea and vomiting, abdominal pain, and amount of analgesic used were assessed. The outcomes were recorded based on the end of operation and times were measured in hours. Demographic data included age, body mass index, educational level, obstetrical history, duration of the operation, kind of cesarian, method of anesthesia, perception of analgesic, prior operations, and associated medical problems. Safety assessments in this study included the report of adverse events. Adverse events were defined as any complication if they occurred after the first dose of study medication and up to 2 days after the last dose. Adverse event related to drug usage include erythema, pruriency, dermatitis, and medical problems. The sample size was adjusted to detect a clinically relevant absolute difference of 6 h in the time to the first flatus between placebo and control group and 4 h in the intervention group with a significance level of 0.05 and a power of 90%. We calculated that 50 patients per three study arm would be needed assuming a standard deviation of 6 h for the intervention group, 10 h for placebo and control groups, and deviation of 6 h for three groups.[20,21] In total, 150 patients were required for the study with an estimated dropout rate of 10% per group. Calculations were performed using G*3power software Universität Düsseldorf, Germany. Continuous variables were expressed as mean (standard deviation) or median (range), and ordinal and categorical data were summarized as counts and percentages. The analysis of categorical data was done using the Chi-square test or Fisher's exact test, as appropriate. The primary endpoint (time to first flatus) and secondary endpoints were analyzed using ANOVA, Robust Welch Tests, and Kruskal–Wallis test. Comparisons between groups were done by the Tukey HSD and Games–Howell test. The value of statistical significance was set at P < 0.05. SPSS version 22 (IBM Company, USA) was used for all statistical analyses.
RESULTS
The hydrodistillation of chamomile oil yielded a blue-colored oil (yield: 0.10% W/V). Fifteen constituents were identified in the essential oil representing 80.95% of the total. The most abundant components were α-bisabolone oxide A (33.10%) and α-bisabolol oxide A (17.18%), respectively.
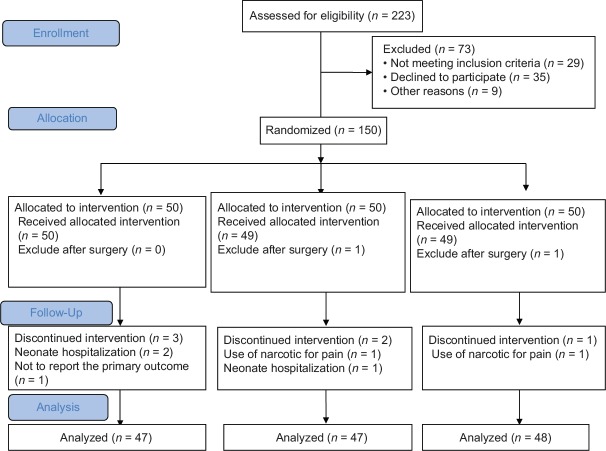
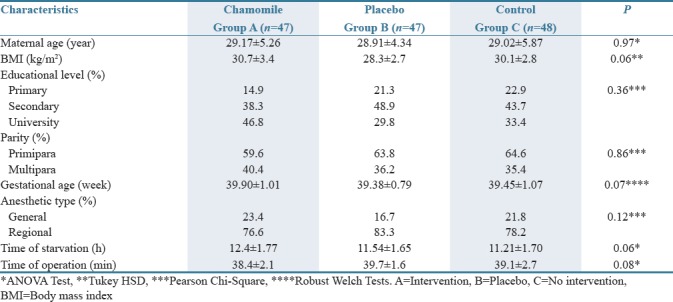
Recruitment of patients into this study occurred between April and December 2015, at Chamran Hospital of Tehran University of Medical Sciences in Iran. Of the 223 screened patients, 73 were excluded before randomization. The patient flow is detailed in the CONSORT diagram [Figure 1]. One hundred and fifty patients were randomly assigned, 50 to the intervention group, 50 to the placebo group, and 50 to the control group. Of the 150 patients, 8 (5.4%) did not complete the allocated treatment (two were excluded after surgery while six discontinued the intervention). The most common reasons for discontinuation of treatment were neonate hospitalization (n = 3), use of narcotic for pain (n = 2), and not to report the primary outcome (n = 1). Therefore, 142 patients were included in the analysis [Figure 1]. Demographic and operation characteristics of the patient had no significant difference among the three study groups [Table 1].
Figure 1.
CONSORT diagram of study
Table 1.
Demographic and surgical characteristics
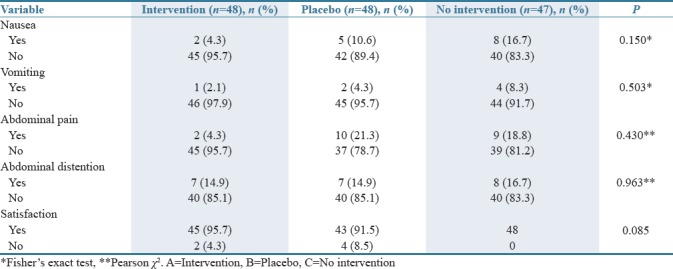
The times to first passing of flatus were significantly shorter in Group A (Group A: 20.58 h vs. Group B: 27.73 h, P < 0.001; Group A: 20.58 h vs. Group C: 28.09 h, P < 0.001). In addition, the times to first bowel sounds (Group A: 11.23 h vs. Group B: 18.24 h, P < 0.001; Group A: 11.23 h vs. Group C: 19.62 h, P < 0.001) and the times to return of appetite (Group A: 10.46 h vs. Group B: 15.61 h, P < 0.001; Group A: 10.46 h vs. Group C: 15.96 h, P < 0.001) were significantly shorter in arm A. Nevertheless, there were no significant differences between Group B and C in these outcomes. The times to first passing of stool were shorter in Group A versus B and Group B versus Group C. However, there was no statistically significant difference between three groups. The time of hospital stay had no significant difference between three groups (P = 0.16) [Table 2]. The rate of nausea, vomiting, abdominal pain, and amount of analgesic use after surgery was less in Group A, but there was no statistically significant difference among three groups [Table 3].
Table 2.
Primary and secondary outcome results in patients who underwent caesarian surgery in Groups of study
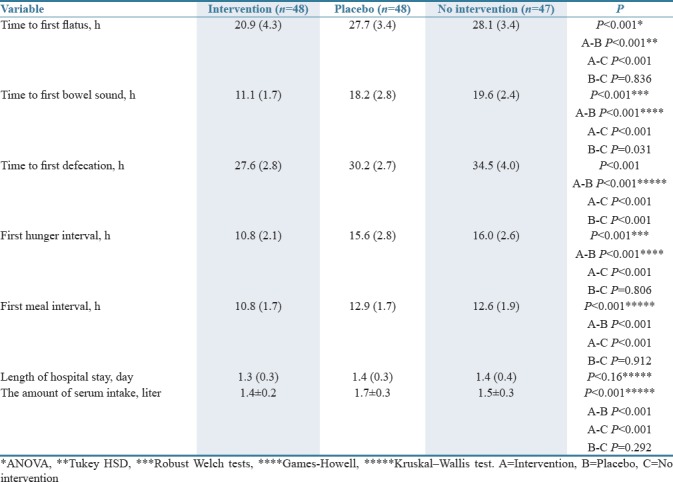
Table 3.
Secondary outcome results in patients who underwent caesarian surgery in groups of study
No side effects were observed during the application of this therapeutic method.
DISCUSSION
The aim of this study was to examine the effect of topical application of chamomile oil on POI after cesarian section. This study was developed based on the principles of traditional Persian medicine, regarding the therapeutic role of topical application of medicinal plants on the gastrointestinal tract. To the best of our knowledge, no other similar studies examining the effects of topical application of chamomile oil on bowel movements during the early stage of POI have been conducted. Our evaluation on 150 parturient patients showed that topical chamomile oil could be effective for the improvement of POI. The data indicated that the postoperative time to first flatus, bowel sound, and defecation in intervention group significantly decreased in comparison with placebo and control groups, but there was not any significant difference in the time of hospital stay.
In our study, the mean time to first flatus in the intervention group was 20.58 while this time in placebo and control groups was 27.73 and 28.09 h, respectively (P < 0.001). Similarly, in a study by Jakkaew and Charoenkwan on the effect of gum chewing on bowel motility after cesarian section, the time to first flatus was 28.8 h in the intervention group and 29.8 h in the control group.[22] Moreover, data in the study of Ajuzieogu et al., on the effects of gum chewing on the recovery of bowel function following cesarian section indicated that the mean times to first flatus were 24.8 and 30.0 in the intervention and placebo group, respectively.[23] The time to the first passage of flatus in the study of Mohsenzadeh Ledari et al., was 25.0 in the intervention group and 31.0 in control group.[24] We reported similar results to these experimental studies.
The pathogenesis of ileus has not been completely known, and it seems that it is a multifactorial problem. Based on some studies, ileus could be due to an inflammatory process related to surgical manipulation of the intestine during surgery that leads to significant leukocyte infiltration of muscular layer of intestine and intensive induction of inducible nitric oxide (NO) synthase.[2] Topical application of herbal medicines affecting the gastrointestinal tract is an emphasized treatment method in traditional Persian medicine.[25] Chamomile oil (M. chamomilla) has been recommended as a topical digestive relaxant in traditional Persian medicine.[26] In the literature, it is demonstrated that chamomile has effective role in the treatment of gastrointestinal and bowel movements disorders.[27] Furthermore, chamomile has anti-inflammatory properties. The flowers of this plant contain a volatile oil that comprises α-bisabolol, matricin, α-bisabolol oxides A and B, and other terpenoids that have anti-inflammatory properties.[28] The flavonoids of chamomile have inhibitory effect on endogenous prostaglandin E2 levels in macrophages. The polyphenols of chamomile have anti-inflammatory property related to inhibition of proinflammatory biomarkers in macrophages (THP1) and can reduce inflammation of neurovascular units in the gastrointestinal tract. In addition, chamomile has neuroprotective property due to the reduction of NO level.[29] These effects can support the beneficial effects of chamomile on controlling the POI based on its pathophysiological nature, i.e., inflammation and neural process.
Our study showed that topical chamomile has a potential therapeutic effect on gastrointestinal motility disorders. This method is emphasized in traditional Persian medicine in the treatment of gastrointestinal disorders. According to this perspective, chamomile can be absorbed topically on the abdominal skin to relieve therapeutic gastrointestinal effects.[11,25] In the modern medicine, there is no strategic approach to the treatment of gastrointestinal disorders using topical drugs. Nevertheless, some studies have shown the effect of using medicinal oils to treat some disorders such as gastrointestinal disorders.[20] Zargaran et al. have demonstrated that flavonoids and volatile oils of chamomile can penetrate into the deeper layers of the skin and relieve migraine pain.[29] Several studies have demonstrated that the topical application of medical oils can enhance the content of the active ingredients in the circulation.[29,30] Muniandy and Sinnathamby demonstrated that the topical application of massage oils could lead to the systemic salicylate toxicity in infants.[30] This evidence suggests that the topical application of medical oils could have systemic effects, depending on the dose and intensity of penetration.[26] Moreover, many studies offer massage aromatherapy as a treatment for some disorders such as gastrointestinal problems.[20] In this regard, Stea et al. stated the therapeutic effect of essential oils on surgical patients.[21] It is believed that essential oils can penetrate through the skin and cause systemic effects due to small molecular size and high penetration of their ingredients.
Topical application of essential oils is often associated with other treatments, such as massage; therefore, it is difficult to separate their effect. Nevertheless, some clinical scientific evidence demonstrated that massage with essential oils was more effective than massage alone.[27] However, in our study, there was no effective massage due to the pain associated with the surgical scars and chamomile oil was gently applied on the skin. Some study demonstrated oral mineral oil can use in the treatment of constipation.[28] This study was showed its use on the abdominal cavity appears to improve bowel movements specially defecation. However, the effect of chamomile with mineral oil was more effective statistically.
In this study, the absence of a large sample size precluded a more definite statement whether the topical application of chamomile oil can reduce the duration of POI. Another limitation of this study was the inability to blind the control group due to the nature of the study. The selection of parturient patients and cesarian surgery might not allow the results of the study to be generalized to other operations of the gastrointestinal tract. More studies are required to stabilize the findings of this study, especially the trend in topical application of medicines in gastrointestinal diseases.
This randomized controlled trial study suggests that topical chamomile oil is able to reduce the time to return of bowel function in the early stage after cesarian section. However, further studies are required to validate and generalize our findings.
AUTHORS' CONTRIBUTION
EKh and MSh study concept and design and study supervision; FGh study concept and analysis and interpretation of data; FGh, RR and PA prepared the manuscript; FGh checking the references; RR plagiarism checker.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This paper was derived from a Ph. D. thesis entitled “Explanation of Paralytic Ileus according to Traditional Persian Medicine” which was supported by the School of Traditional Medicine, Tehran University of Medical Sciences.
REFERENCES
- 1.Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001;182:3S–10S. doi: 10.1016/s0002-9610(01)00781-4. [DOI] [PubMed] [Google Scholar]
- 2.Wolff BG, Viscusi ER, Delaney CP, Du W, Techner L. Patterns of gastrointestinal recovery after bowel resection and total abdominal hysterectomy: Pooled results from the placebo arms of alvimopan phase III North American clinical trials. J Am Coll Surg. 2007;205:43–51. doi: 10.1016/j.jamcollsurg.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Nantasupha C, Ruengkhachorn I, Ruangvutilert P. Effect of conventional diet schedule, early feeding and early feeding plus domperidone on postcesarean diet tolerance: A randomized controlled trial. J Obstet Gynaecol Res. 2016;42:519–25. doi: 10.1111/jog.12942. [DOI] [PubMed] [Google Scholar]
- 4.Mythen MG. Postoperative gastrointestinal tract dysfunction. Anesth Analg. 2005;100:196–204. doi: 10.1213/01.ANE.0000139376.45591.17. [DOI] [PubMed] [Google Scholar]
- 5.Sahin E, Terzioglu F. The effect of gum chewing, early oral hydration, and early mobilization on intestinal motility after cesarean birth. Worldviews Evid Based Nurs. 2015;12:380–8. doi: 10.1111/wvn.12125. [DOI] [PubMed] [Google Scholar]
- 6.Agah J, Baghani R, Rakhshani MH, Rad A. Metoclopramide role in preventing ileus after cesarean, a clinical trial. Eur J Clin Pharmacol. 2015;71:657–62. doi: 10.1007/s00228-015-1845-8. [DOI] [PubMed] [Google Scholar]
- 7.Teoh WH, Shah MK, Mah CL. A randomised controlled trial on beneficial effects of early feeding post-caesarean delivery under regional anaesthesia. Singapore Med J. 2007;48:152–7. [PubMed] [Google Scholar]
- 8.LawGow B. PDR for Herbal Medicine. 4th ed. Montvale, New Jersey: Thomson; 2007. [Google Scholar]
- 9.Vissiennon C, Goos KH, Arnhold J, Nieber K. Mechanisms on spasmolytic and anti-inflammatory effects of a herbal medicinal product consisting of myrrh, chamomile flower, and coffee charcoal. Wien Med Wochenschr. 2017;167:169–76. doi: 10.1007/s10354-016-0538-y. [DOI] [PubMed] [Google Scholar]
- 10.Srivastava JK, Shankar E, Gupta S. Chamomile: A herbal medicine of the past with bright future. Mol Med Rep. 2010;3:895–901. doi: 10.3892/mmr.2010.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khadem E, Shirazi M, Rahimi R, Bioos S, Ghorat F. Perception of paralytic ileus on viewpoint of avicenna. Iran J Public Health. 2017;46:150–2. [PMC free article] [PubMed] [Google Scholar]
- 12.Merfort I, Heilmann J, Hagedorn-Leweke U, Lippold BC. In vivo skin penetration studies of camomile flavones. Pharmazie. 1994;49:509–11. [PubMed] [Google Scholar]
- 13.Evans S, Dizeyi N, Abrahamsson PA, Persson J. The effect of a novel botanical agent TBS-101 on invasive prostate cancer in animal models. Anticancer Res. 2009;29:3917–24. [PubMed] [Google Scholar]
- 14.Patzelt-Wenczler R, Ponce-Pöschl E. Proof of efficacy of Kamillosan (R) cream in atopic eczema. Eur J Med Res. 2000;5:171–5. [PubMed] [Google Scholar]
- 15.Shukla S, Mishra A, Fu P, MacLennan GT, Resnick MI, Gupta S, et al. Up-regulation of insulin-like growth factor binding protein-3 by apigenin leads to growth inhibition and apoptosis of 22Rv1 xenograft in athymic nude mice. FASEB J. 2005;19:2042–4. doi: 10.1096/fj.05-3740fje. [DOI] [PubMed] [Google Scholar]
- 16.Golami A, Tabaraei Y, Ghorat F, Khalili H. The Effect of inhalation of Matricaria chamomile essential oil on patients' anxiety before esophagogastroduodenoscopy. Govaresh. 2018;22:232–8. [Google Scholar]
- 17.Cemek M, Yilmaz E, Büyükokuroğlu ME. Protective effect of Matricaria chamomilla on ethanol-induced acute gastric mucosal injury in rats. Pharm Biol. 2010;48:757–63. doi: 10.3109/13880200903296147. [DOI] [PubMed] [Google Scholar]
- 18.Carnat A, Carnat AP, Fraisse D, Ricoux L, Lamaison JL. The aromatic and polyphenolic composition of Roman camomile tea. Fitoterapia. 2004;75:32–8. doi: 10.1016/j.fitote.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Le Blanc-Louvry I, Costaglioli B, Boulon C, Leroi AM, Ducrotte P. Does mechanical massage of the abdominal wall after colectomy reduce postoperative pain and shorten the duration of ileus? Results of a randomized study. J Gastrointest Surg. 2002;6:43–9. doi: 10.1016/s1091-255x(01)00009-9. [DOI] [PubMed] [Google Scholar]
- 20.Çetinkaya B, Başbakkal Z. The effectiveness of aromatherapy massage using lavender oil as a treatment for infantile colic. Int J Nurs Pract. 2012;18:164–9. doi: 10.1111/j.1440-172X.2012.02015.x. [DOI] [PubMed] [Google Scholar]
- 21.Stea S, Beraudi A, De Pasquale D. Essential oils for complementary treatment of surgical patients: State of the art. Evid Based Complement Alternat Med 2014. 2014:726341. doi: 10.1155/2014/726341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jakkaew B, Charoenkwan K. Effects of gum chewing on recovery of bowel function following cesarean section: A randomized controlled trial. Arch Gynecol Obstet. 2013;288:255–60. doi: 10.1007/s00404-013-2727-x. [DOI] [PubMed] [Google Scholar]
- 23.Ajuzieogu OV, Amucheazi A, Ezike HA, Achi J, Abam DS. The efficacy of chewing gum on postoperative ileus following cesarean section in Enugu, South East Nigeria: A randomized controlled clinical trial. Niger J Clin Pract. 2014;17:739–42. doi: 10.4103/1119-3077.144388. [DOI] [PubMed] [Google Scholar]
- 24.Mohsenzadeh Ledari F, Barat S, Nasiri Amiri F, Aghajani Delavar M, Banihosseini SZ, Khafri S. Effect of gum chewing after cesarean-delivery on return of bowel function. Bosn J Basic Med Sci. 2012;14:19–24. [Google Scholar]
- 25.Al Qanun Fi Al-Tibb (Arabic) Beirut: Alaalami Library; 2005. Avicenna; pp. 324–5. [Google Scholar]
- 26.Mosavat SH, Masoudi N, Hajimehdipoor H, Emami Meybodi MK, Niktabe Z, Tabarrai M, et al. Efficacy of topical Linum usitatissimum L.(flaxseed) oil in knee osteoarthritis: A double-blind, randomized, placebo-controlled clinical trial. Complement Ther Clin Pract. 2018;31:302–7. doi: 10.1016/j.ctcp.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 27.Bakhtshirin F, Abedi S, YusefiZoj P, Razmjooee D. The effect of aromatherapy massage with lavender oil on severity of primary dysmenorrhea in Arsanjan students. Iran J Nurs Midwifery Res. 2015;20:156–60. [PMC free article] [PubMed] [Google Scholar]
- 28.Saneian H, Tavakkol K, Adhamian P, Gholamrezaei A. Comparison of Lactobacillus sporogenes plus mineral oil and mineral oil alone in the treatment of childhood functional constipation. J Res Med Sci. 2013;18:85–8. [PMC free article] [PubMed] [Google Scholar]
- 29.Zargaran A, Borhani-Haghighi A, Faridi P, Daneshamouz S, Kordafshari G, Mohagheghzadeh A, et al. Potential effect and mechanism of action of topical chamomile (Matricaria chammomila L.) oil on migraine headache: A medical hypothesis. Med Hypotheses. 2014;83:566–9. doi: 10.1016/j.mehy.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 30.Muniandy RK, Sinnathamby V. Salicylate toxicity from ingestion of traditional massage oil. BMJ Case Rep 2012. 2012 doi: 10.1136/bcr-2012-006562. pii: bcr2012006562. [DOI] [PMC free article] [PubMed] [Google Scholar]