SUMMARY
Objective:
To validate the Brain Symptom and Impact Questionnaire (BASIQ) version 1.0 for brain metastases.
Methods:
Patients with brain metastases and their healthcare professionals (HCPs) assessed the relevance of the BASIQ on a 0–10 scale with 10 as extremely relevant.
Results:
A total of 52 patients and 20 HCPs participated in this study. In total, 95% of HCPs and 85% of patients found all items relevant. Balance and walking ability were rated relevant by 100% of patients and HCPs. Headache, nausea, energy, memory and ability to do housework were also rated relevant by 100% of HCPs. Over 95% of patients determined the items of ability to do housework, tiredness, energy, vision, memory and putting ideas into words as relevant. There were no items rated below 7 by patients or below 5 by HCPs.
Conclusion:
This study indicates that BASIQ version 1.0 has valid content items encompassing disease-related symptom and impact on daily living.
KEYWORDS: BASIQ, brain metastases, content validation, quality of life, questionnaire
Practice points.
This is the first study examining the content validity of the Brain Symptom and Impact Questionnaire (BASIQ) version 1.0 in both patients and healthcare professionals (HCPs).
The BASIQ instrument focuses on measuring the severity of the most relevant symptoms associated with brain metastases and their impact on patients’ activities of daily living and quality of life.
The BASIQ is brief with only 18 questions, thus alleviating some of the burden felt by brain metastases patients when they are asked to complete a quality of life assessment.
The patient feedback indicated that the questionnaire was overall well received in this patient population. There were no items that were consistently identified as upsetting, confusing or difficult to answer. The majority of patients and HCPs felt that all items included were relevant to brain metastases patients. The study supports the content validity of the BASIQ version 1.0.
Our study only included patients with a relatively good performance status, and excluded those who were cognitively impaired, which may be a limitation.
Further data are needed to examine the psychometric properties of this scale.
Background
An estimated 20–40% of advanced cancer patients will develop brain metastases from their underlying primary cancer [1–4]. The incidence of brain metastases appears to be rising due to the improvements in imaging modalities and treatment of primary cancer [1,3]. Clinically, patients with brain metastases present with a number of symptoms such as loss of motor and sensory function, seizures, cranial neuropathies and cognitive decline [5]. Therapeutic interventions for these patients often include corticosteroids, whole-brain radiotherapy, surgery or stereotactic radiosurgery [3,5,6]. Whole-brain radiotherapy allows for symptomatic relief and tapering of corticosteroids and is commonly used in patients with multiple lesions [7]. More aggressive treatments such as surgery and stereotactic radiosurgery are utilized in patients with solitary or few metastases and good performance status [6,8,9]. Despite treatment, the median length of survival is still limited [8]. Thus, due to the short length of survival, assessment of quality of life (QOL) is of great importance in this patient population [9].
QOL is a subjective, multidimensional construct that includes physical, psychosocial and overall well-being domains [10]. Currently, for this patient population, patient-reported outcome (PRO) tools such as the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire – Brain Neoplasm and the Functional Assessment of Cancer – Brain (FACT-Br) are commonly employed for QOL assessment. Both of these tools, however, were originally created and validated in populations of patients with primary brain cancers [10,11]. These patients with primary brain cancers may experience symptoms different from those with brain metastases. Additionally, those with metastases may have additional symptoms and psychosocial impact on their wellbeing that is not addressed by these primary brain tumor questionnaires. Few studies have assessed the differences between QOL in brain metastases and primary brain tumor patients, thus it cannot be concluded that it is appropriate to assess these two populations utilizing the same instruments. Additionally, the two current brain tumor questionnaires are both quite lengthy and can often be a burden on advanced cancer patients with low performance status, which is why shorter questionnaires are more appropriate and should be developed [12].
The Brain Symptom and Impact Questionnaire (BASIQ) version 1.0 was developed to address the fact that current questionnaires were originally developed for primary brain tumor patients and that these questionnaires are lengthy. The BASIQ was developed with input from clinical experts and interviews with patients with brain metastases. It is a brief 18-item instrument covering both symptom and impact (the degree to which certain symptoms affect daily living) scales relevant to this population with 12 domains: headaches, dizziness, nausea, numbness, energy, balance, vision, memory, cognition, vision, physical activities and self-care (Supplementary material). The relative brevity of this questionnaire reduces patient burden while maintaining the breadth of coverage.
The purpose of this study was to examine the validity of the content assessed in the BASIQ version 1.0 in patients with brain metastases and the healthcare professionals (HCPs) who are involved in the care of these patients. Whether or not items were appropriate to this patient population and how important each item was perceived to be by patients and HCPs alike was analyzed.
Methods
• Patients & HCPs
English-speaking patients over the age of 18 years with histologically proven primary cancer and radiographically proven single or multiple brain metastases were eligible for this study. To ensure patients cognitive ability to complete the assessment, they were required to complete the Mini Mental Status Exam prior to completing the BASIQ version 1.0. Those patients who provided written informed consent and scored greater than 23 points on the Mini Mental Status Exam were included in this study. Patient demographic information such as gender, age, Karnofsky Performance Score, Eastern Cooperative Oncology Group performance status, primary cancer site, number of brain metastases and sites of other metastases were collected.
HCPs involved in the care of patients with brain metastases were included in this study and information on their gender, profession and number of years of experience was collected.
• Validation procedure
Brain metastases patients were administered the BASIQ questionnaire version 1.0 to assess the relevancy of each of the 18 items. Patients were asked whether or not they found each item relevant (yes/no), and subsequently rated that item’s relevancy on a scale of 0 (‘Not at all’) to 10 (‘Very relevant’). After the completion of the relevancy rating of each item of the BASIQ, patients were individually interviewed in regards to the wording of the items. Patients were to identify if they found any items upsetting, difficult to answer, annoying, confusing or irrelevant (and the reason). Patients were also asked to indicate any additional issues they felt should be included in this questionnaire.
HCPs were also asked to rate the relevancy of the BASIQ items on a scale of 0 (‘Not at all’) to 10 (‘Very relevant’). For any items rated below a 4 on the relevancy scale, HCPs were asked to provide their reasoning why. They were also asked if each item was either inappropriate to patients (yes/no) or upsetting to patients (yes/no). HCPs were to list any other symptom and impact items that should be added to the questionnaire, as well as comment on the wording of items.
• Statistical methods
Data were analyzed using Statistical Analysis Software (SAS version 9.2 for Windows). Demographic data were expressed through descriptive statistics. Mean, standard deviation (SD), median and interquartile scores were used to express the degree of relevancy of each item as rated by patients and HCPs. Frequency analysis was used to determine the relevance of each item to patients and HCPs. We calculated 'mean percentage of relevance' from patient and HCP responses, using (% from patients’ response + % from HCPs’ response)/2, in order to ensure equal weight of patients’ and HCPs’ responses if the sample sizes of the two groups were unequal. Mean and the SD of relevant (0–10) responses were also calculated from the two groups, pooled SD was calculated by:
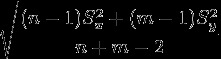 |
where n and m are the number of patients and number of HCPs,  is the variance of patient group, and
is the variance of patient group, and  is the variance of HCP group.
is the variance of HCP group.
To compare relevant scores (0–10) between patient and HCP ratings, Wilcoxon rank-sum nonparametric test was performed. Using Fisher exact test, the comparison between these two groups was also conducted for percentage of relevancy on each item. For multiple comparisons adjustments, two-sided Bonferroni p-value less than 0.05 was considered as statistically significant.
Results
A total of 52 patients and 20 HCPs participated in this study. The median age of patients was 61 years old. The median Karnofsky Performance Score was 80 and the median Eastern Cooperative Oncology Group performance status was 1 (Table 1). The majority of patients (69%) were female, with the most common primary cancers being the lung (54%), breast (21%) and kidney (8%). Most patients (94%) were recruited from a radiotherapy clinic and were outpatients. In total, 56% of patients had only one brain metastasis and 52% of patients had no other site of metastases. Just over half of HCPs were female (55%) and the majority were radiation oncologists (45%) or radiation therapists (45%). The average number of years of professional experience was 9 years (Table 2).
Table 1. . Patient characteristics (n = 52).
| Characteristic | n | % |
|---|---|---|
| Age (years) | ||
| n | 52 | |
| Mean ± SD | 59.9 ± 11.6 | |
| Median (range) | 61.0 (26 – 86) | |
| KPS | ||
| n | 32 | |
| Mean ± SD | 79.4 ± 14.1 | |
| Median (range) | 80 (40 – 100) | |
| ECOG | ||
| n | 32 | |
| Mean | 1 | |
| Median (range) | 1 (0–3) | |
| 0 | 9 | 28.13 |
| 1 | 20 | 62.50 |
| 2 | 1 | 3.12 |
| 3 | 2 | 6.25 |
| 4 | 0 | 0 |
| Gender | ||
| Female | 35 | 68.63 |
| Male | 16 | 31.37 |
| Primary cancer site | ||
| Lung | 28 | 53.85 |
| Breast | 11 | 21.15 |
| Kidney | 4 | 7.69 |
| Gynecology | 3 | 5.78 |
| Melanoma | 3 | 5.78 |
| Others | 2 | 3.85 |
| Unknown | 1 | 1.92 |
| Accrual | ||
| Radiotherapy clinic | 49 | 94.23 |
| Hospital ward | 2 | 3.85 |
| Inpatient ward | 1 | 1.92 |
| Out-/In-patients | ||
| Outpatient | 49 | 94.23 |
| Inpatient | 3 | 5.77 |
| Number of brain metastases | ||
| 1 | 29 | 55.77 |
| 2 | 5 | 9.62 |
| 2–3 | 8 | 15.38 |
| >3 | 10 | 19.23 |
| Other site of metastases | ||
| Bone | 2 | 3.85 |
| Lung | 7 | 13.46 |
| Liver | 3 | 5.77 |
| Lymph | 11 | 21.15 |
| Others | 2 | 3.85 |
| None | 27 | 51.92 |
ECOG: Eastern Cooperative Oncology Group Performance Scale; KPS: Karnofsky Performance Scale; SD: Standard deviation.
Table 2. . Healthcare professionals' demographics (n = 20).
| Demographic | n | % |
|---|---|---|
| Years of professional experience | ||
| n | 20 | |
| Mean ± SD | 9.0 ± 7.2 | |
| Inter-quartiles | 5 – 11 | |
| Median (range) | 7.0 (1.5 – 30) | |
| Gender | ||
| Female | 11 | 55.00 |
| Male | 9 | 45.00 |
| Profession | ||
| Radiation Oncology | 9 | 45.00 |
| Radiation Therapy | 9 | 45.00 |
| Medical Oncology | 1 | 5.00 |
| Nursing | 1 | 5.00 |
SD: Standard deviation.
• Patient responses
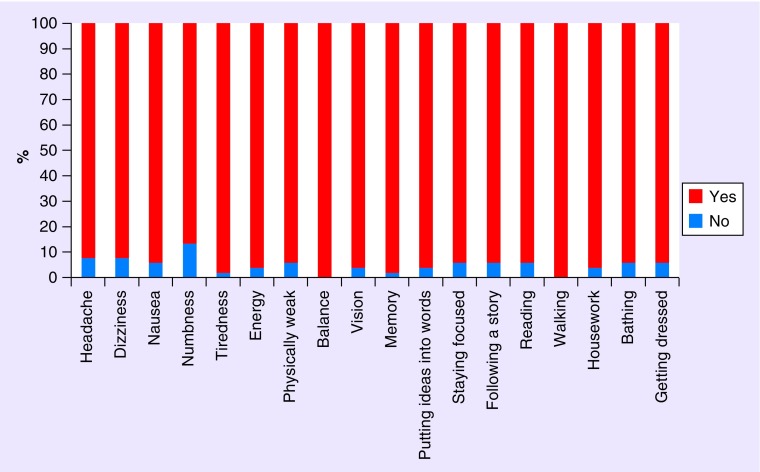
All of 52 patients determined whether the item was relevant (yes/no), and we had 51 patients rating the relevancy scores (0–10). The items of balance and walking were determined to be relevant by 100% of patients (Figure 1). Other highly relevant items included tiredness (98%), memory (98%), energy (96%), vision (96%), ability to put ideas into words (96%) and ability to do housework (96%). All items, except for numbness (87%), were rated as relevant by over 92% of patients. All items were rated as at least 7/10 for degree of relevancy. Items that received a degree of relevancy greater than 8/10 included: tiredness, balance, vision, memory and walking (Table 3).
Figure 1. . Patient responses on whether each item was relevant (yes/no).
n = 52 patients.
Table 3. . Degree of relevancy as rated by patients.
| BASIQ item | n | Mean | SD | Median | Interquartiles | |
|---|---|---|---|---|---|---|
| 1. Headache | 51 | 7.73 | 3.30 | 10.00 | 7.00 | 10.00 |
| 2. Dizziness | 51 | 7.82 | 3.25 | 10.00 | 7.00 | 10.00 |
| 3. Nausea | 51 | 7.25 | 3.45 | 9.00 | 5.00 | 10.00 |
| 4. Numbness | 51 | 7.08 | 3.43 | 8.00 | 6.00 | 10.00 |
| 5. Tiredness | 51 | 8.10 | 2.33 | 9.00 | 5.00 | 10.00 |
| 6. Energy | 51 | 7.98 | 2.30 | 9.00 | 5.00 | 10.00 |
| 7. Physically weak | 51 | 7.86 | 2.66 | 9.00 | 6.00 | 10.00 |
| 8. Balance | 51 | 8.35 | 2.32 | 9.00 | 7.00 | 10.00 |
| 9. Vision | 51 | 8.10 | 2.83 | 10.00 | 7.00 | 10.00 |
| 10. Memory | 51 | 8.24 | 2.57 | 10.00 | 7.00 | 10.00 |
| 11. Putting ideas into words | 51 | 7.63 | 2.92 | 8.00 | 7.00 | 10.00 |
| 12. Staying focused | 51 | 7.59 | 2.96 | 8.00 | 6.00 | 10.00 |
| 13. Following a story | 51 | 7.41 | 3.11 | 8.00 | 6.00 | 10.00 |
| 14. Reading | 51 | 7.47 | 3.04 | 8.00 | 6.00 | 10.00 |
| 15. Walking | 51 | 8.33 | 2.31 | 9.00 | 7.00 | 10.00 |
| 16. Housework | 51 | 7.47 | 2.84 | 8.00 | 5.00 | 10.00 |
| 17. Bathing | 51 | 7.39 | 3.03 | 8.00 | 6.00 | 10.00 |
| 18. Getting dressed | 51 | 7.35 | 3.06 | 8.00 | 5.00 | 10.00 |
BASIQ: Brain Symptom and Impact Questionnaire; SD: Standard deviation.
There were a few additional items identified by patients that should be included in the questionnaire mostly pertaining to emotional issues. However, no single item was mentioned by more than three patients (6%). No items were consistently rated as being inappropriate, upsetting or irrelevant.
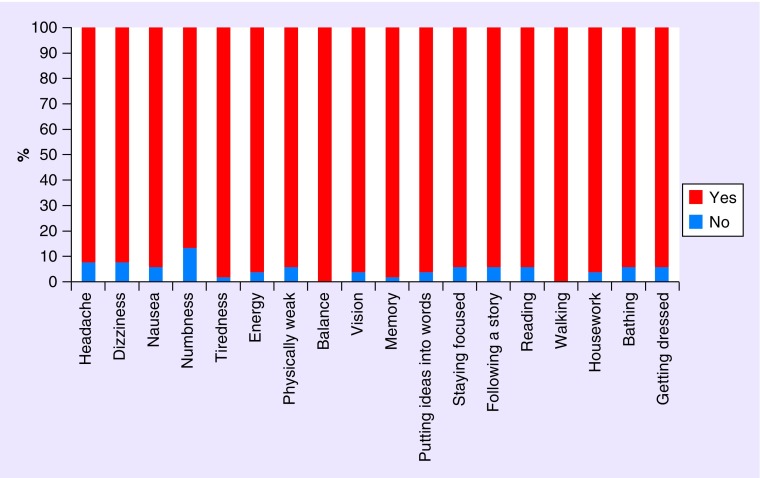
• HCPs' responses
All items were determined relevant by at least 95% of HCPs, except for the items of numbness (90%), staying focused (90%), and following a story (85%) (Figure 2). When rating the degree of relevancy, each item received at least 5/10 on average by HCPs. Top scoring items included headache (8.4), nausea (8.3) and walking (7.8). Less relevant items included the following a story (5.1), bathing (5.8) and getting dressed (6.0) (Table 4).
Figure 2. . Healthcare professionals' responses on whether each item was relevant (yes/no).
n = 20 healthcare professionals.
Table 4. . Degree of relevancy as rated by healthcare professionals.
| BASIQ item | n | Mean | SD | Median | Interquartiles | |
|---|---|---|---|---|---|---|
| 1. Headache | 20 | 8.40 | 1.67 | 9.00 | 8.00 | 10.00 |
| 2. Dizziness | 20 | 7.05 | 1.85 | 7.00 | 6.00 | 8.00 |
| 3. Nausea | 20 | 8.30 | 1.22 | 8.00 | 7.00 | 9.00 |
| 4. Numbness | 20 | 6.25 | 2.00 | 6.50 | 5.00 | 7.00 |
| 5. Tiredness | 20 | 6.95 | 1.73 | 7.00 | 6.00 | 8.00 |
| 6. Energy | 20 | 6.15 | 1.63 | 6.00 | 5.00 | 7.50 |
| 7. Physically weak | 20 | 6.30 | 1.81 | 7.00 | 5.00 | 7.00 |
| 8. Balance | 20 | 7.65 | 1.31 | 7.00 | 7.00 | 8.00 |
| 9. Vision | 20 | 7.35 | 1.76 | 7.00 | 7.00 | 8.00 |
| 10. Memory | 20 | 6.75 | 1.65 | 6.00 | 5.00 | 8.00 |
| 11. Putting ideas into words | 20 | 6.30 | 1.92 | 6.00 | 5.00 | 7.50 |
| 12. Staying focused | 20 | 6.10 | 1.74 | 6.00 | 5.00 | 7.50 |
| 13. Following a story | 20 | 5.10 | 1.80 | 5.00 | 4.00 | 7.00 |
| 14. Reading | 20 | 6.40 | 1.57 | 7.00 | 5.00 | 7.00 |
| 15. Walking | 20 | 7.80 | 1.32 | 8.00 | 7.00 | 9.00 |
| 16. Housework | 20 | 6.65 | 1.63 | 6.50 | 5.50 | 8.00 |
| 17. Bathing | 20 | 5.80 | 1.91 | 6.00 | 5.00 | 6.50 |
| 18. Getting dressed | 20 | 6.00 | 1.97 | 6.00 | 5.00 | 7.00 |
BASIQ: Brain Symptom and Impact Questionnaire; SD: Standard deviation.
HCPs did not consistently identify any items that should be included on the BASIQ that were not already. Two HCPs mentioned that an item about the side effects of dexamethasone and an item about the emotional difficulties may be relevant for inclusion; however, this was not a consistent finding among HCPs.
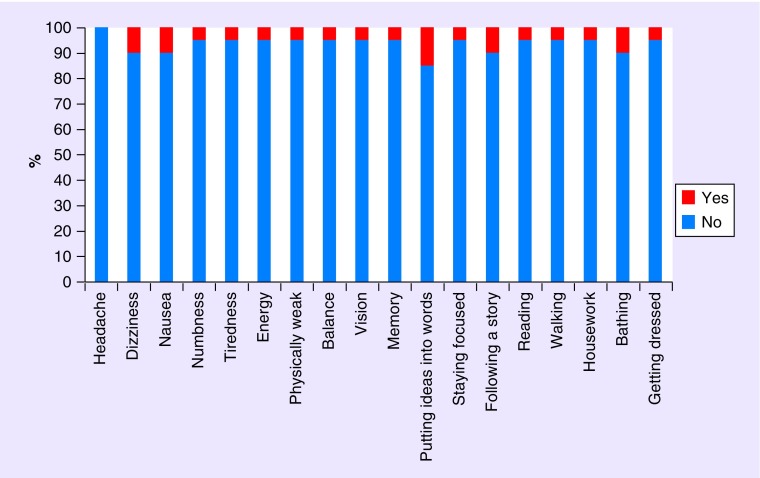
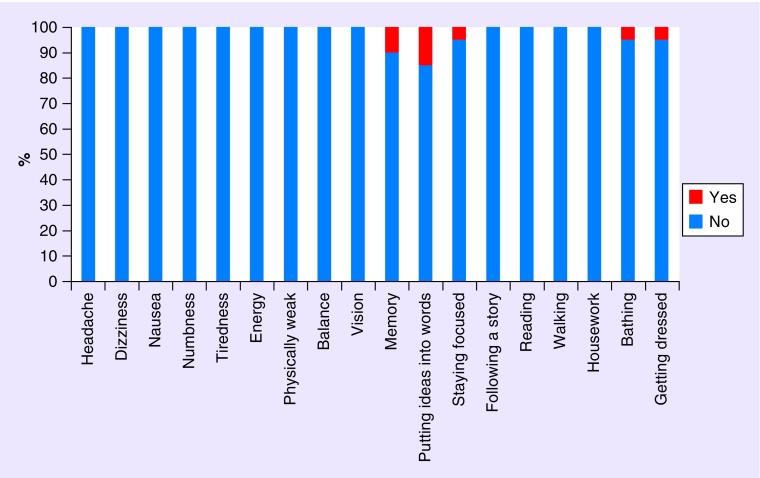
When asked if there were any items that were inappropriate or upsetting to patients no item was identified by more than 10% of HCPs, except for the item of putting ideas into words, which was determined to be inappropriate and upsetting by 15% of HCPs (Figures 3 & 4).
Figure 3. . Healthcare professionals' responses on whether each item was inappropriate to patients (yes/no).
n = 20 healthcare professionals.
Figure 4. . Healthcare professionals' responses on whether each item was upsetting to patients (yes/no).
n = 20 healthcare professionals.
• HCPs & patients combined
The mean percentage of relevance for each item as rated by patients and HCPs was averaged to obtain a combined percentage for each item. In this combined analysis, all items of the BASIQ were determined to be relevant by at least 88% of participants. All items were rated on average at least 6/10. The most relevant items included headache (8.1), walking (8.1) and balance (8.0) (Table 5).
Table 5. . Combined healthcare professionals and patient relevancy scores.
| BASIQ item | Patients responses | HCPs' responses | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean of relevance (0–10) | SD of relevance (0–10) | % of relevant | Mean of relevance (0–10) | SD of relevance (0–10) | % of relevant | Mean of relevance (0–10) | Pooled SD of relevance (0–10) | Average % of relevance | |
| 1. Headache | 7.7 | 3.3 | 92.3 | 8.4 | 1.7 | 100.0 | 8.1 | 2.9 | 96.2 |
| 2. Dizziness | 7.8 | 3.2 | 92.3 | 7.1 | 1.8 | 95.0 | 7.4 | 2.9 | 93.7 |
| 3. Nausea | 7.3 | 3.4 | 94.2 | 8.3 | 1.2 | 100.0 | 7.8 | 3.0 | 97.1 |
| 4. Numbness | 7.1 | 3.4 | 86.5 | 6.3 | 2.0 | 90.0 | 6.7 | 3.1 | 88.3 |
| 5. Tiredness | 8.1 | 2.3 | 98.1 | 7.0 | 1.7 | 95.0 | 7.5 | 2.2 | 96.5 |
| 6. Energy | 8.0 | 2.3 | 96.2 | 6.2 | 1.6 | 100.0 | 7.1 | 2.1 | 98.1 |
| 7. Physically weak | 7.9 | 2.7 | 94.2 | 6.3 | 1.8 | 95.0 | 7.1 | 2.5 | 94.6 |
| 8. Balance | 8.4 | 2.3 | 100.0 | 7.7 | 1.3 | 100.0 | 8.0 | 2.1 | 100.0 |
| 9. Vision | 8.1 | 2.8 | 96.2 | 7.4 | 1.8 | 95.0 | 7.7 | 2.6 | 95.6 |
| 10. Memory | 8.2 | 2.6 | 98.1 | 6.8 | 1.7 | 100.0 | 7.5 | 2.3 | 99.0 |
| 11. Putting ideas into words | 7.6 | 2.9 | 96.2 | 6.3 | 1.9 | 95.0 | 7.0 | 2.7 | 95.6 |
| 12. Staying focused | 7.6 | 3.0 | 94.2 | 6.1 | 1.7 | 90.0 | 6.8 | 2.7 | 92.1 |
| 13. Following a story | 7.4 | 3.1 | 94.2 | 5.1 | 1.8 | 85.0 | 6.3 | 2.8 | 89.6 |
| 14. Reading | 7.5 | 3.0 | 94.2 | 6.4 | 1.6 | 95.0 | 6.9 | 2.7 | 94.6 |
| 15. Walking | 8.3 | 2.3 | 100.0 | 7.8 | 1.3 | 100.0 | 8.1 | 2.1 | 100.0 |
| 16. Housework | 7.5 | 2.8 | 96.2 | 6.7 | 1.6 | 100.0 | 7.1 | 2.6 | 98.1 |
| 17. Bathing | 7.4 | 3.0 | 94.2 | 5.8 | 1.9 | 95.0 | 6.6 | 2.8 | 94.6 |
| 18. Getting dressed | 7.4 | 3.1 | 94.2% | 6.0 | 2.0 | 95.0 | 6.7 | 2.8 | 94.6 |
BASIQ: Brain Symptom and Impact Questionnaire; HCP: Healthcare professional; SD: Standard deviation.
Patient and HCP responses were compared in order to determine if any items were rated differently between the two groups. There were only three items that did not achieve statistically significant differences when comparing the two groups of respondents. The items of headache, nausea and ability to do house work were all rated similarly between HCPs and patients. All other items were rated statistically different between patients and HCPs, with HCPs often rating items as less relevant than patient (Table 6).
Table 6. . Comparison of healthcare professional and patient relevancy median scores or percentage of relevance†.
| BASIQ item | Median of relevance (0–10) | % of relevance | ||||
|---|---|---|---|---|---|---|
| Patients (n = 51) | HCPs (n = 20) | p-value from Wilcoxon Rank-sum test | Patients, % (n = 51) | HCPs, % (n = 20) | p-value from Fisher exact test | |
| 1. Headache | 10.00 | 9.00 | 0.6864 | 92.3 | 100.0 | 0.5704 |
| 2. Dizziness | 10.00 | 7.00 | 0.0128 | 92.3 | 95.0 | 0.6873 |
| 3. Nausea | 9.00 | 8.00 | 0.9947 | 94.2 | 100.0 | 0.5553 |
| 4. Numbness | 8.00 | 6.50 | 0.0451 | 86.5 | 90.0 | 0.6908 |
| 5. Tiredness | 9.00 | 7.00 | 0.0149 | 98.1 | 95.0 | 0.4812 |
| 6. Energy | 9.00 | 6.00 | 0.0014 | 96.2 | 100.0 | 0.3737 |
| 7. Physically weak | 9.00 | 7.00 | 0.0030 | 94.2 | 95.0 | 0.8984 |
| 8. Balance | 9.00 | 7.00 | 0.0196 | 100.0 | 100.0 | 0.9999 |
| 9. Vision | 10.00 | 7.00 | 0.0170 | 96.2 | 95.0 | 0.8263 |
| 10. Memory | 10.00 | 6.00 | 0.0004 | 98.1 | 100.0 | 0.5323 |
| 11. Putting ideas into words | 8.00 | 6.00 | 0.0034 | 96.2 | 95.0 | 0.8263 |
| 12. Staying focused | 8.00 | 6.00 | 0.0031 | 94.2 | 90.0 | 0.6130 |
| 13. Following a story | 8.00 | 5.00 | 0.0002 | 94.2 | 85.0 | 0.3381 |
| 14. Reading | 8.00 | 7.00 | 0.0096 | 94.2 | 95.0 | 0.8984 |
| 15. Walking | 9.00 | 8.00 | 0.0332 | 100.0 | 100.0 | 0.9999 |
| 16. Housework | 8.00 | 6.50 | 0.0659 | 96.2 | 100.0 | 0.3737 |
| 17. Bathing | 8.00 | 6.00 | 0.0044 | 94.2 | 95.0 | 0.8984 |
| 18. Getting dressed | 8.00 | 6.00 | 0.0144 | 94.2 | 95.0 | 0.8984 |
†Bolded items are statistically significant (p < 0.05).
BASIQ: Brain Symptom and Impact Questionnaire;HCP: Healthcare professional.
Discussion
This is the first study examining the content validity of the BASIQ version 1.0 in both patients and HCPs. Although there are a number of other QOL questionnaires such as the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire – Brain Neoplasm and FACT-Br, which are currently being used in this patient population, none of these questionnaires were originally developed for use in the brain metastases population. Moreover, they are long and can be very burdensome on patients [10]. Patients often become tired and do not want to complete lengthy assessments, thus attrition rates increase, especially in the palliative setting [13]. Brain metastases are characterized by substantial symptom burden that often have significant effect on patient functionality [14]. The BASIQ instrument addresses the limitations of the other PRO measures by focusing on measuring the severity of the most relevant symptoms associated with brain metastases and their impact on patients’ activities of daily living and QOL. By focusing on the severity of relevant symptoms and their impact, this gives clinicians a more comprehensive overview of the patient and the issues they are experiencing. In the clinical setting, the impact of symptoms as they are assessed by the patient, will allow clinicians to better focus and tailor treatment plans in order to effectively address these issues. Knowledge of the impact of symptoms could also lead clinicians to involve other HCPs in the patient’s treatment, such as social workers, psychologists, or support workers as the needs arise in accordance to the impacts the patient experiences due to their symptoms. Additionally, the impact of symptoms and treatment can be monitored over the course of the treatment in order to determine if the severity of impact is lessening, as is the goal of treatment. This lessening of impact may occur prior to the improving of the symptom itself, thus giving an earlier indication of whether or not treatment is effective. Therefore, it is of utmost important to monitor the impact of symptoms, as well as the symptoms themselves.
In addition to monitoring symptoms and impact, the BASIQ is brief with only 18 questions as compared with 50 questions of the FACT-Br [11], thus alleviating some of the burden felt by brain metastases patients when they are asked to complete QOL assessment.
In this content validation study, feedback from patients and HCPs were based on methods previously used in a number of studies to examine content validity of QOL instruments [15–17]. The patient feedback indicated that the questionnaire was overall well received in this patient population. There were no items that were consistently identified as upsetting, confusing, or difficult to answer. The majority of patients and HCPs felt that all items included were relevant to brain metastases patients.
Overall, the HCPs underrated items as relevant when compared with patients. A greater portion of HCPs than patients were in agreement that the items were relevant to those with brain metastases, however, the degree of relevancy assigned to each item on the 0–10 scale was less than the degree of relevancy assigned by patients for all items. Interestingly only three items were rated similarly between patients and HCPs. HCPs determined relevancy based upon the frequency of patient complaints and concerns. This is consistent with similar findings in other studies that found that cancer patients often have numerous concerns, but do not make their HCPs aware of all their concerns [18]. Perhaps these three items were not issues that patients made their HCPs aware of and thus, HCPs did not rate the degree of relevancy as highly as patients.
Our study only included patients with a relatively good performance status, and excluded those who were cognitively impaired, which may be a limitation. QOL and symptom severity are both very important end points in this palliative population [8], and at present there is no PRO questionnaire designed specifically for the brain metastases population. The BASIQ, unlike other questionnaires used for this population is brief and gives a thorough assessment of QOL in terms of symptom and impact on daily living. The study supports the content validity of the BASIQ version 1.0. Further data are needed to examine the psychometric properties of this scale.
Supplementary Material
Acknowledgements
The authors thank the sponsor of Abbvie and the survey participants.
Footnotes
Financial & competing interests disclosure
This study was supported by an educational grant from AbbVie. Saurabh Ray is an employee of AbbVie.The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Ethical conduct of research
The authors state that they have obtained appropriate institutional review board approval or have followed the principles outlined in the Declaration of Helsinki for all human or animal experimental investigations. In addition, for investigations involving human subjects, informed consent has been obtained from the participants involved.
References
- 1.Schouten LJ, Rutten J, Huveneers HA, et al. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94:2698–2705. doi: 10.1002/cncr.10541. [DOI] [PubMed] [Google Scholar]
- 2.Sperduto PW, Chao ST, Sneed PK, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int. J. Radiat. Oncol. Biol. Phys. 2010;77:655–661. doi: 10.1016/j.ijrobp.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 3.Eichler AF, Loeffler JS. Multidisciplinary management of brain metastases. Oncologist. 2007;12:884–898. doi: 10.1634/theoncologist.12-7-884. [DOI] [PubMed] [Google Scholar]
- 4.Tsao MN, Lloyd NS, Wong RK, et al. Radiotherapeutic management of brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2005;31:256–273. doi: 10.1016/j.ctrv.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Steeg PS, Camphausen KA, Smith QR. Brain metastases as preventive and therapeutic targets. Nat. Rev. Cancer. 2011;11:352–363. doi: 10.1038/nrc3053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klos KJ, O'Neill BP. Brain metastases. Neurologist. 2004;10:31–46. doi: 10.1097/01.nrl.0000106922.83090.71. [DOI] [PubMed] [Google Scholar]
- 7.Khuntia D, Brown P, Li J, et al. Whole-brain radiotherapy in the management of brain metastasis. J. Clin. Oncol. 2006;24:1295–1304. doi: 10.1200/JCO.2005.04.6185. [DOI] [PubMed] [Google Scholar]
- 8.Wong J, Hird A, Kirou-Mauro A, et al. Quality of life in brain metastases radiation trials: a literature review. Curr. Oncol. 2008;15:25–45. [PMC free article] [PubMed] [Google Scholar]
- 9.Bezjak A, Adam J, Panzarella T, et al. Radiotherapy for brain metastases: defining palliative response. Radiother. Oncol. 2001;61:71–76. doi: 10.1016/s0167-8140(01)00426-1. [DOI] [PubMed] [Google Scholar]
- 10.Caissie A, Nguyen J, Chen E, et al. Quality of life in patients with brain metastases using the EORTC QLQ-BN20+2 and QLQ-C15-PAL. Int. J. Radiat. Oncol. Biol. Phys. 2012;83:1238–1245. doi: 10.1016/j.ijrobp.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 11.Lien K, Zeng L, Nguyen J, et al. FACT-br for assessment of quality of life in patients receiving treatment for brain metastases: a literature review. Expert Rev. Pharmacoecon. Outcomes Res. 2011;11:701–708. doi: 10.1586/erp.11.67. [DOI] [PubMed] [Google Scholar]
- 12.Groenvold M, Petersen MA, Aaronson NK, et al. The development of the EORTC QLQ-C15-PAL: a shortened questionnaire for cancer patients in palliative care. Eur. J. Cancer. 2006;42:55–64. doi: 10.1016/j.ejca.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Chow E, Davis L, Holden L, et al. Prospective assessment of patient-rated symptoms following whole brain radiotherapy for brain metastases. J. Pain Symptom Manage. 2005;30:18–23. doi: 10.1016/j.jpainsymman.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Tsao MN, Lloyd N, Wong RK, et al. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst. Rev. 2012;4:CD003869. doi: 10.1002/14651858.CD003869.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen E, Cella D, Zeng L, et al. Content validation of the FACT-br with patients and health-care professionals to assess quality of life in patients with brain metastases. J. Radiat. Oncol. 2014;3:105–113 . [Google Scholar]
- 16.Nguyen J, Zhang L, Clemons M, et al. Content validation of the EORTC QLQ-BN20+2 with patients and health care professionals to assess quality of life in brain metastases. J. Radiat. Oncol. 2012;1(4):397–409. [Google Scholar]
- 17.Chow E, Hird A, Velikova G, et al. The European Organisation for Research and Treatment of Cancer Quality of Life questionnaire for patients with bone metastases: the EORTC QLQ-BM22. Eur. J. Cancer. 2009;45:1146–1152. doi: 10.1016/j.ejca.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Maguire P. Improving communication with cancer patients. Eur. J. Cancer. 1999;35:2058–2065. doi: 10.1016/s0959-8049(99)00301-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.