Abstract
Objective
Compulsivity refers to a tendency towards repetitive habitual behaviors. Multiple disorders have compulsive symptoms at their core, including substance use disorders, gambling disorder, and obsessive-compulsive disorder. The aim of this study was to validate a scale for the objective, trans-diagnostic measurement of compulsivity.
Methods
The fifteen-item Cambridge-Chicago Compulsivity Trait Scale (CHI-T) was developed for the rapid but comprehensive measurement of compulsivity. Adults aged 18-29y were recruited using media advertisements, and completed the CHI-T in addition to demographic, clinical, and cognitive assessment. The validity and psychometric properties of the scale were quantified.
Results
112 participants completed the study. The scale yielded a normal distribution with very few outliers. It had excellent psychometric properties, with high internal consistency (Cronbach’s alpha = 0.8), and excellent convergent validity against gold-standard assessments of compulsive symptoms (each p<0.001 for gambling disorder, obsessive-compulsive, and substance use disorder symptoms). Total scores on the scale correlated significantly with less risk-adjustment on the decision-making task (rigid response style) and divergent validity was confirmed against other cognitive domains (response inhibition and executive planning). The above significant findings withstood Bonferroni correction. Factor analysis suggested the existence of two latent factors: one related mainly to reward-seeking and the need for perfection; and the other relating to anxiolytic/soothing features of compulsivity.
Conclusion
The CHI-T, a scale designed to measure trans-diagnostic compulsivity, appears to show excellent psychometric properties in a normative population and merits further investigation in the context of clinical patient populations, including in treatment trials.
Introduction
It is increasingly recognized that trans-diagnostic measures of psychopathology may play an important role in the future diagnosis, classification, and treatment of mental disorders. Per the NIMH Research Domain Criteria (RDoC) strategic plan, trans-diagnostic markers would ideally be measurable in a continuous or dimensional fashion, evident to a milder degree in normative populations, extending through to higher levels in mental disorders1,2. The concept of compulsivity is extremely relevant to understanding and treating a variety of mental disorders. Compulsivity has been defined as a tendency towards repetitive, habitual actions, repeated despite adverse consequences3. Additionally, compulsivity relates to the sense of being ‘compelled’ to undertake an act, or getting ‘stuck’ until a situation or act is ‘just right’4.
Compulsivity is central to obsessive-compulsive disorder (OCD; intrusive thoughts and/or repetitive rituals), and substance related and addictive disorders (including gambling disorder)5. Despite the high clinical and research importance of this concept, to the authors’ knowledge there exist no transdiagnostic compulsivity scales designed to measure compulsivity irrespective of particular compulsive symptom category (literature search including PubMed using terms “compulsivity or compulsive scale” dated 13th November 2017). The available scales pertaining to compulsivity were not designed to capture trans-diagnostic compulsivity per se, but rather to quantity presence and/or severity of restricted categories of symptoms for one (or more) mental disorder(s). For example, many scales have been developed for assessing obsessive-compulsive symptoms6, including those designed for normative and clinical settings such as the Padua inventory7. Similarly, instruments exist for other compulsive symptoms related to specific categorical disorders, such the Structured Clinical Interview for Gambling Disorder (SCI-GD)8. Therefore, the aim of the current study was to develop a new trans-diagnostic scale for compulsivity, irrespective of particular diagnostic category, and to validate this scale in a normative setting.
Methods
Participants
A normative sample of participants, aged 18-29 years, was recruited using media advertisements in a large US city. Adverts asked subjects to participate in a research study exploring impulsive and compulsive behaviors. Subjects were excluded if they were unable to give informed consent, were unable to understand/undertake the study procedures, or were seeking treatment for any mental disorders. All study procedures were carried out in accordance with the Declaration of Helsinki. The Institutional Review Boards of the Universities of Minnesota and Chicago approved the study and the consent statement. Participants were compensated with a $50 gift card for a local department store for taking part.
Clinical assessments
The Cambridge-Chicago Compulsivity Trait Scale (CHI-T) was developed with a view to measuring transdiagnostic aspects of compulsivity in a convenient and short format. The scale items were selected based on a review of the existing literature and discussion between the current study authors and professional colleagues, as well as on consensus between the authors. The final self-report scale contained fifteen items, with an additional specifier for functional impairment. The scale covered broad aspects of compulsivity including the need for completion or perfection, being stuck in a habit, reward-seeking, desire for high standards, and avoidance of situations that are hard to control. For each item, participants selected whether the statement applied to them by selecting “strongly disagree”, “disagree”, “agree”, or “strongly agree”. These responses were scored 0, 1, 2, or 3 respectively. Total score on the instrument ranges from 0 – 45.
Participant assessments were conducted in a quiet testing room with a trained rater, and included a clinical interview, completion of questionnaires (including the CHI-T), and a neuropsychological assessment using a touch-screen computer. Relevant demographic information was documented including age, gender, and education level. Presence of a substance use disorder was evaluated using specific modules from the Mini International Neuropsychiatric Inventory (MINI)9. Gambling disorder symptoms were measured using the Structured Clinical Inventory for Gambling Disorder (SCI-GD) (modified for DSM-5)8, and levels of obsessive-compulsive symptoms were measured using the self-completed Padua inventory7.
Cognitive testing comprised three previously validated tests from the Cambridge Neuropsychological Test Automated Battery (CANTABeclipse, version 3, Cambridge Cognition Ltd, UK): the Cambridge Gamble task10, Stop-Signal task11, and Stockings of Cambridge task12. Based on previous literature we expected Gamble task performance to be associated with compulsivity, because impairment on this task occurs even in people at risk of gambling disorder13, and reward-related decision making deficits are prominent in gamblers14,15. Furthermore, symptoms of compulsive disorders such as gambling and substance use are themselves suggestive of decision-making problems. We included the Stop-signal and Stockings of Cambridge tasks to confirm the divergent validity of CHI-T relationship with cognition: we predicted that relationships between CHI-T scores and performance on these tasks would be weak or non-significant, as compared to decision-making performance.
On the Cambridge Gamble task, for each trial, ten boxes were shown, some blue and some red, with a token having been hidden behind one of these. The participant selected the color of box they believed a token was hidden behind, and then decided how many points to gamble on having made the correct decision. The main measures of decision-making on the task were the proportion of points gambled overall, the proportion of rational decisions made (proportion of trials when the volunteer opted for the color that was in the majority), and the extent of risk adjustment (the extent to which individuals modulated the amount gambled depending on the probability of making correct choices).
On the Stop-signal task, participants viewed a series of directional errors appearing one-per-time on the screen, and made speeded motor responses – if a left arrow occurred, they pressed a left button, and vice versa for right facing arrows. When an auditory stop-signal (“beep”) occurred, participants attempted to withhold their motor response for the given trial. The main outcome measure on the task is the stop-signal reaction time, which is an estimate of how long it takes a given individual to suppress an already triggered response.
On the Stockings of Cambridge task, participants attempted to work out the minimum number of moves it would take to move a set of snooker balls in pockets, to match a goal arrangement shown by the computer. To successfully complete trials on this task, participants have to hold “in mind” the moves they have made and sequence their planned course of actions efficiently. The key outcome measure on the task is the number of problems solved correctly on the first attempt.
Data analysis
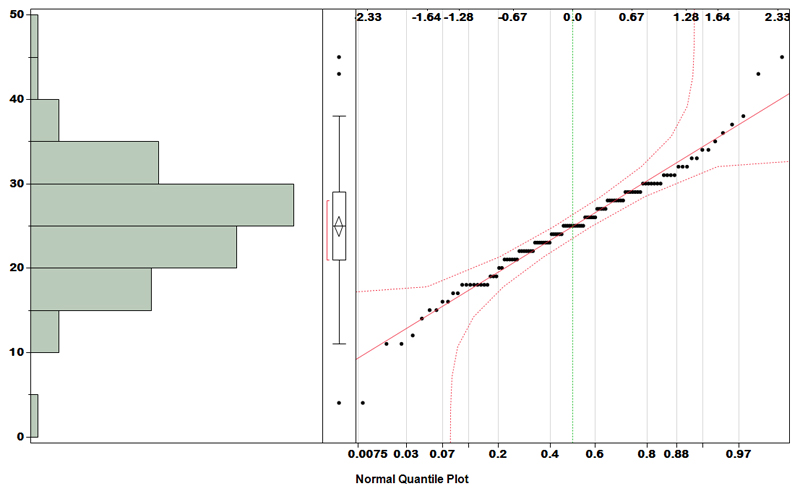
The distributions of CHI-T total scores are characterized graphically in terms of any skew and outliers (see Figure 1). Concurrent validity of the CHI-T was confirmed using correlation analysis (spearman’s rho) against compulsive symptoms, namely scores for gambling (SCI-GD scores) and obsessive-compulsive symptoms (Padua scores). Furthermore, CHI-T total scores were compared between subjects with versus without a current substance use disorder. The functional relevance of the CHI-T was evaluated by comparing total scores between those who did and did not endorse significant functional impairment based on a binary response. Additionally, correlations were computed between CHI-T total scores and cognitive measures, to confirm the specificity of the scale for decision-making as opposed to response inhibition impairment and more generalized executive dysfunction. Lastly, we conducted exploratory factor analysis, with a view to characterizing possible subtypes of compulsive measures within the dataset. The number of variables was selected using the Kaiser criterion16 and factor loadings were explored using the maximum likelihood quartimin method. We regarded the factor analysis as being a secondary analysis and of a preliminary nature, due to the relatively large ratio of scale items to the sample size.
Figure 1.
Distribution plot for CHI-T total scores. Left: histogram; middle: box-plot; right: normal quantile plot. Data were normally distributed with three outliers.
All analyses were conducted using JMP Pro software version 13.2. Statistical significance was defined as p<0.05 uncorrected, two-tailed, though we also indicated in the text when findings would have withstood Bonferroni correction for the number of multiple comparisons.
Results
The sample comprised n=112 adults, mean age (standard deviation) 23.3 (3.6) years, of whom 63 (56.3%) were male (Table 1). The mean scores on gambling disorder and Padua obsessive-compulsive symptoms were as expected for a normative population 17,18, as was the proportion of participants with a substance use disorder 19.
Table 1.
Demographic and clinical characteristics of the sample.
| Variable | Mean (SD) |
|---|---|
| Age, years | 23.3 (3.6) |
| Gender, N [%] male | 63 [56.3%] |
| Education level | 3.8 (0.8) |
| Presence of substance use disorder, yes, N [%] | 12 [11.0%] |
| Padua obsessive-compulsive symptoms (total score) | 11.3 (13.8) |
| Gambling Disorder symptoms (SCI-GD total score) | 0.9 (1.8) |
Primary Analysis
The distribution of total scores on the CHI-T instrument are displayed in Figure 1, where it can be seen that data were normally distributed with minimal skew and only three outliers. Data for the three outliers were excluded from subsequent analyses due to use of parametric statistical tests. The CHI-T demonstrated excellent internal validity (Cronbach’s alpha = 0.80), with all individual scale items exhibiting strong loading onto other items (all alpha > 0.78). Those endorsing marked functional impairment had significantly higher CHI-T total scores (mean [SD] total SCI-T score: 30.4 [4.7] versus 23.9 [5.3]; F(1,105) = 17.3, p < 0.001). Internal validity was also excellent when participants with gambling disorder or substance use disorder were excluded (Cronbach’s alpha = 0.85).
The CHI-T had good convergent validity, with total scores correlating significantly with gambling disorder symptoms (SCI-PG total scores; Spearman’s rho = 0.42, p < 0.001), and with obsessive-compulsive symptoms (Padua total scores; rho = 0.33, p<0.001). CHI-T total scores were also significantly elevated in participants who had a current substance use disorder versus those who did not (mean [SD] total score 30.0 [2.8] versus 24.1 [5.5]; F(1,107) = 13.2, p < 0.001).
Total scores on the CHI-T correlated significantly with less risk adjustment on the Cambridge Gamble Task (rho = 0.26, p = 0.006), but not significantly with quality of decision-making (rho = -0.18, p = 0.067). The correlation between total CHI-T scores and overall proportion bet on the CGT was marginally significant, but would not have withstood statistical correction (rho = 0.21, p = 0.03).
Total CHI-T scores did not correlate significantly with impulsivity on the Stop-signal task (rho = 0.02, p = 0.85), nor with executive planning on the Stockings of Cambridge Task (rho = -0.12, p = 0.22).
All statistically significant results reported above remained significant with Bonferroni correction for the number of statistical tests undertaken, except for proportion of points bet on the Cambridge Gamble test.
At the request of a peer reviewer we also conducted the above analyses without excluding the three individuals with extreme CHI-T total scores. The profile of significant results was unchanged, including the convergent validity, and cognitive findings.
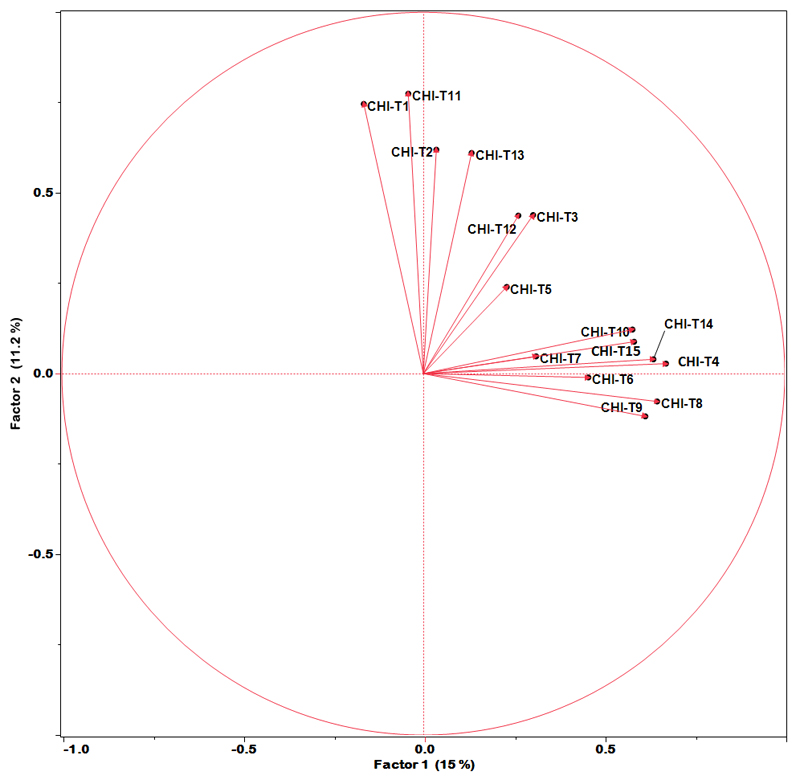
Secondary analysis
Factor analysis yielded an optimal two-factor solution, with eigenvalues of 2.87 and of 1.08 (both p < 0.001 by Chi-square). The cumulative percentage of covariance accounted for was 46%. Results of rotated factor analysis in terms of loadings are shown in Figure 2. Factor 1 was related to getting stuck, addictive personality, failure to resist urges, doing things immediately rewarding even though detrimental, perfectionism, avoiding situations one cannot predict/control, and needing to be the best with new hobbies. Factor 2 was related to hating to leave tasks unfinished, being comfortable when things are done ‘just right’, repetition of tasks until they are done to the highest standards, having high standards in general, parents teaching there is always scope for improvement, and feeling soothed when things are made complete/finished.
Figure 2.
Loading of scale items onto two latent factors from rotation analysis. Factor 1 related to general aspects of compulsivity especially reward-seeking and failure to resist. Factor 2 related to aspects of compulsivity germane to anxiety reduction and self-soothing.
Discussion
Compulsivity, or the tendency towards repetitive habitual actions that an individual feels driven to perform, is evident across a range of mental health disorders including gambling disorder, substance use disorder, and OCD. While rating scales exist for compulsive symptoms within a given disorder, there is a paucity of trans-diagnostic rating scales of the broader construct of compulsivity. Here we developed and piloted a new scale, the Cambridge-Chicago Compulsivity Trait Scale (CHI-T), in a normative sample of adult participants recruited from the general community.
The scale was quick for participants to complete – typically taking less than 3 minutes – and yet the items covered a broad range of compulsive tendencies. Total scores of the CHI-T were normally distributed and had few outliers, and we found good concordance for the scale against three types of compulsive symptoms: disordered gambling, obsessive-compulsive, and maladaptive substance use. These three types of compulsive symptomatology were evaluated using gold-standard instruments6–9. Elevated scores on the scale were associated with functional impairment, as expected. In all, these findings, along with excellent internal validity, support the use of this scale in academic and clinical settings.
From a neuropsychological perspective, the hypothesis that CHI-T scores would be related to decision-making impairment was partially confirmed. In particular, total scores on the CHI-T correlated strongly with inflexible responding on the Cambridge Gamble task. This may suggest that difficulty modulating or adapting decisions bears a particularly strong relationship with compulsivity. There was evidence that CHI-T total scores correlated weakly with the two other Gamble task measures (quality of decision-making and proportion of points gambled) in the expected direction, but these findings were not significant with Bonferroni correction. This may reflect compulsivity being particularly strongly related to a rigid or inflexible response profile even as the likelihood of reward changes. Whereas compulsivity appears less related to making irrational color choices on the task, which can be seen as being more impulsive in nature; and less related to the overall proportion of points gambled, which may reflect more of a risk-taking aspect of decision-making.
No significant correlations were found between CHI-T total scores and the other cognitive measures, including response inhibition and executive planning, highlighting the divergent validity of the scale from a cognitive perspective.
In a preliminary factor analysis, there was evidence to support the existence of two latent factors. We regard this factor analysis as preliminary in view of the relatively large ratio of number of scale items to the sample size. The dominant factor related to various aspects of compulsivity but especially reward-seeking and failure to resist urges; whereas the second factor related more to anxiolytic or ‘soothing’ aspects of compulsivity such as being comfortable when things are done ‘just right’, and completion leading to a sense of calm or soothing.
Several limitations should be considered in relation to this study. This initial pilot work focused on a normative, community-dwelling sample. This was important because trans-diagnostic markers need to be measurable not just in mental disorders, but also in a dimensional or continuous fashion in the background population2,20. Nonetheless, the validity of the scale for categorical disorders of compulsivity merits scrutiny in future work, including in the context of treatment trials. Because there are no prior accepted trans-diagnostic scales for compulsivity, the development of the CHI-T items by necessity relied on professional opinion rather than screening and selection of items from other scales. However, the scale items were designed to encompass a broad range of aspects germane to compulsivity, and strong correlations were found across the scale items, indicating that they reflect this common construct of compulsivity. Future work should recruit larger samples so that more definitive factor analysis can be conducted. We did not evaluate the scale across all cognitive domains that may be relevant for compulsivity – for example, we did not quantify habit learning21. While our scale was designed to measure compulsivity, some items may also reflect impulsivity (e.g. having an ‘addictive’ personality, doing immediately rewarding acts, or acting on urges). Indeed, we believe rewarding elements of habits are central to the concept of compulsivity, as suggested by the preliminary factor analysis reported herein. Overlap is inevitable because these two constructs are positively correlated even at the conceptual (latent factor) level20. Nonetheless, all items showed high concordance by Cronbach’s alpha; and the three items above correlated significantly with compulsive symptomatology (Padua inventory and/or number of disordered gambling criteria endorsed). Future work could examine the items on the scale that best differentiate compulsivity from impulsivity. There were too few participants with mood or anxiety disorders to assess the discriminant validity of CHI-T against these disorders, nor did we include scales of these symptoms. Here it should be noted that compulsive symptoms can lead to depression and anxiety, so one would not necessarily expect these symptoms to be unrelated to compulsivity. Finally, it would be valuable in future work to measure the CHI-T in the context of other psychiatric symptom domains not considered here including impulse control disorders (hair pulling disorder, compulsive stealing), disorders listed by DSM-5 as being in need of further study notably internet use disorder / internet gaming disorder22, and personality disorders (notably obsessive-compulsive personality disorder).
Conclusion
In summary, the CHI-T is a convenient fifteen-item scale designed to capture broad day-to-day aspects of compulsivity without focusing on highly specific symptom domains. Future work should evaluate the utility of this scale as a screening and severity tool for compulsive disorders, and its ability to measure change over time (such as during treatment of compulsive symptoms).
Acknowledgements and Disclosures
Dr. Grant has received research grants from NIDA, National Center for Responsible Gaming, American Foundation for Suicide Prevention, and Forest and Roche Pharmaceuticals Dr. Grant receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, Johns Hopkins University Press, and McGraw Hill. Dr. Chamberlain consults for Cambridge Cognition. Dr. Chamberlain’s research was funded by a Clinical Fellowship from the Wellcome Trust (reference 110049/Z/15/Z).
Footnotes
Previous presentations: none.
References
- 1.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC medicine. 2013;11:126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 3.Dalley JW, Everitt BJ, Robbins TW. Impulsivity, compulsivity, and top-down cognitive control. Neuron. 2011;69(4):680–694. doi: 10.1016/j.neuron.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 4.Sica C, Bottesi G, Orsucci A, Pieraccioli C, Sighinolfi C, Ghisi M. “Not Just Right Experiences” are specific to obsessive-compulsive disorder: further evidence from Italian clinical samples. J Anxiety Disord. 2015;31:73–83. doi: 10.1016/j.janxdis.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Association AP. Diagnostic and statistical manual of mental disorders (5th ed.) (DSM-5) Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 6.Rapp AM, Bergman RL, Piacentini J, McGuire JF. Evidence-Based Assessment of Obsessive-Compulsive Disorder. J Cent Nerv Syst Dis. 2016;8:13–29. doi: 10.4137/JCNSD.S38359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanavio E. Obsessions and compulsions: the Padua Inventory. Behav Res Ther. 1988;26(2):169–177. doi: 10.1016/0005-7967(88)90116-7. [DOI] [PubMed] [Google Scholar]
- 8.Grant JE, Steinberg MA, Kim SW, Rounsaville BJ, Potenza MN. Preliminary validity and reliability testing of a structured clinical interview for pathological gambling. Psychiatry Res. 2004;128(1):79–88. doi: 10.1016/j.psychres.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- 10.Rogers RD, Everitt BJ, Baldacchino A, et al. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: evidence for monoaminergic mechanisms. Neuropsychopharmacology. 1999;20(4):322–339. doi: 10.1016/S0893-133X(98)00091-8. [DOI] [PubMed] [Google Scholar]
- 11.Aron AR, Durston S, Eagle DM, Logan GD, Stinear CM, Stuphorn V. Converging evidence for a fronto-basal-ganglia network for inhibitory control of action and cognition. J Neurosci. 2007;27(44):11860–11864. doi: 10.1523/JNEUROSCI.3644-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owen AM, Downes JJ, Sahakian BJ, Polkey CE, Robbins TW. Planning and spatial working memory following frontal lobe lesions in man. Neuropsychologia. 1990;28(10):1021–1034. doi: 10.1016/0028-3932(90)90137-d. [DOI] [PubMed] [Google Scholar]
- 13.Grant JE, Chamberlain SR, Schreiber LR, Odlaug BL, Kim SW. Selective decision-making deficits in at-risk gamblers. Psychiatry Res. 2011;189(1):115–120. doi: 10.1016/j.psychres.2011.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goudriaan AE, Oosterlaan J, de Beurs E, van den Brink W. Decision making in pathological gambling: a comparison between pathological gamblers, alcohol dependents, persons with Tourette syndrome, and normal controls. Brain research Cognitive brain research. 2005;23(1):137–151. doi: 10.1016/j.cogbrainres.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Goudriaan AE, Oosterlaan J, de Beurs E, van den Brink W. Psychophysiological determinants and concomitants of deficient decision making in pathological gamblers. Drug Alcohol Depend. 2006;84(3):231–239. doi: 10.1016/j.drugalcdep.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Kaiser HF. The application of electronic computers to factor analysis. Educationa and Psychological Measurement. 1960;XX(1):141–150. [Google Scholar]
- 17.Spinella M. Normative data and a short form of the Barratt Impulsiveness Scale. The International journal of neuroscience. 2007;117(3):359–368. doi: 10.1080/00207450600588881. [DOI] [PubMed] [Google Scholar]
- 18.Burns GL, Keortge SG, Formea GM, Sternberger LG. Revision of the Padua Inventory of obsessive compulsive disorder symptoms: distinctions between worry, obsessions, and compulsions. Behav Res Ther. 1996;34(2):163–173. doi: 10.1016/0005-7967(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 19.Merikangas KR, McClair VL. Epidemiology of Substance Use Disorders. Hum Genetic. 2012;131(6):779–789. doi: 10.1007/s00439-012-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chamberlain SR, Stochl J, Redden SA, Grant JE. Latent traits of impulsivity and compulsivity: toward dimensional psychiatry. Psychol Med. 2017:1–12. doi: 10.1017/S0033291717002185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8(11):1481–1489. doi: 10.1038/nn1579. [DOI] [PubMed] [Google Scholar]
- 22.Weinstein A, Livny A, Weizman A. New developments in brain research of internet and gaming disorder. Neurosci Biobehav Rev. 2017;75:314–330. doi: 10.1016/j.neubiorev.2017.01.040. [DOI] [PubMed] [Google Scholar]