Abstract
Objective
Inguinoscrotal hernia (ISH) of the bladder is a rare condition involved in less than 4% of inguinal hernias. In most cases, it occurs to men older than 50 years who are overweight. Little is known about the subject and mainly based on case reports. When undiagnosed, it may be associated with bladder injuries during hernia repair. There is also no consensus on the ideal repair technique to use. The aim of the study is to evaluate the particularity of the management of the inguinal herniation of the bladder in term of diagnosis, choice and results of treatments.
Methods
A Prisma systematic review of the literature was performed over the last 10 years using a database. We selected 51 articles including 64 patients with ISH of the bladder.
Results
ISH of the bladder mainly occurred in overweight men aged over 50 years (Body Mass Index >30). Symptoms were reported for 76% of the patients (n=49), including inguinal swelling 60% of cases (n=38), lower urinary tract symptoms (48%), pain (40%) and a reduction of an inguinal mass after voiding (12.7%). Diagnosis was incidental on imaging for 7 patients, during inguinal repair surgery for 8, or on imaging performed following symptoms for the remaining 49 patients. Surgical repair was reported for 46 patients (71%) including various procedures as open surgery (80%) and laparoscopic approaches (20%). Excellent short term results were reported.
Conclusion
ISH of the bladder seams more likely to occur with patients suffering from lower urinary tract obstruction and best diagnosed with a computerized tomography scan. Various surgical techniques are reported.
Keywords: Inguinoscrotal hernia, review, urinary bladder
Introduction
Inguinoscrotal hernia (ISH) of the bladder is a rare event which is involved in less than 4% of inguinal hernias.[1,2] This disease was first described in 1951 by Levine.[3] It usually develops without specific symptoms that’s why it is discovered in less than 10% of cases prior to an operation and less than 20% during surgical intervention.[4,5] Clinical presentations are very different from one patient to another but symptoms generally include inguinal pain or swelling associated with voiding or storage lower urinary tract symptoms (LUTS) directly linked to the inguinal bladder hernia or antecedent of prostate hyperplasia. Otherwise, an inguinal swelling alone, not necessarily painful, can be observed. In most cases, the ISH of the bladder occurs in overweight men older than 50 years.[6] ISH is a benign affection but complications might occur and should be recognized. Because of its rareness and the lack of standardization for surgical repair, literature is very scarce about this disease. We performed an extended review of the literature on ISH of the bladder, focusing on the symptoms observed during physical examination, possible related complications, imaging and surgical management.
Material and methods
A Prisma systematic review of the literature was performed in April 2017 for the last 10 years. Database were searched with the following criteria (Figure 1): (“inguinal hernia”) AND (“bladder”) AND (“repair”) AND (“inguinoscrotal hernia”). We found 62 articles using PubMed and including 74 patients from September 2005 to April 2017. Out of the 62 articles, we excluded 9 that lacked a summary or were not published in English, and 1 on rabbits. Finally, we selected 51 articles including 64 patients. Articles were mostly case reports or small retrospective studies.
Figure 1.
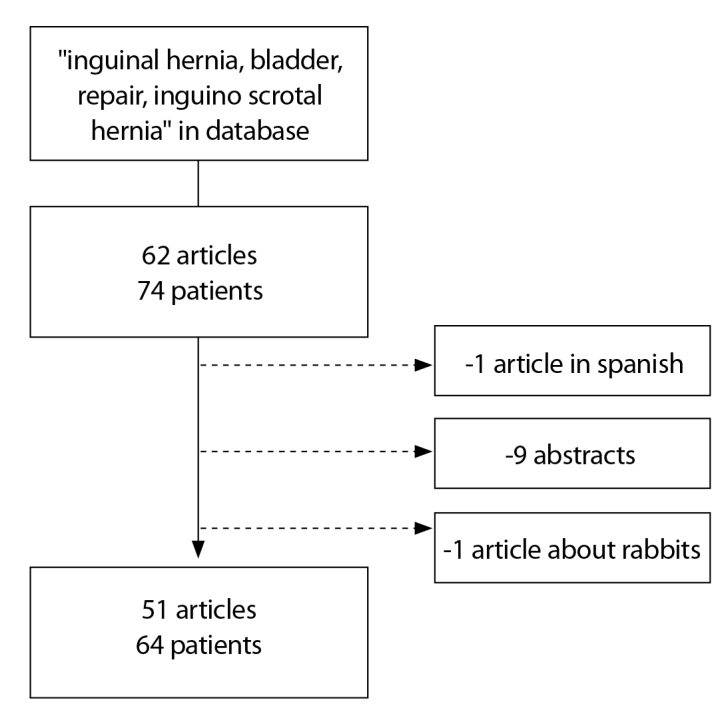
Flowchart
Qualitative variables were described as percentages of the whole population.
Results
1. Physical examination and symptoms (Table 1)
Table 1.
Patients characteristics
| Patients | n | % |
|---|---|---|
| Men | 61 | (95.3) |
| Women | 1 | (1.6) |
| Overweight | 7 | (10.9) |
| Preoperative symptoms | ||
| None | 8 | (12.7) |
| Inguinal swelling | 38 | (60.3) |
| LUTS | 30 | (47.6) |
| Inguinal pain | 25 | (39.7) |
| Manual Inguino scrotal compression when voiding | 8 | (12.7) |
| Acute renal failure | 5 | (7.8) |
| Urinary retention | 3 | (4.8) |
| Preoperative imaging and results | ||
| US Positive | 16 | (25.4) |
| Negative | 1 | (1.6) |
| Not reported | 7 | (11.1) |
| CT Positive | 23 | (36.5) |
| Negative | 0 | (0) |
| Not Reported | 3 | (4.8) |
| Cystoscopy Positive | 3 | (4.8) |
| Negative | 0 | (0) |
| Not Reported | 7 | (11.1) |
| Surgical technique | ||
| Open | 37 | (80.4) |
| Laparoscopy | 3 | (6.5) |
| Robot assisted | 1 | (2.2) |
| Mesh | 16 | (34.8) |
| Post operative complications | ||
| Yes | 8 | (17.4) |
| No | 32 | (69) |
| Not Reported | 6 | (13) |
| Follow up (months) | ||
| Median | 11 | |
| Minimum–Maximum | 1–36 | |
LUTS: lower urinary tract symptoms; US: ultrasonography; CT: computerized tomography
ISH was found especially with adult men (n=61, 95.3%). Three other cases were observed in two children and one dead women during dissection.[7] Note, one of the two children was a premature infant.[8] Most of the studies didn’t provide sufficient information to conclude regarding the population-at-risk but we noticed that 7 men were overweight (10.9%).[9,10] Most patients were showing symptoms [n=49, 76.5% overweight (body mass index >30)], while others were asymptomatic and diagnosed fortuitously on imaging during cancer follow up.[11–14]
The main visual symptom of bladder hernia was inguinal swelling in 60.3% of cases (n=38).[15,16] The symptoms are very close to those usually found in classical inguinal hernia symptoms but, patients described a smaller inguinal mass after voiding and necessity of a scrotal pressure for a complete voiding in 12.7% of cases (n=8).[17–19] We also noticed that 47.6% (n=30) of patients had LUTS which could be voiding (pollakiuria) and storage symptoms (dysuria).[20,21] It was not possible to determine if LUTS was directly related to the hernia or to benign prostatic hyperplasia (BPH) since 5 mens had a medical treatment for PH.[22] Finally, pain associated with inguinal swelling was found in 39.7% of cases (n=25).[23–25]
A complicated ISH was rarely described in the literature as it was only reported with 7 patients (11.1%). Two presentations are possible: an acute renal failure (n=5) and a urinary retention (n=3). Three of renal failure was with men who had undergone a kidney transplant.[26,27] We did not notice any strangulated hernia.
2. Imaging
More than a half of symptomatic patients had imaging in emergency or a few days after (n= 27/49) (Figure 2). Many different imaging types were reported. CT-scan with or without contrast was the most frequent imaging, realised in 47.9% of cases. This highly sensitive imaging enabled hernia diagnosis, confirmed containing, and researched complication like hydronephrosis.[28–30] In 2 patients, a bladder cancer in the hernia content was discovered on the CT-scan.[31] Among the patients who had a CT-scan, 61.6% had an extra-peritoneal hernia (n=14). Otherwise, the hernia was intra-peritoneal and sometime associated with digestive structures (17.4%, n=4).[32] Two authors reported bilateral hernia, called “Mickey Mouse Sign” on CT-scan.[33,34] Sometimes, ultrasonography was realised in first intention (27%) (9) but it was coupled with cystography (29.4%) or CT-scan (35.3%).[35,36] Three patients benefited from a cystoscopy before surgery.[37,38] Cystography showed the ISH and cystoscopy demonstrated the real anatomic structure contained in the hernia before surgery.
Figure 2.
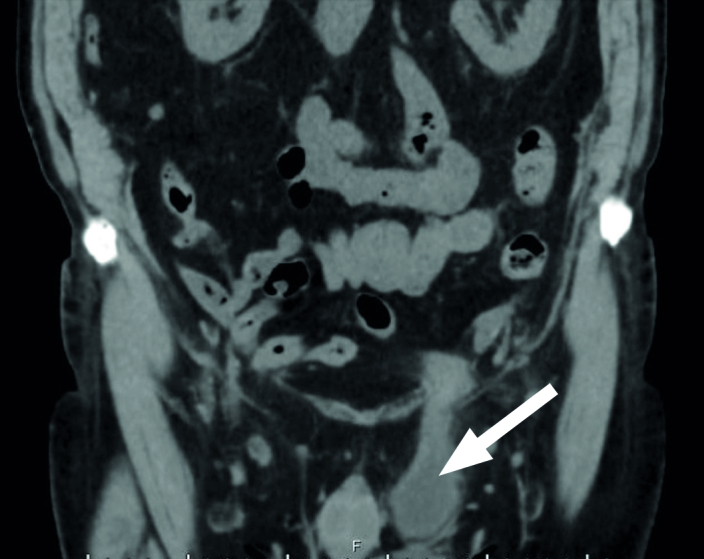
Left inguinoscrotal hernia on CT-scan without contrast
3. Treatment
The treatment of ISH of the bladder included with manual reduction in the abdominal cavity and surgical repair of the hernia. Among the 64 patients, 46 patients (71.9%) were operated on. Open surgery was the most common surgical approach performed in 80.4% (n=37) of cases. Different techniques were also used: Lichtenstein (n=15, 32.6%).[39,40], Bassini (n=7, 15.2%), Mac Way (n=2, 4.3%), Shouldice (n=1, 2.2%) (3). The technique is not reported for the other patients. Three authors described laparoscopic procedures and one robot assisted surgery.[41] Half of laparoscopic surgery was done in double team with cystoscopic control in order to decrease the risk of bladder injury.[4,29] A team reported a case of two-step repair.[32] They performed a laparoscopic reduction and a definitive Lichtenstein repair was performed a few days later.
For one patient hospitalized in intensive care unit, a transscrotal cystostomy, through the bladder hernia, was performed with iterative urinary catheter replacement.[42] Authors reported good result for this patient without urinary infection and a complete bladder drainage.
For patients with BPH and after first failure of medical treatment, transurethral resection of prostate at the time without any complication could be performed.[43]
The main complication reported ISH of the bladder repair was bladder injury occurring in 8 men and one of them had peritonitis.[44] None of these 8 patients had imaging before the surgery and the ISH of the bladder was not recognized during physical examination before surgery. Moufid et al.[4] described a bladder injury during a surgical repair because of the presence of fluid into the operative field. They performed a blue dye test through the urethral catheter to confirm the diagnosis and sutured the injury. They reported another case of bladder injury discovered the next day of surgery because of absence of urine. They did the diagnosis with CT-scan. Sarr et al.[5] reported six cases of bladder injury treated with a cystorraphy and a urethral catheter for 7 days with good results excepted for a vesicocutaneous fistula successfully treated with bladder catheterization. There was no death reported in the literature during an ISH surgical management.
Follow up varied from 3 days to 3 years. Some surgeon did only clinical examination and others completed with cystoscopy during the follow up.[9] No recurrence was reported even in patients with complications. Moreover, LUTS were improved with the surgical management of the hernia.[29]
Discussion
As expected, ISH was most of the time a direct inguinal hernia.[45] Chronic BPH, often associated with this defect and increasing the abdominal pressure, is certainly a risk factor of the occurrence of this pathology. Its clinical presentation is classical with the same signs than inguinal hernia with only digestive structures but a size reduction after voiding has to suggest the presence of the bladder in the hernia sac. In literature, it was named Mery’s sign.[46] It has to be research as intense LUTS which is present in half of the patients before reparation. Surgery complications are rare but with good evolution when they are managed quickly. Actually, imaging is not recommended in routine for inguinal hernia diagnosis. Nevertheless if there is any doubt, we recommend an imaging if a surgical management is expected. In first intention, CT-scan with contrast must be realized to prevent from several imaging and we know that CT-scan has better sensitivity for this pathology.[46] This imaging allowed confirming the presence of bladder in the inguinal hernia and anticipating possible bladder injury. Indeed, the eight patients with bladder injury had no imaging.
Oruc et al.[6] found in 2003 that less than 10% of bladder hernia were diagnosed preoperatively but in the last 10 years nearly 60% were diagnosed. We can explain that with the use of more frequent imaging in the initial evaluation of groin hernia, especially CT. And some of them were observed in imaging for cancer follow up such as scintigraphy or PET-CT.[48] This incidental findings increase the number of asymptomatic hernias.[49,50]
Only 15 patients had herniorrhaphy with the use of a mesh, whereas meshes are highly recommended for groin hernia repair to prevent the risk of recurrences. Except in those cases where the use of a mesh is not reported, one can assume that the different teams did not use a mesh because of the urinary bladder content. In case of laparoscopic hernia repair, a cystoscopic control allows decreasing the risk of bladder injury. In case of association with a bladder cancer, the hernia repair seems possible with no recurrence at 3 years. For patients with BPH and after failure of the medical treatment, it is possible to perform transurethral resection of prostate at the same time as the hernia repair without any complication. However we do not recommend prostate resection for all men with BPH as bladder reintegration can improve LUTS. Of note, to the best of our knowledge, no scientific have been publish so far about this debatable strategy coming only from our experience. The part of the bladder hernia in the LUTS occurrence is probably more important than the PH and the symptoms should be re-evaluate after inguinal surgery. For men who are asymptomatic and not motivated by surgery, waiting strategy is possible.[51]
In conclusion, ISH of the bladder is rare pathology and often unrecognised in particular during surgical hernia repair. Scrotal pressure for voiding in patients over 50 years is a specific sign of urinary bladder in the hernia. If there is any doubt, a preoperative CT-scan should be performed. In case of voluminous ISH of the bladder recognized during the surgical repair, a cystoscopy may be of interest to avoid any bladder injury. Based on this review, no new recommendation can be made about the choice of open or laparoscopic repair of IHS of the bladder or about the use of a mesh. During follow-up, the LUTS should be recognized to make the difference between a recurrence off hernia of the occurrence of new BPH symptoms.
Footnotes
Peer-review: This manuscript was prepared by the invitation of the Editorial Board and its scientific evaluation was carried out by the Editorial Board.
Author Contributions: Concept - B.B.; Design - B.B.; Supervision - B.B., P.L.; Data Collection and/or Processing - B.B.; Analysis and/or Interpretation - B.B., Y.R.; Literature Search - B.B.; Writing Manuscript - P.L., S.L.; Critical Review - Y.R., S.L.
Conflict of Interest: Authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Koontz AR. Sliding hernia of diverticula of bladder. Arch Surg. 1955;70:436–8. doi: 10.1001/archsurg.1955.01270090114025. [DOI] [PubMed] [Google Scholar]
- 2.Madden JL, Hakim S, Agorogiannis AB. The anatomy and repair of inguinal hernias. Surg Clin North Am. 1971;51:1269–92. doi: 10.1016/S0039-6109(16)39582-2. [DOI] [PubMed] [Google Scholar]
- 3.Levine B. Scrotal cystocele. JAMA. 1951;147:1439–41. doi: 10.1001/jama.1951.73670320003013a. [DOI] [PubMed] [Google Scholar]
- 4.Moufid K, Touiti D, Mohamed L. Inguinal bladder hernia: four case analyses. Rev Urol. 2013;15:32–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Sarr A, Ondo CZ, Sow Y, Fall B, Thiam A, Sine B, et al. Inguinal hernia of the bladder: about 8 cases. Pan Afr Med J. 2015;22:7. doi: 10.11604/pamj.2015.22.7.7474. https://doi.org/10.11604/pamj.2015.22.7.7474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oruç MT, Akbulut Z, Ozozan O, Coşkun F. Urological findings in inguinal hernias: a case report and review of the literature. Hernia J Hernias Abdom Wall Surg. 2004;8:76–9. doi: 10.1007/s10029-003-0157-6. [DOI] [PubMed] [Google Scholar]
- 7.Tubbs RS, Loukas M, Shoja MM, Salter EG, Oakes WJ. Indirect inguinal hernia of the urinary bladder through a persistent canal of Nuck: case report. Hernia J Hernias Abdom Wall Surg. 2007;11:287–8. doi: 10.1007/s10029-007-0192-9. [DOI] [PubMed] [Google Scholar]
- 8.Manatt S, Campbell JB, Ramji F, Kuhn A, Frimberger D. Inguinal herniation of the bladder in an infant. Can J Urol. 2006;13:3057–8. [PubMed] [Google Scholar]
- 9.Cybułka B, Podgórny M, Rapeła J, Wach A. Surgical Trap of a Routine Procedure. Scrotal Hernia with Concomitant Sliding of the Urinary Bladder – Case Report. Pol Przegl Chir. 2015;87:587–91. doi: 10.1515/pjs-2016-0007. [DOI] [PubMed] [Google Scholar]
- 10.Omari A, Alghazo M. Urinary bladder diverticulum as a content of femoral hernia: a case report and review of literature. World J Emerg Surg. 2013;8:20. doi: 10.1186/1749-7922-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park SH, Kim MJ, Kim JH, Cho AEH, Park MS, Kim KW. FDG uptake in PET by bladder hernia simulating inguinal metastasis. Yonsei Med J. 2007;48:886–90. doi: 10.3349/ymj.2007.48.5.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilgan S, Ozguven M, Emer MO, Karacalioglu AO. Massive inguinoscrotal herniation of the bladder with ureter: incidental demonstration on bone scan. Ann Nucl Med. 2007;21:371–3. doi: 10.1007/s12149-007-0024-0. [DOI] [PubMed] [Google Scholar]
- 13.Hinojosa D, Joseph UA, Wan DQ, Barron BJ. Inguinal herniationof a bladder diverticulum on PET/CT and associated complications. Clin Imaging. 2008;32:483–6. doi: 10.1016/j.clinimag.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Katsourakis A, Noussios G, Svoronos C, Alatsakis M, Chatzitheoklitos E. Direct inguinal hernia containing bladder carcinoma:A case report and review of the literature. Int J Surg Case Rep. 2014;5:180–2. doi: 10.1016/j.ijscr.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martín Hernández D, Prieto Matos P. Inguinal-scrotal bladder hernia associated with pelvic kidney. Arch Esp Urol. 2011;64:479–80. [PubMed] [Google Scholar]
- 16.Ng ACF, Leung AKC, Robson WLM. Urinary bladder calculi in asliding vesical-inguinal-scrotal hernia diagnosed preoperatively byplain abdominal radiography. Adv Ther. 2007;24:1016–9. doi: 10.1007/BF02877706. [DOI] [PubMed] [Google Scholar]
- 17.Westera J, Meyer J, Reynolds J, Lambrianides A. Massive inguinoscrotal bladder hernia. J Surg Case Rep. 2012;2012:5. doi: 10.1093/jscr/2012.5.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bjurlin MA, DeLaurentis DA, Jordan MD, Richter HM. Clinicaland radiographic findings of a sliding inguinoscrotal hernia containing the urinary bladder. Hernia. 2010;14:635–8. doi: 10.1007/s10029-009-0597-8. [DOI] [PubMed] [Google Scholar]
- 19.Gadodia A, Parshad R, Sharma R. Bladder hernia: Multidetector computed tomography findings. Indian J Urol. 2011;27:413. doi: 10.4103/0970-1591.85453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellimoottil C, Ross M, Hart ST, Milner J. Unusual Videourodynamic Finding: Massive Scrotal Cystocele. Urology. 2012;80:e53–4. doi: 10.1016/j.urology.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Helleman JN, Willemsen P, Vanderveken M, Cortvriend J, VanErps P. Incarcerated vesico-inguinal hernia: a case report. ActaChir Belg. 2009;109:815–7. doi: 10.1080/00015458.2009.11680547. [DOI] [PubMed] [Google Scholar]
- 22.Angus LDG, Cardoza S. Scrotal cystocele: a surgical pitfall. Br JHosp Med (Lond) 2008;69:594. doi: 10.12968/hmed.2008.69.10.31324. https://doi.org/10.12968/hmed.2008.69.10.31324. [DOI] [PubMed] [Google Scholar]
- 23.Tarchouli M, Ratbi MB, Bouzroud M, Aitidir B, Ait-Ali A, Bounaim A, et al. Giant inguinoscrotal hernia containing intestinalsegments and urinary bladder successfully repaired by simple hernioplasty technique: a case report. J Med Case Rep. 2015;9:276. doi: 10.1186/s13256-015-0759-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manfredelli S, Zitelli A, Pontone S, Marcantonio M, Nargi A, Forte A, et al. An inguinal bladder diverticulum Case report of arare finding in a recurrent inguinal hernia. Ann Ital Chir. 2012 pii:S2239253X12019810. [PubMed] [Google Scholar]
- 25.McKay JP, Organ M, Gallant C, French C. Inguinoscrotal hernias involving urologic organs: A case series. Can Urol Assoc J. 2014;8:E429–32. doi: 10.5489/cuaj.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coelho H, Nunes P, Canhoto C, Temido P. Inguinal hernia containingbladder and ureteroneocystostomy: a rare cause for acute renal graftdysfunction. BMJ Case Rep. 2016 doi: 10.1136/bcr-2016-214466. pii: bcr2016214466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vyas S, Chabra N, Singh SK, Khandelwal N. Inguinal herniation ofthe bladder and ureter: an unusual cause of obstructive uropathy ina transplant kidney. Saudi J Kidney Dis Transplant Off Publ SaudiCent Organ Transplant Saudi Arab. 2014;25:153–5. doi: 10.4103/1319-2442.124549. [DOI] [PubMed] [Google Scholar]
- 28.Khan A, Beckley I, Dobbins B, Rogawski K. Laparoscopic repairof massive inguinal hernia containing the urinary bladder. UrolAnn. 2014;6:159. doi: 10.4103/0974-7796.130654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karatzas A, Christodoulidis G, Spyridakis M, Stavaras C, Aravantinos E, Melekos M. A giant inguinoscrotal bladder hernia as acause of chronic renal failure: A rare case. Int J Surg Case Rep. 2013;4:345–7. doi: 10.1016/j.ijscr.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Storm DW, Drinis S. Radiographic Diagnosis of a Large InguinalHernia Involving the Urinary Bladder and Causing ObstructiveRenal Failure. Urology. 2008;72:523. doi: 10.1016/j.urology.2008.03.059. [DOI] [PubMed] [Google Scholar]
- 31.Pastor Navarro H, Martínez Ruiz J, Carrión Lopez P, Martínez Sanchíz C, Lorenzo Romero JG, Cañamares Pabolaza L, et al. Tumor inside an inguinoscrotal bladder hernia. Arch Esp Urol. 2010;63:471–6. [PubMed] [Google Scholar]
- 32.Kramer BA, Minnis JG, Schwartz BF. Large bladder diverticulum presenting as an inguinal hernia. Can J Urol. 2009;16:4946–7. [PubMed] [Google Scholar]
- 33.Sabharwal S, Kekre N, Sagar A. Bilateral vesical inguinal hernia: A perineal ‘Mickey mouse’. Indian J Urol. 2013;29:154. doi: 10.4103/0970-1591.114043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Indiran V. Bilateral Inguinal Hernia Containing Urinary Bladder as Sole Content With ‘Pelvic Mickey Mouse Sign’. Urology. 2016;90:e5–6. doi: 10.1016/j.urology.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 35.Frenkel A, Roy-Shapira A, Shelef I, Shaked G, Brotfain E, Koyfman L, et al. Inguinal Herniation of the Urinary Bladder Presenting as Recurrent Urinary Retention. Case Rep Surg. 2015:1–3. doi: 10.1155/2015/531021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marquez Moreno AJ, Martin Diego A, Heras Joaquin del P, Palanca Alberto M, Villalta Emilio J, Rebollo Celestino G. Images in urology. Inguinoscrotal bladder hernia: multidetector CT scan reconstruction. Arch Esp Urol. 2010;63:565–6. [PubMed] [Google Scholar]
- 37.Cruz Guerra NA, Albarrán Fernández M, Porto Sierra M, Tarroc Blanco A. Giant bladder hernia associated with bilateral incipient obstructive uropathy. Arch Esp Urol. 2005;58:669–71. doi: 10.4321/S0004-06142005000700012. [DOI] [PubMed] [Google Scholar]
- 38.Uchio EM, Calderon JS, Hwang JJ. Laparoscopic Repair of Inguinal Cystocele Using Cystoscopic Light Test. Urology. 2012;79:725–7. doi: 10.1016/j.urology.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 39.Christmas AB, Honaker D. Incarcerated massive sliding hernia treated with bladder resection and mesh repair. Am Surg. 2015;81:E123–4. [PubMed] [Google Scholar]
- 40.Kim KH, Kim MU, Jeong WJ, Lee YS, Kim KH, Park KK, et al. Incidentally Detected Inguinoscrotal Bladder Hernia. Korean J Urol. 2011;52:71. doi: 10.4111/kju.2011.52.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kawaguchi T, Itoh T, Yoshii K, Otsuji E. Laparoscopic repair of a bilateral internal inguinal hernia with supravesical hernia – a case report. Int J Surg Case Rep. 2015;14:108–11. doi: 10.1016/j.ijscr.2015.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ryan ST, Jumper B. Scrotal Cystocele Managed With Trans-scrotal Neocystostomy Tube. Urol Case Rep. 2015;3:117–9. doi: 10.1016/j.eucr.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goyal S, Shrivastva M, Verma RK, Goyal S. ‘Uncommon Contents of Inguinal Hernial Sac’: A Surgical Dilemma. Indian J Surg. 2015;77:305–9. doi: 10.1007/s12262-013-0806-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ko PJ, Lin HY, Lin WH, Lai HS. Sliding inguinal hernia with incarceration of urinary bladder diverticulum in a child. Int Surg. 2010;95:335–7. [PubMed] [Google Scholar]
- 45.Watson LF. Hernia. Saint-Louis: Mosby; 1948. [Google Scholar]
- 46.Gomella LG, Spires SM, Burton JM. The surgical implications of herniation of the urinary bladder. Arch Surg. 1985;120:964–7. doi: 10.1001/archsurg.1985.01390320084018. [DOI] [PubMed] [Google Scholar]
- 47.Dass K, Daloul R, Gupta P. Water under the bridge: a rare case of scrotal cystocele. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-200239. pii: bcr2013200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Durán Barquero C, Serrano Vicente J, García Bernardo L, Domínguez Grande ML, Rayo Madrid JI, Infante de la Torre JR, et al. Herniación inguinal de un divertículo vesical, diagnosticada con PET-TAC. Rev Esp Med Nucl. 2010;29:36–7. doi: 10.1016/j.remn.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 49.Ogul H, Yuce I, Eren S, Kantarci M. Bilateral inguinal hernia with uncommon content. Can J Gastroenterol J Can Gastroenterol. 2013;27:14. doi: 10.1155/2013/873702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shizukuishi T. inguinal bladder hernia: multi-planar reformation and 3-D reconstruction computed tomography images useful for diagnosis. Nephrology. 2009;14:263. doi: 10.1111/j.1440-1797.2008.01063.x. [DOI] [PubMed] [Google Scholar]
- 51.Fuerxer F, Brunner P, Cucchi JM, Mourou MY, Bruneton JN. Inguinal herniation of a bladder diverticulum. Clin Imaging. 2006;30:354–6. doi: 10.1016/j.clinimag.2006.03.001. [DOI] [PubMed] [Google Scholar]


