Abstract
Objective:
The burden of musculoskeletal disease remains high in low-income countries, with a high rate of pediatric disease. Efforts continue for orthopaedic education, but there is little guidance on local needs and desires. Our aim was to determine the specific content and modalities that would be most useful for pediatric orthopaedic educational programs abroad, and we demonstrate a practical method of identifying country-specific educational deficits through a self-reported needs survey in Haiti.
Design:
A cross-sectional survey was administered using an automated response system. We obtained demographic information as well as training and practice patterns, comfort levels with pediatric diagnoses, and desired topics for education using a 5-point Likert Scale.
Setting:
Haitian Annual Assembly for Orthopaedic Trauma (HAAOT), the only national, continuing medical education conference for orthopaedic providers in Haiti.
Participants:
Of 60 eligible participants, 51 were included in the final analysis.
Results:
Time spent on pediatric orthopaedics varied widely, centered at 10-25%. Median comfort level with pediatric orthopaedics was 3 out of 5. Skills with lowest self-reported competence included spica casting, clubfoot casting, and management of supracondylar humerus fractures. Skills with highest self-reported competence were long-leg casting and Salter-Harris classification. Modes of education highly requested included didactics/lectures, hands-on sessions, dedicated rotations, and exchanges with foreign peers/mentors. Diagnoses most encountered were osteomyelitis, trauma, and clubfoot; lowest comfort levels were in neuromuscular, spine, lower extremity deformity, congenital hip, and clubfoot; and most requested for future teaching were congenital hip, neuromuscular, and spine.
Conclusions:
Haitian orthopaedic providers express a strong desire and need for ongoing pediatric orthopaedic education. They describe a high prevalence of trauma and infection, but convey a requirement for more comprehensive, multi-modal teaching that also includes congenital deformities/dysplasias, neuromuscular, and spine. Our results demonstrate the importance of assessing country-specific needs and involving local care providers in curriculum development.
Keywords: surgical education, pediatric orthopaedics, developing country, Haiti, needs assessment
Introduction
The global burden of surgical disease is large and growing, particularly related to orthopaedic problems. An estimated 100 million procedures remain unperformed worldwide for injuries, congenital anomalies, and other musculoskeletal disease alone.1 Moreover, orthopaedic diagnoses are an increasing cause of global disability-adjusted life years lost, most notably in resource-challenged nations with high rates of childhood disease.2–4 Numerous individuals and professional societies are focused on pediatric orthopaedics abroad 5, with long-standing efforts established in Uganda 6, Malawi 7, 8, India 9, 10, and Nepal 11 amongst others.
Ranking as the poorest country in the Americas, and one of the poorest in the world, Haiti has also has been the site of numerous orthopaedic efforts since a magnitude 7.0 earthquake in January 2010.12–15 Orthopaedic training has been established as an important component of improving surgical care in low-resource countries.16–18 Past efforts have provided proof of concept for continuing medical education (CME) in developing countries including Haiti.19 In 2013, the first national CME conference for orthopaedics in Haiti since the earthquake was established – the Haitian Annual Assembly of Orthopaedic Trauma (HAAOT).20 Despite the multiple programs that focus on developing pediatric orthopaedics in developing countries, no study to date has explored educational needs and desires specific to treating children in this context. This has limited the design of any pediatric orthopaedic curriculum abroad including the efforts in the HAAOT. Prior work at this conference demonstrated the benefits of an audience response tool to allow real-time feedback from attendees regarding self-perceived needs on education topics, but content focused only on trauma in the general (adult) patient setting.20
We present a needs assessment survey and analysis of the educational priorities for pediatric orthopaedics in Haiti. We believe this is an important step to guide ongoing pediatric orthopaedic efforts in Haiti and other low-income countries, and an example of incorporating country-specific perspectives into surgical curriculum development abroad.
Materials and Methods
The survey was conducted in April 2015 during the Haitian Annual Assembly for Orthopaedic Trauma (HAAOT). This was the third annual conference in Port-au-Prince and featured original research presentations, didactic lectures, and hands-on learning. It has had demonstrable success in education, expanding beyond trauma into multiple sub-specialties.20, 21 Survey participants included local, Haitian orthopaedic residents and surgeons, as well as a small number of non-orthopaedic physicians and nurses invested in musculoskeletal care. Participation was voluntary and anonymous.
With input from both Haitian and U.S.-based (“foreign”) pediatric orthopaedic surgeons, a 28-question survey was designed to assess pediatric orthopaedic educational needs, including training and practice patterns, levels of comfort in this field, perceived clinical burden, and both the form and content desired for ongoing education. We conducted directed interviews with three senior pediatric orthopaedic surgeons, active for many years educating Haitian surgeons, in order to formulate general themes for query. Specific questions and response options were then formulated with two prior conference organizers familiar with demographics of the attendees, and reviewed for content, clarity and language by a U.S-based pediatric orthopaedic surgeon and expert in American resident and fellow education. Questions were directed towards understanding perceived areas of need, clinical volume, and preferred modes of education in order to objectively guide future conference programming and education.
Responses were collected using a 1 to 5 Likert Scale or by having participants select diagnoses from a list of options - upper extremity (UE) trauma, lower extremity (LE) trauma, spine deformity and trauma, congenital UE, congenital hip, LE deformity, neuromuscular, clubfoot, osteomyelitis and septic arthritis, or compartment syndrome. Demographic information about respondents, including nationality, age, gender, level of training, base hospital, and years in practice was also obtained. Survey questions were collected in real-time using an electronic audience response system (TurningPoint ResponseCard RF, Turning Technologies).22 Cumulative time to answer all questions was approximately 14 minutes. Each answer was registered exclusively to a unique individual while maintaining anonymity.
Median and mean scores were calculated and ranges presented for all Likert scale questions. Responses of Haitian and U.S.-based orthopedic surgeons were collected but given that the vast majority of foreign participants were not pediatric orthopaedic specialists, foreign comfort levels and current practice patterns are not reported. Given all U.S.-based responses were accounted for, respondents with missing data for nationality (n=18) were recorded as Haitian. Participants not responding to at least 50% of the demographic questions were excluded as these 9 individuals either discontinued participation or had markedly higher nonresponse rate overall (data not shown). Individual question response rates ranged from 47% to 96%. For questions in which more than one answer choice was requested, responses were included if at least one answer choice was provided. Missing data for all questions were excluded from the denominator in percent calculations. Analyses were performed using SAS version 9.4 (SAS Institute, Inc.; Cary, NC, USA).
Results
Demographics
Of the 60 eligible participants, 9 did not complete a majority of the demographic questions, and 51 participants were included in the final analysis. Multiple hospitals around the country were represented, including all centers with orthopaedic residency programs. The majority of participants were male (88%), were orthopaedic residents (67%), and had attended the prior year’s conference (61%) (Table 1). The year in training was not available. However, as a proxy, we documented number of years since completing medical school and demonstrate a broad distribution of respondents (Haitian + U.S) by year across residents as well as junior and senior attendings: 8% were <1yr since graduation, 3% 1 yr, 7% 2yrs, 10% 3yrs, 12% 4yrs, 4% 5yrs, 12% 6 yrs, 15% 7-10yrs, 10% 11-20 yrs, and 19% >20 yrs.
TABLE 1. Demographics of conference attendees participating in survey.
Missing responses indicated as unspecified and included in denominator. HUEH - Hôpital de l’Université d’Etat d’Haiti (in Port-au-Prince), HUJ – Hôpital Universitaire Justinien (in Cap-Haïtien), HSN – Hôpital Saint Nicolas (in Saint-Marc). HAAOT – Haitian Annual Assembly of Orthopaedic Trauma.
Demographics of Survey Participants (N = 51)
| Characteristics | Number (%) of Respondents |
|---|---|
| Gender | |
| Male | 45 (88) |
| Female | 3 (6) |
| Unspecified | 3 (6) |
| Years since obtaining MD | |
| 0 - 2 | 10 (20) |
| 3 - 4 | 11 (22) |
| 5 - 6 | 8 (16) |
| 7 - 10 | 9 (18) |
| > 10 | 7 (14) |
| Unspecified | 6 (12) |
| Primary Hospital | |
| HUEH | 17 (33) |
| La Paix | 14 (27) |
| HUJ | 6 (12) |
| Adventist | 2 (4) |
| HSN | 2 (4) |
| Other Haitian | 7 (14) |
| Unspecified | 3 (6) |
| Position | |
| Orthopaedic resident | 34 (67) |
| Orthopaedic attending | 9 (18) |
| Non-orthopaedic physician | 4 (8) |
| Nurse | 2 (4) |
| Unspecified | 2 (4) |
| Attended HAAOT in prior year | |
| Yes | 31 (61) |
| No | 18 (35) |
| Unspecified | 2 (4) |
Training and Practice Patterns
Reported percent of training involving pediatric orthopaedics ranged from 0 to greater than 50%, with a broad distribution and median response of 10-25% (Figure 1). Participants indicated a slightly higher percentage of time involving pediatric orthopaedics in their current or expected careers, with a range from 0 to greater than 50%.
FIGURE 1. Patterns of exposure.
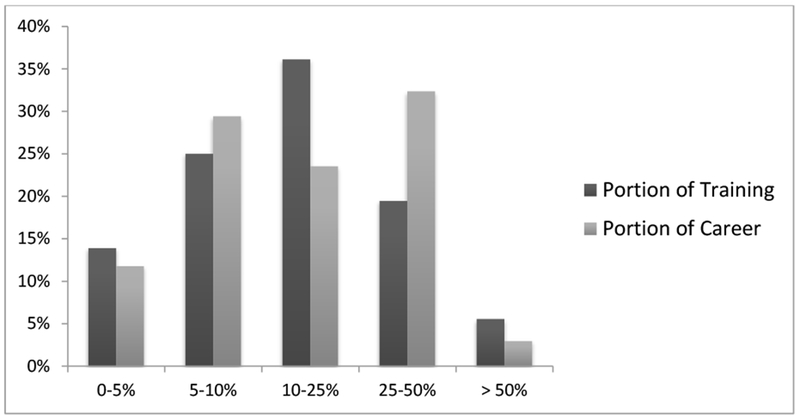
Percentage of training (dark) or career (light) that involves (or will involve) pediatric orthopaedic care. 15/51 and 17/51 missing responses for percent training and career respectively. Missing respondents excluded from denominator.
Comfort Level with Pediatric Orthopaedics
Reported overall comfort level managing pediatric orthopaedic patients ranged from 1 (least comfortable) to 5 (most comfortable), with median 3 out of 5 (38%) (Figure 2). The median response did not differ between residents and attending surgeons (both 3 out of 5), but the interquartile range for residents was [2, 3] compared to [3, 4.5] for attendings. For selected skills/topics in pediatric orthopaedics, respondents were more comfortable with use of the Salter-Harris classification and long leg (above-knee) casting (median 5 out of 5 for each) than with spica casting for a femur fracture (median 3.5), independent management of a supracondylar humerus fracture (median 3.0), or clubfoot casting (median 3.0). The three latter topics had a wide range of responses, with at least 50% of respondents indicating comfort levels of 3 out of 5 or less. Comfort with clubfoot casting revealed a bimodal distribution with approximately 1/3 of respondents stating 3 out of 5 and 1/3 of respondents stating 5 out of 5.
FIGURE 2. Patterns of comfort.
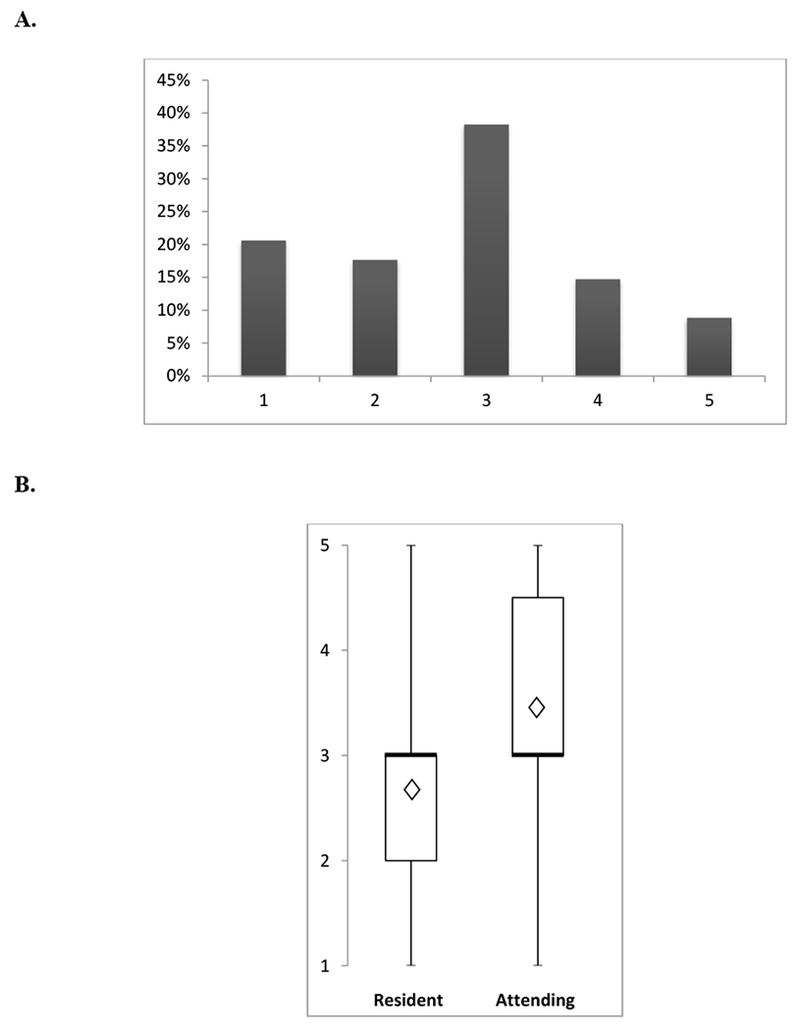
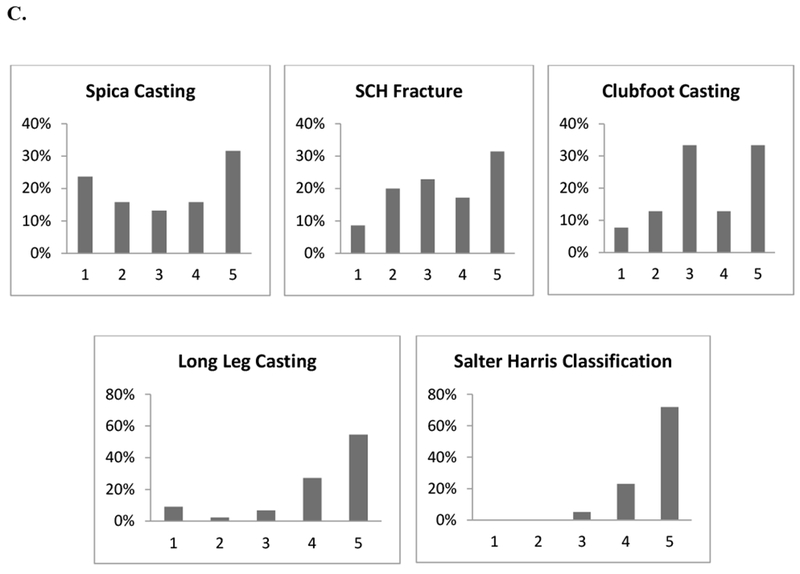
Self-reported comfort level with pediatric orthopaedics (A) in general, (B) by level of training, and (C) by specific pediatric skill. Horizontal dark lines in box-plots represent median, diamonds represent mean, box range indicates 25th to 75th percentile, whiskers extend to minimum and maximum values. Likert scale: 1 = least comfortable, 5 = most comfortable. Missing responses excluded: 17/51 for overall comfort, 11/23 and 2/7 for residents and attendings respectively, range 13/51 to 20/51 for topic areas. SCH – Supracondylar humerus.
Educational Needs and Desires
Sixty five percent of respondents rated the importance of pediatric orthopaedic education in Haiti at a 4 or higher out of 5 (5 = most important). The majority of respondents reported 5 out of 5 need (5 = most needed) for pediatric orthopaedic education in the form of more didactics/lectures (69%), hands-on skills workshops (75%), a dedicated rotation (84%), and access to international peers and mentors (86%).
We then examined patterns of need by diagnosis. Attendees selected the top 3 pediatric orthopaedic diagnoses that they: 1) saw the most in Haiti, 2) were least comfortable with, and 3) most wanted to focus on in future teaching programs (Figure 3). Infection (including osteomyelitis and septic arthritis), trauma, and clubfoot were the most commonly encountered. Respondents were least comfortable managing the diagnoses of lower extremity deformity, congenital hip pathology, neuromuscular disease, and spine disorders. Topics with the highest demand for future teaching were congenital hip pathology, neuromuscular disease, and spine disorders. Of the three diagnoses most seen, the topic respondents felt most uncomfortable with was clubfoot, with 29% of people including it as one of the 3 diagnoses they were least comfortable managing.
FIGURE 3. Patterns of need and desire.
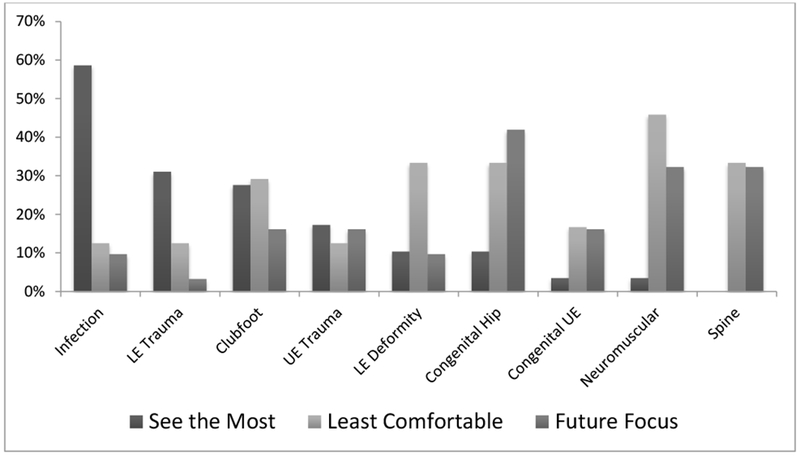
Self-reported rates of pediatric orthopaedic diagnoses that Haitian participants see the most, are least comfortable with, and would like future teaching sessions on. Percentages are percent of individuals who included each diagnosis as 1 of their top 3 choices for each question. Missing rates for each question category ranged from 39% to 53% (considered missing if 0 diagnoses provided). Infection = osteomyelitis and septic arthritis, LE = lower extremity, UE = upper extremity.
Discussion
There is a growing recognition of the importance of orthopaedic surgical education in low-resource settings. Pediatric orthopaedics in particular remains plagued by a lack of specialty training in developing nations despite a disproportionately high rate of pediatric burden due to a younger population and increased rates of trauma compared to high-income countries.4 This clinical gap has motivated several bi-directional initiatives such as travel fellowships for foreign orthopaedic surgeons, including Haiti’s only two pediatric orthopaedic surgeons, to participate in specialty-specific conferences in the United States.23 Another approach in this subspecialty has been to organize outreach courses in resource-challenged environments.5
Given the considerable time and resources required for global orthopaedic programs, it is important to understand local needs and interests in creating sustainable educational interventions desired by and helpful for in-country care providers. This work presents the first published effort to describe pediatric orthopaedic educational needs in a low-income country. In this study of orthopaedic providers, we found a strong desire and self-reported need for opportunities to better learn pediatric orthopaedics through ongoing lectures and skills workshops, a dedicated rotation during residency, and access to international peers/mentors.
While survey results show that the average time spent on pediatric orthopaedics is roughly concordant between training and practice, the wide range of residency time spent on pediatric care suggests a markedly heterogeneous experience across trainees that may leave some unprepared for eventual career needs. In addition, variation in self-reported comfort levels within pediatric orthopaedics may be a result of inconsistent efficacy of training that is received. These findings suggest that more than simply increasing the quantity of education, programs should focus on improving effectiveness and consistency of education across all trainees. A dedicated pediatric orthopaedic rotation or teaching curriculum during residency may help to standardize trainee experience at least to a minimum level of exposure. Discussions continue in Haiti around such a curriculum, including a central rotation in which all trainees rotate with the few pediatric sub-specialists, which our results would support.
Only moderate (3 out of 5) median levels of comfort are seen with pediatric orthopaedics, a concerning result given the relatively high number of children most practitioners treat. While the distribution of comfort level for attendings was skewed higher than residents, even for attending surgeons all comfort levels were represented, with the same overall median as residents. Particular discomfort with spica cast application, independent management of supracondylar humerus fractures, and clubfoot casting, in combination with high self-reported rates of trauma and clubfoot encountered in Haiti, suggest a need for future workshops and teaching focused on mastery of these basic skills in pediatric care. Of note, even long leg casting, the area in which respondents reported highest levels of confidence, showed less than 60% of participants completely comfortable with this skill, with several individuals reporting comfort level 1 out of 5 (least comfortable), indicating clear room for improvement in this critical skill for pediatric trauma.
Infection, trauma, and clubfoot were perceived to be the most frequent pediatric diagnoses encountered. Of these, clubfoot was reported as the diagnosis with which participants felt least comfortable. However, diagnoses most desired for future educational focus correlated with diagnoses seen least frequently. This may reflect more anxiety and less comfort with areas of less experience. In planning future pediatric orthopaedic curricula in low-income nations, topics of high clinical burden, low comfort level, and high surgeon interest should be considered and delivered appropriately.
Our study has several key limitations. The survey was restricted to self-reported measures of comfort, burden of disease, and educational needs. We believe this is a useful initial approach as it engages local providers by making them the central focus of the study. Moreover, learning in CME programs is more likely to yield change of practice when needs assessments have been implemented 24, and we hope pediatric orthopaedic teaching in Haiti will have increased acceptance if aligned with local needs and desires. Ultimately, objective measures can be collected to validate the results our study reports.
Our findings are also limited by a number of missing responses. Using our automated response system we had an excellent sampling of conference attendees present at the start of the survey (low total nonresponse), with the overall 76% response rate due mainly to noncoverage via some conference attendees arriving after survey administration. Our main challenge was progressive item nonresponse and partial nonresponse amongst the participants. We believe the primary contributor was survey fatigue as response rate decreased over time (data not shown). In this case, we expect missing data would be randomly distributed and not impact our conclusions based on the “missing completely at random” (MCAR) assumption, however this cannot be confirmed and the risk remains for non-random loss of data.25 We did utilize deductive imputation where appropriate to minimize missing rates. Our response rate is comparable to other global needs assessment surveys in Haiti 26, but with alternative methods coupling surveys with raffle tickets for textbooks as inducement for participation, our group has found improved participation rates in subsequent surveys (unpublished data). Repeated sampling with improved participation could validate our presently reported results.
Selection or sampling bias is also a possible limitation in our study design surveying attendees at a national conference. However, as HAAOT is the largest gathering of orthopaedic providers in the country, with no dedicated pediatric subspecialty groups, we feel this is the largest feasible sampling of the Haitian orthopaedic community. Furthermore, while the survey was distributed to all Haitian attendees regardless of specialty or focus, pediatric care is distributed broadly across the general orthopaedic community unlike the highly specialized care in developed nations. We do note the majority of survey participants were trainees or attending surgeons in practice for fewer than 10 years but believe this is an appropriate population to help guide interventions in Haiti.
Our study is the first assessment of pediatric orthopaedic educational needs in a developing nation, and our results support the need for a comprehensive pediatric orthopaedic educational effort in Haiti. Prior models exist for pediatric trauma curricula both in developed and developing countries. 27, 28 Based on our findings, however, while topics should continue to include infection and trauma (based on clinical burden), curricula should have a renewed integration of congenital anomalies including clubfoot and congenital hip pathology. Such a program should include a combination of didactic lectures, hands-on skills sessions, and a mechanism for ongoing communication and interaction with visiting pediatric specialists. Efforts are underway for such teaching modules in Haiti through U.S.-based professional societies, and we hope this study can support and guide such work, with a call to integrate the various international pediatric orthopaedic programs into a cohesive educational curriculum based on local provider needs and desires.
Supplementary Material
Acknowledgments:
We would like to acknowledge the American Academy of Pediatrics Section on Orthopaedics for supporting this work with a Global Outreach Mentored Travel Scholarship for the primary author. In addition, the American Academy of Orthopaedic Surgery (AAOS) and the Foundation of Orthopaedic Trauma (FOT) contributed funds towards the HAAOT.
This work was also conducted with consulting from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102). The content is solely the responsibility of the authors and does not necessarily represent the views of supporting centers.
Finally, we sincerely thank Drs. Robert Cady, Kaye Wilkins, and Scott Nelson for their guidance on the state of pediatric orthopaedics in Haiti which informed survey creation and analysis.
Conflicts of Interest and Source of Funding:
RAQ received travel funding in the form of the Global Outreach Mentored Scholarship from the American Academy of Pediatrics Section on Orthopaedics for this work. RAQ is currently receiving support from a T32 training grant (AR055885) from the National Institute of Health. RAQ, HJR, ARB, and GSD all received travel funding in part from the American Academy of Orthopaedic Surgery and the Foundation of Orthopaedic Trauma for conference organization. EL receives funding support from a K24 National Institute of Arthritis and Musculoskeletal and Skin Diseases grant (AR057827). The remaining authors have no other conflicts or funding.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Compliance with Ethical Standards
Ethical Approval and Informed Consent:
The protocol was reviewed and considered exempt by the institutional review board at Partners Healthcare. It did not include animal studies, and human participants proceeded with implied consent through voluntary participation. The study was performed in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW. Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health. 2015;3 Suppl 2:S13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Burden of Disease. Vol 2016: Institute for Health Metrics and Evaluation. [Google Scholar]
- 3.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- 4.Hyder AA, Sugerman DE, Puvanachandra P, et al. Global childhood unintentional injury surveillance in four cities in developing countries: a pilot study. Bulletin of the World Health Organization. 2009;87:345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shirley ED, Sabharwal S, Schwend RM, Cabral C, Spiegel D. Addressing the Global Disparities in the Delivery of Pediatric Orthopaedic Services: Opportunities for COUR and POSNA. Journal of pediatric orthopedics. 2016;36:89–95. [DOI] [PubMed] [Google Scholar]
- 6.Pirani S, Naddumba E, Mathias R, et al. Towards effective Ponseti clubfoot care: the Uganda Sustainable Clubfoot Care Project. Clinical orthopaedics and related research. 2009;467:1154–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorman SL, Graham SM, Paniker J, Phalira S, Harrison WJ. Establishing a children’s orthopaedic hospital for Malawi: A review after 10 years. Malawi Med J 2014;26:119–123. [PMC free article] [PubMed] [Google Scholar]
- 8.Youssef A, Harrison W. Establishing a children’s orthopaedic hospital for Malawi: an assessment after 5 years. Malawi Med J 2010;22:75–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agarwal A, Gupta N. Does initial Pirani score and age influence number of Ponseti casts in children? International orthopaedics. 2014;38:569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gadhok K, Belthur MV, Aroojis AJ, et al. Qualitative assessment of the challenges to the treatment of idiopathic clubfoot by the Ponseti method in urban India. The Iowa orthopaedic journal. 2012;32:135–140. [PMC free article] [PubMed] [Google Scholar]
- 11.Spiegel DA, Shrestha OP, Rajbhandary T, et al. Epidemiology of surgical admissions to a children’s disability hospital in Nepal. World journal of surgery. 2010;34:954–962. [DOI] [PubMed] [Google Scholar]
- 12.Bar-On E, Lebel E, Kreiss Y, et al. Orthopaedic management in a mega mass casualty situation. The Israel Defence Forces Field Hospital in Haiti following the January 2010 earthquake. Injury. 2011;42:1053–1059. [DOI] [PubMed] [Google Scholar]
- 13.Clover AJ, Rannan-Eliya S, Saeed W, et al. Experience of an orthoplastic limb salvage team after the Haiti earthquake: analysis of caseload and early outcomes. Plastic and reconstructive surgery. 2011;127:2373–2380. [DOI] [PubMed] [Google Scholar]
- 14.Lorich DG, Jeffcoat DM, MacIntyre NR, Chan DB, Helfet DL. The 2010 Haiti earthquake: lessons learned? Techniques in hand & upper extremity surgery. 2010;14:64–68. [DOI] [PubMed] [Google Scholar]
- 15.Teicher CL, Alberti K, Porten K, Elder G, Baron E, Herard P. Medecins sans frontieres experience in orthopedic surgery in postearthquake Haiti in 2010. Prehospital and disaster medicine. 2014;29:21–26. [DOI] [PubMed] [Google Scholar]
- 16.Carlson LC, Slobogean GP, Pollak AN. Orthopaedic trauma care in Haiti: a cost-effectiveness analysis of an innovative surgical residency program. Value Health. 2012;15:887–893. [DOI] [PubMed] [Google Scholar]
- 17.Derkash RS, Kelly N. The history of orthopaedics overseas. Clinical orthopaedics and related research. 2002:30–35. [DOI] [PubMed] [Google Scholar]
- 18.Silva JF. The urgent need to train orthopaedic surgeons in Third World countries. Med Educ 1979;13:28–30. [DOI] [PubMed] [Google Scholar]
- 19.Wilkins KE. Providing outreach continuing education in countries with limited resources. Clinical orthopaedics and related research. 2008;466:2413–2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhashyam AR, Fils J, Lowell J, Meara JG, Dyer GS. A novel approach for needs assessment to build global orthopedic surgical capacity in a low-income country. J Surg Educ 2015;72:e2–8. [DOI] [PubMed] [Google Scholar]
- 21.Fils J, Bhashyam AR, Pierre Pierre JB, Meara JG, Dyer GS. Short-Term Performance Improvement of a Continuing Medical Education Program in a Low-Income Country. World journal of surgery. 2015;39:2407–2412. [DOI] [PubMed] [Google Scholar]
- 22.Hussain H, Burfat AM, Samad L, Jawed F, Chinoy MA, Khan MA. Cost-effectiveness of the Ponseti method for treatment of clubfoot in Pakistan. World journal of surgery. 2014;38:2217–2222. [DOI] [PubMed] [Google Scholar]
- 23.Fornari ED, Sabharwal S, Schwend RM. The POSNA-COUR International Scholar Program. Results of the First 7 Years. Journal of pediatric orthopedics. 2016. [DOI] [PubMed] [Google Scholar]
- 24.Grant J, Stanton F. The Effectiveness of Continuing Professional Development Association for the Study of Medical Education. Edinburgh: 2000. [Google Scholar]
- 25.Brick JM, Kalton G. Handling missing data in survey research. Stat Methods Med Res 1996;5:215–238. [DOI] [PubMed] [Google Scholar]
- 26.Nadas M, Bedenbaugh R, Morse M, McMahon GT, Curry CL. A needs and resource assessment of continuing medical education in Haiti. Ann Glob Health. 2015;81:248–254. [DOI] [PubMed] [Google Scholar]
- 27.Kadish HA, Bolte RG, Santora SD, Espinoza R, Woodward GA. Evaluating the effectiveness of a pediatric trauma educational program in Central America. Pediatr Emerg Care. 1996;12:407–410. [DOI] [PubMed] [Google Scholar]
- 28.Valani RA, Yanchar N, Grant V, Hancock BJ. The development of a national pediatric trauma curriculum. Med Teach. 2010;32:e115–119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


