ABSTRACT
Falls are common in elderly patients and comprise 20–30% of all incident reports in hospitals. The current study examined falls in orthopedic patients among 212,617 inpatients admitted to our hospital from April 2012 to March 2017, using a prospective database in the hospital event reporting system. The risk of fall was evaluated using a fall assessment scoresheet at admission and during hospitalization, based on which patients were divided into risk grades 1, 2 and 3. Fall leading to fracture or a life-threatening injury was defined as an adverse event. The number of falls during the study period was 3,925, including 230 in orthopedic patients. Fall cases occurred at all times, but adverse events were significantly more common from 1–7 a.m. (67% vs. 24%, p<0.01). Patients hospitalized for orthopedic surgery had significantly higher fall rates compared to all other patients (3.12% vs. 1.80%, p<0.01), and were older (65.8 vs. 61.4 years, p<0.05) and more frequently >80 years old (23.4% vs. 17.9%, p<0.05). There was a significant difference in fall incidence between risk grades 2 and 3 for patients hospitalized for non-orthopedic surgery, but not for patients hospitalized for orthopedic surgery. We conclude that fall can occur in orthopedic patients with a low predicted risk of fall, and particularly for older patients. This may indicate that frequent specialized fall assessment is desirable after orthopedic surgery.
Key Words: fall, hospital, orthopedic surgery, elderly, adverse events
INTRODUCTION
Falls are the most common adverse events reported for elderly patients1) and comprise 20–30% of all incident reports in hospitals.2-4) Fall of hospitalized patients can cause trauma or fracture that lead to a decrease in activities of daily living (ADL), and may even be fatal. Therefore, prevention of fall is important for medical safety and for reduction of healthcare costs for nursing care during a hospital stay.
Fall-related injuries are steadily increasing in acute care, and these injuries require additional examination or treatment and affect the length and cost of a hospital stay. Some related incidents may even lead to a medical lawsuit. Therefore, prevention of fall has become an important issue in medical safety. Older patients are likely to fall due to a decrease in balance, loss of skeletal muscles, and other physical dysfunctions associated with aging. Chronic medical conditions such as diabetes and hypertension are also risk factors for falls and subsequent fractures.5-7)
Most patients who undergo orthopedic surgery have musculoskeletal disorders. Since our institution is an acute-care hospital and national university, we mostly treat patients who are hospitalized for a surgical procedure, and thus we need to consider circumstances that are specific to the perioperative period. In this context, fall is likely to lead to delayed rehabilitation and may interfere with recovery after surgery.
There have been several reports on fall of elderly patients during hospitalization,3-5,8,9) and we have previously reported the usefulness of a fall assessment scoresheet.10-12) However, none of these reports have focused on orthopedic patients. The current study was performed as a prospective examination of the characteristics over five years of cases of fall in orthopedic patients.
MATERIALS AND METHODS
A total of 212,617 inpatients admitted to our hospital from April 2012 to March 2017 were subjected to analysis. Incidents of fall were examined prospectively using a database in the hospital event reporting system. In our institution, a clinical error or event is submitted as an incident or event report, regardless of whether it results in harm to a patient. A web-based reporting system is used to maintain anonymity and produce a blame-free system. This approach also facilitates easy access for reporting, a shorter data entry time, better legibility of reports, and immediate information sharing among hospital staff. All reports are submitted to the patient safety management office for analysis, and these reports are used to develop measures for future improvements. In this study, we used these data to examine cases of fall in orthopedic patients.
A fall was defined as an involuntary change of posture whereby a patient ended up lying on the floor. An adverse event due to fall was defined as any fracture or life-threatening injury. A case requiring suturing of a wound was excluded if not accompanied by fracture. All patients with a fall were subsequently followed up until discharge.
For assessment of fall risk, we used a fall risk score that was originally developed by a working group in our hospital. This score was evaluated routinely by a nurse at admission, in each week of hospitalization, at the time of a fall, and as the medical condition changed. The assessment at the time of the fall was based on the last evaluation before the fall. The risk was determined using a fall assessment score sheet comprising 33 items, including history of fall, ADL, and cognition (Table 1). The sum of the scores for these items served as the risk score. Patients were classified as grade 1 (low risk), grade 2 (moderate risk), and grade 3 (high risk) based on scores of 0–5, 6–15, and ≥16 and including at least one of all the major items, respectively. Demographic data (incidence of fall, sex, and age), fall risk score, time of occurrence, location of occurrence, and adverse events were obtained from the database.
Table 1.
Risk assessment score sheet
| Assessment | Yes | No |
|---|---|---|
| Past history | ||
| History of fall | 1 | 0 |
| History of syncope | 1 | 0 |
| History of convulsions | 1 | 0 |
| Impairment | ||
| Visual impairment | 1 | 0 |
| Hearing impairment | 1 | 0 |
| Vertigo | 1 | 0 |
| Mobility | ||
| Wheelchair | 1 | 0 |
| Cane | 1 | 0 |
| Walker | 1 | 0 |
| Need assistance | 1 | 0 |
| Cognition | ||
| Disturbance of consciousness | 1 | 0 |
| Restlessness | 1 | 0 |
| Memory disturbance | 1 | 0 |
| Decreased judgment | 1 | 0 |
| Dysuria | ||
| Incontinence | 1 | 0 |
| Frequent urination | 1 | 0 |
| Need helper | 1 | 0 |
| Go to bathroom often at night | 1 | 0 |
| Difficult to reach the toilet | 1 | 0 |
| Drug use | ||
| Sleeping pills | 1 | 0 |
| Psychotropic drugs | 1 | 0 |
| Morphine | 1 | 0 |
| Painkiller | 1 | 0 |
| Antiparkinson drug | 1 | 0 |
| Antihypertensive medication | 1 | 0 |
| Anti-cancer agents | 1 | 0 |
| Laxatives | 1 | 0 |
| Dysfunction | ||
| Muscle weakness | 1 | 0 |
| Paralysis, numbness | 1 | 0 |
| Dizziness | 1 | 0 |
| Bone malformation | 1 | 0 |
| Rigidity | 1 | 0 |
| Brachybasia | 1 | 0 |
The protocol of this study was approved by the Ethics Committee of the Nagoya University Graduate School of Medicine.
Statistical analysis
Differences between two groups were analyzed by Mann-Whitney U test or Student t-test, and those among three groups were analyzed by Kruskal-Wallis test. All analyses were conducted using SPSS ver.23 for Window (IBM Inc., Chicago, IL), with p<0.05 considered to be significant.
RESULTS
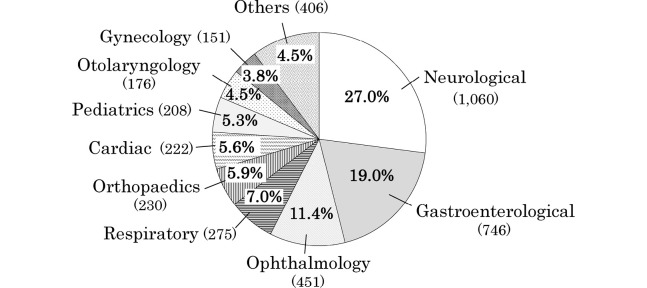
Details of all falls that occurred for 5 years are shown in Table 2. A total of 3,925 patients had falls in the entire hospital, giving a fall rate of 1.85% (3,925/212,617). Based on the fall risk score from the assessment score sheet, 44.0% of fall patients were classified in grade 2 and 45.0% were classified in grade 3. Most falls occurred in hospital rooms (64.9%). Falls in orthopedic patients accounted for 5.9% of all falls, which was fifth after patients in the neurology, gastroenterology, ophthalmology, and respiratory departments (Figure1). Sixty falls had associated adverse events (1.6%).
Table 2.
Comparison between orthopedic patients and all other patients
| Variable | All patients | Orthopedic patients | All other patients | p |
|---|---|---|---|---|
| Incidence of fall | 1.84% (3,926/212,617) |
3.12%
(230/7,353) |
1.80%
(3,696/205,264) |
<0.01 |
| Demographic | ||||
| Age | 61.6±20.4 | 65.8±20.1 | 61.4±20.5 | <0.05 |
| Over 80 years of age | 18.3% (718) | 23.4% (54) | 17.9% (664) | <0.05 |
| Female | 43.4% (1,704) | 47.3% (109) | 43.2% (1,595) | n.s. |
| Fall risk score | ||||
| Grade 1 | 10.9% (431) | 13.0% (30) | 10.8% (401) | n.s. |
| Grade 2 | 43.9% (1,727) | 57.0% (131) | 43.2% (1,596) | <0.01 |
| Grade 3 | 45.0% (1,767) | 30.0% (69) | 45.9% (1,698) | <0.01 |
| Location | ||||
| Hospital room | 64.9% (2,551) | 63.9% (147) | 65.1% (2,404) | n.s. |
| Corridor | 15.0% (589) | 16.5% (38) | 14.9% (551) | n.s. |
| Restroom | 7.9% (314) | 10.4% (24) | 7.8% (290) | n.s. |
| Bathroom | 3.9% (157) | 3.4% (7) | 4.1% (150) | n.s. |
| Rehabilitation ward | 1.9% (76) | 2.6% (6) | 1.9% (70) | n.s. |
| Others | 6.0% (236) | 3.4% (8) | 6.2% (228) | n.s. |
| Adverse event | 1.5% (60) | 2.6% (6) | 1.4% (54) | n.s. |
Fig. 1.
Primary diseases of all patients with fall (n=3926).
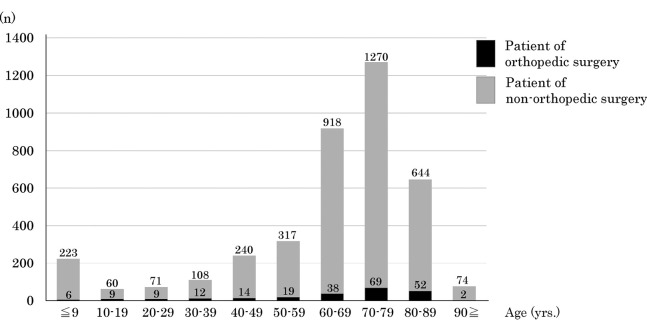
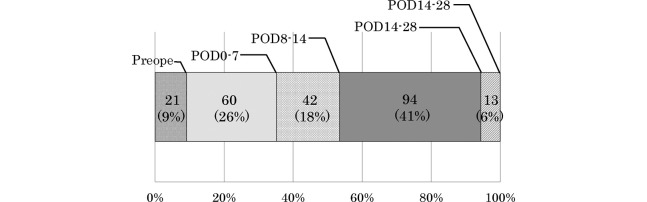
There were 7,353 patients hospitalized for orthopedic surgery over 5 years, and falls occurred in 230 of these patients (121 males, 109 females), giving an incidence of fall of 3.12% (230/7,353) (Table 2). All the patients were hospitalized for a surgical procedure and most falls involved patients in their 70s (Figure 2). Diseases at admission were knee osteoarthritis (n=52), lumbar spinal stenosis (n=41), hip osteoarthritis (n=39), rheumatoid arthritis (n=29), bone and soft tissue tumor (n=28: 8 upper extremities, 20 lower extremities), and achondroplasia (n=19). Fall occurred preoperatively in 21 cases and postoperatively in 209 cases, including 26% (60/230) in postoperative day (POD) 0–7 and 44% (104/230) in POD 0–14 (Figure 3). There were 6 adverse events due to fall in orthopedic patients: 2 rib fractures, 2 lumbar vertebral fractures, one clavicle fracture, and one radial distal fracture.
Fig. 2.
Distribution of patients hospitalized for orthopedic or non-orthopedic surgery by age category.
Fig. 3.
Timing of fall in patient hospitalized for orthopedic surgery. POD: postoperative day
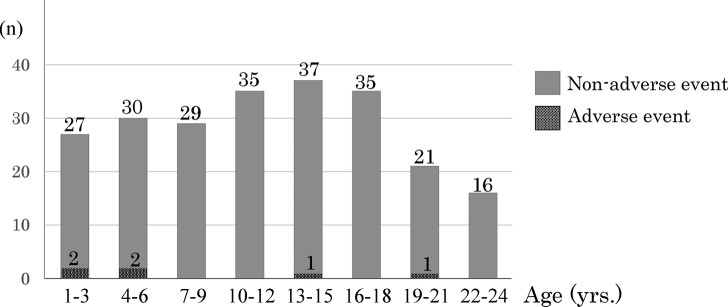
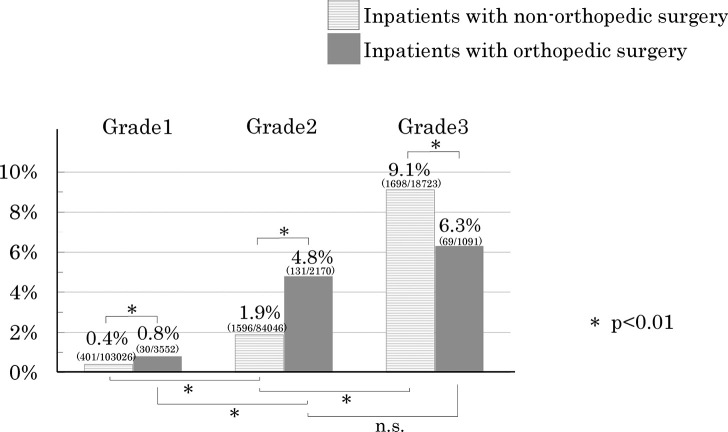
As shown in Table 2, orthopedic patients had a significantly higher rate of fall compared to all other patients (3.12% vs.1.80%, p<0.01), and were also significantly older (65.8 vs. 61.4 years, p<0.05) and significantly more frequently aged over 80 years (23.4% vs. 17.9%, p<0.05). The fall risk score for orthopedic patients was significantly more frequently grade 2 and significantly less frequently grade 3 (both p<0.01). Fall occurred at any time (Figure 4), but fall with an adverse event was significantly more likely at late-night to early morning (1 a.m.–7 a.m.) (67% vs. 24%, p<0.05) (Figure 5). Fall rates were significantly different in each fall risk grade between patients hospitalized for orthopedic and non-orthopedic surgery (p<0.01). The fall incidence between risk grades 2 and 3 was significantly different for patients hospitalized for non-orthopedic surgery (1.9% vs. 9.1%, p<0.01), but not for patients hospitalized for orthopedic surgery (4.8% vs. 6.3%, n.s.) (Figure 6).
Fig. 4.
Time of fall (n=230) in patients hospitalized for orthopedic surgery, including fall leading to adverse events and non-adverse events.
Fig. 5.
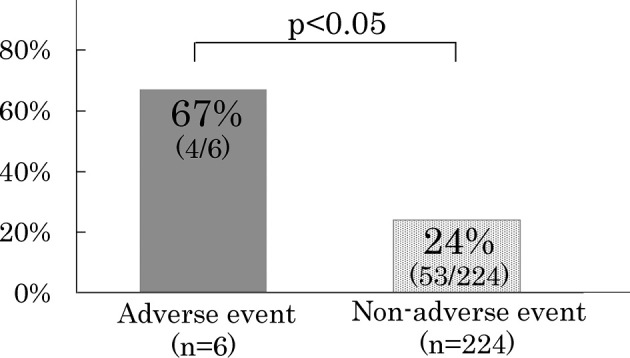
Incidence of adverse events that occurred after fall at late-night to early morning (1 a.m.–7 a.m.). Fall with an adverse event was significantly more likely in this time period.
Fig. 6.
Fall rates in each fall risk grade for patients hospitalized for orthopedic surgery and non-orthopedic surgery. There was a significant difference between these groups of patients for each risk grade, except between grades 2 and 3 in patients hospitalized for orthopedic surgery.
DISCUSSION
Falls are a common health problem in elderly people1, and in the adult population the incidence of fall increases with aging.5,9) In hospital, falls are common adverse events that comprise 20–30% of all incident reports.10) There have been several studies of fall in elderly patients during hospitalization,3-5,8-12) but none have focused on orthopedic patients. Therefore, the current study is the first to examine fall related to orthopedic surgery, and we found that fall rate and age were both significantly higher in orthopedic patients compared to all other patients.
In our hospital, for prevention of falls during hospitalization, we have established a fall-prevention working group for medical quality and safety management. This group has 10 members and includes doctors, nurses, and physiotherapists. The goal of the working group is to improve medical quality and safety management through promotion of fall prevention, verification and analysis of fall cases, and education and training for staff.
In our series, the incidence of fall was 1.85% in all cases, but 3.12% in patients before and after orthopedic surgery. The higher incidence may be due to the significantly older age of orthopedic patients and the background of musculoskeletal disorders in these patients. All patients were hospitalized for surgery, which suggests that they were admitted with a good general condition, despite being elderly. Almost all falls occurred postoperatively (91%), at a time when general condition is temporarily poorer, and recovery may need a long time in elderly people. These factors may increase the risk of fall, and rehabilitation may be particularly important for recovery after surgery. Regarding the time of occurrence of falls, previous reports show that fall is most common at night in patients of more than 70 years of age5. In our series, fall occurred at all times, but fall with an adverse event was significantly more common at late-night to early morning (1 a.m.–7 a.m.). Adverse events were uncommon, but they can influence postoperative ADL and QOL. Therefore, it is important to pay close attention to nighttime postoperative management.
Regarding the relationship between fall rate and fall risk score, as shown in Figure 6, the fall rate in non-orthopedic patients was significantly higher in those with a grade 3 fall risk, showing the utility of the assessment scale in screening for patients at potential risk of falls.10,11) However, in orthopedic patients, those with a grade 2 risk had the highest fall rate, although the incidence of fall did not differ significantly between grade 2 cases and grade 3 cases. We routinely assess fall risk at admission, at the time of a fall, and as the medical condition changes. However, the results for orthopedic patients suggest that the fall risk score might not properly reflect the risk of fall in these patients. As perspective view, regular evaluation at short intervals and evaluation of the validity of the risk score are desirable. Moreover, fall still occurred in patients with a grade 1 risk. Thus, a fall risk assessment method that is specialized for orthopedic surgery is required.
There are some limitations in this study, including 1) the risk assessment scoresheet is original and is used only in our hospital; therefore, its validity is uncertain, especially for orthopedic patients; 2) all fall cases are reported from incident-event web forms; therefore, the report is left to the judgment of an individual; and 3) for non-orthopedic patients, the fall rates in individual departments are not included. However, details of patients hospitalized for orthopedic surgery were investigated prospectively in all fall cases with long-term follow-up of 5 years. Therefore, we believe that the findings are reliable and provide new information.
Perspective and proposal
In our hospital, for prevention of falls during hospitalization, we have established a fall-prevention working group for medical quality and safety management. This group has 10 members and includes doctors, nurses, and physiotherapists. The goal of the working group is to improve medical quality and safety management through promotion of fall prevention, verification and analysis of fall cases, and education and training for staff. Based on the current study, we propose that standardized hospital-wide efforts toward fall prevention and an individually specialized fall assessment process are necessary.
CONCLUSION
Fall rate and age were both higher in orthopedic patients, regardless of a low risk management score. This suggests that regular evaluation at short intervals and a fall risk assessment method specialized for patients hospitalized for orthopedic surgery are necessary.
CONFLICT OF INTEREST
None of the authors have a conflict of interest with regard to the work in the study.
REFERENCES
- 1).Imagama S, Ito Z, Wakao N, Seki T, Hirano K, Muramoto A, et al. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J, 2013; 22: 1346–1353. [DOI] [PMC free article] [PubMed]
- 2).van Weel C, Vermeulen H, van den Bosch W. Falls, a community care perspective. Lancet,1995; 345: 1549–1551. [DOI] [PubMed]
- 3).Healey F, Scobie S, Oliver D, Pryce A, Thomson R, Glampson B. Falls in English and Welsh hospitals: a national observational study based on retrospective analysis of 12 months of patient safety incident reports. Qual Saf Health Care, 2008; 17: 424–430. [DOI] [PubMed]
- 4).Uden G. In-patient accidents in hospital. J Am Geriatic Soc, 1985; 33: 833–841.
- 5).Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health, 1992; 82: 1020–1023. [DOI] [PMC free article] [PubMed]
- 6).Grisso JA, Schwarz DF, Wishner AR, Weene B, Holmes JH, Sutton RL. Injuries in an elderly inner-city population. J Am Geriatr Soc, 1990; 38: 1326–1331. [DOI] [PubMed]
- 7).Nordell E, Jarnlo GB, Jetsén C, Nordström L, Thorngren KG. Accidental falls and related fractures in 65–74 year olds: a retrospective study of 332 patients. Acta Orthop Scand, 2000; 71: 175–179. [DOI] [PubMed]
- 8).Fine W. An analysis of 277 falls in hospital. Gerontol Clin, 1959; 1: 292–300.
- 9).Hill AM, McPhail SM, Waldron N, Etherton-Beer C, Ingram K, Flicker L, et al. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet, 2015; 385: 2592–2599. [DOI] [PubMed]
- 10).Kobayashi K, Imagama S, Ando K, Inagaki Y, Suzuki Y, Nishida Y, et al. Analysis of falls that caused serious events in hospitalized patients. Geriatr Gerontol Int, 2017 Jun 28. [in press] [DOI] [PubMed]
- 11).Kobayashi K, Imagama S, Ando K, Inagaki Y, Suzuki Y, Nishida Y, et al. Incidence and characteristics of accidental falls in hospitalization. Nagoya J Med Sci, 2017; 79: 291–298. [DOI] [PMC free article] [PubMed]
- 12).Kobayashi K, Ando K, Inagaki Y, Suzuki Y, Nagao Y, Ishiguro N, et al. Measures and effects on prevention of fall: the role of a fall working group at a university hospital. Nagoya J. Med. Sci, 2017; 79: 497–504. [DOI] [PMC free article] [PubMed]