Abstract
Aims/hypothesis
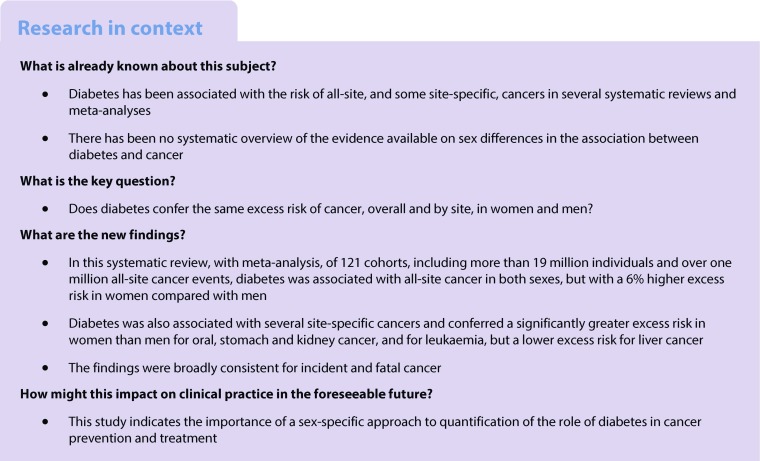
Diabetes has been shown to be a risk factor for some cancers. Whether diabetes confers the same excess risk of cancer, overall and by site, in women and men is unknown.
Methods
A systematic search was performed in PubMed for cohort studies published up to December 2016. Selected studies reported sex-specific relative risk (RR) estimates for the association between diabetes and cancer adjusted at least for age in both sexes. Random-effects meta-analyses with inverse-variance weighting were used to obtain pooled sex-specific RRs and women-to-men ratios of RRs (RRRs) for all-site and site-specific cancers.
Results
Data on all-site cancer events (incident or fatal only) were available from 121 cohorts (19,239,302 individuals; 1,082,592 events). The pooled adjusted RR for all-site cancer associated with diabetes was 1.27 (95% CI 1.21, 1.32) in women and 1.19 (1.13, 1.25) in men. Women with diabetes had ~6% greater risk compared with men with diabetes (the pooled RRR was 1.06, 95% CI 1.03, 1.09). Corresponding pooled RRRs were 1.10 (1.07, 1.13) for all-site cancer incidence and 1.03 (0.99, 1.06) for all-site cancer mortality. Diabetes also conferred a significantly greater RR in women than men for oral, stomach and kidney cancer, and for leukaemia, but a lower RR for liver cancer.
Conclusions/interpretation
Diabetes is a risk factor for all-site cancer for both women and men, but the excess risk of cancer associated with diabetes is slightly greater for women than men. The direction and magnitude of sex differences varies by location of the cancer.
Electronic supplementary material
The online version of this article (10.1007/s00125-018-4664-5) contains peer-reviewed but unedited supplementary material, which is available to authorised users.
Keywords: Cancer, Diabetes, Meta-analysis, Sex differences, Systematic review
Introduction
Cancer is the second leading causes of death in the world [1]. In 2015, there were 17.5 million incident cancer cases and 8.7 million cancer deaths globally, and it is estimated that one in four women and one in three men develop cancer during their lifetime [2]. The incidence of cancer is expected to increase in the next decades, emphasising the importance of efficient prevention and treatment of cancer worldwide.
The prevalence of diabetes has also grown rapidly. In 2015, one in 11 adults (415 million) were reported to have diabetes, five million deaths were attributed to diabetes, and 12% of global health expenditure was spent on diabetes and its complications [3]. Diabetes has been associated with the risk of all-site and some site-specific cancers in several systematic reviews and meta-analyses [4–13]. However, only a minority of these associations are based on robust supporting evidence without question of significant bias [14]. To date, there has been no systematic overview of the evidence available on sex differences in the association between diabetes and cancer. We have previously published compelling evidence that women with diabetes are at an increased risk of stroke [15], coronary heart disease [16] and dementia [17] compared with their male peers. We now question whether this is also true for cancer. In this study, we conducted the most comprehensive systematic review and meta-analysis, to date, to estimate the relative effect of diabetes on the risk of cancer in women compared with men.
Methods
Search strategy and selection criteria
A systematic search was performed in PubMed (https://www.ncbi.nlm.nih.gov/pubmed/) on 23 December 2016 using a combined text word and medical subject heading search strategy (electronic supplementary material [ESM] Table 1). The reference lists of identified reports were also checked for other potentially relevant studies.
Observational cohort studies in general populations were included if they had provided relative risks (RRs), or equivalents, for the association between diabetes and cancer in both women and men. Studies were excluded if they had not adjusted at least for age or did not provide information about the variability around the point estimate, or if they only had data for one sex. In case of duplicate reports from the same study, the study providing the longest follow-up or the highest number of cases was included. We also used individual participant data from the Asia Pacific Cohort Studies Collaboration (APCSC) [18], treated as two separate combinations of data from cohorts in Asia and cohorts from Australia or New Zealand, as in our previous work [15, 16]. One author (TO) did the search and extracted the data. Uncertainties regarding the inclusion or exclusion of articles and data extraction were discussed by all authors and resolved by mutual consent. The meta-analysis was done in accordance with the PRISMA criteria [19].
Data extraction and statistical analysis
The primary endpoint was all-site cancer events (incident or, if this was all that was presented, mortal only). The secondary endpoints were all-site cancer incidence (i.e. omitting studies that only reported mortality), all-site cancer mortality and, for those cancers that could present in both sexes, site-specific cancer events, site-specific incidence and site-specific mortality. In sensitivity analysis we also compared all-site cancer incidence and mortality when restricting to the studies that reported both.
The primary metrics were the pooled adjusted RRs and the women-to-men ratios of RRs (RRRs) for individuals with diabetes vs those without diabetes. For each study, we extracted the sex-specific RRs and 95% CIs for individuals with diabetes vs those without diabetes, from which we estimated the RRRs and 95% CIs. To include the largest set of individuals and cancer endpoints, studies that reported either age-adjusted or multiple-adjusted (maximum-available-adjusted, i.e. the maximum set of adjustments available for each study) results were included in our primary analyses. In pooling multiple-adjusted results, the set of adjustments made were allowed to vary by study, but had to include at least one other risk factor for cancer, in addition to age [15, 16]. We obtained pooled estimates of sex-specific RRs across studies using random-effects meta-analyses applied on the loge scale. Individual studies were weighted according to the inverse variance of loge RRs. The same method was used to pool the RRRs.
The I2 statistic was used to estimate the percentage of variability across studies due to between-study heterogeneity and the Q test was used to assess whether there was a significant lack of homogeneity. The possibility of publication bias was explored using funnel plots and Egger’s and Begg’s tests. Random-effects meta-regression analyses were used to test for differences between pre-assigned subgroups: study region (Asia or Non-Asia), year of baseline study (pre-1985 or 1986 onwards, and also examined as a continuous variable), ascertainment of diabetes (self-reported only or others), type of diabetes (type 1 or type 2, where studies which did not differentiate type were classified as type 2), level of adjustment (age-adjusted or multiple-adjusted), and study quality (the Newcastle–Ottawa Scale [20] [ESM Table 2], ≥7 or <7 points, and also examined as a continuous variable). Post hoc, we also considered absolute risk difference, examined as a categorical and continuous variable) (ESM Table 3). A p value of below 0.05 was considered to be statistically significant in analyses for the primary analyses, i.e. all-site cancer. As many statistical tests were envisaged, a p value of below 0.01 was taken to denote significance for site-specific cancers. All analyses were performed using Stata software (release 13; StataCorp, College Station, TX, USA).
Results
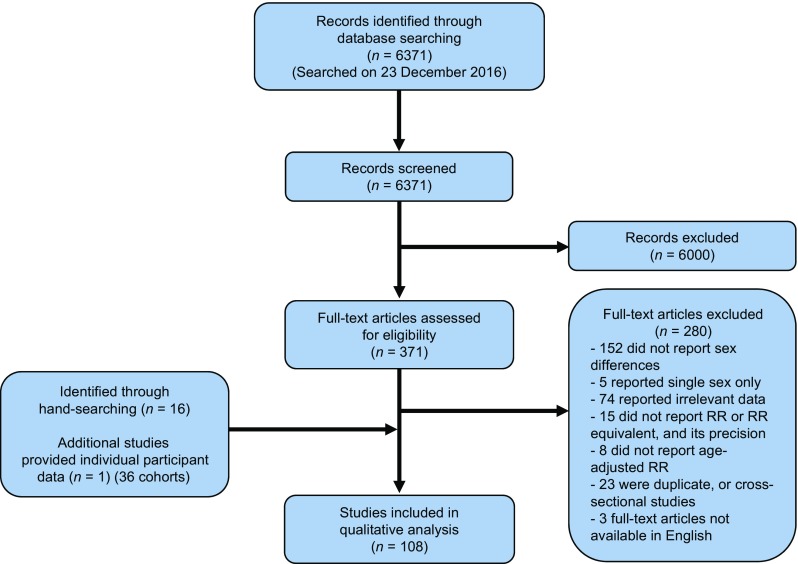
Of the 6371 articles identified through the systematic search, 371 articles qualified for full-text evaluation, and 107 articles provided summary data on the association between diabetes and the risk of cancer for both sexes [21–127]. In addition, 36 cohorts with individual participant data from the APCSC were included (Fig. 1).
Fig. 1.
Flow chart of study selection
Characteristics of the studies that reported the association between diabetes and all-site cancer incidence or mortality are shown in Table 1 and ESM Table 4. Data on all-site cancer were available from 47 studies, involving 121 cohorts, 19,239,302 individuals (not counting one study [25] that did not state the total number of participants), and 1,082,592 events (not counting one study [65] that did not state the total number of cancer events).
Table 1.
Characteristics of the studies reporting on the association between diabetes and all-site cancer
| Cohort | Country | Baseline study (years) | Follow-up (years) | No. participants (% women) | Mean age (years) | No. with diabetes (% women) | Type of diabetes | Ascertainment of diabetes | No. with outcome (% women) | I or M | Maximum adjustment available |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ragozzino et al [21] | USA | 1945–1969 | 8.6 | 1135 (NR) | NR | 1135 (NR) | Both | Measured | 120 (47) | I | Age |
| Sasazuki et al [22] | Japan (8 cohorts) | 1984–1994 | 9.9 | 339,459 (54) | 35–103 | NR | Both | Self-reported | 33,022 (40) | I | Age, area, Hx of cerebrovascular disease, CHD, smoking, alcohol consumption, BMI, physical exercise, green leafy vegetable consumption, coffee intake |
| Gini et al [23] | Italy | 2002–2009 | 3.7 | 32,247 (45) | 65 | 32,247 (45) | T2 | Hospital discharge diagnosis, exemption from medical charges, prescription | 2069 (37) | I | Age, year at cancer diagnosis |
| Berger et al [24] | Denmark | 1996–2011 | 12.6 | 4,826,142 (50) | 41.4 | 65,690 (47) | Both | Discharge diagnosis, claimed prescription | 423,942 (51) | I | Age |
| Carstensen et al [25] | Australia, Denmark, Finland, Scotland, Sweden | 1987–2000 | 8–38 | NR 3,932,900 person-years (50) | NR | NR | T1 | Diabetes registry, impatient dataset | 9149 (56) | I | Age, date of follow-up, date of birth |
| Diabetes II-to-Cancer [26] | Germany | 2003 | 3.3 | 26,742 (53) | 64 | 26,742 (53) | T2 | Physician’s diagnosis | 1364 (44) | I | Age |
| VHM&PP Study Cohort [27] | Austria | 1988–2001 | 8.4 | 140,813 (55) | 43 | 4758 (48) | Both | Measured | 5212 (46) | I | Age (stratified), smoking, occupation, BMI |
| Jee et al [28] | Korea | 1992–1995 | 10 | 1,298,385 (36) | 46.9 | 62,924 (33) | Both | Self-reported, measured | I: 53,833 (30) M: 26,473 (22) |
I, M | Age, smoking, alcohol use |
| Wang et al [29] | China | 2007–2013 | 6 | 327,268 (50) | 59.8 | 327,268 (50) | T2 | Diabetes registry | 7435 (45) | I | Age, urbanisation level |
| Hsu et al [30] | Taiwan | 2000–2007 | 5.9 | 14,619 (53) | 50.2 | 14,619 (53) | T1 | National health insurance research database | 760 (44) | I | Age, calendar year |
| Adami et al [31] | Sweden | 1965–1983 | 5.2 | 51,008 (55) | NR | 51,008 (55) | Both | Hospital discharge diagnosis | 2417 (54) | I | Age |
| Dankner et al [32] | Israel | 2002 | 11 | 2,186,196 (53) | 21–89 | 159,104 (53) | Both | Diabetes registry | 128,720 (50) | I | Age, ethnic origin, socioeconomic status |
| NIH-AARP Diet and Health Study [33] | USA | 1995–1996 | 11 | 494,867 (40) | 62.5 | 44,726 (33) | Both | Self-reported | 82,251 (32) | I | Age, BMI, race/ethnicity, education, marital status, family Hx of cancer, self-reported health status, intake of red meat, white meat, fruits, vegetables, alcohol, and coffee, physical activity, smoking, multivitamin use |
| Xu et al [34] | China | 2004 | 3.7 | 36,379 (56) | 59 | 36,379 (56) | T2 | Diabetes registry | 1205 (53) | I | Age |
| DRT [35] | Austria | 2005 | 8.7 | 5709 (47) | 57.4 | 5709 (47) | T2 | Diabetes registry | 525 (45) | I | Age, period in 5 year period groups |
| NDSS (T2DM) [36] | Australia | 1997 | 5.8 | 872,706 (47) | 60.4 | 872,706 (47) | T2 | Diabetes registry | I: 70,406 (38) M: 26,333 (37) |
I, M | Age, calendar year |
| NDSS (T1DM) [36] | Australia | 1997 | 12 | 80,676 (48) | 27.4 | 80,676 (48) | T1 | Diabetes registry | I: 2079 (50) M: 593 (46) |
I, M | Age, calendar year |
| Walker et al [37] | UK | 2001–2007 | 7 | 80,838 (45) | 55–79 | 80,838 (45) | T2 | Diabetes registry | 4285 (43) | I | Age, socioeconomic status |
| MHS registry [38] | Israel | 2000 | 8 | 100,595 (53) | 61.6 | 16,721 (47) | Both | Healthcare service database | 8977 (43) | I | Age, region, socioeconomic status, use of healthcare services a year prior to index date, BMI, Hx of CVD |
| CLUE II [39] | USA | 1989 | 17 | 18,280 (57) | 51.8 | 599 (56) | Both | Self-reported | I: 2481 (52), M: 907 (50) |
I, M | Age, education, BMI, smoking, HT treatment, high cholesterol treatment, menopausal status (for women), Hx of use of oral contraceptives (for women), Hx of use of hormone replacement therapy (for women) |
| Zhang et al [40] | China | 2002–2008 | 6 | 7950 (52) | 61.1 | 7950 (52) | T2 | Diabetes registry | 366 (47) | I | Age |
| Västerbotten Intervention Project [41] | Sweden | 2003 | 8.3a | 68,301 (51) | 46.1a | NRb | Both | Measured | 2669 (53) | I | Age, year of recruitment, smoking |
| ARIC [42] | USA | 1990–1992 | 15 | 12,792 (55) | 56.9 | 1125 (56) | Both | Self-reported, prescription | I: 2657 (45) M: 887 (42) |
I, M | Age, race/ethnicity, ARIC study site, education, smoking status, cigarette-years smoked, BMI, waist circumference, postmenopausal hormone use (for women) |
| Wideroff et al [43] | Denmark | 1977–1989 | 5.7 | 109,581 (50) | Ma: 64 F: 69 | 109,581 (50) | Both | Hospital discharge diagnosis | 8831 (47) | I | Age, calendar year |
| APCSC (Asia) [18] | Asia (26 cohorts)c | 1961–1993 | 7 | 89,468 (46) | 45 | 4621 (45) | Both | Self-reported, measured | 1800 (33) | M | Age, BMI, education, alcohol, smoking |
| APCSC (Australia and New Zealand) [18] | Australia, New Zealand (9 cohorts) | 1989–1996 | 7 | 82,913 (52) | 51 | 3365 (44) | Both | Self-reported, measured | 2563 (41) | M | Age, BMI, education, alcohol, smoking |
| Singapore Chinese Health Study [44] | Singapore | 1999 | 10.1 | 7388 (52) | 62 | 510 (47) | T2 | Measured | 388 (NR) | M | Age, dialect, interview year, education, smoking, alcohol, BMI |
| Poole Diabetes Study [45] | UK | 1996–1998 | 5.25 | 736 (NR) | Ma: 62.9 F: 65.9 |
368 (NR) | T2 | Diabetes registry | 45 (58) | M | Age (matched) |
| DERI Mortality Study [46] | Japan | 1965–1979 | 24.4 | 1385 (60) | 8.8 | 1385 (60) | T1 | Diabetes registry | 2 (50) | M | Age |
| Diabetes UK cohort study [47] | UK | 1972–1993 | 28 | T1:23,326 (NR) T2: 5040 (NR) |
NR | 23,326 (NR) | T1:23,326 (NR) T2: 5040 (NR) |
Diabetes registry | T1: 89 (48), T2 185 (32) | M | Age, calendar year, countryd |
| JPHC [48] | Japan | 1990, 1993 | 17.8 | 99,584 (54) | 50.2 | 4286 (36) | Both | Self-reported | 5288 (36) | M | Age, BMI, alcohol intake, smoking, Hx of hypertension, physical activity, area (stratified) |
| Fresco study [49] | Spain (pool of 12 cohorts) | 1991 | 10 | 55,283 (54) | 56 | 8627 (47) | Both | Self-reported, measured | 850 (36) | M | Age, smoking, BMI, SBP, TC, HDLC |
| NHIS-NSC [50] | Korea | 2002–2003 | 9.7 | 29,807 (48) | NR | 29,807 (48) | T2 | National health insurance database | 1759 (33) | M | Age |
| DECODE study [51] | Denmark, Finland, Italy, the Netherlands, Poland, Sweden, UK (17 cohorts) | 1966–2004 | 15.8 | 44,655 (41) | 53.4 | 3759 (48) | Both | Measured, self-reported | 3235 (27) | M | Age, cohort, BMI, total cholesterol, BP, smoking |
| Tseng [52] | Taiwan | 1995–1998 | 4.4 | 256,036 (54) | 61.2 | 256,036 (54) | Both | National health insurance database | 8098 (41) | M | Age |
| Piemonte Diabetes Register, Turin Population Register [53] | Italy | 1991–1999 | 7.7 | 906,065 (NR) | 20- | T1: 1608 (NR) T2 29,656 (NR) |
Both | Diabetes registry | 26,251 (44) | M | Age, area of birth |
| Hisayama [54] | Japan | 1988 | 16.9 | 2438 (57) | 57.6 | 298 (45) | Both | Measured, self-reported | 229 (37) | M | Age, BMI, total cholesterol, smoking, alcohol, family Hx of cancer, physical activity, dietary factors (daily intakes of total energy, total fat, salt, vitamin A, vitamin B1, vitamin B2, vitamin C, dietary fibre) |
| Forssas et al [55] | Finland | 2003 | 5 | 5,147,349 in 1997, 5,300,484 in 2007 | 1–79 | 171,596 (54) in 1997 284,832 (49) in 2007 |
Both | Diabetes registry | 54,461 (48) | M | Agee |
| Fedeli et al [56] | Italy | 2008 | 3 | 167,621 (45) | 30–89 | 167,621 (45) | Both | Archives from subjects exempt from medical charges | 5110 (35) | M | Age |
| HSE, SHeS [57] | UK | 1994, 1995 | 17, 16 | 204,533 (55) | 47 | 7199 (48) | Both | Self-reported, prescription | 5571 (NR) | M | Age, smoking, BMI |
| Shen et al [58] | China | 1998–2001 | 10.9 | 66,813 (66) | 65- | 9225 (66) | Both | Self-reported | 6336 (55) | M | Age, alcohol use, smoking, exercise, housing and monthly expenditure, BMI |
| Weiderpass et al [59] | Sweden | 1965–1983 | 6.7 | 144,427 (NR) | Ma: 61.3 F: 65.8 |
144,427 (NR) | Both | Hospital discharge diagnosis | 9661 (49) | M | Age, calendar year, comorbidity |
| CPS II [60] | USA | 1982 | 26 | 1,053,831 (56) | NR | 52,655 (50) | Both | Self-reported | 120,221 (46) | M | Age, education, BMI, smoking, alcohol, vegetable intake, red meat intake, physical activity, aspirin use |
| Verona Diabetes Study [61] | Italy | 1987 | 10 | 7148 (53) | 67 | 7148 (53) | Both | Medical records, drug prescription database | 641 (41) | M | Age |
| Sievers et al [62] | USA | 1975 | 10 | 5131 (52) | 15- | 1266 (58) | T2 | Measured | 40 (50) | M | Age |
| 2001 ENTRED study [63] | France | 2001 | 5 | 9101 (NR) | 66 | 9101 (NR) | Both | Self-reported | 380 (NR) | M | Age |
| Allegheny County Type 1 Diabetes Registry [64] | USA | 1965–1979 | 32.9 | 1075 (47) | 10.9 | 1075 (47) | T1 | Medical records | 10 (NR) | M | Age, race |
| BRFSS [65] | USA | 1992 | 5 | 9074 (NR) | 18- | 392 (NR) | Both | Self-reported | NR | M | Age |
| Wong et al [66] | UK | 1985 | 5 | 4186 (49) | 15- | 4186 (49) | Both | Diabetes registry | 131 (48) | M | Age |
| Bruno et al [67] | Italy | 1988 | 5.7 | 1967 (57) | 66.5 | 1967 (57) | T2 | Medical record, prescription, sale records of reagent strips and syringes | 107 (51) | M | Age, calendar period |
| Shaw et al [68] | Mauritius, Fiji, Nauru | 1980, 1982, 1987 | 5 | 9179 (NR) | 40.7 | 595 (53) | Both | Self-reported | 97 (57) | M | Age, ethnicity, smokingf |
| Moss et al [69] | USA | 1980 | 8.5 | 1772 (NR) | 66.7 | 1772 (NR) | Both | Medical records | 85 (55) | M | Age |
| Takayama study [70] | Japan | 1992 | 6.9 | 29,079 (54) | 54.6 | 1217 (35) | Both | Self-reported | 653 (39) | M | Age, smoking, BMI, physical activity, years of education, Hx of HT, intake of total energy, vegetables, fat and alcohol |
| Chicago Heart Association Detection Project in Industry [71] | USA | 1967–1973 | 12 | 20,755 (42) | 35–64 | 643 (34) | Both | Self-reported | 513 (38) | M | Age, BMI, smoking, SBP, serum cholesterol, education, treatment for HT |
If mean values of age or follow-up year were unavailable, median or range was extracted
Wideroff et al was not included in meta-analysis as they did not provide sufficiently accurate CIs for RRs
Studies by Hsu et al, Adami et al, Walker et al, and the Japan Public Health Center-based prospective study, National Diabetes Services Scheme (type 1 diabetes), Takayama study and Västerbotten Intervention Project were excluded from the meta-analysis of primary outcome (all-site cancer) and included in either of the meta-analyses of all-site cancer incidence or mortality only, because of the overlapping of individuals with other studies
aDerived from total cohort
bProportion with fasting glucose in the diabetic range (>6.9 mmol/l) was 2% for women and 3% for men
cKorean Medical Insurance Corporation cohort was excluded
dFor type 1 diabetes, RRs for non-South Asians were extracted
eRRs for non-insulin-treated diabetes were extracted
fRRs for known diabetes were extracted
ARIC, Atherosclerosis Risk in Communities; BRFSS, Behavioral Risk Factor Surveillance System; CLUE II, Give Us a Clue to Cancer and Heart Disease; CPS II, Cancer Prevention Study II; CVD, cardiovascular diseases; DECODE, Diabetes Epidemiology: Collaborative analysis of Diagnostic criteria in Europe; DERI, Diabetes Epidemiology Research International; DRT, Diabetes Registry Tyrol; F, female; HDLC, HDL-cholesterol; HSE, Health Survey for England; HT, hypertension; Hx, history; I, incidence; JPHC, Japan Public Health Center-based prospective study; M, mortality; Ma, male; MHS, Maccabi Healthcare Services; NDSS, National Diabetes Services Scheme; NIH-AARP, National Institutes of Health-American Association of Retired Persons; NHIS-NSC, Korean National Health Insurance Service-National Sample Cohort; NR, not reported; SBP, systolic BP; SHeS, Scottish Health Survey; T1(DM), type 1 diabetes; T2(DM), type 2 diabetes; TC, total cholesterol; VHM&PP, The Vorarlberg Health Monitoring and Promotion Programme; 2001 ENTRED study, 2001–2006 National representative sample of people with diabetes study
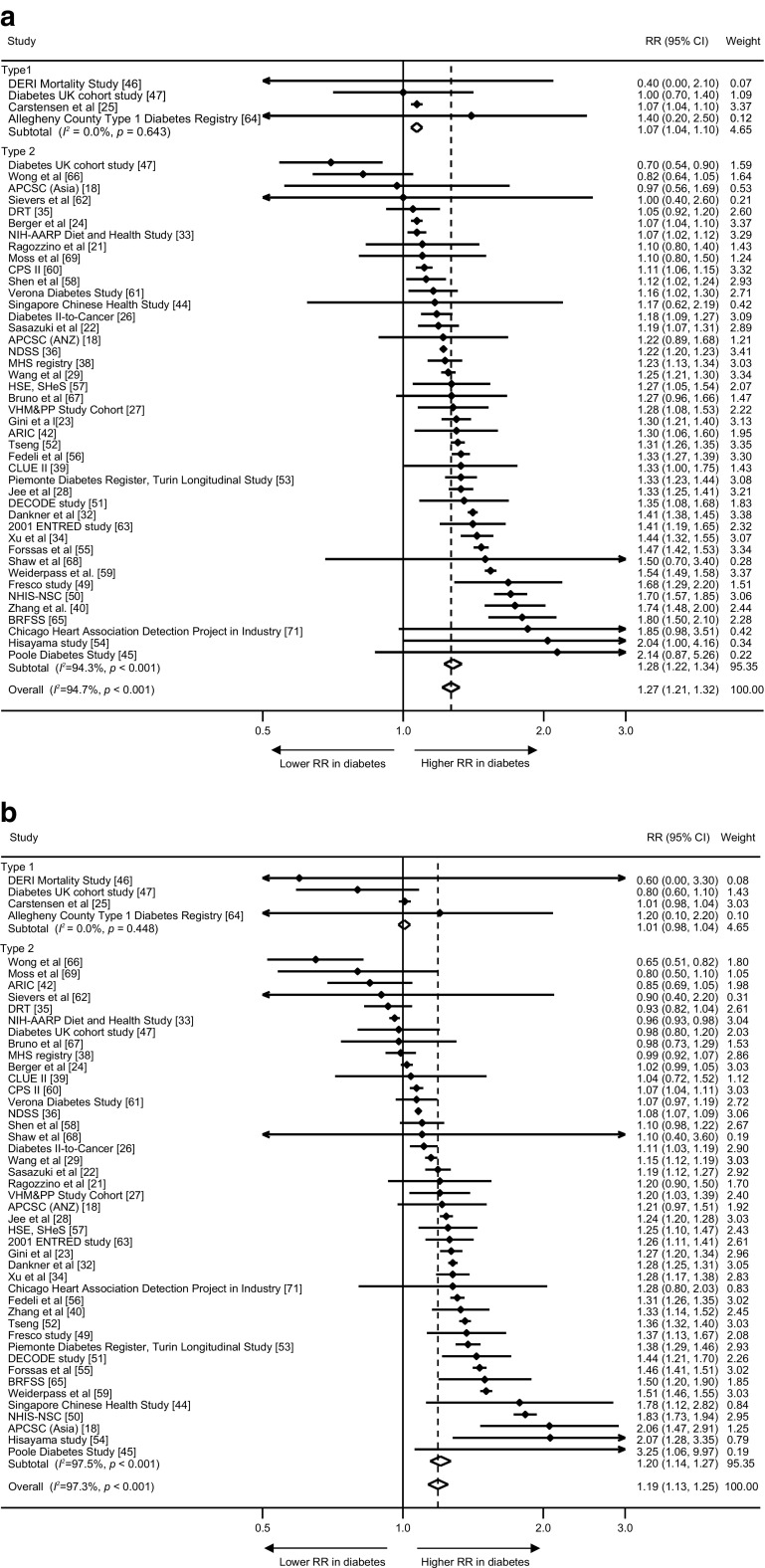
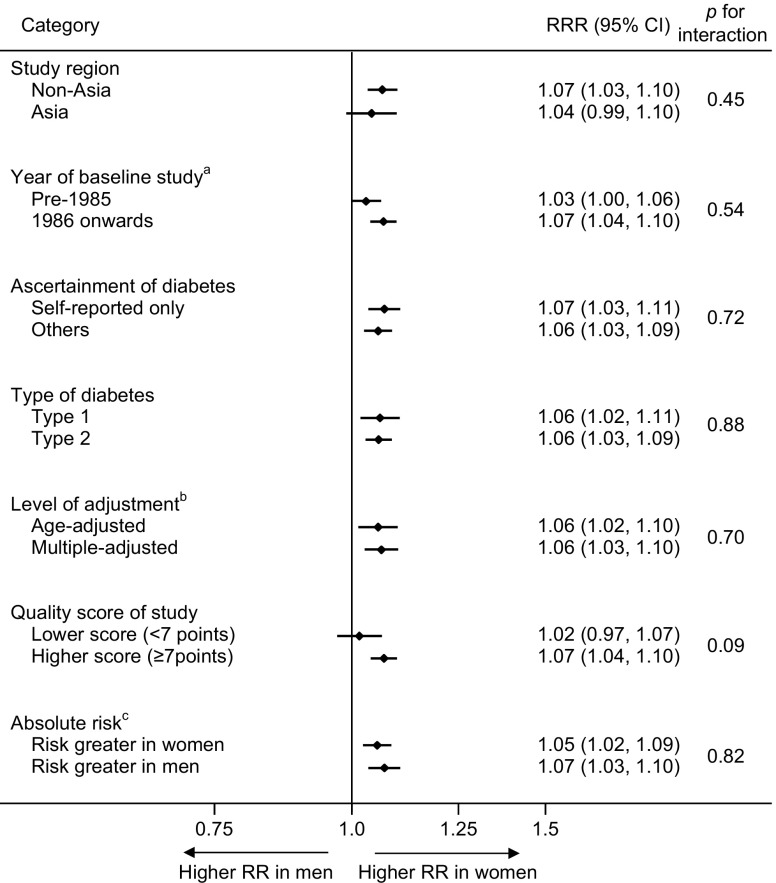
The maximum-available-adjusted pooled sex-specific RR estimates for combined fatal and non-fatal cancer associated with diabetes were 1.27 (95% CI 1.21, 1.32, p < 0.001) for women and 1.19 (1.13, 1.25, p < 0.001) for men (Fig. 2). The pooled women-to-men RRR was 1.06 (1.03, 1.09, p < 0.001, Fig. 3). The I2 statistic for heterogeneity between studies was 66.7%, with no evidence of publication bias (Egger’s test p = 0.13, Begg’s test p = 0.16, ESM Fig. 1). The corresponding RRR was 1.06 (1.02, 1.11, p = 0.005) for type 1 diabetes and 1.06 (1.03, 1.09, p < 0.001) for type 2 diabetes, without evidence of significant heterogeneity by type of diabetes (p for interaction = 0.88, Fig. 4). Exclusion of 22 studies that provided only age-adjusted results had no appreciable effect on the pooled RR estimates (multiple-adjusted pooled RR in women 1.25 [1.17, 1.34], p < 0.001, RR in men 1.20 [1.11, 1.29], p < 0.001, RRR 1.06 [1.03, 1.10], p < 0.001, I2 = 48.9%) (ESM Figs 2 and 3).
Fig. 2.
Maximum-available-adjusted RR for all-site cancer, comparing individuals with diabetes with those without diabetes by sex: (a) women; and (b) men. ANZ, Australia and New Zealand; ARIC, Atherosclerosis Risk in Communities; BRFSS, Behavioral Risk Factor Surveillance System; CLUE II, Give Us a Clue to Cancer and Heart Disease; CPS II, Cancer Prevention Study II; DECODE, Diabetes Epidemiology: Collaborative analysis of Diagnostic criteria in Europe; DERI, Diabetes Epidemiology Research International; DRT, Diabetes Registry Tyrol; 2001 ENTRED study, 2001–2006 National representative sample of people with diabetes study; HSE, Health Survey for England; MHS, Maccabi Healthcare Services; NDSS, National Diabetes Services Scheme; NIH-AARP, National Institutes of Health-American Association of Retired Persons; NHIS-NSC, Korean National Health Insurance Service-National Sample Cohort; SHeS, Scottish Health Survey; VHM&PP, The Vorarlberg Health Monitoring and Promotion Programme
Fig. 3.
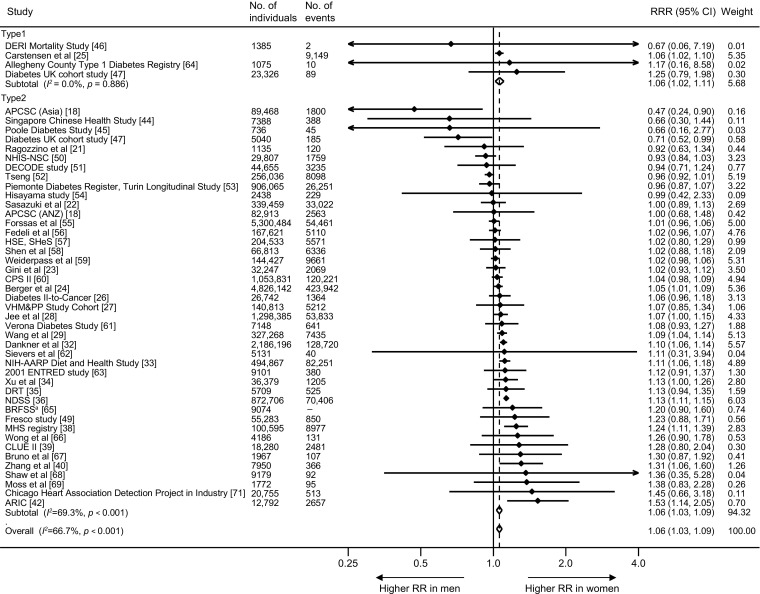
Maximum-available-adjusted women-to-men RRR for all-site cancer, comparing individuals with diabetes with those without diabetes. For definition of study acronyms, please refer to Fig. 2 legend. aThe BRFSS did not report the total number of cancer events
Fig. 4.
Subgroup analyses of women-to-men RRR for all-site cancer, comparing individuals with diabetes with those without diabetes. aSix studies were excluded because the baseline year bridged over 1985 (i.e. included both pre-1985 and 1986 onwards). bResults using multiple adjustment were used when available and age-adjusted otherwise, as in Fig. 3. cTen studies were excluded because absolute risks for men and women were unavailable
The pooled RRR did not vary substantially by study region (p = 0.45), year of baseline study (p = 0.54 for categorical analysis, p = 0.18 for continuous analysis), ascertainment of diabetes (p = 0.72), level of adjustment (p = 0.70), quality of study (p = 0.09 for categorical analysis) or absolute risk difference between men and women (p = 0.82 for categorical analysis, p = 0.99 for continuous analysis), with the exception of continuous analysis for quality of study, p = 0.01) (Fig. 4 and ESM Fig. 4).
Secondary analyses of incidence (fatal or not) and mortality alone for all-site cancer are described in the ESM. The pooled women-to-men RRR for incidence was 1.10 (1.07, 1.13, p < 0.001) (ESM Fig. 5) and for mortality was 1.03 (0.99, 1.06, p = 0.16) (ESM Fig. 6).
In sensitivity analysis using only those studies which provided the RRs for both incidence and mortality, the pooled maximum-available-adjusted RRR was 1.12 (1.06, 1.17, p < 0.001) for all-site cancer incidence, and 1.10 (1.00, 1.21, p = 0.04) for all-site cancer mortality (ESM Fig. 7).
Data on site-specific cancer were available for 50 sites (50 sites for incidence and 29 sites for mortality) (https://www.georgeinstitute.org/sites/default/files/esm-table.pdf). Diabetes was associated with an increased risk of cancer in 43 sites in women and 42 sites in men, with a statistically significant increase (p < 0.01) in risk for those with diabetes in 20 sites in women and 18 sites in men (ESM Fig. 8). The pooled maximum-available-adjusted RRR was statistically significantly higher in women than men for kidney (1.11 [99% CI 1.04, 1.18], p < 0.001), oral (1.13 [1.00, 1.28], p = 0.009), stomach cancer (1.14 [1.07, 1.22], p < 0.001) and leukaemia (1.15 [1.02, 1.28], p = 0.002), whereas it was statistically significantly lower for liver cancer (0.88 [0.79, 0.99], p = 0.005) (Fig. 5). Separate results for incidence and mortality by site of cancer are described in the ESM (ESM Figs 5, 6, 9–24).
Fig. 5.
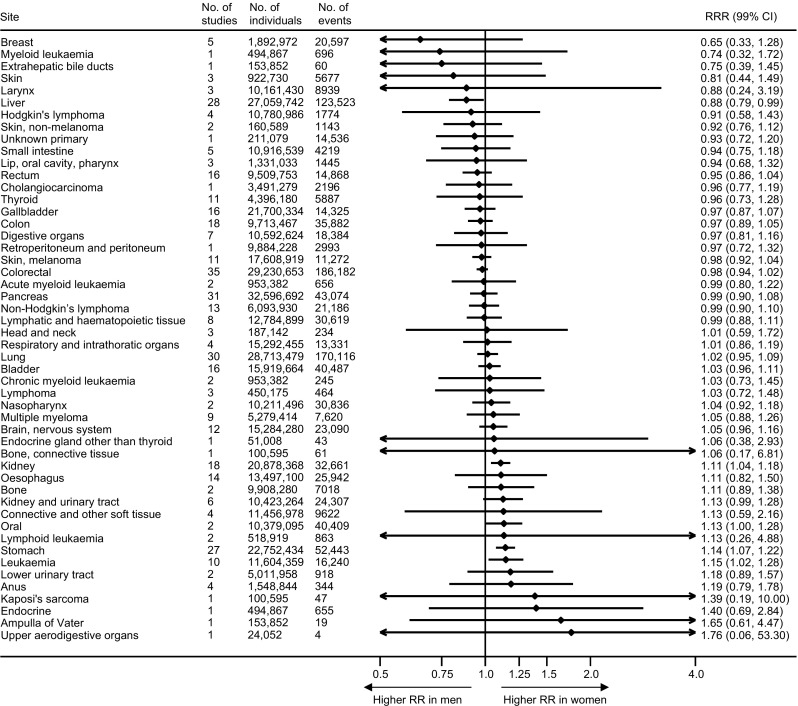
Maximum-available-adjusted pooled women-to-men RRR for cancer at each site, comparing individuals with diabetes with those without diabetes
Discussion
This systematic review, with meta-analysis, of 121 cohorts including more than 19 million individuals and over one million all-site cancer events, demonstrated that diabetes was associated with a 6% higher excess risk of all-site cancer in women than men. Diabetes was associated with several site-specific cancers and conferred a significantly greater excess risk in women than men for oral, stomach and kidney cancer and for leukaemia, but a lower excess risk for liver cancer. The findings were broadly consistent for incident and fatal cancers and across a wide range of prespecified subgroups.
Our findings are in agreement with a previous meta-analysis, which found that the risk of all-site cancer incidence and mortality was significantly increased in both sexes [4]. However, this previous meta-analysis was about a tenth of the size of the current study, and included single-sex studies, and therefore was not able to reliably quantify sex differences as they could have been explained by differences in methods, confounders adjusted for, and the background risks between studies of women and men alone.
As we found some evidence to suggest that the women-to-men RRRs tended to be smaller in studies of lower quality (Fig. 4 and ESM Fig. 4), our results may underestimate any true sex difference. A significant degree of heterogeneity was also observed between studies conducted in and outside Asia with regards to all-site cancer mortality (ESM Fig. 19). However, we did not find heterogeneity between regions for our primary outcome, nor for the other secondary outcomes (all-site cancer incidence), and thus we speculate that this may be a chance finding consequent to the high number of statistical tests conducted.
Although we found a slightly higher women-to-men RRR for cancer incidence than cancer mortality, the finding may be explained by chance differences between the included studies, as almost identical pooled RRR estimates were obtained in the sensitivity analysis restricted to five studies which provided the sex-specific RRs for both incidence and mortality from the same study.
With regard to cancer at specific sites, previous meta-analyses have yielded inconsistent results of increased (stomach [5], lung [6], kidney [7]), similar (oesophagus [8], colorectum [9], pancreas [10], bladder [11], thyroid [12]) or decreased (liver [13]) excess risk of cancer associated with diabetes in women compared with men. However, unlike our methods, these analyses included single-sex studies as well as studies among both women and men.
There are several possible explanations for the excess risk of cancer conferred by diabetes in women than men. One possible mechanism is poor glycaemic control in women with diabetes compared with men with diabetes [128, 129]. Hyperglycaemia may have carcinogenic effects by causing DNA damage [130], which could result from increased oxidative stress due to hyperglycaemia [130] or from hyperglycaemia itself [131]. Historically, women were likely to be undertreated or receive less intensive care compared with men [128, 132]. Further, a recent study showed that adherence to glucose-lowering medication was lower in women than men [133]. As such, the carcinogenic effects of hyperglycaemia may be enhanced in women and subsequently lead to an increased cancer risk compared with men. Alternatively, cumulative exposure to insulin resistance and subsequent hyperinsulinaemia may be longer in women compared with men. The average duration of impaired glucose tolerance or impaired fasting glucose has been found to be more than 2 years longer in women than men [134], suggesting that women may have more exposure to, often untreated, hyperinsulinaemia in the prediabetic state. Hyperinsulinaemia promotes cancer cell proliferation by stimulating the insulin receptor directly and insulin-like growth factor-1 indirectly [135]. Another factor that may, to some extent, explain the smaller RR for incidence of all-site cancer in men compared with women is the apparent protective effect of diabetes on prostate cancer in men with diabetes [136]. Sex-specific cancers or site-specific cancers in which diabetes conferred greater or lower excess risk in women than men may also account for the association, although the degree of contribution cannot be determined from our analyses. In addition to sex difference for all-site cancer, we found also that diabetes conferred a significantly greater RR in women than men for oral, stomach and kidney cancer and for leukaemia, but a lower RR for liver cancer. The underlying mechanisms for sex differences in each specific association are not clear. However, unmeasured confounding factors specific to each site, such as Helicobacter pylori infection for stomach cancer [137] and hepatitis virus infection for liver cancer [138], might be involved. However, the literature around mechanisms underpinning the sex differences in site-specific cancers is scant and further studies are required to confirm and clarify these sex differences in site-specific associations. Finally, the studies in our analyses were not adjusted for female-specific factors including pregnancy, menopausal status and use of hormone replacement therapy that have also been associated with diabetes [139] and cancer [140].
We quantified sex differences based on RRs rather than risk differences. This might introduce a statistical artefact, in which the generally higher absolute risk for cancer in men, and the same risk difference subsequent to diabetes in each sex, would translate to a greater relative risk in women than men. However, this would require that risks of cancers associated with diabetes are additive rather than multiplicative, which is not generally considered to be the case in epidemiology. Indeed, RRs are much more commonly reported than risk differences in both epidemiological studies and clinical trials. Also, unlike risk differences, RRs are typically fairly stable across populations with different background risks, which make them suitable for summarisation of effects in meta-analyses. Furthermore, our previous meta-analyses on risk factors for cardiovascular diseases demonstrated that detection of a female disadvantage in RRs is not inevitable when men have higher absolute risk [141, 142]. We thus believe that the use of RRs in the present analyses is both practical and justifiable.
The strengths of this meta-analysis are its size and the inclusion of studies on the sex-specific effects of diabetes on all-site cancer and 50 site-specific cancers, which enabled us to conduct the most comprehensive analyses to date on the sex-specific effects of diabetes on cancer risk. To limit the risk of bias, we only included cohort studies that were conducted in men and women and had adjusted for at least age. Limitations of this study are inherent to the use of published data and the heterogeneity between studies in ascertainment of diabetes, study design and duration, endpoint definition and degree of adjustment for confounders. Nevertheless, a range of subgroup analysis provided broadly consistent results. However, as we compared women and men from within the same study, any effect of differences in methods between studies is likely to have affected women and men similarly. We therefore assume that the sex comparisons reported in this analysis are still valid. Second, the lack of data on duration of diabetes and the degree of glycaemic control precluded more detailed analyses on the effect of diabetes on the risk of cancer. Third, as this meta-analysis largely used published data, endpoint definition varied across the studies. Fourth, in analysis of all-site cancer, the women-to-men RRRs depend not only on the strengths of the RRRs of site-specific cancers (as illustrated by Fig. 5), but also on the relative incidence of site-specific cancers, which varies considerably between populations. This is likely to be a key factor in the high between-study heterogeneity we show in Fig. 3. Finally, studies generally did not adjust for obstetric and gynaecological history and unmeasured confounding is likely in the current estimates. However, confounding is likely to have been non-differentially distributed between women and men from the same study and we therefore assume that it had only a negligible effect on the reported associations.
In conclusion, diabetes is a risk factor for all-site cancer in both sexes, with a stronger effect in women than men. Sex differences varied across the location of the cancer, heightening the importance of a sex-specific approach to quantification of the role of diabetes in cancer research, prevention and treatment. Further studies are needed to clarify the mechanisms underlying the sex differences in the diabetes–cancer association.
Electronic supplementary material
(PDF 1.26 MB)
Abbreviations
- APCSC
Asia Pacific Cohort Studies Collaboration
- RRR
Ratio of RR
Contribution statement
TO searched the scientific literature, did the statistical analyses, participated in data interpretation and drafted the report. SAEP contributed data, did the statistical analyses, participated in data interpretation and made revisions to the draft report. MW conceived the study, contributed data, oversaw the data analyses, participated in data interpretation and made revisions to the draft report. All authors gave final approval of the version to be published and are responsible for the integrity of the work as a whole. TO is the guarantor of this work.
Funding
This study received no external funding. TO is supported by the Japan Society for the Promotion of Science Overseas Research Fellowships. SAEP is supported by a UK Medical Research Council Skills Development Fellowship (MR/P014550/1). MW is a National Health and Medical Research Council of Australia Principal Research Fellow.
Data availability
The datasets generated during and/or analysed in the current study are available from the corresponding author on reasonable request.
Duality of interest
MW is a consultant to Amgen. Both other authors declare that there is no duality of interest associated with their contribution to this manuscript.
Contributor Information
Toshiaki Ohkuma, Email: tohkuma@georgeinstitute.org.au.
Mark Woodward, Email: mark.woodward@georgeinstitute.ox.ac.uk.
References
- 1.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–548. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Diabetes Federation (2015) IDF Diabetes Atlas, 7th edn. IDF, Brussels. Available from https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/13-diabetes-atlas-seventhedition.html. Accessed 12 May 2018
- 4.Noto H, Tsujimoto T, Sasazuki T, Noda M. Significantly increased risk of cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Endocr Pract. 2011;17:616–628. doi: 10.4158/EP10357.RA. [DOI] [PubMed] [Google Scholar]
- 5.Ge Z, Ben Q, Qian J, Wang Y, Li Y. Diabetes mellitus and risk of gastric cancer: a systematic review and meta-analysis of observational studies. Eur J Gastroenterol Hepatol. 2011;23:1127–1135. doi: 10.1097/MEG.0b013e32834b8d73. [DOI] [PubMed] [Google Scholar]
- 6.Lee JY, Jeon I, Lee JM, Yoon JM, Park SM. Diabetes mellitus as an independent risk factor for lung cancer: a meta-analysis of observational studies. Eur J Cancer. 2013;49:2411–2423. doi: 10.1016/j.ejca.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 7.Bao C, Yang X, Xu W, et al. Diabetes mellitus and incidence and mortality of kidney cancer: a meta-analysis. J Diabetes Complicat. 2013;27:357–364. doi: 10.1016/j.jdiacomp.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Huang W, Ren H, Ben Q, Cai Q, Zhu W, Li Z. Risk of esophageal cancer in diabetes mellitus: a meta-analysis of observational studies. Cancer Causes Control. 2012;23:263–272. doi: 10.1007/s10552-011-9874-9. [DOI] [PubMed] [Google Scholar]
- 9.Kramer HU, Schottker B, Raum E, Brenner H. Type 2 diabetes mellitus and colorectal cancer: meta-analysis on sex-specific differences. Eur J Cancer. 2012;48:1269–1282. doi: 10.1016/j.ejca.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Ben Q, Xu M, Ning X, et al. Diabetes mellitus and risk of pancreatic cancer: a meta-analysis of cohort studies. Eur J Cancer. 2011;47:1928–1937. doi: 10.1016/j.ejca.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Zhu Z, Wang X, Shen Z, Lu Y, Zhong S, Xu C. Risk of bladder cancer in patients with diabetes mellitus: an updated meta-analysis of 36 observational studies. BMC Cancer. 2013;13:310. doi: 10.1186/1471-2407-13-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmid D, Behrens G, Jochem C, Keimling M, Leitzmann M. Physical activity, diabetes, and risk of thyroid cancer: a systematic review and meta-analysis. Eur J Epidemiol. 2013;28:945–958. doi: 10.1007/s10654-013-9865-0. [DOI] [PubMed] [Google Scholar]
- 13.Wang Y, Wang B, Yan S, et al. Type 2 diabetes and gender differences in liver cancer by considering different confounding factors: a meta-analysis of cohort studies. Ann Epidemiol. 2016;26:764–772. doi: 10.1016/j.annepidem.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;350:g7607. doi: 10.1136/bmj.g7607. [DOI] [PubMed] [Google Scholar]
- 15.Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet. 2014;383:1973–1980. doi: 10.1016/S0140-6736(14)60040-4. [DOI] [PubMed] [Google Scholar]
- 16.Peters SA, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57:1542–1551. doi: 10.1007/s00125-014-3260-6. [DOI] [PubMed] [Google Scholar]
- 17.Chatterjee S, Peters SA, Woodward M, et al. Type 2 diabetes as a risk factor for dementia in women compared with men: a pooled analysis of 2.3 million people comprising more than 100,000 cases of dementia. Diabetes Care. 2016;39:300–307. doi: 10.2337/dc15-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lam EK, Batty GD, Huxley RR, et al. Associations of diabetes mellitus with site-specific cancer mortality in the Asia-Pacific region. Ann Oncol. 2011;22:730–738. doi: 10.1093/annonc/mdq405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wells G, Shea B, O’Connell D et al. (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 17 Jun 2017
- 21.Ragozzino M, Melton IIILJ, Chu CP, Palumbo PJ. Subsequent cancer risk in the incidence cohort of Rochester, Minnesota, residents with diabetes mellitus. J Chronic Dis. 1982;35:13–19. doi: 10.1016/0021-9681(82)90025-x. [DOI] [PubMed] [Google Scholar]
- 22.Sasazuki S, Charvat H, Hara A, et al. Diabetes mellitus and cancer risk: pooled analysis of eight cohort studies in Japan. Cancer Sci. 2013;104:1499–1507. doi: 10.1111/cas.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gini A, Bidoli E, Zanier L, et al. Cancer among patients with type 2 diabetes mellitus: a population-based cohort study in northeastern Italy. Cancer Epidemiol. 2016;41:80–87. doi: 10.1016/j.canep.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Berger SM, Gislason G, Moore LL, et al. Associations between metabolic disorders and risk of cancer in Danish men and women—a nationwide cohort study. BMC Cancer. 2016;16:133. doi: 10.1186/s12885-016-2122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carstensen B, Read SH, Friis S, et al. Cancer incidence in persons with type 1 diabetes: a five-country study of 9,000 cancers in type 1 diabetic individuals. Diabetologia. 2016;59:980–988. doi: 10.1007/s00125-016-3884-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hense HW, Kajuter H, Wellmann J, Batzler WU. Cancer incidence in type 2 diabetes patients—first results from a feasibility study of the D2C cohort. Diabetol Metab Syndr. 2011;3:15. doi: 10.1186/1758-5996-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rapp K, Schroeder J, Klenk J, et al. Fasting blood glucose and cancer risk in a cohort of more than 140,000 adults in Austria. Diabetologia. 2006;49:945–952. doi: 10.1007/s00125-006-0207-6. [DOI] [PubMed] [Google Scholar]
- 28.Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM. Fasting serum glucose level and cancer risk in Korean men and women. JAMA. 2005;293:194–202. doi: 10.1001/jama.293.2.194. [DOI] [PubMed] [Google Scholar]
- 29.Wang M, Hu RY, Wu HB, et al. Cancer risk among patients with type 2 diabetes mellitus: a population-based prospective study in China. Sci Rep. 2015;5:11503. doi: 10.1038/srep11503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hsu PC, Lin WH, Kuo TH, Lee HM, Kuo C, Li CY. A population-based cohort study of all-cause and site-specific cancer incidence among patients with type 1 diabetes mellitus in Taiwan. J Epidemiol. 2015;25:567–573. doi: 10.2188/jea.JE20140197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adami HO, McLaughlin J, Ekbom A, et al. Cancer risk in patients with diabetes mellitus. Cancer Causes Control. 1991;2:307–314. doi: 10.1007/BF00051670. [DOI] [PubMed] [Google Scholar]
- 32.Dankner R, Boffetta P, Balicer RD, et al. Time-dependent risk of cancer after a diabetes diagnosis in a cohort of 2.3 million adults. Am J Epidemiol. 2016;183:1098–1106. doi: 10.1093/aje/kwv290. [DOI] [PubMed] [Google Scholar]
- 33.Lai GY, Park Y, Hartge P, Hollenbeck AR, Freedman ND. The association between self-reported diabetes and cancer incidence in the NIH-AARP Diet and Health Study. J Clin Endocrinol Metab. 2013;98:E497–E502. doi: 10.1210/jc.2012-3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu HL, Fang H, Xu WH, et al. Cancer incidence in patients with type 2 diabetes mellitus: a population-based cohort study in Shanghai. BMC Cancer. 2015;15:852. doi: 10.1186/s12885-015-1887-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oberaigner W, Ebenbichler C, Oberaigner K, Juchum M, Schonherr HR, Lechleitner M. Increased cancer incidence risk in type 2 diabetes mellitus: results from a cohort study in Tyrol/Austria. BMC Public Health. 2014;14:1058. doi: 10.1186/1471-2458-14-1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harding JL, Shaw JE, Peeters A, Cartensen B, Magliano DJ. Cancer risk among people with type 1 and type 2 diabetes: disentangling true associations, detection bias, and reverse causation. Diabetes Care. 2015;38:264–270. doi: 10.2337/dc14-1996. [DOI] [PubMed] [Google Scholar]
- 37.Walker JJ, Brewster DH, Colhoun HM, et al. Type 2 diabetes, socioeconomic status and risk of cancer in Scotland 2001-2007. Diabetologia. 2013;56:1712–1715. doi: 10.1007/s00125-013-2937-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chodick G, Heymann AD, Rosenmann L, et al. Diabetes and risk of incident cancer: a large population-based cohort study in Israel. Cancer Causes Control. 2010;21:879–887. doi: 10.1007/s10552-010-9515-8. [DOI] [PubMed] [Google Scholar]
- 39.Yeh HC, Platz EA, Wang NY, Visvanathan K, Helzlsouer KJ, Brancati FL. A prospective study of the associations between treated diabetes and cancer outcomes. Diabetes Care. 2012;35:113–118. doi: 10.2337/dc11-0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang PH, Chen ZW, Lv D, et al. Increased risk of cancer in patients with type 2 diabetes mellitus: a retrospective cohort study in China. BMC Public Health. 2012;12:567. doi: 10.1186/1471-2458-12-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stattin P, Bjor O, Ferrari P, et al. Prospective study of hyperglycemia and cancer risk. Diabetes Care. 2007;30:561–567. doi: 10.2337/dc06-0922. [DOI] [PubMed] [Google Scholar]
- 42.Joshu CE, Prizment AE, Dluzniewski PJ, et al. Glycated hemoglobin and cancer incidence and mortality in the Atherosclerosis in Communities (ARIC) Study, 1990-2006. Int J Cancer. 2012;131:1667–1677. doi: 10.1002/ijc.27394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wideroff L, Gridley G, Mellemkjaer L, et al. Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst. 1997;89:1360–1365. doi: 10.1093/jnci/89.18.1360. [DOI] [PubMed] [Google Scholar]
- 44.Bancks MP, Odegaard AO, Pankow JS, et al. Glycated hemoglobin and all-cause and cause-specific mortality in Singaporean Chinese without diagnosed diabetes: the Singapore Chinese Health Study. Diabetes Care. 2014;37:3180–3187. doi: 10.2337/dc14-0390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guzder RN, Gatling W, Mullee MA, Byrne CD. Early mortality from the time of diagnosis of type 2 diabetes: a 5-year prospective cohort study with a local age- and sex-matched comparison cohort. Diabet Med. 2007;24:1164–1167. doi: 10.1111/j.1464-5491.2007.02223.x. [DOI] [PubMed] [Google Scholar]
- 46.Morimoto A, Onda Y, Nishimura R, Sano H, Utsunomiya K, Tajima N. Cause-specific mortality trends in a nationwide population-based cohort of childhood-onset type 1 diabetes in Japan during 35 years of follow-up: the DERI Mortality Study. Diabetologia. 2013;56:2171–2175. doi: 10.1007/s00125-013-3001-2. [DOI] [PubMed] [Google Scholar]
- 47.Swerdlow AJ, Laing SP, Dos Santos Silva I, et al. Mortality of South Asian patients with insulin-treated diabetes mellitus in the United Kingdom: a cohort study. Diabet Med. 2004;21:845–851. doi: 10.1111/j.1464-5491.2004.01253.x. [DOI] [PubMed] [Google Scholar]
- 48.Kato M, Noda M, Mizoue T, et al. Diagnosed diabetes and premature death among middle-aged Japanese: results from a large-scale population-based cohort study in Japan (JPHC study) BMJ Open. 2015;5:e007736. doi: 10.1136/bmjopen-2015-007736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baena-Diez JM, Penafiel J, Subirana I, et al. Risk of cause-specific death in individuals with diabetes: a competing risks analysis. Diabetes Care. 2016;39:1987–1995. doi: 10.2337/dc16-0614. [DOI] [PubMed] [Google Scholar]
- 50.Kang YM, Kim YJ, Park JY, Lee WJ, Jung CH. Mortality and causes of death in a national sample of type 2 diabetic patients in Korea from 2002 to 2013. Cardiovasc Diabetol. 2016;15:131. doi: 10.1186/s12933-016-0451-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou XH, Qiao Q, Zethelius B, et al. Diabetes, prediabetes and cancer mortality. Diabetologia. 2010;53:1867–1876. doi: 10.1007/s00125-010-1796-7. [DOI] [PubMed] [Google Scholar]
- 52.Tseng CH. Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care. 2004;27:1605–1609. doi: 10.2337/diacare.27.7.1605. [DOI] [PubMed] [Google Scholar]
- 53.Gnavi R, Petrelli A, Demaria M, Spadea T, Carta Q, Costa G. Mortality and educational level among diabetic and non-diabetic population in the Turin Longitudinal Study: a 9-year follow-up. Int J Epidemiol. 2004;33:864–871. doi: 10.1093/ije/dyh089. [DOI] [PubMed] [Google Scholar]
- 54.Hirakawa Y, Ninomiya T, Mukai N, et al. Association between glucose tolerance level and cancer death in a general Japanese population: the Hisayama Study. Am J Epidemiol. 2012;176:856–864. doi: 10.1093/aje/kws178. [DOI] [PubMed] [Google Scholar]
- 55.Forssas E, Sund R, Manderbacka K, Arffman M, Ilanne-Parikka P, Keskimaki I. Increased cancer mortality in diabetic people treated with insulin: a register-based follow-up study. BMC Health Serv Res. 2013;13:267. doi: 10.1186/1472-6963-13-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fedeli U, Zoppini G, Gennaro N, Saugo M. Diabetes and cancer mortality: a multifaceted association. Diabetes Res Clin Pract. 2014;106:e86–e89. doi: 10.1016/j.diabres.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 57.Gordon-Dseagu VL, Shelton N, Mindell J. Diabetes mellitus and mortality from all-causes, cancer, cardiovascular and respiratory disease: evidence from the Health Survey for England and Scottish Health Survey cohorts. J Diabetes Complicat. 2014;28:791–797. doi: 10.1016/j.jdiacomp.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 58.Shen C, Schooling CM, Chan WM, Lee SY, Leung GM, Lam TH. Self-reported diabetes and mortality in a prospective Chinese elderly cohort study in Hong Kong. Prev Med. 2014;64:20–26. doi: 10.1016/j.ypmed.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 59.Weiderpass E, Gridley G, Nyren O, Pennello G, Landstrom AS, Ekbom A. Cause-specific mortality in a cohort of patients with diabetes mellitus: a population-based study in Sweden. J Clin Epidemiol. 2001;54:802–809. doi: 10.1016/s0895-4356(01)00342-0. [DOI] [PubMed] [Google Scholar]
- 60.Campbell PT, Newton CC, Patel AV, Jacobs EJ, Gapstur SM. Diabetes and cause-specific mortality in a prospective cohort of one million U.S. adults. Diabetes Care. 2012;35:1835–1844. doi: 10.2337/dc12-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Verlato G, Zoppini G, Bonora E, Muggeo M. Mortality from site-specific malignancies in type 2 diabetic patients from Verona. Diabetes Care. 2003;26:1047–1051. doi: 10.2337/diacare.26.4.1047. [DOI] [PubMed] [Google Scholar]
- 62.Sievers ML, Nelson RG, Knowler WC, Bennett PH. Impact of NIDDM on mortality and causes of death in Pima Indians. Diabetes Care. 1992;15:1541–1549. doi: 10.2337/diacare.15.11.1541. [DOI] [PubMed] [Google Scholar]
- 63.Romon I, Rey G, Mandereau-Bruno L, et al. The excess mortality related to cardiovascular diseases and cancer among adults pharmacologically treated for diabetes—the 2001-2006 ENTRED cohort. Diabet Med. 2014;31:946–953. doi: 10.1111/dme.12435. [DOI] [PubMed] [Google Scholar]
- 64.Secrest AM, Becker DJ, Kelsey SF, Laporte RE, Orchard TJ. Cause-specific mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes. Diabetes. 2010;59:3216–3222. doi: 10.2337/db10-0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tierney EF, Geiss LS, Engelgau MM, et al. Population-based estimates of mortality associated with diabetes: use of a death certificate check box in North Dakota. Am J Public Health. 2001;91:84–92. doi: 10.2105/ajph.91.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wong JS, Pearson DW, Murchison LE, Williams MJ, Narayan V. Mortality in diabetes mellitus: experience of a geographically defined population. Diabet Med. 1991;8:135–139. doi: 10.1111/j.1464-5491.1991.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 67.Bruno G, Merletti F, Boffetta P, et al. Impact of glycaemic control, hypertension and insulin treatment on general and cause-specific mortality: an Italian population-based cohort of type II (non-insulin-dependent) diabetes mellitus. Diabetologia. 1999;42:297–301. doi: 10.1007/s001250051154. [DOI] [PubMed] [Google Scholar]
- 68.Shaw JE, Hodge AM, de Courten M, Chitson P, Zimmet PZ. Isolated post-challenge hyperglycaemia confirmed as a risk factor for mortality. Diabetologia. 1999;42:1050–1054. doi: 10.1007/s001250051269. [DOI] [PubMed] [Google Scholar]
- 69.Moss SE, Klein R, Klein BE. Cause-specific mortality in a population-based study of diabetes. Am J Public Health. 1991;81:1158–1162. doi: 10.2105/ajph.81.9.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Oba S, Nagata C, Nakamura K, Takatsuka N, Shimizu H. Self-reported diabetes mellitus and risk of mortality from all causes, cardiovascular disease, and cancer in Takayama: a population-based prospective cohort study in Japan. J Epidemiol. 2008;18:197–203. doi: 10.2188/jea.JE2008004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Levine W, Dyer AR, Shekelle RB, Schoenberger JA, Stamler J. Post-load plasma glucose and cancer mortality in middle-aged men and women. 12-year follow-up findings of the Chicago Heart Association Detection Project in Industry. Am J Epidemiol. 1990;131:254–262. doi: 10.1093/oxfordjournals.aje.a115495. [DOI] [PubMed] [Google Scholar]
- 72.Idilbi NM, Barchana M, Milman U, Carel RS. Incidence of cancer among diabetic and non-diabetic adult Israeli Arabs. Isr Med Assoc J. 2013;15:342–347. [PubMed] [Google Scholar]
- 73.Hippisley-Cox J, Coupland C. Development and validation of risk prediction algorithms to estimate future risk of common cancers in men and women: prospective cohort study. BMJ Open. 2015;5:e007825. doi: 10.1136/bmjopen-2015-007825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shu X, Ji J, Li X, Sundquist J, Sundquist K, Hemminki K. Cancer risk among patients hospitalized for type 1 diabetes mellitus: a population-based cohort study in Sweden. Diabet Med. 2010;27:791–797. doi: 10.1111/j.1464-5491.2010.03011.x. [DOI] [PubMed] [Google Scholar]
- 75.Lin CC, Chiang JH, Li CI, et al. Cancer risks among patients with type 2 diabetes: a 10-year follow-up study of a nationwide population-based cohort in Taiwan. BMC Cancer. 2014;14:381. doi: 10.1186/1471-2407-14-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xu HL, Tan YT, Epplein M, et al. Population-based cohort studies of type 2 diabetes and stomach cancer risk in Chinese men and women. Cancer Sci. 2015;106:294–298. doi: 10.1111/cas.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N. Preliminary communication: glycated hemoglobin, diabetes, and incident colorectal cancer in men and women: a prospective analysis from the European prospective investigation into cancer-Norfolk study. Cancer Epidemiol Biomark Prev. 2004;13:915–919. [PubMed] [Google Scholar]
- 78.Limburg PJ, Vierkant RA, Fredericksen ZS, et al. Clinically confirmed type 2 diabetes mellitus and colorectal cancer risk: a population-based, retrospective cohort study. Am J Gastroenterol. 2006;101:1872–1879. doi: 10.1111/j.1572-0241.2006.00725.x. [DOI] [PubMed] [Google Scholar]
- 79.Schoen RE, Tangen CM, Kuller LH, et al. Increased blood glucose and insulin, body size, and incident colorectal cancer. J Natl Cancer Inst. 1999;91:1147–1154. doi: 10.1093/jnci/91.13.1147. [DOI] [PubMed] [Google Scholar]
- 80.Campbell PT, Deka A, Jacobs EJ, et al. Prospective study reveals associations between colorectal cancer and type 2 diabetes mellitus or insulin use in men. Gastroenterology. 2010;139:1138–1146. doi: 10.1053/j.gastro.2010.06.072. [DOI] [PubMed] [Google Scholar]
- 81.Goto A, Noda M, Sawada N, et al. High hemoglobin A1c levels within the non-diabetic range are associated with the risk of all cancers. Int J Cancer. 2016;138:1741–1753. doi: 10.1002/ijc.29917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Will JC, Galuska DA, Vinicor F, Calle EE. Colorectal cancer: another complication of diabetes mellitus? Am J Epidemiol. 1998;147:816–825. doi: 10.1093/oxfordjournals.aje.a009534. [DOI] [PubMed] [Google Scholar]
- 83.Seow A, Yuan JM, Koh WP, Lee HP, Yu MC. Diabetes mellitus and risk of colorectal cancer in the Singapore Chinese Health Study. J Natl Cancer Inst. 2006;98:135–138. doi: 10.1093/jnci/djj015. [DOI] [PubMed] [Google Scholar]
- 84.Magliano DJ, Davis WA, Shaw JE, Bruce DG, Davis TM. Incidence and predictors of all-cause and site-specific cancer in type 2 diabetes: the Fremantle Diabetes Study. Eur J Endocrinol. 2012;167:589–599. doi: 10.1530/EJE-12-0053. [DOI] [PubMed] [Google Scholar]
- 85.Jarvandi S, Davidson NO, Schootman M. Increased risk of colorectal cancer in type 2 diabetes is independent of diet quality. PLoS One. 2013;8:e74616. doi: 10.1371/journal.pone.0074616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sikdar KC, Walsh SJ, Roche M, Jiang Y, Syrowatka A, Collins KD. Diabetes and sex-specific colorectal cancer risks in Newfoundland and Labrador: a population-based retrospective cohort study. Can J Public Health. 2013;104:e101–e107. doi: 10.1007/BF03405668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.He J, Stram DO, Kolonel LN, Henderson BE, Le Marchand L, Haiman CA. The association of diabetes with colorectal cancer risk: the Multiethnic Cohort. Br J Cancer. 2010;103:120–126. doi: 10.1038/sj.bjc.6605721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.de Kort S, Simons CC, van den Brandt PA, et al. Diabetes mellitus type 2 and subsite-specific colorectal cancer risk in men and women: results from the Netherlands Cohort Study on diet and cancer. Eur J Gastroenterol Hepatol. 2016;28:896–903. doi: 10.1097/MEG.0000000000000626. [DOI] [PubMed] [Google Scholar]
- 89.Nilsen TI, Vatten LJ. Prospective study of colorectal cancer risk and physical activity, diabetes, blood glucose and BMI: exploring the hyperinsulinaemia hypothesis. Br J Cancer. 2001;84:417–422. doi: 10.1054/bjoc.2000.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Koskinen SV, Reunanen AR, Martelin TP, Valkonen T. Mortality in a large population-based cohort of patients with drug-treated diabetes mellitus. Am J Public Health. 1998;88:765–770. doi: 10.2105/ajph.88.5.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tan C, Mori M, Adachi Y, et al. Diabetes mellitus and risk of colorectal Cancer mortality in Japan: the Japan Collaborative Cohort Study. Asian Pac J Cancer Prev. 2016;17:4681–4688. doi: 10.22034/APJCP.2016.17.10.4681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ren X, Zhang X, Zhang X, et al. Type 2 diabetes mellitus associated with increased risk for colorectal cancer: evidence from an international ecological study and population-based risk analysis in China. Public Health. 2009;123:540–544. doi: 10.1016/j.puhe.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 93.Chen HF, Chen P, Su YH, Su HF, Li CY. Age- and sex-specific risks of colorectal cancers in diabetic patients. Tohoku J Exp Med. 2012;226:259–265. doi: 10.1620/tjem.226.259. [DOI] [PubMed] [Google Scholar]
- 94.Weiderpass E, Gridley G, Nyren O, Ekbom A, Persson I, Adami HO. Diabetes mellitus and risk of large bowel cancer. J Natl Cancer Inst. 1997;89:660–661. doi: 10.1093/jnci/89.9.660. [DOI] [PubMed] [Google Scholar]
- 95.Onitilo AA, Berg RL, Engel JM, et al. Increased risk of colon cancer in men in the pre-diabetes phase. PLoS One. 2013;8:e70426. doi: 10.1371/journal.pone.0070426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Adami HO, Chow WH, Nyren O, et al. Excess risk of primary liver cancer in patients with diabetes mellitus. J Natl Cancer Inst. 1996;88:1472–1477. doi: 10.1093/jnci/88.20.1472. [DOI] [PubMed] [Google Scholar]
- 97.Campbell PT, Newton CC, Freedman ND, et al. Body mass index, waist circumference, diabetes, and risk of liver Cancer for U.S. adults. Cancer Res. 2016;76:6076–6083. doi: 10.1158/0008-5472.CAN-16-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yang WS, Shu XO, Gao J, et al. Prospective evaluation of type 2 diabetes mellitus on the risk of primary liver cancer in Chinese men and women. Ann Oncol. 2013;24:1679–1685. doi: 10.1093/annonc/mdt017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Koh WP, Wang R, Jin A, Yu MC, Yuan JM. Diabetes mellitus and risk of hepatocellular carcinoma: findings from the Singapore Chinese Health Study. Br J Cancer. 2013;108:1182–1188. doi: 10.1038/bjc.2013.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wild SH, Morling JR, McAllister DA, et al. Type 2 diabetes and risk of hospital admission or death for chronic liver diseases. J Hepatol. 2016;64:1358–1364. doi: 10.1016/j.jhep.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 101.Fujino Y, Mizoue T, Tokui N, Yoshimura T. Prospective study of diabetes mellitus and liver cancer in Japan. Diabetes Metab Res Rev. 2001;17:374–379. doi: 10.1002/dmrr.214. [DOI] [PubMed] [Google Scholar]
- 102.Shibata A, Ogimoto I, Kurozawa Y, et al. Past medical history and risk of death due to hepatocellular carcinoma, univariate analysis of JACC study data. Kurume Med J. 2003;50:109–119. doi: 10.2739/kurumemedj.50.109. [DOI] [PubMed] [Google Scholar]
- 103.Chiang CH, Lee LT, Hung SH, et al. Opposite association between diabetes, dyslipidemia, and hepatocellular carcinoma mortality in the middle-aged and elderly. Hepatology. 2014;59:2207–2215. doi: 10.1002/hep.27014. [DOI] [PubMed] [Google Scholar]
- 104.Chen HF, Chen P, Li CY. Risk of malignant neoplasms of liver and biliary tract in diabetic patients with different age and sex stratifications. Hepatology. 2010;52:155–163. doi: 10.1002/hep.23641. [DOI] [PubMed] [Google Scholar]
- 105.Yagyu K, Lin Y, Obata Y, et al. Bowel movement frequency, medical history and the risk of gallbladder cancer death: a cohort study in Japan. Cancer Sci. 2004;95:674–678. doi: 10.1111/j.1349-7006.2004.tb03328.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tsai MS, Lee PH, Lin CL, Peng CL, Kao CH. Type II diabetes mellitus is associated with a reduced risk of cholangiocarcinoma in patients with biliary tract diseases. Int J Cancer. 2015;136:2409–2417. doi: 10.1002/ijc.29292. [DOI] [PubMed] [Google Scholar]
- 107.Larsson SC, Permert J, Hakansson N, Naslund I, Bergkvist L, Wolk A. Overall obesity, abdominal adiposity, diabetes and cigarette smoking in relation to the risk of pancreatic cancer in two Swedish population-based cohorts. Br J Cancer. 2005;93:1310–1315. doi: 10.1038/sj.bjc.6602868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nilsen TI, Vatten LJ. A prospective study of lifestyle factors and the risk of pancreatic cancer in Nord-Trondelag, Norway. Cancer Causes Control. 2000;11:645–652. doi: 10.1023/a:1008916123357. [DOI] [PubMed] [Google Scholar]
- 109.Chow WH, Gridley G, Nyren O, et al. Risk of pancreatic cancer following diabetes mellitus: a nationwide cohort study in Sweden. J Natl Cancer Inst. 1995;87:930–931. doi: 10.1093/jnci/87.12.930. [DOI] [PubMed] [Google Scholar]
- 110.Lin Y, Tamakoshi A, Kawamura T, et al. Risk of pancreatic cancer in relation to alcohol drinking, coffee consumption and medical history: findings from the Japan collaborative cohort study for evaluation of cancer risk. Int J Cancer. 2002;99:742–746. doi: 10.1002/ijc.10402. [DOI] [PubMed] [Google Scholar]
- 111.Hall GC, Roberts CM, Boulis M, Mo J, MacRae KD. Diabetes and the risk of lung cancer. Diabetes Care. 2005;28:590–594. doi: 10.2337/diacare.28.3.590. [DOI] [PubMed] [Google Scholar]
- 112.Yang WS, Yang Y, Yang G, et al. Pre-existing type 2 diabetes and risk of lung cancer: a report from two prospective cohort studies of 133 024 Chinese adults in urban Shanghai. BMJ Open. 2014;4:e004875. doi: 10.1136/bmjopen-2014-004875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Setiawan VW, Stram DO, Nomura AM, Kolonel LN, Henderson BE. Risk factors for renal cell cancer: the Multiethnic Cohort. Am J Epidemiol. 2007;166:932–940. doi: 10.1093/aje/kwm170. [DOI] [PubMed] [Google Scholar]
- 114.Lindblad P, Chow WH, Chan J, et al. The role of diabetes mellitus in the aetiology of renal cell cancer. Diabetologia. 1999;42:107–112. doi: 10.1007/s001250051122. [DOI] [PubMed] [Google Scholar]
- 115.Washio M, Mori M, Khan M, et al. Diabetes mellitus and kidney cancer risk: the results of Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC Study) Int J Urol. 2007;14:393–397. doi: 10.1111/j.1442-2042.2007.01744.x. [DOI] [PubMed] [Google Scholar]
- 116.Goossens ME, Zeegers MP, Bazelier MT, De Bruin ML, Buntinx F, de Vries F. Risk of bladder cancer in patients with diabetes: a retrospective cohort study. BMJ Open. 2015;5:e007470. doi: 10.1136/bmjopen-2014-007470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Newton CC, Gapstur SM, Campbell PT, Jacobs EJ. Type 2 diabetes mellitus, insulin-use and risk of bladder cancer in a large cohort study. Int J Cancer. 2013;132:2186–2191. doi: 10.1002/ijc.27878. [DOI] [PubMed] [Google Scholar]
- 118.Woolcott CG, Maskarinec G, Haiman CA, Henderson BE, Kolonel LN. Diabetes and urothelial cancer risk: the Multiethnic Cohort study. Cancer Epidemiol. 2011;35:551–554. doi: 10.1016/j.canep.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Inoue M, Iwasaki M, Otani T, Sasazuki S, Noda M, Tsugane S. Diabetes mellitus and the risk of cancer: results from a large-scale population-based cohort study in Japan. Arch Intern Med. 2006;166:1871–1877. doi: 10.1001/archinte.166.17.1871. [DOI] [PubMed] [Google Scholar]
- 120.Khan M, Mori M, Fujino Y, et al. Site-specific cancer risk due to diabetes mellitus history: evidence from the Japan Collaborative Cohort (JACC) Study. Asian Pac J Cancer Prev. 2006;7:253–259. [PubMed] [Google Scholar]
- 121.Khan AE, Gallo V, Linseisen J, et al. Diabetes and the risk of non-Hodgkin’s lymphoma and multiple myeloma in the European Prospective Investigation into Cancer and Nutrition. Haematologica. 2008;93:842–850. doi: 10.3324/haematol.12297. [DOI] [PubMed] [Google Scholar]
- 122.Yang WS, Li HL, Xu HL, et al. Type 2 diabetes and the risk of non-Hodgkin’s lymphoma: a report from two population-based cohort studies in China. Eur J Cancer Prev. 2016;25:149–154. doi: 10.1097/CEJ.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Erber E, Lim U, Maskarinec G, Kolonel LN. Common immune-related risk factors and incident non-Hodgkin lymphoma: the Multiethnic Cohort. Int J Cancer. 2009;125:1440–1445. doi: 10.1002/ijc.24456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Weiderpass E, Gridley G, Ekbom A, Nyren O, Hjalgrim H, Adami HO. Medical history risk factors for non-Hodgkin’s lymphoma in older women. J Natl Cancer Inst. 1997;89:816–817. doi: 10.1093/jnci/89.11.816. [DOI] [PubMed] [Google Scholar]
- 125.Weiderpass E, Gridley G, Persson I, Nyren O, Ekbom A, Adami HO. Risk of endometrial and breast cancer in patients with diabetes mellitus. Int J Cancer. 1997;71:360–363. doi: 10.1002/(sici)1097-0215(19970502)71:3<360::aid-ijc9>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 126.Kitahara CM, Platz EA, Beane Freeman LE, et al. Physical activity, diabetes, and thyroid cancer risk: a pooled analysis of five prospective studies. Cancer Causes Control. 2012;23:463–471. doi: 10.1007/s10552-012-9896-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hemminki K, Forsti A, Sundquist K, Li X. Cancer of unknown primary is associated with diabetes. Eur J Cancer Prev. 2016;25:246–251. doi: 10.1097/CEJ.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 128.Kautzky-Willer A, Kamyar MR, Gerhat D, et al. Sex-specific differences in metabolic control, cardiovascular risk, and interventions in patients with type 2 diabetes mellitus. Gend Med. 2010;7:571–583. doi: 10.1016/j.genm.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 129.Petitti DB, Klingensmith GJ, Bell RA, et al. Glycemic control in youth with diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr. 2009;155:668–672.e661-663. doi: 10.1016/j.jpeds.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Abe R, Yamagishi S. AGE-RAGE system and carcinogenesis. Curr Pharm Des. 2008;14:940–945. doi: 10.2174/138161208784139765. [DOI] [PubMed] [Google Scholar]
- 131.Lorenzi M, Montisano DF, Toledo S, Barrieux A. High glucose induces DNA damage in cultured human endothelial cells. J Clin Invest. 1986;77:322–325. doi: 10.1172/JCI112295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kramer HU, Raum E, Ruter G, et al. Gender disparities in diabetes and coronary heart disease medication among patients with type 2 diabetes: results from the DIANA study. Cardiovasc Diabetol. 2012;11:88. doi: 10.1186/1475-2840-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kirkman MS, Rowan-Martin MT, Levin R, et al. Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care. 2015;38:604–609. doi: 10.2337/dc14-2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bertram MY, Vos T. Quantifying the duration of pre-diabetes. Aust N Z J Public Health. 2010;34:311–314. doi: 10.1111/j.1753-6405.2010.00532.x. [DOI] [PubMed] [Google Scholar]
- 135.Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674–1685. doi: 10.2337/dc10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bansal D, Bhansali A, Kapil G, Undela K, Tiwari P. Type 2 diabetes and risk of prostate cancer: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2013;16:151–158. doi: 10.1038/pcan.2012.40. [DOI] [PubMed] [Google Scholar]
- 137.Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–789. doi: 10.1056/NEJMoa001999. [DOI] [PubMed] [Google Scholar]
- 138.Tsukuma H, Hiyama T, Tanaka S, et al. Risk factors for hepatocellular carcinoma among patients with chronic liver disease. N Engl J Med. 1993;328:1797–1801. doi: 10.1056/NEJM199306243282501. [DOI] [PubMed] [Google Scholar]
- 139.Szmuilowicz ED, Stuenkel CA, Seely EW. Influence of menopause on diabetes and diabetes risk. Nat Rev Endocrinol. 2009;5:553–558. doi: 10.1038/nrendo.2009.166. [DOI] [PubMed] [Google Scholar]
- 140.Shapiro S. Recent epidemiological evidence relevant to the clinical management of the menopause. Climacteric. 2007;10(Suppl 2):2–15. doi: 10.1080/13697130701606754. [DOI] [PubMed] [Google Scholar]
- 141.Peters SA, Huxley RR, Woodward M. Comparison of the sex-specific associations between systolic blood pressure and the risk of cardiovascular disease: a systematic review and meta-analysis of 124 cohort studies, including 1.2 million individuals. Stroke. 2013;44:2394–2401. doi: 10.1161/STROKEAHA.113.001624. [DOI] [PubMed] [Google Scholar]
- 142.Mongraw-Chaffin ML, Peters SA, Huxley RR, Woodward M. The sex-specific association between BMI and coronary heart disease: a systematic review and meta-analysis of 95 cohorts with 1.2 million participants. Lancet Diabetes Endocrinol. 2015;3:437–449. doi: 10.1016/S2213-8587(15)00086-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1.26 MB)
Data Availability Statement
The datasets generated during and/or analysed in the current study are available from the corresponding author on reasonable request.