Abstract
Plantar fasciopathy is very prevalent, affecting one in ten people in their lifetime.
Around 90% of cases will resolve within 12 months with conservative treatment.
Gastrocnemius tightness has been associated with dorsiflexion stiffness of the ankle and plantar fascia injury.
The use of eccentric calf stretching with additional stretches for the fascia is possibly the non-operative treatment of choice for chronic plantar fasciopathy.
Medial open release of approximately the medial third of the fascia and release of the first branch of the lateral plantar nerve has been the most accepted surgical treatment for years.
Isolated proximal medial gastrocnemius release has been reported for refractory plantar fasciopathy with excellent results and none of the complications of plantar fasciotomy.
Cite this article: EFORT Open Rev 2018;3:485-493. DOI: 10.1302/2058-5241.3.170080.
Keywords: plantar fasciitis, heel pain, fasciotomy, gastrocnemius recession
Introduction
Plantar fasciopathy (PF) involves pain and structural changes at the proximal insertion of the plantar fascia in the os calcis. Thickening and degenerative tissue findings are more common than inflammatory changes, so the term ‘plantar fasciopathy’ should better define the disorder known as ‘plantar fasciitis’.
One in ten people will suffer from PF in their lifetime. Around 2 million people worldwide receive treatment every year for this condition.1 We attend around 500 cases of chronic PF in our foot and ankle unit each year, although most cases are possibly managed by primary healthcare practices and do not reach our clinic. Frequently, patients do not look for primary health advice until symptoms are already chronic. Most patients are not referred to the orthopaedic clinic until their symptoms are recalcitrant. The peak incidence of PF occurs in persons aged between 45 and 65 years.1 Around 90% of patients with PF will find that their symptoms resolve within 12 months with conservative treatment.2
In the last 15 years, the focus of non-operative treatment has changed from orthoses and splints to different types of stretching routines. The focus of operative treatment has also changed from understanding the mechanical disturbance caused by plantar fasciotomy, to understanding pathomechanics with risk factors predisposing to PF. Thus, proximal plantar fasciotomy has also given way to gastrocnemius recession as the most common surgical procedure for recalcitrant PF.
The aim of this study was to critically evaluate literature investigating epidemiology, pathomechanics, and management of chronic PF. A search of PubMed, SPORTSDiscus, PEDro, Cochrane Database, CINHAL, and Web of Science was conducted using the search terms “plantar fasciitis”, “plantar fasciopathy”, “heel pain”, “fasciotomy”, and “gastrocnemius recession/release”. Our focus was on articles that provided information on epidemiology, pathomechanics and treatment of chronic PF. Systematic reviews and randomized controlled trials were studied as well as seminal papers that have introduced changes in treatment over the last 30 years.
This review aims to summarize the current literature with special attention to pathomechanics and recent changes in management of chronic PF.
Epidemiology: risk factors
The aetiology of PF is unknown. A number of factors that may increase the risk of suffering from recalcitrant PF have been suggested.3 However, the evidence supporting these factors and their impact in the response to different treatments is unclear. Most of the reviews are not systematic and include foot conditions other than PF.4
Beeson studied the different risk factors for PF.5 Intrinsic factors included age, gender, body weight, heel spurs, nerve entrapment, systemic disease, biomechanical dysfunction, and genetics. Extrinsic factors included footwear, sport, lifestyle, foot/ankle/leg deformities, and occupation.
Age: There is a body of literature on the association of PF with increasing age.5,6 Age-related degenerative changes may cause a decrease in elasticity and in shock-absorbing capabilities, resulting in plantar fascia being more prone to injury.7 Older athletes seem to suffer from PF more often than younger athletes.8
Gender: There is no apparent difference in prevalence between women and men.5
Body weight: Overweight or obese patients have a 1.4-fold increased probability of suffering from chronic PF.9,10
Heel spurs: Calcaneal spurs are apparently formed at the origin of the flexor digitorum brevis muscle and not at the proximal insertion of the plantar fascia. There is insufficient evidence to confirm an association between the presence of a co-existing calcaneal spur and PF. According to a recent study, neither the shape nor size of the spur has a correlation with function or pain before or after treatment.11
Nerve entrapment: Neuritis or nerve entrapments, especially Baxter’s nerve, may be another risk factor for the development of pain that simulates PF. Although a different condition, nerve entrapment can co-exist with PF. Sensory disturbance and radiation of pain is indicative of this condition, which should be suspected when PF does not resolve after surgery.12
Systemic disease: Spondyloarthropathy should be ruled out in patients who are younger than the typical age of presentation of PF and who present with bilateral heel pain.7
Genetics: Genetics may play a role in the progressive contracture of connective tissue. Genetics interacting with other predisposing factors may explain why an individual person is more prone to muscle contractures causing recurrent tendon problems in one location.5
Lifestyle/occupation: Recreational running, military activities, and Irish dancing have been found to be related to PF.6,13,14 Although a significant association between PF and time spent standing at work has been found, no data have been presented on the extent and time of either exposure or the type of occupation of cases and controls.3 Another study considering prolonged weight-bearing as a risk factor found low-quality evidence of an association between weight-bearing tasks and PF.4
Biomechanical dysfunction: Foot/ankle/leg deformities and biomechanical dysfunction may be the underlying cause of recalcitrant PF. Some authors believe that the real association of each of the previous intrinsic and extrinsic factors is the presence of a tight gastrocnemius.15 Most risk factors reviewed may be linked to increasing the degree/rate of an already underlying tight gastrocnemius.
Pathomechanics
In the 1990s, orthopaedic surgeons were worried about the biomechanical complications that could follow plantar fasciotomy, particularly lateral column destabilization and medial arch collapse.16,17 But there was apparently no such wondering about the pathomechanics leading to chronic PF. Around 20 years later there was a growing trend among foot and ankle surgeons of recognizing associated pathology, i.e. isolated gastrocnemius shortening as an underlying abnormality involved in many foot and ankle disorders.18
Patients with planovalgus feet, gastrocnemius contracture and severe hallux valgus are more prone to suffer from PF.16 Diagnosis of gastrocnemius tightness is based on clinical examination with the Silfverskiöld test.19 It is important to correctly perform the Silfverskiöld test by placing the forefoot supinated to eliminate sagittal movement at the midtarsal joints. There is gastrocnemius tightness (positive test) when there is an equinus deformity with the knee extended which disappears when the knee is flexed (Fig. 1).
Fig. 1.

Silfverskiöld test reveals gastrocnemius tightness when there is an equinus deformity with knee extended (a) which disappears when the knee is flexed (b).
Patel and DiGiovanni showed that 83% of patients with recalcitrant PF had limited ankle dorsiflexion.20 In the majority of patients, calf contracture is dependent on gastrocnemius tightness. Several authors have found a significant association between gastrocnemius tightness and PF in different controlled trials.21–23 Gastrocnemius tightness increases Achilles tendon tension and dorsiflexion stiffness of the ankle, thus increasing plantar fascia tension during weight-bearing activities. Damaging forces appear when leveraged forces are transmitted to the foot and ankle as the tibia (and the body) passes over the planted foot.24 Shortening of the gastrocnemius, congenital or acquired, is the most common cause of the lack of ankle joint dorsiflexion. During the late part of the second rocker of gait (just before heel lift) ankle dorsiflexion should be coupled with full knee extension. If the gastrocnemius is tight, the combination of hindfoot plantarflexion moments and forefoot dorsiflexion moments exerted by the muscle tension increases plantar fascia passive longitudinal tension counteracting the arch-flattening effect of gastrocnemius tightness.25 Patients with a short gastrocnemius and PF tend to adopt an antalgic gait and compensate for lack of ankle dorsiflexion with external rotation of the leg/foot and a characteristic limp (‘bouncy gait’). As a result of taking around 7000 steps per day, the plantar fascia is injured, victim to a subtle repetition of the damaging longitudinal tension moments (Fig. 2).
Fig. 2.
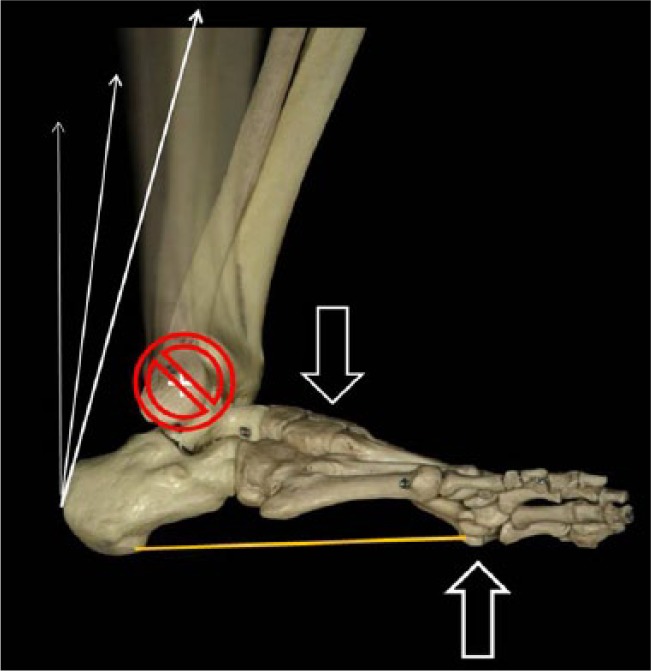
At the end of the second rocker of gait, in the presence of a tight gastrocnemius, repetition of subtle longitudinal tension moments may result in injury to the plantar fascia.
Clinical presentation
Diagnosis is clinical and patients suffering from PF typically present with ‘start-up pain’, a sharp pain at the plantarmedial aspect of the heel on first walking in the morning and after a period of rest that gets better after walking for a while. It usually worsens at the end of the day and with impact sports and activities.7 Peak incidence is between 45 and 65 years of age and one in three patients will present bilateral PF. Tenderness on examination is located at the plantar aspect of the medial calcaneal tuberosity around the fascia insertion in the os calcis. Tinel’s sign and altered sensations should be tested behind the medial malleolus to rule out the diagnosis of tarsal tunnel syndrome. Tenderness on calcaneal squeeze may suggest a calcaneal stress fracture or Haglund disease and these conditions should be further investigated.26
Image and other studies
Plain weight-bearing x-rays may reveal the presence of heel spurs. Although there is a higher incidence of heel spurs in patients suffering from PF (75% vs 63% in asymptomatic patients) there is no apparent correlation between spurs and pain.27 Ultrasonography scanning and magnetic resonance imaging (MRI) are useful to rule out other disorders and atypical findings around the heel (calcaneal stress fracture, tumours). Thickening of the plantar fascia may be measured, although there is no apparent significant correlation between thickness and pain.26 Laboratory tests should be performed to rule out underlying endocrine and inflammatory conditions, especially in bilateral cases.
Treatment
Approximately 90% of patients with PF can be successfully treated without surgery. Numerous treatment options exist but limited Level-I or Level-II-evidence studies are available to suggest an optimal treatment for recalcitrant PF (Table 1).28 Both non-operative and operative management is based mostly on Level-III and Level-IV-evidence studies. DiGiovanni et al studied the preferred non-operative and operative treatment of recalcitrant PF among a group of orthopaedic foot and ankle surgeons.29 At 4 months of symptoms, most surgeons chose plantar-fascia-specific stretching. At 10 months, most respondents chose surgery or extracorporeal shock wave therapy as the next step in treatment. When it came to the choice of surgical treatment, there was a considerable heterogeneity of operative techniques for chronic PF that suggests higher levels of evidence studies are needed.
Table 1.
American Academy of Orthopaedic Surgeons (AAOS) levels of evidence and grades of recommendation
| Levels of evidence | Grades of recommendation |
|---|---|
| Level I: High-quality randomized controlled trial (RCT) Systematic review of Level-I RCTs |
Grade A: Supported by good evidence (Level-I studies with consistent findings) for or against recommending intervention |
| Level II: Lesser-quality RCT Prospective comparative study Systematic review of Level-II studies |
Grade B: Supported by fair evidence (Level-II or Level-III studies with consistent findings) for or against recommending intervention |
| Level III: Case control study Retrospective comparative study Systematic review of Level-III studies |
Grade C: Conflicting or poor quality evidence (Level-IV or Level-V studies) not allowing a recommendation for or against intervention |
| Level IV: Case series |
Grade I: Insufficient evidence to make a recommendation |
| Level V: Expert opinion |
Source: Adapted from AAOS.28
PF may be a disabling condition and frustrating for both the patient and the orthopaedic surgeon. Despite the progress made with different conservative treatments, controversy still exists on how to proceed with a patient suffering from chronic PF.
Non-operative treatment
The most useful conservative treatment for PF is explaining to patients that pain will possibly settle over time and managing patient expectations. Some therapies focus on the proximal insertion of the fascia (orthoses, injections, shock wave therapies) while others (night splints, stretching) address the relationship between gastrocnemius tension and the plantar fascia during weight-bearing activities
Orthoses and splints: Mechanical treatments affecting loading of the plantar fascia have been extensively used for the treatment of PF. Foot orthoses aiming to decrease pronation and off-load the proximal insertion of the fascia have been studied.30 A randomized, controlled study (Level I) comparing over-the-counter shoe inserts with customized shoe inserts found no significant difference in pain relief between the two groups at 12-month follow-up.31 Nocturnal splints are applied to stretch the fascia to prevent morning stiffness and pain.32 Several high-level studies support the use of night splints, but poor patient tolerance may be an issue for compliance.32–35
Injections: One or more injections of cortisone and local anaesthetics may result in variable responses and duration of relief. Multiple injections may increase the risk of rupture of the plantar fascia and fat pad atrophy. Controlled, randomized clinical trials demonstrated low-quality evidence of moderate short-term positive effects of cortisone injections when compared to a placebo, but they usually lasted no more than 1 month.2,36 Potential complications of fat pad atrophy and plantar fascia rupture together with limited results are in contrast with the wide use of cortisone injections for PF worldwide. Other injection therapies that have also been shown to have short-term and variable benefits include hyperosmolar dextrose, botulinum toxin A, and autologous blood.37–40
Platelet-rich plasma (PRP): A recent systematic review of published literature for studies comparing PRP injections and corticosteroid injections for PF shows PRP injections were associated with improved pain and function at 3-month follow-up when compared with corticosteroid injections.41 But there was no information regarding either relative adverse event rates or costs. The authors concluded that large-scale, high-quality, randomized controlled trials with blinding of outcome assessment and longer follow-up were required.
Extracorporeal shock wave therapy (ECSWT): Some well-designed Level-I clinical studies have shown ECSWT to be effective in the treatment of PF.42–45 In a recent meta-analysis on the efficacy of the different variants of ECSWT, nine studies involving 935 patients were included.46 It was suggested that focused shock wave (FSW) can relieve pain but no firm conclusions of general ECSWT and radial shock wave (RSW) effectiveness can be drawn. Radial shock wave is dispersed from the applicator and does not concentrate on the tissue as FSW does. However, other authors showed there was a considerably lower success rate of ECSWT in patients with gastrocnemius shortening.27 There are also concerns regarding availability and costs of this therapy, with different insurance companies not covering ECSWT in our practice.
Strengthening exercises
Atrophy of intrinsic foot muscles has been associated with symptoms of PF in runners by destabilizing the medial longitudinal arch.47 In a randomized controlled single-blind clinical trial, 83 patients with PF were allocated to one of three treatment options – extrinsic and intrinsic foot muscles; abductor and lateral rotator hip muscles; and stretching alone – for an 8-week period. All three protocols led to improvements at 8-week follow-up in pain and function in patients with PF.48 However, in a systematic review of the literature regarding strength training for PF, it was not possible to identify the extent to which strengthening interventions for intrinsic musculature may benefit symptomatic or at-risk PF populations.49
Stretching exercises
There is evidence that increased plantar fascia strain is associated with increased calf tension.50 Calf-stretching exercises with eccentric loading, widely considered to be the most effective conservative treatment for non-insertional Achilles tendinopathy, also work well for recalcitrant PF.51,52 A prospective, randomized, double-blinded study compared two calf-stretching regimens for PF and it was confirmed that Achilles stretching alone was an effective treatment.53 Several Level-I and Level-II clinical studies demonstrate the efficacy of home-based plantar-fascia-specific stretching.51,52,54
In a recent meta-analysis, although several therapies (ECSWT, laser therapy, orthoses, pulsed radiofrequency, dry-needling, and calcaneal taping) seemed effective when compared to placebo, improvements were very small, and quality of evidence was low or moderate for most interventions and no conclusions were drawn to be considered in clinical practice.55 At present the use of eccentric calf stretching (as popularized by Alfredson et al) with additional stretches for the fascia is possibly the first-line choice in non-operative treatment for chronic PF.51,52,56
Operative treatment
Because of the self-limiting condition of PF and the high rate of success with conservative treatment, non-operative measures should be exhausted before surgery is considered. Around 95% of patients with PF will be pain-free within around 12 months so surgery should not be considered until 12 months have elapsed.57 At present, operative treatment is directed by case series and retrospective reviews (Level-III and Level-IV evidence) and the design of most of the studies undermines most intended comparisons between different modalities of treatment. The combination of open plantar fascia release combined with the release of the first branch of the lateral plantar nerve, dating back to the mid-1980s, is a popular approach among orthopaedic surgeons.58 But in the last 10 years, with a better understanding of the pathomechanics underlying PF, there is a growing trend towards the use of gastrocnemius release as an isolated procedure to treat recalcitrant PF.
Nerve decompression
Entrapment of the first branch of the lateral plantar nerve has been advocated as a cause of PF in some patients with sensory and motor symptoms over the abductor digiti quinti muscle.58 The release of the nerve is commonly associated with plantar fascia release in recalcitrant PF.29
Fasciotomy
Plantar proximal fasciotomy has been the most common surgical procedure for PF for a long time, but controversy still exists over the different techniques that may be used (open, endoscopic, minimal incision) as well as over the amount of fascia that should be cut.
In the early 1990s, all surgical procedures comprised a release of the plantar fascia but there was no consensus over the amount of fascia to be incised. Barret and Day advocated the complete resection of the plantar fascia.59 However, 2 years later the same authors recommended the release of the medial 2/3 of the fascia.60 Four years from their initial recommendation their final advice was to release the medial 1/3 of the fascia.61 The reason for the change in amount of the release was the potential complication of lateral column destabilization via the disruption of the locking mechanism for the calcaneocuboid joint. The windlass mechanism may also be affected by proximal fascia release.17
Kitaoka showed that complete fasciotomy was the standard technique in 21 clinical studies (1963–1995) with only two surgeons advocating partial fasciotomy.16 Plantar fasciotomy in normal feet did not lead directly to obvious flatfoot deformity but fasciotomy influenced tarsal bone motion significantly. The increased joint motion after fasciotomy might indicate that the fascia contributes substantially to stabilizing intertarsal joints. The most marked changes in joint rotation and arch displacement occurred in unstable feet with pre-existing arch instability. These findings suggest that the plantar fascia should not be surgically sectioned with impunity, as this may have an effect on stability of the foot, particularly in patients with flat feet.
Medial open approach with the release of approximately the medial third of the fascia has been the most accepted surgical treatment for a long time (Fig. 3). Direct open approach to the plantar fascia through a direct plantar incision was associated with no morbidity relating to the sensory nerves or the heel pad.62 Long-term results of complete plantar fascia release via transverse heel pad incision were around 75% relief of symptoms.
Fig. 3.

Medial open approach with proximal partial fasciotomy.
Endoscopic release of the plantar fascia appeared to obtain results as good as with open release but with considerably fewer complications.63,64 The more common indication to release the first branch of the lateral plantar nerve under careful dissection in recent years may explain the lack of popularity of endoscopic approaches.
Spur removal has been associated with fasciotomy in several studies.57,59,65 But excessive spur removal led to calcaneal stress fractures in four patients in a study by Manoli et al.66
Radiofrequency coblation has been proposed as a minimally invasive treatment modality for chronic PF. By inducing tissue destruction with minimal thermal damage, healing through controlled inflammation and focal angiogenesis was expected. But no significant differences were found in patients who underwent plantar fasciotomy, radiofrequency microtenotomy, or both procedures.67,68
The most common complications arising from plantar fasciotomy include instability of the lateral column which may lead to sinus tarsi pain, metatarsalgia, secondary pes planus, stress fractures, continued pain due to Baxter’s nerve entrapped in fibrotic tissue and hypertrophic painful scarring.16,17,62 These complications may explain why fasciotomy for PF is not always clinically successful, with 10% to 50% of patients unsatisfied after surgery.57 Patients should also know that the average time of recovery from plantar fasciotomy is around 7 months.57,69 This scenario, together with the understanding of foot biomechanics, led to the development of a new approach to the surgical treatment of chronic PF around the early 2000s.
Gastrocnemius release
In the early 2000s, DiGiovanni and colleagues noted PF to be related to an isolated gastrocnemius contracture.18 Barouk et al reported a safe and simple surgical technique for the proximal release of the gastrocnemius and communicated excellent results for chronic PF.70 The procedure could be performed under local anaesthesia with sedation and patients mobilized immediately after surgery (Fig. 4). The wound healed well and was free from the complications seen with the Strayer release (risk of weakness caused by overlengthening, lengthy rehabilitation). So if the contracture was confined to the gastrocnemius, proximal gastrocnemius release was safer than Strayer. In 2009, Solan’s group studied the relative contribution of each of the gastrocnemius heads for an effective release and found the medial head to be the major contributing factor.71 The proximal medial head of the gastrocnemius could be accessed safely at the medial crease of the popliteal fossa (Fig. 5).
Fig. 4.
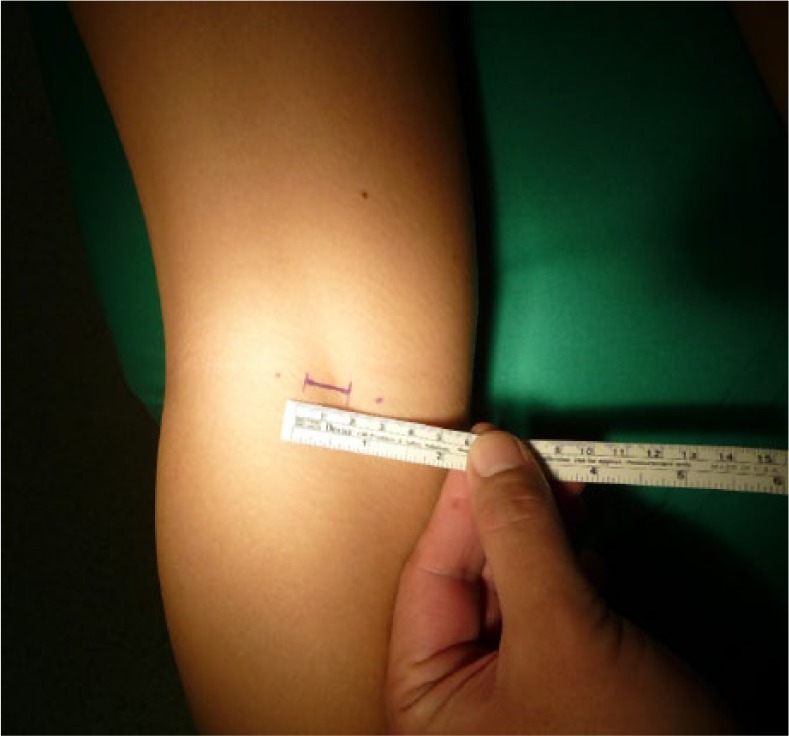
Surgical approach for proximal medial gastrocnemius release at the popliteal fossa.
Fig. 5.
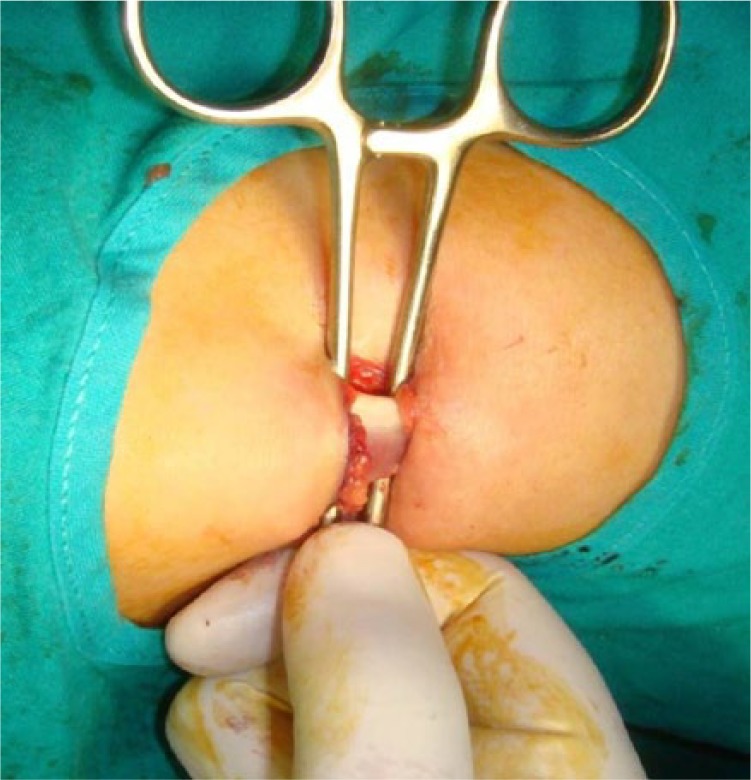
With the help of a blunt instrument, the proximal medial gastrocnemius head is exposed to be safely released.
Kohls-Gatzoulis and Solan corroborated the efficacy of isolated proximal gastrocnemius release for the treatment of recalcitrant PF.72 In 2010, Maskill et al reported good results of gastrocnemius recession at the musculotendinous junction to treat different cases of foot pain (metatarsalgia and PF).73 Isolated proximal medial gastrocnemius release has been reported for refractory PF with excellent results.74 At an average of 24 months from surgery, 17 of the 21 patients (81%) reported total or significant pain relief. It is interesting to note that 10 (58%) noticed this improvement within 1 to 2 weeks of their gastrocnemius release. The remaining seven reported a progressive improvement over 3 to 6 months postoperatively. Fifteen patients (88%) would recommend this procedure to a friend. There were no major complications with just one minor wound problem that resolved uneventfully.
Proximal medial gastrocnemius release has been associated with lower complication rates than plantar fasciotomy in a Level-III study.75 The authors retrospectively reviewed 60 patients who had undergone surgery for chronic PF over a 4-year period. Thirty patients had an isolated open partial proximal fasciotomy and 30 had an isolated proximal medial gastrocnemius release. Pain relief and patient satisfaction were higher in the gastrocnemius release cohort at an average of 12 months from surgery. Only 45% of patients in the fasciotomy group would recommend the procedure to a close friend, and 35% would undergo the same surgery if they had a recalcitrant PF in the contralateral foot. Ninety-five per cent of patients in the gastrocnemius release group would recommend the procedure and 95% would undergo the same surgery for their contralateral leg. It is interesting to note that about 20% of those who improved with gastrocnemius release did so within 1 week of surgery, about 60% between weeks one and eight, and the remaining 20% of improvements appeared between the second and the sixth months from surgery. In the fasciotomy group, none of the patients noticed improvement within 6 weeks of their surgery.
Evidence-based literature on gastrocnemius tightness and release has more than doubled from the review by Barske et al in 2012.76 Cychosz et al assigned grades of recommendation to gastrocnemius recession as a therapeutic intervention for different foot and ankle conditions. Based on different Level-III, IV, and V studies, gastrocnemius recession received a Grade B (fair evidence) recommendation for the treatment of midfoot or forefoot overload.77
Conclusions
Pain at the proximal insertion of the plantar fascia is a common foot condition treated by orthopaedic surgeons worldwide and is prevalent in both athletic and non-athletic populations. Chronic PF is a self-limiting condition that responds to conservative treatment in almost 90% of patients within 9 to 12 months from the onset of symptoms.
The specific cause of PF is poorly understood and multifactorial. Altered biomechanics is believed to contribute to the onset of this condition through a decreased ankle joint range of motion. Reduced dorsiflexion of the ankle is possibly the most important risk factor for the development of chronic PF. Gastrocnemius tightness has been implicated in several foot and ankle conditions, including PF. Isolated gastrocnemius tightness has been associated with failure of conservative measures. In this context, the use of eccentric calf stretching with additional stretches for the fascia is nowadays possibly the non-operative treatment of choice for chronic PF.
When conservative management fails, proximal partial fasciotomy is the most common surgical procedure performed. But success rates following plantar fascia release are variable. High-quality evidence to support the surgical release of the plantar fascia alone or in combination with the release of the first branch of the lateral plantar nerve is lacking.
Over the last 10 years, isolated proximal medial gastrocnemius release has been the preferred technique for most patients because it has low morbidity, it can be performed under local anaesthesia with sedation, and recovery is rapid. Although already a safer and more effective procedure than fasciotomy, further high-quality studies are needed to build a larger base of evidence. Large-scale randomized controlled trials with longer follow-up are needed to fully explore the long-term efficacy of gastrocnemius release vs plantar fasciotomy in the treatment of chronic PF. Perhaps those studies might allow us to understand why 5–10% of patients do not show resolution of symptoms after surgery and might provide valuable evidence to guide clinical and surgical decision-making in chronic PF.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int 2004;25:303–310. [DOI] [PubMed] [Google Scholar]
- 2. Crawford F, Thompson CE. Interventions for treating plantar heel pain. Cochrane Database Syst Rev 2003;3:CD000416. [DOI] [PubMed] [Google Scholar]
- 3. Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg Am 2003;85:872–877. [DOI] [PubMed] [Google Scholar]
- 4. Wackawski ER, Beach J, Milne A, Yacyshyn E, Dryden DM. Systematic review: plantar fasciitis and prolonged weight bearing. Occup Med (Lond) 2015;65:97–106. [DOI] [PubMed] [Google Scholar]
- 5. Beeson P. Plantar fasciopathy: revisiting the risk factors. Foot Ankle Surg 2014;20:160–165. [DOI] [PubMed] [Google Scholar]
- 6. Scher DL, Belmont PJ, Jr, Bear R, et al. The incidence of plantar fasciitis in the United States military. J Bone Joint Surg Am 2009;91:2867–2872. [DOI] [PubMed] [Google Scholar]
- 7. Barouk LS, Baudet B, Bonnel F, et al. Gastrocnemius tightness: from anatomy to treatment. Montpellier: Sauramps Médical, 2012. [Google Scholar]
- 8. Petraglia F, Ramazzina I, Costantino C. Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review. Muscles Ligaments Tendons J 2017;10:107–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Frey C, Zamora J. The effects of obesity on orthopaedic foot and ankle pathology. Foot Ankle Int 2007;28:996–999. [DOI] [PubMed] [Google Scholar]
- 10. Van Leeuwen KD, Rogers J, Winzenberg T, van Middelkoop M. Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: systematic review and meta-analysis of various clinical and imaging risk factors. Br J Sports Med 2016;50:972–981. [DOI] [PubMed] [Google Scholar]
- 11. Ahmad J, Karim A, Daniel JN. Relationship and classification of plantar heel spurs in patients with plantar fasciitis. Foot Ankle Int 2016;37:994–1000. [DOI] [PubMed] [Google Scholar]
- 12. Ferkel E, Davis WH, Ellington JK. Entrapment neurophaties of the foot and ankle. Clin Sports Med 2015;34:791–801. [DOI] [PubMed] [Google Scholar]
- 13. Sobhani S, Dekker R, Postema K, Dijkstra PU. Epidemiology of ankle and foot overuse injuries in sports: a systematic review. Scand J Med Sci Sports 2013;23:669–686. [DOI] [PubMed] [Google Scholar]
- 14. Noon M, Hoch AZ, McNamara L, Schimke J. Injury patterns in female Irish dancers. PM R 2010;2:1030–1034. [DOI] [PubMed] [Google Scholar]
- 15. Amis J. The gastrocnemius: a new paradigm for the human foot and ankle. Foot Ankle Clin N Am 2014;19:637–647. [DOI] [PubMed] [Google Scholar]
- 16. Kitaoka HB, Luo ZP, An KN. Mechanical ulticent of the foot and ankle after plantar fascia release in the unstable foot. Foot Ankle Int 1997;18:1–15. [DOI] [PubMed] [Google Scholar]
- 17. Thordarson DB, Kumar PJ, Hedman TP, Ebramzadeh E. Effect of partial versus complete plantar fasciotomy on the windlass mechanism. Foot Ankle Int 1997;18:16–20. [DOI] [PubMed] [Google Scholar]
- 18. DiGiovanni CW, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. J Bone Joint Surg [Am] 2002;84(A):962–970. [DOI] [PubMed] [Google Scholar]
- 19. Silfverskiöld N. Reduction of the uncrossed two-joint muscles of the leg to one joint muscles in spastic conditions. Acta Chir Scand 1923;56:315–330. [Google Scholar]
- 20. Patel A, DiGiovanni B. Association between plantar fasciitis and isolated contracture of the gastrocnemius. Foot Ankle Int 2011;32:5–8. [DOI] [PubMed] [Google Scholar]
- 21. Labovitz JM, Yu J, Kim C. The role of hamstring tightness in plantar fasciitis. Foot Ankle Spec 2001;4:141–144. [DOI] [PubMed] [Google Scholar]
- 22. Harty J, Soffe K, O’Toole G, Stephens MM. The role of hamstring tightness in plantar fasciitis. Foot Ankle Int 2005;26:1089–1092. [DOI] [PubMed] [Google Scholar]
- 23. Bolivar YA, Munuera PV, Padillo JP. Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot Ankle Int 2013;34:42–48. [DOI] [PubMed] [Google Scholar]
- 24. Amis J. The split second effect: the mechanism of how equinus can damage the human foot and ankle. Front Surg 2016;3:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pascual-Huerta J. The effect of the gastrocnemius on the plantar fascia. Foot Ankle Clin 2014;19:701–718. [DOI] [PubMed] [Google Scholar]
- 26. Toomey EP. Plantar heel pain. Foot Ankle Clin 2009;14:229–245. [DOI] [PubMed] [Google Scholar]
- 27. Solan MC, Carne A, Davies MS. Gastrocnemius shortening and heel pain. Foot Ankle Clin 2014;19:719–738. [DOI] [PubMed] [Google Scholar]
- 28. No authors listed. American Academy of Orthopaedic Surgeons (AAOS). http://www2.aaos.org/bulletin/apr05/fline9.asp (date last accessed 03 May 2017).
- 29. DiGiovanni BF, Moore AM, Zlotnicki JP, Pinney SJ. Preferred management of recalcitrant plantar fasciitis among orthopaedic foot and ankle surgeons. Foot Ankle Int 2012;33:507–512. [DOI] [PubMed] [Google Scholar]
- 30. Rasenberg N, Fuit L, Poppe E, et al. The STAP-study: the (cost) effectiveness of custom made orthotic insoles in the treatment for plantar fasciopathy in general practice and sports : design of a randomized controlled trial. BMC Musculoskelet Disord 2016;16:17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med 2006;166:1305–1310. [DOI] [PubMed] [Google Scholar]
- 32. Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int 2006;27:606–611. [DOI] [PubMed] [Google Scholar]
- 33. Batt ME, Tanji SL, Skattum N. Plantar fasciitis: a prospective randomized clinical trial of the tension night splint. Clin J Sport Med 1996;6:158–162. [PubMed] [Google Scholar]
- 34. Powell M, Post WR, Keener J, et al. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized outcome study. Foot Ankle Int 1998;19:10–18. [DOI] [PubMed] [Google Scholar]
- 35. Probe RA, Baca M, Adams R, Preece C. Night splint treatment for plantar fasciitis: a prospective randomized study. Clin Orthop Relat Res 1999;368:190–195. [PubMed] [Google Scholar]
- 36. David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev 2017;11:CD009348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ryan M, Hartwell J, Fraser S, Newsham-West R, Taunton J. Comparison of a physiotherapy program versus dexamethasone injections for plantarfasciopathy in prolonged standing workers: a randomized clinical trial. Clin J Sport Med 2014;24:211–217. [DOI] [PubMed] [Google Scholar]
- 38. Babcock MS, Foster L, Pasquina P, Jabbari B. Treatment of pain attributed to plantar fasciitis with botulinum toxin A: a short-term, randomized, placebo-controlled, double-blind study. Am J Phys Med Rehabil 2005;84:649–654. [DOI] [PubMed] [Google Scholar]
- 39. Kalaci A, Cakici H, Hapa O, et al. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc 2009;99:108–113. [DOI] [PubMed] [Google Scholar]
- 40. Wheeler P. Autologous blood injections for chronic plantar fasciitis: a pilot case-series study shows promising results. Int Musculoskelet Med 2013;35:3–7. [Google Scholar]
- 41. Singh P, Madanipour S, Bhamra JS, Gill I. A systematic review and meta-analysis of platelet-rich plasma versus corticosteroid injections for plantar fasciopathy. Int Orthop 2017;41:1169–1181. [DOI] [PubMed] [Google Scholar]
- 42. Buchbinder R, Ptasznik R, Gordon J, et al. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA 2002;288:1364–1372. [DOI] [PubMed] [Google Scholar]
- 43. Odgen J, Alvarez RG, Cross GL, Jaakkola JL. Plantar fasciopathy and Orthotripsy: the effect of prior cortisone injection. Foot Ankle Int 2005;26:231–233. [DOI] [PubMed] [Google Scholar]
- 44. Gerdesmeyer L, Frey C, Vester J, et al. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled ulticentre study. Am J Sports Med 2008;36:2100–2109. [DOI] [PubMed] [Google Scholar]
- 45. Agil A, Siddiqui MR, Solan M, et al. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Clin Orthop Relat Res 2013;471:3645–3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sun J, Gao F, Wang Y, et al. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Medicine (Baltimore) 2017;96:e6621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cheung RT, Sze LK, Mok MW, Ng GY. Intrinsic foot muscle volume in experienced runners with and without chronic plantar fasciitis. J Sci Med Sport 2016;19:713–715. [DOI] [PubMed] [Google Scholar]
- 48. Kamonseki DH, Gonçalves GA, Yi LC, Júnior IL. Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: a randomized controlled single-blind clinical trial. Man Ther 2016;23:76–82. [DOI] [PubMed] [Google Scholar]
- 49. Huffer D, Hing W, Newton R, Clair M. Strength training for plantar fasciitis and the intrinsic foot musculature: a systematic review. Phys Ther Sport 2017;24:44–52. [DOI] [PubMed] [Google Scholar]
- 50. Carlson RE, Fleming LL, Hutton WC. The biomechanical relationship between the tendoachilles, plantar fascia and metatarsophalangeal joint dorsiflexion angle. Foot Ankle Int 2000;21:18–25. [DOI] [PubMed] [Google Scholar]
- 51. DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: a prospective, randomized study. J Bone Joint Surg Am 2003;85:1270–1277. [DOI] [PubMed] [Google Scholar]
- 52. DiGiovanni BF, Nawoczenski DA, Malay DP. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up. J Bone Joint Surg Am 2006;88:1775–1781. [DOI] [PubMed] [Google Scholar]
- 53. Porter D, Barrill E, Oneacre K, et al. The effects of duration and frequency of Achilles tendon stretching on dorsiflexion and outcome in painful heel syndrome: a randomized, blinded, control study. Foot Ankle Int 2002;7:619–624. [DOI] [PubMed] [Google Scholar]
- 54. Flanigan RM, Nawoczenski DA, Chen L, et al. The influence of foot position on stretching of the plantar fascia. Foot Ankle Int 2007;28:815–822. [DOI] [PubMed] [Google Scholar]
- 55. Salvioli S, Guidi M, Marcotulli G. The effectiveness of conservative, non-pharmacological treatment, of plantar heel pain: a systematic review with meta-analysis. Foot 2017;33:57–67. [DOI] [PubMed] [Google Scholar]
- 56. Alfredson H, Pietila T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 1998;26:360–366. [DOI] [PubMed] [Google Scholar]
- 57. Davies MS, Weiss GA, Saxby TS. Plantar fasciitis: how successful is surgical intervention? Foot Ankle Int 1999;20:803–807. [DOI] [PubMed] [Google Scholar]
- 58. Baxter DE, Thigpen CM. Heel pain-operative results. Foot Ankle 1984;5:16–25. [DOI] [PubMed] [Google Scholar]
- 59. Barret SL, Day SV. Endoscopic plantar fasciotomy for chronic plantar fasciitis/heel spur syndrome: surgical technique – early clinical results. J Foot Surg 1991;30:568–570. [PubMed] [Google Scholar]
- 60. Barret SL, Day SV. Endoscopic plantar fasciotomy: two portal endoscopic surgical techniques – clinical results of 65 procedures. J Foot Ankle Surg 1993;32:248–256. [PubMed] [Google Scholar]
- 61. Barret SL, Day SV, Pignetti TT, Robinson LB. Endoscopic plantar fasciotomy: a multi-surgeon prospective analysis of 652 cases. J Foot Ankle Surg 1995;34:400–406. [DOI] [PubMed] [Google Scholar]
- 62. Brown JN, Roberts S, Taylor M, Paterson RS. Plantar fascia release through a transverse plantar incision. Foot Ankle Int 1999;20:364–367. [DOI] [PubMed] [Google Scholar]
- 63. Hofmeister EP, Elliot MJ, Juliano PJ. Endoscopic plantar release: an anatomical study. Foot Ankle Int 1995;16:719–723. [DOI] [PubMed] [Google Scholar]
- 64. Bader L, Park K, Gu Y, O’Malley MJ. Functional outcome of endoscopic plantar fasciotomy. Foot Ankle Int 2012;33:37–43. [DOI] [PubMed] [Google Scholar]
- 65. Kinley S, Frascone S, Calderone D, et al. Endoscopic plantar fasciotomy versus traditional heel spur surgery: a prospective study. J Foot Ankle Surg 1993;32:595–603. [PubMed] [Google Scholar]
- 66. Manoli A, Harper MC, Fitzgibbons TC, McKernan DJ. Calcaneal fracture after cortical bone removal. Foot Ankle 1992;13:523–525. [DOI] [PubMed] [Google Scholar]
- 67. Chou AC, Ng SY, Su DH, Singh IR, Koo K. Radiofrequency microtenotomy is as effective as plantar fasciotomy in the treatment of recalcitrant plantar fasciitis. Foot Ankle Surg 2016;22:270–273. [DOI] [PubMed] [Google Scholar]
- 68. Tay KS, Ng YC, Singh IR, Chong KW. Open technique is more effective than percutaneous technique for TOPAZ radiofrequency coblation for plantar fasciitis. Foot Ankle Surg 2012;18:287–292. [DOI] [PubMed] [Google Scholar]
- 69. Sammarco GJ, Helfrey RB. Surgical treatment of recalcitrant plantar fasciitis. Foot Ankle Int 1996;17:520–526. [DOI] [PubMed] [Google Scholar]
- 70. Barouk LS, Barouk P, Toulec E. Resultats de la liberation proximale des gastrocnemiens. Etude prospective symposium ‘Brieveté des gastrocnemiens’, journées de Printemps SFMCP-AFCP, Toulouse Med Chir Pied 2006;22:151–156. [Google Scholar]
- 71. Hamilton PD, Brown M, Ferguson N, et al. Surgical anatomy of the proximal release of the gastrocnemius: a cadaveric study. Foot Ankle Int 2009;30:1202–1206. [DOI] [PubMed] [Google Scholar]
- 72. Kohls-Gatzoulis JA, Solan M. Results of proximal medial gastrocnemius release. J Bone Joint Surg Br 2009;91-B:361.19258613 [Google Scholar]
- 73. Maskill JD, Bohay DR, Anderson JG. Gastrocnemius recession to treat isolated foot pain. Foot Ankle Int 2010;31:19–23. [DOI] [PubMed] [Google Scholar]
- 74. Abbassian A, Kohls-Gatzoulis J, Solan MC. Proximal medial gastrocnemius release in the treatment of recalcitrant plantar fasciitis. Foot Ankle Int 2012;33:14–19. [DOI] [PubMed] [Google Scholar]
- 75. Monteagudo M, Maceira E, García-Virto V, Canosa R. Chronic plantar fasciitis: plantar fasciotomy versus gastrocnemius recession. Int Orthop 2013;37:1845–1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Barske HL, DiGiovanni BF, Douglass M, Nawoczenski DA. Current concepts review: isolated gastrocnemius contracture and gastrocnemius recession. Foot Ankle Int 2012;33:915–921. [DOI] [PubMed] [Google Scholar]
- 77. Cychosz CC, Phisitkul P, Belatti DA, Glazebrook MA, DiGiovanni CW. Gastrocnemius recession for foot and ankle conditions in adults: evidence-based recommendations. Foot Ankle Surg 2015;21:77–85. [DOI] [PubMed] [Google Scholar]


