ABSTRACT
A fall may cause trauma and bone fracture, which can affect ADL and QOL. Therefore, countermeasures to prevent falls are important. There are many reports on falls in hospitalized patients, but few for outpatients. Therefore, the purpose of this study is to report the characteristics of outpatient falls that occurred in hospital over five years to identify factors associated with fall in these patients. From April 2012 to March 2017, we investigated fall cases in outpatients using a hospital database. Fall that led to fracture or a life-threatening injury was defined as an adverse event. A total of 3,758 patients had falls in the hospital, and this included 146 outpatients, giving an incidence of 3.9% (146/3,758). Most falls involved outpatients in their 70s, and most occurred in operating rooms (15%), followed by examination rooms (13%), escalators (10%), and waiting rooms (7%). Falls in neurology patients accounted for 12%, followed by neurosurgery (10%), and ophthalmology (8%). Among all falls, 5% occurred in patients wearing slippers, and 54% and 46% occurred in patients without and with a need for assistance with mobility, respectively. There were 6 adverse events (4%) due to fall in outpatients: 4 femoral neck fractures, 1 teeth injury, and 1 pubic bone fracture. In conclusion, a fall accident occurs most commonly in outpatients suffering from a neurological disease and in ophthalmologic outpatients aged about 70 years old, and is likely to occur in the operating room, examination room, escalator and waiting room. Our findings suggest that countermeasures for each location are necessary.
Key Words: elderly patients, fall, outpatient, prevention, risk management
INTRODUCTION
A fall in a hospital may cause trauma and bone fracture, which can greatly affect ADL and QOL,1) and may lead to lawsuits and additional medical costs.2-4) For these reasons, medical institutions are taking initiatives to reduce fall. We have established a fall-prevention working group composed of 10 members, including doctors, nurses, and physiotherapists. The mission of the working group is to improve medical quality and safety management through prevention of falls, which includes accurate identification and analysis of fall cases, and the development of education and training programs for hospital staff. These approaches are important for prevention of falls, but mostly concern hospitalized patients; in contrast, there are few reports on fall in outpatients.
Our hospital is a university hospital with 1035 beds, and we have an average of 3000 outpatients daily. We have previously examined the effectiveness of a fall assessment scoresheet and we have evaluated adverse events caused by fall.5-9) The incidence of falls in inpatients over 4 years was 1.89%, the incidence of adverse events was 0.22%, most falls involved patients in their 70s, and the time of occurrence was most commonly 4:00–6:59 AM.8,9,12) In this study, we report the characteristics of outpatient falls in our hospital over five years, with the purpose of identifying factors associated with fall in these patients.
MATERIALS AND METHODS
From April 2012 to March 2017, we investigated incidents of outpatient falls prospectively using a database in our hospital event reporting system. Age, sex, location, adverse events, primary clinical department, footwear, mobility, and cause of falls were examined for outpatients. In our institution, a clinical error or event is submitted as an incident or event report, regardless of whether it results in harm to a patient. All reports are submitted to the medical safety management office for analysis. We used these data to examine cases of fall in outpatients. A fall was defined as an involuntary change of posture whereby a patient ended up lying on the floor. An adverse event due to a fall was defined as any fracture or life-threatening injury. A case requiring suturing of a wound was excluded if not accompanied by fracture. All patients with a fall were followed up. The protocol of this study was approved by the Ethics Committee of our institution (IRB No. 354-3).
RESULTS
Details of all falls in outpatient falls that occurred in hospital for 5 years are shown in Table 1. A total of 3,758 patients had falls in the hospital, and falls occurred in 146 outpatients (64 males, 82 females), giving an incidence of fall of 3.9% (146/3,758). There were 2.7 million outpatients in 5 years, and thus the fall rate in outpatients was 0.054%. Most falls involved patients in their 70s (Figure 1) and most occurred in operating rooms (15%), followed by examination rooms (13%), escalators (10%), and waiting rooms (7%). Falls in neurology patients accounted for 12%, followed by neurosurgery (10%), ophthalmology (8%), emergency (7%), pediatrics (5%), and orthopedics (5%). Among all falls, 5% involved outpatients wearing slippers. Outpatients without and with a need for assistance with mobility accounted for 54% and 46% of falls, respectively (Table 2). There were 6 adverse events (4%) due to fall in outpatients: 4 femoral neck fractures, 1 teeth injury, and 1 pubic bone fracture.
Table 1.
Demographics and characteristics of cases of outpatient falls that occurred in hospital (n=146)
| Variable | Cases |
|---|---|
| Percentage of outpatients in all falls | 3.9% (146/3,758) |
| Demographics | |
| Age | 58.6 (8–93) |
| Sex (M/F) | 64/82 |
| Location | |
| Operating room | 15% (22) |
| Examination room | 13% (19) |
| Escalator | 10% (14) |
| Waiting room | 10% (14) |
| Consultation room | 7% (10) |
| Entrance | 6% (9) |
| Hall way | 6% (9) |
| Reception | 5% (8) |
| Emergency room | 5% (7) |
| Parking place | 5% (7) |
| X-ray room | 4% (6) |
| Rehabilitation ward | 3% (5) |
| Bathroom | 2% (3) |
| Others | 9% (13) |
| Adverse events | |
| Total | 4% (6) |
| Femoral neck fracture | 3% (4) |
| Pubic bone fracture | 1% (1) |
| Skull base fracture with teeth injury | 1% (1) |
Fig.1.
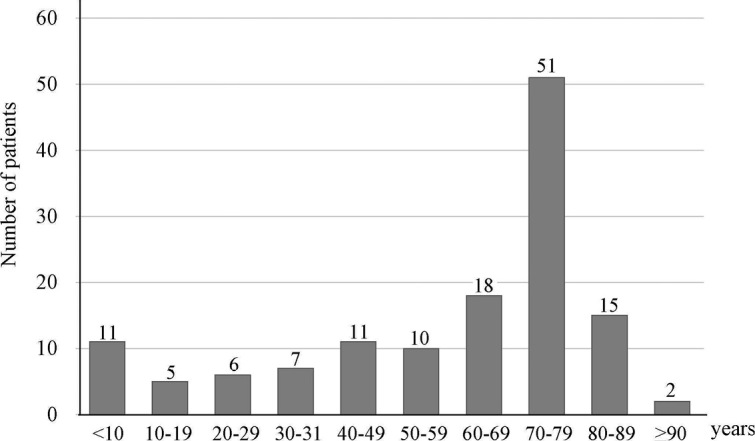
Distribution of patients by age category.
Table 2.
Details of cases of outpatient falls that occurred in hospital (n=146)
| Variable | Cases |
|---|---|
| Primary clinical department | |
| Neurology | 12% (18) |
| Neurosurgery | 10% (14) |
| Ophthalmology | 8% (11) |
| Emergency | 7% (10) |
| Pediatrics | 5% (8) |
| Orthopedics | 5% (8) |
| Gastroenterological | 4% (6) |
| Dental surgery | 3% (5) |
| Cardiology | 3% (5) |
| Dermatology | 3% (5) |
| Geriatrics | 3% (5) |
| Gynecology | 3% (4) |
| Psychiatry | 3% (4) |
| Endocrinology | 3% (4) |
| Others | 27% (39) |
| Footwear | |
| Shoes | 75% (109) |
| Slippers | 5% (8) |
| Others | 20% (29) |
| Mobility | |
| No need for assistance | 54% (79) |
| Wheelchair | 19% (28) |
| Cane | 16% (23) |
| Walker | 11% (16) |
Characteristics including location of and countermeasures against outpatient falls that occurred in hospital are shown in Table 3. Falls occurred in operating rooms or examination rooms due to taking off shoes and lying down, on escalators due to fast movements, in waiting rooms due to the arrangement of chairs, at entrances because of slippery mats, in parking places due to their distance from hospital wards and because of stairs (Table 3).
Table 3.
Environmental factors of outpatient falls that occurred in hospital.
| Location | Typical cause |
|---|---|
| Operating room / Examination room | Taking off shoes and lying down |
| Escalator | Fast movement |
| Waiting room | Arrangement of chairs |
| Entrance | Material of mat was slippery |
| Parking place | Far from hospital ward and there are stairs |
DISCUSSION
In hospital, falls are common adverse events accounting for 20–30% of all incident reports.7) Falls are a common health problem in elderly people, and in the adult population the incidence of fall increases with aging.10,11) Elderly people are likely to fall due to a decrease in balance, body weakening and cardiovascular factors associated with aging, skeletal muscle factors, and neurological factors.5,6) Injuries occur in approximately half of falls and 10% lead to adverse injuries such as fracture and head or joint injuries.2) Thus, there is a need to prevent fall in older people.
In our previous reports of falls in hospitalized patients, incidents of fall were obtained from a database of 163,558 inpatients in our hospital from April 2012 to March 2016. Falls occurred in 3,099 patients for 4 years (1.89%). Adverse events associated with fall occurred in 36 of the 3,099 patients (1.2%) and the overall incidence of adverse events was 0.22%. Most falls involved patients in their 70s, followed by patients in their 60s and 80s. The time of occurrence was most commonly 4:00-6:59 AM.8,9,12,13) For prevention of fall, we have shown the usefulness of fall risk assessment in hospitalized patients.8,9,12) On the other hand, in this series, the fall rate of outpatients over 5 years was 0.054%, which is lower than that for hospitalized patients. One difference for outpatients is the difficulty of assessment of the risk of fall, and there is no previous study of outpatient fall cases at a university hospital. A further characteristic of outpatients is that nurses are not always able to care for them directly, and because they are lying down for an outpatient examination, there are many opportunities to take off their shoes, which may increase the risk of fall.
There are some limitations in this study, including all fall cases are reported from incident-event web forms; therefore, the report is left to the judgment of an individual, and the frequency of falls is lower in outpatients compared to inpatients; thus, the number of cases examined is low. Also, the fall-related information was limited to age, gender, environmental factors, and primary clinical department of the outpatients. We could not examine physical factors such as muscular strength, endurance and balance ability, and this limited our analysis of the risk of falls in outpatients. For these reasons, analysis of detailed cause has not been performed. Therefore, it is necessary to investigate detailed cause for the prevention of outpatient falls. However, this is the first report of fall focused on outpatients, and long-term follow-up of 5 years allowed details of the outpatients to be investigated in all fall cases, which is a strong point of the study. These findings should be useful to medical staff with responsibilities for outpatients. We propose recommendations for countermeasures in each fall situation in Table 4.
Table 4.
Preventive countermeasures for outpatient falls
| Situation | Countermeasures |
| Operating room / Examination room | Assess patient fall risk individually |
| Assistance from the side | |
| Escalator | Slow down speed |
| Promote safe use | |
| Restrict use for patients who have difficulty walking without assistance | |
| Waiting room | Eliminate obstacles to patient’s path |
| Provide guidance | |
| Entrance | Change to a non-slippery material |
| Fasten with tape | |
| Parking place | Post notices of danger |
| Neurology / Neurosurgery | Assistance for patients who use a cane or walker |
| Ophthalmology | Warning notice for mydriasis |
| Brighten places with steps | |
| Do not have cords in patient’s path |
In conclusion, fall is common in outpatients suffering from a neurological disease and in ophthalmologic outpatients aged about 70 years old, and is likely to occur in the operating room, examination room, escalator and waiting room. Countermeasures for fall prevention at each location are necessary.
CONFLICT OF INTEREST
None of the authors have a conflict of interest with regard to the work in the study.
REFERENCES
- 1).Imagama S, Ito Z, Wakao N, Seki T, Hirano K, Muramoto A, et al. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J, 2013; 22: 1346–1353. [DOI] [PMC free article] [PubMed]
- 2).van Weel C, Vermeulen H, van den Bosch W. Falls, a community care perspective. Lancet, 1995; 345: 1549–1551. [DOI] [PubMed]
- 3).Healey F, Scobie S, Oliver D, Pryce A, Thomson R, Glampson B. Falls in English and Welsh hospitals: a national observational study based on retrospective analysis of 12 months of patient safety incident reports. Qual Saf Health Care, 2008; 17: 424–430. [DOI] [PubMed]
- 4).Uden G. In-patient accidents in hospital. J Am Geriatic Soc, 1985; 33: 833–841.
- 5).Fine W. An analysis of 277 falls in hospital. Gerontol Clin, 1959; 1: 292–300.
- 6).Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health, 1992; 82: 1020–1023. [DOI] [PMC free article] [PubMed]
- 7).Hill AM, McPhail SM, Waldron N, Etherton-Beer C, Ingram K, Flicker L, et al. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet, 2015; 385: 2592–2599. [DOI] [PubMed]
- 8).Kobayashi K, Imagama S, Ando K, Inagaki Y, Suzuki Y, Nishida Y et al. Analysis of falls that caused serious events in hospitalized patients. Geriatr Gerontol Int, 2017; 17:2403–2406. [DOI] [PubMed]
- 9).Kobayashi K, Imagama S, Ando K, Suzuki Y, Ando K, Nishida Y, et al. Incidence and characteristics of accidental falls in hospitalization. Nagoya J Med Sci, 2017; 79:291–298. [DOI] [PMC free article] [PubMed]
- 10).Nordell E, Jarnlo GB, Jetsén C, Nordström L, Thorngren KG. Accidental falls and related fractures in 65–74 year olds: a retrospective study of 332 patients. Acta Orthop Scand, 2000; 71: 175–179. [DOI] [PubMed]
- 11).Mathers LJ, Weiss HB. Incidence and characteristics of fall-related emergency department visits. Acad Emerg Med, 1998; 5: 1064–1070. [DOI] [PubMed]
- 12).Kobayashi K, Imagama S, Ando K, et al. Measures and effects on prevention of fall: the role of a fall working group at a university hospital. Nagoya J Med Sci, 2017; 79: 497–504. [DOI] [PMC free article] [PubMed]
- 13).Kobayashi K, Ando K, Inagaki Y, et al. Characteristics of falls in orthopedic patients during hospitalization. Nagoya J Med Sci, 2018 [in press] [DOI] [PMC free article] [PubMed]


