Abstract
Background:
A major goal in neurotrauma management is the prevention of secondary neuronal injuries. This goal is time bound as neurological deficits once established are usually irreversible. Late presentation is the norm in most neurotrauma patients in developing countries.
Aims:
The aim of the study was to review the timing of presentation of neurotrauma patients and the possible causes of their late presentation for neurosurgical care in our practice.
Methods:
A cross-sectional study of a 4-month prospective database of neurotrauma patients presenting to the University College Hospital, Ibadan, was done. The participants’ biodata, injury characteristics, initial-care details before referral, and information on timing and causes of delay were analyzed.
Results:
The study subjects included 111 patients, 80.2% (89/111) were males, and 52.8% aged 21–40 years. Head injury (HI), spinal cord injury (SCI), and combined HI and SCI occurred, respectively, in 80.2%, 14.4%, and 5.4%. Road accidents followed by falls were seen in 73.9% and 14.4% (16), respectively. Just 46.8% (52/111) cases presented within 12 h of injury and only 37 (33.3%) within 4 h. Majority, 83.8% (93/111) were referrals from primary care. These referrals were delayed in 81.7% (76/93) of these. The referring health facilities were located intracity with our center in 54%. Other causes of delayed presentation of these study participants included long-distance travel to our center, lack of funds, or a combination of the above factors. Eighty-nine patients (80.2%) were brought in by family members and the remaining minority by passers-by and road safety personnel.
Conclusions:
Delayed referral from primary care features prominently in timing of presentation of neurotrauma patients in Nigeria. There is a need for collaboration as well as continuing medical education between the neurotrauma specialists and primary care physicians.
KEYWORDS: Developing country, neurosurgery, neurotrauma, timing of presentation
INTRODUCTION
Neurotrauma, that is, traumatic injury to the brain and/or the spinal cord, remains a major public health problem globally. Data are scarce on their true prevalence in Sub-Saharan African region, but traumatic brain injury (TBI) is estimated to have an incidence of 200/100,000 in West Africa.[1] The incidence of spinal cord injury (SCI) on the other hand is only an extrapolated estimate, put at 21–29/100,000.[2] These injuries, if not outrightly fatal, usually have significant debilitating effects on the survivors; affect mainly the productive, mobile, working-age groups in the world; and as such are a major source of economic loss in Nigeria, as well as most of Sub-Saharan Africa.[3,4,5]
Increase in motorization and urbanization is a key factor in the rising incidence in these parts of the world; hence, there is a gradual rise in neurotrauma from motor vehicle and motorbike origin. Road traffic accidents place a huge economic burden on the society as well as the individual and have been estimated to have direct and indirect economic costs of about 50 billion dollars in the developed countries.[5] In most of the recent reports, these mechanisms of injury from road trauma account for the largest number of TBI in Nigeria.[6,7]
Delay in receiving health care has been described as a key factor leading to poor outcome.[8] The care of the neurotrauma patient starts from the point of trauma where things such as basic on-site resuscitation can be done, airway secured, and the spine immobilized long before the patient gets to a specialized trauma facility. These early interventions play a significant role in facilitating good outcomes in these groups of patients.[9,10,11] In the absence of a dedicated service to carry out these functions, patients should be transferred as soon as possible to specialized trauma care with specialized neurosurgical facilities.
In the nervous system, neural pathologic lesions resulting from the primary impact of the trauma lead to direct injury to neuronal structures. This is the usual and most direct cause of fatality in TBI in the first few posttrauma golden hours. Avoidable causes of death such as hypovolemia, hypotension, and hypoxia are secondary assaults that are usually compounded by delays in getting specialized care in developing countries. Almost 50% of such delays can be merely as a result of slowness in transfer from a primary care facility to a specialized care facility.[12] Such delay in receiving neurotrauma patients from the primary care health facilities for definitive care is a daily experience in our neurosurgical practice in Nigeria.
The aim of this study, therefore, is to quantify this delay and its determinants in our study population.
METHODS
We prospectively reviewed the prehospital characteristics of neurotrauma patients who presented for neurosurgical care at the University College Hospital (UCH), Ibadan, Nigeria, during the study period. The UCH is our country's foremost university teaching hospital, a nationally designated center of excellence in neurosciences. It is located in Southwestern Nigeria but receives neurosurgical referrals from at least two-thirds of the nation's geographical spread. These referrals are usually from all strata of the national health pyramid: primary, secondary, tertiary, and private health-care facilities within and out of state.[13]
Head injury (HI) was defined in this study using the United States Department of Veterans Affairs definition as traumatically induced structural injury and/or physiologic disruption of brain function as a result of an external force that is indicated by new onset or worsening of at least one of the following clinical signs, immediately following the event: any period of loss of or a decreased level of consciousness, any loss of memory for events immediately before or after the injury (posttraumatic amnesia), any alteration in mental state at the time of the injury (confusion, disorientation, slowed thinking, etc.), and neurologic deficits (weakness, loss of balance, change in vision, praxis, paresis/plegia, sensory loss, aphasia, etc.) that may or may not be transient or intracranial lesion.[14] Classification into mild, moderate, and severe HI was done using the Glasgow Coma Score (GCS). Patients with GCS 13–15, 9–12, and 3–12 were classified as mild, moderate, and severe HI, respectively.
The participants for this study were recruited at the time of presentation to the hospital over a 4-month period between July and October 2016. A total sampling of all prospective, consecutive patients presenting during the study period was done. The information obtained included the biodata, cause of trauma, and details of initial care before referral for neurosurgical care. Information regarding timing from trauma to presentation for neurosurgical care as well as causes of delay (in those presenting late) was obtained from their letters of referral when available, as well as from the history obtained from the patients or their relations/eyewitnesses when the patients were themselves not lucid enough to give the history. Delay was described as a presentation to our facility >4 h posttrauma Seelig et al.[15]
Data management/statistical analysis
The clinical variables for this study were gathered consecutively with clinical summary forms. The data were entered into an electronic spreadsheet using the Statistical package for social sciences Version 22 (SPSS, Inc. Illinois USA). The data were analyzed and presented with descriptive statistics.
RESULTS
One hundred and eleven patients were recruited to the study: 89 males and 22 females, male:female ratio of 4:1. Eighty-nine patients (80.2%) had HI, 16 patients (14.4%) had SCI, while 6 (5.4%) patients had combined HI and SCI. Forty-eight (53.9%) of the head injured patients had mild HI. Moderate HI and severe HI were sustained in 20 (22.5%) and 21 (23.6%) of the patients, respectively. Complete SCI, that is, American Spinal Injury Association (ASIA) grading scale A was seen in 9 (40.9%) of the 22 patients with spinal cord injuries. ASIA C, D, and E were seen in 4 (18.1%), 3 (13.6%), and 6 (27.3%) patients, respectively. The patients with the ASIA E injuries also fell into the group with combined head and spinal cord injuries. The head injuries were all mild in these groups of patients. Twenty patients (18.0%) had injury to other organs/systems. Injury to the long bones formed the largest number of extra craniospinal axis injuries [Table 1].
Table 1.
Distribution of patients with extra craniospinal axis injury secondary to road trauma

Fifteen (52.8%) of the patients were between the ages of 21 and 40 years. There was a steady increase in the number of cases up to 40 years of age among the patients after which there was a sharp decline in the number of cases [Figure 1].
Figure 1.
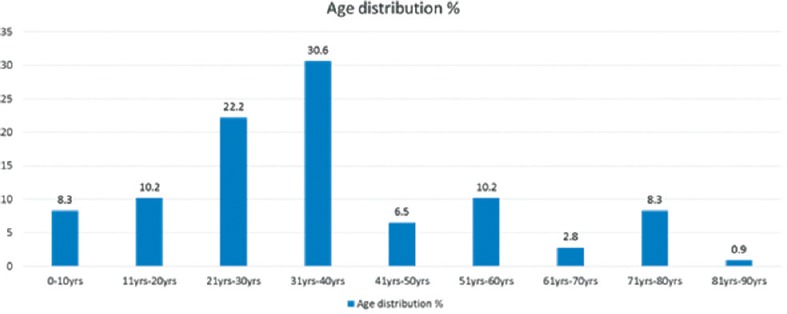
Timing of presentation of neurotrauma victims for neurosurgery in Nigeria: age distribution of the patient population
Causes of trauma were mainly road traffic accidents (82 [73.9%]) and falls (16 [14.4%]) [Table 2]. More than half of the patient population (59 [53.2%]) presented after 12 h of injury, [Figure 2], and only one-third (36 [33.3%]) within 4 h, [Table 3].
Table 2.
Timing of presentation of neurotrauma victims for neurosurgery in Nigeria: mechanism ofinjury

Figure 2.
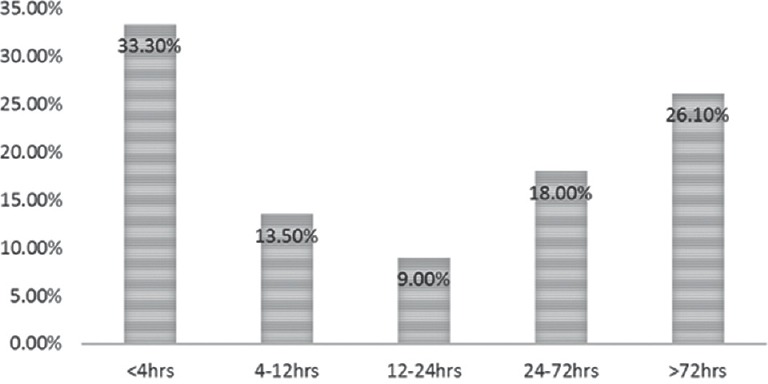
Timing of presentation of neurotrauma victims for neurosurgery in Nigeria
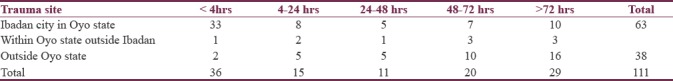
Table 3.
Timing of presentation of neurotrauma victims for neurosurgery in Nigeria: location of trauma and duration (h) before presentation
Ninety-three patients (83.8%) were referrals from other facilities while 18 patients (16.2%) presented directly from the site of trauma to our health facility, the study center. More than half (51%) of the referred patients presented first to a private hospital, as shown in Figure 3. Of all the referred patients, 16 patients were referred from tertiary facilities, 13 of those patients were from facilities with neurosurgical facilities; however, the patients were referred due to lack of bed space for admission at those facilities. Referrals from other facilities were due to lack of neurosurgical facilities and expertise to manage patients with a diagnosis of HI, irrespective of the grade of HI.
Figure 3.
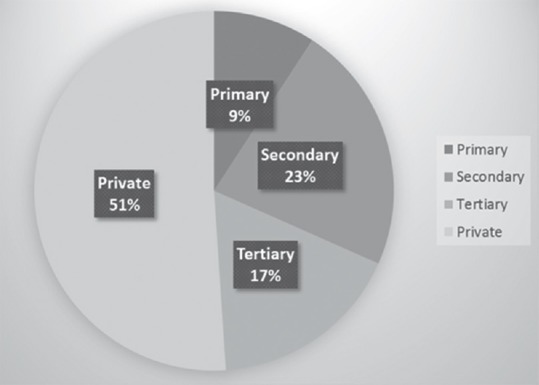
Timing of presentation of neurotrauma victims for neurosurgery in Nigeria: preneurosurgical disposition of the study participants
Sixty-two (56%) patients sustained the neurotrauma intracity, within the Ibadan metropolis, our study center's location; 10 patients (9%) had the trauma within our state, Oyo state but out of the Ibadan metropolis, while 38 (35%) had the trauma out-of-state. Delayed referral was the most common cause of the late presentation, followed by long-distance travel to access our center, [Figure 4].
Figure 4.
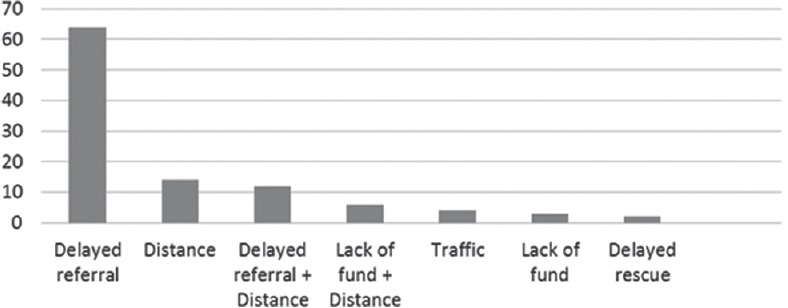
Timing of presentation of neurotrauma victims for neurosurgery in Nigeria: reasons for delay
Ninety-six (86%) patients were brought in by their relatives. The remaining patients were brought in by neighbors, police, or other road safety officials and sometimes by mere passers-by, the so-called “good Samaritans,” [Figure 5].
Figure 5.
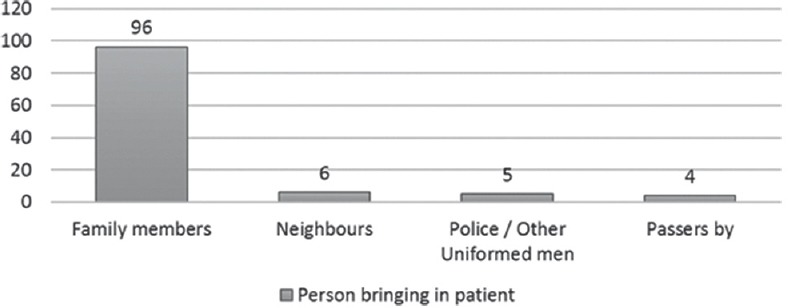
Delayed neurosurgical presentation of neurotrauma patients in Ibadan: persons bringing in the patients
DISCUSSION
Motor vehicle accidents are a major cause of neurotrauma in this series with the pattern of etiology described being similar to that of Adeleye et al., where 143 patients were reviewed in another major Southwestern Nigerian state. One hundred and five patients (73.4%) in that report presented first to other facilities before presenting to the trauma center with neurosurgical services. The details of the prior treatment received by these patients before their neurosurgical referrals could not be ascertained in 80% of the participants.[7]
Delay in the treatment of HI, especially evacuation of intracranial hematoma, is a well-known preventable cause of mortality and significant morbidity, posttrauma.[15] Delay occurs when there is an unreasonable time lapse between the onset of deterioration and subsequent positive diagnostic or therapeutic action.[12] In this series, 34.1% of the patients presented after 24 h and only 33.3% of patients presented within the acceptable time frame of 4 h. Hence, a larger percentage of patients that could possibly be saved could be lost due to this sort of delayed presentation. Trauma occurring within Ibadan metropolis, our center's city of location, tends to present earlier to us for neurosurgical care: 33 of the 36 such patients presented within 4 h; hence, a neurotrauma service located in a large city can be, not unexpectedly, a major facilitation to reducing delay in presenting for dedicated specialist care following neurotrauma. Fifty-seven patients presented from private facilities; hence; there is a need for cooperation between the primary care physicians/general practitioners and the neurotrauma care team. Delay in patient referral in tandem with long distance to a specialized service accounts for 64% of the delay in presentation in this study. The above along factors as well as long distance travelled to get to our service to access specialized neurotrauma service, accunt for 90% of the factors respoonsible for delayed presentation.
There are several interventions aimed at reduction of the incidence and severity of neurotrauma following road traffic accidents. Use of seat belts for vehicle occupants is one of these and has been mandated in many industrialized countries. However, this intervention has not had the desired effect in developing countries for lack of compliance with this road-safety rule, and many of the old, over-used vehicles plying the roads in these low-resource regions actually lack functional seat belts.[16,17,18,19] Strategies targeted at the two-wheelers have also been devised and include the use of helmets. In some places, laws are passed to ensure two-wheelers are sold with appropriate helmet.[20,21] Other interventions described include building of wider sidewalks to protect civilians; yet, other cross-cutting interventions aimed at protecting all road users include enforcing speed limits and placing of speed bumps.[18] All these, along with well-developed emergency medical services, have continued to help in mitigating the burdens of neurotrauma in most developed countries. These interventions are as a rule not readily adopted in most developing countries, thereby contributing to the already bleak outlook of neurotrauma patients. Early referral and quick intervention could be a point of intervention in our peculiar environment. There is a need to carry out continuing medical education to teach physicians on initial care of HI and identifying features of worsening HI.
Hence, as seen in this study, determinants of delay of presentation could be deemed:
Infrastructural: Poor road network, lack of emergency medical and ambulance services, and unavailability of patient transfer network
Delay in decision: For those in the preneurosurgical heath facilities, private or tertiary health facilities, there is the tendency to first attend to other injuries, suture lacerations, and secure hemostasis while observing the patient for signs of possible recovery. When recovery is not imminent, the decision to transfer is made. We actually received some unstable patients; hence, we suspect that the clinical status of the patient with regard to clinical stability is insignificant in deciding to refer the patients
Finances: Medical treatment in Nigeria is largely paid for out of pocket by patients at the points of care; hence, funds are first expended in the primary care facility, such that by the time of referral, relatives that tend to bring the patient to the hospital have exhausted a significant amount of their finances on the initial care.[22]
Study limitations
One main limitation of this study is its short duration, small sample size, and the fact that it was a single-center one. Other limitations include the fact that the outcomes’ pre- and post-admissions could not be included in the result due to poor records which is a bane of medical research in Sub-Saharan Africa. Nevertheless, the findings were in agreement with what is our daily experience in the neurosurgical care of neurotrauma patients in our service.
CONCLUSIONS
Neurotrauma is still a silent epidemic in the developing countries and interventions to stem the tide of mortalities and poor outcomes at present are not adequate. Delayed presentation due to late referral and long distance remains a modifiable problem. There is a need for better cooperation between the neurotrauma experts and the primary care physicians.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bruns J, Jr, Hauser WA. The epidemiology of traumatic brain injury: A review. Epilepsia. 2003;44(Suppl 10):2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 2.Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: Update 2011, global incidence rate. Spinal Cord. 2014;52:110–6. doi: 10.1038/sc.2012.158. [DOI] [PubMed] [Google Scholar]
- 3.Solagberu B, Adekanye A, Ofoegbu C, Udoffa U. Epidemiology of trauma deaths. West Afr J Med. 2004;22:177–81. doi: 10.4314/wajm.v22i2.27944. [DOI] [PubMed] [Google Scholar]
- 4.Joshipura MK, Shah HS, Patel PR, Divatia PA, Desai PM. Trauma care systems in India. Injury. 2003;34:686–92. doi: 10.1016/s0020-1383(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 5.Basso A, Previgliano I, Duarte JM, Ferrari N. Advances in management of neurosurgical trauma in different continents. World J Surg. 2001;25:1174–8. doi: 10.1007/s00268-001-0079-3. [DOI] [PubMed] [Google Scholar]
- 6.Adeolu A, Malomo A, Shokunbi M, Komolafe E, Abiona T. Etiology of head injuries in Southwestern Nigeria: A public health perspective. Internet J Epidemiol. 2005:2. Doi: 10.5580/21d2. [Google Scholar]
- 7.Adeleye AO, Olowookere KG, Olayemi OO. Clinicoepidemiological profiles and outcomes during first hospital admission of head injury patients in Ikeja, Nigeria. A prospective cohort study. Neuroepidemiology. 2009;32:136–41. doi: 10.1159/000182821. [DOI] [PubMed] [Google Scholar]
- 8.Nantulya VM, Reich MR. Equity dimensions of road traffic injuries in low – and middle-income countries. Inj Control Saf Promot. 2003;10:13–20. doi: 10.1076/icsp.10.1.13.14116. [DOI] [PubMed] [Google Scholar]
- 9.Pollack A, Barnes L, Ciotola J, Gulli B, editors. Emergency Care and Transportation of the Sick and Injured. 10th ed. Chapter 15. Burlington, Massachusetts, United States: Jones and Bartlet Publishers; 2013. American Academy of Orthopaedic Surgeons (AAOS) pp. 566–97. [Google Scholar]
- 10.Spaite DW, Hu C, Bobrow BJ, Chikani V, Barnhart B, Gaither JB, et al. The effect of combined out-of-hospital hypotension and hypoxia on mortality in major traumatic brain injury. Ann Emerg Med. 2017;69:62–72. doi: 10.1016/j.annemergmed.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spaite DW, Bobrow BJ, Stolz U, Sherrill D, Chikani V, Barnhart B, et al. Evaluation of the impact of implementing the emergency medical services traumatic brain injury guidelines in Arizona: The Excellence in Prehospital Injury Care (EPIC) study methodology. Acad Emerg Med. 2014;21:818–30. doi: 10.1111/acem.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rose J, Valtonen S, Jennett B. Avoidable factors contributing to death after head injury. Br Med J. 1977;2:615–8. doi: 10.1136/bmj.2.6087.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adeleye AO. Pattern of referrals of head injury to the University College Hospital, Ibadan. Ann Ib Postgrad Med. 2017;15:34–40. [PMC free article] [PubMed] [Google Scholar]
- 14.The Management of Concussion-Mild Traumatic Brain Injury Working Group. VA/DoD Clinical Practice Guideline for the Management of Concussion-Mild Traumatic Brain Injury VA/DoD Clinical Practice Guideline for the Management of Concussion-Mild Traumatic Brain Injury the Management of Concussion-Mild Traumatic Brain Injury Working Group the Office of Quality, Safety and Value, VA, Washington, DC & Office of Evidence Based Practice, U.S Army Medical Command VA/DoD Clinical Practice Guideline for the Management of Concussion-Mild Traumatic Brain Injury. 2016. [Last accessed on 2017 Nov 10]. Available from: https://www.healthquality.va.gov/guidelines/Rehab/mtbi/mTBICPGFullCPG50821816.pdf .
- 15.Seelig JM, Becker DP, Miller JD, Greenberg RP, Ward JD, Choi SC, et al. Traumatic acute subdural hematoma: Major mortality reduction in comatose patients treated within four hours. N Engl J Med. 1981;304:1511–8. doi: 10.1056/NEJM198106183042503. [DOI] [PubMed] [Google Scholar]
- 16.Mohan D. Road traffic deaths and injuries in India: Time for action. Natl Med J India. 2004;17:63–6. [PubMed] [Google Scholar]
- 17.Forjuoh SN. Traffic-related injury prevention interventions for low-income countries. Inj Control Saf Promot. 2003;10:109–18. doi: 10.1076/icsp.10.1.109.14115. [DOI] [PubMed] [Google Scholar]
- 18.Forjuoh SN, Li G. A review of successful transport and home injury interventions to guide developing countries. Soc Sci Med. 1996;43:1551–60. doi: 10.1016/s0277-9536(96)00051-2. [DOI] [PubMed] [Google Scholar]
- 19.Hazen A, Ehiri JE. Road traffic injuries: Hidden epidemic in less developed countries. J Natl Med Assoc. 2006;98:73–82. [PMC free article] [PubMed] [Google Scholar]
- 20.Nakahara S, Wakai S. Underreporting of traffic injuries involving children in Japan. Inj Prev. 2001;7:242–4. doi: 10.1136/ip.7.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu BC, Ivers R, Norton R, Boufous S, Blows S, Lo SK. Helmets for preventing injury in motorcycle riders. In: Liu BC, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2008. [DOI] [PubMed] [Google Scholar]
- 22.Adeleye AO, Jite IE, Smith OA. A tale of two acute extradural hematomas. Surg Neurol Int. 2016;7:54. doi: 10.4103/2152-7806.181905. [DOI] [PMC free article] [PubMed] [Google Scholar]


